Abstract
Background
Patellar dislocation is common in young people. Although isolated anatomic double-bundle reconstruction of the MPFL is a common and effective surgical treatment for patellofemoral instability, concerns about the risk of injury to the epiphysis remain.
Methods
A total of 21 children and adolescents (9 males, 12 females; mean age: 10.7 years; range: 8 to 13 years) with recurrent patella dislocation or symptomatic instability following a primary dislocation were enrolled in the study. In all patients, double-bundle medial patellofemoral ligament (MPFL) reconstruction and femoral sling procedure were performed under arthroscopy, using an anterior half peroneus longus tendon (AHPLT) autograft. Functional outcomes were evaluated preoperatively and during follow-ups based on Kujala and Lysholm scores. Radiological examinations including radiographs, 3D-CT, and MRI were performed pre- and post-operatively.
Results
Among two-year postoperative follow-up (range: 24–42 months) showed significant improvement in functional scores (p < 0.01). The Lysholm score increased from 68 (44.5) to 100 (0) and the Kujala score increased from 26 (34.5) to 100 (2) The patellar tilt angel improved significantly (p < 0.01) from 24.3° ± 10.4 preoperatively to 11.9° ± 7.0 postoperatively. MRIs performed 6- and 12-months post operation did not show any signs of dysfunction of the reconstructed MPFL or cartilage degeneration.
Study design
Case Series; Level of evidence, 4.
Conclusion
Arthroscopic reconstruction of the MPFL using the modified sling procedure is an effective procedure for the treatment of patellar instability in skeletally immature patients.
Similar content being viewed by others
Introduction
The medial patellofemoral ligament (MPFL) is the main medial static stabilizer that restrains patellar lateralization during the initial 30° of knee flexion prior to patellar engagement into trochlea groove [1]. Rupture of the MPFL occurs in over 90% of all first patella dislocations and approximately 100% of re-dislocations [2]. Isolated MPFL reconstruction, especially anatomic double-bundle reconstruction, is the most common and effective surgical treatment for patellar instability in pediatric patients without severe osseous deformity [3,4,5]. However, femoral insertion of the MPFL is near to the distal femoral physis in children and adolescents [6]. The femoral drilling in the MPFL insertion is safe when performed properly but technically challenging [7, 8].
To avoid drilling at the femoral insertion and preserve the epiphysis, several MPFL reconstruction techniques, such as pedicled adductor transplantation, adductor sling technique, and medial collateral ligament (MCL) sling, have been proposed [9, 10]. However, the clinical outcomes of these techniques in children and adolescents have not been sufficiently investigated. In this study, we conducted anatomic double-bundle reconstruction in skeletally immature patients using a modified sling procedure (Scheme 1) under arthroscopy to minimize the risk of epiphyseal injury. The aim of this study was to evaluate outcomes of the modified adductor tendon sling procedure in children and adolescents with patellofemoral instability.
Methods
This retrospective study enrolled 21 patients with open physes who underwent double-bundle MPFL reconstruction under arthroscopy using anterior half peroneus longus tendon (AHPLT) autograft and femoral sling procedure between 2018 and 2020 (Table 1). The study was approved by the Medical Ethics Committee of Taizhou Hospital Affiliated to Wenzhou Medical University (K20211225). Children and adolescents with recurrent patella dislocation or symptomatic instability following primary dislocation were enrolled for the study. The exclusion criteria were as follows: fractures requiring open reduction or fixation and ipsilateral anterior/posterior cruciate ligament injury. Elevated tibial tuberosity trochlear groove distance (TT-TG > 2.0) and patella alta (Caton-Deschamps > 1.2) were no contraindication.
The functional outcomes preoperatively and in subsequent follow-ups (6, 12, 24 months post-operation) were evaluated based on Kujala and Lysholm scores. Further, radiological examination, including preoperative and postoperative radiographs, 3D-CT, and MRI, were conducted. The main evaluation parameter was the patellar tilt angle (the angle between the femoral posterior condylar line and the line defining the maximal patellar width) (Fig. 1). In addition, fracture, cartilage degeneration, tendon healing, and complications were recorded.
Surgical technique
Patients were placed on the operation table in a supine position. A physical examination was carried out under anesthesia to evaluate patellar stability before surgery. Standard arthroscopy was performed through anteromedial and anterolateral portals (Fig. 2a) to verify the MPFL injury and other pathologies (Fig. 3a). A 1.5–2 cm longitudinal incision was made over the peroneus tendon behind the lateral ankle (Fig. 2b). The peroneus longus tendon was exposed, and the anterior half of the tendon (1/2 to 2/3) was harvested (Fig. 2c). Subsequently, the graft was trimmed to the required length (14–20 cm), and the ends were braided with No.5 Ethibond sutures (Ethicon, Somerville, NJ, USA) (Fig. 2d).
Arthroscopic the medial patellofemoral ligament (MPFL) reconstruction procedure. a Tear of the MPFL and the capsule was viewed at the patellar attachment (11 o’clock position); b A superomedial capsular window above the synovia plication in the medial gutter was created from inside; c The adductor magnus tendon proximal to the MPFL was exposed through the capsular window; d The proximal insertion of the adductor magnus was separated by a right-angle clamp and a shuttle suture was threaded; e The implanted autograft was introduced under the suture guidance and fixed with a sling around the adductor magnus tendon; f The double-bundle autograft was located at the outer layer of the capsule and fastened to the medial facet of the patella. White arrow: adductor magnus; black arrow: capsure; * autograft; # MPFL
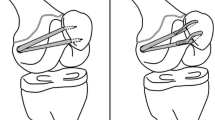
The arthroscope was moved to the anteromedial approach for observation. Thereafter, auxiliary approaches were established on the medial and lateral sides of the patella and over the medial epicondyle (Fig. 2a). Two 2.0 mm Kirschner wires were used to drill tunnels from the medial upper corner and middle part of the patella to the lateral side. Further, two No. 0 PDSII suture loops were passed through the bone tunnels and reserved as suture shuttles. The posteromedial capsule above the synovia plication in the medial gutter was opened from inside while maintaining knee extension (Fig. 3b). Loose fibrous tissues were debrided to expose the residual MPFL and insertion of the proximal adductor tendon (Fig. 3c). A No.0 PDSII suture was introduced to loop around the adductor magnus tendon (Fig. 3d). Thereafter, the autograft was pulled in (Fig. 3e) under the suture guidance. A vessel clamp was bluntly penetrated from the medial patellar edge to the adductor tuberosity between the second and third tissue layer outside the joint capsule. Both free ends of the autograft were grabbed out and passed across the patella from the patellar aponeurosis surface. Furthermore, the Ethibond sutures of the free ends were folded back through the bone tunnel under the guidance of the reserved PDSII sutures (Scheme 1). The sutures were tensioned and knotted to fasten the tendon to the medial facet of the patella with the knee flexed at 30° (Fig. 3f). To verify appropriate tension of the constructed MPFL, the patella was displaced laterally with the knee flexed at 20°. The range shifted within one quadrant of the patella [11].
Postoperative rehabilitation
A hinged knee brace was used to protect the injured knee. The patient was encouraged to perform ankle exercise, isometric contraction of the quadriceps. In addition, active extension and passive flexion of knee were encouraged using the contralateral limb. The range of motion was not limited in the non-weight-bearing position. Full weight-bearing walking was allowed with the knee brace locked at full extension in patients who could fully extend the knee joint actively or maintain a straight leg raise for more than one minute. Patients who achieved 90° flexion were discharged from hospital. Full range and full weight-bearing exercises were encouraged under the protection of the brace at three weeks post-surgery. The brace was removed after six weeks. Moreover, the patient was encouraged to perform exercises, such as cycling, jogging, or squatting. They were also allowed participate in recreational sports after three months. After four to six months, patients were allowed to participate in more strenuous sports. Thereafter, they were allowed to engage in competitive sports depending on the muscle strength.
Statistical analysis
Data analysis was performed with statistical software (SPSS v.25, IBM Inc., Harmonk, NY, USA). Normality of numerical data were assessed by Shapiro–Wilk test. Descriptive statistics were reported as means and standard deviations (SD) for normally distributed numerical data, otherwise medians and interquartile ranges (IQR) were used. Comparisons between groups both at baseline and at follow-up were performed by use of Student’s t test for normally distributed data, otherwise the Wilcoxon matched pairs signed rank test was used. Significance was set at p ≤ 0.05.
Results
21 patients (9 males, 12 females; mean age: 10.7 years; range: 8 to 13 years) completed the scheduled follow-up (6, 12, 24 months). The mean age of patients was 10.7 years (range, 8–13) with two years follow-up. Six patellar avulsion fractures and two lateral condylar cartilage exfoliation fractures were recorded during the operation, and debridement was performed. A two-year follow up showed that the functional scores had improved significantly (p < 0.01) (Table 2). Lysholm score increased from 68 (44.5) to 100 (0) and the Kujala score increased from 26 (34.5) to 100 (2). There were no recurrent patellar dislocations at the final follow-up. Moreover, the patellar tilt angel improved significantly (p < 0.01) from 24.3° ± 10.4 preoperatively to 11.9° ± 7.0 12-months postoperatively (Table 2). Furthermore, no patellar fractures were reported. MRIs of the knee conducted 6 and 12 months postoperatively did not show any signs of dysfunction of the reconstructed MPFL or cartilage degeneration (Fig. 4).
After surgery, patients were followed up every 6 months. The inflammatory response was present postoperatively at 6 months (a, b), but was disappeared postoperatively at 12 months (c, d). The reconstructed ligament healed well and no signs of dysfunction were observed in both time points. Relaxation, creep deformation or discontinuity of the reconstructed MPFL was considered to be dysfunction. White arrow: reconstructed MPFL; *: inflammatory response
Discussion
In this study, we conducted MPFL reconstruction in skeletally immature patients using a modified sling procedure under arthroscopy to prevent the risk of epiphyseal injury. Postoperative follow-ups revealed a significant improvement in functional scores and radiological parameters.
Patellar dislocation is common in the young people. Although conservative management has a certain therapeutic effect in patellar dislocation, it is associated with a recurrent rate of 69% [12]. The morphology of patella and femoral trochlear can be improved by maintaining the correct contrapuntal relationship [13,14,15]. Therefore, early surgical intervention is indicated in skeletally immature patients with primary or recurrent patellar dislocation [16, 17]. Isolated anatomic double-bundle reconstruction of the MPFL is the common and effective surgical treatment for patellofemoral instability [5]. The femoral tunnel point is commonly identified using Schottle’s method [18]. However, in skeletally immature patients, the “Schottle point” is close to the distal femoral physis, which increases risk of injury to the epiphysis [6]. To avoid tunneling on the femoral attachment or hardware placement, non-anatomical reconstruction techniques have been developed. Using adductor magnus insertion as the femoral attachment point of MPFL may show a quasi-isometric effect because the adductor tubercle is close to the superior aspect of the MPFL femoral attachment (the most isometric point) [19]. Additionally, the attachment of MPFL and adductor tendon is a way of elastic fixation, which can compensate for the slight length mismatch of the reconstructed MPFL during mobility [10, 20]. Therefore, the adductor sling procedure with free graft was proposed for the reconstruction of MPFL.
The sling procedure has been described in various studies (Table 3). Gomes et al. showed that the dynamic femoral fixation was superior to that of rigid alternative. Patients who underwent the sling procedure were more likely to feel subjectively better and could participate in sports. The graft was passed through the osteoperiosteal tunnel under the adductor insertion and then looped around the adductor insertion. However, this procedure is associated with a risk of insertion detachment. Furthermore, it is less elastic compared with the adductor magnus tendon fixation. Monllau et al. reported excellent clinical and radiological outcomes in 16 adults who underwent isolated double-bundle MPFL reconstruction using the adductor magnus tendon sling technique. However, Gomes et al. and Monllau et al. included adult patients with different anatomical and biomechanical characteristics from children and adolescents. Yercan et al. reported no redislocations in three cases (four knees) following reconstruction using the sling technique. In contrast, Lind et al. reported 20% redislocation rates and 25% subluxation rates in 24 patients who underwent single-bundle MPFL reconstructions using the sling procedure. Notably, 5 of the 24 patients needed revision within one year of surgery due to recurrent patellar instability. Suturing the graft to the proximal (MCL) insertion area beside the adductor sling may result in graft elongation, which increases the risk of instability. In this study, we performed double-bundle MPFL reconstructions using a modified sling procedure whereby an isolated adductor magnus tendon sling was adopted at the femoral side. The procedure did not involve suturing or osteoperiosteal tunneling at the femoral side. It had the following advantages: (i) simple operation. (ii) fixation by looping against the adductor insertion maximized the quasi-isometric and elastic characteristics without causing over elongation of the graft. (iii) because no suturing of the adductor tendon or MCL was performed, the dynamic fixation allowed for rebalancing of the length and tension of the two bundles during postoperative flexion and extension. (iv) once a balance was achieved, the graft was immobilized and gradually healed together with the surrounding tissue. The MRI conducted postoperatively did not show any graft dysfunction (Fig. 4).
Adolescents have a smaller patellar volume and thus tunneling may increase the risk of patellar fractures. Therefore, in this study, patella perforation and graft fixation were performed using looped back braided sutures. In previous studies, the use of similar techniques was shown to be effective [21]. In this study, two 2.0 mm holes were drilled into the patella. Further, the bone bridge was maintained at 10 to 15 mm. This method significantly reduced the risk of patella fracture and improved patella growth. More importantly, the method allowed precise regulation of the reconstructed MPFL tension intraoperatively.
According to Zhao et al., the average failure load of the AHPLT was 322.35 ± 63.18 N [22], closing to the strength of the semitendinosus tendon, and the applicable length of AHPLT was about 24 cm. Besides, cutting only the anterior 1/2 to 2/3 of AHPLT maximizes structural integrity. The small incision point for harvesting the tendon is hidden behind the ankle joint, making it aesthetically appealing (Fig. 2b, c). Therefore, the AHPLT is an efficient autograft for the reconstruction of MPFL.
In arthroscopic surgery, only a small capsular window is required to expose the adductor and the medial patellar facet [23]. Furthermore, lateral retinacular release, debridement of small chondral fragments, and meniscus plasty or repair can be performed simultaneously. Arthroscopic surgeries are minimally invasive and more aesthetically appealing than open surgeries. Additionally, arthroscopic surgeries are more suitable for obese patients and patients who are overly distressed by scars. This study provides ideas for the improvement of MPFL reconstruction. Future large-scale studies are warranted to evaluate the long-term outcomes of the proposed technique.
Conclusion
Arthroscopic reconstruction of the MPFL using a modified sling procedure is an effective procedure for the treatment of patellar instability in skeletally immature patients. This technique improved functional scores and radiological outcomes without major complications.
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Hensler D, Sillanpaa PJ, Schoettle PB. Medial patellofemoral ligament: anatomy, injury and treatment in the adolescent knee. Curr Opin Pediatr. 2014;26(1):70–8.
Yeung M, Leblanc MC, Ayeni OR, Khan M, Hiemstra LA, Kerslake S, Peterson D. Indications for medial patellofemoral ligament reconstruction: a systematic review. J Knee Surg. 2016;29(7):543–54.
Bouras T, Brown EUA, Gallacher P, Barnett A. Isolated medial patellofemoral ligament reconstruction significantly improved quality of life in patients with recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3513–7.
Zhang L, Li Z. Long-term clinical results of double bundle reconstruction of the medial patellofemoral ligament for patellar instability. J Knee Surg. 2019;32(2):153–9.
Weinberger JM, Fabricant PD, Taylor SA, Mei JY, Jones KJ. Influence of graft source and configuration on revision rate and patient-reported outcomes after MPFL reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2511–9.
Farrow LD, Alentado VJ, Abdulnabi Z, Gilmore A, Liu RW. The relationship of the medial patellofemoral ligament attachment to the distal femoral physis. Am J Sports Med. 2014;42(9):2214–8.
Seitlinger G, Moroder P, Fink C, Wierer G. Acquired femoral flexion deformity due to physeal injury during medial patellofemoral ligament reconstruction. Knee. 2017;24(3):680–5.
Nguyen CV, Farrow LD, Liu RW, Gilmore A. Safe drilling paths in the distal femoral epiphysis for pediatric medial patellofemoral ligament reconstruction. Am J Sports Med. 2017;45(5):1085–9.
Monllau JC, Masferrer-Pino A, Ginovart G, Perez-Prieto D, Gelber PE, Sanchis-Alfonso V. Clinical and radiological outcomes after a quasi-anatomical reconstruction of medial patellofemoral ligament with gracilis tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2453–9.
Dalla-Rosa J, Nogales JJ, Verdejo M, Nogales JI. Medial patellofemoral ligament reconstruction: use of all-suture anchors for patellar fixation and a dynamic femoral attachment. Arthrosc Tech. 2021;10(5):e1345–50.
Elias JJ, Jones KC, Lalonde MK, Gabra JN, Rezvanifar SC, Cosgarea AJ. Allowing one quadrant of patellar lateral translation during medial patellofemoral ligament reconstruction successfully limits maltracking without overconstraining the patella. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):2883–90.
Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41(3):575–81.
Li W, Wang Q, Li H, Wang S. Changes in patellar morphology following surgical correction of recurrent patellar dislocation in children. J Orthop Surg Res. 2021;16(1):607.
Richmond CG, Shea KG, Burlile JF, Heyer AM, Ellis HB, Wilson PL, Arendt EA, Tompkins MA. Patellar-Trochlear morphology in pediatric patients from 2 to 11 years of age: a descriptive analysis based on computed tomography scanning. J Pediatr Orthop. 2020;40(2):e96–102.
Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):663–70.
Migliorini F, Eschweiler J, Betsch M, Knobe M, Tingart M, Maffulli N. Prognostic factors for isolated medial patellofemoral ligament reconstruction: a systematic review. Surg: J R Coll Surg Edinb Ireland. 2022;20(4):e112–21.
Vetrano M, Oliva F, Bisicchia S, Bossa M, De Carli A, Di Lorenzo L, Erroi D, Forte A, Foti C, Frizziero A, Gasparre G, Via AG, Innocenti B, Longo UG, Mahmoud A, Masiero S, Mazza D, Natali S, Notarangelo C, Osti L, Padulo J, Pellicciari L, Perroni F, Piccirilli E, Ramponi C, Salvatore G, Panni AS, Suarez T, Tarantino U, Vittadini F, Vulpiani MC, Ferretti A, Maffulli N, Mu IS. L.T. first-time patellar dislocation guidelines, Muscles Ligaments Tendons J 2017;7(1), 1–10.
Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–4.
Melegari TM, Parks BG, Matthews LS. Patellofemoral contact area and pressure after medial patellofemoral ligament reconstruction. Am J Sports Med. 2008;36(4):747–52.
Perez-Prieto D, Capurro B, Gelber PE, Ginovart G, Reina F, Sanchis-Alfonso V, Monllau JC. The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2420–3.
Pilone C, Bonasia DE, Rosso F, Cottino U, Mazzola C, Blonna D, Rossi R, Sigascot C. Knee, medial patellofemoral ligament reconstruction and nonanatomic stabilization techniques in skeletally immature patients. Joints 2019;7(3), 98–106.
Zhao J, Huangfu X. The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med. 2012;40(3):662–71.
Gao G, Liu P, Xu Y. Treatment of patellar dislocation with arthroscopic medial patellofemoral ligament reconstruction using gracilis tendon autograft and modified double-patellar tunnel technique: minimum 5-year patient-reported outcomes. J Orthop Surg Res. 2020;15(1):25.
Yercan HS, Erkan S, Okcu G, Ozalp RT. A novel technique for reconstruction of the medial patellofemoral ligament in skeletally immature patients. Arch Orthop Trauma Surg. 2011;131(8):1059–65.
Gomes JE. Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy. 2008;24(4):430–5.
Lind M, Enderlein D, Nielsen T, Christiansen SE, Fauno P. Clinical outcome after reconstruction of the medial patellofemoral ligament in paediatric patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):666–71.
Funding
This work was funded by Zhejiang Provincial Health Science and Technology Project of Traditional Chinese Medicine (2019329567).
Author information
Authors and Affiliations
Contributions
Research design/Writing and revision: Q.Z., L.Y.; Data collection/ Data analysis: P.L., D.H., L.Y., T.-H.T., J.L.; Concept/idea/project management: X.Z. All the author have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Medical Ethics Committee of Taizhou Hospital Affiliated to Wenzhou Medical University (K20211225).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Q., Ying, L., Han, D. et al. Arthroscopic reconstruction of the medial patellofemoral ligament in skeletally immature patients using the modified sling procedure: a novel technique for MPFL reconstruction. J Orthop Surg Res 18, 334 (2023). https://doi.org/10.1186/s13018-023-03775-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03775-9