Abstract
Objective
The objective of this study is to quantify volume changes in the gross target volume (GTV) during preoperative radiotherapy for extremity soft tissue sarcomas (ESTS).
Methods
Twenty-seven patients with ESTS, treated with preoperative radiotherapy, were included in this study. Weekly cone-beam CT scans acquired for setup correction were used for GTV delineation in order to quantify volume changes over the course of treatment. Age, anatomical location, tumour type and tumour volume were evaluated as predictive factors for volume changes. Finally, the optimal time point for adaptive intervention was quantified.
Results
A GTV increase to a maximum of 28 % occurred in five patients. Thirteen patients showed no change and nine patients (all diagnosed with myxoid liposarcoma (MLS)) showed a GTV decrease to a maximum of 57 % of the GTV volume at start of treatment. In the multivariate analysis, only the relative volume change for tumour type was significant (p = 0.001). The optimal time point for adaptive intervention in non-MLS patients was the first week and for MLS patients the third week.
Conclusions
Volume changes were quantified during preoperative RT of ESTS. Volume decrease was observed only in MLS patients. Individualised treatment resulting in plan adaptations could result in a clinically useful volume reduction for MLS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery is the standard management for extremity soft tissue sarcomas (ESTS). Administration of (neo)adjuvant radiotherapy (RT) is dependent on the site, size, grade, histological subtype and pathologically assessed resection margins. RT improves local control and possibly overall survival while allowing higher extremity preservation rates [1–3]. In postoperative RT, the first 50 Gy is applied to the whole surgically treated area which may be at risk of contamination, including the scar and drain sites. Generally, these volumes are much larger than the sarcoma volume itself. A boost is subsequently applied to the original tumour location. The recommended dose for the boost is 10 Gy when ample surgical resection margins are negative and 16–20 Gy when resection margins are positive, narrow or indistinct. In preoperative RT, a conventional dose of 50 Gy is prescribed to the gross primary tumour (the gross target volume (GTV)), with a margin to include the volume that is at risk for containing microscopic extension (the clinical target volume (CTV)). A margin to account for geometrical uncertainties is added to the CTV to generate the planning target volume (PTV). Although there is a higher risk for wound complications [4], preoperative RT is often preferred. Smaller RT fields and a lower total dose for preoperative RT seem to be important prognostic factors for endpoints, such as fibrosis, oedema, arthrosis and bone fractures [5–8].
The introduction of image-guided radiotherapy, by means of, e.g. in-room cone-beam CT scan (CBCT), facilitates improved verification of the volumetric behaviour and position of the tumour during treatment. The position of the tumour relative to anatomical structures can change during the 5 weeks of treatment due to variations in patient position and/or changes in tumour volume. These changes in volume are difficult to assess when electronic portal imaging (EPI) is used but can be visualised on CBCT due to its 3D nature and improved soft tissue contrast. To realise smaller RT fields, optimal information about the location of the tumour (with respect to the bony anatomy) and the volumetric behaviour during RT is essential. Visa versa, from a local control point of view, field sizes need to be enlarged in case of GTV increase.
Therefore, the purpose of this study is to quantify changes in the GTV during preoperative RT of ESTS.
Methods
Patients and tumour characteristics
A group of 44 patients was retrospectively analysed. All patients were scheduled for preoperative RT for ESTS. Forty-two had various types of intermediate to high-grade deep-seated primary ESTS, while two patients were diagnosed with aggressive fibromatosis.
Twenty-seven patients were treated on a linear accelerator equipped with CBCT (Elekta Synergy, Elekta Oncology Systems Ltd., Crawley, West Sussex, UK), augmented with in-house developed software) [9]. All 27 patients were included in the study, and their setup correction was based on a CBCT-guided protocol. The remaining 17 patients were treated on a linear accelerator without CBCT. Setup verification for this patient group was performed with EPI. As soft tissue registration is not possible with EPI, these patients were not included in this study. The tumours were categorised using the WHO classification for STS [10]. Classification was performed preoperatively by a Tru-cut core biopsy or a small volume incision biopsy. The histopathological grading of STS by Coindre [11] was used.
Preparation procedure
A planning CT scan was acquired in treatment position for each patient. The treatment position (prone/supine, exo/endorotation of the lower limbs) depended on the location of the tumour. The position was chosen individually to be confident that an optimal treatment could be planned. Care was taken to assure the patient’s comfort and to the position of the opposite unaffected limb. Patients with a tumour in the buttock were scanned in prone position using an ankle support. No additional immobilisation device was used. Several individual immobilisation techniques were used for patients with tumours in the upper and lower leg. Most of these patients were scanned in supine position. The affected leg was fixated with an individual thermoplastic cast around the knee and/or the ankle. If necessary, the unaffected leg was lifted using Styrofoam blocks. In some patients both legs were immobilised. Skin marks were created on the patient for repositioning in the treatment room. A planning CT scan and diagnostic MR scan (T1 weighted, gadolinium enhanced) were acquired for each patient in treatment position. Both scans were acquired on the same day. The CT and MR scans were registered to the bony anatomy using in-house developed software and diagnostic information from both scans was used to aid GTV delineation.
Treatment
RT was administered by a linear accelerator with photon energies of 6–10 MV, to a dose of 50 Gy in 25 fractions. Planning and dose prescription were in conformity with the ICRU 50/62 guidelines [12]. The aim of the treatment planning was to spare the circumference of the long bones as much as possible (e.g. to prevent fractures [7]). For prevention of lymph oedema, at least one side of the skin of the extremity had to be spared. The chosen techniques changed during the overall time of this study from predominantly 3D conformal fields towards full IMRT. CBCT scans were acquired for setup verification based on bony anatomy, according to an offline shrinking action level decision protocol [13]. For each patient, at least seven CBCT scans were acquired; a minimum of two CBCT scans in the first week followed by at least one CBCT scan each week.
GTV changes
To quantify changes in volume and position for each patient during treatment, the GTV was delineated on the registered MRI/planning CT scan, the GTV in the CBCT scans acquired during the first two fractions and on the CBCT scans during each week of treatment. Delineation was performed with in-house developed software. With this software it was possible to visualise all scans in one overview. Delineation was performed after a registration on bony anatomy. To reduce intra-observer variation, the original GTV was copied to the first CBCT scan and adjusted. Next, the GTV of the first CBCT scan was copied to the second CBCT scan and so on. The delineations were performed in the axial view of the scans and verified in coronal and sagittal views. An example of the GTV delineations is presented in Fig. 1.
The absolute and relative volumes of the GTV were calculated for all scans. An increase or decrease in volume was defined by a change of 5 % in the relative volume. To acquire the most reliable volume estimation at start of treatment, the average GTV of the first two CBCT scans was used as a reference volume (CBCT reference). The relative volume changes were calculated in relation to CBCT reference to quantify changes during the whole course of treatment.
Out of the calculated volumes, an estimation was made of the GTV diameters. For that purpose, all GTVs were assumed to be spherical.
Adaptive radiotherapy
Bony anatomy registration simulates an online correction strategy. Volume changes however cannot be corrected using a simple couch shift. Adaptive re-planning could be considered as an alternative. To determine the optimal moment for such an adaptive intervention, the relative volume changes were not only calculated in relation to the planning CT scan but also in relation to the CBCT scan acquired during each week of treatment. Subsequently, the overall volume deviations (calculated as the root mean square (RMS) volume difference between the first N CBCT scans relative to the planning CT scan and the subsequent scans relative to the Nth CBCT scan) were calculated. The N that minimises the volume deviations indicates the optimal time point for a single adaptive intervention for the subsequent weeks. In formula:
with V i the volume at scan i, V p the volume of the planning CT, and T the total number of scans.
In this paper, we only evaluate a single adaptive intervention. We consider more than one adaptive intervention currently not practical in daily patient management, taking the time for re-scanning, re-delineation and re-planning into account.
Statistical analysis
For statistical analysis SPSS version 17.0 (SPSS, Chicago, Illinois) was used. Radiosensitivity of myxoid liposarcomas (MLS) is known from literature [14–18]. Therefore, the tumours were divided in two groups: non-MLS and MLS. Differences in volume changes were analysed using the Mann–Whitney U test. Furthermore, linear regression was used to quantify the influence of age, anatomical location, tumour type, and tumour volume. As there was a wide range in tumour volumes, these were divided into three groups: volume, <300 cm3, between 300 and 1,000 cm3 and >1,000 cm3. These cut-off levels divided our population into three equally sized subgroups of nine patients. A 5 % significance level was used in all analyses.
Results
Patient and tumour characteristics
Patient and tumour characteristics are presented in Table 1. The median age of the patients was 58 years (range, 19–79). There were 15 male and 12 female patients. All tumours were located in the lower extremities, 14 in the upper leg, 7 in the lower leg and 6 in the buttock. All tumours were located deep. MLS and malignant fibrous histiocytoma (MFH) were the most common subtypes, followed by myxo-fibrosarcoma (MFS), synovial sarcoma (SS) and malignant peripheral nerve sheath tumours (MPNST). The majority of patients received a dose of 50 Gy in 25 fractions, followed 4–6 weeks later by surgery. Two patients received a slightly different dose; one patient received 40 Gy, followed by a boost of 10 Gy, another patient appeared to be inoperable and was treated with a dose of 56 Gy, guided according to anticipated normal tissue complications due to its specific location. The time interval between the planning CT-scan and the first treatment fraction was 7–20 days. The mean GTV on the planning CT scan was 820 cm3 (range, 42–3,128 cm3). The mean GTV on CBCT reference was 829 cm3 (range, 34–3,513 cm3)
GTV volume and volume changes
The absolute and relative volumes, volume changes on CBCT reference and last CBCT scan and the histological subtypes of the sarcomas are presented in Table 2. The mean absolute GTV volume change was −22 cm (range, −313 to +292 cm3). The relative change was −5 % (range, −57 to +28 %). The table is divided into three parts: top, patients with GTV increase; middle, patients without significant change in GTV; and bottom, patients with GTV decrease.
The volume changes during treatment are presented in Fig. 2a–c. The x-axis shows the overall treatment time; the start of the treatment is defined as day zero. The time of the planning CT scan is indicated in negative numbers. The y-axis shows the percentage of volume change during the whole treatment. Not all CBCT scans were acquired during the same fraction for each patient due to the applied setup correction protocol. This accounts for the difference in length of the lines indicating the volumes. The colours used in the figures in this section are an indication for the histological type of ESTS (Fig. 2d). The yellow lines represent MLS; purple = MFH; green = MFS; light green = SS; blue = MPNST, and pink = others.
GTV increase was seen in five patients (Fig. 2a). One patient (No. 18—Table 2) showed an initial GTV decrease of 10 % before the start of treatment, followed by an increase of 28 % towards the end of treatment. In general, the other patients in this group, showed a constant GTV increase. Two patients had a MPNST, two a MFH and one patient was classified in the “other” group. Thirteen patients showed a rather constant GTV during the whole course of treatment (Fig. 2b). Also in this patient group, no clear relation was observed for a specific histological subtype. Three patients showed an initial GTV increase during the interval between planning CT scan and the start of treatment. In one patient a GTV increase of 10 % was observed up to the fourth week, but the volume remained constant to the end of treatment in relation to the CBCT reference. Another patient, with a relatively small MFH, showed a GTV decrease during the first 2 weeks, but showed no volume decrease at the end of treatment compared with the CBCT reference. Nine patients showed a GTV decrease (Fig. 2c). Only one of these patients had a small GTV increase during the first 2 weeks. All patients in this group were classified as MLS. The rate of decrease was similar but the time to onset differed. The estimated diameters changes of the GTV were between −1.6 and +0.8 cm (mean, −0.2 cm).
The baseline volume distribution of the 16 non-MLS patients (mean, 891 cm3; range, 48–3,246 cm3) was not significantly different from the volume of the 11 MLS patients (mean, 790 cm3; range, 81–1,839 cm3; p = 0.69). However, the relative volume change for non-MLS (mean, +4 %; range, −4 to +28 %) vs. MLS patients (mean, −19 %; range, −57 to +3 %) was significant (p = 0.001). The relative volume change was evaluated in the regression analysis. Univariate regression analysis showed significance for age (p = 0.03) and tumour type (p < 0.0001). No significance was shown for anatomical location (p = 0.76) or tumour volume per group (<300 cm3, between 300 and 1,000 and >1,000 cm3; p = 0.48). In the multivariate regression analysis, tumour type remained significant (p = 0.001) but age was no longer significant (p = 0.48). As MLS patients were generally younger than non-MLS patients (43 vs. 60), age and MLS are well correlated.
Adaptive radiotherapy
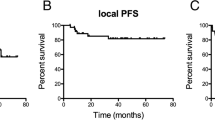
The optimal time point for adaptive intervention varied between the first week and the fourth week. For two patients, there was no benefit in ART. On average, for the non-MLS patients, the optimal time point was after week 1 (Fig. 3a) and for MLS patients after week 3 (Fig. 3b).
Lowest RMS values calculated in the 5 weeks of treatment. On the left, the lowest RMS of the non-MLS patients (a), and on the right, the lowest RMS of the MLS patients (b). The optimal CBCT scan as reference scan varied between the CBCT scan of the first week and the CBCT scan acquired in the fourth week. On average, the lowest RMS for the non-MLS patients was calculated in week 1 and for MLS patients in week 3
Discussion
Patients and tumour characteristics
The distribution between the subtypes in our patient group differs from the general distribution, where MFH is found to be the most common subtype [11]. This distribution however is a general distribution without difference in treatment (pre/postoperative RT, chemotherapy and surgery) and location. The patients selected for this study are only patients with Extremity STS, all treated preoperatively. Furthermore, when diagnosis is uncertain, pathologists tend to define the specimen as MFH. In a multidisciplinary institute, experienced in treatment of STS the diagnosis will in most cases be more specific.
GTV changes
Criteria for staging and grading of STS have changed over time, and therefore it is difficult to compare results of older studies to results of present studies.
Miki et al. studied size and change of STS during preoperative RT in relation to treatment outcome [19]. In this study, an increase of more than 10 % in tumour diameter was noted in 31 % of the patients. No change or decrease was seen in the other patients. In our study, an increase or decrease in tumour volume was defined by a change in the relative volume of 5 %.
STSs in general are not responsive to radiation. Nevertheless, a similar radiation response for MLS as described in literature [14–18] was also found in this study. However, not all MLS patients showed a GTV decrease with respect to the start of treatment. For two patients, no change was seen.
On the other hand, for a number of patients, a GTV increase was seen during treatment time. One should be aware of the fact that a GTV increase could lead to an under dosage of the tumour and possibly to a failure of the preoperative RT treatment. In all patients, after visual assessment, the GTV remained within the PTV; therefore, no patients required re-planning due to GTV increase.
Magierowski et al. [20] presented similar results at the 14th Connective Tissue Oncology Society (CTOS) meeting. They also performed a retrospective study of volume changes in two pathological subtypes of STS: MLS (n = 10) and MFH (n = 10). The GTV and bone were delineated on a pre- and post-RT CT scan. They calculated the discrepancies between the delineated contours of the GTV in both scans using a deformable registration algorithm. In the MLS patients, a median tumour reduction of 51 % was seen and in the MFH patients a median growth of 11 %. However, they found no statistical significance.
Delineation
Inter-observer variability could not be qualified as the delineations of the GTV were performed once by only one observer. Moreover, the delineations were performed on CBCT scans, which have a lower image quality than the planning CT scan or an MR scan. Volume changes between planning CT scan and the reference CBCT scan and changes during RT could also be the result of delineation uncertainties. Delineation on MR scan could be more accurate, but even in this modality significant inter- and intra-observer variation have been demonstrated [21]. Furthermore, we assumed that changes in the CTV behaved similar to changes in the GTV. After generation of the CTV from the GTV it was necessary in all patients to manually edit the CTV near structures such as the fascia or bone, unless the tumour was invasive at these areas. The image quality of the CBCT scan was insufficient to distinguish structures such as the fascia or small blood vessels, making delineation of the CTV quite complicated. For a more accurate quantification of target volumes, it may be advisable to repeat the study with delineations of the GTV and edited CTV on repeat scans of better image quality (CT or MRI). However, this option is less practical. Further improvement of the image quality of the CBCT scans may enable improved and more accurate delineations of the CTV in the future.
Adaptive radiotherapy
The optimal CBCT scan as a reference scan for re-planning appeared to be in week 1 for the non-MLS patients. For the MLS patients, a re-planning in week 3 would be more useful. For the latter, a reduction in field size and a possible reduction in toxicity could be achieved. However, the clinical relevance of ART must be considered if the tumour volume is already small, or the volume change is in the direction of air. Furthermore, without accurate GTV delineation, reduction in field size must be performed with great care. Even in postoperative RT, the CTV covers the original invaded tissue.
Note that the optimal time points for ART were derived from a geometrical surrogate: the RMS volume deviations from the (adaptive) planning anatomy. Dosimetric evaluation of actual adaptive re-planning should be performed to validate these time points.
There is a possibility that the sarcoma continues to grow in the interval between planning CT scan and start of treatment (median, 11 days; range, 7–20 days). To rule out the volume changes prior to RT, all changes have been performed with respect to the start of treatment. Ideally patients should start in the week of the planning CT scan. In that case, volume changes could be calculated between the planning CT scan and consecutive CBCT-scans. The necessity to re-plan in week 1 for the non-MLS group would also be reduced if preparation time is shortened.
Statistics
The number of patients (27) in this study was too small to differentiate between tumour behaviour in STS subtypes other than MLS. In this study, all other subtypes were evaluated as one group.
Conclusions
This study confirms that MLS regress more than other STS and demonstrates the potential for more individual RT treatment approach. Since positioning of ESTS patients can sometimes be troublesome, direct visualisation of the tumour by CBCT offers a significant advantage for target alignment before treatment and allows monitoring of therapy-induced changes during treatment. In patients with a GTV decrease, the PTV encompasses excess normal tissues with increasing normal tissue complication probability. In patients with a GTV increase, there is a risk of a geographical miss. These phenomena are only truly appreciated using 3D image-guided RT.
References
Suit HD, Mankin HJ, Wood WC, Proppe KH (1985) Preoperative, intraoperative, and postoperative radiation in the treatment of primary soft tissue sarcoma. Cancer 55(11):2659–2667
Wilson AN, Davis A, Bell RS, O’Sullivan B, Catton C, Madadi F, Kandel R, Fornasier VL (1994) Local control of soft tissue sarcoma of the extremity: the experience of a multidisciplinary sarcoma group with definitive surgery and radiotherapy. Eur J Cancer 30A(6):746–751
Yang JC, Chang AE, Baker AR, Sindelar WF, Danforth DN, Topalian SL, DeLaney T, Glatstein E, Steinberg SM, Merino MJ, Rosenberg SA (1998) Randomized prospective study of the benefit of adjuvant radiation therapy in the treatment of soft tissue sarcomas of the extremity. J Clin Oncol 16(1):197–203
O’Sullivan B et al (2002) Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 359(9325):2235–2241
Nielsen OS, Cummings B, O’Sullivan B, Catton C, Bell RS, Fornasier VL (1991) Preoperative and postoperative irradiation of soft tissue sarcomas: effect of radiation field size. Int J Radiat Oncol Biol Phys 21(6):1595–1599
Davis AM, O’Sullivan B, Turcotte R, Bell R, Catton C, Chabot P, Wunder J, Hammond A, Benk V, Kandel R, Goddard K, Freeman C, Sadura A, Zee B, Day A, Tu D, Pater J (2005) Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol 75(1):48–53
Dickie CI, Parent AL, Griffin AM, Fung S, Chung PW, Catton CN, Ferguson PC, Wunder JS, Bell RS, Sharpe MB, O’Sullivan B (2009) Bone fractures following external beam radiotherapy and limb-preservation surgery for lower extremity soft tissue sarcoma: relationship to irradiated bone length, volume, tumour location and dose. Int J Radiat Oncol Biol Phys 75(4):1119–1124
Gortzak Y, Lockwood GA, Mahendra A, Wang Y, Chung PW, Catton CN, O’Sullivan B, Deheshi BM, Wunder JS, Ferguson PC (2010) Prediction of pathologic fracture risk of the femur after combined modality treatment of soft tissue sarcoma of the thigh. Cancer 116(6):1553–1559
Jaffray DA, Siewerdsen JH, Wong JW, Martinez AA (2002) Flat-panel cone-beam computed tomography for image-guided radiation therapy. Int J Radiat Oncol Biol Phys 53(5):1337–1349
Fletcher CD, Unni K, Mertens F (2005) Pathology and genetics of tumours of soft tissue and bone, edn 5. WHO classification of tumours. IARC Press, Lyon
Coindre JM (2006) Grading of soft tissue sarcomas: review and update. Arch Pathol Lab Med 130(10):1448–1453
International Commission of Radiation Units and Measurements (2007). ICRU report 50/62. Prescribing, recording and reporting photon beam therapy. International Commission on Radiation Units and Measurements, Bethesda
Bel A, van Herk M, Bartelink H, Lebesque JV (1993) A verification procedure to improve patient set-up accuracy using portal images. Radiother Oncol 29(2):253–260
Chung PW, Deheshi BM, Ferguson PC, Wunder JS, Griffin AM, Catton CN, Bell RS, White LM, Kandel RA, O’Sullivan B (2009) Radiosensitivity translates into excellent local control in extremity myxoid liposarcoma: a comparison with other soft tissue sarcomas. Cancer 115(14):3254–3261
de Vreeze RS, de Jong D, Haas RL, Stewart F, van Coevorden F (2008) Effectiveness of radiotherapy in myxoid sarcomas is associated with a dense vascular pattern. Int J Radiat Oncol Biol Phys 72(5):1480–1487
Pitson G, Robinson P, Wilke D, Kandel RA, White L, Griffin AM, Bell RS, Catton CN, Wunder JS, O’Sullivan B (2004) Radiation response: an additional unique signature of myxoid liposarcoma. Int J Radiat Oncol Biol Phys 60(2):522–526
Engstrom K, Bergh P, Cederlund CG, Hultborn R, Willen H, Aman P, Kindblom LG, Meis-Kindblom JM (2007) Irradiation of myxoid/round cell liposarcoma induces volume reduction and lipoma-like morphology. Acta Oncol 46(6):838–845
Roberge D, Skamene T, Nahal A, Turcotte RE, Powell T, Freeman C (2010) Radiological and pathological response following preoperative radiotherapy for soft-tissue sarcoma. Radiother Oncol 97(3):404–407
Miki Y, Ngan S, Clark JCM, Akiyama T, Choong PFM (2010) The significance of size change of soft tissue sarcoma during preoperative radiotherapy. EJSO 36:678–683
Magierowski K, Moseley J, Lockwood G, Parent A, Euler C, Sharpe M, Griffin A, Brock K, Catton C, O’Sullivan B (2008) Retrospective study of volume changes in two pathological subtypes of sarcomas using deformation image registration. In: Proceedings of 14th Connective Tissue Oncology Society (CTOS) meeting.
Roberge D, Skamene T, Turcotte RE, Powell T, Saran N, Freeman C (2011) Inter- and intra-observer variation in soft-tissue sarcoma target definition. Cancer Radiother 15:421–425
Conflict of interest statement
The authors of this manuscript have no actual or potential conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Betgen, A., Haas, R.L.M. & Sonke, JJ. Volume changes in soft tissue sarcomas during preoperative radiotherapy of extremities evaluated using cone-beam CT. J Radiat Oncol 2, 55–62 (2013). https://doi.org/10.1007/s13566-012-0085-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-012-0085-0