Abstract
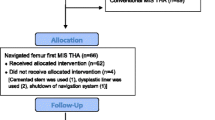
Combined cup and stem anteversion in THA based on femoral anteversion has been suggested as a method to compensate for abnormal femoral anteversion. We investigated the combined anteversion technique using computer navigation. In 47 THAs, the surgeon first estimated the femoral broach anteversion and validated the position by computer navigation. The broach was then measured with navigation. The navigation screen was blocked while the surgeon estimated the anteversion of the broach. This provided two estimates of stem anteversion. The navigated stem anteversion was validated by postoperative CT scans. All cups were implanted using navigation alone. We determined precision (the reproducibility) and bias (how close the average test number is to the true value) of the stem position. Comparing the surgeon estimate to navigation anteversion, the precision of the surgeon was 16.8° and bias was 0.2°; comparing the navigation of the stem to postoperative CT anteversion, the precision was 4.8° and bias was 0.2°, meaning navigation is accurate. Combined anteversion by postoperative CT scan was 37.6° ± 7° (standard deviation) (range, 19°–50°). The combined anteversion with computer navigation was within the safe zone of 25° to 50° for 45 of 47 (96%) hips. Femoral stem anteversion had a wide variability.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.









Similar content being viewed by others
References
ASTM. Standard Practice for Use of the Terms Precision and Bias in ASTM Test Methods. In: Annual Book of ASTM Standards ed. Philadelphia, PA: American Society for Testing and Materials; 2002:E177–E190a.
Barrack RL, Lavernia C, Ries M, Thornberry R, Tozakoglou E. Virtual reality computer animation of the effect of component position and design on stability after total hip arthroplasty. Orthop Clin North Am. 2001;32:569–577.
Best DE, Horii SC, Bennett W, Thomson B, Snavely D. Review of the American College of Radiology–National Electrical Manufacturers’ Association standards activity. Comput Methods Programs Biomed. 1992;37:305–309.
Bidgood WD Jr, Horii SC. Introduction to the ACR-NEMA DICOM standard. Radiographics. 1992;12:345–355.
DiGioia AM, Jaramaz B, Blackwell M, Simon DA, Morgan F, Moody JE, Nikou C, Colgan BD, Aston CA, Labarca RS, Kischell E, Kanade T. The Otto Aufranc Award. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res. 1998;355:8–22.
DiGioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364.
D’Lima DD, Chen PC, Colwell CW Jr. Optimizing acetabular component position to minimize impingement and reduce contact stress. J Bone Joint Surg Am. 2001;83(Suppl 2 Pt 2):87–91.
D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–321.
Dobzyniak M, Fehring TK, Odum S. Early failure in total hip arthroplasty. Clin Orthop Relat Res. 2006;447:76–78.
Dorr LD. Hip Arthroplasty, Minimally Invasive Techniques and Computer Navigation. Philadelphia, PA: Saunders, Elsevier; 2006.
Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14:231–242.
Dorr LD, Hishiki Y, Wan Z, Newton D, Yun A. Development of imageless computer navigation for acetabular component position in total hip replacement. Iowa Orthop J. 2005;25:1–9.
Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–99.
Dorr LD, Wan Z. Ten years of experience with porous acetabular components for revision surgery. Clin Orthop Relat Res. 1995;319:191–200.
Harris M, Dorr LD, Wan Z, Sirianni L, Boutary M. Total hip arthroplasty with the APR stem and cup follow-up of a previous report. J Arthroplasty. 2005;20:828–831.
Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty. 1998;13:80–84.
Inaba Y, Dorr LD, Wan Z, Sirianni L, Boutary M. Operative and patient care techniques for posterior mini-incision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:104–114.
Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179.
Kalteis T, Handel M, Bathis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88:163–167.
Kang JS, Dorr LD, Wan Z. The effect of diaphyseal biologic fixation on clinical results and fixation of the APR-II stem. J Arthroplasty. 2000;15:730–735.
Komeno M, Hasegawa M, Sudo A, Uchida A. Computed tomographic evaluation of component position on dislocation after total hip arthroplasty. Orthopedics. 2006;29:1104–1108.
Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–1842.
Maruyama M, Feinberg JR, Capello WN, D’Antonio JA. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;393:52–65.
McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–159.
Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232.
Nishii T, Sugano N, Miki H, Koyama T, Takao M, Yoshikawa H. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty. J Arthroplasty. 2004;19:162–166.
Patil S, Bergula A, Chen PC, Colwell CW Jr, D’Lima DD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85(Suppl 4):56–63.
Pierchon F, Pasquier G, Cotten A, Fontaine C, Clarisse J, Duquennoy A. Causes of dislocation of total hip arthroplasty. CT study of component alignment. J Bone Joint Surg Br. 1994;76:45–48.
Ranawat CS, Maynard MJ. Modern Techniques of Cemented Total Hip Arthroplasty. Tech Orthopedics. 1991;6:17–25.
Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008;23:51–56.
Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821.
Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701.
Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39:1315–1323.
Acknowledgments
We thank Patricia Paul for her help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more authors (LDD) have received funding from Good Samaritan Hospital (Los Angeles, CA) for conducting this study.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Appendix 1. Operative Technique
Appendix 1. Operative Technique
Computer Registration for Navigation
The instrumentation for computer navigation was calibrated while the patient was prepared for anesthesia. After the patient was anesthetized, a metal base plate for the pelvic tracker was secured with three 1/8-inch threaded pins to the thickest portion of the pelvic brim. With the patient supine, the anterior pelvic plane registration was performed by bony contact to both anterosuperior iliac spines and the pubic bone near the pubic tubercles. The skin and fat over the pubis (mons pubis) was always punctured to contact the pubic bone. In obese patients with approximately 5 mm of skin and fat over the anterosuperior iliac spines, a stab wound to the bone was made to insure bone contact. The patient was then “flipped” to the lateral position and secured with two pelvic supports and two chest supports (Sunmed, Redding, CA). The registration pointer was used to contact the two posterior supports with three points in triangular geometry to register the longitudinal axis of the body. The software can then compute the tilt of the pelvis relative to this longitudinal reference plane. The pelvic tilt permits adjustment of inclination and anteversion into the radiographic coronal plane.
The femoral pins and tracker were placed with the patient in the lateral position. The femoral baseplate was attached to the anterior lateral femur 8 cm cephalad from the superior pole of the patella and anterior to the palpable anterior edge of the iliotibial band. The pins were drilled through the anterior lateral cortex into, but not through, the medial cortex. For determination of femoral anteversion the longitudinal plane of the leg is registered. This is done after the incision and posterior approach have been undertaken with exposure of the greater trochanter but before femur dislocation. Five points are registered: the greater trochanter, the two femoral epicondyles, and two ankle malleoli. The knee must be at 90° of flexion. These points are used to determine the plane of the leg from which the software defines the femoral plane to determine femoral anteversion. In obese patients the epicondyles are difficult to identify percutaneously and this may contribute to inaccurate values of the plane of the leg and consequently femoral anteversion. The navigation system software was programmed only for the APR anatomic stem (Zimmer, Warsaw, IN) during the time of this study.
Posterior Approach
The incision is made over the posterior border of the greater trochanter, and extends proximally from the level of the vastus tubercle for 10 cm cephalad. The first incision into hip tissue is done in the gluteus maximus muscle, which is incised for 6 to 8 cm along the posterior border of the greater trochanter. The second is through the small external rotators and the posterior capsule with the leg in internal rotation. It is made as a single flap from just proximal to the quadratus femoris muscle either to or through the piriformis tendon. If the piriformis tendon is transected, the incision extends through 1 to 2 cm of the gluteus minimus muscle. In flexible hips, the piriformis tendon is preserved and an L-shaped incision is made with one arm parallel to the piriformis tendon. The hip is dislocated and the corresponding templated neck cut for restoration of leg length made. The third incision is of the inferior medial capsule, which is incised from the anterior femur to the acetabulum through the transverse acetabular ligament.
Femoral Preparation
The preparation of the femur was performed first so that the anteversion of the femur was known prior to the preparation and implantation of the acetabulum. The femur is presented into the wound by positioning of long-handled retractors (Zimmer, Warsaw, IN). Femoral preparation was done by reaming and broaching. Five points of the intramedullary canal of the femur were registered with a metal registration tool. The software could then determine the position of the implants in the femoral bone by calculating the intramedullary canal relative to the plane of the leg. The anteversion of the broach (and subsequently the stem) was computed as it was implanted into the bone and displayed on the computer screen.
Acetabular Preparation
Three long-handled retractors are placed to obtain correct exposure of the acetabulum.The labrum is removed as is any floor osteophyte overlying the cotyloid fossa. The cortical bone of the cotyloid notch is registered as the medial wall. Two registrations of the native acetabulum are done prior to acetabular preparation. (1) The acetabulum is digitized 16 times to obtain the center of rotation and diameter of the bony acetabulum. (2) Four points on the cortical bone of the cotyloid notch digitized the medial wall. The change in center of rotation by depth of reaming in both the medial and superior directions can be visualized on the computer screen. Reaming medially is done to the cotyloid notch which medializes the center of rotation 3 to 6 mm; removal of the lunate bone and formation of a hemisphere moves the center of rotation cephalad to 5 mm. The cup is targeted to 40° ± 5° inclination and the anteversion is customized according to the femoral anteversion to provide a combined anteversion of 30° to 45° (with 5° margin of error for safe zone of 25° to 50°), lower for men and hips with low femoral anteversion, and higher for women and hips with high femoral anteversion. The coverage of the cup is to have the inferior-medial edge flush with the cortical bone of the cotyloid notch (just inside the transverse acetabular ligament) and 3 mm below the pubis cortex; the anterior-superior edge is level with the anterior iliac bone; posteriorly, it is below the ischial cortex and may be prominent by up to 3 mm posterior-superiorly.
About this article
Cite this article
Dorr, L.D., Malik, A., Dastane, M. et al. Combined Anteversion Technique for Total Hip Arthroplasty. Clin Orthop Relat Res 467, 119–127 (2009). https://doi.org/10.1007/s11999-008-0598-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0598-4