Abstract
Background
Femoral neck fractures (FNFs) in young adults are usually caused by high-energy trauma, and their treatment remains a challenging issue for orthopedic surgeons. The quality of reduction is considered an important factor in improving the poor prognosis of patients with FNFs. In recent years, positive buttress closed reduction technique has received widespread attention in the treatment of FNFs. This comprehensive literature review is designed to encapsulate the impacts of both non-anatomic and anatomic reduction on the biomechanical stability, clinical outcomes, and postoperative complications in the management of FNFs, conjecture the efficacy of positively braced reduction techniques and provide a thorough summarization of the clinical outcomes.
Methods
In this literature review, we have examined all clinical and biomechanical studies related to the treatment of FNFs using non-anatomical reduction or positive and negative buttress reduction. PubMed, Web of Science, Google Scholar and Embase Library databases were searched systematically for studies published before September 1, 2023. Published literature on fracture reduction techniques for treating FNFs was reviewed. In addition, we evaluated the included literature using the MINORs tool.
Results
Although the “arch bridge” structure formed by the positive buttress reduction technique improved the support to the cortical bone and provided a more stable biomechanical structure, no significant differences were noted in the clinical efficacy and incidence of postoperative complications between the positive buttress reduction and anatomical reduction.
Conclusion
Positive buttress reduction is an effective treatment method for young patients with FNFs. When facing difficult-to-reduce FNF, positive buttress reduction should be considered first, followed by anatomical reduction. However, negative buttress reduction should be avoided.
Similar content being viewed by others
Introduction
As a result of an aging population, the number of people with hip fractures continues to increase and is expected to reach 63 million by 2050 [1, 2]. Most (54%) of the fractures occur in the neck of the femur [3]. The incidence of femoral neck fractures (FNFs) in middle-aged and young people is also on the increase [4]. FNFs in young adults are usually caused by high-energy trauma, which may involve displaced fracture patterns, leading to instability at the fracture site [5]. The treatment of these injuries remains a challenging issue for orthopedic surgeons [6, 7]. The vascular supply to bone is often damaged in displaced FNFs. As a result, displaced FNFs are often accompanied by a high rate of complications, including nonunion and osteonecrosis of the femoral head (ONFH) [8, 9].
The treatment of displaced FNFs often necessitates surgical intervention and comprehensive rehabilitation to restore mobility and function. Anatomical reduction is a common surgical technique used to realign fractured or dislocated bones and can be executed through an open or closed surgical approach. The fracture reduction technique aims to maximize the contact between the surface of the fractured ends to promote bone healing. In addition, it should also avoid excessive repeat reductions and the twisting of the intra-articular capsule artery to reduce the risk of damaging the blood supply [10,11,12]. However, the efficacy of this technique heavily relies on the surgeon’s experience. Moreover, anatomical reduction can not always be achieved, particularly in complex commuted fractures. Failure to achieve anatomical reduction can increase the risk of adverse events after surgery [13,14,15,16]. Unfortunately, postoperative complications such as nonunion, internal fixation failure, ONFH, infection, and nerve paralysis are common after FNFs reduction surgery, particularly in young people [17]. The risk of postoperative complications can increase if poor bone alignment is not detected. Poor alignment is more difficult to detect during closed reduction surgery. Immediate postoperative computed tomography scanning and three-dimensional reconstruction could be used to assess the quality of the reduction and reduce the risk of post-surgical complications. However, not all hospitals have the facilities to perform postoperative scanning.
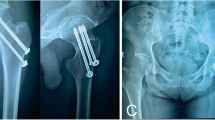
Non-anatomical reduction involves realigning the bone segments without necessarily restoring them to their original anatomical position. In 2012, Gotfried et al. introduced the non-anatomical closed positive and negative buttress reduction techniques to treat young patients with FNFs [18]. The term “positive buttress reduction mode” (Fig. 1C) refers to the situation where the proximal medial cortex of a FNF is located above the distal medial cortex on the outside, meaning that the distal medial cortex of the FNF protrudes towards the inner lower edge of the proximal end compared to an anatomical reduction (Fig. 1B). In contrast, in the “negative buttress reduction mode” (Fig. 1A), the proximal medial cortex of a FNF is located above the distal medial cortex on the inside, meaning that the proximal medial cortex of the FNF protrudes towards the inner upper edge of the distal end compared to an anatomical reduction (Fig. 1B). Intraoperative or postoperative anteroposterior X-rays of the hip joint are used to determine whether a positive reduction has been achieved [19]. However, to our knowledge, very few comprehensive literature reviews have been conducted evaluating the efficacy of the positive buttress reduction surgical technique for FNFs. Therefore, this comprehensive literature review is designed to encapsulate the impacts of both non-anatomic and anatomic reduction on the biomechanical stability, clinical outcomes, and postoperative complications in the management of FNFs, conjecture the efficacy of positively braced reduction techniques and provide a thorough summarization of the clinical outcomes.
Materials and methods
Literature search
Details of the literature search process are shown in Fig. 2. The PubMed, Web of Science, Google Scholar, and Embase electronic database-s were searched to identify research articles comparing the biomechanical implants used to perform non-anatomical reduction for FNF and the clinical outcome of the different techniques. The following keywords were used to search for relevant articles “hip” OR “femur” OR “femoral” OR “femoral neck”) AND (fracture) AND (“anatomical” OR “anatomy” OR “positive” OR “negative” OR “Non-anatomical”) AND (reduction). All articles published before 2023 with no language restrictions were included in this literature review.
Methodological quality of studies
The methodological quality of studies was assessed using the methodological index for non-randomized studies (MINORS) criteria [20], of which the first 8 criteria were used for all studies and all 12 for comparative studies. These outcomes are all displayed in Table 1. The level of evidence of all studies was assessed using the Oxford Centre for Evidence-Based Medicine (adjusted) [21].
Results
Characteristics of the studies
A total of 16 relevant studies were retrieved, of which 11 evaluated the clinical efficacy and 6 evaluated the biomechanics. Most studies evaluated the clinical efficacy of different reduction techniques in young patients (< 65 years old) with FNFs during and after closed reduction and internal fixation. Various implants were used to fix the fractures, including percutaneous compression plates (PCCP), cannulated screws (CS), dynamic hip screws (DHS) and derotation screws (DS), and femoral neck system (FNS). In the study of biomechanics, the implants model included cannulated screws (CS), dynamic hip screws (DHS) and derotation screws (DS), femoral neck system (FNS), and physiological hip nail (PHN) by three-dimensional finite element modeling. The summary information is presented in Tables 2 and 3.
Metrics used to assess the clinical outcomes post-surgery
The incidences of complications post-surgery, including ONFH, shortening (femoral neck shortening exceeding 5 cm [22]) and displacement (changes in neck-shaft angle exceeding 10° [23]) of the femoral neck, nonunion, infection, and postoperative fractures, were assessed in most studies. In addition, most studies used the Harris Hip score to evaluate the outcomes and function of the patient’s hip joint after surgery [24]. The Harris Hip Score consists of a series of questions and physical assessments, with a total score ranging from 0 to 100 points. Higher scores indicate better hip function and less pain.
Hip function score post-surgery
A total of 11 studies, including 1032 young patients with unilateral FNF, were evaluated. Among them, 373 had positive buttress reduction, 406 had anatomical reduction, and 253 had negative buttress reduction. Table 4 provide a summary of the postoperative complications. The majority of the patients were followed up for more than one year. None of the studies identified a statistical difference in the Harris hip score one year after surgery between patients treated with positive buttress reduction and anatomical reduction [25]. However, in some studies, patients treated with positive buttress reduction had a higher rate of excellent Harris scores (> 80 points) than those treated with anatomical reduction [26, 27] (P < 0.05). The patients treated with positive buttress reduction and anatomical reduction had a better Harris hip score than those treated with negative buttress reduction (P < 0.05) [28,29,30,31,32,33].
Incidence of postoperative complications
Most research results found no significant difference in the incidence of complications between the positive buttress reduction group and the anatomical reduction group (P > 0.05). Conversely, the negative buttress reduction group had a significantly higher incidence of postoperative complications than the positive buttress reduction and anatomical reduction groups (P > 0.05) [23, 28,29,30,31,32,33,34,35]. Some research studies reported a lower incidence of ONFH, shortening and displacement of the femoral neck, and fracture nonunion complications in the positive buttress reduction group when compared with the anatomical reduction group [26, 27]. However, it’s important to note that the difference in the incidence of fracture nonunion was not statistically significant between the 2 groups, possibly due to the limited sample size. (P > 0.05) [23, 26, 27, 31, 34, 35]. The summary information is presented in Table 4.
Biomechanical evaluation
The postoperative effect is inseparable from the biomechanical performance of the internal fixator. At present, most biomechanical studies use finite element analysis, which directly reflects the stability of the model by measuring the maximum displacement value and maximum stress value of the fracture end under external load. The smaller the displacement value, the more solid the fixation [36]. The stress cloud map can reflect the situation of stress transmission when force is applied to the corresponding part. The summary information is presented in Table 3.
Although the internal fixation methods used to develop biomechanical 3D models varied widely between studies, they all reached similar conclusions. Compared to negative buttress reduction, the positive buttress reduction technique resulted in better stability, stress transmission, biomechanical performance, and safer internal fixation [37, 38]. However, there is still controversy about whether positive buttress reduction or anatomical reduction is better. So far, biomechanical performance studies comparing positive buttress reduction in relation to anatomical reduction showed that the biomechanical performance brought by positive buttress reduction (displacement 0-2 mm) is closest to anatomical reduction [38,39,40]. In the positive buttress reduction (displacement 2 mm ) mode, the screws bear less stress, indicating that the medial cortex can disperse some screw stress in positive buttress reduction mode [39, 41]. If the displacement is too large, it will weaken the mechanical advantage of positive buttress mode and even approach negative buttress [38,39,40].
Wang et al. [39] proposed a four-tier classification to guide positive buttress reduction mode based on the extent of displacement whereby grade 1 includes displacement from 0 to 2 mm, grade II includes displacement in the range of 2–3 mm, grade III includes displacement ranging from 3 to 4 mm and grade IV includes displacement exceeding 4 mm. Studies have shown that in cases where anatomical reduction is not feasible, positive buttress reduction grade I can achieve biomechanical effects similar to anatomical reduction for FNF. And then positive buttress reduction grade II is a relatively acceptable range. However, the use of positive buttress reduction Grade III and IV for displaced FNF is not recommended. In addition, Wang et al. [42] found that Gotfried positive buttress reduction was more effective than open precision reduction and Gotfried negative buttress reduction for bone healing and blood supply recovery in rabbits with FNFs, but the bone growth capacity of open precision reduction is greater than that of Gotfried positive buttress reduction.
Jia et al. [38] and Fan et al. [40] showed that the biomechanical performance of positive buttress reduction was also related to the angle of inclination of the FNF in relation to the femoral shaft, also known as the Pauwels angle. For Pauwels type I fractures (below 30°), the biomechanical performance of positive buttress reduction was very close to that of the anatomical reduction. However, as the Pauwels angle increases, the mechanical performance of positive buttress reduction gradually weakens [38, 40]. Eventually, for Pauwels type III fractures (above 70°), anatomical reduction provided better stability than positive buttress reduction.
Discussion
Anatomical reduction and rigid internal fixation have been considered the treatment of choice for decades for young patients (below 65 years) with displaced and unstable FNFs [43, 44]. However, in cases of complex commuted fractures, closed surgical anatomical reduction is not always possible [39]. Positive buttress reduction can provide an alternative reasoning to the reduction of FNF. However, it is important to note that despite the growing interest in the Gotfried positive buttress reduction technique, there appears to be a noticeable gap in comprehensive literature reviews and systematic evaluations of its clinical efficacy and biomechanical stability. Therefore, in this literature review, we aimed to evaluate the clinical efficacy and biomechanical properties of the positive buttress reduction technique in relation to anatomical reduction techniques for FNF.
Development and clinical efficacy of the positive buttress reduction method
The objective of Gotfried positive buttress reduction is to align the bones to attain a line measuring between 160° to 180° on the hip joint lateral X-ray, with both the proximal and distal fracture ends aligning with the positive buttress position on the hip joint anterior X-ray. Simultaneously, the femoral neck-shaft angle should demonstrate a minimum of 135° with external rotation. Studies have found [38,39,40] that the biomechanical performance, safety of the internal fixator implantation, and reliability of the postoperative fracture alignment of positive buttress reduction (displacements ranging between 0 and 2 mm) are similar to those obtained following anatomical reduction. Positive buttress reduction with a displacement within 2 mm joint a fixed nail system can provide stable mechanical fixation in displaced FNF that can not be fixed with anatomical reduction. However, negative buttress reduction should be avoided whenever possible. Moreover, compared with anatomical reduction, the positive buttress reduction technique has demonstrated favorable clinical outcomes, characterized by swift recovery of hip joint function and a reduced or comparable incidence of postoperative complications, including femoral neck shortening and ONFH. Consequently, based on the findings of this literature review we suggest that, for FNF, positive buttress reduction can be the first choice, followed by anatomical reduction. Conversely, using negative buttress reduction is discouraged, and patients should receive dependable internal fixation instead.
Stability of the positive buttress reduction post-surgery
Irrespective of the quality of the anatomical reduction, during the healing process, bone absorption and shear force at the fracture site may still cause secondary sliding and displacement, leading to shortening of the femoral neck and reduction of the neck-shaft angle. It is well known that an important predictive indicator of failure after surgery is the bending displacement of the femoral neck [45]. Positive buttress reduction can effectively avoid the negative effects of bone absorption and shear force by improving the bone support at the fracture site. During the positive buttress reduction procedure, the inner cortex of the proximal head and neck bone block of the fracture is positioned on the outer and upper side of the inner cortex of the distal fracture. A lateral displacement is then applied so that the cortices at both ends of the fracture come into contact with each other to eventually form a small arch-like step that helps distribute some of the stress from above. Additionally, the head and neck region receives added support from the inner cortex of the femoral neck, thus reducing excessive displacement of the proximal fracture end. These arrangements eventually maintain a stable cortical-to-cortical configuration, reducing the risk of bone displacement post-surgery [41]. Conversely, during anatomical reduction, the head and neck fragments are only supported by fixation screws, and no support is received from the inner cortex of the femoral neck. As a result, positive buttress reduction can establish a more stable structural alignment and reduce the risk of femoral neck shortening while preserving the neck-shaft angle.
Adaptation of the positive buttress reduction technique based on fracture location
In FNFs or intertrochanteric fractures, positive buttress reduction has a different application. A prerequisite for the performance of Gotfried positive buttress reduction is a head and neck bone block located on the outside of the inner cortex of the distal femur. However, while this approach works well for FNF, it may not be suitable for intertrochanteric fractures. In view of this, Zhang et al. [46] first proposed that in the reduction of intertrochanteric fractures, the position of the buttresses is altered so that the inner cortex of the proximal head and neck bone block is situated on the inside of the inner cortex of the distal femur to form the positive buttress. Conversely, the inner cortex of the proximal head and neck bone block is positioned on the outside of the inner cortex of the distal femur to form the negative buttress. Moreover, it is important to note that the mechanical forces of the hip post-surgery vary between FNF and intertrochanteric fractures [47, 48]. In FNF, the vertical shear force is the main factor affecting fracture stability. In contrast, the shear force and hip joint internal rotation coexist in intertrochanteric fractures due to the long proximal lever arm. Therefore, in order to obtain a secondary stable sitting at the fracture end, the surgical management of these 2 types of fractures requires different strategies. In FNF, an uplifting force should be applied to the proximal cortical bone against the distal cortical bone to prevent downward movement. This technique is known as uplifting reduction. However, for intertrochanteric fractures, a push-out force should be applied to the proximal cortical bone to prevent inward displacement of the proximal bone block. This approach is known as push-out reduction.
Conclusion
The Gotfried positive buttress reduction mode is an effective treatment strategy for young patients with FNF. However, most of the current clinical efficacy analysis studies on positive buttress reduction are based on small retrospective studies with a primary emphasis on using hollow nails as the chosen internal fixation method in positive buttress reduction procedures. Therefore, larger prospective multicenter studies are required to confirm the efficacy of this technique. Moreover, additional research is required to compare the efficacy of different fixation methods.
Data availability
Not applicable.
Abbreviations
- PBR :
-
positive buttress reduction
- AR :
-
anatomical reduction
- NBR :
-
negative buttress reduction
- FNFs :
-
femoral neck fractures
- ONFH :
-
osteonecrosis of the femoral head
- DHS :
-
dynamic hip screws
- CS :
-
cannulated screws
- PCCP :
-
percutaneous compression plates
- DS :
-
derotation screws
- FNS :
-
femoral neck system
- PHN :
-
physiological hip nail
References
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22(5):1277–88.
Quaranta M, Miranda L, Oliva F, Migliorini F, Pezzuti G, Maffulli N. Haemoglobin and transfusions in elderly patients with hip fractures: the effect of a dedicated orthogeriatrician. J Orthop Surg Res. 2021;16(1):387.
Rogmark C, Leonardsson O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Joint J. 2016;98–b(3):291–7.
Wan L, Zhang X, Wu D, Li Z, Yuan D, Li J, et al. Application of Robot Positioning for Cannulated Screw Internal Fixation in the treatment of femoral Neck fracture: Retrospective Study. JMIR Med Inf. 2021;9(1):e24164.
Yang JJ, Lin LC, Chao KH, Chuang SY, Wu CC, Yeh TT, et al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J bone Joint surgery-american Volume. 2013;95(1):61–9.
Huang TW, Hsu WH, Peng KT, Lee CY. Effect of integrity of the posterior cortex in displaced femoral neck fractures on outcome after surgical fixation in young adults. Injury-international J care Injured. 2011;42(2):217–22.
Maffulli N, Aicale R. Proximal femoral fractures in the Elderly: a few things to know, and some to forget. Med (Kaunas Lithuania). 2022;58(10).
Porubský P, Trč T, Havlas V, Smetana P. [Avascular necrosis of the femoral head]. Casopís lékar̆ů c̆eských. 2016;155(8):423–6.
Ma JX, He WW, Zhao J, Kuang MJ, Bai HH, Sun L, et al. Bone microarchitecture and biomechanics of the necrotic femoral head. Sci Rep. 2017;7(1):13345.
Beltran MJ, Collinge CA, Gardner MJ. Stress modulation of fracture fixation implants. J Am Acad Orthop Surg. 2016;24(10):711–9.
Lindtner RA, Kammerlander C, Goetzen M, Keiler A, Malekzadeh D, Krappinger D, et al. Fracture reduction by postoperative mobilisation for the treatment of hyperextension injuries of the thoracolumbar spine in patients with ankylosing spinal disorders. Arch Orthop Trauma Surg. 2017;137(4):531–41.
Xue W, Guan XL, Wang ZP, Liu L. [Treatment of displaced femoral neck fracture in young adults with close reduction and femoral neck locking plate fixation]. Zhongguo Gu shang = China J Orthop Traumatol. 2016;29(7):645–7.
Su Y, Chen W, Zhang Q, Li B, Li Z, Guo M, et al. An irreducible variant of femoral neck fracture: a minimally traumatic reduction technique. Injury-international J care Injured. 2011;42(2):140–5.
Zhuang L, Wang L, Xu D, Wang Z. Anteromedial femoral neck plate with cannulated screws for the treatment of irreducible displaced femoral neck fracture in young patients: a preliminary study. Eur J Trauma Emerg Surg. 2019;45(6):995–1002.
Pei F, Zhao R, Li F, Chen X, Guo K, Zhu L. Osteonecrosis of femoral head in young patients with femoral neck fracture: a retrospective study of 250 patients followed for average of 7.5 years. J Orthop Surg Res. 2020;15(1):238.
Wang T, Sun JY, Zha GC, Jiang T, You ZJ, Yuan DJ. Analysis of risk factors for femoral head necrosis after internal fixation in femoral neck fractures. Orthopedics. 2014;37(12):e1117–23.
Cui L, Zhao S, Tian H, Guo W, Dong X. Curative efficacy of surgical procedures for older patients with femoral neck fracture: a network meta-analysis and systematic review. J Orthop Surg Res. 2022;17(1):127.
Gotfried Y. The Gotfried (Nonanatomic, closed) reduction of unstable subcapital femoral fractures. Techniques Orthop. 2012;27:259–61.
Gotfried Y, Kovalenko S, Fuchs D. Nonanatomical reduction of displaced subcapital femoral fractures (gotfried reduction). J Orthop Trauma. 2013;27(11):e254–9.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;9:73.
Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the Journal. JBJS. 2003;85(1):1–3.
Zlowodzki M, Ayeni O, Ayieni O, Petrisor BA, Bhandari M. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J trauma-injury Infect Crit care. 2008;64(1):163–9.
Xiong WF, Chang SM, Zhang YQ, Hu SJ, Du SC. Inferior calcar buttress reduction pattern for displaced femoral neck fractures in young adults: a preliminary report and an effective alternative. J Orthop Surg Res. 2019;14(1):70.
Mahomed NN, Arndt DC, McGrory BJ, Harris WH. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty. 2001;16(5):575–80.
Chen YP, Kuo YJ, Hung SW, Wen TW, Chien PC, Chiang MH, et al. Loss of skeletal muscle mass can be predicted by Sarcopenia and reflects poor functional recovery at one year after surgery for geriatric hip fractures. Injury-international J care Injured. 2021;52(11):3446–52.
LS T. Long-term follow-up observation of anatomical reduction and Gotfried support reduction for femoral neck fractures in young people. Chin J Mod Med. 2018;20(01):26–9.
Zhu J, Li Y, Zhang Y, Cheng X. Clinical outcome and biomechanical analysis of dynamic hip screw combined with Derotation Screw in treating displaced femoral Neck fractures based on different reduction qualities in young patients (≤ 65 years of age). Biomed Res Int. 2022;2022:9505667.
Lu YGFJ. The effect of gotfried support reduction combined with internal fixation on hip joint function and hemodynamics in young and middle-aged patients with femoral neck fractures. Chin J Mod Med. 2017;27(24):96–100.
Ding SCYY, Ge YL, et al. Short-term efficacy of Gotfried positive support reduction combined with hollow screw internal fixation in the treatment of femoral neck fractures in young and middle-aged people. Chin J Trauma Orthop. 2016;18(8):655–61.
Huang K, Fang X, Li G, Yue J. Assessing the effect of Gotfried reduction with positive buttress pattern in the young femoral neck fracture. J Orthop Surg Res. 2020;15(1):511.
Zhao G, Liu M, Li B, Sun H, Wei B. Clinical observation and finite element analysis of cannulated screw internal fixation in the treatment of femoral neck fracture based on different reduction quality. J Orthop Surg Res. 2021;16(1):450.
Yang L, Mo G, Xu L, Li Y, Ruan S. [Study on effectiveness of treating femoral neck fractures based on theory of positive support]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi = Zhongguo Xiufu chongjian waike zazhi = Chinese. J Reparative Reconstr Surg. 2023;37(8):958–63.
Jiang Q, Liu Y, Bai X, Deng Y, Cao Y, Yu C, et al. Nonanatomical reduction of femoral neck fractures in young patients treated with femoral neck system: a retrospective cohort study. BMC Musculoskelet Disord. 2023;24(1):412.
Zhao G, Liu C, Chen K, Lyu J, Chen J, Shi J, et al. Nonanatomical reduction of femoral Neck fractures in Young patients (≤ 65 years old) with internal fixation using three parallel cannulated screws. Biomed Res Int. 2021;2021:3069129.
Li LT, He RF, Wang YB. Analysis of hip joint function, biomechanics and complications in the treatment of femoral neck fractures in young and middle-aged people with Gotfried positive support reduction combined with percutaneous compression plate. Heilongjiang Med. 2022;46(06):648–51.
Samsami S, Augat P, Rouhi G. Stability of femoral neck fracture fixation: a finite element analysis. Proc Institution Mech Eng part h-journal en. 2019;233(9):892–900.
Zheng X, Xu JH, Huang JR. Finite element analysis of two kinds of non-anatomical reduction internal fixation for Pauwels type III subcapital femoral neck fractures. Chin J Clin Anat. 2017;35(06):665–70.
Jia JZ, Yin GK, Xie H, Fu WM, Han S. Finite element analysis of femoral neck system internal fixation for femoral neck fracture under non-anatomical reduction. Chin J Tissue Eng Res. 2024;28(21):3319–25.
Wang G, Wang B, Tang Y, Yang HL. A quantitative biomechanical study of positive buttress techniques for femoral neck fractures: a finite element analysis. Chin Med J. 2019;132(21):2588–93.
Fan Z, Chen P, Yu X, Li X, Su H, Chen H, et al. Biomechanical study of femoral neck system for young patients with nonanatomically reduced femoral neck fractures: a finite element. BMC Musculoskelet Disord. 2023;24(1):54.
Zhang YQ, Chang SM. Mechanism of Gotfried reduction in femoral neck fracture. J Orthop Trauma. 2013;27(12):e291.
Wang G, Wang B, Wu X, Yang H. Gotfried positive reduction promotes the repair of femoral neck fracture potentially via enhancing osteogenesis and angiogenesis. Biomed Pharmacother. 2020;123:109801.
Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121–9.
MS. Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. Lancet. 2017;389(10078):1519–27.
Krischak G, Beck A, Wachter N, Jakob R, Kinzl L, Suger G. Relevance of primary reduction for the clinical outcome of femoral neck fractures treated with cancellous screws. Arch Orthop Trauma Surg. 2003;123(8):404–9.
Zhang SM, Zhang YQ, Lin Q, Du SC. The effect of medial cortical positive support reduction on the internal fixation of elderly intertrochanteric femoral fractures Chinese. J Orthop. 2014;22(14):1256–61.
Gargano G, Poeta N, Oliva F, Migliorini F, Maffulli N. Zimmer Natural Nail and ELOS nails in pertrochanteric fractures. J Orthop Surg Res. 2021;16(1):509.
Marsillo E, Pintore A, Asparago G, Oliva F, Maffulli N. Cephalomedullary nailing for reverse oblique intertrochanteric fractures 31A3 (AO/OTA). Orthop Rev. 2022;14(6):38560.
Acknowledgements
We are grateful to all participating patients.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
S-H performed a literature search and was a major contributor in writing the manuscript; ZY-Z was a major contributor in writing the manuscript; K-Z, GK-Y, and YC-L were contributors in writing the manuscript; BJ-W and Z-W was responsible for reviewing and editing the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Affiliated Zhongshan Hospital of Dalian University.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Han, S., Zhang, ZY., Zhou, K. et al. Positive buttress reduction in femoral neck fractures: a literature review. J Orthop Surg Res 19, 262 (2024). https://doi.org/10.1186/s13018-024-04649-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04649-4