Abstract
Background
A structured approach involves systematic management of trauma patients. We aim to conduct an overview of reviews about the clinical efficacy and safety of structured approach (i.e., primary and secondary survey) by guideline checklist compared to non-structured approach (i.e. clinical examination); moreover, routine screening whole-body computer tomography (WBCT) was compared to non-routine WBCT in patients with suspected major trauma.
Methods
We systematically searched MEDLINE (PubMed), EMBASE and Cochrane Database of Systematic Reviews up to 3 May 2022. Systematic reviews (SRs) that investigated the use of a structured approach compared to a non-structured approach were eligible. Two authors independently extracted data, managed the overlapping of primary studies belonging to the included SRs and calculated the corrected covered area (CCA). The certainty of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology.
Results
We included nine SRs investigating two comparisons in stable trauma patients: structured approach vs non-structured approach (n = 1) and routine WBCT vs non-routine WBCT (n = 8). The overlap of included primary studies was generally high across outcomes (CCA ranged between 20.85 and 42.86%) with some discrepancies in the directions of effects across reviews. The application of a structured approach by checklist may improve adherence to guidelines (e.g. Advanced Trauma Life Support) during resuscitation and might lead to a reduction in mortality among severely injured patients as compared to clinical examination (Adjusted OR 0.51; 95% CI 0.30–0.89; p = 0.018; low certainty of evidence). The use of routine WBCT seems to offer little to no effects in reducing mortality and time spent in emergency room or department, whereas non-routine WBCT seems to offer little to no effects in reducing radiation dose, intensive care unit length of stay (LOS) and hospital LOS (low-to-moderate certainty of evidence).
Conclusions
The application of structured approach by checklist during trauma resuscitation may improve patient- and process-related outcomes. Including non-routine WBCT seems to offer the best trade-offs between benefits and harm. Clinicians should consider these findings in the light of their clinical context, the volume of patients in their facilities, the need for time management, and costs.
Similar content being viewed by others
Introduction
Trauma injuries account for 4.5 million deaths globally [1] and approximately 530 000 deaths in Europe every year [2]. Almost 10% of the global burden of disease is due to trauma, and trauma is the top contributor to the burden of disease in children and adults aged 10–49 years [3].
Accurate diagnosis is essential for the best therapeutic process. Trauma care is time-sensitive, and early management of life-threatening or limb-threatening conditions is critical. The complexity of the diagnostic process of trauma patients depends not only on its time-dependent nature but it is also due to the numerous settings of care in which diagnosis occurs, the potential existence of multiple injuries in different body areas and the involvement of different specialists within a single diagnostic process [4]. Alongside the diagnostic process, it is also essential to establish adequate management of trauma patients, which represents another critical step that adds complexity to trauma cases. In general, the management of trauma patients can be performed through a structured or a non-structured approach.
The structured approach involves the management of the trauma patient in a systematic manner. For trauma patients, several checklists based on a structured approach have been developed to improve the early management, such as the life support checklist explored in training programmes for trauma assessment and treatment [5,6,7]. The first training programmes were introduced by the American College of Surgeons with a worldwide spread in the past 20 years: Prehospital Trauma Care (PTC) and Advanced Trauma Life Support (ATLS®) [8]. Moreover, a branch of the ATLS programme was established also for nurses, the Advanced Trauma Course for Nurses (ATCN®) [9]. In Europe, in 2008 a new European Trauma Course (ETC®) was organized, with the non-technical skills of the trauma team as the main objective [10]. Within all of these programmes, there is a comprehensive evaluation of the trauma patient, followed by accurate diagnostic imaging.
Conventionally after hospital admission, the trauma team performs a clinical examination, laboratory examinations and emergency room diagnostic imaging, extended focussed assessment sonography for trauma (eFAST) and chest and pelvis X-ray (primary survey). After this initial evaluation and stabilization, the team performs a secondary survey whose goal is to make a definitive and complete diagnosis of all the injuries produced by trauma (secondary survey). Contrast-enhanced Computed Tomography (CT) can be selectively obtained in patients with evidence or suspicion of some abnormality. Alternatively, thanks to the availability of even faster devices in the proximity of the emergency room, a whole body contrast-enhanced CT scan (WBCT) has been suggested as a non-selective imaging to screen all patients with suspected major trauma, even with borderline vital signs [11, 12].
Although the structured approach is widely used worldwide, the real advantages over a non-structured approach in terms of clinical safety and cost-effectiveness are still not well established. Therefore, we aimed to systematically review the literature to determine the effects of the application of a structured approach and of different diagnostic imaging strategies on critical outcomes during patient trauma resuscitation, in the context of the development of the Italian National Institute of Health guidelines on major trauma-integrated management. We aim to investigate the clinical efficacy and safety of structured approach (primary and secondary survey) by guideline checklist compared to non-structured approach (i.e. clinical examination). Moreover, routine WBCT screening was compared to non-routine WBCT in patients with suspected major trauma.
Methods
Study design and setting
This is an overview of reviews conducted following the Cochrane Guidelines [13] to support the major trauma-integrated management guideline panel of the Italian National Institute of Health (Istituto Superiore di Sanità) in formulating recommendations. We followed the Grading of Recommendations Assessment, Development and Evaluation (GRADE)-ADOLOPMENT methodology [14] and the standards defined by the Sistema Nazionale Linee Guida (SNLG) [15].
We followed the reporting guideline for an overview of reviews of healthcare interventions PRIOR [16, 17]. The protocol of the present overview of reviews is stored at the following link: https://osf.io/2s68r/.
Eligibility criteria
According to Cochrane’s definition, a systematic review (SR) is a review of the literature in which one “attempts to identify, appraise and synthesize all the empirical evidence that meets pre-specified eligibility criteria to answer a specific research question by using explicit, systematic methods that are selected with a view aimed at minimizing bias, to produce more reliable findings to inform decision-making” [18]. We included SRs if they met the following criteria: (1) population: children, young people and adults experiencing major trauma; (2) interventions: structured approach (primary and secondary survey) following guidelines such as Advanced Trauma Life Support (ATLS) or European Trauma Course (ETC) or sequence Airway, Breathing, Circulation, Disability, Exposure (ABCDE) compared to non-structured approach (e.g. clinical examination without a predefined sequence and diagnostic examinations as needed); moreover routine WBCT screening was compared to non-routine WBCT. Patients in non-routine WBCT may receive after initial evaluation and standards radiological examinations, CT scans of the selected district (e.g. C-spine) or WBCT as needed; (3) setting: in-hospital, emergency department (ED) and emergency room (ER) resuscitation phase. Studies including patients with trauma resulting from burns were excluded.
Outcome measures
Primary outcomes selected for the analyses were: overall mortality, mortality at 24 h, intensive care unit (ICU) admission/ICU length of stay (LOS), complications (e.g. multiple organ failure [MOF], multiple organ dysfunction syndrome [MODS], missed injuries), adherence and disability. Secondary outcomes were: hospital admission/ hospital LOS, time spent in Emergency Department (ED), time spent in Emergency Room (ER) and radiation dose. Outcomes were prioritized by the panel of the Italian National Institute of Health within the major trauma-integrated management guideline, Additional file 1: Appendix A. In addition, as an important domain of the GRADE approach, costs were included.
Search strategy
We searched the following electronic databases: MEDLINE (PubMed), EMBASE (Elsevier, EMBASE.com) and Cochrane Database of Systematic Reviews up to 3 May 2022 with language restricted to English, Italian, Spanish, French and German. We checked the reference lists of all studies included. The search strategy is outlined in Additional file 1: Appendix B.
Study selection and data extraction
Two independent authors screened titles and abstracts according to the eligibility criteria. Following the first phase, they independently assessed the full text of potentially relevant studies for inclusion. Any disagreement was solved by a discussion with one of the authors. A standardized data collection form was used to extract the following information: (i) SR characteristics, (ii) Patient, Intervention, Comparison and Outcome (PICO) questions, and (iii) outcome data. The authors of the selected studies were contacted if the study data were not reported in detail or were incomplete.
Internal validity and certainty of the evidence
We used the Assessing of Methodological quality of Systematic Reviews 2 (AMSTAR 2) for assessing SRs [19].
The certainty of evidence (CoE) of each outcome was judged through five dimensions (risk of bias, consistency of effect, imprecision, indirectness and publication bias) by the GRADE approach [20]. The evidence was downgraded from “high quality” by one level if serious, or by two levels if very serious limitations were found for each of the five above-mentioned dimensions. We presented a summary of findings describing the treatment effects, the CoE and the reasons for limitations.
In order to consider more reviews, a GRADE algorithm, developed for Cochrane overviews of reviews, was used to ascertain the strength of evidence of the reviews included in each treatment comparison for all primary outcomes. In this algorithm, each review starts with a ranking of high certainty and is downgraded:
-
by 1 level for serious methodological concerns such as sample size between 100 and 199 participants; high risk of bias in randomization and blinding for > 75% of included studies; high heterogeneity (I2 > 75%); and “No” on one of these AMSTAR 2 items: a priori research design, comprehensive literature search, duplicate study selection, or duplicate data extraction
-
by 2 levels for very serious concerns such as sample size < 100 participants and “No” on two or more of these AMSTAR 2 items: a priori research design, comprehensive literature search, duplicate study selection, or duplicate data extraction [21].
Data synthesis
We followed the methodology outlined in the Cochrane Handbook’s chapter on overviews of reviews [22] and the decision tree proposed by Hennessy et al. [23] to interpret the results providing context for clinical implications.
Managing overlapping
We provided a list of the primary studies included in each SR that were collated and cross-referenced in a matrix of evidence table to ascertain the degree of overlap between reviews. We calculated the corrected cover area (CCA) for the overall sample of SRs according to different comparisons stratified by outcomes. We examined the matrix for each outcome providing an interpretation of overlapping: “slight” (CCA 0–5%), “moderate” (CCA 6–10%), “high” (CCA 11–15%) or “very high” (CCA > 15%) [24].
Summary of evidence
We provided a narrative synthesis of the characteristics of the included SRs. We presented outcome data in results tables reporting effect size (e.g. mean difference [MD], standardized mean difference [SMD], relative risk [RR], odds ratio [ORs]) and their 95% CI, the number of studies and participants, treatment comparison and CoE. For the primary outcome, a visual map of the scientific evidence was created to visually display the information of each review [25]. The graphic display of the mapping is based on bubble plots, where each bubble represents one SR. This graphic provides information in three dimensions: (1) on the y-axis there is the rating of authors’ conclusions as “beneficial for intervention”, “no effect” and “beneficial for control” (they were further described in the data extraction section); (2) on the x-axis, the GRADE assessment is shown; and (3) we displayed the bubble size proportionally to the number of participants included in each SR.
We interpreted results using a conceptual framework presenting discordant results by comparisons for each outcome [26, 27]. Specifically, we examined the concordance or discordance of results in terms of different directions of the effects (e.g. effective interventions, ineffective interventions, no differences [13]) and explored the sources of heterogeneity. To assess discordances in the direction, we moved from a model in which measures of association are lower or higher than 1.0 for dichotomous outcomes, or 0 for continuous outcomes (i.e. OR of 0.80 is a favourable profile for the intervention group reducing overall mortality).
Statistical significance is set at p < 0.05. All tests will be two-sided. Data analysis was performed with STATA software.
Decision tree for overlapping reviews analysis
A decision tree was applied in case of discordant results and/or very high overlapping of included systematic reviews addressing the same PICO question, in order to avoid time-consuming and repetition of the same information (i.e. double counting of primary studies). Only the best systematic review with (i) the highest quality of evidence, (ii) the most updated bibliographic search, and (iii) a large covered area (i.e. overlapping) of included primary studies was considered for each outcome of interest in order to hypothesize the implication for practice.
Results
Study selection
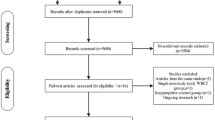
After the removal of duplicates, 1059 records were retrieved and 35 records were assessed for eligibility. Finally, nine SRs were included. The flow diagram is shown in Fig. 1.
General characteristics
The included reviews were conducted between 2012 and 2020 with one-third (33.33%) published in the past 5 years (i.e. after 2017). Literature search dates for the included reviews ranged from 2010 to 2019. Across SRs a total of 22 unique primary studies were found. Additional file 1: Appendix C reported study characteristics. A median of 7 primary studies (Interquartile range [IQR] 3–11) were included. Non-randomized controlled trials were the most common design of primary studies (n = 19) followed by controlled before-and-after studies (n = 2), and randomized controlled trials (RCTs) (n = 1). We categorized the two following comparisons: (1) “structured approach vs non-structured approach” (n = 1) and (2) “routine WBCT (always in all patients with suspected major trauma) vs non-routine WBCT (selective scans in selected patients on the basis of emergency room tests)” (n = 8). The first comparison included studies investigating trauma in adults and children carried out mainly in America, Asia and Australia. The second comparison included studies investigating trauma only in adults carried out mainly in North America, Europe, Asia and Australia (Fig. 2).
The general characteristics are reported in Table 1. The overall mortality was the most investigated outcome (9 SRs, 100%). We mapped the frequency of the outcomes across all included SRs in Table 2.
Internal validity and quality of evidence
All SRs were judged to be critically low with AMSTAR 2 (Additional file 1: Appendix D). The certainty of evidence in comparison 1 (structured approach vs non-structured approach) was very low across all investigated outcomes (Additional file 1: Appendix E). The certainty of evidence in comparison 2 (routine WBCT vs non-routine WBCT) ranged from very low to moderate with the GRADE approach (Additional file 1: Appendix E). We mainly downgraded the evidence for risk of bias in included studies and imprecision of the estimates. In most analyses, confidence intervals crossed the line of no difference with plausible effects in favour of the experimental group.
Overlapping and summary of evidence
Comparison 1. Structured approach vs non-structured approach
Overall mortality
One SR [28] (including one study in adult population) investigated this outcome reporting no difference in odds of mortality in the overall study sample (OR 1.02; CI 0.77–1.34 p = 0.904), whereas there was a statistically significant mortality reduction of 50% among patients with the most severe injuries (Injury Severity Score > 25) (adjusted OR [aOR] 0.51; 95% CI 0.30–0.89; p = 0.018).
Adherence to structured approach
One SR [28] including two studies reported this outcome without performing a meta-analysis. In one study in the paediatric setting, 14 of the 30 ATLS tasks were completed by doctors more often after checklist introduction (for all p ≤ 0.01). After adjustment, the ORs were 2.66 (95% CI 2.07–3.42) and 2.46 (95% CI 2.04–2.98) times higher for completing, respectively, primary survey, and secondary survey tasks, after the introduction of a checklist. In the other study in the adult population, 18 of the 19 clinical tasks were significantly (p < 0.05) more frequently performed after the implementation of the World Health Organization (WHO) trauma care checklist.
Complications
One SR [28] including one study reported this outcome in the adult population. The incidence of one of the ten complications (pneumonia) was slightly higher after the introduction of the checklist (aOR 1.69, 95% CI 1.03–2.80). The aOR for the other nine complications was not significantly different.
Complications as missed injuries
One SR [28] including one study reported this outcome in 3422 adult trauma patients: incidence of missed injuries did not differ before and implementation of a checklist (aOR 0.62; 95% CI 0.19–2.03; p = 0.437).
Comparison 2. Routine WBCT vs non-routine WBCT
Overall mortality
Seven SRs reported the overall mortality outcome [29,30,31,32,33,34,35], and one SR did not report any results because it did not include any eligible study [36]. The CCA showed a very high overlapping of citation primary studies (33%, Fig. 3). Compared to non-routine WBCT, routine WBCT was effective in reducing mortality in all SRs (concordant results), except for three SRs [29, 33, 35] that found no difference between groups.
24-h mortality
Two SRs with a very high overlapping of citation primary studies (42.86%) reported mortality at 24 h with discordant results: one SR showed statistically significant results favouring routine WBCT and the other no difference between groups [29, 34].
ICU LOS
Three SRs investigated ICU LOS [29, 31, 34] with a very high overlapping of citation primary studies (27.78%). There are no differences between routine WBCT and non-routine WBCT in two SRs [29, 31], whereas non-routine WBCT was effective compared to routine WBCT for reducing ICU LOS in one SR [34].
Complications
Two SRs investigated complications, reported as MODS or MOF [29, 31], with a very high overlapping of citation primary studies (50%). With concordant results, there are no differences between routine WBCT and non-routine WBCT in both SRs [29, 31].
Radiation dose
One SR [29] reported a statistically significant reduction in dose with non-routine WBCT.
Hospital LOS
Four SRs reported the hospital LOS [29, 31, 33, 34] with very high overlapping of citation primary studies (20.83%). No differences between routine WBCT and non-routine WBCT were reported in all SRs except for one SR [34] reporting non-routine WBCT as more effective than routine WBCT to reduce hospital LOS.
Time spent in ER
Two SRs reported this outcome of interest [33, 34] with a very high overlapping of citation primary studies (25%). In one SR, routine WBCT was effective compared to non-routine WBCT [34] to reduce time spent in ER. The other SR [33] did not perform a meta-analysis due to the heterogeneity of measurements.
Time spent in ED
Three SRs reported this outcome [29, 31, 35] with a very high overlapping of citation primary studies (27.78%). All SRs [29, 31, 35] showed concordant results: routine WBCT compared to non-routine WBCT was effective in reducing time spent in ED.
Hospital costs
One SR [29] including three studies investigated hospital stay cost-based parameters. Two primary studies [37, 38] conducted in Taiwan and Europe discovered that the costs associated were not statistically significant between routine WBCT and non-routine WBCT. Particularly, data reported from a multicentre RCT showed that the hospital costs of European hospital stay were €24 967 (95% CI 21 880–28 752) for the WBCT group and €26 995 (23 326–30 908) for the standard work-up group (p = 0.44). Alternatively, another primary study [39] conducted in North America found that the mean cost of a blunt trauma patient’s hospital stay increased by $4 971 after the WBCT protocol was introduced.
Decision tree for overlapping reviews analysis
In the comparison “routine WBCT versus non-routine WBCT”, SRs showed discordant results in the presence of very high overlapping of primary studies (33.33%) for the primary outcome of overall mortality. Thus, a decision tree was applied to guide the interpretation of findings.
The most updated SR was Arruzza et al. [29] including 63 539 patients: with low certainty of the evidence, mortality showed a non-statistically significant difference between groups (OR 0.85, 95% CI 0.71–1.02). Accordingly, a similar direction of effect was first reported by Sierink [33] with moderate certainty of evidence (OR 0.91, 95% CI 0.79–1.05). Figure 4 shows the evidence map of overall mortality linking the direction of the effects and the certainty of the evidence. Considering all outcomes, routine WBCT seems to offer little to no effects in reducing mortality and time spent in ER or ED, whereas non-routine WBCT seems to offer little to no effects in reducing radiation dose, ICU LOS and hospital LOS (low-to-moderate certainty of evidence). In Table 3, we reported the evidence for all outcomes for routine WBCT versus non-routine WBCT.
Discussion
This comprehensive overview of reviews included nine systematic reviews representing 22 unique primary studies and offers positive clinical results with very low to moderate-high evidence in patients with trauma.
The application of a structured approach by checklist may improve adherence to guidelines and workflow (e.g. ATLS) during resuscitation and might lead to a reduction in mortality among severely injured patients as compared to non-structured approach. The structured approach starts with the primary evaluation, which includes a classic sequence of clinical (e.g. ABCDE) and instrumental (i.e., eFAST, chest and pelvis X-ray) investigations aimed at verifying the existence of life-threatening conditions which need immediate correction. It is well recognized that this is the key to reducing mortality in severely injured patients with unstable vital signs [40]. This approach has been popularized in North America by the American College of Surgeons at the end of the twentieth century and quickly spread all over the world [8, 9, 41]. Interestingly, in our SRs no primary study was found from European countries of either the ATLS or the ETC courses about the improvement in trauma care. Probably, ATLS approach to trauma was diffused in Europe when there was already a general acceptance of the ATLS method, while ETC did not have such a diffusion to allow for significant evaluations.
After primary evaluation and stabilization of vital signs, if needed, the secondary evaluation (clinical history, head-to-toe physical examination) aims to obtain a definitive diagnosis of all the injuries produced by trauma. The routine WBCT has the undoubted advantage of high diagnostic accuracy for almost all types of post-trauma injuries [42]. Surprisingly, in our SRs there is little to no evidence of the effectiveness of routine WBCT across multiple outcomes reported in more than one review. Even if routine WBCT reduces time in ED and ER, it does not seem to reduce the mortality rate and complications, while it involves more radiation doses than non-routine WBCT. Moreover, a preliminary hospital cost analysis showed that there were no differences between WBCT and non-routine WBCT in two out of three primary studies. However, this can depend on different management of sources across countries.
The major dispute is on overall mortality and 24-h mortality rates showing discordant results across SRs. During the past years, several studies have shown an association between routine WBCT scanning and survival in patients with trauma: in some hospitals, especially in Germany, the emergency room has been organized with a CT scan device inside and the trauma patient receives a total-body scan during initial resuscitation. This approach has been associated with an improved outcome, but it has been investigated only in retrospective observational studies [11]. Furthermore, the availability of a CT scan in the emergency room is rare and could be associated with the overuse of this imaging. Discrepancies between SRs may be due to different included primary studies. The most recent SR [29] found no differences between routine WBCT and non-routine WBCT. This SR included the unique RCT [38] (multicentre, including 1 403 patients) published in 2016 which demonstrated no difference between groups, but did not include the retrospective study of Wada et al. [43], which demonstrated significant favourability towards routine WBCT. However, Wada et al. study can be at risk of some selection bias: i) CT performed at the discretion of the attending physician based on individual patient condition and not according to a predefined protocol, ii) the small sample size in non-routine WBCT group (20 vs 132) compared to routine WBCT and iii) significant differences in baseline characteristics (e.g. injury severity score, systolic blood pressure, revised trauma score) between groups. In fact, patients included in the non-routine WBCT group were probably less severely injured and consequently underwent a shorter hospital stay [43].
With concordance of all SRs, no differences between routine WBCT and non-routine WBCT on complication (e.g. MOF and MODS) were found. There is little evidence of the effectiveness of routine WBCT in reducing time spent in ED and ER but probably an increase in radiation dose. These findings have implications entailing faster diagnosis time for definitive treatment and lessening the impact of ED overcrowding but it is certainly also possible that routine WBCT scanning may do more harm than good (e.g. cancer rates, contrast-induced nephropathy). The need to limit the radiation dose is another important factor in deciding which patients might benefit from an immediate WBCT scan [38] with important implications not only from an ethical perspective but also from broader societal and national health care policy point of view.
Another condition associated with the futile use of routine WBCT could be the high rate of over-triage in trauma patients admitted after a high-energy impact and with normal vital signs, which can be as high as 75%. Modern protective devices (pre-tensioned seatbelts, airbags, helmets and car bodies with progressive deformation) have reduced the severity of injuries and many patients with high-energy impact show only minor injuries. Indiscriminate use of WBCT in these patients could lead to a significant “over-scanning”. Emergency room tests and 6–8 h of observation, followed by a careful re-evaluation, can select patients who need WBCT and discharge those with no injuries [44].
Implication for future
We found that the use of checklist for a structured approach is not investigated in Europe; in fact, primary studies were mainly carried out in America, Asia and Australia. This can reflect the clinical practice, where differences between countries can impact the use of structured approaches, as well as for the use of routine WBCT versus non-routine WBCT. In some countries, the use of structured approach is already a standard of care (e.g. North America) but not in others (e.g. Europe) [45,46,47,48].
Future studies across countries should assess the introduction of a structured approach by using a checklist to promote its adoption in trauma care as a tool for changing clinical practice, to increase the robustness of scientific evidence and to guarantee equity in healthcare assistance. Our findings support the use of structured approaches including the use of non-routine WBCT after initial assessment in selected patients.
Because of the increased radiation dose and possible other harms (e.g. induced malignancies), future research should focus on the selection of patients who would benefit from immediate total-body CT.
As well, more RCTs should be conducted to confirm preliminary results. RCTs should explore impacts on more specific patient subgroups and other relevant outcomes such as cost-effectiveness, complication rates, diagnostic accuracy and missed injury rates. Such exploration will inform a more holistic perspective regarding the efficacy of WBCT within the clinical environment.
Strength and limitations
This is the first overview of reviews evaluating the clinical implications using a structured versus non-structured approach. However, some limitations must be taken into account. Firstly, we considered SRs including one RCT and 21observational studies. The retrospective nature of some studies introduces biases otherwise minimized in prospective cohorts or RCTs. Only one RCT was considered in two SRs and it was inappropriately combined with other observational studies in the same meta-analysis [29, 34]. Secondarily, the control group encompassed all non-routine WBCT-related protocols (both ATLS and strictly selective CT), as the definition of “conventional” varies among countries and even between institutions within the same region. Third, in the first comparison, one SR included both adult and children population reporting separate results according to a specific population [28], whereas in the second comparison the paediatric field was not assessed and we were aware that the management of injuries (including the use of imaging and different modalities) is not the same. Thus, these findings cannot be generalized to children. Fourth, we planned to investigate other primary and secondary outcomes than mortality, but scarce literature is at the moment available. For instance, missed injury rates, as part of complications, were reported only in one study in a SR [28]. Few SRs investigated ICU and hospital LOS, preventing to deeply inspect the relationship between early discharges or avoided admissions and days of observation. Another difficulty in data collection regarded all patient-reported outcome measures (PROMs) such as disability and quality of life. However, it is known that PROMs collection can be particularly challenging in trauma care: low response of questionnaires administration, time-consuming and requirement of ad hoc training or specialist staff [49,50,51]. Despite barriers to PROMs collection in trauma registries, policymakers should address these challenges as PROMs have the potential to inform and guide patient-centred care and clinical decision-making in trauma care.
Conclusion
The results of the present overview show that the application of a structured approach using a checklist including non-routine WBCT after initial assessment in selected patients during trauma resuscitation can offer positive patient- and process-related outcomes. Clinicians should consider these findings in the light of their clinical context, particularly in terms of balance between harm and benefits, volume of patients in their facilities, need for timely management, and the cost of WBCT.
Availability of data and materials
The data sets generated and/or analysed during the current study are available in the Open Science Framework repository at the following link: https://osf.io/2s68r/.
Abbreviations
- ABCDE:
-
Airway, breathing, circulation, disability, exposure
- AMSTAR 2:
-
Assessing the Methodological Quality of Systematic Reviews
- aOR:
-
Adjusted odds ratio
- ATCN:
-
Advanced trauma course for nurses
- ATLS:
-
Advanced trauma life support
- CCA:
-
Corrected cover area
- CT:
-
Computed Tomography
- CI:
-
Confidence intervals
- CoE:
-
Certainty of evidence
- eFAST:
-
Extended focussed assessment sonography
- ED:
-
Emergency department
- ER:
-
Emergency room
- ETC:
-
European trauma course
- GRADE:
-
Grading of recommendations assessment, development and evaluation
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- ISS:
-
Injury severity score
- LOS:
-
Length of stay
- MD:
-
Mean difference
- MOF:
-
Multiple organ failure
- MODS:
-
Multiple organ dysfunction syndrome
- OR:
-
Odds ratio
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PICO:
-
Patient, intervention, comparison and outcome
- PTC:
-
Prehospital trauma care
- RCT:
-
Randomized controlled trials
- RoB:
-
Cochrane risk of bias
- RR:
-
Relative risk
- SMD:
-
Standardized mean difference
- SNLG:
-
Sistema Nazionale Linee Guida
- SR:
-
Systematic review
- WBCT:
-
Whole-body computer tomography
- WHO:
-
World Health Organization
References
Collaborators GBDCoD. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1151–210.
Aldridge E, Sethi D, Yon Y. Injuries: a call for public health action in Europe: an update using the 2015 WHO global health estimates. Copenhagen: World Health Organization. Regional Office for Europe; 2017. p. 2017.
Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Academies of Sciences, Engineering, and Medicine; Balogh EP, Miller BT, Ball JR, editors. Improving Diagnosis in Health Care. Washington (DC): National Academies Press (US); 2015 Dec 29. 2, The Diagnostic Process. Available from: https://www.ncbi.nlm.nih.gov/books/NBK338593/.
Kadhum M, Sinclair P, Lavy C. Are primary trauma care (PTC) courses beneficial in low- and middle-income countries–A systematic review. Injury. 2020;51(2):136–41.
Jayaraman S, Sethi D, Chinnock P, Wong R. Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev. 2014;8:CD004173.
Mohammad A, Branicki F, Abu-Zidan FM. Educational and clinical impact of advanced trauma life support (ATLS) courses: a systematic review. World J Surg. 2014;38(2):322–9.
Gerdin Wärnberg M, Berg J, Bhandarkar P, Chatterjee A, Chatterjee S, Chintamani C, et al. A pilot multicentre cluster randomised trial to compare the effect of trauma life support training programmes on patient and provider outcomes. BMJ Open. 2022;12(4): e057504.
Koestner AJ. ATCN–a door to trauma nursing leadership. J Trauma Nurs. 2002;9(1):5.
Thies KC, Deakin CD, Lott C, Robinson D, Sabbe MB, Arafat R, et al. The European trauma course–trauma teaching goes European. Resuscitation. 2014;85(1):19–20.
Huber-Wagner S, Lefering R, Qvick LM, Korner M, Kay MV, Pfeifer KJ, et al. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet. 2009;373(9673):1455–61.
Fabian TC. Whole-body CT in multiple trauma. Lancet. 2009;373(9673):1408–9.
Pollock M, Fernandes RM, Becker LA et al. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Schünemann HJ, Wiercioch W, Brozek J, Etxeandia-Ikobaltzeta I, Mustafa RA, Manja V, et al. GRADE evidence to decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J Clin Epidemiol. 2017;81:101–10.
Iannone P, Coclite D, Napoletano A, Fauci A. Manuale metodologico per la produzione di linee guida di pratica clinica: Centro Nazionale per l’Eccellenza Clinica, la Qualità e la Sicurezza delle Cure dell’Istituto Superiore di Sanità. 2018 Available from https://snlg.iss.it/wp-content/uploads/2019/04/MM_v1.3.2_apr_2019.pdf.
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335.
Gates M, Gates A, Pieper D, Fernandes RM, Tricco AC, Moher D, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ. 2022;378: e070849.
About Cochrane reviews. Available: https://www.cochranelibrary.com/about/about-cochrane-reviews [Accessed 28 January 2022].
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358: j4008.
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. An algorithm was developed to assign GRADE levels of evidence to comparisons within systematic reviews. J Clin Epidemiol. 2016;70:106–10.
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Hennessy EA, Johnson BT. Examining overlap of included studies in meta-reviews: guidance for using the corrected covered area index. Res Synth Methods. 2020;11(1):134–45.
Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Miake-Lye IM, Mak S, Lee J, Luger T, Taylor SL, Shanman R, et al. Massage for pain: an evidence map. J Altern Complement Med. 2019;25(5):475–502.
Moja L, Fernandez del Rio MP, Banzi R, Cusi C, D’Amico R, Liberati A, et al. Multiple systematic reviews: methods for assessing discordances of results. Intern Emerg Med. 2012;7(6):563–8.
Lucenteforte E, Moja L, Pecoraro V, Conti AA, Conti A, Crudeli E, et al. Discordances originated by multiple meta-analyses on interventions for myocardial infarction: a systematic review. J Clin Epidemiol. 2015;68(3):246–56.
van Maarseveen OEC, Ham WHW, van de Ven NLM, Saris TFF, Leenen LPH. Effects of the application of a checklist during trauma resuscitations on ATLS adherence, team performance, and patient-related outcomes: a systematic review. Eur J Trauma Emerg Surg. 2020;46(1):65–72.
Arruzza E, Chau M, Dizon J. Systematic review and meta-analysis of whole-body computed tomography compared to conventional radiological procedures of trauma patients. Eur J Radiol. 2020;129: 109099.
Caputo ND, Stahmer C, Lim G, Shah K. Whole-body computed tomographic scanning leads to better survival as opposed to selective scanning in trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;77(4):534–9.
Jiang L, Ma Y, Jiang S, Ye L, Zheng Z, Xu Y, et al. Comparison of whole-body computed tomography vs selective radiological imaging on outcomes in major trauma patients: a meta-analysis. Scand J Trauma Resusc Emerg Med. 2014;22:54.
Hajibandeh S, Hajibandeh S. Systematic review: effect of whole-body computed tomography on mortality in trauma patients. J Inj Violence Res. 2015;7(2):64–74.
Sierink JC, Saltzherr TP, Reitsma JB, Van Delden OM, Luitse JS, Goslings JC. Systematic review and meta-analysis of immediate total-body computed tomography compared with selective radiological imaging of injured patients. Br J Surg. 2012;99(Suppl 1):52–8.
Chidambaram S, Goh EL, Khan MA. A meta-analysis of the efficacy of whole-body computed tomography imaging in the management of trauma and injury. Injury. 2017;48(8):1784–93.
Healy DA, Hegarty A, Feeley I, Clarke-Moloney M, Grace PA, Walsh SR. Systematic review and meta-analysis of routine total body CT compared with selective CT in trauma patients. Emerg Med J. 2014;31(2):101–8.
Van Vugt R, Keus F, Kool D, Deunk J, Edwards M. Selective computed tomography (CT) versus routine thoracoabdominal CT for high-energy blunt-trauma patients. Cochrane Database Syst Rev. 2013;12:CD009743.
Hong ZJ, Chen CJ, Yu JC, Chan DC, Chou YC, Liang CM, et al. The evolution of computed tomography from organ-selective to whole-body scanning in managing unconscious patients with multiple trauma: a retrospective cohort study. Medicine. 2016;95(37): e4653.
Sierink JC, Treskes K, Edwards MJ, Beuker BJ, den Hartog D, Hohmann J, et al. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. Lancet. 2016;388(10045):673–83.
James MK, Schubl SD, Francois MP, Doughlin GK, Lee SW. Introduction of a pan-scan protocol for blunt trauma activations: what are the consequences? Am J Emerg Med. 2017;35(1):13–9.
Navarro S, Montmany S, Rebasa P, Colilles C, Pallisera A. Impact of ATLS training on preventable and potentially preventable deaths. World J Surg. 2014;38(9):2273–8.
Hedges JR, Adams AL, Gunnels MD. ATLS practices and survival at rural level III trauma hospitals, 1995–1999. Prehosp Emerg Care. 2002;6(3):299–305.
Huber-Wagner S, Kanz KG, Hanschen M, van Griensven M, Biberthaler P, Lefering R. Whole-body computed tomography in severely injured patients. Curr Opin Crit Care. 2018;24(1):55–61.
Wada D, Nakamori Y, Yamakawa K, Yoshikawa Y, Kiguchi T, Tasaki O, et al. Impact on survival of whole-body computed tomography before emergency bleeding control in patients with severe blunt trauma. Crit Care. 2013;17(4):R178.
Reitano E, Granieri S, Sammartano F, Cimbanassi S, Galati M, Gupta S, et al. Avoiding immediate whole-body trauma CT: a prospective observational study in stable trauma patients. Updates Surg. 2022;74(1):343–53.
Spanjersberg WR, Bergs EA, Mushkudiani N, Klimek M, Schipper IB. Protocol compliance and time management in blunt trauma resuscitation. Emerg Med J. 2009;26(1):23–7.
Santora TA, Trooskin SZ, Blank CA, Clarke JR, Schinco MA. Video assessment of trauma response: adherence to ATLS protocols. Am J Emerg Med. 1996;14(6):564–9.
McCrum ML, McKee J, Lai M, Staples J, Switzer N, Widder SL. ATLS adherence in the transfer of rural trauma patients to a level I facility. Injury. 2013;44(9):1241–5.
Tsang B, McKee J, Engels PT, Paton-Gay D, Widder SL. Compliance to advanced trauma life support protocols in adult trauma patients in the acute setting. World J Emerg Surg. 2013;8(1):39.
Polinder S, van Beeck EF, Essink-Bot ML, Toet H, Looman CW, Mulder S, et al. Functional outcome at 2.5, 5, 9, and 24 months after injury in the Netherlands. J Trauma. 2007;62(1):133–41.
Gabbe BJ, Sutherland AM, Hart MJ, Cameron PA. Population-based capture of long-term functional and quality of life outcomes after major trauma: the experiences of the Victorian State Trauma Registry. J Trauma. 2010;69(3):532–6.
Turner GM, Slade A, Retzer A, McMullan C, Kyte D, Belli A, et al. An introduction to patient-reported outcome measures (PROMs) in trauma. J Trauma Acute Care Surg. 2019;86(2):314–20.
Acknowledgements
We thank the Istituto Superiore di Sanità documentalist Scilla Pizzarelli who performed the search strategy.
Funding
The work was supported by Istituto Superiore di Sanità that played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
SG, SB, GC, PI and OC provided substantial contributions to the conception or design of the work. SG, SB, GC, PI and OC performed acquisition, analysis, or interpretation of data for the work. SG, SB and GC drafted the work. All authors contributed to important intellectual content, reviewed the version to be published, and agreed for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplementary Information. Appendix A. Research question and search strategy;Appendix B. Modified Rand Delphi Process for prioritization of critical, important and unimportant outcomes;Appendix C. Primary studies and characteristics;Appendix D. Internal validity of systematic reviews;Appendix E. Certainty of Evidence.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gianola, S., Bargeri, S., Biffi, A. et al. Structured approach with primary and secondary survey for major trauma care: an overview of reviews. World J Emerg Surg 18, 2 (2023). https://doi.org/10.1186/s13017-022-00472-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-022-00472-6