Abstract
Background
To evaluate the effect of intramedullary nail and locking plate in the treatment of proximal humerus fracture (PHF).
Methods
China National Knowledge Infrastructure (CNKI), Chinese Scientific Journals Database (VIP), Wan-fang database, Chinese Biomedicine Database (CBM), PubMed, EMBASE, Web of Science, and Cochrane Library were searched until July 2018. The eligible references all show that the control group uses locking plates to treat PHF, while the experimental group uses intramedullary nails to do that. Two reviewers independently retrieved and extracted the data. Reviewer Manager 5.3 was used for statistical analysis.
Results
Thirty-eight retrospective studies were referred in this study which involves 2699 patients. Meta-analysis results show that the intramedullary nails in the treatment of proximal humeral fractures are superior to locking plates in terms of intraoperative blood loss, operative time, fracture healing time, postoperative complications, and postoperative infection. But there is no significance in constant, neck angle, VAS, external rotation, antexion, intorsion pronation, abduction, NEER, osteonecrosis, additional surgery, impingement syndrome, delayed union, screw penetration, and screw back-out.
Conclusions
The intramedullary nail is superior to locking plate in reducing the total complication, intraoperative blood loss, operative time, postoperative fracture healing time and postoperative humeral head necrosis rate of PHF. Due to the limitations in this meta-analysis, more large-scale, multicenter, and rigorous designed RCTs should be conducted to confirm our findings.
Trial registration
PROSPERO CRD42019120508
Similar content being viewed by others
Background
PHF is the third common limb fracture, accounting for 4 to 5% of total body fractures [1]. The incidence is located after hip fracture and distal radius fracture [2]. Most proximal humeral fractures occur in the elderly population. With the gradual arrival of the elderly society, the incidence has increased nearly threefold in the past 30 years [3,4,5]. There is no uniform standard for the diagnosis and treatment of proximal humeral fractures. Different treatment methods have their own advantages and disadvantages [6]. Most of the simple humeral greater tuberosity fractures are not obvious and can be treated conservatively, but there is still a risk of secondary displacement during conservative treatment [7, 8]. For patients with significant shifts, surgical treatment is recommended. Plate internal fixation is a more common method, which provides a reliable internal fixation for patients with second, third, and fourth fractures, but it has great damage to tissues and blood vessels [9,10,11]. The intramedullary nail has less soft tissue and less damage to the periosteum and blood vessels and can achieve minimally invasive effects [12]. Intramedullary nails are mainly used for the treatment of fractures of the second and third parts of the proximal humerus. A series of reports of intramedullary nails have achieved satisfactory results in the treatment of proximal humeral fractures [13, 14].
Due to the good biomechanical properties of the locking plate and the intramedullary nail, its exact clinical efficacy has become the main treatment [15,16,17,18,19]. However, due to the difference in the principle of internal fixation biomechanics and the surgical method, its efficacy and application are still unclear in clinical practice. According to our understanding, in recent years, relevant scholars have conducted several meta-analyses, but the analysis of postoperative indicators is incomplete, especially the analysis of postoperative complications. In the past 5 years, the comparative analysis of intramedullary nails and locking plates in the treatment of proximal humeral fractures has gradually increased, and we have included more studies. Finally, we conducted a meta-analysis of 38 studies.
Methods
Database and searching strategies
A literature retrieve was carried out in eight databases from their inception to July 2018, like CNKI, VIP, Wan-fang database, CBM, PubMed, EMBASE, Web of Science, and Cochrane Library. Search terms including “Proximal humerus fracture,” “Intramedullary nail,” “Locking plate,” and “Internal fixation” were used individually or in combination. The publishing language was restricted to Chinese and English.
Inclusion criteria
The inclusion criteria are as follows: (i) internal fixation of displaced proximal humeral fractures; (ii) included both locking plates and intramedullary nails; (iii) greater than a minimum of 6 months of follow-up; (iv) a minimum of 21 patients for a given study; and (v) clinical outcomes during follow-ups included at least one of the following: intraoperative blood loss, operative time, fracture healing time, postoperative complications and postoperative infection, constant, neck angle, VAS, external rotation, antexion, intorsion pronation, abduction, NEER, osteonecrosis, additional surgery, impingement syndrome, delayed union, screw penetration, and screw back-out.
Exclusion criteria
The exclusion criteria are as follows: (i) non-humeral proximal fracture; (ii) treatment mode non-locking plate or intramedullary nail treatment; (iii) non-clinical researches, basic researches, and review articles were excluded, as case reports and theoretical discussions; (iv) improper statistical methods, data defect literature; (v) genetic research; (vi) grey literature; and (vii) letters to editor.
Data extraction
Two investigators (Xiaoqing Shi and Hao Liu) independently extracted and screened the data according to the inclusion criteria. We extracted the general details, such as patients’ characteristics, interventions, and outcomes, and a cross-check was done. Any disagreements were resolved through discussion or verification by a third investigator (Runlin Xing).
Quality assessment
The quality of the non-randomized controlled trials was assessed by the MINORS entry, and trials with MINORS scores > 12 were included in the study [20]. The methodological quality and risk of bias of RCTs used the Cochrane Handbook.
Statistical analysis
Revman 5.3 software was employed to pool the effect size. Mean difference (MD) or standardized mean difference (SMD) and 95% confidence intervals (CIs) were used for continuous variables. For the two-category data, we used OR (odds ratio)/RR (risk ratio) and 95% CIs as the efficacy analysis statistic. Heterogeneity was evaluated statistically using the χ2 test and inconsistency index statistic (I2). If substantial heterogeneity existed (I2 > 50% or P < 0.05), a random effect model was applied; otherwise, we adopted a fixed effect model [21]. Sensitivity analyses were explored to ensure the potential sources of heterogeneity and inspect the stability of the result. Evaluation of publication bias was made by plotting the funnel plot.
Results
Search results
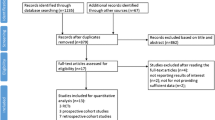
A total of 506 articles were initially obtained through the search strategy. After excluding 298 duplications, the remaining articles were screened based on their titles and abstracts, and 148 records were removed. By reading the full text, 14 literatures that did not meet the inclusion criteria were excluded. Finally, 38 trials [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59] were enrolled in the systematic review and meta-analysis. The flowchart of the process for literature retrieval was shown in Fig. 1.
Study characteristics
There were a total of 2699 patients (1238 in the locking plate group and 1461 in the intramedullary nail group) enrolled in our studies. More details of the included studies were presented in Table 1.
Intraoperative blood loss
Twenty-two studies [22, 24,25,26,27,28, 32, 37,38,39,40,41,42, 44, 47, 48, 50, 53,54,55,56,57] reported intraoperative blood loss, including 742 cases in the experimental group and 840 cases in the control group, I2 = 96%, P < 0.00001, and the heterogeneity was high. Therefore, the random effect model was used to calculate the combined effect. The results showed that intramedullary nail in the treatment of PHF is statistically significant, as its intraoperative blood loss is less than the locking plate [SMD = − 2.67, 95% CI (− 3.36, − 1.98), Fig. 2].
Operation time
A total of 878 cases in the experimental group and 1055 cases in the control group, in 26 studies [22, 24,25,26,27,28, 32, 37,38,39,40,41,42,43,44, 46,47,48, 50,51,52,53,54,55, 57], had reported that the operation time, including 878cases in the experimental group and 1055 cases in the control group, I2 = 92%, P < 0.00001, and the heterogeneity was higher. Therefore, the random effect model was used to calculate the combined effect. The results showed that intramedullary nailing for the treatment of PHF was statistically significant in reducing surgical time compared with locking plates [SMD = − 1.59, 95% CI (− 1.97, − 1.20), Fig. 3].
Fracture healing time
Twenty studies [22, 25,26,27,28, 32, 37,38,39,40,41, 44, 47, 48, 50, 52,53,54,55,56] reported fracture healing time, including 678 cases in the experimental group and 778 cases in the control group, I2 = 92%, P < 0.00001, and the heterogeneity was high. Therefore, the random effect model was used to calculate the combined effect. The results showed that intramedullary nailing for the treatment of PHF was statistically significant in reducing surgical time compared with locking plates [SMD = − 0.68, 95% CI (− 1.07, − 0.28), Fig. 4].
Overall complication
Complications were reported in 29 studies [22, 24,25,26,27,28, 30, 31, 33, 35,36,37, 39, 41,42,43, 45, 46, 48,49,50,51, 53,54,55,56,57,58,59], including 915 cases in the experimental group and 1151 cases in the control group, I2 = 0%, P = 0.52, and there was no heterogeneity. Thus, the combined effect model was used to calculate the combined effect. The results showed that intramedullary nailing for the treatment of PHF was better than the locking plate in the incidence of complications [OR = 0.75, 95% CI (0.57, 0.97), Fig. 5].
Other outcomes
We also analyzed other outcome indicators. Detailed information was shown in Table 2.
Quality assessment
For the methodological quality and risk of bias of RCTs, we used the Cochrane Handbook for Systematic Reviews of Interventions 5.2.0 for evaluation. The results showed that no studies used double blindness. On the other hand, for non-RCTs studies, we used MINORS to assess the methodological quality of the included studies. The results showed that the score interval was 13–18 points. Specifically, 13 points for five studies, 14 points for nine studies, 15 points for ten studies, 16 points for three studies, 17 points for seven studies, and 18 points for four studies. In general, this meta-analysis has qualitative limitations and most of the included studies had high risk of bias and low methodological quality.
Sensitivity analysis and publication bias
To further confirm the stability of the above outcomes, we replaced the fixed effect model with random effect model and excluded the most and least weighted trials. Comparing with previous results, the outcome exhibited no obvious difference which revealed that our study was robust and reliable. We mainly assessed the publication bias of overall complications (Fig. 6). The results manifested there was no obvious publication bias in our analysis. However, most of the included studies were published in mainland China, and potential publication bias still likely existed.
Discussion
In recent years, intramedullary nail and locking plate have been the main choices of internal fixation for PHF. From the biomechanics analysis, Edwards et al. [60] established an in vitro biomechanical comparison of an unstable humeral surgical neck fracture model and found that the locking plate has obvious advantages in bending resistance and torsion resistance. Relative to the eccentric fixation of the locking plate, Lekic [58] believed that the central fixation of the intramedullary nail can resist the greater varus force which is generated by the shoulder sleeve and the attached muscle. Biomechanics also shows that the axial load, torsional load, and bending load of the surgical neck fracture of the humerus are higher than that of the plate. Kitson [17] et al. also found that intramedullary nails have better stability in terms of eversion, flexion, and extension. Foruria [61] pointed out that there is no difference in dynamic torsional and static torsion resistance when treating proximal humeral fractures. Also both fixations provide stable biomechanical fixation, but the locking plate has better static torsional resistance. The previous researcher has conducted evidence-based medical analysis [62,63,64,65,66]; however, the conclusions reached are more limited, as the limited literature included and the types of research are mixed. In the past 3 years, many clinical experts have done more discussions on this. Based on the published literatures and incorporated new researches in recent years, we developed more stringent inclusion and exclusion criteria and reached a series of new conclusions.
The results of this meta-analysis show that (1) intramedullary nail in the treatment of PHF, intraoperative blood loss, operation time, fracture healing time, postoperative complications, and postoperative infection is better than locking plate treatment; (2) there were no significant differences in constant, neck angle, VAS, external rotation, antexion, intorsion pronation, abduction, NEER, osteonecrosis, additional surgery, impingement syndrome, delayed union, screw penetration, screw back-out between intramedullary nail, and locking plate in the treatment of proximal humeral fractures; (3) the screw back-out rate of the two-part fracture is better than the intramedullary nail in the locking plate; the shoulder anterior flexion angle intramedullary nail of the four-part fracture is better than the locking plate.
In terms of follow-up constant score, the intramedullary nail was not superior to the locking plate, and the results were not statistically different. Some studies concluded that may be related to surgical techniques [67,68,69,70,71]. In the meta-analysis done by Wang et al. [62], the same conclusions were obtained in terms of postoperative Constant score. von Ruden [72] also pointed out that both intramedullary nails and locking plates are suitable methods for the treatment of proximal humeral fractures. And these internal fixations have no significant differences in clinical function and imaging findings. The cause of this outcome may be related to postoperative pain, functional activity, muscle strength, and shoulder mobility, as these markers constitute the constant score. In this article, we know that shoulder mobility and VAS are not statistically significant in two different surgical procedures (Table 2). However, since this article does not comprehensively evaluate the outcomes, its conclusions may be changed.
Previous studies have suggested that there is no difference in the time of fracture healing between the two internal fixations. Jiang pointed out that this bias may be related to that the research is not enough in this area [64]. In our study, more stringent inclusion and exclusion criteria were developed, and more recent literatures were included, and different conclusions were drawn. We presume the reason for this result is that intramedullary nail treatment has less effect on blood flow around the fracture and surrounding soft tissue and can provide relatively stable fixation strength.
In terms of the incidence of screw penetration, Konrad et al. [33] found that the intramedullary nail was lower than the steel plate and that the steel plate was considered to be eccentrically fixed, which was prone to screw cutting. However, our study found that the use of locking plate and intramedullary nail in the treatment of proximal humeral fractures was not statistically significant. The cause of this result may be the crushing of the medial column, the complex degree of fracture, and the different screw positions.
There was a statistically significant difference in the overall risk of postoperative complications between the two groups, which is different from previous evidence-based studies [13,14,15,16,17]. In our meta-analysis, the total complication rates were 16.1% and 12.5% for locking plates and the intramedullary nails, respectively. Among them, intramedullary nail therapy is superior to locking plate therapy in reducing the postoperative infection rate. However, in other postoperative complications, we did not find the difference between the two procedures. Among these outcomes, intramedullary nail treatment is more dominant, but not statistically significant. The possible reasons for this result are (1) the size of the incision in the intramedullary nail and the area of the incision exposed to air are relatively small, which is less likely to be infected than the long incision of the locking plate; (2) the operation time of the locking plate is longer than that of the intramedullary nail. But with more high-quality RCTs, the conclusions may be different, and we should be cautious about this conclusion.
The limitations of this study are as follows: (1) this study cannot examine the use of surgical instruments by various subjects and evaluate the skill level and proficiency of the surgeon, which may cause clinical heterogeneity and affect the reliability of the meta-analytical strength and conclusion; (2) the type of study is retrospective analysis, and there is risk of selective bias, which may affect the authenticity and reliability of the research results; (3) the lack of clinical randomized controlled study, and the level of evidence is not high; (4) the doctor’s procedure is not completely unified, bringing a part of clinical heterogeneity; and (5) in all trials, the manufacturers of intramedullary nails and locking plates are different, and their quality is not the same.
Clinical outcomes have the potential to improve with time because the rate of the postoperative index can change with time. Despite the shortcomings in this study, we still try to avoid the risk of bias during the analysis and try subgroup analysis. Sensitivity analysis showed that the study has good stability and clinical reference value.
Additionally, there are fewer reliable randomized controlled trials included in this article. The level of evidence was reduced. It is difficult to control bias or confounding factors effectively. The evaluation efficiency may be reduced, and there may be publication bias, selection bias, implementation bias, and measurement bias. The inverted funnel plot shows that the included literature is basically within 95% CI. The article has certain reference value, but its results and applications should be treated with cautious attitude. If there are more clinical randomized controlled trials in this area, then a reliable conclusion will be drawn.
Conclusion
Intramedullary nailing for the treatment of proximal humeral fractures, intraoperative blood loss, operation time, fracture healing time, overall complication, and postoperative infection is better than locking plate treatment. In the treatment of proximal humeral fractures, the intramedullary nail and the locking plate are both mature. Before the proficiency of the technique, considering the treatment of proximal humeral fracture with intramedullary nail can bring effective results, such as reducing the surgical trauma, protecting the blood supply of the fracture end, promoting fracture healing, and reducing the occurrence of postoperative complications, especially the occurrence of postoperative infection. The author believes that intramedullary nail treatment is a better choice in the strict control of surgical indications. However, because the quality of the literature included in this study is various, there is a risk of bias. This conclusion needs to be demonstrated by more well-designed, high-quality, large-sample, multi-center, randomized, double-blind controlled clinical trials. In addition, the study and discussion of increasing related complications are conducive to obtaining more rigorous and objective clinical evidence.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CBM:
-
Chinese Biomedicine Database
- CIs:
-
Confidence intervals
- CNKI:
-
China National Knowledge Infrastructure
- I 2 :
-
Inconsistency index statistic
- MD:
-
Mean difference
- OR:
-
Odds ratio
- PHF:
-
Proximal humerus fracture
- RCT:
-
Randomized controlled trial
- SMD:
-
Standardized mean difference
- VAS:
-
Visual analog score
- VIP:
-
Chinese Scientific Journals Database
References
Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39(3):284–98.
Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, Tosteson AN. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93(2):121–31.
Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(4):365–71.
Launonen AP, Lepola V, Flinkkila T, Strandberg N, Ojanpera J, Rissanen P, Malmivaara A, Mattila VM, Elo P, Viljakka T, et al. Conservative treatment, plate fixation, or prosthesis for proximal humeral fracture. A prospective randomized study. BMC Musculoskelet Disord. 2012;13:167.
Kannus P, Palvanen M, Niemi S, Sievanen H, Parkkari J. Rate of proximal humeral fractures in older Finnish women between 1970 and 2007. Bone. 2009;44(4):656–9.
Sperling JW, Cuomo F, Hill JD, Hertel R, Chuinard C, Boileau P. The difficult proximal humerus fracture: tips and techniques to avoid complications and improve results. Instr Course Lect. 2007;56:45–57.
Hanson B, Neidenbach P, de Boer P, Stengel D. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg. 2009;18(4):612–21.
Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand. 2003;74(5):580–5.
Ring D. Current concepts in plate and screw fixation of osteoporotic proximal humerus fractures. Injury. 2007;38(Suppl 3):S59–68.
Konrad G, Bayer J, Hepp P, Voigt C, Oestern H, Kaab M, Luo C, Plecko M, Wendt K, Kostler W, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am. 2010;92(Suppl 1 Pt 1):85–95.
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42(4):408–13.
Dilisio MF, Nowinski RJ, Hatzidakis AM, Fehringer EV. Intramedullary nailing of the proximal humerus: evolution, technique, and results. J Shoulder Elbow Surg. 2016;25(5):e130–8.
Sforzo CR, Wright TW. Treatment of acute proximal humerus fractures with a polarus nail. J Surg Orthop Adv. 2009;18(1):28–34.
Giannoudis PV, Xypnitos FN, Dimitriou R, Manidakis N, Hackney R. Internal fixation of proximal humeral fractures using the Polarus intramedullary nail: our institutional experience and review of the literature. J Orthop Surg Res. 2012;7:39.
Koval KJ, Blair B, Takei R, Kummer FJ, Zuckerman JD. Surgical neck fractures of the proximal humerus: a laboratory evaluation of ten fixation techniques. J Trauma. 1996;40(5):778–83.
Fuchtmeier B, May R, Hente R, Maghsudi M, Volk M, Hammer J, Nerlich M, Prantl L. Proximal humerus fractures: a comparative biomechanical analysis of intra and extramedullary implants. Arch Orthop Trauma Surg. 2007;127(6):441–7.
Kitson J, Booth G, Day R. A biomechanical comparison of locking plate and locking nail implants used for fractures of the proximal humerus. J Shoulder Elbow Surg. 2007;16(3):362–6.
Sanders BS, Bullington AB, McGillivary GR, Hutton WC. Biomechanical evaluation of locked plating in proximal humeral fractures. J Shoulder Elbow Surg. 2007;16(2):229–34.
Koike Y, Komatsuda T, Sato K. Internal fixation of proximal humeral fractures with a Polarus humeral nail. J Orthop Traumatol. 2008;9(3):135–9.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J. Surg. 2003;73(9):712–6.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). 2003;327(7414):557–60.
Bi H, Wang Y, Li Y, Ceng P, Wang Y, Zhao Z, Yang Z. Comparison of proximal humerus locking plate and intramedullary nail in the treatment of two-part fracture of the proximal humerus in the elderly. Chin J Trad Med Traumatol Orthop. 2015;23(12):34–7.
Boudard G, Pomares G, Milin L, Lemonnier I, Coudane H, Mainard D, Delagoutte JP. Locking plate fixation versus antegrade nailing of 3- and 4-part proximal humerus fractures in patients without osteoporosis. Comparative retrospective study of 63 cases. Orthop Traumatol Surg Res. 2014;100(8):917–24.
Chen Z, Chen J. Comparison of open reduction and locking plate internal fixation with acumed fixation in the treatment of two-or three-part proximal humeral fractures. J Crit Care. 2018;6(01):29–31.
Cheng G, Tao Z, Zhang B, Jiao G. Clinical comparative study of locking plate and intramedullary nail in the treatment of neer III and IV fractures of proximal humerus. J Med Res. 2016;45(07):108–11.
Cui W, Lu Y, He X, Liu W, Zhou X, Yang L. Clinical comparative study of proximal humerus locking plate and intramedullary nail in the treatment of humeral surgical neck fracture. Chin J Bone and Joint Injury. 2014;29(01):41–3.
Ding Y, Wang W, Ma T, Wei M, Li Z. Comparison of the efficacy of locking plate and intramedullary nail in the treatment of two and three parts of proximal humerus fracture in elderly patients. J Clin Ortho. 2016;19(01):75–8.
Dong Y, Lu C, Li W, Chen H. Therapeutic effect of locking plate and intramedullary nail in the treatment of senile humeral surgical neck fracture. Chin J Trad Med Traumatol Orthop. 2017;25(06):48–50.
Gadea F, Favard L, Boileau P, Cuny C, d'Ollone T, Saragaglia D, Sirveaux F. Fixation of 4-part fractures of the proximal humerus: can we identify radiological criteria that support locking plates or IM nailing? Comparative, retrospective study of 107 cases. Orthop Traumatol Surg Res. 2016;102(8):963–70.
Gracitelli ME, Malavolta EA, Assuncao JH, Kojima KE, dos Reis PR, Silva JS, Ferreira Neto AA, Hernandez AJ. Locking intramedullary nails compared with locking plates for two- and three-part proximal humeral surgical neck fractures: a randomized controlled trial. J Shoulder Elbow Surg. 2016;25(5):695–703.
Gradl G, Dietze A, Kaab M, Hopfenmuller W, Mittlmeier T. Is locking nailing of humeral head fractures superior to locking plate fixation? Clin Orthop Relat Res. 2009;467(11):2986–93.
Ke Z. Clinical effect of locking plate of proximal humerus and intramedullary nail in the treatment of neer II type humeral surgical neck fracture. Clin Med Eng. 2017;24(05):685–6.
Konrad G, Audige L, Lambert S, Hertel R, Sudkamp NP. Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures. Clin Orthop Relat Res. 2012;470(2):602–9.
Li S. Comparative study of locking plate fixation and intramedullary nail fixation for proximal humeral fractures. World Latest Medicine Information. 2018;18(15):43–4.
Li Y, Zhao H, Liu Q, Lu Y, Zhou J. Clinical comparative study of interlocking intramedullary nail and locking plate in the treatment of proximal humerus fracture in elderly patients. Beijing Med J. 2015;37(11):1044–7.
Matziolis D, Kaeaeb M, Zandi SS, Perka C, Greiner S. Surgical treatment of two-part fractures of the proximal humerus: comparison of fixed-angle plate osteosynthesis and Zifko nails. Injury. 2010;41(10):1041–6.
Pan Y, Tan Y, Xu J, Liu G, Chen Q. Treatment of 33 cases of complex fracture of proximal humerus in elderly patients with proximal humerus locking system. Guizhou Med J. 2016;40(08):869–71.
Pu Y. Comparison of clinical effects of proximal humeral locking plate and intramedullary nail in the treatment of humeral surgical neck fractures. Hina Practical Medical | Chin Prac Med. 2015;10(14):91–2.
Qi L. Clinical observation of interlocking intramedullary nail and locking plate in the treatment of two and three parts fracture of proximal humerus. J Changchun University of Chinese Med. 2017.
Shao P, Chen Z, Yu Z. Treatment of neer II type humeral surgical neck fracture with locking plate of proximal humerus and intramedullary nail. China Practical Medical | Chin Prac Med. 2017;12(06):27–9.
Shen S. Efficacy of locking plate and interlocking intramedullary nail in the treatment of two-part surgical neck fracture of proximal humerus in elderly patients Dalian Medical University. J Dalian Medical University. 2012.
Shi L, Li X, Zhao J, Sun Y. Treatment of proximal humeral fractures with philos plate and intramedullary nail. J Trauma Surg. 2018;20(03):228–30.
Sui J, Wang Q, Zeng Y. Efficacy and safety of interlocking intramedullary nail in the treatment of proximal humeral fractures E. J Transl Med. 2016;3(12):20–1.
Tian F, Li C, Shao J. Comparison of proximal humeral locking plate and intramedullary nail in the treatment of humeral surgical neck fractures. Chinese J Modern Drug Appli| Chin J Mod Drug Appl. 2016;10(14):22–3.
Trepat AD, Popescu D, Fernández-Valencia JA, Cuñé J, Rios M, Prat S. Comparative study between locking plates versus proximal humeral nail for the treatment of 2-part proximal humeral fractures. Eur J Orthop Surg Traumatol. 2012;22(5):373–9.
Urda A, Gonzalez A, Colino A, Lopiz Y, Garcia-Fernandez C, Marco F. Management of displaced surgical neck fractures of the humerus: health related quality of life, functional and radiographic results. Injury. 2012;43(Suppl 2):S12–9.
Wang H, Wang Q, Ding R, Wang B, Huang J, Xianhua XC. Treatment of proximal humeral fractures with locking plate and intramedullary nail. Orthop J China. 2017;25(20):1899–901.
Wang L. A comparative study of locking plate and intramedullary nail in the treatment of two parts of proximal humeral fractures Jilin University. Journal of Jilin University (Medicine Edition) | J Jilin Univ (Med Ed). 2017.
Wang Z, Sheng W. Effect of interlocking intramedullary nail fixation in the treatment of old humeral fracture complicated with osteoporosis. J Aerospace Med. 2018;29(05):537–9.
Wu X. Clinical comparative analysis of proximal humerus locking plate and intramedullary nail in the treatment of humeral surgical neck fracture. World Latest Medicine Information. 2018;18(20):96 + 99.
Xu X, Zhang D, Fu Z, Wang T, Chen J, Yang M, Lu H. Treatment of proximal humeral fractures with locking plate and interlocking intramedullary nail. Chinese J Shoulder and Elbow (Electronic Edition). 2014;2(04):230–4.
Xue F. Comparison of efficacy and safety of intramedullary nail and anatomically locked plate internal fixation for proximal humeral fractures. Chinese J Convalescent Medicine. 2018;27(05):493–4.
Yu H. Comparative analysis of clinical effects of interlocking intramedullary nail and locking plate in the treatment of proximal humerus fracture in elderly patients. China Modern Doctor. 2016;54(11):42–5.
Yu Z, Bai L, Ye J, Chen K, Liu D, Lin L. Treatment of humeral surgical neck fracture with locking plate and interlocking intramedullary nail. Chinese J Bone Joint Injur. 2016;31(03):260–2.
Zhou Q, Cao L, Weng W, Chen X, Zhang J, Wang L, Wang Y, Su J. Clinical comparative study of interlocking intramedullary nail and locking plate in the treatment of proximal humeral fractures. Chinese J Shoulder and Elbow (Electronic Edition). 2017;5(02):84–9.
Zhou X, Wei M, Wang W, Zhang C, Dong Y. Comparison of proximal humeral locking plate and intramedullary nail fixation in the treatment of neer 3 proximal humeral fractures. Chinese J Bone and Joint Injur. 2018;33(01):28–31.
Zhu Y, Lu Y, Shen J, Zhang J, Jiang C. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am. 2011;93(2):159–68.
Lekic N, Montero NM, Takemoto RC, Davidovitch RI, Egol KA. Treatment of two-part proximal humerus fractures: intramedullary nail compared to locked plating. HSS J. 2012;8(2):86–91.
Tamimi I, Montesa G, Collado F, Gonzalez D, Carnero P, Rojas F, Nagib M, Perez V, Alvarez M, Tamimi F. Displaced proximal humeral fractures: when is surgery necessary? Injury. 2015;46(10):1921–9.
Edwards SL, Wilson NA, Zhang LQ, Flores S, Merk BR. Two-part surgical neck fractures of the proximal part of the humerus. A biomechanical evaluation of two fixation techniques. J Bone Joint Surg Am. 2006;88(10):2258–64.
Foruria AM, Carrascal MT, Revilla C, Munuera L, Sanchez-Sotelo J. Proximal humerus fracture rotational stability after fixation using a locking plate or a fixed-angle locked nail: the role of implant stiffness. Clin biomechanics (Bristol, Avon). 2010;25(4):307–11.
Wang G, Mao Z, Zhang L, Zhang L, Zhao Y, Yin P, Gao L, Tang P, Kang H. Meta-analysis of locking plate versus intramedullary nail for treatment of proximal humeral fractures. J Orthop Surg Res. 2015;10:122.
Zhang J, Yuan C, Cao L, Chen X, Weng W, Su J. Meta analysis of treatment of proximal humeral fractures with locking plate and intramedullary nail. Chinese J Shoulder and Elbow (Electronic Edition). 2016;4(04):207–13.
Jiang C, Chen G, Jiang X, Li W, Zhang W, Ren S. Treatment of proximal humeral fractures with intramedullary nail and locking plate: meta analysis. Chinese J Shoulder and Elbow (Electronic Edition). 2015;3(04):211–8.
Lei W, Wang F, Ma Y, Jie Z, Hu F, Ma J, Liu M, Ma Z. Meta analysis of intramedullary nail and locking plate in the treatment of proximal humeral fractures Journal of Clinical Rehabilitative Tissue Engineering Research |. J Clin Rehabil Tis Eng Res. 2017;21(03):478–84.
Luo S. Meta analysis of the efficacy of intramedullary nail and locking plate in the treatment of proximal humeral fractures. Shanxi Medical University. J Shanxi Medical University. 2017.
Huang Y, Xu Y, Yan G, Kang Y, Wei L, Wang Y. Comparison of therapeutic effects between intramedullary nail and locking plate in the treatment of 2-part fracture of proximal humerus. Chinese J Bone and Joint Injury. 2014;29(07):725–6.
Jianxi C, Chaohe X, Jiarong Z. Treatment of proximal humerus fracture with locking plate under proximal humerus compression versus traditional plate. China and Foreign Med Treat. 2016;35(21):70–2.
Zhang K, Feng G. Clinical observation on the treatment of proximal tibial fractures with locking compression plate and minimally invasive internal fixation. China Practical Medical | Chin Prac Med. 2016;11(22):73–4.
Li Y, Dong R. Treatment of proximal humerus fracture: status quo and research progress. Medical Recapitulate. 2016;22(14):2788–91.
Tian W, Hou J, Wang X, Gao C. Treatment of proximal humerus fracture with locking plate. China Health Standard Management | Chin Heal standard management. 2015;6(21):22–3.
von Ruden C, Trapp O, Hierholzer C, Prohaska S, Wurm S, Buhren V. Intramedullary nailing vs. locking plate osteosynthesis in proximal humeral fractures: long-term outcome. Der Unfallchirurg. 2015;118(8):686–92.
Acknowledgements
We gratefully acknowledge the invaluable contribution of Yingying Yang, Junyao Xu, and Chenghua Zhang (Nanjing University of Chinese Medicine) in the study design and data analysis.
Funding
This study was supported by the project Leading Talents of Traditional Chinese Medicine in Jiangsu Province: (SLJ0207); National Natural Science Foundation of China: (81774334); Jiangsu Provincial Science and Technology Department Social Development Fund: (BE2017774);
Author information
Authors and Affiliations
Contributions
XS participated in conception and design of this study. XS, HL, RX, and LD performed the acquisition of data. XS and WM performed the statistical analyses. LZ was involved in the interpretation of data. XS drafted the manuscript. PW revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Shi, X., Liu, H., Xing, R. et al. Effect of intramedullary nail and locking plate in the treatment of proximal humerus fracture: an update systematic review and meta-analysis. J Orthop Surg Res 14, 285 (2019). https://doi.org/10.1186/s13018-019-1345-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-019-1345-0