Abstract
Background
High-performance total hip arthroplasty (THA) depends on the accurate position of components. However, femoral anteversion is variable, and current studies only used traditional instruments to evaluate it, such as protractor and spirit level with limited cases. This study aimed to identify the variability in the measured femoral native anteversion and intraoperative stem anteversion under different measurement methods, including intraoperative robotic method. We hypothesized that robotic technology was more accurate than traditional instruments for femoral anteversion evaluation.
Methods
This study included 117 hips of patients who underwent robotic-assisted THA between November 2019 and March 2021. Preoperative native femoral anteversion was measured using a robotic system. Intraoperative femoral stem anteversion was evaluated visually, and then measured with a goniometer and a robotic system, respectively. Variability in the measured femoral native anteversion and intraoperative femoral stem anteversion was calculated and compared. Intraclass correlation coefficient (ICC) and Pearson correlation analysis were used to assess the consistency and correlation of anteversion of different measurements and postoperative CT-measured stem anteversion, respectively.
Results
The result of measurement for preoperative native femoral anteversion was more variable than the intraoperative robotic-measured stem anteversion. Intraoperative robotic-measured stem version showed the highest correlation with postoperative CT measurement of stem version (r = 0.806, P < 0.001), while intraoperative surgeon estimation had the lowest correlation coefficient (r = 0.281, P = 0.025). As for the consistency with postoperative CT measurement of femoral stem anteversion, the intraoperative robotic-measured femoral stem version also had the highest value (ICC = 0.892, P < 0.001).
Conclusion
Native femoral anteversion was variable preoperatively. Using cementless stems, anteversion was also highly variable. Robotic assessment for stem anteversion during surgery was more consistent with the final position than the preoperative assessment and conventional intraoperative estimation.
Similar content being viewed by others
Introduction
Minimizing the dislocation rate after total hip arthroplasty (THA) largely depends on the accurate positioning of the components [1,2,3]. Suboptimal placement of the acetabular component or femoral stem may increase polyethylene wear, resulting in instability or even aseptic loosening [4,5,6]. Among the parameters of component position, anteversion is of great value because it could help avoid impingement during hip motion, which is required for activities in daily living [7]. Previously, Jolles et al. found that the dislocation rate was 6.9 times higher if the total anteversion (the sum of cup anteversion and stem anteversion) was outside of a range of 40°–60° [8]. With further understanding of the mechanism of spinopelvic motion, the problem of acetabular anteversion has been emphasized dynamically, not only in the standing position, but also in the sitting position [9, 10]. Tezuka et al. believed that hip dislocation was related to the combined sagittal index (CSI), which is the sum of ante-inclination and pelvic femoral angle [11]. However, CSI was related to acetabular anteversion, and pelvic femoral angle was related to hip flexion, while femoral anteversion was ignored.
Femoral anteversion is an important component of the concept of "combined version," which was initially proposed by Mckibbin [12]. Excessive femoral anteversion may induce posterior impingement and anterior dislocation of the hip when the hip extends. In contrast, inadequate femoral anteversion or retroversion may result in anterior impingement and posterior dislocation of the hip when the hip flexes [13]. Padgett emphasized the importance of femoral anteversion in THA stability, which cannot be fully compensated by acetabular anteversion [14]. This theory is further demonstrated using a mathematical model [15]. However, femoral anteversion is variable, and it was demonstrated by Reikeras et al. [16], in which the femoral version ranged from 17° of retroversion to 60° of anteversion using CT to measure anteversion. Park et al. studied the variation from preoperative CT to postoperative femoral anteversion and found that the difference was from 2.3° to 9.4° [17]. Hirata et al. even found that the results of femoral anteversion measured using a goniometer during surgery are different from those measured by postoperative CT scans [18]. Recently, the application of robotic-assisted THA has enabled surgeons to evaluate femoral anteversion during surgery accurately, which may be a potentially promising accurate technology [14]. However, few studies have reported on the variation of the femoral anteversion angle during robotic-assisted THA [19, 20]. Nodzo et al. assessed the accuracy of femoral anteversion using a robotic system, but the number of subjects included in this study was limited to 20 patients [21]. Until now, no studies have compared the accuracy of different evaluation methods for femoral anteversion during surgery, including robotic-assisted technology.
This study aimed to identify the variability in the measured femoral native anteversion (FNA) and intraoperative stem anteversion in our cohort of patients, and to answer whether robotic technology was more accurate than traditional instruments for evaluation of femoral anteversion. We hypothesized that there exists a wide range of FNA, and robotic-assisted THA would be a more accurate approach for the evaluation of stem anteversion.
Material and methods
Study design and participants
This study was approved by the institutional review board. Patients who underwent robotic-assisted THA between November 2019 and March 2021 were retrospectively included in this study. The exclusion criteria were intraoperative abortion of robotic surgery, intraoperative loosening of the screw anchoring the infrared trackers on the femoral side, and subtrochanteric or extended greater trochanter osteotomy of the femur. Finally, 117 hips of patients were included in our study. Among these, 64 hips had postoperative CT scans for other study programs to assess the position of acetabular components. Demographic data are summarized in Table 1.
Preoperative planning and measurement of femoral anteversion
All patients who underwent robotic-assisted THA (MAKO Stryker Inc., Fort Lauderdale, FL, USA) underwent a CT scan (Toshiba 320; 0.5 mm for pelvis and 2.0 mm for knee) for preoperative planning. Preoperative femoral anteversion was measured on the Mako workstation, which was the angle formed by the projection of the line connecting the femoral head center and femoral neck center with the line of the surgical epicondylar axis on the transverse plane when the patient's thigh was adjusted to parallel the longitudinal axis of the body.
Surgical technique and intraoperative measurement of stem anteversion
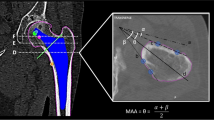
All surgical procedures were performed by three surgeons (Drs Yixin Zhou, Hongyi Shao, and Dejin Yang) with high levels of experience in hip arthroplasty. All of the included patients underwent THA with a posterior approach. First, we prepared the femoral side using the combined anteversion technique [22]. After inserting the trial into the femur, we tried to measure the femoral stem anteversion using three independent methods (visual assessment, goniometer, and robotic system) sequentially to figure out which method was more accurate and reliable. We then decided the acetabular anteversion to ream and implant cups using a robotic-assisted system. Finally, we implanted stems and measured stem anteversion using a goniometer. The angle was between the low limb and stem axis when flexing the knee and letting the tibia be vertically positioned (Fig. 1). Subsequently, we used the robotic system to measure femoral stem anteversion (Fig. 2).
Radiographic measurement
Mimics software (version 20.0; Materialize, Leuven, Belgium) was used to reconstruct the postoperative CT scan image and perform radiographic measurements, which we regarded as "gold standard." Two doctors (Dr. Hongyi Shao, and Dr. Dejin Yang) measured the postoperative stem anteversion based on the definition proposed by Dorr et al. [23]. The angle is formed by the femoral neck axis and the femoral coronal plane. Femoral neck axis is defined as line connects femoral head center and center of femoral neck. While femoral coronal plane is defined by using the middle high point of the greater trochanter and the surgical epicondylar axis. The first 20 cases were measured by both of them, and the remaining cases were measured separately. One surgeon measured 20 randomly selected cases again after 4 weeks.
In 2020, Widmer reported that functional stem anteversion from 5° to 25° provided the largest combined target zones [3]. We classified patients into in-range anteversion (from 5° to 25°) and out-of-range (less than 5° or more than 25°) groups depending on anteversion measurement.
Statistical analysis
Continuous data were expressed as mean and standard deviation, while categorical data were expressed as frequencies and percentages. The Chi-square test was used to compare categorical data. Standard deviation (SD) and coefficient of variation were used to represent the data variation. Intraclass correlation coefficient (ICC) was used to assess the consistency of anteversion of different measurements and postoperative CT-measured stem anteversion, which represents the value of difference, respectively. Pearson correlation analysis was used to assess the correlation of stem anteversion from different measurement methods, and postoperative CT-measured stem anteversion, which represents the relevance, respectively. P < 0.05 was considered statistically significant. SPSS 19.0 (SPSS Inc., Chicago, IL, USA) and GraphPad Prism 5 (GraphPad Software Inc., California, USA) were used to analyze the data.
Results
All the 117 included patients were used the Mako robotic system to complete THA, including preoperative planning. All of them were implanted cementless cups (Trident, Stryker, Mahwah, NJ, USA). Among them, 11 patients received modular stems or conical stems (Table 2), while the other 106 patients received wedge-shaped cementless stems (Accolade II, Stryker, Mahwah, NJ, USA). The mean preoperative femoral anteversion measured by the robotic system was 13.8° ± 14.5° (range, − 36° to 50°; coefficient of variation, 104.62%), it was more variable than the intraoperative stem anteversion measured by the robotic system, which was 13.6° ± 7.9° (range, − 9° to 34°; coefficient of variation, 58.57%) (Fig. 3).
Variation in the preoperative robotic-measured native femoral anteversion and intraoperative robotic-measured stem anteversion. The scatter diagram of the preoperative robotic-measured femoral anteversion with more variation (mean: 13.85; SD: 14.49; coefficient of variation: 104.62%), and intraoperative robotic-measured stem anteversion with less variation (mean: 13.57: SD: 7.948; coefficient of variation: 58.57%)
Among them, 63 cases have been diagnosed as developmental dysplasia of the hip (DDH), and the remaining 54 cases were non-DDH. Compared with non-DDH patients, DDH patients were more likely to have out-of-range preoperative anteversion (P = 0.028). However, after stem implantation, approximately one-fifth of the patients had out-of-range intraoperative stem anteversion in both DDH and non-DDH cases where after modular or conical stems were used (Table 3).
The intra-observer and inter-observer correlation coefficients of postoperative stem anteversion measurement were 0.995 and 0.986, respectively. Intraoperative robotic-measured stem anteversion showed the highest correlation with postoperative CT measurement of stem anteversion (r = 0.806, P < 0.001), while intraoperative surgeon estimation had the lowest correlation coefficient (r = 0.281, P = 0.025). Meanwhile, preoperative robotic measured native femoral anteversion (r = 0.435, P < 0.001) and intraoperative goniometer measured stem anteversion (r = 0.459, P < 0.001) had modest correlations (Table 4). As for the consistency with postoperative CT measurement of femoral stem anteversion, intraoperative robotic-measured femoral stem anteversion also had the highest value (ICC = 0.892, P < 0.001, Table 4, Fig. 4).
Consistency of femoral or stem anteversion of different measurements and stem anteversion postoperative CT measurement. Bland–Altman diagram demonstrating that the intraoperative robotic-measured stem version (D) was the most consistent with the postoperative CT-measured stem version when compared with the preoperative native femoral version (A), intraoperative surgeon estimated stem version (B), and intraoperative goniometer-measured stem version (C)
Discussion
The current study investigated variability in different measurement results of femoral anteversions and the relationship between different assessment methods of femoral and postoperative stem anteversions in our cohort of patients. We found that the measurement results of femoral anteversion and intraoperative stem anteversion were highly variable, which may compromise surgeons' ability to target functional combined safe zones. Among the different evaluation methods for stem anteversion, intraoperative measurement with the robotic system had a significant correlation and consistency with postoperative stem anteversion, which may help surgeons adjust the acetabular anteversion to achieve a specific safe zone intraoperatively.
Dorr et al. concluded that CSI, which combines acetabular and femoral positions in the sagittal plane, was a predictor of hip dislocation [10, 11]. However, they did not consider femoral anteversion, which influences femoroacetabular impingement of the hip joint [3]. Padgett reported that even though we should consider the relationship between the spine and hip for late dislocations, femoral stem anteversion was also important [14]. Increased femoral anteversion could induce posterior impingement in the standing position, while decreasing femoral anteversion could induce anterior impingement in the sitting position. Using the computerized 3-D model simulation technique, the findings were consistent with this trend [3]. Therefore, optimizing femoral anteversion is an important factor that should be considered. Since cementless stems are gaining popularity in clinical practice and their anteversion is difficult to adjust due to the dramatic change in the proximal femur morphology, surgeons usually prepare the femur first when they use the combined anteversion technique [22]. During our study, we found that preoperative femoral anteversion was highly variable, and nearly half of the patients had out-of-range femoral anteversion. Even after using modular or metaphyseal fixation stems to achieve optimal anteversion, approximately one-fifth of the patients remaining had out-of-range stem anteversion. This reaffirms the importance of preoperative and intraoperative measurements of femoral anteversion. Emerson et al. used MRI to compare postoperative stem anteversion and preoperative femoral anteversion and found that their results were inconsistent and variable [24]. They also postulated that the anatomic shape of the femoral canal determines the anteversion of the stem and highlights the importance of intraoperative measurement for stem anteversion.
Dysplastic hips may have a straighter diaphyseal canal, smaller neck shaft, and increased anteversion on the femoral side [25]. Wells et al. studied the femoral morphology of dysplastic hips based on CT scan data and found that the variety of femoral anteversion angles was very large [26]. They found that 8% of patients had relative femoral retroversion (< 5°), and 52% had excessive femoral anteversion (> 25°). Our findings are similar, and there were more dysplastic hips that had too large or too small femoral anteversion. After cementless stem insertion, more patients received in-range femoral anteversion, while nearly one-fifth were still outside the range. Femoral morphology, neck cutting level, and stem design all influence final stem anteversion, which makes it different from native femoral anteversion [27, 28]. Using a modular or conical stem to adjust anteversion and targeting in-range anteversion could explain why we obtained more optimal stem anteversion. However, cases of out-of-range anteversion should draw surgeons' attention, which may compromise clinical results.
In our study, we found that the preoperative femoral anteversion measured by the robotic system was not consistent with postoperative femoral stem anteversion. In the robotic system, preoperative femoral anteversion was defined by the angle of the projection of the line connecting the femoral head center with the femoral neck center and transverse epicondylar axis on the transverse plane. This measurement method and results were similar to those of a previous study that reported preoperative femoral anteversion from a 3-D CT scan, which was a little less than the postoperative results [17]. Although the postoperative femoral anteversion measurement method for the femoral component was the same as preoperative, the component position was related to the femoral morphology, the types of the femoral stem we used, and the surgical technique[23, 24, 29]. Thus, we suppose that the measurement of preoperative anteversion of the femur from the robotic system does not provide us with consistent intraoperative anteversion.
Both robotic systems and traditional instruments for measurements of intraoperative femoral anteversion provide more accurate results than preoperative estimation. The robotic measurements were more consistent with the real results. All THAs were performed using the posterior approach, and osseous landmarks were limited. Dorr et al. first reported the error of surgeon's estimation for femoral anteversion by as much as 11°, which was similar to our results [23]. Hirata et al. further reported that surgeons tended to overestimate femoral anteversion when they used the posterior approach, which was related to the severity of knee osteoarthritis [18]. Our results are consistent with this trend. Our study found that the robotic technique had highest accuracy for intraoperative femoral anteversion evaluation. Nodzo et al. used a robot to assist hip arthroplasty and found that the femoral anteversion measured during the operation was highly consistent with that measured by postoperative CT [21]. However, in three of the 20 hips, there was a difference of more than 5° between the intraoperative and postoperative CT measurements. The error of intraoperative registration and potential displacement of the markers may be the causes of bias. Nevertheless, the robotic system is still a reliable and accurate method that helps determine femoral anteversion intraoperatively. Because postoperative CT measurements, as the gold standard, cannot provide real-time intraoperative data. Using different intraoperative measurement methods to assist joint surgeons in obtaining estimates of intraoperative femoral anteversion can help them to perform surgeries more accurately.
There are several limitations to our study. First, this was a retrospective study, which has inherent limitations for the method itself. However, it was difficult do such kind of study prospectively and blindly. Second, the surgical technique and conceptions may influence stem anteversion. However, all surgeons who performed these surgeries were well-trained in our hospital, and their targets and approaches were the same. Third, only half of the patients in this study had postoperative CT data for analysis. Since CT had more radiation than X-ray, it was difficult to perform a CT scan for every patient after surgery, and the demographic data of patients who underwent CT were similar to those of patients who did not undergo CT. Finally, femoral stem anteversion assessment by visual and goniometer was relatively subjective, especially after the robotic system measured the stem trial. However, we routinely measured stem anteversion before we used the robotic system as previously described. Further prospective studies with more cases for femoral anteversion are warranted to confirm our findings and address these limitations.
Conclusion
In conclusion, native femoral anteversion was variable preoperatively. With the use of cementless stems, anteversion was also highly variable. Robotic assessment for stem anteversion during surgery was more consistent with the final position than preoperative assessment and conventional intraoperative estimation, while the visual assessment was inaccurate.
References
Barsoum WK, Patterson RW, Higuera C, Klika AK, Krebs VE, Molloy R. A computer model of the position of the combined component in the prevention of impingement in total hip replacement. J Bone Joint Surg Br. 2007;89:839–45.
Patel AB, Wagle RR, Usrey MM, Thompson MT, Incavo SJ, Noble PC. Guidelines for implant placement to minimize impingement during activities of daily living after total hip arthroplasty. J Arthroplasty. 2010;25:1275–81.
Widmer KH. The impingement-free, prosthesis-specific, and anatomy-adjusted combined target zone for component positioning in THA depends on design and implantation parameters of both components. Clin Orthop Relat Res. 2020;478:1904–18.
Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–42.
Cheung A, Yan CH, Fu H, Cheung MH, Chan PK, Chiu KY. Ten- to sixteen-year follow-up of highly cross-linked polyethylene in total hip arthroplasty: what factors affect wear? J Arthroplasty. 2019;34:2016–21.
Watts CD, Abdel MP, Hanssen AD, Pagnano MW. Anatomic hip center decreases aseptic loosening rates after total hip arthroplasty with cement in patients with crowe type-II dysplasia: a concise follow-up report at a mean of thirty-six years. J Bone Joint Surg Am. 2016;98:910–5.
Hemmerich A, Brown H, Smith S, Marthandam SS, Wyss UP. Hip, knee, and ankle kinematics of high range of motion activities of daily living. J Orthop Res. 2006;24:770–81.
Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–8.
Pierrepont J, Hawdon G, Miles BP, et al. Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. Bone Joint J. 2017;99B:184–91.
Heckmann N, Tezuka T, Bodner RJ, Dorr LD. Functional anatomy of the hip joint. J Arthroplasty. 2021;36:374–8.
Tezuka T, Heckmann ND, Bodner RJ, Dorr LD. Functional Safe zone is superior to the lewinnek safe zone for total hip arthroplasty: why the lewinnek safe zone is not always predictive of stability. J Arthroplasty. 2019;34:3–8.
McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–59.
Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39:1315–23.
Padgett DE. The hip-spine relationship: the importance of femoral version. J Arthroplasty. 2021;36:S99–103.
Tang H, Li Y, Zhou Y, Wang S, Zhao Y, Ma Z. A modeling study of a patient-specific safe zone for THA: calculation, validation, and key factors based on standing and sitting sagittal pelvic tilt. Clin Orthop Relat Res. 2022;480:191–205.
Reikerås O, Gunderson RB. Components anteversion in primary cementless THA using straight stem and hemispherical cup: a prospective study in 91 hips using CT-scan measurements. Orthop Traumatol Surg Res. 2011;97:615–21.
Park KK, Tsai TY, Dimitriou D, Kwon YM. Utility of preoperative femoral neck geometry in predicting femoral stem anteversion. J Arthroplasty. 2015;30:1079–84.
Hirata M, Nakashima Y, Ohishi M, Hamai S, Hara D, Iwamoto Y. Surgeon error in performing intraoperative estimation of stem anteversion in cementless total hip arthroplasty. J Arthroplasty. 2013;28:1648–53.
Kanawade V, Dorr LD, Banks SA, Zhang Z, Wan Z. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty. 2015;30(3):392–7.
Domb BG, Redmond JM, Louis SS, et al. Accuracy of component positioning in 1980 total hip arthroplasties: a comparative analysis by surgical technique and mode of guidance. J Arthroplasty. 2015;30(12):2208–18.
Nodzo SR, Chang CC, Carroll KM, et al. Intraoperative placement of total hip arthroplasty components with robotic-arm assisted technology correlates with postoperative implant position: a CT-based study. Bone Joint J. 2018;100B:1303–9.
Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467:119–27.
Dorr LD, Wan Z, Malik A, Zhu J, Dastane M, Deshmane P. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am. 2009;91:2598–604.
Emerson RH Jr. Increased anteversion of press-fit femoral stems compared with anatomic femur. Clin Orthop Relat Res. 2012;470:477–81.
Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009;467:128–34.
Wells J, Nepple JJ, Crook K, et al. Femoral morphology in the dysplastic hip: three-dimensional characterizations with CT. Clin Orthop Relat Res. 2017;475:1045–54.
Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am. 2011;93:500–9.
Marcovigi A, Ciampalini L, Perazzini P, Caldora P, Grandi G, Catani F. Evaluation of native femoral neck version and final stem version variability in patients with osteoarthritis undergoing robotically implanted total hip arthroplasty. J Arthroplasty. 2019;34:108–15.
Nakashima Y, Hirata M, Akiyama M, et al. Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop. 2014;38:27–32.
Acknowledgements
We would like to thank Dr. Siyuan Wang, and Dr. Shaoyi Guo, for their help in radiographic measurement, and Editage (www.editage.cn) for English language editing.
Funding
This work was supported by the Haidian Original Innovation United Fund of Beijing Natural Science Foundation (Grant No. L202051), Beijing Municipal Administration of Hospitals Incubating Program (Grant No. pX2020019), the National Natural Science Foundation of China (Grant No. 82102641), Beijing Jishuitan Hospital horizontal project (the clinical study of custom bone and joint prosthesis), and Beijing Jishuitan Hospital Natural Fund Incubation Program (Grant No. ZR-202304).
Author information
Authors and Affiliations
Contributions
Hongyi Shao performed conceptualization, formal analysis, investigation, methodology, funding acquisition, and writing—original draft. Yong Huang developed conceptualization, formal analysis, methodology, and writing—review & editing. Dejin Yang provided conceptualization, formal analysis, and writing—review & editing. Wang Deng analyzed conceptualization, methodology, and writing—review & editing. Xiang-Dong Wu carried out conceptualization, methodology, and writing—review & editing. Yixin Zhou approved conceptualization, formal analysis, funding acquisition, methodology, and writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shao, H., Huang, Y., Yang, D. et al. Variety of femoral anteversion and its measurement in cementless total hip arthroplasty: Does robotic technology improve accuracy?. J Orthop Surg Res 19, 47 (2024). https://doi.org/10.1186/s13018-024-04527-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04527-z