Abstract
Background
Soft tissue sarcomas (STS) represent a diverse group of rare malignant tumors. Currently, five to six weeks of preoperative radiotherapy (RT) combined with surgery constitute the mainstay of therapy for localized high-grade sarcomas (G2–G3). Growing evidence suggests that shortening preoperative RT courses by hypofractionation neither increases toxicity rates nor impairs oncological outcomes. Instead, shortening RT courses may improve therapy adherence, raise cost-effectiveness, and provide more treatment opportunities for a wider range of patients. Presumed higher rates of adverse effects and worse outcomes are concerns about hypofractionated RT (HFRT) for STS. This systematic review summarizes the current evidence on preoperative HFRT for the treatment of STS and discusses toxicity and oncological outcomes compared to normofractionated RT.
Methods
We conducted a systematic review of clinical trials describing outcomes for preoperative HFRT in the management of STS using PubMed, the Cochrane library, the Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, Embase, and Ovid Medline. We followed the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Trials on retroperitoneal sarcomas, postoperative RT, and hyperthermia were excluded. Articles published until November 30th, 2021, were included.
Results
Initial search yielded 94 articles. After removal of duplicate and ineligible articles, 13 articles qualified for analysis. Eight phase II trials and five retrospective analyses were reviewed. Most trials applied 5 × 5 Gy preoperatively in patients with high-grade STS. HFRT courses did not show increased rates of adverse events compared to historical trials of normofractionated RT. Toxicity rates were mostly comparable or lower than in trials of normofractionated RT. Moreover, HFRT achieved comparable local control rates with shorter duration of therapy. Currently, more than 15 prospective studies on HFRT + / − chemotherapy are ongoing.
Conclusions
Retrospective data and phase II trials suggest preoperative HFRT to be a reasonable treatment modality for STS. Oncological outcomes and toxicity profiles were favorable. To date, our knowledge is mostly derived from phase II data. No randomized phase III trial comparing normofractionated and HFRT in STS has been published yet. Multiple ongoing phase II trials applying HFRT to investigate acute and late toxicity will hopefully bring forth valuable findings.
Similar content being viewed by others
Introduction
Soft tissue sarcomas (STS) are a heterogenous group of malignant tumors arising from mesenchymal tissue in virtually all anatomic locations and age groups [1, 2]. STS account for less than 1% of all tumor entities in adults and 7% in pediatric patients [3, 4]. The estimated incidence rate in Europe is 4–5 per 100 000 per year [5]. The World Health Organization applies two standard histopathological grading systems for STS based on histological, morphological and molecular characteristics [6,7,8]. This review will analyze data on adult patients with STS of the extremities and trunk and exclude retroperitoneal STS and trials on hyperthermia, which are discussed elsewhere [9, 10].
Owing to STS heterogeneity, the disease-associated morbidity and mortality are highly variable. Positive surgical margins, recurrent disease at presentation, histological grade, tumor depth, and previous local recurrences (LR) are independent risk factors for subsequent recurrences and mortality [11,12,13,14]. Moreover, specific histological subtypes, e.g., malignant peripheral nerve sheath tumors or myxofibrosarcomas, are associated with unfavorable clinical outcomes [11, 12, 15, 16]. In high-grade STS (G2-G3), current standard of care comprises surgery combined with preoperative conventionally fractionated RT, preferably carried out in sarcoma reference centers [17,18,19]. Preoperative (neoadjuvant) conventionally fractionated RT is applied over five to six weeks in daily fractions of 1.8–2.0 Gy to a total dose of 50–50.4 Gy [18, 20]. The role of perioperative chemotherapy remains controversial and depends on the above-mentioned risk factors [21]. Although preoperative RT causes higher wound complication rates, postoperative RT leads to irreversible fibrosis-related toxicities adversely affecting patients’ function. This has caused an increasing notion of preferring pre- over postoperative RT among radiation oncologists [22,23,24,25,26].
In daily practice, single doses higher than 2.2 Gy are usually considered as hypofractionated radiotherapy (HFRT), although no exact definition exists. It has been hypothesized that increasing radiation doses per fraction would raise the toxicity rate in normal tissue [27, 28]. Therefore, HFRT was mainly applied in palliative settings where fast symptom relief (e.g., pain relief in bone metastases) and lower total doses than in definitive RT settings are required. However, within the last two decades, further evidence on the efficacy and safety of hypofractionated therapy regimens has come from RT trials of breast cancer, prostate cancer, and rectal cancer, where hypofractionation is now routinely applied [29,30,31].
When comparing outcomes of different clinical trials, it is essential to bear in mind that over the last decades, RT has been—and is to this date—subject to tremendous technological advances. Technical innovation in all sections of radiation oncology (imaging, treatment planning, linear accelerators) have remarkably improved radiation precision and tolerability [32,33,34]. In line with this, a more recent trial applying modern radiation techniques and image guidance has shed new light on RT in STS: By using advanced and more precise radiation techniques, the investigators were able to reduce toxicity rates in preoperative, normofractionated RT for STS (10.5% of at least one grade ≥ 2 toxicity at two years vs. 35% in the SR-2 trial) [35].
Another rationale in favor of hypofractionation is based on radiobiological observations in STS. STS like liposarcomas and rhabdomyosarcomas are likely to have lower α/β ratios (< 10), making them rather sensitive to larger fraction sizes [36,37,38]. Rather interestingly, other tumor entities with similar α/β ratios of less than 10 (e.g., breast and rectal cancer) have shown similar local control (LC) rates after HFRT as compared to conventionally fractionated RT [39, 40].
Supporters of HFRT also argue with practical advantages of this therapy regimen. The treatment of STS at specialized, multidisciplinary sarcoma centers has shown beneficial outcomes for patients and improves overall survival (OS) [19, 41,42,43]. By shortening RT courses through hypofractionation without compromising patient outcomes, access to high-volume sarcoma centers can be particularly improved for immobile, frail, and elderly patients [44]. Shortening RT regimens is not only preferred by patients; it also reduces the economic burden on the health care system while increasing patient throughput at high-volume centers [45,46,47,48,49]. Especially during the COVID-19 pandemic, when medical care is less widely available, and patient contact is aimed to be reduced to a minimum, hypofractionation may constitute a preferred treatment modality [50].
To the best of our knowledge, no review has systematically analyzed the literature on preoperative HFRT regimens for STS treatment. To address this topic and give deeper insights into the advantages and drawbacks of hypofractionation, we conducted a systematic review of the literature to assess patient outcome parameters, toxicity rates, and feasibility. The current evidence and findings for preoperative HFRT in the treatment of STS in adults are summarized herein.
Materials and methods
A systematic review of the literature was performed in accordance to the guidelines of the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA, PRISMA 2020 study protocol checklist, Additional file 1: The PRISMA 2020 checklist, supplementary materials) [51]. The databases PubMed, ClinicalTrials.gov, the Cochrane library and the Cochrane Central Register of Controlled Trials, Embase, and Ovid Medline were used. Variably combined search items included “hypofractionation”, “soft tissue sarcoma”, “radiotherapy”, “trunk and extremity sarcoma”, “neoadjuvant radiotherapy”, “oncological outcomes”, “wound complication”, “toxicity”, “safety”, “feasibility” and “efficacy”. For ongoing clinical trials, the ClinicalTrials.gov webpage was used with the following search items: “soft tissue sarcoma”, “hypofractionated radiotherapy” and “radiotherapy”. Databases were searched on November 30th, 2021 (Table 1). No filters or limits were applied. All English studies published before November 30th, 2021, were included. The first reviewer (S.R.) excluded duplicates, trials on hyperthermia or postoperative RT (trials adding postoperative boost to preoperative RT were not excluded), trials not matching the search items and trials on retroperitoneal sarcomas (due to their profound differences regarding the clinical course, treatment, and histological subtypes). The following types of articles were included: randomized controlled trials, open-label trials, retrospective analyses, phase II and III clinical trials, as well as single and multicenter trials applying preoperative HFRT on adults (≥ 18 years) with STS. This review was not registered.
Data items
The data items extracted from all eligible studies were author list, publication date, number of patients, patient demographics, histological subtypes of STS, anatomical locations, median tumor size, dose per fraction, number of fractions, time from RT to surgery and from surgery to RT, chemotherapy regimens, median follow-up, overall survival, local control, local recurrence, local recurrence-free survival (LRFS), progression-free survival (PFS), disease-free survival (DFS), wound complication (WC)- and late toxicity rates. If an article lacked any data on the aforementioned items, the specific field was left blank in the summary table resulting in lower validity and comparability of the respective trial. After initial selection of data items by the first reviewer (S.R.), the second reviewer (D.K.) checked for suitability and accuracy.
Quality control and assessment
To ensure adequate quality standards for included articles, both the titles, abstracts, and full texts were thoroughly examined by the first reviewer. All resources obtained online were saved as PDF files in case the online record was edited or removed. Risk of bias was assessed individually for every study by using the Risk of Bias In Non-randomized Studies of Interventions tool (ROBINS-I) developed by the Cochrane Bias Methods Group [52] (Additional file 2: Risk of bias assessment according to ROBINS-I, Table 1). After initial evaluation by the first reviewer, the second reviewer then critically edited the bias assessment, list of results, data and added further articles, if required. In cases of uncertainty, the third reviewer (F.E.) gave critical input.
Results
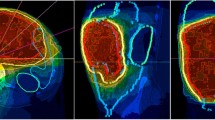
The PRISMA flow diagram depicted in Fig. 1 shows all initial search results, excluded articles and the final number of articles meeting the inclusion criteria. Systemically reviewed studies on preoperative hypofractionated radiotherapy are summarized in Table 2; major studies on conventionally fractionated radiotherapy are summarized in Table 3.
Flow diagram for study selection according to the PRISMA 2020 guidelines [51]
Discussion
Herein, we review the current literature on preoperative HFRT in the management of STS. The most frequently voiced criticism of this treatment approach concerns the following points: (i) the possibilty of increased toxicity with pre- and postoperative complications; (ii) assumed worse oncological outcomes compared to standard fractionated RT; (iii) financial concerns due to the reduced number of therapy sessions in HFRT [72, 73]. From a logistical and health economic standpoint, HFRT is undoubtedly the preferred and better applicable treatment modality for all patients and age groups seeking care at sarcoma centers [41, 42, 44]. Regional hyperthermia has historically been used in combination with chemotherapy showing promising results for the treatment of STS [74,75,76,77,78]. Combined with neoadjuvant chemotherapy, regional hyperthermia improves OS and local progression-free survival for patients with localized high-grade STS [79, 80]. As part of a first study, hypofractionated radiotherapy was combined with hyperthermia on 30 patients with marginally or unresectable, mostly G1 STS. This phase II feasibility study from the Warsaw sarcoma center by Spałek et al. met its primary endpoint of testing feasibility as it was well tolerated and adherence to the therapy protocol was successful [81]. Due to the scope of the present review to describe and compare preoperative HFRT to current standard treatment (normo-fractionated RT), trials on regional hyperthermia were not included.
Acute and late toxicity
The first and foremost concern about increased early and late toxicity with HFRT cannot be confirmed based on the available data. Firstly, to define major WCs, most trials adopted their definition from the largest phase III trial (SR-2 trial) that compared toxicity rates in pre- vs. postoperative normofractionated RT. In this trial, a major WC was defined as a second surgery under general or regional anesthesia for wound repair up to four months after primary surgery. Additionally, aspiration of seromas, re-admission for wound care such as intravenous antibiotics or persistent deep packing for 120 days or beyond were included in that definition [26]. Preoperative RT was associated with a WC rate of 35%, while 17% of participants showed postoperative WCs (Table 3) [26].
In a 2021 published, non-controlled, interventional trial by Koseła-Paterczyk et al., 311 patients treated with a short preoperative course of 5 × 5 Gy showed lower WC rates of 28% compared to the SR-2 trial [53]. The average tumor size was even larger while the histological grade, tumor location, and median age of participants were comparable. Treatment planning was also similar in both trials: In the trial by Koseła-Paterczyk et al. the clinical target volume (CTV) was 2 cm transversally and 4 cm longitudinally. The planning target volume (PTV) was 1 cm in all directions (Table 2). In the SR-2 trial, preoperative RT treatment consisted of 25 × 2 Gy to a volume of 5 cm proximal and distal to the tissue at risk displayed on computed tomography (CT). A minor subgroup of patients with positive surgical margins after preoperative RT received a sequential boost (16–20 Gy in 2 Gy fractions) defined as lesion volume plus 2 cm in all directions.
Possible explanations for the difference in WC rates between both trials may be: (i) Increased precision by image-guided radiotherapy (IGRT) conducted via daily cone-beam CTs in the trial by Koseła-Paterczyk et al.; (ii) the use of contrast enhanced magnetic resonance imaging (MRI) fused with CT for planning, although the exact proportion of patients where MRI was applied is not given; (iii) a possible difference in the tumor depth as another risk factor for WC, also not given in the trial by Koseła-Paterczyk et al.; (iv) a difference in patients comorbidities (e.g. increased body mass index (BMI), smoking, diabetes) adversely affecting wound complication rates [82,83,84,85].
One essential limitation of the 2021 trial of Koseła-Paterczyk et al. is the absence of intensity modulated radiotherapy (IMRT) technique. It would have been interesting to observe whether adding IMRT techniques to the hypofractionated 5 × 5 Gy regimen would have reduced toxicity rates even more. In 2014, Koseła-Paterczyk et al. had applied HFRT to a comparable group of 272 patients (mostly G3 sarcomas located in the lower extremity), but without IMRT or IGRT. Herein, major WC rates were higher and similar to the rates in the SR-2 trial (32.4% vs. 35% in the SR-2), while late toxicities were less common, suggesting IMRT and IGRT as important influence parameters [64].
For normofractionated RT, more data exists suggesting a clear benefit of image-guided and intensity modulated radiotherapy (IG-IMRT) techniques. The group of O'Sullivan et al. published another trial showing beneficial toxicity rates by using IG-IMRT and standard target volume delineations [67]. Although the rate of WCs was numerically lower, yet not statistically significant, the need for tissue transfer was significantly reduced [67]. Supporting this approach, Wang et al. investigated the impact of normofractionated IGRT on toxicity rates in preoperative normofractionated RT for STS applying the same definitions for late toxicity and acute WCs as in the SR-2 trial [24, 26]. By adding IGRT, the late toxicity rate again dropped substantially to 10.5% in the RTOG-0630 trial [35].
Interestingly, two interventional trials evaluating stereotactic body radiotherapy (SBRT) used even higher doses of 5 × 8 and 5 × 7 Gy and revealed acute WC rates similar to conventional HFRT yet lower than in the normofractionated SR-2 trial (28% and 28.5% respectively) [55, 61]. Notable other adverse events were vascular occlusions described in a small proportion of patients after 5 × 8 Gy SBRT requiring disarticulation surgery (n = 3) and one case of amputation [55]. The amount of literature describing damage to tumor vasculature under intense hypofractionation has been growing recently [86, 87]. This effect has first been described in in vitro experiments after single fractions ≥ 10 Gy which may explain the described adverse effects [88]. Nevertheless, the SBRT data on STS are limited by the small number of participants (25 in the trial of Leite et al. vs. 13 in the trial of Kubicek et al.) and the short median follow-up of 9.3 months in the latter trial, which therefore could detect no late toxicities [55, 61]. Nevertheless, it is undoubted that advances in RT planning and techniques such as IGRT and IMRT have improved precision and reduced toxicity rates for STS patients. An upcoming Russian trial is currently recruiting patients for a 3-step sequence of preoperative stereotactic RT (5 × 5 Gy), surgery, and postoperative normofractionated RT (25 × 2 Gy). The primary endpoint is the complication rate after each step of the protocol [89](NCT04330456).
To further elucidate the effect of preoperative HFRT and chemotherapy on R0 limb-sparing surgery and toxicity rates for marginally resectable STS, a phase II trial with 46 patients from the Warsaw sarcoma center by Spałek et al. was published in 2021. R0 resection was achieved in 72% of patients while acute WCs were observed in 34% of patients comparable to the 35% in the SR-2 trial. Data on late toxicity rates are still pending [26, 54]. However, in this trial the median tumor diameter of 17.4 cm was remarkably larger compared to most other trials with perioperative HFRT for STS and to the SR-2 trial (< 10 cm in 65% in the preoperative RT group). Supporting this association, the multivariable analysis in the SR-2 trial also revealed a significant correlation between baseline tumor size and WCs [26]. Thus, having almost equal WC rates in hypofractionated and normofractionated RT despite a substantial difference in size attenuates the argument of increased WCs in HFRT for STS.
Only one trial has shown slightly higher rates of acute WCs using HFRT (37.9% vs. 35% in SR-2) [63]. However, in this trial, the sample size was relatively small (n = 34) because only myxoid liposarcomas (MLPS) were included. Moreover, most patients were irradiated with conventional 3D conformal radiotherapy (3D-CRT) and a short time gap of 3–7 days between RT and surgery [63]. Besides, MLPS are known for their favorable prognosis and radiosensitivity [90, 91]. So, even if further trials on this rare malignant tumor would bring forth more evidence of increased toxicity with HFRT, one could still discuss a de-escalation concept due to their high radiosensitivity. The Dutch multicenter DOREMY trial has applied reduced preoperative normofractionated RT (18 × 2 Gy instead of 25 × 2 Gy standard dose) for MLPS patients in an attempt to deescalate radiation dose. The authors achieved remarkably low acute WCs of 17% when compared to the preoperative RT group in the SR-2 trial. However, while the definition of major WC as a clinical diagnosis is equal, the DOREMY trial defined acute WCs by 30 days after surgery while the SR-2 trial applied 120 days [92] (NCT02106312).
A lot of knowledge on risk factors for major WCs stems from large surgical and RT data analyses. As such, it is an interesting finding throughout all treatment modalities and trials investigated in this review that the vast majority of WCs are located in the lower extremities, accounting for substantial postoperative morbidity (Table 2). This observation has been confirmed in different multicenter data analyses [84, 85]. In addition, the authors also found influenceable risk factors like increased BMI and smoking to be associated with postoperative WCs [84, 85]. In line with this, further trials confirmed the above-mentioned risk factors and added diabetes, tumor size > 10 cm, vascular tumor infiltration, and proximity to the skin < 3 mm as further predictors of major WCs [82, 83]. These findings may alter the preoperative management (nutrition, smoking cessation, diabetes training, surgical technique) to optimize post-surgical outcomes in STS patients [82, 83].
Furthermore, while acute WCs constitute serious adverse events, they are usually curable by local treatment. In contrast, long-term analysis of the patients in the Canadian SR-2 trials has revealed significantly lower functional scores in patients suffering from late and irreversible toxicities such as fibrosis, joint stiffness, and edema [24]. This observation may explain the increasing trend towards preferring pre- over postoperative RT in the treatment of STS [22, 23].
Apart from one trial, no other trials analyzed in our systematic review have found higher rates of early or late toxicity with HFRT for STS [63]. Quite the contrary, most trials have shown reduced risks of toxicity with advanced RT techniques. However, no large randomized phase III controlled trial has yet compared HFRT to normofractionated RT with a particular focus on toxicity rates and morbidity. One of the few controlled trials investigating this very topic is currently enrolling patients at the University of Wisconsin Hospital and Clinics (Madison, Wisconsin, United States, section 4.3 Upcoming data) [93].
Oncological outcomes
The outcome benefits of HFRT for STS are promising. Well-established independent risk factors for LR and mortality comprise positive surgical margins, histological grade, tumor depth, and previous LR for subsequent recurrences and mortality. Additionally, specific histological subtypes (e.g., malignant peripheral nerve sheath tumor or myxofibrosarcomas) are associated with disadvantageous clinical outcomes [11, 12, 15, 16].
Overall, LC as a quality criterion for HFRT shows good to excellent results, ranging between 80–100% between 3 to 5 years in the largest studies analyzed herein (Table 2). The most comprehensive trial comprising 311 representative patients with locally advanced sarcomas treated with a short course of 5 × 5 Gy has achieved acceptable rates of 5-year LR of 13.8% when compared to previous literature [14, 53, 94]. About 83% of tumors were resected with clear margins, a protective factor for LR as described in previously published analyses [95]. The additional preoperative chemotherapy with doxorubicin and ifosfamide or dacarbazine administered to one third of patients did not significantly alter survival or LR, although the trial was not powered for this factor [53]. On multivariable analysis, specific histological subtypes such as malignant peripheral nerve sheath tumors or leiomyosarcomas have confirmed the previous literature on their increased malignancy and resistance to treatment (5-year LC of approximately 65–70%) [11, 96].
Again, the addition of IG-IMRT to HFRT has substantial benefits and improves LC rates. Kalbasi et al. have applied 5 × 6 Gy IMRT in 76% of patients and IGRT in almost all 50 patients enrolled in 2020 [47]. With a minimum follow-up of two years, only 5.7% of patients with LR were observed [47]. Limitations in comparability are the pending long-term follow-up data [47]. The improvement by IMRT is supported by data on normofractionated postoperative RT, where IMRT has shown significant benefits on LC compared to conventional external beam RT [97, 98]. Altogether, the presented data on preoperative HFRT has shown similar LC rates when compared to preoperative normofractionated RT for STS [70, 71].
An interesting secondary finding in the study by Kalbasi et al. is the significant increase in both patient accrual and distance traveled by patients, when they were enrolled into 5 × 6 Gy RT compared to standard 25 × 2 Gy in the 2-year period preceding study initiation [47]. This approves the logistical and convenience argument by many other studies on patient preferences and therapy adherence to shorter RT courses, which particularly holds true for elderly patients [44, 46, 99].
MLPS repeatedly stand out by their remarkably high radiosensitivity, which sustains also in HFRT regimens. In 27 patients with large MLPS (median size: 13 cm), treated with preoperative 5 × 5 Gy and a median follow-up of 27 months, none of the patients had a LR. OS was 93% because of two patients who died after metastatic spread [58]. In another trial, published four years earlier, the same authors from the Warsaw sarcoma center have used 5 × 5 or 5 × 4 Gy for MLPS patients and have shown similarly favorable LC rates of 90% after five years. The 5-year OS was 68%. All deaths were related to distant recurrences, again proving the excellent radiosensitivity and local controllability by HFRT [63]. This radiosensitivity is confirmed in multiple previous studies and large database analyses on normofractionated RT and may be exploited to further deescalate local therapy regimens [90, 91, 100].
We can therefore conclude that the present data strongly suggests modern HFRT regimens and techniques to be comparable to normofractionated RT in LC rates of STS. However, the present results are, at best, derived from phase II trials. So far, no randomized phase III trial comparing normofractionated RT to HFRT for STS has been conducted. Both the study population and the specific tumor entities are highly heterogeneous, and most of the trials are non-controlled trials or retrospective data analyses (Table 2) [101]. The included articles demonstrated moderate to serious overall risk of bias and therefore hamper comparability (Additional file 2: Risk of bias assessment according to ROBINS-I, Table 1). Moreover, the available trials differ in RT, surgical techniques, concomitant chemotherapy regimens, and the therapy modalities’ order. Research on STS as "orphan diseases" is impeded by low prevalence and lower funding compared to other cancer entities [102]. Thus, the present data is generating strong hypotheses and future results are eagerly awaited.
Upcoming data
More than 15 trials on HFRT + / − chemotherapy in STS are currently ongoing (Table 4). Due to the low prevalence, most trials have long recruiting phases. Among the first trials to compare conventionally fractionated vs. HFRT for STS has recently begun accruing patients at the University of Wisconsin, USA [93] (NCT05109494). Another randomized interventional trial focuses on acute postoperative WCs in localized head and neck, trunk and extremity STS after 14 × 3 Gy preoperative RT (study arm B) compared to standard preoperative RT (25 × 2 Gy) [103]. The study began recruiting in June 2021 at two Dutch university medical centers in Leiden and Groningen and is expected to reach primary completion by April 2025 [103] (NCT04425967).
Many studies are testing different preoperative, HFRT regimens to shorten therapy time and improve patient convenience. For instance, 15 × 2.85 Gy is applied to investigate major WCs (as defined by O'Sullivan et al.) for an estimated number of 120 STS patients at the Mayo Clinic, Rochester, USA [26]. Secondary outcome measures include oncological outcomes and for the first time, patient reported outcomes with regard to changes in the quality of life. Estimated primary completion is November 2025 [104] (NCT04562480). The same regimen also investigating major WC rates in localized, resectable STS and comparing them to historical controls is conducted at the M.D. Anderson Cancer Center and expected to reach completion by August 2023 [105] (NCT03819985). Similarly, the McGill University in Montreal, Canada, is accruing patients to apply a short, preoperative, HFRT regimen of 5 × 7 Gy within one week (PRESTO trial). The primary outcome is radiation-associated toxicity. For the secondary outcomes, the authors apply established questionnaires and functional scoring systems (Toronto Extremity Salvage Score [TESS], Musculoskeletal Tumor Society Score MSTS) to evaluate patients' daily performance activity and quality of life. The study commenced in June 2020 and is estimated to reach primary completion by January 2025 [106] (NCT04617327).
Other groups apply evolving technology to improve outcomes for STS patients under HFRT: Another phase II trial at the University of Wisconsin will be accruing around 48 patients to test advanced highly conformal HFRT with 2-year LC rates as primary endpoint; the estimated primary completion date is July 2023 [107] (NCT03972930). Moreover, two phase II randomized German trials are investigating the feasibility of modern, neoadjuvant, hypofractionated particle therapy (C12 carbon ions vs. protons) with 3 Gy to 39 Gy for STS of the extremities and retroperitoneal STS. Both are currently accruing patients at the University of Heidelberg [108, 109] (NCT04946357 and NCT04219202).
Summary
STS are rare, heterogenous malignancies and therefore challenging in both research and multidisciplinary treatment. Preoperative, five to six weeks RT regimens currently represent the mainstay of management at high-volume sarcoma centers in high-grade STS (G2-G3). Shortening RT courses can improve therapy convenience, raise cost-effectiveness, and provide more treatment opportunities for a wider range of patients. The suggested risk of higher rates of adverse effects and worse oncological outcomes cannot be confirmed by the available data and studies. Toxicity rates are mostly equal or less than in representative trials for normofractionated RT. Preoperative RT is preferred over postoperative RT due to lower rates of irreversible late toxicity. Preoperative HFRT achieves comparable LC rates with shorter duration of therapy. However, all data are derived from retrospective data analyses and phase II trials. The interpretation must therefore be made with caution. Multiple trials on HFRT are underway and the results in this evolving field are awaited with great interest.
Availability of data and materials
Not applicable.
Abbreviations
- 3D-CRT:
-
3D conformal radiotherapy
- AI:
-
Doxorubicin/ifosfamide
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- CTV:
-
Clinical target volume
- CTX:
-
Chemotherapy
- DFS:
-
Disease-free survival
- GTV:
-
Gross tumor volume
- HFRT:
-
Hypofractionated radiotherapy
- IGRT:
-
Image-guided radiotherapy
- IG-IMRT:
-
Image-guided intensity modulated radiotherapy
- IMRT:
-
Intensity modulated radiotherapy
- LC:
-
Local control
- LR:
-
Local recurrence
- LRFS:
-
Local recurrence-free survival
- MLPS:
-
Myxoid liposarcomas
- MRI:
-
Magnetic resonance imaging
- MSTS:
-
Musculoskeletal Tumor Society Score
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTV:
-
Planning target volume
- ROBINS-I:
-
Risk of Bias In Non-randomized Studies of Interventions tool
- RT:
-
Radiotherapy
- SBRT:
-
Stereotactic body radiotherapy
- STS:
-
Soft tissue sarcoma
- TESS:
-
Toronto Extremity Salvage Score
- USA:
-
United States of America
- VMAT:
-
Volumetric Intensity Modulated Arc Therapy
- WC:
-
Wound complication
References
Clark MA, Fisher C, Judson I, Thomas JM. Soft-tissue sarcomas in adults. N Engl J Med. 2005;353(7):701–11.
Goldblum JR, Weiss SW, Folpe AL. Enzinger and Weiss's soft tissue tumors E-book: Elsevier Health Sciences;2013.
Lahat G, Lazar A, Lev D. Sarcoma epidemiology and etiology: potential environmental and genetic factors. Surg Clin N Am. 2008;88(3):451–81.
Burningham Z, Hashibe M, Spector L, Schiffman JD. The epidemiology of sarcoma. Clin Sarcoma Res. 2012;2(1):14.
Gatta G, Capocaccia R, Botta L, Mallone S, De Angelis R, Ardanaz E, et al. Burden and centralised treatment in Europe of rare tumours: results of RARECAREnet—a population-based study. Lancet Oncol. 2017;18(8):1022–39.
Trojani M, Contesso G, Coindre JM, Rouesse J, Bui NB, de Mascarel A, et al. Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system. Int J Cancer. 1984;33(1):37–42.
Costa J, Wesley RA, Glatstein E, Rosenberg SA. The grading of soft tissue sarcomas. Results of a clinicohistopathologic correlation in a series of 163 cases. Cancer. 1984;53(3):530–41.
WHO. Classification of tumors, Soft tissue and bone tumours 5th Edition ed. Lyon: International Agency for Research on Cancer;2020.
van Houdt WJ, Zaidi S, Messiou C, Thway K, Strauss DC, Jones RL. Treatment of retroperitoneal sarcoma: current standards and new developments. Curr Opin Oncol. 2017;29(4):260–7.
Lindner LH, Issels RD. Hyperthermia in soft tissue sarcoma. Curr Treat Options Oncol. 2011;12(1):12–20.
Pisters PW, Leung DH, Woodruff J, Shi W, Brennan MF. Analysis of prognostic factors in 1,041 patients with localized soft tissue sarcomas of the extremities. J Clin Oncol. 1996;14(5):1679–89.
Biau DJ, Ferguson PC, Chung P, Griffin AM, Catton CN, O’Sullivan B, et al. Local recurrence of localized soft tissue sarcoma: a new look at old predictors. Cancer. 2012;118(23):5867–77.
Callegaro D, Miceli R, Bonvalot S, Ferguson P, Strauss DC, Levy A, et al. Development and external validation of two nomograms to predict overall survival and occurrence of distant metastases in adults after surgical resection of localised soft-tissue sarcomas of the extremities: a retrospective analysis. Lancet Oncol. 2016;17(5):671–80.
Eilber FC, Rosen G, Nelson SD, Selch M, Dorey F, Eckardt J, et al. High-grade extremity soft tissue sarcomas: factors predictive of local recurrence and its effect on morbidity and mortality. Ann Surg. 2003;237(2):218–26.
Harati K, Goertz O, Pieper A, Daigeler A, Joneidi-Jafari H, Niggemann H, et al. Soft tissue sarcomas of the extremities: surgical margins can be close as long as the resected tumor has no ink on it. Oncologist. 2017;22(11):1400–10.
Haglund KE, Raut CP, Nascimento AF, Wang Q, George S, Baldini EH. Recurrence patterns and survival for patients with intermediate- and high-grade myxofibrosarcoma. Int J Radiat Oncol Biol Phys. 2012;82(1):361–7.
Deutsche Krebsgesellschaft DK, AWMF. S3-Leitlinie Adulte Weichgewebesarkome, Langversion Version 1.0, 2021. Leitlinienprogramm Onkologie. 2021.
Gronchi A, Miah AB, Dei Tos AP, Abecassis N, Bajpai J, Bauer S, et al. Soft tissue and visceral sarcomas: ESMO–EURACAN–GENTURIS Clinical Practice Guidelines for diagnosis, treatment and follow-up<sup>☆</sup>. Ann Oncol. 2021;32(11):1348–65.
Blay JY, Honoré C, Stoeckle E, Meeus P, Jafari M, Gouin F, et al. Surgery in reference centers improves survival of sarcoma patients: a nationwide study. Ann Oncol. 2019;30(7):1143–53.
Haas RL, Delaney TF, O’Sullivan B, Keus RB, Le Pechoux C, Olmi P, et al. Radiotherapy for management of extremity soft tissue sarcomas: Why, when, and where? Int J Radiat Oncol Biol Phys. 2012;84(3):572–80.
Rothermundt C, Fischer GF, Bauer S, Blay JY, Grünwald V, Italiano A, et al. Pre- and postoperative chemotherapy in localized extremity soft tissue sarcoma: a European organization for research and treatment of cancer expert survey. Oncologist. 2018;23(4):461–7.
Lazarev S, McGee H, Moshier E, Ru M, Demicco EG, Gupta V. Preoperative vs postoperative radiation therapy in localized soft tissue sarcoma: nationwide patterns of care and trends in utilization. Pract Radiat Oncol. 2017;7(6):e507–16.
Salerno KE, Alektiar KM, Baldini EH, Bedi M, Bishop AJ, Bradfield L, et al. Radiation therapy for treatment of soft tissue sarcoma in adults: executive summary of an ASTRO clinical practice guideline. Pract Radiat Oncol. 2021;11(5):339–51.
Davis AM, O’Sullivan B, Turcotte R, Bell R, Catton C, Chabot P, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol. 2005;75(1):48–53.
O'Sullivan B, Davis AM, Turcotte RE, Bell R, Wunder JS, Catton CN, et al. Five-year results of a randomized phase III trial of pre-operative vs post-operative radiotherapy in extremity soft tissue sarcoma. J Clin Oncol 2004;22 14_suppl:9007.
O’Sullivan B, Davis AM, Turcotte R, Bell R, Catton C, Chabot P, et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet. 2002;359(9325):2235–41.
Barnett GC, West CML, Dunning AM, Elliott RM, Coles CE, Pharoah PDP, et al. Normal tissue reactions to radiotherapy: towards tailoring treatment dose by genotype. Nat Rev Cancer. 2009;9(2):134–42.
Wang K, Tepper JE. Radiation therapy-associated toxicity: Etiology, management, and prevention. CA A Cancer J Clin. 2021;71(5):437–54.
Whelan TJ, Pignol J-P, Levine MN, Julian JA, MacKenzie R, Parpia S, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med. 2010;362(6):513–20.
Widmark A, Gunnlaugsson A, Beckman L, Thellenberg-Karlsson C, Hoyer M, Lagerlund M, et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial. Lancet. 2019;394(10196):385–95.
Haviland JS, Owen JR, Dewar JA, Agrawal RK, Barrett J, Barrett-Lee PJ, et al. The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol. 2013;14(11):1086–94.
Ma L, Wang L, Tseng CL, Sahgal A. Emerging technologies in stereotactic body radiotherapy. Chin Clin Oncol. 2017;6(Suppl 2):S12.
Ahmad SS, Duke S, Jena R, Williams MV, Burnet NG. Advances in radiotherapy. BMJ Br Med J. 2012;345: e7765.
Advanced and emerging technologies in radiation oncology physics. [s.l.]: CRC Press;2020.
Wang D, Zhang Q, Eisenberg BL, Kane JM, Li XA, Lucas D, et al. Significant reduction of late toxicities in patients with extremity sarcoma treated with image-guided radiation therapy to a reduced target volume: results of radiation therapy oncology group RTOG-0630 trial. J Clin Oncol. 2015;33(20):2231–8.
van Leeuwen CM, Oei AL, Crezee J, Bel A, Franken NAP, Stalpers LJA, et al. The alfa and beta of tumours: a review of parameters of the linear-quadratic model, derived from clinical radiotherapy studies. Radiat Oncol. 2018;13(1):96.
Thames HD, Suit HD. Tumor radioresponsiveness versus fractionation sensitivity. Int J Radiat Oncol Biol Phys. 1986;12(4):687–91.
Haas RL, Floot BGJ, Scholten AN, van der Graaf WTA, van Houdt W, Schrage Y, et al. Cellular radiosensitivity of soft tissue sarcoma. Radiat Res. 2021;196(1):23–30.
Bentzen SM, Agrawal RK, Aird EG, Barrett JM, Barrett-Lee PJ, Bentzen SM, et al. The UK Standardisation of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet. 2008;371(9618):1098–107.
Bujko K, Nowacki MP, Nasierowska-Guttmejer A, Michalski W, Bebenek M, Kryj M. Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br J Surg. 2006;93(10):1215–23.
Abarca T, Gao Y, Monga V, Tanas MR, Milhem MM, Miller BJ. Improved survival for extremity soft tissue sarcoma treated in high-volume facilities. J Surg Oncol. 2018;117(7):1479–86.
Venigalla S, Nead KT, Sebro R, Guttmann DM, Sharma S, Simone CB 2nd, et al. Association between treatment at high-volume facilities and improved overall survival in soft tissue sarcomas. Int J Radiat Oncol Biol Phys. 2018;100(4):1004–15.
Vos M, Blaauwgeers HGT, Ho VKY, van Houdt WJ, van der Hage JA, Been LB, et al. Increased survival of non low-grade and deep-seated soft tissue sarcoma after surgical management in high-volume hospitals: a nationwide study from the Netherlands. Eur J Cancer. 2019;110:98–106.
Pfeffer MR, Blumenfeld P. The changing paradigm of radiotherapy in the elderly population. Cancer J. 2017;23(4):223–30.
Yan M, Gouveia AG, Cury FL, Moideen N, Bratti VF, Patrocinio H, et al. Practical considerations for prostate hypofractionation in the developing world. Nat Rev Urol. 2021;18(11):669–85.
Hoopes DJ, Kaziska D, Chapin P, Weed D, Smith BD, Hale ER, et al. Patient preferences and physician practice patterns regarding breast radiotherapy. Int J Radiat Oncol Biol Phys. 2012;82(2):674–81.
Kalbasi A, Kamrava M, Chu FI, Telesca D, Van Dams R, Yang Y, et al. A Phase II trial of 5-day neoadjuvant radiotherapy for patients with high-risk primary soft tissue sarcoma. Clin Cancer Res. 2020;26(8):1829–36.
Zemplényi AT, Kaló Z, Kovács G, Farkas R, Beöthe T, Bányai D, et al. Cost-effectiveness analysis of intensity-modulated radiation therapy with normal and hypofractionated schemes for the treatment of localised prostate cancer. Eur J Cancer Care (Engl). 2018;27(1).
Voong KR, Lal LS, Kuban DA, Pugh TJ, Swint JM, Godby J, et al. Long-term economic value of hypofractionated prostate radiation: Secondary analysis of a randomized trial. Adv Radiat Oncol. 2017;2(3):249–58.
Spałek MJ, Rutkowski P. Coronavirus disease (COVID-19) outbreak: hypofractionated radiotherapy in soft tissue sarcomas as a valuable option in the environment of limited medical resources and demands for increased protection of patients. Front Oncol. 2020;10:993.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355: i4919.
Koseła-Paterczyk H, Teterycz P, Spałek MJ, Borkowska A, Zawadzka A, Wągrodzki M, et al. Efficacy and safety of hypofractionated preoperative radiotherapy for primary locally advanced soft tissue sarcomas of limbs or trunk wall. Cancers (Basel). 2021;13(12).
Spałek MJ, Koseła-Paterczyk H, Borkowska A, Wągrodzki M, Szumera-Ciećkiewicz A, Czarnecka AM, et al. Combined preoperative hypofractionated radiotherapy with doxorubicin-ifosfamide chemotherapy in marginally resectable soft tissue sarcomas: results of a phase 2 clinical trial. Int J Radiat Oncol Biol Phys. 2021;110(4):1053–63.
Leite ETT, Munhoz RR, Camargo VP, Lima L, Rebolledo DCS, Maistro CEB, et al. Neoadjuvant stereotactic ablative radiotherapy (SABR) for soft tissue sarcomas of the extremities. Radiother Oncol. 2021;161:222–9.
Potkrajcic V, Traub F, Hermes B, Scharpf M, Kolbenschlag J, Zips D, et al. Hypofractionated preoperative radiotherapy for high risk soft tissue sarcomas in a geriatric patient population. Radiol Oncol. 2021;55(4):459–66.
Gobo Silva ML, Lopes de Mello CA, Aguiar Junior S, D'Almeida Costa F, Stevanato Filho PR, Santoro Bezerra T, et al. Neoadjuvant hypofractionated radiotherapy and chemotherapy for extremity soft tissue sarcomas: safety, feasibility, and early oncologic outcomes of a phase 2 trial. Radiother Oncol. 2021;159:161–7.
Koseła-Paterczyk H, Spałek M, Borkowska A, Teterycz P, Wągrodzki M, Szumera-Ciećkiewicz A, et al. Hypofractionated radiotherapy in locally advanced myxoid liposarcomas of extremities or trunk wall: results of a single-arm prospective clinical trial. J Clin Med. 2020;9(8).
Parsai S, Lawrenz J, Kilpatrick S, Rubin B, Hymes C, Gray M, et al. Early outcomes of preoperative 5-fraction radiation therapy for soft tissue sarcoma followed by immediate surgical resection. Adv Radiat Oncol. 2020;5(6):1274–9.
Pennington JD, Eilber FC, Eilber FR, Singh AS, Reed JP, Chmielowski B, et al. Long-term outcomes with ifosfamide-based hypofractionated preoperative chemoradiotherapy for extremity soft tissue sarcomas. Am J Clin Oncol. 2018;41(12):1154–61.
Kubicek GJ, LaCouture T, Kaden M, Kim TW, Lerman N, Khrizman P, et al. Preoperative radiosurgery for soft tissue sarcoma. Am J Clin Oncol. 2018;41(1):86–9.
Kılıç L, Ekenel M, Karabulut S, Ağaoğlu F, Darendeliler E. Neoadjuvant sequential chemoradiotherapy versus radiotherapy alone for treatment of high-risk extremity soft tissue sarcoma: a single-institution experience. Contemp Oncol (Pozn). 2017;21(1):60–5.
Koseła-Paterczyk H, Szumera-Ciećkiewicz A, Szacht M, Haas R, Morysiński T, Dziewirski W, et al. Efficacy of neoadjuvant hypofractionated radiotherapy in patients with locally advanced myxoid liposarcoma. Eur J Surg Oncol. 2016;42(6):891–8.
Koseła-Paterczyk H, Szacht M, Morysiński T, Ługowska I, Dziewirski W, Falkowski S, et al. Preoperative hypofractionated radiotherapy in the treatment of localized soft tissue sarcomas. Eur J Surg Oncol. 2014;40(12):1641–7.
Lansu J, Bovée J, Braam P, van Boven H, Flucke U, Bonenkamp JJ, et al. Dose reduction of preoperative radiotherapy in myxoid liposarcoma: a nonrandomized controlled trial. JAMA Oncol. 2021;7(1): e205865.
Lansu J, Groenewegen J, van Coevorden F, van Houdt W, van Akkooi ACJ, van Boven H, et al. Time dependent dynamics of wound complications after preoperative radiotherapy in extremity soft tissue sarcomas. Eur J Surg Oncol. 2019;45(4):684–90.
O’Sullivan B, Griffin AM, Dickie CI, Sharpe MB, Chung PW, Catton CN, et al. Phase 2 study of preoperative image-guided intensity-modulated radiation therapy to reduce wound and combined modality morbidities in lower extremity soft tissue sarcoma. Cancer. 2013;119(10):1878–84.
Hui AC, Ngan SY, Wong K, Powell G, Choong PF. Preoperative radiotherapy for soft tissue sarcoma: the Peter MacCallum Cancer Centre experience. Eur J Surg Oncol. 2006;32(10):1159–64.
Kraybill WG, Harris J, Spiro IJ, Ettinger DS, DeLaney TF, Blum RH, et al. Phase II study of neoadjuvant chemotherapy and radiation therapy in the management of high-risk, high-grade, soft tissue sarcomas of the extremities and body wall: Radiation Therapy Oncology Group Trial 9514. J Clin Oncol. 2006;24(4):619–25.
Zagars GK, Ballo MT, Pisters PW, Pollock RE, Patel SR, Benjamin RS. Preoperative vs. postoperative radiation therapy for soft tissue sarcoma: a retrospective comparative evaluation of disease outcome. Int J Radiat Oncol Biol Phys. 2003;56(2):482–8.
Pollack A, Zagars GK, Goswitz MS, Pollock RA, Feig BW, Pisters PW. Preoperative vs. postoperative radiotherapy in the treatment of soft tissue sarcomas: a matter of presentation. Int J Radiat Oncol Biol Phys. 1998;42(3):563–72.
Mayinger M, Straube C, Habermehl D, Duma MN, Combs SE. Hypo- vs. normofractionated radiation therapy in breast cancer: a patterns of care analysis in German speaking countries. Rep Pract Oncol Radiother. 2020;25(5):775–9.
Mowery YM, Blitzblau RC. Whole-breast radiation therapy: the long and short of it. Int J Radiat Oncol Biol Phys. 2014;90(5):990–2.
Wendtner CM, Abdel-Rahman S, Baumert J, Falk MH, Krych M, Santl M, et al. Treatment of primary, recurrent or inadequately resected high-risk soft-tissue sarcomas (STS) of adults: results of a phase II pilot study (RHT-95) of neoadjuvant chemotherapy combined with regional hyperthermia. Eur J Cancer. 2001;37(13):1609–16.
Issels RD, Mittermüller J, Gerl A, Simon W, Ortmaier A, Denzlinger C, et al. Improvement of local control by regional hyperthermia combined with systemic chemotherapy (ifosfamide plus etoposide) in advanced sarcomas: updated report on 65 patients. J Cancer Res Clin Oncol. 1991;117(4):S141–7.
Issels RD, Abdel-Rahman S, Wendtner CM, Falk MH, Kurze V, Sauer H, et al. Neoadjuvant chemotherapy combined with regional hyperthermia (RHT) for locally advanced primary or recurrent high-risk adult soft-tissue sarcomas (STS) of adults: long-term results of a phase II study. Eur J Cancer. 2001;37(13):1599–608.
Wendtner CM, Abdel-Rahman S, Krych M, Baumert J, Lindner LH, Baur A, et al. Response to neoadjuvant chemotherapy combined with regional hyperthermia predicts long-term survival for adult patients with retroperitoneal and visceral high-risk soft tissue sarcomas. J Clin Oncol. 2002;20(14):3156–64.
Issels RD, Prenninger SW, Nagele A, Boehm E, Sauer H, Jauch KW, et al. Ifosfamide plus etoposide combined with regional hyperthermia in patients with locally advanced sarcomas: a phase II study. J Clin Oncol. 1990;8(11):1818–29.
Issels RD, Lindner LH, Verweij J, Wessalowski R, Reichardt P, Wust P, et al. Effect of Neoadjuvant Chemotherapy Plus Regional Hyperthermia on Long-term outcomes among patients with localized high-risk soft tissue sarcoma: The EORTC 62961-ESHO 95 Randomized Clinical Trial. JAMA Oncol. 2018;4(4):483–92.
Issels RD, Lindner LH, Verweij J, Wust P, Reichardt P, Schem B-C, et al. Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: a randomised phase 3 multicentre study. Lancet Oncol. 2010;11(6):561–70.
Spałek MJ, Borkowska AM, Telejko M, Wągrodzki M, Niebyłowska D, Uzar A, et al. The feasibility study of hypofractionated radiotherapy with regional hyperthermia in soft tissue sarcomas. Cancers (Basel). 2021;13(6).
Baldini EH, Lapidus MR, Wang Q, Manola J, Orgill DP, Pomahac B, et al. Predictors for major wound complications following preoperative radiotherapy and surgery for soft-tissue sarcoma of the extremities and trunk: importance of tumor proximity to skin surface. Ann Surg Oncol. 2013;20(5):1494–9.
Schwartz A, Rebecca A, Smith A, Casey W, Ashman J, Gunderson L, et al. Risk factors for significant wound complications following wide resection of extremity soft tissue sarcomas. Clin Orthop Relat Res. 2013;471(11):3612–7.
Slump J, Bastiaannet E, Halka A, Hoekstra HJ, Ferguson PC, Wunder JS, et al. Risk factors for postoperative wound complications after extremity soft tissue sarcoma resection: a systematic review and meta-analyses. J Plast Reconstr Aesthet Surg. 2019;72(9):1449–64.
Bedi M, Ethun CG, Charlson J, Tran TB, Poultsides G, Grignol V, et al. Is a nomogram able to predict postoperative wound complications in localized soft-tissue sarcomas of the extremity? Clin Orthop Relat Res. 2020;478(3):550–9.
Song CW, Kim MS, Cho LC, Dusenbery K, Sperduto PW. Radiobiological basis of SBRT and SRS. Int J Clin Oncol. 2014;19(4):570–8.
Li S, Shen L. Radiobiology of stereotactic ablative radiotherapy (SABR): perspectives of clinical oncologists. J Cancer. 2020;11(17):5056–68.
Song CW, Levitt SH. Vascular changes in walker 256 carcinoma of rats following X irradiation. Radiology. 1971;100(2):397–407.
Combined Treatment of Patients With Soft Tissue Sarcoma Including Preoperative Stereotactic Radiation Therapy and Postoperative Conformal Radiation Therapy. https://ClinicalTrials.gov/show/NCT04330456.
Pitson G, Robinson P, Wilke D, Kandel RA, White L, Griffin AM, et al. Radiation response: an additional unique signature of myxoid liposarcoma. Int J Radiat Oncol Biol Phys. 2004;60(2):522–6.
Betgen A, Haas RL, Sonke JJ. Volume changes in soft tissue sarcomas during preoperative radiotherapy of extremities evaluated using cone-beam CT. J Radiat Oncol. 2013;2(1):55–62.
Dose Reduction of Preoperative Radiotherapy in Myxoid Liposarcomas. https://ClinicalTrials.gov/show/NCT02106312.
Hypofractionated vs Conventional Fractionated RT in Soft Tissue Sarcomas. https://ClinicalTrials.gov/show/NCT05109494.
Zagars GK, Ballo MT, Pisters PW, Pollock RE, Patel SR, Benjamin RS, et al. Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: an analysis of 1225 patients. Cancer. 2003;97(10):2530–43.
Biau DJ, Ferguson PC, Chung P, Griffin AM, Catton CN, O’Sullivan B, et al. Local recurrence of localized soft tissue sarcoma. Cancer. 2012;118(23):5867–77.
Farid M, Demicco EG, Garcia R, Ahn L, Merola PR, Cioffi A, et al. Malignant peripheral nerve sheath tumors. Oncologist. 2014;19(2):193–201.
Folkert MR, Singer S, Brennan MF, Kuk D, Qin LX, Kobayashi WK, et al. Comparison of local recurrence with conventional and intensity-modulated radiation therapy for primary soft-tissue sarcomas of the extremity. J Clin Oncol. 2014;32(29):3236–41.
Alektiar KM, Brennan MF, Healey JH, Singer S. Impact of intensity-modulated radiation therapy on local control in primary soft-tissue sarcoma of the extremity. J Clin Oncol. 2008;26(20):3440–4.
Lazovich DA, White E, Thomas DB, Moe RE. Underutilization of breast-conserving surgery and radiation therapy among women with stage I or II breast cancer. JAMA. 1991;266(24):3433–8.
Chung PW, Deheshi BM, Ferguson PC, Wunder JS, Griffin AM, Catton CN, et al. Radiosensitivity translates into excellent local control in extremity myxoid liposarcoma: a comparison with other soft tissue sarcomas. Cancer. 2009;115(14):3254–61.
Board WCoTE. Soft Tissue and Bone Tumours: International Agency for Research on Cancer; 2020.
Haas RL, Miah AB, LePechoux C, DeLaney TF, Baldini EH, Alektiar K, et al. Preoperative radiotherapy for extremity soft tissue sarcoma; past, present and future perspectives on dose fractionation regimens and combined modality strategies. Radiother Oncol. 2016;119(1):14–21.
Short Course Of Preoperative Radiotherapy in Head and Neck-, Trunk- and Extremity Soft Tissue Sarcomas.
Hypofractionated Radiation Therapy Before Surgery for the Treatment of Localized, Resectable Soft Tissue Sarcoma of the Extremity and Superficial Trunk. https://ClinicalTrials.gov/show/NCT04562480.
Shorter Course, Hypofractionated Pre-Surgery Radiation Therapy in Treating Patients With Localized, Resectable Soft Tissue Sarcoma of the Extremity of Superficial Trunk.
Pre-operative RadiothErapy for Soft Tissue SarcOmas. https://ClinicalTrials.gov/show/NCT04617327.
Hypofractionated Radiotherapy for Soft Tissue Sarcomas. https://ClinicalTrials.gov/show/NCT03972930.
Neoadjuvant Irradiation of Extremity Soft Tissue Sarcoma With Ions. https://ClinicalTrials.gov/show/NCT04946357.
Neoadjuvant Irradiation of Retroperitoneal Soft Tissue Sarcoma With Ions Retro-Ion. https://ClinicalTrials.gov/show/NCT04219202.
Acknowledgements
Felix Ehret is participant in the BIH Charité Junior Clinician Scientist Program funded by the Charité – Universitätsmedizin Berlin and Berlin Institute of Health at Charité (BIH).
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, D.K.; investigation, data acquisition and analysis: S.R., D.K.; writing—original draft preparation, S.R.; writing—review and editing, all authors; visualization, S.R.; supervision, D.K. and V.B. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Due to the nature of this paper and its methodology, no institutional review board approval was required.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. The PRISMA 2020 checklist.
Additional file 2
. Risk of bias assessment according to ROBINSI.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Roohani, S., Ehret, F., Kobus, M. et al. Preoperative hypofractionated radiotherapy for soft tissue sarcomas: a systematic review. Radiat Oncol 17, 159 (2022). https://doi.org/10.1186/s13014-022-02072-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-022-02072-9