Abstract
Background
PSMA-PET is increasingly used for staging prostate cancer (PCA) patients. However, it is not clear if quantitative imaging parameters of positron emission tomography (PET) have an impact on disease progression and are thus important for the prognosis of localized PCA.
Methods
This is a monocenter retrospective analysis of 86 consecutive patients with localized intermediate or high-risk PCA and PSMA-PET before treatment The quantitative PET parameters maximum standardized uptake value (SUVmax), tumor asphericity (ASP), PSMA tumor volume (PSMA-TV), and PSMA total lesion uptake (PSMA-TLU = PSMA-TV × SUVmean) were assessed for their prognostic significance in patients with radiotherapy or surgery. Cox regression analyses were performed for biochemical recurrence-free survival, overall survival (OS), local control, and loco-regional control (LRC).
Results
67% of patients had high-risk disease, 51 patients were treated with radiotherapy, and 35 with surgery. Analysis of metric PET parameters in the whole cohort revealed a significant association of PSMA-TV (p = 0.003), PSMA-TLU (p = 0.004), and ASP (p < 0.001) with OS. Upon binarization of PET parameters, several other parameters showed a significant association with clinical outcome. When analyzing high-risk patients according to the primary treatment approach, a previously published cut-off for SUVmax (8.6) showed a significant association with LRC in surgically treated (p = 0.048), but not in primary irradiated (p = 0.34) patients. In addition, PSMA-TLU (p = 0.016) seemed to be a very promising biomarker to stratify surgical patients.
Conclusion
Our data confirm one previous publication on the prognostic impact of SUVmax in surgically treated patients with high-risk PCA. Our exploratory analysis indicates that PSMA-TLU might be even better suited. The missing association with primary irradiated patients needs prospective validation with a larger sample size to conclude a predictive potential.
Trial registration Due to the retrospective nature of this research, no registration was carried out.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Prostate cancer (PCA) accounted for 7.1% of all cancer cases in 2018, being the second most common cancer in men worldwide [1]. Therapeutic options for localized PCA include radical prostatectomy, radiotherapy, and active surveillance. The D’Amico classification is routinely used for clinical risk stratification [2]. While PCA-specific ten-year mortality is negligible for low-risk patients regardless of the chosen therapeutic approach [3], cancer-specific mortality is considerably higher in high-risk patients despite treatment intensification, i.e. concomitant androgen deprivation therapy (ADT), dose-escalated radiotherapy or extended pelvic lymph node dissection [3,4,5,6]. Even in intermediate-risk patients around 15% present tumor progression within 5 years after treatment, even with high-dose radiotherapy [7]. Current primary treatment approaches for unfavorable intermediate-risk or high-risk PCA with disease limited to the prostate is either surgery or radiotherapy combined with ADT. While both treatment approaches show a similar oncological outcome, treatment-related side effects differ considerably between both treatment approaches [8]. Additionally, surgical patients usually receive adjuvant or salvage radiotherapy to the prostate fossa in case of biochemical recurrence, leading to a combination of surgical and radiation-induced side effects [9]. Therefore, biomarkers for better treatment personalizations are urgently needed.
Positron emission tomography (PET)/Computer tomography (CT) with prostate-specific membrane antigen (PSMA) is increasingly used for staging high-risk patients due to its high sensitivity and specificity regarding the detection of lymph nodes or distant metastases [10, 11]. The diagnostic accuracy of PSMA-PET/CT for staging therapy-naïve patients [12, 13] and the greater efficacy in detecting early recurrences, small lymph node metastases, and bone metastases [14] has been shown to be superior to bone scintigraphy and CT.
In addition to improved staging of patients, quantitative PET parameters can potentially be used as imaging biomarkers. This holds true for the most frequently investigated parameter SUVmax (maximum standardized uptake value, normalized to body weight) which delivers additional prognostic information in various diseases and for various PET tracers [15,16,17]. Due to the novelty of PSMA-PET imaging, data on the prognostic value of quantitative imaging parameters for this specific tracer is sparse and mostly limited to advanced stages of disease. So far, most data have been published on metastatic patients treated with PSMA radioligand therapy [18, 19]. Two recent publications showed that quantitative PSMA-PET parameters are associated with biochemical recurrence-free survival in PCA patients treated with primary surgery [20, 21].
This study aimed to investigate the prognostic value of various quantitative PSMA-PET parameters, including previously published cutoff values [21], in a cohort of intermediate/high-risk patients. In contrast to existing publications, these analyses were restricted to PET-staged localized PCA treated with curative intent (either surgery or radiotherapy ± ADT), i.e., patients without nodal or distant metastatic disease after PSMA-PET staging.
Patients and methods
Patient cohort
For this retrospective analysis, all patients who underwent PSMA-PET at Charité – Universitätsmedizin Berlin, Campus Virchow-Klinikum between January 2015 and December 2018 were reviewed and checked for inclusion and exclusion criteria. Results of imaging and implications for staging of patients included up to March 2018, have been published [22]. For this analysis, we re-evaluated the existing patient cohort and added patients with pre-treatment PSMA-PET until to December 2018, as recently published [23].
This allowed identification of all treatment-naïve patients with biopsy-proven PCA who underwent PSMA-PET/CT for initial staging. Patients were eligible for this analysis if they presented with intermediate/high-risk disease and underwent active therapy, i.e., radiotherapy with/without ADT or surgery, and if at least one follow-up visit was available. Exclusion criteria were patients with detectable lymph nodes or distant metastases by PET imaging. This resulted in a cohort of eighty-six patients. From this cohort, thirty-five patients underwent radical prostatectomy (RP), and fifty-one patients underwent radiotherapy (RT).
Referral for PSMA-PET was at the discretion of the treating urologists and radiation oncologists, particularly because PSMA-PET has not been established for routine staging. The study was approved by the local ethics committee (EA4/168/16).
Clinical parameters
Clinical data including prostate-specific antigen (PSA), clinical T-stage, and Gleason score assessed at biopsy before imaging were available from electronic databases, as well as from patient records. For the subgroup of patients who underwent surgery, the surgical Gleason scores were recorded. The Gleason scores were classified according to the recommendations of the consensus conference of the International Society of Urological Pathology (ISUP) of 2014 on Gleason grading of PCA [24]. Additionally, ADT usage at the time of PSMA-PET/CT, during active therapy (RT, RP) and during follow-up was assessed.
Based on the clinical parameters, a three-tiered classification was made into low, intermediate, or high-risk patients according to D’Amico scoring. During follow-up, patients usually underwent repeated PSA examinations every three months. In case of biochemical recurrence (BCR), further diagnostic examination was left at the discretion of the treating urologist/radiation oncologist. The endpoints of the study were local tumor control (LC), loco-regional tumor control (LRC), biochemical recurrence-free survival (BRFS), and overall survival (OS). LC and LRC were defined as local/loco-regional recurrence detected by magnetic resonance imaging (MRI) or PSMA-PET. Since surgically treated patients underwent salvage radiotherapy to the prostate fossa usually at low PSA values and therefore did not present macroscopic local recurrence, we used the following approach: A local recurrence after surgery was considered if patients presented a biochemical recurrence with complete biochemical remission after salvage radiotherapy to the prostate fossa. Patients who received additional radiotherapy to the lymphatic drainage had to be excluded in this analysis regarding the endpoint local recurrence as the complete remission after irradiation could also have been due to microscopic regional recurrences. Biochemical recurrence was defined as follows: In patients treated with primary radiotherapy, BCR was defined according to the Radiation Therapy Oncology Group- American Society for Therapeutic Radiology and Oncology (RTOG-ASTRO)-Phoenix consensus recommendation [25] as an increase of 2 ng/ml or more above the lowest PSA level achieved (PSA nadir). After radical prostatectomy, the American Urological Association (AUA) expert panel recommends defining biochemical recurrence as a first serum prostate specific antigen of > or = 0.2 ng/ml, with a second confirmatory PSA value of > 0.2 ng/ml [26].
Imaging
Imaging was previously described [22], briefly, PSMA-PET/CT was performed with the radiotracer [68Ga]Ga-PSMA-HBED-CC on a dedicated PET/CT scanner (Gemini TF 16; Philips, The Netherlands) with Philips Astonish TF technology. Injection of [68Ga]Ga-PSMA-HBED-CC was given intravenously (median activity 153 MBq; range: 71–227 MBq), Median activity per kg body weight: 1.6 MBq/kg (range: 0.8–2.6 MBq/kg). PET imaging was conducted at a Median of 98 min after injection (range: 39–188 min). Patients were positioned supine and scanned from the head to the proximal thighs (emission, 90–180 s per bed position; 3D acquisition mode; bed overlap, 53.3%). Attenuation correction was based on non-enhanced low-dose CT (automatic tube current modulation; maximum tube current–time product, 50 mA; tube voltage, 120 kV; gantry rotation time, 0.5 s) reconstructed with a slice thickness of 5 mm (convolution kernel, B08). Raw PET data were reconstructed using iterative reconstruction with TOF analysis (Philips Astonish TF technology; BLOB-OS-TF; iterations, 3; subsets, 33). Projection data were reconstructed with matrix size 144 × 144 and voxel size 4 × 4 × 4 mm3 [22].
Image evaluation
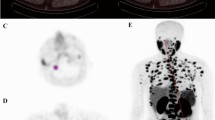
All 3D region of interest (ROI) definitions and image analyses were performed using ROVER software, version 3.0.41 (ABX, Radeberg, Germany). Initially, a large spherical mask was placed around the prostate and the base of the seminal vessels to delineate the metabolically active part of the primary tumor based on a threshold of 41% SUVmax, as suggested in a recent analysis [20].
The resulting ROIs were visually analyzed by an experienced observer (SZ) to manually exclude tracer uptake of surrounding normal tissue (bladder and/or rectum). An example of delineation is shown in Supplementary Fig. 1. In patients with low diffuse tracer accumulation in the prostate, the most intense single voxel was manually delineated for calculation of Maximum standardized uptake value (SUVmax). SUVmax, average standardized uptake value (SUVmean), the delineated tumor volume according to PSMA uptake (PSMA-TV) and the PSMA total lesion uptake (PSMA-TLU = PSMA-TV × SUVmean) were calculated. In addition, the novel quantitative PET parameter tumor asphericity (ASP) was calculated. ASP calculation was described in detail before. ASP is defined as
where S und V are surface and volume of the lesion and it measures the fractional increase of the surface area of a lesion compared to the surface area of spherical lesion with the same volume (which would have a value of zero). More details can be found in [23, 27, 28].
Statistical analyses
Differences between groups (surgery vs. radiotherapy) were analyzed by Mann–Whitney U test. The association of BRFS, OS, LRC and LC, measured from start of therapy to death and/or event, with clinically relevant parameters as well as quantitative PET parameters was analyzed using univariable Cox proportional hazards regression in which the PET parameters were included as metric parameters. In a second step, the PET parameters were binarized and again analyzed in univariable Cox regression. For SUVmax the previously published value of 8.6 was used for this purpose. The cutoff values for all other parameters were calculated by performing a univariable Cox regression for each measured value. In each variable, the value leading to the hazard ratio (HR) with the highest significance was used as cutoff. Cutoff values for the clinical parameters age and iPSA were computed accordingly. The cutoff values were separately computed for each endpoint. The probability of survival was computed and rendered as Kaplan–Meier curves. Statistical significance was assumed at a p value of 0.05 or lower. Statistical analysis was performed with the R language and environment for statistical computing version 4.2.3 [29].
Results
Patient cohort
During the study period, 136 patients underwent PSMA-PET/CT staging for treatment naïve localized PCA. After excluding all patients that did not meet the specified inclusion criteria, eighty-six patients were evaluable for further analyses. Exclusion was most frequently due to low-risk tumors, refusal of any therapy by the patient or missing data on treatment or follow-up information. Figure 1 shows a flowchart of all patients that have been screened for this study. Median follow up time in analyzed patients was 42 months. In the whole cohort thirteen patients had a biochemical relapse and seven patients died during follow-up. In the intermediate risk biochemical relapse/death occurred in three/one patients, in the high-risk group there were ten/six event.
Table 1 summarizes the patient and clinical tumor characteristics for all patients (D’Amico intermediate and high risk groups).
Association of quantitative PET parameters with clinical outcome in the whole cohort
Analysis of metric PET parameters revealed a significant association of PSMA-TV (p = 0.003), PSMA-TLU (p = 0.004) and ASP (p < 0.001) with OS as shown in Table 2.
Upon binarization of PET parameters, ASP, PSMA-TV and PSMA-TLU showed a significant association or a statistical trend for OS. In addition, an association with several other investigated endpoints was observed, as shown in Table 3.
Quantitative PET parameters in high-risk patients
Since most data are available for high-risk patients and this group is of greatest interest for treatment personalization, high-risk patients were evaluated seperately. Results for binarized PET parameters were similar. Details are shown in Supplementary Table 1. Supplementary Table 2 summarizes the patient and clinical tumor characteristics for the high-risk patients according to the primary treatment approach, radiotherapy vs. radical prostatectomy, and shows results of statistical group comparison. Fifty-nine men met high-risk criteria, of whom 26 underwent RP and 33 received RT. Baseline characteristics were similar in the two groups except for age. Patients in the radiotherapy group were significantly older (p = 0.04).
Quantitative PET parameters in patients according to primary treatment approach
Finally, all quantitative PET parameters were analyzed according to primary treatment approach. While cut-offs for PSMA-TV and PSMA-TLU were optimized for each clinical endpoint, for SUVmax a previously published cut-off was chosen for each endpoint. Figure 2 shows results for these three PET parameters in surgically treated high-risk patients.
PSMA-TV significantly stratified patients at high versus low-risk for biochemical recurrence (p = 0.05), and PSMA-TLU showed a significant discrimination for patients at high versus low-risk for loco-regional tumor recurrence (p = 0.016). The previously published cut-off value SUVmax = 8.6 which was established in surgically treated patients, showed a significant discrimination between patients at high versus low risk for loco-regional recurrence after surgical treatment (p = 0.048). The same analyses in patients treated with primary radiotherapy did not reveal a significant association with outcome, including SUVmax = 8.6 with the endpoint LRC (p = 0.34), there were also no significant associations of quantitative PET metrics with BCR (see Supplementary Fig. 2). Results for surgical patients remained comparable when including intermediate and high-risk patients, as shown in Supplementary Fig. 3. As PSMA-TLU 97.8 showed the highest potential for risk stratification in surgical patients, this parameter was further analyzed. PSMA-TLU > 97.8 does not seem to be associated with risk for biochemical recurrence in irradiated patients as irradiated patients with higher values presented no case of biochemical recurrence as shown in Fig. 3.
Risk for biochemical recurrence according to primary treatment approach (surgery vs. no surgery, i.e., radiotherapy or ADT plus radiotherapy). Patients are stratified according to TLU 97.8 and treatment approach: Patients with TLU below 97.8 (A) and above 97.8 (B). Outcome of the whole cohort is shown on C
Discussion
Here, we report the most comprehensive analysis of quantitative PSMA PET parameters and patient outcome for localized PCA treated with curative intent. To our best knowledge, this is the first evaluation of patients treated with primary radiotherapy, as two recent publications only evaluated surgically treated patients [20, 30]. While it was possible to validate a previously published cut-off for SUVmax in surgically treated patients [21, 30], it was not possible to validate this cutoff in patients treated with primary radiotherapy.
Recent ex vivo analyses for radiosensitivity seem to encourage the potential of PSMA-PET as a predictive biomarker for radiotherapy. Marinescu and colleagues used an assay with residual γH2AX foci after ex vivo radiotherapy and reported a positive correlation between radiation-induced γH2AX foci, i.e. a surrogate of irradiation-induced DNA double-strand breaks, and PSMA uptake, measured by SUVmax [31]. These analyses would suggest an association between radiosensitivity and higher uptake of PSMA.
Our results suggest that quantitative PET parameters have prognostic potential in terms of disease progression and outcome in high-risk patients with surgically treated PCA, which may allow better stratification of patients. This could mean that these patients should preferentially be treated by primary radiotherapy and ADT or, if surgery has to be performed, these high-risk patients could for example receive neoadjuvant ADT before surgery with the aim to reduce the risk for local recurrence by downsizing. While it was possible to validate a recently published cut-off value for SUVmax [21], other quantitative parameters have not been investigated in this setting before. Our preliminary analyses suggest that PSMA-TV and PSMA-TLU might be even better quantitative parameters regarding risk stratification. The missing association of the quantitative parameters with primary irradiated patients could indicate a potential predictive value that might be used for treatment guidance in adjunct to other key factors, i.e. side effects of the chosen therapeutic approach and individual patient preference.
Several recent studies investigated the prognostic value of quantitative PSMA-PET parameters. Most of these studies analyzed advanced stage disease. For example, PSMA uptake has been associated with prognosis and outcome in advanced metastatic disease. Calderoni and colleagues reported an association between SUVmax and treatment response in 160 metastatic castration-resistant PCA patients undergoing various systemic treatments [32]. Due to extensive PET imaging, most data is available for patients undergoing PSMA radioligand therapy. In a small cohort of 40 patients with advanced PCA and radioligand therapy, Seifert and colleagues reported that semiautomatically quantified pre-treatment tumor volume (PSMATV50) was significantly associated with OS and independent from other important prognostic factors like alkaline phosphatase (ALP) and PSA [33]. In another study with 38 patients who underwent [177Lu]Lu-PSMA-617 radioligand therapy (RLT), the change in total tumor volume before and after RLT was significantly associated with PSA response and overall survival after a median follow-up of 17 months [19]. A recent retrospective multicenter analysis of 237 men treated with RLT established the tumor-to-salivary gland ratio as a prognostic factor, as the authors were able to show an association with PSA response and OS [34].
Given the available data in metastatic disease, determining quantitative imaging parameters as an indicator of disease progression is also of interest in less advanced tumor stages. So far, only few studies investigated patients with localized PCA. It is important to note that in these stages OS is usually not reported due to the short follow-up period and often particularly good prognosis in low- and intermediate-risk patients. Therefore, surrogate parameters are frequently used, for example, biochemical recurrence, measured by serum PSA. However, these surrogate markers are controversial since the association with important clinical outcome parameters like OS is only weak [35, 36]. This limitation also holds true for our study, as there were only few deaths during the follow-up period. Additionally, it is not clear if these events were caused by tumor aggressiveness or due to comorbidities in an old patient population. Regarding BCR, its definition is subject to different criteria and depends on the type of local therapy: Prostatectomy or radiotherapy [25, 26]. Differences in the definition of PSA relapse thus have an additional impact on comparability. Due to the known limitations of BCR [37, 38], we included local control and loco-regional control as additional, clinical more relevant endpoints. So far only data on the association of quantitative PSMA PET parameters and BCR after surgery has been published.
Xuefeng et al. reported good efficacy in predicting biochemical recurrence (BCR) using PET-CT before prostatectomy. They found a significant association between SUVmax and BCR (p < 0.01) [39]. Another large retrospective cohort study with 848 men also supports the association between quantitative PSMA parameters and patient outcome: Roberts and colleagues reported that PSMA intensity measured by SUVmax is a novel independent prognostic factor for biochemical recurrence-free survival (BRFS) after radical prostatectomy. PSMA intensity was significantly associated with a shorter time to biochemical recurrence [30]. This corroborates previous reports by Wang and colleagues who found an association of SUVmax and SUVmean with BCR in 186 surgically treated patients [40]. Interestingly, this is one of the few studies, that investigated other quantitative PET parameters like tumor volume and total lesion uptake. Contrary to our findings, these other parameters did not perform better than SUV, which might indicate an accidental finding due to the small numbers of patients in our study. In another study, SUVmax of the primary tumor was associated with pre-and postoperative variables as it was highly associated with known conventional prognostic factors such as the International Society of Urological Pathology (ISUP) pathological score and lymph node status [41].
In our study, we successfully confirmed previous evidence on the prognostic value of quantitative PET parameters in surgically treated patients with high-risk PCA by applying a published cut-off for SUVmax [21, 30]. Our study has several strengths: it includes extensive imaging evaluation of different quantitative PET parameters and is restricted to patients without evidence of metastases by all imaging techniques, including PSMA-PET. We think the latter is particularly important because otherwise the prognostic accuracy of PET parameters might be heavily confounded by the better diagnostic accuracy to detect lymph nodes or distant metastases (both factors have a known strong detrimental effect on patient outcome [20]). In addition, the same PSMA tracer and PET device were used in all patients, facilitating comparability of PET parameters between individual patients. Nevertheless, our data must be interpreted as preliminary and hypothesis-generating because our study also has several important limitations. First, this was a retrospective evaluation with a population of a single center. Second, the quantitative values were collected retrospectively and without standardization (e.g., in terms of recording time), so they may be subject to measurement and reader variation but also reflect a real-world application environment. A major limitation is the high variability of injected dose per kg. We think this can partially be explained by the long follow-up of analyzed patients. One must bear in mind that these patients have been scanned immediately after the introduction of PSMA-PET. Therefore, standardized protocols were not available at that time for this specific tracer. As an additional limitation, the PET scanner is therefore not the most recent one and has a lower resolution compared to the newest generation scanners. In modern PET scanners, voxel sizes are usually smaller than in the scanner that was used for the current analysis, owing to the improved intrinsic spatial resolution and/or system sensitivity of these scanners. In small target lesions, a larger voxel size could result in an underestimation of the SUVmax compared to a scanner or reconstruction with a smaller voxel size. This effect would have to be considered when attempting to harmonize SUV values, for example, through the use of adaptive Gaussian filters [42].
Especially the high variability in injected dose and scan duration directly affects the SUV quantification. Additionally, it is a well-known phenomenon that the comparability of SUVs across different PET scanners or reconstruction methods is limited. The scanner used for the current analysis complies with the initial standard set by the EANM Research GmbH’s (EARL) initiative in 2010. It has already been demonstrated that SUV values from newer generation scanners, which adhere to the updated EARL standard [43], cannot be directly compared, and established prognostic SUV thresholds may not necessarily be transferrable [44]. Consequently, when transferring the currently used thresholds or quantitative (SUV) results to new PET scanners, correction methods or harmonization steps would have to be applied [42]. This is particularly true for small lesions, whose activity or SUV might be underestimated due to the limited reconstructed spatial resolution of the used scanner compared to newer scanners or advanced reconstruction methods.
However, it should be noted that even in this suboptimal setting we were able to confirm the previously published prognostic value of SUV, underlining the validity of these results. Third, the follow-up time of patients is still relatively short and needs to be confirmed by longer follow-up. As mentioned earlier, this is particularly true for OS, which would require 10 years of follow-up even in high-risk patients. Another limitation regards the relatively small number of patients, especially when analyzing sub-groups. Due to the small sub-groups, we did not perform multivariate analyses, which is another limitation of the current study. Due to the small number of patients, our results should be interpreted as hypothesis generating. Especially the association of quantitative PET parameters with outcome in surgically treated, but not in irradiated patients. While these findings are of great interest since they could indicate a predictive biomarker that could potentially be used for better treatment decisions, these findings must be regarded as exploratory. It is an important limitation that the number of events in the group of irradiated patients is low, therefore the missing statistical association might only be due to this. In addition, our chosen approach to classify complete biochemical response after salvage radiotherapy as local recurrence might be debatable, as local control is usually defined based on follow-up imaging. Furthermore, clinical and pathological staging might differ in surgical patients, as previously reported [23]. We decided to compare patients according to clinical staging, as this would be the information available for treatment decisions in a clinical setting.
Conclusion
Our exploratory analysis suggests that SUVmax, PSMA-TV and PSMA-TLU are promising parameters for better patient stratification in curatively treated high and intermediate-risk PCA patients. Quantitative PSMA-PET parameters might also have a predictive value regarding the chosen therapeutic approach. After successful prospective validation of these findings, these parameters could aid physicians in treatment selection and shared decision making.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADT:
-
Androgen deprivation therapy
- ALP:
-
Alkaline phosphatase
- ASP:
-
Tumour asphericity
- AUA:
-
American Urological Association
- BRFS:
-
Biochemical recurrence-free survival
- CT:
-
Computer tomography
- ISUP:
-
International Society of Urological Pathology
- LC:
-
Local control
- LRC:
-
Loco-regional control
- MRI:
-
Magnetic resonance imaging
- OS:
-
Overall survival
- PCA:
-
Prostate cancer
- PET:
-
Positron emission tomography
- PSA:
-
Prostate specific antigen
- PSMA-PET:
-
Prostata-Specific Membrane Antigen-positron emission tomography
- PSMA-TLU:
-
PSMA total lesion uptake
- PSMA-TV:
-
PSMA tumor volume
- PSMATV50:
-
Pre-treatment tumor volume
- RLT:
-
Radioligand therapy
- ROI:
-
Region of interest
- RTOG-ASTRO-Phoenix:
-
Radiation Therapy Oncology Group-American Society for Therapeutic Radiology and Oncology Phoenix
- RP:
-
Radical prostatectomy
- RT:
-
Radiotherapy
- SUVmax :
-
Maximum standardized uptake value
- SUVmean :
-
Mean standardized uptake value
- SZ:
-
Sebastian Zschaeck
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. https://doi.org/10.3322/caac.21492.
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969–74. https://doi.org/10.1001/jama.280.11.969.
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, et al. 10-Year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med. 2016;375:1415–24. https://doi.org/10.1056/NEJMoa1606220.
Jiang T, Markovic D, Patel J, Juarez JE, Ma TM, Shabsovich D, et al. Radiation therapy dose and androgen deprivation therapy in localized prostate cancer: a meta-regression of 5-year outcomes in phase III randomized controlled trials. Prostate Cancer Prostatic Dis. 2022;25:126–8. https://doi.org/10.1038/s41391-021-00432-2.
Roach M. Dose escalated external beam radiotherapy versus neoadjuvant androgen deprivation therapy and conventional dose external beam radiotherapy for clinically localized prostate cancer: do we need both? Strahlenther Onkol Organ Dtsch Rontgengesellschaft Al. 2007;183(S2):26–8. https://doi.org/10.1007/s00066-007-2011-8.
Lestingi JFP, Guglielmetti GB, Trinh Q-D, Coelho RF, Pontes J, Bastos DA, et al. Extended versus limited pelvic lymph node dissection during radical prostatectomy for intermediate- and high-risk prostate cancer: early oncological outcomes from a randomized phase 3 trial. Eur Urol. 2021;79:595–604. https://doi.org/10.1016/j.eururo.2020.11.040.
Michalski JM, Winter KA, Prestidge BR, Sanda MG, Amin M, Bice WS, et al. Effect of brachytherapy with external beam radiation therapy versus brachytherapy alone for intermediate-risk prostate cancer: NRG Oncology RTOG 0232 Randomized Clinical Trial. J Clin Oncol Off J Am Soc Clin Oncol. 2023;41:4035–44. https://doi.org/10.1200/JCO.22.01856.
Chen RC, Basak R, Meyer A-M, Kuo T-M, Carpenter WR, Agans RP, et al. Association between choice of radical prostatectomy, external beam radiotherapy, brachytherapy, or active surveillance and patient-reported quality of life among men with localized prostate cancer. JAMA. 2017;317:1141–50. https://doi.org/10.1001/jama.2017.1652.
Kneebone A, Fraser-Browne C, Duchesne GM, Fisher R, Frydenberg M, Herschtal A, et al. Adjuvant radiotherapy versus early salvage radiotherapy following radical prostatectomy (TROG 08.03/ANZUP RAVES): a randomised, controlled, phase 3, non-inferiority trial. Lancet Oncol. 2020;21:1331–40. https://doi.org/10.1016/S1470-2045(20)30456-3.
Cytawa W, Seitz AK, Kircher S, Fukushima K, Tran-Gia J, Schirbel A, et al. 68Ga-PSMA I&T PET/CT for primary staging of prostate cancer. Eur J Nucl Med Mol Imaging. 2020;47:168–77. https://doi.org/10.1007/s00259-019-04524-z.
Petersen LJ, Zacho HD. PSMA PET for primary lymph node staging of intermediate and high-risk prostate cancer: an expedited systematic review. Cancer Imaging Off Publ Int Cancer Imaging Soc. 2020;20:10. https://doi.org/10.1186/s40644-020-0290-9.
Herlemann A, Wenter V, Kretschmer A, Thierfelder KM, Bartenstein P, Faber C, et al. 68Ga-PSMA positron emission tomography/computed tomography provides accurate staging of lymph node regions prior to lymph node dissection in patients with prostate cancer. Eur Urol. 2016;70:553–7. https://doi.org/10.1016/j.eururo.2015.12.051.
Maurer T, Gschwend JE, Rauscher I, Souvatzoglou M, Haller B, Weirich G, et al. Diagnostic efficacy of (68)Gallium-PSMA positron emission tomography compared to conventional imaging for lymph node staging of 130 consecutive patients with intermediate to high risk prostate cancer. J Urol. 2016;195:1436–43. https://doi.org/10.1016/j.juro.2015.12.025.
Dorff TB, Fanti S, Farolfi A, Reiter RE, Sadun TY, Sartor O. The Evolving role of prostate-specific membrane antigen-based diagnostics and therapeutics in prostate cancer. Am Soc Clin Oncol Educ Book Am Soc Clin Oncol Annu Meet. 2019;39:321–30. https://doi.org/10.1200/EDBK_239187.
Zhang Q, Gao X, Wei G, Qiu C, Qu H, Zhou X. Prognostic value of MTV, SUVmax and the T/N Ratio of PET/CT in patients with glioma: a systematic review and meta-analysis. J Cancer. 2019;10:1707–16. https://doi.org/10.7150/jca.28605.
Lee MI, Jung YJ, Kim DI, Lee S, Jung CS, Kang SK, et al. Prognostic value of SUVmax in breast cancer and comparative analyses of molecular subtypes: a systematic review and meta-analysis. Medicine. 2021;100: e26745. https://doi.org/10.1097/MD.0000000000026745.
Berghmans T, Dusart M, Paesmans M, Hossein-Foucher C, Buvat I, Castaigne C, et al. Primary tumor standardized uptake value (SUVmax) measured on fluorodeoxyglucose positron emission tomography (FDG-PET) is of prognostic value for survival in non-small cell lung cancer (NSCLC): a systematic review and meta-analysis (MA) by the European Lung Cancer Working Party for the IASLC Lung Cancer Staging Project. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2008;3:6–12. https://doi.org/10.1097/JTO.0b013e31815e6d6b.
Seifert R, Kessel K, Schlack K, Weber M, Herrmann K, Spanke M, et al. PSMA PET total tumor volume predicts outcome of patients with advanced prostate cancer receiving [177Lu]Lu-PSMA-617 radioligand therapy in a bicentric analysis. Eur J Nucl Med Mol Imaging. 2021;48:1200–10. https://doi.org/10.1007/s00259-020-05040-1.
Grubmüller B, Senn D, Kramer G, Baltzer P, D’Andrea D, Grubmüller KH, et al. Response assessment using 68Ga-PSMA ligand PET in patients undergoing 177Lu-PSMA radioligand therapy for metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2019;46:1063–72. https://doi.org/10.1007/s00259-018-4236-4.
Moradi F, Duan H, Song H, Davidzon GA, Chung BI, Thong AEC, et al. 68Ga-PSMA-11 PET/MRI in patients with newly diagnosed intermediate or high-risk prostate adenocarcinoma: PET findings correlate with outcomes after definitive treatment. J Nucl Med Off Publ Soc Nucl Med. 2022. https://doi.org/10.2967/jnumed.122.263897.
Roberts MJ, Morton A, Donato P, Kyle S, Pattison DA, Thomas P, et al. 68Ga-PSMA PET/CT tumour intensity pre-operatively predicts adverse pathological outcomes and progression-free survival in localised prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48:477–82. https://doi.org/10.1007/s00259-020-04944-2.
Rogasch JM, Cash H, Zschaeck S, Elezkurtaj S, Brenner W, Hamm B, et al. Ga-68-PSMA PET/CT in treatment-naïve patients with prostate cancer: Which clinical parameters and risk stratification systems best predict PSMA-positive metastases? Prostate. 2018. https://doi.org/10.1002/pros.23685.
Zschaeck S, Andela SB, Amthauer H, Furth C, Rogasch JM, Beck M, et al. Correlation between quantitative PSMA PET parameters and clinical risk factors in non-metastatic primary prostate cancer patients. Front Oncol. 2022;12: 879089. https://doi.org/10.3389/fonc.2022.879089.
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, et al. The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol. 2016;40:244–52. https://doi.org/10.1097/PAS.0000000000000530.
Roach M, Hanks G, Thames H, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65:965–74. https://doi.org/10.1016/j.ijrobp.2006.04.029.
Cookson MS, Aus G, Burnett AL, Canby-Hagino ED, D’Amico AV, Dmochowski RR, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol. 2007;177:540–5. https://doi.org/10.1016/j.juro.2006.10.097.
Apostolova I, Steffen IG, Wedel F, Lougovski A, Marnitz S, Derlin T, et al. Asphericity of pretherapeutic tumour FDG uptake provides independent prognostic value in head-and-neck cancer. Eur Radiol. 2014;24:2077–87. https://doi.org/10.1007/s00330-014-3269-8.
Hofheinz F, Lougovski A, Zöphel K, Hentschel M, Steffen IG, Apostolova I, et al. Increased evidence for the prognostic value of primary tumor asphericity in pretherapeutic FDG PET for risk stratification in patients with head and neck cancer. Eur J Nucl Med Mol Imaging. 2015;42:429–37. https://doi.org/10.1007/s00259-014-2953-x.
R Core Team. R: A Language and Environment for Statistical Computing. R Found Stat Comput (2013).
Roberts MJ, Morton A, Papa N, Franklin A, Raveenthiran S, Yaxley WJ, et al. Primary tumour PSMA intensity is an independent prognostic biomarker for biochemical recurrence-free survival following radical prostatectomy. Eur J Nucl Med Mol Imaging. 2022. https://doi.org/10.1007/s00259-022-05756-2.
Marinescu IM, Rogg M, Spohn S, von Büren M, Kamps M, Jilg CA, et al. Ex vivo γH2AX assay for tumor radiosensitivity in primary prostate cancer patients and correlation with clinical parameters. Radiat Oncol Lond Engl. 2022;17:163. https://doi.org/10.1186/s13014-022-02131-1.
Calderoni L, Maietti E, Farolfi A, Mei R, Louie KS, Groaning M, et al. Prostate-specific membrane antigen expression on positron emission tomography/computed tomography in patients with metastatic castration-resistant prostate cancer: a retrospective observational study. J Nucl Med Off Publ Soc Nucl Med. 2023. https://doi.org/10.2967/jnumed.122.264964.
Seifert R, Kessel K, Schlack K, Weckesser M, Kersting D, Seitzer KE, et al. Total tumor volume reduction and low PSMA expression in patients receiving Lu-PSMA therapy. Theranostics. 2021;11:8143–51. https://doi.org/10.7150/thno.60222.
Hotta M, Gafita A, Murthy V, Benz MR, Sonni I, Burger IA, et al. PSMA PET tumor-to-salivary gland ratio to predict response to [177Lu]PSMA radioligand therapy: an international multicenter retrospective study. J Nucl Med Off Publ Soc Nucl Med. 2023. https://doi.org/10.2967/jnumed.122.265242.
Kupelian PA, Buchsbaum JC, Patel C, Elshaikh M, Reddy CA, Zippe C, et al. Impact of biochemical failure on overall survival after radiation therapy for localized prostate cancer in the PSA era. Int J Radiat Oncol Biol Phys. 2002;52:704–11. https://doi.org/10.1016/s0360-3016(01)02778-x.
Abramowitz MC, Li T, Buyyounouski MK, Ross E, Uzzo RG, Pollack A, et al. The Phoenix definition of biochemical failure predicts for overall survival in patients with prostate cancer. Cancer. 2008;112:55–60. https://doi.org/10.1002/cncr.23139.
Roy S, Romero T, Michalski JM, Feng FY, Efstathiou JA, Lawton CAF, et al. Biochemical recurrence surrogacy for clinical outcomes after radiotherapy for adenocarcinoma of the prostate. J Clin Oncol Off J Am Soc Clin Oncol. 2023;41:5005–14. https://doi.org/10.1200/JCO.23.00617.
Falagario UG, Abbadi A, Remmers S, Björnebo L, Bogdanovic D, Martini A, et al. Biochemical recurrence and risk of mortality following radiotherapy or radical prostatectomy. JAMA Netw Open. 2023;6: e2332900. https://doi.org/10.1001/jamanetworkopen.2023.32900.
Qiu X, Chen M, Yin H, Zhang Q, Li H, Guo S, et al. Prediction of biochemical recurrence after radical prostatectomy based on preoperative 68Ga-PSMA-11 PET/CT. Front Oncol. 2021;11: 745530. https://doi.org/10.3389/fonc.2021.745530.
Wang H, Amiel T, Würnschimmel C, Langbein T, Steiger K, Rauscher I, et al. PSMA-ligand uptake can serve as a novel biomarker in primary prostate cancer to predict outcome after radical prostatectomy. EJNMMI Res. 2021;11:76. https://doi.org/10.1186/s13550-021-00818-2.
Bodar YJL, Veerman H, Meijer D, de Bie K, van Leeuwen PJ, Donswijk ML, et al. Standardised uptake values as determined on prostate-specific membrane antigen positron emission tomography/computed tomography is associated with oncological outcomes in patients with prostate cancer. BJU Int. 2022;129:768–76. https://doi.org/10.1111/bju.15710.
Quak E, Le Roux P-Y, Hofman MS, Robin P, Bourhis D, Callahan J, et al. Harmonizing FDG PET quantification while maintaining optimal lesion detection: prospective multicentre validation in 517 oncology patients. Eur J Nucl Med Mol Imaging. 2015;42:2072–82. https://doi.org/10.1007/s00259-015-3128-0.
Kaalep A, Burggraaff CN, Pieplenbosch S, Verwer EE, Sera T, Zijlstra J, et al. Quantitative implications of the updated EARL 2019 PET-CT performance standards. EJNMMI Phys. 2019;6:28. https://doi.org/10.1186/s40658-019-0257-8.
Houdu B, Lasnon C, Licaj I, Thomas G, Do P, Guizard A-V, et al. Why harmonization is needed when using FDG PET/CT as a prognosticator: demonstration with EARL-compliant SUV as an independent prognostic factor in lung cancer. Eur J Nucl Med Mol Imaging. 2019;46:421–8. https://doi.org/10.1007/s00259-018-4151-8.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. There was no specific funding for this project.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: S.Z., S.B.A; Drafting of the manuscript: S.B.A., S.Z., and F.H.; Image editing and statistical analysis: F.H., S.B.A; Study Investigators: S.Z., S.B.A., F.H., H.A., C.F., J.R., M.B., F.M., P.G., J.VDH, T.K., R.T., D.Z.; Interpretation of the data: all authors; All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies with human participants were conducted in accordance with the Declaration of Helsinki and were reviewed and approved by the Ethics Committee of Charité Universitätsmedizin Berlin, Germany (EA4/168/16). All patients provided written informed consent to evaluate their data for research purpose, a specific consent for this analysis was waived by the Ethical committee.
Consent for publication
Not applicable.
Competing interests
Holger Amthauer declares research grants, travel grants, and lecture fees from Sirtex Medical Europe; Dr. Amthauer confirms that none of the above funding sources were involved in the preparation of this paper. All other authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bela Andela, S., Amthauer, H., Furth, C. et al. Quantitative PSMA-PET parameters in localized prostate cancer: prognostic and potential predictive value. Radiat Oncol 19, 97 (2024). https://doi.org/10.1186/s13014-024-02483-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-024-02483-w