Abstract
Background
Fatigue is one of the most common and distressing side-effects of breast cancer radiotherapy. According to current guidelines, accelerated partial breast irradiation (APBI) may be considered as an alternative treatment option for women with early-stage low-risk breast cancer. One method for APBI is single-dose intraoperative radiotherapy (IORT) applied directly to the tumor bed during breast conserving surgery (BCS). The COSMOPOLITAN trial therefore aims to analyze the intensity of fatigue following single-shot IORT with electrons (IOERT) compared to conventional hypofractionated whole breast irradiation (WBI) in low risk early breast cancer patients.
Methods
This trial is conducted as a multicenter, prospective, randomized, two-arm phase II study comparing the intensity of fatigue in early-stage breast cancer (cT1cN0cM0, tumor size < 2,5 cm, ER pos. Her2neu neg., age > 50 years) treated either with WBI or APBI after BCS. Secondary outcomes investigated are tumor control, overall survival (OS), disease-free survival (DFS), acute and chronic toxicity, quality of life (QoL) and cosmesis. A total of 202 patients will be randomized into two arms: Patients in arm A will receive WBI (40.05 Gy, 15 fractions) after surgical resection, while patients in arm B will receive IOERT (21 Gy to the 90%-isodose) during BCS. Fatigue will be assessed 12 weeks post surgery with the help of the Functional Assessment of Chronic Illness Therapy (FACIT) Fatigue Scale.
Discussion
The present trial aims to evaluate treatment response to compare single-shot intraoperative electron APBI to conventional WBI following BCS in early-stage low risk breast cancer patients. Fatigue is selected as the primary, patient-reported endpoint due its major clinical relevance.
Trial registration
The study is prospectively registered on February 12th, 2019: Clinicaltrials.gov, NCT03838419. “Intraoperative Electron Radiotherapy for Low-risk Early Breast Cancer (COSMOPOLITAN)”.
Study status
Ongoing study. Start of recruitment was December 2019.
Similar content being viewed by others
Background
Breast cancer is the most frequent cancerous disease in women [1, 2]. For patients with early stage breast cancer standard of care is breast conserving-surgery (BCS) followed by adjuvant radiotherapy and adjuvant systemic therapy according to the estrogen (ER) and progesterone receptor (PR) as well as human epidermal growth factor receptor 2 (HER2) status [1]. In several randomized controlled trials (RCTs) and meta-analyses, adjuvant whole-breast radiotherapy (WBI) after BCS has been shown to significantly decrease the risk of local (in-breast) recurrence and to improve breast-cancer mortality as well as OS [3, 4]. However, when selecting patients at a low a priori risk of local recurrence, only a small breast-cancer specific mortality benefit but no overall survival advantage was detected in the recent meta-analysis by the Early Breast Cancer Trialists Collaborative Group (EBCTCG) [4]. Consequently, several RCTs addressed the question whether the addition of adjuvant WBI to endocrine therapy improves the outcome of patients with early stage, low risk breast cancer [5,6,7,8,9]. Nevertheless, all of the individual trials detected a significant benefit for adjuvant WBI in terms of local control while no benefit for OS was found [5,6,7,8,9]. The effect of adjuvant WBI in addition to endocrine therapy was not limited to improved local control but also significantly improved DFS, as especially fewer axillary recurrences were reported in patients undergoing radiotherapy [6, 9]. This positive result was also confirmed after 10-year long term observation [10]. Thus, adjuvant WBI remains the standard of care after BCS in patients with early stage, low risk breast cancer.
As most of local recurrences occur in the proximity of the primary tumor bed, partial breast-irradiation delivered exclusively to the original tumor location has gained increased attention during the past couple of years [11,12,13]. Hereby, smaller target volumes allow for an increase in dose per fraction combined with a decrease in overall treatment time enabling accelerated partial breast irradiation (APBI). Several different techniques have been used to deliver APBI. Multicatheter brachytherapy has been one of the first techniques studied for APBI. 10-year results are available from a small single-center RCT and show comparable outcomes after WBI and APBI with multicatheter brachytherapy [14]. In 2016, 5-year results from a multi-center RCT conducted by the GEC-ESTRO have been published showing that APBI is non-inferior compared to WBI [15].
The probably most easily implementable approach for APBI is the application of percutaneous radiotherapy with a conventional linear accelerator as it is universally available. Besides some other studies, the IMPORT LOW-Trial compared partial-breast to whole-breast radiotherapy for low-risk early breast cancer using a standard external beam technique [16]. Five-year local recurrence rate were similar in all 3 arms and non-inferiority of the reduced dose-arm and the partial breast irradiation arm was shown [16]. Adverse events were comparable between the treatment arms with significantly fewer adverse effects in breast appearance and firmness in one or both of the experimental arms [16].
The ultimate form of APBI is single-dose IORT delivered exclusively to the tumor bed during BCS. Two large RCTs employing different techniques of IORT have been published so far: the ELIOT and the TARGIT-A-trial [17, 18]. Although, both trials presented promising results, significantly more local recurrences were detected in the IORT arms compared to standard WBI due to different shortcomings: While in the ELIOT-trial the inclusion criteria were non-restrictive resulting in the enrollment of a considerable number of patients with higher risk factors [18], the TARGIT-A trial also allowed the inclusion of patients who received IORT during a second operative procedure (post-pathology stratum), which impeded non-inferiority of results [18]. A meta-analysis of 5 RCTs comparing APBI to WBI was conducted by the TARGIT A-investigators [19]. While breast cancer-related mortality was similar, APBI resulted in a significant decrease of non-breast cancer-related mortality and a borderline significant improvement in OS when using a random-effects model [19]. Based on the above mentioned studies, both national guidelines in Germany, but also international guidelines suggest the use of APBI in patients with early stage, low risk breast cancer [1, 2, 20, 21]. Nevertheless, most guidelines recommend the application of APBI preferably within a clinical trial [1, 21].
Fatigue is one of the most common and distressing side-effects reported by breast cancer patients and occurs in more than 80% of patients during radiotherapy [22,23,24,25,26,27]. During the course of radiotherapy, fatigue usually increases, but typically subsides within weeks after the end of radiation treatment [24, 28]. However, in up to 40% of cases, it can persist long after the completion of therapy [29,30,31]. Fatigue is usually described as a general physical or mental exhaustion that negatively affects QoL due to functional disability and psychological distress [28, 32]. Psychosocial problems like fatigue, depression or cognitive limitations in occupationally active cancer survivors are distinctly associated with problems at work [33]. The potential economic impact of fatigue is considerably high: 75% of patients and 40% of caregivers are forced to change their employment status due to cancer-related fatigue [34, 35]. A recent study about employment participation in early-breast cancer patients further highlighted the enormous socioeconomic impact of fatigue by showing that fatigue patients were more likely to experience diminished employment after 2 years of follow-up [36].
Previous analyses reported that the level of fatigue rises with cumulative radiation dose and might be related to the duration of treatment [37, 38]. Both, total doses as well as field sizes are known to influence severity of fatigue [38,39,40]. For APBI the target volume only includes the former tumor cavity and not the whole breast tissue and total treatment time is usually reduced compared to WBI. Hence, early stage breast cancer patients treated with APBI instead of WBI are expected to recover faster from cancer-related fatigue leading to improved QoL compared to patients receiving WBI.
The aim of the present trial is to compare single-shot intraoperative APBI with electrons to standard hypofractionated WBI for patients with low-risk early stage breast cancer. Due to its high socio-economic and clinical impact fatigue is chosen as the primary, patient-reported endpoint for this study.
Methods/design
Trial aim
The purpose of this trial is to analyze intensity of fatigue in early-stage breast cancer treated with WBI or APBI after BCS. We propose that patients treated with APBI have lower fatigue levels after radiotherapy based on the FACIT Fatigue Assessment Questionnaire compared with patients treated with standard WBI.
Trial design
The COSMOPOLITAN trial is a multicenter, prospective, randomized, two-arm phase II study. The trial has been designed by the study initiators at the Department of Radiation Oncology of the University of Heidelberg. The trial is carried out at the University of Heidelberg, Department of Radiation Oncology and at the Helios Hospital Berlin-Buch, Department of Radiation Oncology. The inclusion of further study sites is planned. A list of study sites can be obtained from the corresponding author on reasonable request. The University of Heidelberg is responsible for trial management and coordination, as well as quality assurance including reporting, monitoring and database management. The current version of the study protocol is version 1.1 from January, 24th 2019 (supplementary material 1). The study workflow and treatment arms are depicted in Fig. 1. Two-hundred-and-two women with early stage, low risk breast cancer eligible for breast-conserving surgery fulfilling the inclusion criteria will be enrolled in this phase II clinical trial.
Inclusion criteria
Patients meeting the following criteria will be included in the trial:
-
Histologically confirmed invasive breast cancer
-
Total tumor size < 2.5 cm
-
cN0
-
Estrogen receptor positive, HER2-negative on immunohistochemistry
-
Age ≥ 50 years
-
ECOG Performance status ≤2
-
Ability of subject to understand character and individual consequences of the clinical trial
-
Written informed consent (must be available before enrolment in the trial)
Exclusion criteria
Patients presenting with one of the following criteria will not be included in the trial:
-
G3
-
Extensive microcalcifications
-
Invasive lobular carcinoma
-
Clinically involved lymph nodes
-
No invasive axillary lymph node staging planned
-
Patients with significant mental or physical comorbidities that preclude regular follow-up
-
Neoadjuvant chemotherapy or neoadjuvant endocrine therapy
-
Previous radiotherapy of the breast
-
Known carcinoma < 5 years ago (excluding Carcinoma in situ of the cervix, basal cell carcinoma, squamous cell carcinoma of the skin) requiring immediate treatment interfering with study therapy
-
Pregnant or lactating women
-
Participation in another competing clinical study or observation period of competing trials
Patients are withdrawn from the study, if a R1/2 resection status is diagnosed postoperatively. In this case, re-resection and additional whole-breast irradiation should be taken into account.
Randomization
After meeting eligibility criteria, 202 patients will be randomly assigned to intraoperative APBI or WBI. Appropriate patients will be allocated in a concealed fashion in a 1:1 ratio by means of randomization using a centralized web-based tool (www.randomizer.at), to achieve comparable intervention groups. Randomization will be stratified with respect to invasive tumor size (≤ 1 cm3, > 1 cm3) and age (≤ 60 years, > 60 years). Block randomization with varying block lengths will be performed to achieve in total equal group sizes.
Study treatment
Arm A - conventional arm
WBI with a total dose to the breast of 40.05 Gy in 15 fractions is administered after full recovery from surgical resection.
Arm B - experimental arm
During BCS, patients will receive IOERT with a total dose of 21 Gy prescribed to the 90%-isodose.
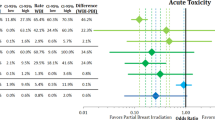
Trial objectives
The primary objective is the assessment of fatigue from baseline (before treatment start) compared to 12 weeks after treatment start as assessed by the FACIT Fatigue Assessment Questionnaire. Secondary outcomes investigated are local tumor control in the index quadrant of the breast and in the ipsilateral breast (time from randomization until local tumor progression, death without prior local progression, or end of follow-up at the respective site), regional tumor control (time from randomization until occurrence of regional lymph node metastases, death without prior regional tumor progression, or end of follow-up), distant tumor control (time from randomization until occurrence of distant metastases, death without prior distant progression, or end of follow-up), OS (time from randomization until death or end of follow-up), DFS (time from randomization until the first occurrence of local recurrence, regional lymph node metastases, distant metastases, tumor-related death, death without prior progression, or end of follow-up), secondary malignancies, acute and chronic toxicity, QoL and cosmesis. Toxicity, cosmesis and QoL assessment are performed according to international validated scores and questionaires (Table 2). Fatigue at 5 weeks after treatment start (T1) will be evaluated in both study groups as secondary endpoint to assess the potential influence of IORT on fatigue. Additionally, the Prosigna/PAM50-assay will be applied to further evaluate the potential prognostic impact of tumor biology and gene expression-analysis in supporting adequate patient selection.
Treatment planning and radiation therapy
Arm A
Radiotherapy is administered after full recovery from surgical resection, usually after 5 weeks of BCS. Patients will receive computed tomography-based 3-dimensional treatment planning. The total dose to the breast is 40.05 Gy in 15 fractions. No tumor bed boost or regional nodal irradiation shall be delivered.
Target contouring of the CTV-breast is performed according to the ESTRO-guidelines [41, 42]. An additional margin for inter- and intrafractional positioning uncertainties of 5–10 mm is added to generate the PTV-breast. The PTV-breast_EVAL (generated by subtraction of the 3 mm below the skin from the PTV-breast) should receive 95–107% of the prescribed dose. Dose constraints of normal tissue will be respected according to Table 1.
Physical Quality assurance (QA) is not defined in the protocol, but is done according to standard operating procedures of the resepctive study centers. At Heidelberg University, for the standard arm of the COSMOPOLITAN trial, both 3D-conformal radiotherapy (3-D-CRT) and intensity-modulated radiotherapy (IMRT) are used. For QA, secondary dose calculations are performed with a Monte Carlo algorithm for the IMRT plans, while simpler algorithms are applied for the 3-D-CRT plans. IMRT plans are intermittently measured.
Arm B
Patients will receive IOERT with a total dose of 21 Gy prescribed to the 90%-isodose. After resection of the tumor, a lead or aluminum shield will be inserted between the back side of the breast tissue and the anterior part of the major pectoralis muscle to protect the thoracic wall. The resection margins are sutured over the shield according to the instructions by Veronesi et al. [43]. An appropriate size and shape of the tube will be selected, taking into account the tumor size, the size of the treated breast and the potential effect on cosmesis. However, the minimum tube size shall be at least 4 cm, in order to create a 2 cm safety margin around the sutured resection margins of the tumor bed. The disk diameter of the shield will be at least 1.5 cm larger than the chosen tube size. The linear accelerator delivers electrons at variable energies (6, 9 and 12 MeV). Depending on the target thickness the adequate electron energy is chosen.
Follow up
The baseline Visit will be performed after enrolment of the patient into the study and will be scheduled − 7 to − 1 day before planned treatment start. During the baseline visit (T0) a clinical assessment as well as analysis of QoL including fatigue is scheduled. Patients will also receive photographic documentation in standardized patient positions for cosmetic assessment: Two frontal photographs (one with the arms raised above the head and the other with both arms alongside the body) and one profile photograph of the treated breast (arms raised) will be taken.
Both study groups will be evaluated after BCS at 5 weeks after treatment start (T1), to assess the potential influence of IORT on fatigue (secondary endpoint). In group A this time point corresponds to 5 weeks after BCS, just before the start of RT; in group B this corresponds to 5 weeks after BCS incl. IORT.
The second, third, fourth and fifth study visits (T2-T5) are planned 12 weeks (primary endpoint), 6 months, 2 and 5 years (secondary endpoints) after the treatment start. These visits will include a clinical assessment as well as analysis of QoL including fatigue (EORTC and Fatigue Assessment Questionnaires, BREAST-Q and BCTOS, see below for details). Photographic assessment of cosmetic results is also planned except for the last visit after 5 years. The follow-up workflow is depicted in Table 2.
Outcome measures
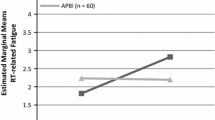
Primary endpoint: fatigue testing
The primary endpoint is change of fatigue after APBI or WBI from baseline to 12 weeks after treatment start (T2 vs. T0). Fatigue will be assessed with the help of the Functional Assessment of Chronic Illness Therapy (FACIT) Fatigue Scale, which consists of a 13-item multidimensional self-assessment form evaluating quantity of fatigue and distress [44]. The FACIT Fatigue Scale is extensively applied in cancer patients [45, 46]. Using the FACIT Fatigue Scale questionnaire, patients are asked to indicate how frequent each item was for them “during the past 7 days” applying a 5-point scale (“not at all” to “very much”). The range of possible scores is 0–52, with 0 being the worst possible score and 52 the best.
Secondary endpoints
Secondary analysis include local tumor control, regional and distant recurrence rates, disease-free as well as overall survival, assessment of acute and chronic toxicity (CTCAE v5.0), QoL (EORTC QLQ-C30, BREAST-Q BCS [47, 48], BCTOS-12 [49]) and cosmesis. Cosmesis will be evaluated according to the proposed method by Vrieling et al. [50]. Additionally, there will be a cosmesis assessment by both the treating physician and the patient. Furthermore, gene expression analysis using the Prosigna/PAM50-assay will be performed on the operatively resected tumor tissue as a secondary endpoint to evaluate the potential prognostic/predictive impact on choice of radiotherapy modality [51, 52].
The BREAST-Q questionnaire is a validated survey instrument especially developed for patients undergoing breast surgery. An extra BREAST-Q BCS module exists, which is specifically designed for patients undergoing BCS measuring QoL and satisfaction [47, 48]. Both of these topics are divided into three subscales i.e., QOL: physical, psychosocial and sexual well-being; Satisfaction: satisfaction with cosmetic outcome (breast appearance), satisfaction with overall outcome and satisfaction with care. Patients are asked to rate each item question on a four-point scale. The BREAST-Q is separated into a pre- and post-surgery version.
The Breast Cancer Treatment outcome scale (BCTOS-12) contains 12 items, which are assigned to two internally consistent subscales: [49] 1) Functional Status (e.g. change in shoulder mobility etc.), 2) Aesthetic Status (e.g. shape of the breast etc.). Patients are instructed to rate each item of the BCTOS-12 on a four-point scale evaluating the differences between the treated and the untreated breast (1 = no difference, 4 = large difference). The score for each subscale is the mean of the ratings over all items belonging to that subscale. A higher score reflects a poorer status (i.e. a larger difference between the treated and the untreated breast).
Statistical analysis
Hypotheses
The null hypothesis to be tested states that the change in the FACIT-Fatigue score, between baseline and week 12 after treatment start is equal for both groups. This hypothesis will be tested at a two-sided level of significance of α= 0.05 against the alternative hypothesis.
Sample size calculation
The sample size calculation is based on the primary endpoint change of fatigue from baseline to week 12 after Treatment start (study visit T2) between the groups APBI and WBI measured via the FACIT-Fatigue score. An improvement in 6 of 13 items by one point is considered clinically relevant resulting in a clinically relevant effect size of 6 points. Assuming a standard deviation of 12 [53] and with a type I error rate of α = 0.05 (two-sided), a two sample t-test requires a total sample size of n = 172 patients (86 per group) to achieve a power of 1 − β = 0.90 for revealing an effect of 6 points. Adjusting for the covariates baseline fatigue, age, and tumor size in a linear model is assumed to yield less unexplained variance and thus to an additionally increased power. Taking a dropout rate of 15% percent into account, n = 202 patients need to be randomized. Sample size calculation was carried out using ADDPLAN v 6.1.
Analysis methods
The full analysis set (FAS) includes all randomized patients and they will be analyzed according to the intention-to-treat (ITT) principle. In addition to the evaluation of the FAS, a per-protocol population (PP) analysis will be performed as a sensitivity analysis. The hypothesis test will be conducted using a linear model with the dependent variable “change in FACT-F score between baseline and week 12 after treatment start” and the independent factors treatment group (A/B), baseline FACT-F score, tumor size, and age. The effect will be calculated alongside a 95% confidence interval. Missing data for the primary outcome variable will be replaced using multiple imputation [54] taking the covariates treatment group, baseline FACT-F score, tumor size, and age into account by application of the fully conditional specification method [55]. In addition to the evaluation of the FAS, a PP analysis will be performed as a sensitivity analysis. The secondary outcomes will be analyzed descriptively by tabulation of the measures of the empirical distributions. According to the scale level of the variables, means, standard deviations, medians, 1st and 3rd quartiles as well as minimum and maximum or absolute and relative frequencies, respectively, will be reported. Further, for the secondary endpoints OS, DFS, local, regional, and distant tumor control, a Kaplan-Meier analysis will be performed and a between-groups comparison via a descriptive log-rank test will be conducted. Adverse and Serious Adverse Events will be tabulated and absolute and relative frequencies with 95% confidence intervals will be calculated. The severity and the relationship to the treatment will be given. Possible differences between the treatment groups will be tested using the chi-squared test. Descriptive p-values of the corresponding statistical tests comparing the treatment groups and associated 95% confidence intervals will be given. Further exploratory analyses will be performed to identify subgroups and potential moderator variables of patients profiting distinctly from the investigated interventions. Analyses will be conducted using SAS v9.4 (SAS Institute, Cary, NC).
Discussion
As studies investigating APBI are still scarce, current international and German guidelines suggest the use of APBI for low-risk early stage breast cancer patients but recommend the application of APBI preferably within a clinical trial [1, 2, 21]. Two recent RCTs analyzed the role of intraoperative single-shot APBI for early-stage low-risk breast cancer patients: the ELIOT and the TARGIT-A-trial [17, 18]. However, the results of both studies were impaired by limitations in selecting adequate patients.
On the one hand, the TARGIT-A trial compared single-shot 20 Gy of 50 kV-IORT with 50 Gy of WBI in 25 fractions and reported an increased 5-year local recurrence rate of 3.3% for the IORT-arm vs. 1.3% for WBI-arm, which was still acceptable within the predefined threshold level (p = 0.042). However, the borderline increased local recurrence rate for the IORT-arm was attributed to the inclusion of patients in whom IORT was delivered as a delayed second procedure by reopening the lumpectomy cavity (postpathology stratum). While local recurrence was 2.1% with IORT and 1.1% with WBI in the prepathology stratum (p = 0.31), the local recurrence rate rose to 5.4% for IORT and 1.7% for WBI in the postpathology stratum (p = 0.069), which was higher than the pre-specified non-inferiority margin of 2·5% at 5 years. This particularly important result underlines the need for concomitant delivery of intraoperative radiotherapy and lumpectomy [56].
On the other hand, the ELIOT-trial compared one dose of 21 Gy of IOERT to WBI with 50 Gy and a tumor bed boost over 6 weeks and described an increased 5-year local recurrence rate of 4.4% for patients receiving IORT and 0.4% for patients treated with WBI (p = 0·0001), which was still below the pre-specified equivalence margin of 7.5% [18]. However, the trial also included less suitable patients with risk factors such as tumor size > 2 cm, tumor grade G3, positive nodes, and triple-negative tumors. After excluding these patients with risk factors, the 5-year local recurrence rate decreased to only 1.5% in the IORT-arm. Based on the above mentioned results, inclusion criteria will be highly restrictive in the COSMOPOLITAN trial. The ASTRO has recently published selection criteria for APBI, which will be used for guaranteeing that only low-risk early-breast cancer patients will be treated with APBI in the current trial [20].
Due to its considerably high socio-economic and clinical impact fatigue is chosen as the primary, patient-reported endpoint for this study [34, 35]. Few first and mainly retrospective studies with small patient numbers reported lower levels of acute fatigue in breast cancer patients receiving APBI instead of WBI [40, 45, 57]. Perez et al. retrospectively evaluated side-effects and QoL following WBI vs. APBI for early-stage low-risk cancer and described significantly reduced severity of fatigue besides other factors after APBI compared to WBI [57]. In a matched-pair analysis, Taunk et al. retrospectively compared radiation-induced fatigue in patients treated with APBI or hypofractionated WBI to patients receiving normofractionated WBI [40]. During radiotherapy and the first follow-up visit, significantly lower fatigue levels were detected for patients in the APBI group [40]. A pilot study by Albuquerque et al. evaluated the impact of partial versus whole breast irradiation on fatigue, perceived stress, QoL and natural killer cell activity in 30 women with breast cancer and supported the above mentioned findings by reporting that partial breast irradiation results in more rapid recovery from cancer-related fatigue compared to WBI [45]. Furthermore, the GEC-ESTRO study group recently investigated QoL following APBI with interstitial brachytherapy and described significantly reduced fatigue after APBI compared to WBI [58].
The primary goal of the COSMOPOLITAN study is to show that BCS followed by APBI with electrons results in a significantly better tolerability of adjuvant radiotherapy in terms of fatigue compared to BCS followed by hypofractionated WBRT. Fatigue is a major side effect of cancer treatments and is a main contributor to long-term quality of life-impairment as well as unemployment [32, 34,35,36]. The prognosis of women with early stage, low risk breast cancer is excellent and the risk of local recurrence after BCS has been shown to be in the range of 1–2% at 5 years after diagnosis [59]. Thus, maintaining a high QoL and minimizing morbidity and mortality of adjuvant treatment is crucial.
Availability of data and materials
The data is collected, managed and processed electronically in the in-house research database. To ensure data quality and consistency, internal quality control measures will be carried out. The originals of all central study documents are kept at the Study Center for at least 15 years after the final report has been prepared. The dataset used and analyzed during the current study will be available from the corresponding author on reasonable request. Regulatory authorities may request access to all source documents, CRF and other trial documentation.
Abbreviations
- 3-D-CRT:
-
3D-conformal radiotherapy
- AE:
-
Adverse Events
- AMG:
-
German Drug Law (Deutsches Arzneimittelgesetz)
- APBI:
-
Accelerated partial breast irradiation
- ASTRO:
-
American Society for Therapeutic Radiology and Oncology
- BCS:
-
Breast conserving-surgery
- BDSG:
-
Bundesdatenschutzgesetz
- BRA:
-
Breast retraction assessment
- CHT:
-
Chemotherapy
- CRF:
-
Case Report Form
- CT:
-
Computer tomography
- CTCAE:
-
Common Toxicity Criteria for Adverse Events
- CTV:
-
Clinical target volume
- DFS:
-
Disease-free survival
- DSGVO:
-
Datenschutzgrundverordnung, General Data Protection Regulation
- DVH:
-
Dose volume histogram
- EC:
-
Ethics Committee
- ER:
-
Estrogen receptor
- FDA:
-
US Food and Drug Administration
- FSI:
-
First Subject In
- GCP:
-
Good Clinical Practice
- Gy:
-
Gray
- HIRO:
-
Heidelberger Institut für Radioonkologie
- IMRT:
-
Intensity-modulated radiotherapy
- IOERT:
-
Intraoperative electron radiotherapy
- IORT:
-
Intraoperative radiotherapy
- ISF:
-
Investigator Site File
- ISRCTN:
-
International Standard Randomised Controlled Trial Number
- IT:
-
Information technology
- ITT:
-
Intention-to-treat
- KPS:
-
Karnofsky Performance Score
- LPI:
-
Last Patient In
- LPO:
-
Last Patient Out
- OS:
-
Overall survival
- PI:
-
Principle investigator
- pBRA:
-
Percentage BRA
- PP:
-
Per protocol
- PR:
-
Progesterone receptor
- PTV:
-
Planning target volume
- QA:
-
Quality assurance
- QoL:
-
Quality of Life
- RCT:
-
Randomized controlled trials
- Ref:
-
Reference length
- RT:
-
Radiation therapy
- RTOG:
-
Radiation Therapy Oncology Group
- SAE:
-
Severe adverse events
- SOP:
-
Standard operating procedures
- TS:
-
Treatment start
- WBI:
-
Whole-breast radiotherapy
References
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, D.K., AWMF):. S3-Leitlinie Früherkennung, Diagnose, Therapie und Nachsorge des Mammakarzinoms. Version 4.0, AWMF Registernummer: 032-045OL 2017; Available from: http://www.leitlinienprogramm-onkologie.de/leitlinien/mammakarzinom/.
Liedtke C, Thill M, Jackisch C, Thomssen C, Müller V, Janni W. AGO recommendations for the diagnosis and treatment of patients with early breast Cancer: update 2017. Breast Care. 2017;12(3):172–83.
Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans V, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366(9503):2087–106.
Early Breast Cancer Trialists’ Collaborative, Darby GS, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378(9804):1707–16.
Blamey RW, Bates T, Chetty U, Duffy SW, Ellis IO, George D, et al. Radiotherapy or tamoxifen after conserving surgery for breast cancers of excellent prognosis: British Association of Surgical Oncology (BASO) II trial. Eur J Cancer. 2013;49(10):2294–302.
Fyles AW, McCready DR, Manchul LA, Trudeau ME, Merante P, Pintilie M, et al. Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast Cancer. N Engl J Med. 2004;351(10):963–70.
Hughes KS, Schnaper LA, Bellon JR, Cirrincione CT, Berry DA, McCormick B, et al. Lumpectomy plus Tamoxifen with or without irradiation in women age 70 years or older with early breast Cancer: long-term follow-up of CALGB 9343. J Clin Oncol. 2013;31(19):2382–7.
Kunkler IH, Williams LJ, Jack WJL, Cameron DA, Dixon JM. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. Lancet Oncol. 2015;16(3):266–73.
Pötter R, Gnant M, Kwasny W, Tausch C, Handl-Zeller L, Pakisch B, et al. Lumpectomy plus tamoxifen or anastrozole with or without whole breast irradiation in women with favorable early breast cancer. Int J Radiat Oncol Biol Phys. 2007;68(2):334–40.
Fastner G, Sedlmayer F, Widder J, Metz M, Geinitz H, Kapp K, et al. Endocrine therapy with or without whole breast irradiation in low-risk breast cancer patients after breast-conserving surgery: 10-year results of the Austrian breast and colorectal Cancer study group 8A trial. Eur J Cancer. 2020;127:12–20.
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing Total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast Cancer. N Engl J Med. 2002;347(16):1233–41.
Mannino M, Yarnold JR. Local relapse rates are falling after breast conserving surgery and systemic therapy for early breast cancer: can radiotherapy ever be safely withheld? Radiother Oncol. 2009;90(1):14–22.
Salvadori B, Marubini E, Miceli R, Conti AR, Cusumano F, Andreola S, et al. Reoperation for locally recurrent breast cancer in patients previously treated with conservative surgery. Br J Surg. 1999;86(1):84–7.
Polgar C, Fodor J, Major T, Sulyok Z, Kasler M. Breast-conserving therapy with partial or whole breast irradiation: ten-year results of the Budapest randomized trial. Radiother Oncol. 2013;108(2):197–202.
Strnad V, Ott OJ, Hildebrandt G, Kauer-Dorner D, Knauerhase H, Major T, et al. 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. Lancet. 2016;387(10015):229–38.
Coles CE, Griffin CL, Kirby AM, Titley J, Agrawal RK, Alhasso A, et al. Partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. Lancet. 2017;390(10099):1048–60.
Vaidya JS, Joseph DJ, Tobias JS, Bulsara M, Wenz F, Saunders C, et al. Targeted intraoperative radiotherapy versus whole breast radiotherapy for breast cancer (TARGIT-A trial): an international, prospective, randomised, non-inferiority phase 3 trial. Lancet. 2010;376(9735):91–102.
Veronesi U, Orecchia R, Maisonneuve P, Viale G, Rotmensz N, Sangalli C, et al. Intraoperative radiotherapy versus external radiotherapy for early breast cancer (ELIOT): a randomised controlled equivalence trial. Lancet Oncol. 2013;14(13):1269–77.
Vaidya JS, Bulsara M, Wenz F, Coombs N, Singer J, Ebbs S, et al. Reduced mortality with partial-breast irradiation for early breast cancer: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys. 2016;96(2):259–65.
Correa C, Harris EE, Leonardi MC, Smith BD, Taghian AG, Thompson AM, et al. Accelerated partial breast irradiation: executive summary for the update of an ASTRO evidence-based consensus statement. Pract Radiat Oncol. 2017;7(2):73–9.
Salerno KE. NCCN guidelines update: evolving radiation therapy recommendations for breast Cancer. J Natl Compr Cancer Netw. 2017;15(5S):682–4.
Bower JE. Prevalence and causes of fatigue after cancer treatment: the next generation of research. J Clin Oncol. 2005;23(33):8280–2.
Bower JE. Cancer-related fatigue—mechanisms, risk factors, and treatments. Nat Rev Clin Oncol. 2014;11:597.
Geinitz H, Zimmermann FB, Stoll P, Thamm R, Kaffenberger W, Ansorg K, et al. Fatigue, serum cytokine levels, and blood cell counts during radiotherapy of patients with breast cancer. Int J Radiat Oncol Biol Phys. 2001;51(3):691–8.
Montgomery GH, David D, Kangas M, Green S, Sucala M, Bovbjerg DH, et al. Randomized controlled trial of a cognitive-behavioral therapy plus hypnosis intervention to control fatigue in patients undergoing radiotherapy for breast cancer. J Clin Oncol. 2014;32(6):557–63.
Potthoff K, Schmidt ME, Wiskemann J, Hof H, Klassen O, Habermann N, et al. Randomized controlled trial to evaluate the effects of progressive resistance training compared to progressive muscle relaxation in breast cancer patients undergoing adjuvant radiotherapy: the BEST study. BMC Cancer. 2013;13:162.
Tavio M, Milan I, Tirelli U. Cancer-related fatigue (review). Int J Oncol. 2002;21(5):1093–9.
Schmidt ME, Chang-Claude J, Vrieling A, Heinz J, Flesch-Janys D, Steindorf K. Fatigue and quality of life in breast cancer survivors: temporal courses and long-term pattern. J Cancer Surviv. 2012;6(1):11–9.
Bower JE, Ganz PA, Desmond KA, Bernaards C, Rowland JH, Meyerowitz BE, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106(4):751–8.
Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18(4):743–53.
Noal S, Levy C, Hardouin A, Rieux C, Heutte N, Ségura C, et al. One-year longitudinal study of fatigue, cognitive functions, and quality of life after adjuvant radiotherapy for breast cancer. Int J Radiat Oncol Biol Phys. 2011;81(3):795–803.
Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, et al. Cancer-related fatigue, version 2.2015. J Natl Compr Cancer Netw. 2015;13(8):1012–39.
Duijts SF, van Egmond MP, Spelten E, van Muijen P, Anema JR, van der Beek AJ. Physical and psychosocial problems in cancer survivors beyond return to work: a systematic review. Psychooncology. 2014;23(5):481–92.
Curt, G.A., Fatigue in cancer. Like pain, this is a symptom that physicians can and should manage, 2001. 322(7302): p. 1560.
Curt GA, Breitbart W, Cella D, Groopman JE, Horning SJ, Itri LM, et al. Impact of Cancer-related fatigue on the lives of patients: new findings from the fatigue coalition. Oncologist. 2000;5(5):353–60.
Ekenga CC, Perez M, Margenthaler JA, Jeffe DB. Early-stage breast cancer and employment participation after 2 years of follow-up: a comparison with age-matched controls. Cancer. 2018;124(9):2026–35.
Hickok JT, Morrow GR, Roscoe JA, Mustian K, Okunieff P. Occurrence, severity, and longitudinal course of twelve common symptoms in 1129 consecutive patients during radiotherapy for Cancer. J Pain Symptom Manag. 2005;30(5):433–42.
Schwartz AL, Nail LM, Chen S, Meek P, Barsevick AM, King ME, et al. Fatigue patterns observed in patients receiving chemotherapy and radiotherapy. Cancer Investig. 2000;18(1):11–9.
Beard CJ, Propert KJ, Rieker PP, Clark JA, Kaplan I, Kantoff PW, et al. Complications after treatment with external-beam irradiation in early-stage prostate cancer patients: a prospective multiinstitutional outcomes study. J Clin Oncol. 1997;15(1):223–9.
Taunk NK, Haffty BG, Chen S, Khan AJ, Nelson C, Pierce D, et al. Comparison of radiation-induced fatigue across 3 different radiotherapeutic methods for early stage breast cancer. Cancer. 2011;117(18):4116–24.
Offersen BV, Boersma LJ, Kirkove C, Hol S, Aznar MC, Biete Sola A, et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer. Radiother Oncol. 2015;114(1):3–10.
Offersen BV, Boersma LJ, Kirkove C, Hol S, Aznar MC, Sola AB, et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer, version 1.1. Radiother Oncol. 2016;118(1):205–8.
Veronesi U, Gatti G, Luini A, Intra M, Orecchia R, Borgen P, et al. Intraoperative radiation therapy for breast cancer: technical notes. Breast J. 2003;9(2):106–12.
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the functional assessment of Cancer therapy (FACT) measurement system. J Pain Symptom Manag. 1997;13(2):63–74.
Albuquerque K, Tell D, Lobo P, Millbrandt L, Mathews HL, Janusek LW. Impact of partial versus whole breast radiation therapy on fatigue, perceived stress, quality of life and natural killer cell activity in women with breast cancer. BMC Cancer. 2012;12:251.
Cella D, Lai J-s, Chang C-H, Peterman A, Slavin M. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94(2):528–38.
Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124(2):345–53.
Pusic AL, Lemaine V, Klassen AF, Scott AM, Cano SJ. Patient-reported outcome measures in plastic surgery: use and interpretation in evidence-based medicine. Plast Reconstr Surg. 2011;127(3):1361–7.
Hennigs A, Heil J, Wagner A, Rath M, Moosbrugger H, Kelava A, et al. Development and psychometric validation of a shorter version of the breast Cancer treatment outcome scale (BCTOS-12). Breast. 2018;38:58–65.
Vrieling C, Collette L, Bartelink E, Borger JH, Brenninkmeyer SJ, Horiot J-C, et al. Validation of the methods of cosmetic assessment after breast-conserving therapy in the EORTC “boost versus no boost” trial. Int J Radiat Oncol Biol Phys. 1999;45(3):667–76.
Prosigna™ Breast Cancer Prognostic Gene Signature Assay [Package Insert]. Seattle: NanoString Technologies, Inc.; 2013. Available from:http://prosigna.com/docs/Prosigna_Packet_Insert_US.pdf.
Nielsen T, Wallden B, Schaper C, Ferree S, Liu S, Gao D, et al. Analytical validation of the PAM50-based Prosigna breast Cancer prognostic gene signature assay and nCounter analysis system using formalin-fixed paraffin-embedded breast tumor specimens. BMC Cancer. 2014;14:177.
Moadel AB, Shah C, Wylie-Rosett J, Harris MS, Patel SR, Hall CB, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: effects on quality of life. J Clin Oncol. 2007;25(28):4387–95.
van Buuren S. Flexible Imputation of Missing Data. Boca Raton: Chapman & Hall/CRC; 2012.
van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16(3):219–42.
Vaidya JS, Wenz F, Bulsara M, Tobias JS, Joseph DJ, Keshtgar M, et al. Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-A randomised trial. Lancet. 2014;383(9917):603–13.
Perez M, Schootman M, Hall LE, Jeffe DB. Accelerated partial breast irradiation compared with whole breast radiation therapy: a breast cancer cohort study measuring change in radiation side-effects severity and quality of life. Breast Cancer Res Treat. 2017;162(2):329–42.
Schafer R, Strnad V, Polgar C, Uter W, Hildebrandt G, Ott OJ, et al. Quality-of-life results for accelerated partial breast irradiation with interstitial brachytherapy versus whole-breast irradiation in early breast cancer after breast-conserving surgery (GEC-ESTRO): 5-year results of a randomised, phase 3 trial. Lancet Oncol. 2018;19(6):834–44.
Matuschek C, Bolke E, Haussmann J, Mohrmann S, Nestle-Kramling C, Gerber PA, et al. The benefit of adjuvant radiotherapy after breast conserving surgery in older patients with low risk breast cancer- a meta-analysis of randomized trials. Radiat Oncol. 2017;12(1):60.
Acknowledgements
Not applicable.
Funding
The trial is financed using funds of the Department of Radiation Oncology at University Hospital of Heidelberg. According to the research agreement of our clinic with IntraOP Medical, this trial is financially supported by IntraOP Medical, 570 Del Rey Avenue, Sunnyvale, CA 94085. IntraOP Medical is not involved in the design of the study, nor the collection, storage or analysis of the data gathered in this study.
Author information
Authors and Affiliations
Contributions
JHR, CJ and JD planned the study. JHR, TF, SA, DK, RK, AH, JH, MU, MFH, LK, SH, DB, CS and SAK are responsible for patient recruitment. MU, MFH, LK, SH and SAK perform planning and radiation therapy. RB and JK perform biometric and statistical analysis. Medical care and follow up is provided by JHR, TF and LK. TF and JHR drafted the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The final study protocol was approved by the ethics committee of the Medical Faculty of Heidelberg University (S-826/2018). In the clinical study, no ionizing radiation in humans for the purpose of medical research will be used, since all treatments within this protocol are clinically indicated and performed within the medical responsibility of the participating centers and only clinically established therapies and diagnostics are used. Therefore, concerning radiation protection law (StrSchV), the authors of this protocol presume that a submission to the Bundesamt für Strahlenschutz (BfS) is not required. To confirm this position, the investigators submitted this protocol to the expert commission of the German Society of Radiation Oncology (DEGRO). This study complies with the Helsinki Declaration and its recent German version, the Medical Association code of conduct, the principles of Good Clinical Practice (GCP) and the Federal Data Protection Act. The trial will be carried out in keeping with local legal and regulatory requirements. Each patient must provide written informed consent for participation in the study and for publication before enrollment.
Consent for publication
Not applicable.
Competing interests
This trial is financially supported by IntraOP Medical, 570 Del Rey Avenue, Sunnyvale, CA 94085. IntraOP Medical is not involved in the design of the study, nor the collection, storage or analysis of the data gathered in this study. All authors declare that there is no conflict of interest in connection with the implementation and evaluation of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Supplementary material 1: Current version of the study protocol, version 1.1 from January, 24th 2019.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Forster, T., Jäkel, C., Akbaba, S. et al. Fatigue following radiotherapy of low-risk early breast cancer – a randomized controlled trial of intraoperative electron radiotherapy versus standard hypofractionated whole-breast radiotherapy: the COSMOPOLITAN trial (NCT03838419). Radiat Oncol 15, 134 (2020). https://doi.org/10.1186/s13014-020-01581-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-020-01581-9