Abstract
Aims
The objective of this study was to evaluate the accuracy of acetabular cup positioning in the obese patients when using robotic-assisted technology during total hip arthroplasty (THA).
Methods
Data were retrospectively collected from patients who underwent primary (THA) with a body mass index (BMI) ≥ 28 kg/m2 and ≥ 1 year of follow-up between January 2018 and December 2019. Their demographics, diagnosis, acetabular cup positioning, American Society of Anesthesiologists (ASA) score, Harris Hip Score (HHS), and Forgotten Joint Score (FJS) at the final follow-up were recorded for analysis.
Results
There were no statistically significant differences between the two groups in height, weight, BMI, ASA score, or preoperative Harris Hip Score (HHS). Also, there was no difference in inclination angle between the two groups (R-THA: 41.29° ± 3.04°; manual THA (M-THA): 40.47° ± 5.46°; P = 0.312). However, the mean anteversion angle was greater in the R-THA group (20.71° ± 1.98° vs. 19.08° ± 4.04°; P < 0.001). Compared to M-THA, R-THA more frequently achieved an acetabular cup angle within 5° of the target (anteversion, 98.1% vs. 78.1% P = 0.001; inclination, 88.5% vs. 53.1%, P < 0.001). The R-THA group was more advantageous in restoring the hip center of rotation (COR) and leg length difference (LLD). There was no statistical difference in postoperative HHS (P = 0.404) or FJS (P = 0.497) between the two groups.
Conclusions
Compared to manual technique, robotic-assisted technique provided more precise acetabular cup positioning and better leg length restoration for obese patients. The robotic-assisted technique was more advantageous in recovering the center of rotation position and achieved a higher proportion of the acetabular cup placed in the target safety zone. Further studies are needed to confirm the clinical outcomes of surgeries in obese patients using robotic-assisted technology.
Similar content being viewed by others
Introduction
Body mass index (BMI) is defined as the weight in kilograms divided by the square of the height in meters (kg/m2); a BMI ≥ 24 kg/m2 is classified as overweight and a BMI ≥ 28 kg/m2 as obese, according to Chinese standards [1]. Obesity is a major risk factor for hypertension, diabetes, dyslipidemia, coronary artery disease, myocardial infarction, stroke, breast cancer, and other cancers and has been identified by the World Health Organization as the fifth risk factor affecting health. It is also associated with increased rates of osteoarthritis, particularly in load-bearing joints such as the hip [2].
The increasing prevalence of obesity, combined with the growing demand for THA in the older population, presents a unique set of challenges to the surgeon [3]. Obesity had been shown to negatively affect the outcome of total hip arthroplasty, with a higher incidence of hip dislocation, aseptic loosening, infection, and venous thromboembolism [4,5,6]. Acetabular cup mispositioning can increase the risk of dislocation, bearing surface wear, and cup instability [7,8,9]. How to precisely implant cups in THA in obese patients to avoid obesity-related complications and obtain good clinical and radiological results is the focus and difficulty of this procedure.
At our institution, we use robotic-assisted computer navigation technology during THA for more precise positioning of the acetabular cup and better clinical outcomes [10, 11]. This study compared the accuracy of robotic-assisted THA (R-THA) and manual THA (M-THA) for acetabular placement in obese patients, to clarify the value of robotic-assisted techniques for obese patients.
Materials and methods
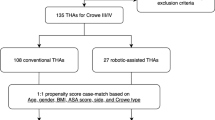
This study retrospectively reviewed M-THA and R-THA procedures carried out in our institute between January 2018 and December 2019. Inclusion criteria were: (1): obese patients undergoing primary THA (BMI ≥ 28 kg/m2), (2) all surgeries were performed through the posterolateral approach, (3) follow-up time ≥ 1 year. Exclusion criteria were: (1) age less than 18 years old or more than 75 years old, (2) abnormal gait due to neuromuscular insufficiency (including paralysis, rhabdomyolysis, abductor muscle weakness, etc.), (3) combined inflammatory diseases affecting normal activities, cooperation and poor compliance, unable to complete postoperative follow-up assessment, and (4) the patients with incomplete clinical data or nonstandard radiographs. Patients were informed preoperatively that the use of robotic-assisted techniques could result in increased radiation doses, longer operating times, and increased bleeding, costs, and complications. Ultimately, each patient decided whether to undergo robotic-assisted surgery. Patients who met the inclusion criteria were divided into R-THA and M-THA groups according to whether they underwent robotic-assisted technology. All preoperative planning and surgery were performed by one senior surgeon. The MAKO robotic hip system (MAKO Rio Robot; Stryker, USA) was used in our institution, which the system was programmed with THA3.1 for acetabular reaming during bone preparation and cup placement. Institutional review board approval was obtained before starting this study (S2019⁃052⁃01).
Preoperative planning
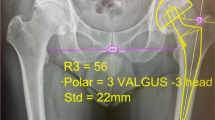
Patients scheduled for manual THA had a preoperative plan based on anteroposterior pelvic radiographs using OrthoView 7.0 software (Meridian, UK) to determine cup placement, size, and balance the difference of lower limbs. Patients scheduled for R-THA had a preoperative computed tomography (CT) scan from the iliac wing to the femoral condyle. The CT data were transferred to the MAKO planning module for preoperative planning, with coronal alignment performed based on the anterior superior iliac spine line, anatomical landmarks, and acetabular segmentation modeling. Virtual cup implantation was performed to determine the optimal cup size, angle, and position, which were confirmed by the senior surgeon. The target position of the acetabular cup was 40° of inclination and 20° of anteversion, which could be fine-tuned preoperatively and intraoperatively according to the bone coverage of the acetabular cup.
Robotic-assisted THA surgical technique
The surgical technique has been described previously [12]. A standardized posterolateral surgical approach was adopted under general anesthesia in both groups. During the procedure, three pins were implanted at the anterior superior iliac spine to fix the pelvic reference frame and fixed adhesive electrodes attached to the patella for intraoperative assessment of leg length. The surgeon began preliminary exposure after the pelvic array had been attached and a locating pin was inserted at the outer edge of the greater trochanter to assess leg length and offset. Subsequently, joint dislocation and femoral neck osteotomy were performed. The acetabulum was registered using a pelvic checkpoint screw inserted outside the acetabulum. The acetabular registration includes 3 acetabular direction determination points, 32 registration points, and 8 confirmation points. The three-dimensional (3D) model based on preoperative CT corresponds to the real anatomical structure of the hip joint. Robotic-assisted acetabular reaming and acetabular cup implantation were performed under 3D real-time navigation according to the preoperative plan. The acetabular screws and liner impacted in place and the femur were prepared manually. Stability of the hip joint was checked by the surgeon through a full range of hip motion and captured the landmarks to measure leg length and offset. Finally, the real femoral stem and head were implanted.
Manual THA surgical technique
The surgical steps were the same for M-THA, except that the acetabular surgery was performed manually. The smallest reamer was used to determine the acetabular bottom, then the larger reamers in turn to prepare the acetabulum. When the acetabular cup was implanted, we ensured that the cup was implanted at a (20/40) angle by using an antenna. Leg length was assessed intraoperatively by palpating the alignment of the inferior poles of both patellae. Patients in both treatment groups received the Accolade II femoral stem (Stryker, USA) and Trident acetabular shell (Stryker, USA).
Clinical and radiographic measurements
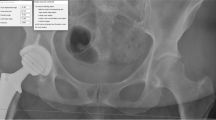
Patients were followed up routinely at 3, 6, and 12 months postoperatively, and annually thereafter. Anteroposterior pelvic radiographs were taken in the supine position at follow-up, and demographic, radiographic, and surgical data were collected from patients, including gender, age, BMI, diagnosis, acetabular cup positioning, postoperative complications, Harris Hip Score (HHS), and Forgotten Joint Score (FJS). When taking postoperative X-rays, the hips were in 10°–15° of internal rotation and the X-ray beam centered over the pubic symphysis. The longitudinal axis of the body and legs was parallel to the imaging table. The ceramic femoral head was used to calibrate the radiographs to eliminate magnification error. Acetabular cup positioning was measured from supine anteroposterior pelvic radiographs at the 1-year follow-up using OrthoView 7.0 (Meridian), which has shown good accuracy for measuring inclination and anteversion [12,13,14].
Anteversion was the angle between the short and long axes of the ellipse projected by the cup and was equal to arcsin (short axis/long axis). Inclination of cup was the angle between the cup’s long axis and the trans-teardrop line or the trans-ischial tuberosity line [12, 15,16,17]. The leg length difference (LLD) was the difference in distance from the line of the bilateral teardrop to the most prominent point of the small trochanter by Ranawat [18]. The horizontal center of rotation (HCOR) was measured as the distance between the center of rotation and a vertical line intersecting the trans-teardrop line, and the vertical center of rotation (VCOR) was measured as the vertical distance between the COR and the trans-teardrop line [19]. The discrepancy between the horizontal and vertical distances of the bilateral COR was taken to evaluate the position of the COR, expressed as HCOR-d and VCOR-d, respectively. Measurements were completed by two experienced physicians, and the interobserver intra-group correlation coefficient was 0.911, indicating good agreement. The final mean value of the two measurements was taken.
Statistical analysis
Descriptive statistics were presented as means with the standard deviation. The Student’s t test was used for between-group comparisons parametric continuous variables, and categorical variables were analyzed using Chi-squared tests or Fisher’s exact test. All statistical tests were performed at a probability level of 95% (α = 0.05). SPSS for Windows (version 25.0; SPSS Inc., Chicago, IL, USA) was used for the analysis.
Results
Demographics
A total of 89 patients (116 hips) were included, of whom 41 patients (52 hips) underwent robotic-assisted THA and 48 patients (64 hips) underwent manual THA (Table 1). The mean patient age was lower in the M-THA group (R-THA: 53.38 ± 11.57 vs M-THA: 44.02 ± 12.003 years, P < 0.001). There were no statistically significant differences in gender, BMI, diagnosis, ASA, and preoperative HHS between the two groups.
Acetabular cup positioning
The mean inclination in the R-THA and M-THA groups was 41.29° ± 3.04° and 40.47° ± 5.46°, respectively (P > 0.05). However, the mean anteversion in the R-THA and M-THA groups was 20.71° ± 1.98° and 19.08° ± 4.04°, respectively, with a statistically significant difference between the two groups (P < 0.001) (Table 2). The frequency of an angle within 10° of the target was not different between the R-THA and M-THA groups, but acetabular cup positioning within 5° of the target was significantly (P = 0.001) more prevalent in the R-THA group for anteversion (98.1% vs. 78.1%). In the R-THA group, 88.5% of the acetabular cups were within 5° of the target angle with respect to inclination, which was a significantly higher rate compared to the M-THA group (53.1%; P < 0.001). The robotic-assisted technique was thus more accurate and consistent with respect to placement of the acetabular cups than manual surgery (Figs. 1, 2) (Table 3).
The robotic-assisted technique was significantly more accurate than the manual technique in restoring the COR (Table 2) and had a significant advantage in balancing leg length (2.9 ± 1.6 vs. 7.3 ± 2.6 mm, P < 0.001), as confirmed by further analysis (Table 2).
Postoperative function
The HHS and FJS were significantly higher in both groups compared to the preoperative period with no statistical difference between the two groups (HHS: P = 0.404; FJS: P = 0.497) (Table 2).
Complications
There were no THA-related complications, signs of cup loosening, and revision during follow-up.
Discussion
To our knowledge, this is the first case–control study comparing acetabular cup positioning between R-THA and M-THA in obese patients. A previous study showed that higher BMI does not affect the accuracy of cup placement in robot-assisted total hip arthroplasty [10]. However, that study did not compare R-THA to the manual technique, and patient clinical outcomes were not studied. Robotic-assisted THA had been in the clinic for nearly 30 years. Some studies had shown that robotic-assisted THA had advantages in terms of cup position, lower extremity length control, complications, and short-term functional prognosis [12, 15, 20,21,22]. Another advantage of robotic-assisted technique was the preparation of the surgical plan based on preoperative CT and the use of easily identifiable bone landmarks as reference points during surgery, which can help the surgeon perform procedures in cases where the soft tissue envelope may make accurate implant positioning difficult.
The main difficulties in THA for obese patients include the thick subcutaneous soft tissue, difficulty exposing the acetabulum and femur, and narrow field, which can lead to inadequate intraoperative acetabular bone preparation, poor cup placement, and an increased risk of cup mispositioning [23]. However, the relationship between higher BMI and higher risk of instability or related mechanical complications had not been universally established [4, 24, 25]. Therefore, THA in obese patients presents a formidable challenge to surgeons, and the precise acetabular cup and femoral stem placement were the keys to reduce prosthesis loosening, dislocation, and achieving good outcomes after THA [4, 26]. Accurate acetabular cup positioning and avoidance of cup-related complications remain the primary surgical goals.
We showed that the target acetabular cup positioning could be excellent achieved using both robotic-assisted and manual techniques. However, the standard deviations of both anteversion and inclination were lower in the robot-assisted group. In further analysis, we found that with the target angle of the acetabular cup within 10°, 100% of the anteversion and 98.1% of inclination in both groups were within this range. However, within 5° of the target angles of the acetabular cup, the percentages of the R-THA and M-THA anteversions were 98.1% and 78.1%, respectively, and the inclinations were 88.5% and 53.1%, respectively. This showed that the robotic-assisted technique could be able to achieve the target acetabular cup position (20/40) more precisely and reproducibly than the manual technique in obese patients.
Inaccurate center of rotation (COR) restoration is associated with impingement, reduced hip abductor strength, altered gait kinematics, reduced postoperative hip range of motion, trochanteric pain, instability, and higher rates of wear [19, 27,28,29]. The horizontal distance of the COR is also considered as the acetabular offset. In addition, a study has shown that the concept of the offset cannot be limited to that of the femoral offset, which acetabular offset widely varies between individuals, and the acetabular floor distance can be up to 13 mm, which should not be ignored by surgeons [30]. Therefore, accurate restoration of the COR is essential for accurate reconstruction of the normal hip anatomy. Our results showed that the robotic-assisted technique was more accurate for restoring the horizontal and vertical distances of centers of rotation with less variation; although the difference between was relatively small, there may be small but important improvements for obese patients.
Leg length discrepancy is a common problem after THA, which is associated with persistent postoperative pain, decreased abductor function, hip instability, impingement, increased surface wear, and early failure, leading to poorer outcomes and patient dissatisfaction, and is a major cause of litigation against orthopedic surgeons [31,32,33]. Previous studies have shown an obvious advantage of robotic-assisted techniques in restoring leg length discrepancy [15, 22, 34]. This was also demonstrated in our study, as no patients had LLD exceeding 10 mm in the robotic group. In the manual group, there were eight patients with LLD exceeding 10 mm. We analyzed that the first reason could be that obese patients could not achieve the standard lateral position during surgery, resulting in an inability to accurately determine LLD intraoperatively. Second, because obese patients had more soft tissue, which resulted in increased exposure and soft tissue release and the risk of dislocation, therefore, sacrificing leg length was unavoidable in order to achieve satisfactory soft tissue tension and joint stability.
There are several limitations in our study. Firstly, it was a retrospective case–control study, where this design has inherent flaws and biases. Secondly, when comparing the demographics of the two groups, the robotic group was elder (53.38 ± 11.57 vs. 44.02 ± 12.003), which was mainly due to the fact that the MAKO robot system can only use a ceramic-to-polyethylene interface, while relatively younger patients prefer ceramic-to-ceramic prostheses. However, there was no difference in the preoperative functional status of the hip between the two group, and the postoperative follow-up results of both groups were significantly improved and not statistically different compared to the preoperative period, which to a certain extent reflects the advantage of robotic-assisted technology in short-term clinical outcomes. Thirdly, although the accuracy of OrthoView system measurements has been demonstrated, measurement bias cannot be ignored. X-ray-based postoperative measurements are inferior to computed tomography (CT) and magnetic resonance imaging (MRI); however, studies have confirmed that X-rays have the same accuracy as CT [35,36,37]. Fourthly, due to the relatively small sample size of our study, and the relatively small number of morbidly obese patients in China, no analysis stratified by BMI was conducted. Finally, the follow-up period of patients in this study was greater than 1 year, but it was still a short-term study, in which the long-term clinical outcomes and complications also need to be further followed up.
Conclusion
Compared to manual technique, robotic-assisted technique provided more precise acetabular cup positioning and better leg length restoration for obese patients. The robotic-assisted technique was more advantageous in recovering the center of rotation position and achieved a higher proportion of the acetabular cup placed in the target safety zone. The postoperative functional scores of the two groups were significantly improved compared with preoperative, and there was no statistical difference. Further studies are needed to confirm the clinical outcomes of surgeries in obese patients using robotic-assisted technology.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- THA:
-
Total hip arthroplasty
- HHS:
-
Harris Hip Score
- BMI:
-
Body mass index
- SD:
-
Standard deviation
- ONFH:
-
Osteonecrosis of the femoral head
- OA:
-
Osteoarthrosis
- DDH:
-
Developmental dysplasia of hip
- CT:
-
Computerized tomography
- MRI:
-
Magnetic resonance imaging
- R-THA:
-
Robotic-assisted total hip arthroplasty
- M-THA:
-
Manual total hip arthroplasty
- ASA:
-
American Society of Anesthesiologists
- LLD:
-
Leg length discrepancy
- COR:
-
Center of rotation
- HCOR-d:
-
The horizontal center of rotation discrepancy
- VCOR-d:
-
The vertical center of rotation
- FJS:
-
Forgotten Joint Score
References
Hu L, Huang X, You C, Li J, Hong K, Li P, et al. Prevalence and risk factors of prehypertension and hypertension in Southern China. PLoS ONE. 2017;12(1):e0170238.
Andrew JG, Palan J, Kurup HV, Gibson P, Murray DW, Beard DJ. Obesity in total hip replacement. J Bone Joint Surg Br. 2008;90(4):424–9.
Smith EL, Shahien AA, Chung M, Stoker G, Niu R, Schwarzkopf R. The Obesity Paradox: body mass index complication rates vary by gender and age among primary total hip arthroplasty patients. J Arthroplasty. 2020;35(9):2658–65.
Haverkamp D, Klinkenbijl MN, Somford MP, Albers GH, van der Vis HM. Obesity in total hip arthroplasty—does it really matter? A meta-analysis. Acta Orthop. 2011;82(4):417–22.
Goodnough LH, Finlay AK, Huddleston JI, Goodman SB, Maloney WJ, Amanatullah DF. Obesity is independently associated with early aseptic loosening in primary total hip arthroplasty. J Arthroplasty. 2018;33(3):882–6.
Liu W, Wahafu T, Cheng M, Cheng T, Zhang Y, Zhang X. The influence of obesity on primary total hip arthroplasty outcomes: a meta-analysis of prospective cohort studies. Orthop Traumatol Surg Res OTSR. 2015;101(3):289–96.
Conroy JL, Whitehouse SL, Graves SE, Pratt NL, Ryan P, Crawford RW. Risk factors for revision for early dislocation in total hip arthroplasty. J Arthroplasty. 2008;23(6):867–72.
Kelley SS, Lachiewicz PF, Hickman JM, Paterno SM. Relationship of femoral head and acetabular size to the prevalence of dislocation. Clin Orthop Relat Res. 1998;355:163–70.
Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13(5):530–4.
Chai W, Xu C, Guo RW, Kong XP, Fu J, Tang PF, et al. Does robotic-assisted computer navigation improve acetabular cup positioning in total hip arthroplasty for Crowe III/IV hip dysplasia? A propensity score case-match analysis. Int Orthop. 2022;46:769–77.
Kong X, Yang M, Jerabek S, Zhang G, Chen J, Chai W. A retrospective study comparing a single surgeon’s experience on manual versus robot-assisted total hip arthroplasty after the learning curve of the latter procedure—a cohort study. Int J Surg. 2020;77:174–80.
Kong X, Yang M, Li X, Ni M, Zhang G, Chen J, et al. Impact of surgeon handedness in manual and robot-assisted total hip arthroplasty. J Orthop Surg Res. 2020;15(1):159.
Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75(2):228–32.
Restrepo C, Parvizi J, Kurtz SM, Sharkey PF, Hozack WJ, Rothman RH. The noisy ceramic hip: is component malpositioning the cause? J Arthroplasty. 2008;23(5):643–9.
Domb BG, El Bitar YF, Sadik AY, Stake CE, Botser IB. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472(1):329–36.
Liaw CK, Yang RS, Hou SM, Wu TY, Fuh CS. Measurement of the acetabular cup anteversion on simulated radiographs. J Arthroplasty. 2009;24(3):468–74.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–20.
Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16(6):715–20.
Parry MC, Povey J, Blom AW, Whitehouse MR. Comparison of acetabular bone resection, offset, leg length and post operative function between hip resurfacing arthroplasty and total hip arthroplasty. J Arthroplasty. 2015;30(10):1799–803.
Illgen RLN, Bukowski BR, Abiola R, Anderson P, Chughtai M, Khlopas A, et al. Robotic-assisted total hip arthroplasty: outcomes at minimum two-year follow-up. Surg Technol Int. 2017;30:365–72.
Lim SJ, Ko KR, Park CW, Moon YW, Park YS. Robot-assisted primary cementless total hip arthroplasty with a short femoral stem: a prospective randomized short-term outcome study. Comput Aided Surg. 2015;20(1):41–6.
Emara AK, Samuel LT, Acuna AJ, Kuo A, Khlopas A, Kamath AF. Robotic-arm assisted versus manual total hip arthroplasty: systematic review and meta-analysis of radiographic accuracy. Int J Med Robot Comput Assist Surg MRCAS. 2021;17(6):e2332.
Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469(2):319–29.
Correa-Valderrama A, Stangl-Herrera W, Echeverry-Vélez A, Cantor E, Ron-Translateur T, Palacio-Villegas JC. Relationship between body mass index and complications during the first 45 days after primary total hip and knee replacement: a single-center study from South America. Clin Orthop Surg. 2019;11(2):159–63.
Hung CY, Chang CH, Lin YC, Lee SH, Chen SY, Hsieh PH. Predictors for unfavorable early outcomes in elective total hip arthroplasty: does extreme body mass index matter? BioMed Res Int. 2019;2019:4370382.
Gwam CU, Mistry JB, Mohamed NS, Thomas M, Bigart KC, Mont MA, et al. Current epidemiology of revision total hip arthroplasty in the United States: national inpatient sample 2009 to 2013. J Arthroplasty. 2017;32(7):2088–92.
Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instruct Course Lect. 2005;54:131–41.
Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001;388:125–34.
Weber M, Merle C, Nawabi DH, Dendorfer S, Grifka J, Renkawitz T. Inaccurate offset restoration in total hip arthroplasty results in reduced range of motion. Sci Rep. 2020;10(1):13208.
Bonnin MP, Archbold PH, Basiglini L, Fessy MH, Beverland DE. Do we medialise the hip centre of rotation in total hip arthroplasty? Influence of acetabular offset and surgical technique. Hip Int J Clin Exp Res Hip Pathol Ther. 2012;22(4):371–8.
Kayani B, Giebaly D, Haddad FS. Leg length and total hip arthroplasty: old problem, new standards? Bone Joint J. 2021;103-b(11):1642–5.
Meermans G, Doorn JV, Kats JJ. Restoration of the centre of rotation in primary total hip arthroplasty: the influence of acetabular floor depth and reaming technique. Bone Joint J. 2016;98-b(12):1597–603.
Kayani B, Konan S, Thakrar RR, Huq SS, Haddad FS. Assuring the long-term total joint arthroplasty: a triad of variables. Bone Joint J. 2019;101-b(1_Supple_A):11–8.
Cozzi Lepri A, Villano M, Innocenti M, Porciatti T, Matassi F, Civinini R. Precision and accuracy of robot-assisted technology with simplified express femoral workflow in measuring leg length and offset in total hip arthroplasty. Int J Med Robot Comput Assist Surg MRCAS. 2020;16(5):1–6.
Lahy J, Stevens J, McKenzie D, de Steiger R. The reliability of measuring acetabular component position on radiographs using everyday diagnostic imaging software. J Orthop Surg (Hong Kong). 2017;25(2):2309499017718953.
Pichl J, Kremer M, Hoffmann R. Conventional cup navigation with 2D fluoroscopy in THA: accurate cup positioning respecting pelvic tilt. Zeitschrift fur Orthopadie und Unfallchirurgie. 2011;149(5):510–7.
Alzohiry MA, Abdelnasser MK, Moustafa M, Mahran M, Bakr H, Khalifa Y, et al. Accuracy of plain antero-posterior radiographic-based methods for measurement of acetabular cup version. Int Orthop. 2018;42(12):2777–85.
Acknowledgements
Not applicable.
Funding
This study was supported by National Clinical Research Center for Orthopedics, Sports Medicine and Rehabilitation Subject: 2021-NCRC-CXJJ-ZH-01.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the following: (1) the conception and design of the study, acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, and (3) final approval of the version to be submitted. SZ was primarily responsible for all computational analyses in the article and the drafting of the manuscript. XK and WC were primarily responsible for oversight of the research project, including all data acquisition and analysis, and manuscript preparation and approval. XK and WC contributed to this work equally, and both of them were co-corresponding author. MY, YL, MM, and ZC revised the manuscript and helped perform the analysis with constructive discussions. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The medical ethics committee of General Hospital of Chinese PLA approved the study “Clinical outcome study of robotic-assisted orthopedic surgery in total hip arthroplasty.” All procedures were conducted in compliance with the guidelines of the Declaration of Helsinki. The patients were informed consent prior to their participation in the study.
Consent for publication
We have obtained consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, S., Liu, Y., Yang, M. et al. Robotic-assisted versus manual total hip arthroplasty in obese patients: a retrospective case–control study. J Orthop Surg Res 17, 368 (2022). https://doi.org/10.1186/s13018-022-03263-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03263-6