Abstract
Background
To investigate the radiologic and prognostic outcomes after using arthroscopic-assisted reduction and internal fixation (ARIF) in complex tibial plateau fractures with mid- to long-term follow-up.
Methods
This retrospective study reviewed complex tibial plateau fractures that underwent ARIF from 1999 to 2019. Radiologic outcomes, including tibial plateau angle (TPA), posterior slope angle (PSA), Kellgren–Lawrence classification and Rasmussen radiologic assessment, were measured and evaluated. The prognosis and complications were assessed by the Rasmussen clinical assessment with a minimum follow-up of 2 years.
Results
Ninety-two consecutive patients (mean age: 46.9 years) with a mean follow-up of 74.8 months (24–180) were included in our series. Using AO classification, there were 20 type C1 fractures, 21 type C2 fractures, and 51 type C3 fractures. All the fractures achieved solid union. TPA was maintained well on average at the last follow-up and showed no significant difference compared to postoperatively (p = 0.208). In the sagittal plane, the mean PSA increased from 9.3 ± 2.9° to 9.6 ± 3.1° (p = 0.092). A statistically significant increase in PSA was also noted in the C3 group (p = 0.044). Superficial or deep infection was noted in 4 cases (4.3%), and total knee arthroplasty (TKA) was performed in 2 cases (2.2%) due to grade 4 osteoarthritis (OA). Ninety (97.8%) and 89 (96.7%) patients had good or excellent results in the Rasmussen radiologic assessment and Rasmussen clinical assessment, respectively.
Conclusions
The complex tibial plateau fracture could be treated successfully using arthroscopy-assisted reduction and internal fixation. Most patients achieve excellent and good clinical outcomes with low complication rates. In our experience, a higher incidence of increased slope was noted, especially in type C3 fractures. Reduction of the posterior fragment should be done cautiously during the operation.
Levels of evidence
Level III.
Similar content being viewed by others
Background
The treatment of complex tibial plateau fractures remains challenging during daily clinical practice. The definition of these types of fractures can be classified by Schatzker classification as type V or VI or by AO classification as AO/OTA 41-C. Complex tibial plateau fractures account for up to 39% of all tibial plateau fractures and are often accompanied by severe soft tissue injuries or multiple trauma due to the mechanism of high energy [1]. Due to the complicated situation, the rate of complications during or after the operation for complex tibial plateau fractures was reported to be higher than that for simple types. Posttraumatic osteoarthritis (OA) also occurs more frequently due to the complexity of joint surface depression, and the risk for arthroplasty in the long-term follow-up is higher [2,3,4,5,6].
A number of operative procedures have been described for the treatment of complex tibial plateau fractures, and controversy remains regarding the best surgical method [7]. Techniques of arthroscopic-assisted reduction and internal fixation (ARIF) were introduced and have been reported for years with good preliminary results [8,9,10,11,12,13,14,15,16,17,18]. The beneficial outcome can be attributed to direct visualization and reduction of the joint surface, combined treatment of intra-articular soft tissue injury, and a minimally invasive incision compared to traditional open reduction using arthroscopy. However, there remains a paucity of studies focusing on complex tibial plateau fractures using ARIF. The long-term outcomes of fractures in these types are also scarce. The purpose of this study was to investigate the clinical and radiographic prognosis of complex tibial plateau fractures using ARIF in our institute with long-term follow-up.
Methods
Study design
This study was a retrospective cohort review from November 1999 to April 2019 under a protocol approved by the institutional review board. A total of 321 consecutive tibial plateau fractures were treated using arthroscopy-assisted surgery with internal fixation at our hospital. The inclusion criteria in this study included the presence of complex tibial plateau fracture (AO/OTA 41-C) in skeletally mature patients. Patients with pathological fractures, skeletal immaturity, previous surgery, systemic joint diseases, fractures involving the same extremity, prior limitations of motion over knee joint and cases with less than 2 years of follow-up postoperatively were excluded from the study. All the fractures were classified and confirmed by computed tomography (CT) scan before the surgery (Fig. 1).
Patient demographic data, including sex, age and associated injuries, were reviewed and collected from the charts. All included cases were divided into 3 subgroups according to AO/OTA 41 types C1–C3. Radiographic data, including tibial plateau angle (TPA) and posterior slope angle (PSA), were used for assessment of joint alignment on the X-ray postoperatively and at the time of final follow-up (Figs. 2. and 3). Grading of OA was recorded by classification of Kellgren–Lawrence on the X-ray preoperatively and the last follow-up. If the patient had converted to arthroplasty, the last radiograph of the status with internal fixation was used for measurement. The status of union was evaluated using the presence of bridging callus on both planes of radiography. Rasmussen radiologic assessment was used for further evaluation of the quality of reduction on the last radiography. Patient functional outcomes were assessed by the Rasmussen clinical assessment using questionnaires in the clinic. The scores of both assessments were graded as poor, fair, good, and excellent. All patients were examined by an independent observer (Y-H.C.)
Arthroscopic-assisted reduction and internal fixation intraoperatively. A, B In addition to double plating, the posteromedial fragment was fixed with 2 interfragment screws. Both planes of radiographic alignment were well maintained. C, D, E Using the arthroscopic technique, joint depression due to the posteromedial fragment was directly visible and could be reduced perfectly through the fracture site. ACL avulsion was also treated simultaneously with arthroscopic suture fixation using 4 No. 5 Ethibond sutures
Surgical technique
All surgical procedures were performed by a single surgeon (Y-S.C.). Under general anesthesia, patients were in the supine position with a tourniquet over the proximal thigh. Arthroscopic examination was routinely performed first. Standard anteromedial and anterolateral portals were created, and gravity inflow was used to minimize fluid extravasation. In addition to the articular depression, other possible associated intra-articular lesions were inspected and checked meticulously using arthroscopic techniques to further determine the optimal treatment. Hematoma, loose bodies or synovitis were debrided or removed. The associated injuries were treated prior to or following internal fixation according to the type of injury. We preferred to perform meniscal repair or partial meniscectomy prior to fracture fixation due to better accessibility to the meniscus. After cautious evaluation of the soft-tissue structures inside the knee, reduction with a minimally invasive wound was performed. To avoid arthrotomy and extensive soft-tissue stripping, double incisions were performed around the proximal tibia with anteromedial and anterolateral approaches. Two wounds should be separated as far as possible to prevent necrosis of the skin. A cannulated impactor or bone tamp was used through the fracture site over the metaphysis to elevate the fragments (Fig. 2). If there was no space for the impactor to enter, we preferred using a standard anterior cruciate ligament (ACL) tibial guide to alternatively create a window around the proximal tibia. Using the ACL guide, a Kirschner wire could pass through the fracture site precisely. Subchondral bone could be elevated, and the articular surface could be reduced accurately with visualization under the arthroscope. Other techniques for more severe and comminuted tibial plateau fractures around the posteromedial corner were often used, as mentioned in our previous study [19]. After acceptable reduction was performed and confirmed by arthroscopy and an image intensifier, multiple Kirschner wires were used temporarily to maintain the reduction. Interfragment screws were sometimes used for fixation of larger bony fragments. Double plating was then applied for the final fixation. After fixation, valgus and varus stress tests were routinely performed to confirm stability and rule out other ligamentous injuries. Wounds were then closed layer by layer with two drains left in a stable knee. If there were associated ligamentous injuries or avulsion fractures, repair of the associated injuries was performed simultaneously in the acute phase. If the injuries met the criteria for reconstruction, a staged operation would be planned.
Statistical analysis
Statistical data were analyzed utilizing SPSS software (IBM Corp. in Armonk, NY.). Radiographic data for maintenance of the reduction were compared and evaluated from the postoperative condition to the final follow-up. Data for intergroup comparisons were analyzed by independent t tests. Comparisons for intragroup classification by AO/OTA 41 types C1–C3 were performed using one-way analysis of variance (ANOVA). A p value < 0.05 indicated statistical significance.
Results
General data
A total of 105 patients with a diagnosis of complex tibial plateau fracture were treated with ARIF in our institution. Fourteen patients were excluded with a loss to follow-up rate of 12.5%. Among the final 91 cases, the mean age at surgery was 46.9 years (21–81), and the mean duration of follow-up was 74.8 months (24 to 180). The mean time interval from injury to surgery was 7.8 ± 2.4 days. The periods of follow-up of more than 10 years, 5 years and 2 years were 24 (26.1%), 28 (30.4%) and 40 (43.5%), respectively. Classified by AO/OTA 41, there were 20 type C1 fractures, 21 type C2 fractures, and 51 type C3 fractures. The average duration of the arthroscopic portion of the surgery was 35.7 ± 6.3 min. The main general data of the involved patients and their associated injuries sorted by classification are shown in Table 1.
Radiologic assessment
At the last follow-up, all the patients achieved bony union under radiography. The mean TPA and PSA were 87.1 ± 2.9° and 9.3 ± 2.9° on the day after surgery, respectively. The reduction remained stable at the final follow-up, with a TPA of 86.7 ± 4.5° (p = 0.208) and PSA of 9.6 ± 3.1° (p = 0.092). However, the posterior slope revealed a statistically significant difference in the type C3 group (p = 0.044). No significant differences in TPA or PSA were noted between the groups (Table 2). Using the Rasmussen radiologic assessment to evaluate the quality of reduction, the mean score was 16.41. Thirty-nine of 92 (42.4%) cases were classified as excellent, and 51 cases (55.4%) were classified as good. Two cases in the C3 group were graded as fair. The mean score of type C1 was statistically superior to that of type C3 (p = 0.029) (Table 3). The condition of OA according to Kellgren–Lawrence classification was listed in Table 4. Only two patients revealed grade 4 OA in the last follow-up.
Clinical assessment and complications
The mean Rasmussen clinical score was 27.55. Sixty-seven patients (72.8%) were classified as excellent, and 22 patients (23.9%) were classified as good. Three patients were graded as fair. One of the cases was a 52-year-old male with a type AO-OTA 41/C3 fracture combined with medial collateral ligament (MCL) and lateral collateral ligament (LCL) tears. ARIF and ligament repair were performed simultaneously. However, malalignment with valgus deformity was gradually revealed in our clinical follow-up. The other two cases with fair outcomes received arthroplasty due to pain and wounds, as mentioned below in detail. There were no significant differences between the groups (Table 5).
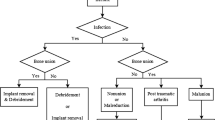
Complications were noted in 6 patients. None of them were directly associated with arthroscopic procedures. Each case of type C2 and C3 fractures developed wound dehiscence with superficial infections noted in our clinic. Symptoms were relieved well after oral antibiotics and cautious wound care, and no further surgery was needed. High energy-related soft tissue compromise might be the reason for the delayed healing of the wound. Deep wound infections were noted in two cases (1 type C1, 1 type C3) with initial open fractures. Debridement was performed, and then admission for antibiotic treatment was arranged for 2 weeks and then shifted to oral form for an additional 4 weeks in both cases. Two patients with comminuted C3 fractures developed grade 4 OA after ARIF for 3 years and 5 years. Conversion to total knee arthroplasty (TKA) was then arranged with satisfactory outcomes.
Discussion
Until now, there has been no general agreement on how complex tibial plateau injuries should be managed. This is the first study to assess the use of ARIF for the treatment of complex tibial plateau fractures with long-term follow-up. Our series revealed good or excellent long-term prognosis in most of the patients.
The treatment of complex tibial plateau fractures is challenging. Substantial soft-tissue injuries were common, and up to 43% were open fractures [1, 20,21,22]. Poor soft tissue conditions and comminuted intra-articular fragments related to high-energy mechanisms are the main factors predisposing patients to high complication rates using traditional open reduction and internal fixation (ORIF). Arthroscopic-assisted reduction and internal fixation for tibial plateau fractures was first introduced by Caspari et al. and Jennings, with series focusing on relatively simple fracture types (Schatzker types I, II and III) [17, 18]. Through the years, some techniques have been developed to overcome the more complex plateau fractures under arthroscopy, especially fragments involving the posterior compartment [9, 16, 19, 23]. Several studies have already shown satisfactory functional and radiological results. The incidence of associated injuries, including chondral injury, meniscus tears or rupture of ligaments, was high, followed by tibial plateau fractures. In a large matched cohort study with 7950 cases, 7.6% of tibial plateau fractures needed secondary knee arthroscopy compared to 2.0% of the reference group [24]. In our series, the incidence of associated injury was 69.5% after complex tibial plateau fracture. Although it is more technically demanding, ARIF allows surgeons to treat plateau fractures and intra-articular soft tissue simultaneously. The avoidance of arthrotomy when using arthroscopy could prevent the risk of stiffness, further tenderness or iatrogenic meniscal injuries [25, 26]. Moreover, with the direct visualization of the joint surface, reduction could be made easily with a minimally invasive incision of the wound for internal fixation. The abovementioned benefits might explain the good prognosis in our series.
Reduction of the joint surface is one of the primary goals while treating tibial plateau fractures. In the cases classified by Schatzker type V/VI and AO 41-C, the fracture is usually more comminuted and often involves the posterior compartment. In our experience, using an ACL tibial guide to create an accurate cortical window could efficiently reduce the depressed fragment. Combined with buttress plates and cannulated screws for fixation with arthroscopic techniques, the posterior compartment of the fractures could be restored with well-documented radiographic healing, good clinical outcomes, and low complication rates [19]. We used the same technique for the treatment of complex tibial plateau fractures and used TPA and PSA to evaluate the quality of coronal and sagittal reduction. We noticed no difference in the TPA between the postoperative day and the last follow-up in the AO-41 C1, C2 and C3 groups, which indicated that the reduction in the coronal plane was well maintained. However, increased PSA was shown in the final follow-up in all the groups, with a significant difference in the type C3 group compared to the postoperative radiograph. It revealed the difficult maintenance of the posterior fragment, especially in AO-41 C3 type. Recently, the role of the posterior slope has received more attention due to its influence on stability, activity, and load sharing biomechanically [27,28,29,30,31]. Streubel et al. demonstrated that most patients had significant sagittal displacement that would require surgical reduction of at least one condyle in C-type bicondylar tibial plateau fractures [32]. Barei et al. [20] reported the radiographic result of complex AO/OTA 41-C3 tibial plateau fractures after double plating using ORIF and found that only 72% satisfactory sagittal alignment can be achieved with the range of PSA of 9 ± 5°. Eggli et al. [33] demonstrated that in 13 out of 14 complex tibial plateau fractures, the posterior proximal tibial angle was measured as anatomically aligned. In our series, 87 of 92 (94.6%) patients reached satisfactory sagittal alignment at the last follow-up. This result demonstrated that using the arthroscopic technique and ACL drill guide could restore the posterior fragment well. Although our study highlighted the importance of anatomic alignment, further investigations are warranted to establish the correlation between radiographic alignment and clinical outcomes. We also used the Rasmussen criteria for further radiographic assessment, and 98.9% of cases achieved good or excellent results. The outcome is comparable to other series using ORIF or other minimally invasive techniques [34,35,36]. Between the groups, we noticed that the type C1 group was statistically superior to the C3 group. This further revealed the difficulty for the reduction in the C3 group, even if most of our cases in C3 could achieve good to excellent results and only two cases had fair outcomes. Rasmussen clinical assessment was also applied to the series, with all but one of the patients reporting a good or excellent prognosis. In contrast to the radiologic evaluation, there was no significant difference between the three groups. This might also indicate that the advantages of avoiding extensive stripping of soft tissue led to satisfactory outcomes, even if the posterior slope might increase in the long-term follow-up.
The complication rate of complex tibial plateau fractures was high [1, 36,37,38]. Lee et al. reviewed bicondylar plateau fractures and reported an overall complication rate as high as 39% after operative treatment [1]. Deep wound infections, nonunions and failed treatment requiring revision are common complications due to poor soft tissue conditions combined with high-energy trauma [21, 39]. Ochen et al. retrospectively collected 214 cases with AO/OTA 41-C or Schatzker V/VI tibial plateau fractures and noted that infection occurred in 12% of patients after ORIF, and three-fourths of the infections were deep infections [40]. In a recent systemic review comparing ORIF and ARIF for plateau fractures, the reported complication rates were 5.6% and 9.1% in the ARIF and ORIF groups, respectively. Even if there was no significant difference, the ARIF group showed lower complication rates than the ORIF group [41]. In our series, the complication rate was 6.5%, which was superior to the prognosis reported in complex tibial plateau fractures using ORIF. Four cases of infection were noted, and half of them were deep wound infections and might initially be related to open fractures. The higher incidence in our study is reasonable because most of the fracture patterns using ARIF in previous series were simple plateau fractures. Two cases (2.2%) were converted to TKA due to grade 4 OA. The incidence in the current series is relatively low compared to that in previous studies. Dreumel et al. [42] reported a 7.3% incidence rate in which TKA was eventually required in plateau fractures after 1 year of follow-up on average. Elsoe et al. [2] found that 5.7% of tibial plateaus were treated with a TKA in a large series collected from 5290 patients. Conversely, a superior prognosis for arthroplasty due to OA was reported recently. Ochen et al. [40] reported that the incidence for subsequent arthroplasty following initial ORIF in complex fractures was 3%, which was 6 of 214 cases. Dreumel et al. [42] reported that the rate of arthroplasties was 2.4% in 83 intra-articular tibial plateau fractures. The comparably satisfactory rate in our series might be due to the direct visualization of the joint surface for reduction. We assumed that the minimally invasive soft tissue stripping that led to faster rehabilitation could also be another reason for the low rate of conversion to TKA. Some studies have reported that high-energy complex fracture patterns are contraindications for knee arthroscopy due to the potential risk of iatrogenic compartment syndrome resulting from arthroscopy fluid extravasation [43, 44]. However, in our series, none of the complications were attributed to the arthroscopic procedure. This may be due to the use of temporary external fixation in cases involving open fractures or significant soft tissue swelling at our institution. The ARIF procedure was then performed after a delay of 1 to 2 weeks. To our knowledge, this was the first study to report the long-term prognosis of ARIF in complex tibial plateau fractures. We believe that the use of meticulous arthroscopic techniques for the reduction could achieve excellent results.
Our study has some limitations that should be mentioned. First, this is a retrospective series, and all the limitations of retrospective studies apply to our cohort. Second, plain radiographs were used for evaluation postoperatively rather than CT scans and might cause some bias due to rotation or different positions. Third, surgeries were performed by a single surgeon. The possibility cannot be ruled out that the good prognosis in our study may be due to the practiced skills and training by the experienced surgeon. Fourth, our study lacked a control group of ORIF for comparative analysis. Finally, we also had a moderate rate of loss to follow-up. However, to our knowledge, this is the largest cohort to evaluate long-term outcomes focusing on complex tibial plateau fractures.
Conclusions
This study demonstrated that complex tibial plateau fractures can be successfully treated using arthroscopy-assisted reduction and minimally invasive internal fixation. Most patients exhibited good to excellent clinical outcomes, low complications and good maintenance of radiography in mid- to long-term follow-up. In our experience, there was a higher incidence of increased slope in type C3 fractures. The posterior fragments thus should be reduced meticulously.
Availability of data and materials
The datasets analyzed in the current study are available from the corresponding author on reasonable request.
References
Lee AK, Cooper SA, Collinge C. Bicondylar tibial plateau fractures: a critical analysis review. JBJS Rev. 2018;6(2):e4. https://doi.org/10.2106/jbjs.Rvw.17.00050.
Elsoe R, Larsen P. Tibial plateau fractures are associated with a long-term increased risk of mortality: a matched cohort study of 7950 patients. Arch Orthop Trauma Surg. 2020;140(11):1705–11. https://doi.org/10.1007/s00402-020-03408-4.
Ebraheim NA, Sabry FF, Haman SP. Open reduction and internal fixation of 117 tibial plateau fractures. Orthopedics. 2004;27(12):1281–7. https://doi.org/10.3928/0147-7447-20041201-18.
Rademakers MV, Kerkhoffs GM, Sierevelt IN, Raaymakers EL, Marti RK. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma. 2007;21(1):5–10. https://doi.org/10.1097/BOT.0b013e31802c5b51.
Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Jt Surg Am. 2014;96(2):144–50. https://doi.org/10.2106/jbjs.L.01691.
Wong MT, Bourget-Murray J, Johnston K, Desy NM. Understanding the role of total knee arthroplasty for primary treatment of tibial plateau fracture: a systematic review of the literature. J Orthop Traumatol. 2020;21(1):7. https://doi.org/10.1186/s10195-020-00546-8.
Metcalfe D, Hickson CJ, McKee L, Griffin XL. External versus internal fixation for bicondylar tibial plateau fractures: systematic review and meta-analysis. J Orthop Traumatol. 2015;16(4):275–85. https://doi.org/10.1007/s10195-015-0372-9.
Rossi R, Bonasia DE, Blonna D, Assom M, Castoldi F. Prospective follow-up of a simple arthroscopic-assisted technique for lateral tibial plateau fractures: results at 5 years. Knee. 2008;15(5):378–83. https://doi.org/10.1016/j.knee.2008.04.001.
Chan YS, Chiu CH, Lo YP, Chen AC, Hsu KY, Wang CJ, et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthrosc J Arthrosc Relat Surg. 2008;24(7):760–8. https://doi.org/10.1016/j.arthro.2008.02.017.
Di Caprio F, Buda R, Ghermandi R, Ferruzzi A, Timoncini A, Parma A, et al. Combined arthroscopic treatment of tibial plateau and intercondylar eminence avulsion fractures. J Bone Jt Surg Am. 2010;92(Suppl 2):161–9. https://doi.org/10.2106/jbjs.J.00812.
Atesok K, Doral MN, Whipple T, Mann G, Mei-Dan O, Atay OA, et al. Arthroscopy-assisted fracture fixation. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):320–9. https://doi.org/10.1007/s00167-010-1298-7.
Chan YS, Yuan LJ, Hung SS, Wang CJ, Yu SW, Chen CY, et al. Arthroscopic-assisted reduction with bilateral buttress plate fixation of complex tibial plateau fractures. Arthrosc J Arthrosc Relat Surg. 2003;19(9):974–84. https://doi.org/10.1016/j.arthro.2003.09.038.
Abdel-Hamid MZ, Chang CH, Chan YS, Lo YP, Huang JW, Hsu KY, et al. Arthroscopic evaluation of soft tissue injuries in tibial plateau fractures: retrospective analysis of 98 cases. Arthrosc J Arthrosc Relat Surg. 2006;22(6):669–75. https://doi.org/10.1016/j.arthro.2006.01.018.
Chan YS. Arthroscopy- assisted surgery for tibial plateau fractures. Chang Gung Med J. 2011;34(3):239–47.
Chen XZ, Liu CG, Chen Y, Wang LQ, Zhu QZ, Lin P. Arthroscopy-assisted surgery for tibial plateau fractures. Arthrosc J Arthrosc Relat Surg. 2015;31(1):143–53. https://doi.org/10.1016/j.arthro.2014.06.005.
Duan XJ, Yang L, Guo L, Chen GX, Dai G. Arthroscopically assisted treatment for Schatzker type I-V tibial plateau fractures. Chin J Traumatol. 2008;11(5):288–92. https://doi.org/10.1016/s1008-1275(08)60058-9.
Jennings JE. Arthroscopic management of tibial plateau fractures. Arthrosc J Arthrosc Relat Surg. 1985;1(3):160–8. https://doi.org/10.1016/s0749-8063(85)80003-7.
Caspari RB, Hutton PM, Whipple TL, Meyers JF. The role of arthroscopy in the management of tibial plateau fractures. Arthros J Arthrosc Relat Surg. 1985;1(2):76–82. https://doi.org/10.1016/s0749-8063(85)80035-9.
Chiu CH, Cheng CY, Tsai MC, Chang SS, Chen AC, Chen YJ, et al. Arthroscopy-assisted reduction of posteromedial tibial plateau fractures with buttress plate and cannulated screw construct. Arthrosc J Arthrosc Relat Surg. 2013;29(8):1346–54. https://doi.org/10.1016/j.arthro.2013.05.003.
Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004;18(10):649–57. https://doi.org/10.1097/00005131-200411000-00001.
Ruffolo MR, Gettys FK, Montijo HE, Seymour RB, Karunakar MA. Complications of high-energy bicondylar tibial plateau fractures treated with dual plating through 2 incisions. J Orthop Trauma. 2015;29(2):85–90. https://doi.org/10.1097/bot.0000000000000203.
Morris BJ, Unger RZ, Archer KR, Mathis SL, Perdue AM, Obremskey WT. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J Orthop Trauma. 2013;27(9):e196-200. https://doi.org/10.1097/BOT.0b013e318284704e.
Krause M, Preiss A, Meenen NM, Madert J, Frosch KH. “Fracturoscopy” is superior to fluoroscopy in the articular reconstruction of complex tibial plateau fractures-an arthroscopy assisted fracture reduction technique. J Orthop Trauma. 2016;30(8):437–44. https://doi.org/10.1097/bot.0000000000000569.
Elsoe R, Johansen MB, Larsen P. Tibial plateau fractures are associated with a long-lasting increased risk of total knee arthroplasty a matched cohort study of 7950 tibial plateau fractures. Osteoarthritis Cartil. 2019;27(5):805–9. https://doi.org/10.1016/j.joca.2018.12.020.
Elabjer E, Benčić I, Ćuti T, Cerovečki T, Ćurić S, Vidović D. Tibial plateau fracture management: arthroscopically-assisted versus ORIF procedure - clinical and radiological comparison. Injury. 2017;48(Suppl 5):S61–4. https://doi.org/10.1016/s0020-1383(17)30742-8.
Deng X, Hu H, Zhang Y, Liu W, Song Q, Cheng X, et al. Comparison of outcomes of ORIF versus bidirectional tractor and arthroscopically assisted CRIF in the treatment of lateral tibial plateau fractures: a retrospective cohort study. J Orthop Surg Res. 2021;16(1):289. https://doi.org/10.1186/s13018-021-02447-w.
Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35(9):1443–9. https://doi.org/10.1177/0363546507304665.
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–82. https://doi.org/10.1177/0363546503258880.
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthrosc J Arthrosc Related Surg. 2006;22(8):894–9. https://doi.org/10.1016/j.arthro.2006.04.098.
Lee CC, Youm YS, Cho SD, Jung SH, Bae MH, Park SJ, et al. Does posterior tibial slope affect graft rupture following anterior cruciate ligament reconstruction? Arthrosc J Arthrosc Relat Surg. 2018;34(7):2152–5. https://doi.org/10.1016/j.arthro.2018.01.058.
Dean RS, Larson CM, Waterman BR. Posterior tibial slope: understand bony morphology to protect knee cruciate ligament grafts. Arthrosc J Arthrosc Relat Surg. 2021;37(7):2029–30. https://doi.org/10.1016/j.arthro.2021.05.006.
Streubel PN, Glasgow D, Wong A, Barei DP, Ricci WM, Gardner MJ. Sagittal plane deformity in bicondylar tibial plateau fractures. J Orthop Trauma. 2011;25(9):560–5. https://doi.org/10.1097/BOT.0b013e318200971d.
Eggli S, Hartel MJ, Kohl S, Haupt U, Exadaktylos AK, Röder C. Unstable bicondylar tibial plateau fractures: a clinical investigation. J Orthop Trauma. 2008;22(10):673–9. https://doi.org/10.1097/BOT.0b013e31818b1452.
Rohra N, Suri HS, Gangrade K. Functional and Radiological Outcome of Schatzker type V and VI Tibial Plateau Fracture Treatment with Dual Plates with Minimum 3 years follow-up: A Prospective Study. J Clin Diagn Res. 2016;10(5):RC05-10. https://doi.org/10.7860/jcdr/2016/18732.7855.
El Barbary H, Abdel Ghani H, Misbah H, Salem K. Complex tibial plateau fractures treated with Ilizarov external fixator with or without minimal internal fixation. Int Orthop. 2005;29(3):182–5. https://doi.org/10.1007/s00264-005-0638-6.
Chang H, Zheng Z, Yu Y, Shao J, Zhang Y. The use of bidirectional rapid reductor in minimally invasive treatment of bicondylar tibial plateau fractures: preliminary radiographic and clinical results. BMC Musculoskelet Disord. 2018;19(1):419. https://doi.org/10.1186/s12891-018-2343-9.
Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1(2):97–119.
Khatri K, Lakhotia D, Sharma V, Kiran Kumar GN, Sharma G, Farooque K. Functional evaluation in high energy (Schatzker type V and Type VI) tibial plateau fractures treated by open reduction and internal fixation. Int Sch Res Not. 2014;2014:589538. https://doi.org/10.1155/2014/589538.
Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005;439:207–14. https://doi.org/10.1097/00003086-200510000-00036.
Ochen Y, Peek J, McTague MF, Weaver MJ, van der Velde D, Houwert RM, et al. Long-term outcomes after open reduction and internal fixation of bicondylar tibial plateau fractures. Injury. 2020;51(4):1097–102. https://doi.org/10.1016/j.injury.2020.03.003.
Jiang L, Chen E, Huang L, Wang C. Arthroscopy-assisted reduction percutaneous internal fixation versus open reduction internal fixation for tibial plateau fracture: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(12):23259671211027840. https://doi.org/10.1177/23259671211027838.
van Dreumel RL, van Wunnik BP, Janssen L, Simons PC, Janzing HM. Mid- to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46(8):1608–12. https://doi.org/10.1016/j.injury.2015.05.035.
Belanger M, Fadale P. Compartment syndrome of the leg after arthroscopic examination of a tibial plateau fracture. Case report and review of the literature. Arthrosc J Arthrosc Relat Surg. 1997;13(5):646–51. https://doi.org/10.1016/s0749-8063(97)90196-1.
Herbort M, Domnick C, Petersen W. Arthroscopic treatment of tibial plateau fractures. Oper Orthop Traumatol. 2014;26(6):573–88. https://doi.org/10.1007/s00064-014-0328-x.
Acknowledgements
Not applicable
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Study concept and design, YSC; data analysis and interpretation, YHC; drafting of the article, YHC and CPY; writing—review and editing, CJW and SSC; supervision, CHC and YSC. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research study was conducted retrospectively from data obtained for clinical purposes and was approved by the Institutional Review Board of the authors’ hospital (No. 202101158B0C101). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, YH., Yang, CP., Chang, SS. et al. Arthroscopic-assisted reduction and internal fixation for complex tibial plateau fracture: radiographic and clinical outcomes with 2- to 15-year follow-up. J Orthop Surg Res 18, 448 (2023). https://doi.org/10.1186/s13018-023-03938-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03938-8