Abstract
Background
Proximal humeral fractures occur frequently. Displaced or unstable fractures require open reduction and internal fixation. Our objective was to investigate the clinical and radiographic results of the internal fixation using Polarus humeral nails for fractures of the proximal humerus.
Materials and methods
From January 2001 to April 2006, 54 shoulders of 54 patients (44 females, 10 males) underwent the intramedullary fixation using Polarus humeral nail. Mean age of the patients was 66-year-old (39–89) at the time of the surgery. Fracture-type by Neer classification was 2-part (29 shoulders), 3-part (22 shoulders) and 4-part (3 shoulders). The clinical and radiological outcomes were evaluated.
Results
All the shoulders after osteosynthesis obtained bone-union. There was no osteonecrosis of the humeral head. Functional outcome measured by JOA score averaged 81 points. Totally 43 patients (79%) had satisfactory to excellent results. Varus deformity was seen in 4 shoulders (8%) and the deformity of the greater tuberosity in 4 (8%).
Conclusion
The Polarus intramedullary humeral nail is effective for the treatment of proximal humeral fractures.
Similar content being viewed by others
Introduction
Proximal humeral fractures occur frequently. Most proximal humeral fractures are minimally displaced or non-displaced and are treated conservatively with good results. However, unstable or displaced fractures may lead to non-union, malunion or limited function [1]. Therefore, these displaced or unstable fractures require operative reduction and stabilization for favorable outcome. Various devices have been proposed for fixation, including plates and screws, staples, wire, multiple pins, intramedullary nails, and combination of these items. Intramedullary fixation has been thought as less invasive because it, compared with plate fixation, requires less extensive soft tissue dissection [2, 3].
The Polarus intramedullary nail (Acumed LLC, Hillsboro, OR, USA) is a stabilization device specialized for proximal humeral fixation. It provides screw stabilization of the humeral head and the tuberosities. Published reports about using Polarus intramedullary nails for proximal humeral fractures are satisfactory [2–8], but unsatisfied results with high complication rate of up to 32% has also been reported [9].
The purpose of this report was to evaluate the clinical and radiographic results of the Polarus nail retrospectively. Our hypothesis was that Polarus intramedullary nail could be effectively used to treat displaced proximal humeral fractures.
Materials and methods
This study received approval from the ethical board of Tohoku Rosai Hospital. This study was conducted in accordance with the Declaration of Helsinki. All the patients gave informed consent to be enrolled. From January 2001 to April 2006, 54 patients with displaced proximal humeral fractures (44 females and 10 males, mean 66 years old (range 39–89), 24 right and 30 left side) were treated by open reduction and internal fixation (Table 1). The mechanisms of injury included 39 pedestrian stumbles, 5 automobile clashes, 4 severe falls, 3 bicycle accidents and 3 pedestrian-versus-automobile impacts. A fracture was considered to be displaced if the fracture fragment had a displacement more than 1 cm or an angulation more than 45° in at least one view of the trauma-series radiographs [10]. On radiographs and computed tomography, the fractures were classified using the Neer system [10]; 29 were 2-part surgical neck fractures, 22 were 3-part fractures and 3 were 4-part fractures. The time between injury and surgery averaged 9 days (range, 2–28 days). The proximal humeral fracture with poor bone stock, non-union, and fracture-dislocation of the glenohumeral joint were contraindicated for this study.
Each fracture was fixed with a Polarus nail, which is an intramedullary locked, cannulated nail made of Titanium alloy and having specific features (Fig. 1). Its tapered profile reduces distal stress concentration. It has four screw-holes for proximal locking. These are directed in anterio-posterior, lateral, and oblique directions to maximize fracture fragment fixation. The design of the screw hole-pattern prevents damage to anatomical structures, such as the axillary nerve, bicipital groove, and the biceps tendon. A radiolucent targeting device facilitates the accurate insertion of proximal and distal locking screws.
Under general anesthesia, the patient was placed in beach-chair position on a radiolucent operating table. A longitudinal skin incision was made along the greater tuberosity of the humerus. The deltoid muscle was bluntly split to expose the rotator cuff. In cases of 2-part (surgical neck) fracture, a Kirschner pin was inserted through the rotator cuff, and its position was confirmed by C-arm. A 10 mm longitudinal incision was made on the supraspinatus tendon right medial to the greater tuberosity and the entry portal of the nail was created with a drill and enlarged with a hand reamer. While maintaining fracture reduction by manual manipulation, a 2.0-mm guide wire was passed across the fracture and then the nail was inserted correctly. Finally, the nail was locked proximally and distally. In cases of 3- or 4-part fracture, the rotated or displaced articular fragment was reduced first and lined up with the shaft fragment. The entry portal of the nail was created on the articular fragment carefully, not to crack the articular fragment. Next, the displaced greater or lesser tuberosity fragment was identified and reduced. One suture inserted on the supraspinatus tendon pulled out the greater tuberosity fragment. The lesser tuberosity fragment was also manipulated by a suture inserted on the infraspinatus tendon. A guide wire was passed across the head-shaft fracture and then the nail was inserted. The fragment of greater or lesser tuberosity was reduced and then fixed with the locking screws or nonabsorbable sutures. Finally, the supraspinatus tendon and deltoid muscle were meticulously closed.
Postoperatively, the patient’s arm was supported in a neck sling. Active exercise of the elbow and wrist joint was encouraged immediately. Pendulum motion of the shoulder joint was started in 2 days and followed by passive elevation and rotation of the shoulder joints in the following week. Active motion was started at about 4 weeks. The patients are seen at 2, 4 weeks and at 3-month intervals.
Evaluation of the Polarus nail focused on the clinical and radiological outcomes. During the postoperative course, such complications as neurologic injury, avascular necrosis, infection and implant failure were recorded. Also, functional outcomes at 12 months was graded according to the Japanese Orthopaedic Association Shoulder score (JOA score), which has a maximum 95 points: 30 for pain, 20 for function, 30 for range of motion (ROM), and 15 for stability [11]. The results were excellent for a score of 85–95 points; satisfactory, 75–84; unsatisfactory, 65–74; and poor, <65.
Radiological outcomes included the bone-union and the degree of residual deformity at 12 months. The bone-union was defined as the continuity of cortex visible on at least two views of radiographs. The residual deformities of the proximal humerus were assessed by the neck-shaft angle and the deformity of the greater tuberosity [3, 12]. To measure the neck/shaft angle, a line (B) is drawn from the inferior articular surface to the superior articular margin/ sulcus junction (Fig. 2). A second line (C) is drawn perpendicular to line B. A third line (A) is drawn collinear to the long axis of the humeral shaft. The neck shaft angle is defined as the angle formed by the intersection of lines A and C. The residual varus-deformity was defined as less than 120° of neck/shaft angle [3]. Deformity of the greater tuberosity was defined by a >5-mm residual displacement or alteration of the countour of the greater tuberosity [12–14].
Results
The average operation time was 84 min [95% confidence interval (CI), 54–114 min] and the average blood loss was 110 ml (95% CI, 30–190 ml). The average follow-up period was 18 months (range, 13–35 months). Of the 54 shoulders, no cases of neurologic injury or avascular necrosis of the humeral head were noted. One superficial infection (2%) was noted but it responded to local wound care and antibiotics. Four shoulders (7%) had one or more proximal interlocking screws that loosened. Three screws in 2 shoulders (4%) were removed because it might potentially create the local irritation. One nail (2%) was removed because of proximal protrusion causing subacromial impingement. Postoperative outcomes as measured by JOA score averaged 81 points (95% CI 69–93): pain 26 points (22–30), function 18 points (16–20), ROM 22 points (15–29) and stability 15 points (Table 2). Totally 43 patients (79%) had satisfactory to excellent results while 11 patients (21%) had unsatisfactory results. Among the patients with unsatisfactory results (average 69 points, 95% CI 66–72), JOA score was mainly deducted in term of pain, function, and shoulder ROM: pain 21 points (20–22), function 16 points (14–17), ROM 17 points (14–20), stability 15 points.
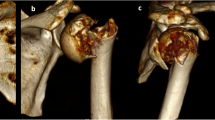
All fractures healed by 6 months (Fig. 3). The average neck/shaft alignment at the time of bone union was 135° (95% CI 120–150). Residual deformities were observed in 8 (16%) shoulders: varus deformity was seen in 4 shoulders (8%) and the deformity of the greater tuberosity in 4 (8%) (Table 3).
Discussion
Proximal humeral fractures occur frequently. Displaced or unstable fractures require open reduction and internal fixation. Various treatment options are available but no single technique has been demonstrated to be superior or without complications [15–17]. The Polarus intramedullary nail (Acumed LLC, Hillsboro, OR, USA) is an intramedullary device for proximal humeral fixation. This study evaluated the clinical and radiographic results of the Polarus nail retrospectively.
The average operation time and the blood loss was comparable to other reports using the similar device [9]. Absence of avascular necrosis of the humeral head was notable as it is one of the major complications after displaced fractures of the proximal humerus [1, 17, 18]. Besides the severity of the fracture, extensive soft tissue dissection has been cautioned as a major contributing factor [1]. Sturzenegger et al. [18] reported a 34% incidence of avascular necrosis in a series of 17 patients treated with a T plate. The extensive exposure of the fragment for plate fixation was thought to compromise blood supply to the fracture-fragments in his series [1]. We believe that intramedullary fixation jeopardizes less blood supply to the fracture-fragments because it requires less extensive soft tissue dissection.
The frequency of the loosening of the proximal cancellous screws (7%) was comparable to other reports, ranging from 4 to 20% [3, 5, 7, 9]. As Polarus nail didn’t have locking mechanism, the nail might have failed to hold the proximal cancellous screw. To prevent the loosening of the proximal screws, Inoue et al recommended that the second and third proximal cancellous screws should be ensured by penetrating themselves into the far cortex [5]. These surgical method would reduce the screw loosening.
In this study, satisfactory functional recovery was obtained in 79%, a rate comparable with that reported in the literature, ranging from 75 to 80% [7, 9, 12]. Among the patients with unsatisfactory results, shoulder function was impaired by pain and loss of ROM. Degenerative shoulder problems before trauma have been reported to exert negative influence on functional prognosis [17]. Wilmanns and Bonnaire [19] indicated the possible influence of a coexistent rotator cuff tear on functional recovery after proximal humeral fractures. The presence of painful hardware has also been reported as major risk factors causing stiff shoulder [1]. In case where the stiff shoulder persists, performing an open release of adhesions with removal of painful hardware is recommended [1].
Although the rate of residual deformity (16%) was less desired, satisfactory bone union was obtained in all cases (100%). The present study supported the claim that as long as bone union is obtained, some residual deformities still lead to less-painful and functional activities [12]. As many reports suggest, however, varus deformity of the humeral head might interfere with shoulder elevation [8] and the displaced greater tuberosity might cause subacromial impingement [1]. Therefore the displacement should be corrected during the surgery, if possible.
The present study had limitations. Most of the study group comprised of selective patients with relatively preserved bone stock. Therefore the method used in the present study may not be applicable to patients with non-union, fracture-dislocation or severe osteoporosis. Also, longer follow-up of the patients may be necessary because osteoporosis, osteonecrosis or secondary osteoarthritis might develop or worsen at a later time.
References
Bigliani LU, Flatow EL, Pallock RG (1998). Fracture of the proximal humerus. In: Rockwood CA Jr, Matsen FA III (eds) The Shoulders, 2nd edn, vol 1, W.B. Sounders company, pp 337–389
Adedapo AO, Ikpeme JO (2001) The results of internal fixation of three- and four-part proximal humeral fractures with the Polarus nail. Injury 32:115–121
Agel J, Jones CB, Sanzone AG, Camuso M, Henley MB (2004) Treatment of proximal humeral fractures with Polarus nail fixation. J Shoulder Elbow Surg 13:191–195
Inawashiro T, Inoue H, Watanabe K, Taira R, Sato K, Komatsuda T, Ito K, Matsuya S (2003) Fixation of proximal humeral fractures with the Polarus nail. Kossetsu Fract 25:633–636 (Japanese)
Inoue H, Sato K, Ito K, Inawashiro T (2003) Internal fixation of proximal humeral fractures with a Polarus humeral nail. Bessatsu Seikeigeka 44:23–27 (Japanese)
Momose T (2005) Internal fixation of proximal humeral fractures with a Polarus humeral nail. Shoulder Joint 29:539–541 (Japanese)
Rajasekhar C, Ray PS, Bhamra MS (2001) Fixation of proximal humeral fractures with the Polarus nail. J Shoulder Elbow Surg 10:7–10
Sasaki D, Abe Y, Takahashi S, Watanabe S, Saito T, Sugano H, Shibata T (2004) Results of the treatment for proximal humeral fractures. Kossetsu (Fracture) 26:153–158 (Japanese)
Hirose J, Nomura K, Hirano M (2005) Fixation and postoperative complicationss of proximal humeral fractures with a Polarus humeral nail. Shoulder Joint 29:323–327 (Japanese)
Neer CSII (1970) Displaced proximal humeral fractures. Part I. Classification and evaluation. J Bone Joint Surg 52:1077–1089
The journal of the shoulder joint editorial committee (2005) Manual for evaluation of the shoulder (JOA score). The shoulder joint 29:747–748 Japanese
Lin J (2006) Effectiveness of locked nailing for displaced three-part proximal humeral fractures. J Trauma 61:363–374
Robinson CM, Christie J (1993) The two-part proximal humeral fracture: a review of operative treatment using two techniques. Injury 24:123–125
Robinson CM, Page RS (2003) Severely impacted valgus proximal humeral fractures. Results of operative treatment. J Bone Joint Surg 85:1647–1655
Bernard J, Charalambides C, Aderinto J, Mok D (2000) Early failure of intramedullary nailing for proximal humeral fractures. Injury 31:789–792
Smith AM, Mardones RM, Sperling JW, Cofield RH (2007) Early complications of operatively treated proximal humeral fractures. J Shoulder Elbow Surg 16:14–24
Sperling JW, Cuomo F, Hill JD, Hertel R, Chuinard C, Boileau P (2007) The difficult proximal humerus fracture: tips and techniques to avoid complications and improve results. Instr Course Lect 56:45–57
Sturzenegger M, Fornaro E, Jakob RP (1982) Results of surgical treatment of multifragmented fractures of the humeral head. Arch Orthop Trauma Surg 100:249–259
Wilmanns C, Bonnaire F (2002) Rotator cuff alterations resulting from humeral head fractures. Injury 33:781–789
Conflict of interest statement
The authors have no financial relationship with any organization that sponsored the research. The authors have full control of all primary data. The authors agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Koike, Y., Komatsuda, T. & Sato, K. Internal fixation of proximal humeral fractures with a Polarus humeral nail. J Orthopaed Traumatol 9, 135–139 (2008). https://doi.org/10.1007/s10195-008-0019-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-008-0019-1