Abstract
Background
With advances in understanding liver tolerance, conformal techniques, image guidance, and motion management, dose-escalated radiotherapy has become a potential treatment for inoperable hepatocellular carcinoma (HCC). We aimed to evaluate the possible impact of biologically effective dose (BED) on local control and toxicity among patients with HCC.
Methods and materials
Patients treated at our institution from 2009 to 2018 were included in this retrospective analysis if they received definitive-intent radiotherapy with a nominal BED of at least 60 Gy. Patients were stratified into small and large tumors using a cutoff of 5 cm, based on our clinical practice. Toxicity was assessed using ALBI scores and rates of clinical liver function deterioration.
Results
One hundred and twenty-eight patients were included, with a mean follow-up of 16 months. The majority of patients (90.5%) had a good performance status (ECOG 0–1), with Child-Pugh A (66.4%) and ALBI Grade 2 liver function at baseline (55.4%). Twenty (15.6%) patients had a local recurrence in the irradiated field during the follow-up period. Univariate and multivariate Cox proportional hazard analyses showed that only BED significantly predicted local tumor recurrence. Higher BED was associated with improved local control in tumors with equivalent diameters over 5 cm but not in smaller tumors. There was no difference in liver toxicity between the low and high-dose groups.
Conclusions
Higher radiotherapy dose is associated with improved local control in large tumors but not in tumors smaller than 5 cm in diameter. High-dose radiotherapy was not associated with increased liver toxicity.
Similar content being viewed by others
Background
The evolution of conformal radiotherapy techniques brought enthusiasm for dose escalation to improve oncologic outcomes. Liver neoplasms, once a challenging disease site for external beam radiotherapy, have represented a promising test case of dose escalation in this new therapeutic era. With HCC as the fourth-leading cause of cancer death worldwide and its incidence rising, questions related to the efficacy of therapy are increasingly critical [1].
External beam radiotherapy for HCC is typically reserved for patients with advanced HCC who are poor candidates for a liver transplant or partial hepatectomy [2]. Radiation oncologists now utilize highly modulated beams and image guidance to deliver high-dose radiation to liver tumors with moderate- or ultra-hypofractionation. Treating with higher doses could be especially important in larger tumors, which are more prone to local recurrence after radiation [3, 4]. However, the optimal dose of radiotherapy remains controversial. Some studies have shown that treating HCC with high BED improves outcomes [5,6,7,8,9], while others found no association between a higher BED and better local control [10, 11]. This question is critical in the context of the well-documented risk of subjecting large volumes of liver parenchyma to high-radiation doses, especially when treating large tumors [11, 12]. Acknowledging the uncertainty regarding dose response, the recently published American Society for Radiation Oncology (ASTRO) recommendations for liver cancer encompass a wide range of dose- fractionation regimens, taking into account tumor size and patient’s liver function [13].
At our institution, HCC lesions with a diameter less than or equal to 5 cm are typically treated with five-fraction stereotactic body radiotherapy (SBRT) to a BED10 of 100 Gy. This has been driven by the established high rate of local control and low toxicity of SBRT in this population [14]. Tumors with a larger diameter are treated with a more fractionated regimen, sometimes compromising on the radiation dose to meet normal tissue constraints. This heterogeneity in dose and fractionation schedules creates an opportunity to investigate the dose-response relationship of radiotherapy for local control and liver toxicity in small and large HCC tumors treated at our department. We hypothesized that higher radiotherapy doses would be associated with improved local control and similar toxicity compared to lower doses.
Methods
Data source and patient cohort
Patients with non-metastatic HCC treated at the University of Pennsylvania with radiotherapy between 2009 and 2018 were identified from ARIA patient information system (Varian Medical Systems, Palo Alto, CA). Clinical data were extracted from the hospital’s Epic electronic medical record (Epic Systems Corporation, Verona, WI) following approval of the institutional review board. Patients treated with any fractionation were included as long as the target received a BED10 dose of at least 60 Gy. BED was calculated based on the prescribed dose per fraction, the number of fractions delivered, and a presumed α/β = 10 in accordance with the recently published ASTRO clinical practice guidelines for liver cancer [13] and as mostly done by previous investigators [4, 15,16,17,18]. However, Given some uncertainty in the true α/β ratio, we repeated the analysis with BEDs calculated with α/β = 7 and α/β = 3. A BED10 threshold of 60 Gy was chosen as it equals an equivalent dose in 2 Gy fractions (EQD2) of 50 Gy, which, based on our institutional practice, would exclude patients treated with palliative intent (as opposed to definitive therapy for durable control). Of note, patients at our institution with Child-Pugh B 8–9 or C liver disease routinely undergo a treatment break to identify those who develop early radiation-induced liver function decline. The initial course of radiotherapy in these split course regimens is at least 60 Gy BED10.
Outcome variables
The primary outcome in this study was local recurrence, defined as the progression of the tumor in the irradiated field. Local recurrences were diagnosed based on follow-up imaging — most commonly dynamic contrast-enhanced MRI performed routinely every three months under the National Comprehensive Cancer Network (NCCN) guidelines [19]. Follow-up time was calculated from the end of the radiotherapy course. Patients without recurrence or death were censored at the last follow-up. Patients were divided into low BED10 and high BED10 groups with a cutoff at the median BED10.
ALBI score, an objective prognostic measure of liver function developed and externally validated in large international cohorts of patients with HCC, was calculated based on albumin and bilirubin values [20, 21]. Toxicity endpoints were the maximum ALBI index in the four months following the initiation of radiotherapy and clinical liver function deterioration at four months and one year following the initiation of radiotherapy. Toxicity was defined based on the radiation start date as treatment courses in our sample ranged from 3 to 33 fractions. Clinical liver function deterioration was defined as new or increased ascites, bleeding due to coagulopathy, hepatic encephalopathy, hepatic hydrothorax, or variceal hemorrhage, and was determined from the electronic health record (EHR). Covariates, including age, sex, vascular invasion, ECOG performance status, baseline Child-Pugh group, and history of prior local therapy, were also obtained from the EHR. Baseline ALBI was defined as the mean ALBI score over the six weeks preceding the start of radiotherapy. Radiotherapy treatment data were obtained from the ARIA. Gross tumor volume (GTV) was measured using the treatment planning system and converted to equivalent sphere diameter based on the sphere volume formula V = 4πR3/3.
Statistical methods
Variables were compared using a two-tailed Student’s T-test for continuous variables and Chi-square for categorical variables. To identify parameters associated with local recurrence following radiation therapy, a univariate and multivariate Cox proportional hazard analysis was performed. Local recurrence-free survival and overall survival were calculated using the Kaplan-Meier method. Survival outcome differences were evaluated using the log-rank test [22]. A propensity score-matched analysis with a 1:1 ratio and a caliper of 0.2 was conducted to balance the baseline characteristics between high and low-BED groups in order to minimize their effect on the oncologic outcome. A logistic regression model was used to calculate the propensity score, which included the following variables: Child-Pugh score and Treatment modality (photon vs. proton radiation therapy). Statistical analysis was performed using SPSS version 28 (SPSS, Inc., Chicago, Illinois, USA) and R version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria). For all calculations, P values < 0.05 were considered statistically significant.
Results
Patient characteristics and radiation treatment
The analytic cohort included one hundred twenty-eight patients (Table 1). A majority were male, in good performance status, with Child-Pugh A and ALBI Grade 2 baseline liver function, and had received prior local therapy. A third of the patients underwent SBRT. A minority of patients underwent a planned treatment break, with the vast majority completing the planned treatment course. The median BED10 was 78 Gy. The median follow-up time for the cohort was 16 months (484 days).
Treatment outcome and predictors of local recurrence for the entire cohort
Of the 128 patients included in the study, 20 (15.6%) had a local recurrence in the irradiated field, and 71 (55.5%) died during the follow-up period. In patients with a local recurrence, the median time to recurrence was 197 days. Table 2 shows the results of a univariate and multivariate Cox proportional hazard analysis using the patient’s age, gender, ECOG performance status, Child-Pugh Group, ALBI grade, history of prior local therapy, vascular invasion, planned treatment break, proton radiation, GTV diameter, and BED10. Only BED10 over the median dose significantly predicted local recurrence-free survival. We next performed a multivariate Cox proportional hazard analysis for local recurrence-free survival. We included BED10 and GTV diameter, given previous studies demonstrating an association between tumor size and treatment outcomes in HCC [23, 24]. In our analysis, only BED10 was a significant predictor of local recurrence after radiation, with a hazard ratio of 0.324. No significant differences in the occurrence of local failure were noted between tumors with a diameter over and under 5 cm.
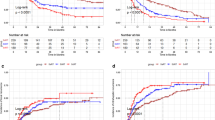
Impact of the radiation dose on local control in large and small tumors
Patients with small tumors (< 5 cm equivalent sphere diameter) had comparable mean age, Child-Pugh Group, and ECOG performance status compared to patients with large tumors (Table 3). Compared to patients with large tumors, patients with smaller tumors received significantly more ultrahypofractionated radiation regimens, higher BED, and fewer treated with proton therapy. There was no difference in local recurrence-free survival between patients with small and large tumors (Supplementary Fig. 1A); however, patients with large tumors had shorter overall survival (Supplementary Fig. 1B). We further explored the potential impact of radiation dose on local recurrence in small and large tumors. In tumors with a diameter under 5 cm, treating with a radiation dose higher than the median BED10 (78 Gy) did not result in improved local recurrence-free survival compared to a lower dose (Fig. 1A). However, in tumors with a diameter over 5 cm, treating with a higher than median BED10 significantly improved the local recurrence-free survival (Fig. 1B). Supplementary Fig. 2 shows the HR of each 10 Gy increase in BED10 as a function of tumor size. The plot shows that the impact of the 10 Gy increment in BED10 increased at a non-linear rate, with gradual improvement in the HR at a cutoff of 1.7 cm, with a steep benefit in tumors over 5 cm in diameter.
The results of our analyses using an α/β of 7 and 3 to calculate the BED are presented in Supplementary Tables 1, 2, and 3 and Supplementary Fig. 3A, 3B, 4A, 4B, 5A, and 5B. There were no differences compared to our primary analyses using an α/β of 10. In addition, we performed a propensity score matching based on the covariates: Child-Pugh Score and treatment modality (proton vs. photon). As can be seen in Supplementary Tables 4, the propensity-matched cohort in the low-BED group was evenly matched with the high-BED cohort in terms of baseline liver function and treatment modality. After propensity-matching, there was no difference in survival between the high and low-BED-treated groups, but the improved local recurrence-free survival after high-BED radiation treatment persisted (Supplementary Figs. 6, 7). Subgroup analysis reaffirmed that high BED-radiation treatment improves local control in tumors with a diameter over 5 cm but not smaller tumors (Supplementary Fig. 8A, B).
Effects of radiation dose on liver toxicity
Table 4 compares liver toxicity at different time points, as a function of the BED10, in the entire cohort and patients with small and large tumors. Comparing patients treated with high vs. low BED10, there were no significant differences in liver function before radiation, four months after, and one year after completion of therapy in the entire cohort and the sub-group of patients with tumors < 5 cm. In the subset of patients with larger tumors, patients with the worst ALBI score at baseline received a lower radiation dose. However, when comparing high vs. low BED10, there was no difference in the mean maximum ALBI score and liver decompensation at four months and one year after radiation. Our institution’s constraints for the organs at risk for a fractionated regimen (7000 cGy in 20 fractions) and SBRT (5000 cGy in 5 fractions) are provided in Supplementary Table 5A, B.
Discussion
Our study explored the dose-response relationship of radiotherapy for local control and liver toxicity in small and large HCC tumors treated at our department. We found that only the radiation BED was a significant factor for predicting local tumor control following radiation therapy. Higher BED and improved local control were significant for tumors over 1.7 cm and paramount for patients with tumors over 5 cm equivalent sphere diameter. Patients with small tumors did not seem to benefit from dose escalation. In addition, we observed similar liver toxicity among patients treated with high vs. low dose radiotherapy, as measured by ALBI and clinical liver function deterioration. Therefore, patients with non-metastatic HCC tumors over 5 cm in diameter may benefit from escalated doses of radiotherapy without increasing the risk of liver toxicity. At the same time, in small tumors, the local control was excellent, even if a high BED could not be achieved.
Historically, radiotherapy was considered ill-suited to treating liver tumors because of the organ’s limited radiotolerance [25]. With the advent of conformal therapy, image guidance, and motion management techniques, radiotherapy was incorporated into the American Association for the Study of Liver Disease’s national guidelines as a potential treatment for inoperable HCC [2]. The optimal dose and fractionation of radiotherapy remain a matter of debate, and prior studies are heterogeneous in their patient populations, study designs, and analytic approaches, precluding a clear conclusion. Our study’s association between high-BED radiotherapy and tumor control depends on the GTV diameter. Previous studies of Korean and American patients showed improved outcomes with higher radiotherapy BED, including objective response rate, local recurrence, progression-free survival, and overall survival [5,6,7,8,9]. However, other non-randomized studies found no association between higher BED doses and improved outcomes [10, 11]. These contradictory findings may be due to the non-linear relationship between GTV size and the improved local control in higher BED radiation. Our results suggest that an equivalent sphere diameter of around 5 cm is a critical threshold at which the relative impact of BED increases substantially as GTV volume rises.
An important clinical question is how to deliver higher radiation doses safely without an increase in liver toxicity. Prior work using older, less conformal radiotherapy techniques showed more significant toxicity with higher doses of radiotherapy. Some groups have delivered escalated doses based on Normal Tissue Complication Probability models [26,27,28]. To avoid liver toxicity, at our institution, we prescribe a split-course regimen for patients with a Child-Pugh score greater than 7. Treatment is discontinued in patients who show early liver toxicity at one-month follow-up [29]. Additionally, we use more conservative mean liver dose constraints for patients with worse liver function: 28 Gy for Child-Pugh A 5–6 to 24 Gy for Child-Pugh B > 7. Reassuringly, we did not observe increased ALBI scores or clinical liver function deterioration in patients treated with higher doses of radiotherapy.
Our study is subject to potential limitations common to all retrospective analyses, primarily the existence of confounding factors. However, different from typical retrospective reviews, where heterogeneity of treatment might be a problem, herein, the heterogeneity of dose is an advantage in that it allows the observation of a dose response if one were to exist. We recognize that our median follow-up time may seem short. However, we would submit that the population we see in our clinic is advanced; in fact, 55% of patients have died within this follow-up interval. Hence, this is a mature series despite a relatively short follow-up time. We also recognize that avoidance of liver toxicity at higher radiation doses likely depends on an approach (involving split-course and differential liver constraints that varies with liver function) that is not widely practiced. In addition, although radiation-induced liver toxicity typically manifests shortly after radiation, commonly within three months [26, 30,31,32,33], there are a few reports of liver toxicity occurring later [30]. Given the natural history of cirrhosis, characterized by decompensation secondary to many various causes, the relationship to radiation is difficult to establish with any certainty after six months. Nevertheless, we recognize that a small number of late radiation-induced liver toxicities may have been missed, leading to a small underestimation of liver toxicity.
In conclusion, higher BED is associated with improved local control in patients with tumors larger than 5 cm in diameter. Patients treated with a higher dose do not appear to have a higher rate of liver toxicity. Hence, for these larger tumors, radiation oncologists should strive to deliver the highest possible dose that can be safely delivered, respecting organs-at-risk (OAR) tolerance. For tumors smaller than 5 cm in diameter, OAR tolerance should be prioritized, as compromising target coverage is not likely to result in a substantial loss of local control.
Data Availability
Please contact the author for data requests.
Data sharing: Data are not available for reuse.
Abbreviations
- ALBI:
-
Albumin-bilirubin prognostic score
- ASTRO:
-
American Society for Radiation Oncology
- BED:
-
Biologically effective dose
- ECOG:
-
Eastern Cooperative Oncology Group
- EHR:
-
Electronic health record.
- GTV:
-
Gross tumor volume
- HCC:
-
Hepatocellular carcinoma
- NCCN:
-
National Comprehensive Cancer Network
- OAR:
-
Organs-at-risk
References
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68:394–424.
Heimbach JK, Kulik LM, Finn RS, et al. Aasld guidelines for the treatment of hepatocellular carcinoma. Hepatology (Baltimore MD). 2018;67:358–80.
Jang WI, Kim M-S, Bae SH, et al. High-dose stereotactic body radiotherapy correlates increased local control and overall survival in patients with inoperable hepatocellular carcinoma. Radiat Oncol. 2013;8:1–12.
Sun J, Zhang T, Wang J, et al. Biologically effective dose (bed) of stereotactic body radiation therapy (sbrt) was an important factor of therapeutic efficacy in patients with hepatocellular carcinoma (≤ 5 cm). BMC Cancer. 2019;19:846.
Jang WI, Kim MS, Bae SH, et al. High-dose stereotactic body radiotherapy correlates increased local control and overall survival in patients with inoperable hepatocellular carcinoma. Radiation Oncol (London England). 2013;8:250.
Park HC, Seong J, Han KH, et al. Dose-response relationship in local radiotherapy for hepatocellular carcinoma. Int J Radiation Oncology*Biology*Physics. 2002;54:150–5.
Dawson LA, McGinn CJ, Normolle D, et al. Escalated focal liver radiation and concurrent hepatic artery fluorodeoxyuridine for unresectable intrahepatic malignancies. J Clin oncology: official J Am Soc Clin Oncol. 2000;18:2210–8.
Ben-Josef E, Normolle D, Ensminger WD, et al. Phase ii trial of high-dose conformal radiation therapy with concurrent hepatic artery floxuridine for unresectable intrahepatic malignancies. J Clin oncology: official J Am Soc Clin Oncol. 2005;23:8739–47.
Byun HK, Kim HJ, Im YR, et al. Dose escalation by intensity modulated radiotherapy in liver-directed concurrent chemoradiotherapy for locally advanced bclc stage c hepatocellular carcinoma. Radiotherapy and oncology: journal of the European Society for Therapeutic Radiology and Oncology. 2019;133:1–8.
Ohri N, Tomé WA, Méndez Romero A, et al. Local control after stereotactic body radiation therapy for liver tumors. Int J Radiat Oncol Biol Phys. 2021;110:188–95.
Bujold A, Massey CA, Kim JJ, et al. Sequential phase i and ii trials of stereotactic body radiotherapy for locally advanced hepatocellular carcinoma. J Clin oncology: official J Am Soc Clin Oncol. 2013;31:1631–9.
Lawrence TS, Robertson JM, Anscher MS, et al. Hepatic toxicity resulting from cancer treatment. Int J Radiat Oncol Biol Phys. 1995;31:1237–48.
Apisarnthanarax S, Barry A, Cao M, et al. External beam radiation therapy for primary liver cancers: an astro clinical practice guideline. Practical radiation oncology. 2022;12:28–51.
Baumann BC, Wei J, Plastaras JP, et al. Stereotactic body radiation therapy (sbrt) for hepatocellular carcinoma: high rates of local control with low toxicity. Am J Clin Oncol. 2018;41:1118–24.
van Leeuwen CM, Oei AL, Crezee J, et al. The alfa and beta of tumours: a review of parameters of the linear-quadratic model, derived from clinical radiotherapy studies. Radiat Oncol. 2018;13:96.
Cheung MLM, Kan MWK, Yeung VTY, et al. Analysis of hepatocellular carcinoma stereotactic body radiation therapy dose prescription method using uncomplicated tumor control probability model. Adv radiation Oncol. 2021;6:100739.
Su TS, Liu QH, Zhu XF, et al. Optimal stereotactic body radiotherapy dosage for hepatocellular carcinoma: a multicenter study. Radiation Oncol (London England). 2021;16:79.
Lee HL, Tsai JT, Chen CY, et al. Effectiveness of stereotactic ablative radiotherapy in patients with advanced hepatocellular carcinoma unsuitable for transarterial chemoembolization. Therapeutic Adv Med Oncol. 2019;11:1758835919889002.
Benson AB, D’Angelica MI, Abbott DE, et al. Hepatobiliary cancers, version 2.2021, nccn clinical practice guidelines in oncology. J Natl Compr Cancer Network: JNCCN. 2021;19:541–65.
Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the albi grade. J Clin oncology: official J Am Soc Clin Oncol. 2015;33:550–8.
Pinato DJ, Sharma R, Allara E, et al. The albi grade provides objective hepatic reserve estimation across each bclc stage of hepatocellular carcinoma. J Hepatol. 2017;66:338–46.
Goel MK, Khanna P, Kishore J. Understanding survival analysis: Kaplan-meier estimate. Int J Ayurveda Res. 2010;1:274–8.
Han Y, Liu J, Pan J, et al. Prognosis and risk factors of recurrence in hbv-related small hepatocellular carcinoma after stereotactic body radiation therapy. Front Oncol. 2022;12:903355.
Zhang W, Wang X, Jiang R et al. Effect of tumor size on cancer-specific survival in small hepatocellular carcinoma. Mayo Clinic proceedings 2015;90:1187-95.
Keane FK, Hong TS. Role and future directions of external beam radiotherapy for primary liver cancer. Cancer control: journal of the Moffitt Cancer Center. 2017;24:1073274817729242.
Pan CC, Kavanagh BD, Dawson LA, et al. Radiation-associated liver injury. Int J Radiat Oncol Biol Phys. 2010;76:94–100.
McGinn CJ, Ten Haken RK, Ensminger WD, et al. Treatment of intrahepatic cancers with radiation doses based on a normal tissue complication probability model. J Clin oncology: official J Am Soc Clin Oncol. 1998;16:2246–52.
Pursley J, El Naqa I, Sanford NN, et al. Dosimetric analysis and normal-tissue complication probability modeling of child-pugh score and albumin-bilirubin grade increase after hepatic irradiation. Int J Radiat Oncol Biol Phys. 2020;107:986–95.
Jackson WC, Suresh K, Maurino C, et al. A mid-treatment break and reassessment maintains tumor control and reduces toxicity in patients with hepatocellular carcinoma treated with stereotactic body radiation therapy. Radiotherapy and oncology: journal of the European Society for Therapeutic Radiology and Oncology. 2019;141:101–7.
Kim J, Jung Y. Radiation-induced liver disease: current understanding and future perspectives. Exp Mol Med. 2017;49:e359.
Yamasaki SA, Marn CS, Francis IR, et al. High-dose localized radiation therapy for treatment of hepatic malignant tumors: ct findings and their relation to radiation hepatitis. AJR Am J Roentgenol. 1995;165:79–84.
da Silveira EB, Jeffers L, Schiff ER. Diagnostic laparoscopy in radiation-induced liver disease. Gastrointest Endosc. 2002;55:432–4.
Guha C, Kavanagh BD. Hepatic radiation toxicity: avoidance and amelioration. Semin Radiat Oncol. 2011;21:256–63.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
UA, JM, and EBJ performed the study’s design and writing of the manuscript, UA and JH performed the statistical analysis, AW, GW, SM, NG, JP, and AD contributed to the acquisition of data, and the review of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of the University of Pennsylvania.
Consent for publication
Not applicable.
Competing interests
Dr. Metz reports consulting fees from Varian and IBA, outside of the submitted work. Dr. Plastaras reports consulting fees from IBA, outside of the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amit, U., Mohiuddin, J.J., Wojcieszynski, A.P. et al. Radiation dose is associated with improved local control for large, but not small, hepatocellular carcinomas. Radiat Oncol 18, 133 (2023). https://doi.org/10.1186/s13014-023-02318-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-023-02318-0