Abstract
Background
Three-dimensional (3D) printing technology has developed rapidly in orthopaedic surgery and effectively achieves precise and personalized surgery. The purpose of this meta-analysis was to assess the efficacy of 3D printing technology in the management of displaced intra-articular calcaneal fractures (DICFs) by extended lateral approach (ELA).
Methods
We searched PubMed, Web of Science, Embase, Cochrane Library, CNKI, VIP, and VANFUN databases were searched up to October 2020. All clinical studies comparing traditional surgery and 3D printing-assisted surgery in the management of DICFs were obtained, evaluating the quality of the included studies and extracting data. For each study, we assessed odds ratios (ORs), standard mean difference (SMD), and 95% confidence interval (95% CI) to assess and synthesize the outcomes.
Results
Three RCTs and nine retrospective studies involving 732 patients were included met our inclusion criteria with 366 patients in the 3D group and 366 patients in the conventional group. The meta-analysis showed that there were significant differences of the operative time in the 3D group [SMD = − 1.86, 95% CI (− 2.23, − 1.40), P < 0.001], intraoperative blood loss [SMD = − 1.26, 95% CI (− 1.82, − 0.69), P < 0.001], the number of intraoperative X-ray exposures [SMD = − 0.66, 95% CI (− 1.20, − 0.12), P < 0.001], postoperative complications [OR = 0.49, 95% CI (0.31, 0.79), P < 0.001], excellent and good rate of calcaneal fracture outcome [OR = 4.09, 95% CI (2.03, 8.22), P < 0.001].
Conclusion
The current study indicates that 3D printing-assisted ELA surgery showed a better rate of excellent and good outcome, shorter operation time, less intraoperative blood loss, fewer intraoperative fluoroscopies, fewer complications. Besides, there is still a need for large-sample, high-quality, long-term randomized controlled trials to confirm the conclusion.
Similar content being viewed by others
Introduction
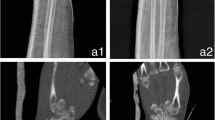
Calcaneus fractures make up about 2% of all fractures [1], most of which are caused by severe high-energy injuries such as falls from height or road traffic accidents [2, 3], and 70 to 75% are intra-articular fractures [4]. The management of calcaneal intra-articular fractures has been controversial [5], and various complex DICFs, after surgery, there is still a risk of deformity and complications such as traumatic arthritis, leg and foot stiffness, deformation, and pain [6, 7]. Traditional surgery usually performs preoperative planning based on X-ray and CT, which cannot involve the 3D structure of the fracture, and only have a limited understanding of the fracture patterns. The increased surgery's invasiveness inevitably leads to unnecessary tissue damage and increases intraoperative bleeding and operation time [8]. In consequence, the outcome of that management is still far from satisfaction.
With the development of digital medicine, more fracture relative information has been available in recent years, and 3D measurements based on CT processing are highly reliable. Preoperative 3D modelling allows for more effective diagnosis and simulates the surgical procedure, 3D printing technology, and digital image processing allow for assessing the post repositioning situation [9, 10]. 3D printing technology has become one of the leading advanced methods of preoperative planning. Several studies reported that 3D printing led to fewer misplacements and errors during the procedure [11, 12]. Some studies point to using 3D technology to reduce the number of postoperative complications and improve the safety of surgical patients [13, 14].
However, an study reported that 3D printing to assist in managing DICFs cannot improve postoperative function compared to routine treatment [15]. Meanwhile, the results in comparing the application of 3D printing-assisted ELA with conventional ELA for DICFs are not entirely consistent in terms of excellent rates of the outcome, operative time, intraoperative bleeding, the number of X-ray exposures, postoperative complications [16, 17]. Furthermore, previous meta-analyses indicated no significant results regarding the rate of excellent and good outcomes, and complications [18]. Considering the above controversies and uncertainties, we conducted a meta-analysis of the effectiveness and safety of applying 3D printing for DICFs to provide a basis for clinical decision-making.
Materials and methods
This systematic review was designed, undertaken, and reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [19] and the Cochrane Collaboration guidelines.
Search strategy
PubMed, Web of Science, Embase, Cochrane Library, CNKI, VIP, and VANFUN databases were searched up to October 2020. All clinical studies comparing conventional surgery and 3D printing-assisted surgery in the management of DICFs by ELA were obtained. The search terms for the Chinese and English databases were “calcaneal fractures” and “3D printing”. Two researchers independently screened the literature for inclusion and exclusion criteria according to the Cochrane Handbook 5.2 evaluation criteria, read the title and/or abstract information for initial screening, then read the full text to eliminate further literature that cannot meet the criteria and cross-checked the results. The final data was extracted from the literature that met the criteria. In case of disagreement between two researchers, a third researcher is involved in the discussion and negotiates the decision, and if necessary, the authors of the literature may be contacted to clarify further information about the study. Following the PICOS (Participants, Interventions, Comparisons, Outcomes, and Study design) principle, the key search terms included (P) patients with calcaneal fracture; (I) patients were treated by 3D printing-assisted ELA; (C/O) the primary outcome indicator was the rate of excellent and good outcome, and the secondary outcome indicators were operative time, intraoperative bleeding, number of intraoperative X-rays, and postoperative complications. Inclusion and exclusion criteria applied to articles identified in the literature are shown in Table 1.
Data extraction
The trial selection process complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [20]. For each included study, two types of information were extracted: basic information and primary study outcome. Basic information relevant to this meta-analysis included: author, year, number of cases, age, fracture subtype, study type, and follow-up time. The primary outcome indicator and the secondary outcome indicators: the rate of excellent and good outcome, the duration of operation time, intraoperative blood loss, number of fluoroscopies, complications rate.
Risk of bias assessment
Both reviewers independently assessed the risk of bias using the Cochrane Collaboration's Risk of bias tool [21]. Appraisal criteria included: sequence generation for randomization, concealment of allocation, blinding, incomplete outcome data, selective outcome reporting, and other potential sources of bias (for example, an extreme imbalance in baseline patient characteristics). Each of these factors was recorded as yes (‘low’ risk of bias), no (‘high-risk), or unclear with a summary provided in table format (see the Characteristics of included studies). Where data were ambiguous, we contacted authors for clarification, where possible. After this process, each paper was graded as low, unclear, or high risk of bias.
Statistical analysis
Statistical analysis of the data was performed Rev Man 5.4 software provided by the Cochrane Collaboration Network. The results of each study were tested for heterogeneity using I2 and P values. If (P ≥ 0.05, I2 ≤ 50%), there was homogeneity between the results of the studies, and meta-analysis was performed using a fixed-effects model. If the results of each study (P < 0.05, I2 > 50%), there was substantial heterogeneity between the studies, and meta-analysis was performed using a random-effects model. Standard mean differences (SMD) and 95% confidence intervals (CI) were used for measurement data, and ratio (OR) and 95% CI were used for dichotomous variable data. P < 0.05 was considered a statistically significant difference.
Results
Literature search
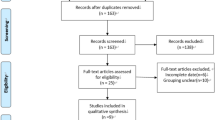
The database was searched to obtain 154 relevant papers. After importing them into EndNote X9 software, 122 were checked, 35 were obtained after reading the titles and abstracts, and 12 studies were finally included after reading the full text. The literature selection process is shown in Fig. 1. Seven hundred thirty-two patients were included, 366 patients in 3D printing technology-assisted ELA and 366 patients in conventional ELA.
Characteristics of the included studies and quality and bias assessment
An assessment of study quality and risk of bias was performed Rev Man 5.4 software offset risk table. Sensitivity analyses were performed in the excellent calcaneal fracture outcome rate. The analysis results showed that the overall results did not show significant changes and the results were relatively stable so that individual studies could be considered not to have a significant effect on the overall results. When the literature with the greatest weight was excluded, the combined effect size (OR = 4.76), 95% CI (1.94, 11.68), and the results did not show a significant change (Fig. 2). Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies (Fig. 3). Table 2 summarizes the basic information for each study.
The rate of excellent and good outcome
Four studies reported postoperative outcomes based on Maryland score results of the heterogeneity analysis showed homogeneity between the studies (P > 0.05, I2 = 0%), so a fixed-effects model was used to analyze the results. The results showed a statistically significant difference between the two groups: OR = 4.09, 95% CI (2.03, 8.22), Z = 3.95 (Fig. 4).
Operation duration
Eleven studies reported the duration of operation time, with significant heterogeneity between studies (P < 0.001, I2 = 96%), so a random-effects model was used for statistical analysis. The results showed a statistically significant difference between the two groups: SMD = − 1.86, 95% CI (− 2.23, − 1.40), Z = 7.93, P < 0.05 (Fig. 5).
Intraoperative blood loss
Nine studies reported intraoperative blood loss, and the results of the heterogeneity analysis showed significant heterogeneity between the nine studies (P < 0.001, I2 = 89%), so a random-effects model was chosen for statistical analysis and combined. The research showed a statistically significant difference between the two groups: SMD = − 1.26, 95% CI (− 1.82, − 0.69), Z = 4.38, P < 0.05 (Fig. 6).
Number of intraoperative X-ray exposures
Five studies reported the number of intraoperative X-ray exposures. The heterogeneity analysis results showed heterogeneity between the studies (P < 0.001, I2 = 76%), so a random-effects model was chosen for statistical analysis and combined. The research showed a statistically significant difference in the number of intraoperative X-ray exposures between the two groups: SMD = − 0.66, 95% CI (− 1.20, − 0.12), Z = 2.38, P < 0.05 (Fig. 7).
Postoperative complications
Nine studies reported postoperative complications and the results of the heterogeneity analysis showed homogeneity between the nine studies (χ2 = 2.82, P = 0.95, I2 = 0%), so a fixed-effects model was chosen for statistical analysis and combined. The results of the analysis showed a statistically significant difference in the incidence of postoperative complications between the two groups: OR = 0.49, 95% CI (0.31, 0.79), Z = 2.94, P = 0.003 < 0.05 (Fig. 8).
Discussion
DICF can cause displacement of the articular surface and is a mighty destructive fracture. The subtalar joint, in particular, may be severely disrupted [1]. DICFs remains one of the most challenging problems to manage [22, 23]. Therefore, understanding the morphological characteristics of calcaneal fractures may conduce to treatment. The 3D printing-assisted surgery was critical for surgeons to understand the fracture patterns fully, make a detailed and reliable preoperative plan, and perform individualized therapy for patients. Although there had been some retrospective articles on 3Dprinting-assisted DICFs surgery, there was still a lack of future high-quality articles for further analysis. The current study indicates that 3D printing-assisted ELA surgery outperforms conventional surgery, with shorter operation duration, fewer complications, less intraoperative blood loss, less intraoperative fluoroscopies. Furthermore, our research has shown that the application of 3D printing-assisted ELA can improve the excellent and good rate of calcaneal fracture outcomes.
The excellent and good rate of calcaneal fracture outcome was evaluated according to the Maryland score criteria. Zhang et al. reported that the application of 3D printing-assisted lateral incision cannot improve the excellent and good rate of outcome compared to the conventional group for DICFs, and the difference between the total incidence of the two groups was not statistically significant (P > 0.05). This meta-analysis revealed that there was a significant difference in an excellent and good rate of outcome [OR = 4.09, 95% CI (2.03, 8.22)], between the two groups. We found that the application of 3D printing to assist ELA surgical treatment could significantly improve the excellent and good rate of calcaneal fracture outcome.
Postoperative complications included infection, persistent deformity, incongruent joint surfaces with a stiff, painful, deformed foot, osteoarthritis of the subtalar joint are common outcomes [6]. Li et al.[16] reported that no statistically significant difference in postoperative complications and intraoperative X-ray fluoroscopy with 3D printing-assisted ELA compared to the conventional group for DICFs (P > 0.05). Zhang et al. also concluded that there was no difference in the efficacy of applying 3D printing to treat DICFs. The meta-analysis revealed that there was a significant difference in postoperative complications [OR = 0.49, 95% CI (0.31, 0.79)], especially wound infection. We believed that the application of 3D printing to assist ELA surgical treatment could significantly reduce the occurrence of postoperative complications. We were considering that being a small sample of studies and mostly non-randomized controlled trials significantly reduces the credit quality rating of the studies. Meta-analysis and systematic evaluation have not been used to compare the efficacy of the 3D printing-assisted ELA to conventional treatment of DICFs, and this is the first time we have used meta-analysis to evaluate the efficacy of the 3D printing-assisted ELA in the treatment of DICFs. The evidence for the results of the meta-analysis is largely conclusive, and further studies are unlikely to reverse the results. Besides, sensitivity analyses confirmed that the advantages of 3D printing-assisted ELA are still stable, which may contribute to the spread of 3D printing in the treatment of DICFs.
There have been many studies confirming the value of 3D printing for applications. 3D printing is emerging as a powerful tool for tissue engineering by enabling 3D cell culture within complex 3D biomimetic architectures [24]. The 3D-printed model offers the benefits of haptic feedback, direct manipulation, and enhanced understanding of cardiovascular anatomy and underlying pathology. 3D printing span from diagnostic assistance and optimization of management algorithms in complex cardiovascular diseases to planning simulating surgical and interventional procedures [25]. The use of 3D printing is proving to be more effective than traditional 2D imaging models in surgical procedures [26]. Chung et al. [27] showed that the application of 3D printing technology to assist in the internal fixation of steel plates can be more beneficial. Misselyn et al. [28] concluded that the 3D printing improves interobserver agreement in assessing calcaneal fractures. 3D printing has become one of the most revolutionary and powerful tools [15]. However, Xu et al. [29] and Chen et al. [30] concluded that 3D printing technology requires a high level of professional expertise and increases the cost of treatment for patients, limiting its widespread availability. The cost of this technique is another reason limiting its diffusion [31,32,33]. Indeed, the cost is often a concern when new and expensive technologies are introduced into medical practice. However, this may be resolved in the coming years as the cost of 3D printing decreases. Indeed, the cost is often a concern when new and expensive technologies are introduced into medical practice. A systematic evaluation noting the additional cost and time required to manufacture devices with current 3D technology is still widely used in hospitals. Still, guidelines need to be developed to improve the reporting of experience with 3D printing in orthopedic surgery is highly desirable [34]. However, this may be resolved in the coming years as the cost of 3D printing decreases.
Although this study was conducted by comprehensively screening and obtaining all relevant literature, the inclusion–exclusion criteria and the literature quality evaluation system were strictly adhered to ensure the quality of the included literature as much as possible. The results of this Meta-analysis have certain clinical guidance implications. However, this study also has certain limitations: (1) The relatively low quality of the included studies severely reduced the quality level of the evidence and compromised the credibility of the overall pooled effect estimates (2) The inclusion language was restricted to Chinese and English, and literature published in other languages was not included in the study. (3) Preoperative communication satisfaction, incision length, length of stay, fracture healing time, and AOFAS score outcome indicators were not included in the study. (4) Despite this, the sensitivity analysis results were generally consistent with the overall pooled effect, which supports the robustness and reliability of the benefits of 3D printing ELA treatment of DICFs. (5) It is hard to ignore the potential clinical and methodological heterogeneity across included studies due to our systematic review's broad inclusion criteria, although the statistical heterogeneity was low. Conservative estimation of the effect of 3D printing-assisted ELA on the efficacy of calcaneal fracture treatment using a random-effects model.
Conclusion
The current study indicates that 3D printing-assisted ELA surgery showed a better rate of excellent and good outcome, shorter operation time, less intraoperative blood loss, fewer intraoperative fluoroscopies, fewer complications. Besides, there is still a need for large-sample, high-quality, long-term randomized controlled trials to confirm the conclusion.
Availability of data and materials
All data generated or used during the study appear in the submitted article.
Abbreviations
- 3D:
-
Three-dimensional
- ELA:
-
Extended lateral approach
- DICFs:
-
Displaced intra-articular calcaneal fractures
References
Griffin D, Parsons N, Shaw E, et al. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ. 2014;349:g4483.
Humphrey JA, Woods A, Robinson AHN. The epidemiology and trends in the surgical management of calcaneal fractures in England between 2000 and 2017. Bone Jt J. 2019;101-b:140–6.
Gougoulias N, McBride D, Maffulli N. Outcomes of management of displaced intra-articular calcaneal fractures. Surg J R Coll Surg Edinb Ireland. 2021;19:e222–9.
Daftary A, Haims AH, Baumgaertner MR. Fractures of the calcaneus: a review with emphasis on CT. Radiogr Rev Publ Radiol Soc N Am Inc. 2005;25:1215–26.
Wei N, Zhou Y, Chang W, et al. Displaced intra-articular calcaneal fractures: classification and treatment. Orthopedics. 2017;40:e921–9.
Scammell BE. Calcaneal fractures. BMJ. 2014;349:g4779.
Tsubone T, Toba N, Tomoki U, et al. Prediction of fracture lines of the calcaneus using a three-dimensional finite element model. J Orthop Res Off Publ Orthop Res Soc. 2019;37:483–9.
Shon HC, Choi S, Yang JY. Three-dimensional printing-assisted surgical technique with limited operative exposure for both-column acetabular fractures. Ulusal travma ve acil cerrahi dergisi Turk J Trauma Emerg Surgery TJTES. 2018;24:369–75.
Qiang M, Chen Y, Zhang K, et al. Measurement of three-dimensional morphological characteristics of the calcaneus using CT image post-processing. J Foot Ankle Res. 2014;7:19.
Zhang J, Wang L, Hao SS, et al. Preliminary application of 3D printing technology in the surgical treatment of complex calcaneal fractures. J Clin Misdiagn Mistreatment. 2019;32:80–5.
Li J, Hsu Y, Luo E, et al. Computer-aided design and manufacturing and rapid prototyped nanoscale hydroxyapatite/polyamide (n-HA/PA) construction for condylar defect caused by mandibular angle ostectomy. Aesthet Plast Surg. 2011;35:636–40.
Zhou LB, Shang HT, He LS, et al. Accurate reconstruction of discontinuous mandible using a reverse engineering/computer-aided design/rapid prototyping technique: a preliminary clinical study. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2010;68:2115–21.
Jeong HS, Park KJ, Kil KM, et al. Minimally invasive plate osteosynthesis using 3D printing for shaft fractures of clavicles: technical note. Arch Orthop Trauma Surg. 2014;134:1551–5.
Yamazaki M, Akazawa T, Okawa A, et al. Usefulness of three-dimensional full-scale modeling of surgery for a giant cell tumor of the cervical spine. Spinal Cord. 2007;45:250–3.
Jamróz W, Szafraniec J, Kurek M, et al. 3D printing in pharmaceutical and medical applications—recent achievements and challenges. Pharm Res. 2018;35:176.
Li DH, Zhong CR, Lin ZH, et al. Three dimensional printing navigation template assisted plate internal fixation for sanders type III and lV calcaneal fractures. J Trauma Surg. 2020;22(4):250–4.
Shen MH, Shi KB, Zhang H, et al. Application of 3D printing technology in surgical treatment of Sanders III and IV calcaneal fractures. J Chin J Orthop Surg. 2018;26:1259–63.
Xiong L, Li X, Li H, et al. The efficacy of 3D printing-assisted surgery for traumatic fracture: a meta-analysis. Postgrad Med J. 2019;95:414–9.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:000142.
Gusic N, Fedel I, Darabos N, et al. Operative treatment of intraarticular calcaneal fractures: anatomical and functional outcome of three different operative techniques. Injury. 2015;46(Suppl 6):S130–3.
Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Jt Surg Am. 2000;82:225–50.
Zhu W, Ma X, Gou M, et al. 3D printing of functional biomaterials for tissue engineering. Curr Opin Biotechnol. 2016;40:103–12.
Giannopoulos AA, Mitsouras D, Yoo SJ, et al. Applications of 3D printing in cardiovascular diseases. Nat Rev Cardiol. 2016;13:701–18.
Pugliese L, Marconi S, Negrello E, et al. The clinical use of 3D printing in surgery. Updat Surg. 2018;70:381–8.
Chung KJ, Hong DY, Kim YT, et al. Preshaping plates for minimally invasive fixation of calcaneal fractures using a real-size 3D-printed model as a preoperative and intraoperative tool. Foot Ankle Int. 2014;35:1231–6.
Misselyn D, Nijs S, Fieuws S, et al. Improved interobserver reliability of the sanders classification in calcaneal fractures using segmented three-dimensional prints. J Foot Ankle Surg. 2018;57:440–4.
Xu W, Zhang X, Ke T, et al. 3D printing-assisted preoperative plan of pedicle screw placement for middle-upper thoracic trauma: a cohort study. BMC Musculoskelet Disord. 2017;18:348.
Chen C, Cai L, Zheng W, et al. The efficacy of using 3D printing models in the treatment of fractures: a randomised clinical trial. BMC Musculoskelet Disord. 2019;20:65.
Ciocca L, Fantini M, De Crescenzio F, et al. Computer-aided design and manufacturing construction of a surgical template for craniofacial implant positioning to support a definitive nasal prosthesis. Clin Oral Implant Res. 2011;22:850–6.
Kataoka T, Oka K, Miyake J, et al. 3-Dimensional prebent plate fixation in corrective osteotomy of malunited upper extremity fractures using a real-sized plastic bone model prepared by preoperative computer simulation. J Hand Surg. 2013;38:909–19.
Liacouras P, Garnes J, Roman N, et al. Designing and manufacturing an auricular prosthesis using computed tomography, 3-dimensional photographic imaging, and additive manufacturing: a clinical report. J Prosthet Dent. 2011;105:78–82.
Martelli N, Serrano C, van den Brink H, et al. Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery. 2016;159:1485–500.
Jiménez-Almonte JH, King JD, Luo TD, et al. Classifications in brief: Sanders classification of intraarticular fractures of the calcaneus. Clin Orthop Relat Res. 2019;477:467–71.
van Hoeve S, de Vos J, Verbruggen JP, et al. Gait analysis and functional outcome after calcaneal fracture. J Bone Jt Surg Am. 2015;97:1879–88.
Chen K, Pan ZY. Clinical application of 3D printing technique in surgical treatment of Sanders II & III type calcaneal fracture. J Trauma Surg. 2017;19:508–12.
Duan MM, Yin YB, Zhao CJ, et al. Effect analysis of 3D printing technology in doctor-patient communication and surgery of complex calcaneal fractures. J Chin J Bone Jt Injury. 2019;34:1109–11.
He ZP, Li W, Liu JW, et al. Application of 3D printing technology in complex calcaneal fractures. J China Pract Med. 2017;12:54–6.
Song JJ, Niu ZY, Wang TC. Application of computer aided design 3D printing technology in calcaneal fracture surgery. J Chin J Pract Med. 2020;47:94–7.
Zheng W, Tao Z, Lou Y, et al. Comparison of the Conventional surgery and the surgery assisted by 3d printing technology in the treatment of calcaneal fractures. J Investig Surg. 2018;31:557–67.
Wu QS, Sun P, Li L, et al. Clinical study on open reduction and internal fixation assisted by digital orthopedic technology in the treatment of calcaneal fractures. J Bone Setting Tradit Chin Med. 2015;27:20–3.
Xiong MJ, Tang LY, Zhu XY, et al. Discussion on the effectiveness of application of 3D printing technology in surgerical treatment of calcaneal fractures. J Chin Contemp Med. 2018;25:87–9.
Zhong H, Chen J, Li JW, et al. 3D printing assisted Sanders CT classification for the treatment of intra-articular calcaneal fractures. J Chin J Orthop Clin Basic Res. 2017;9:29–35.
Zheng P, Zhu XM, Bai BL, et al. Application analysis of computer-aided design 3D printing technology in the treatment of complex calcaneal fractures. In: The second annual conference of neurosurgery Professional Committee of Chinese Medical Education Association. Xiamen, Fujian Province, China; 2018:3.
Acknowledgements
Our deepest gratitude goes first and foremost to Xiyu Cai, my supervisor, for their constant encouragement and guidance. They have walked me through all the stages of the writing of this thesis. Without them consistent and illuminating instruction, this thesis could not have reached its present form.
Funding
This study was funded by the basic and applied research project of Zhuhai science and technology innovation Bureau (ZH22036201210060PWC).
Author information
Authors and Affiliations
Contributions
YS participated in the literature search, study selection, data extraction, and quality assessment. GS and WL writing, data analysis, data collections, finished the manuscript, GS and WL made the same contribution to this paper. XYC conceived of the design of the study and revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a systematic review, and therefore, IRB approval is not required. Each author agrees to participate.
Consent for publication
Each author agrees to publish.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, G., Liu, W., Shen, Y. et al. 3D printing-assisted extended lateral approach for displaced intra-articular calcaneal fractures: a systematic review and meta-analysis. J Orthop Surg Res 16, 682 (2021). https://doi.org/10.1186/s13018-021-02832-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02832-5