Abstract
Background
Germline genetic testing is recommended by the National Comprehensive Cancer Network (NCCN) for individuals including, but not limited to, those with a personal history of ovarian cancer, young-onset (< 50 years) breast cancer, and a family history of ovarian cancer or male breast cancer. Genetic testing is underused overall, and rates are consistently lower among Black and Hispanic populations. Behavioral economics-informed implementation strategies, or nudges, directed towards patients and clinicians may increase the use of this evidence-based clinical practice.
Methods
Patients meeting eligibility for germline genetic testing for breast and ovarian cancer will be identified using electronic phenotyping algorithms. A pragmatic cohort study will test three sequential strategies to promote genetic testing, two directed at patients and one directed at clinicians, deployed in the electronic health record (EHR) for patients in OB-GYN clinics across a diverse academic medical center. We will use rapid cycle approaches informed by relevant clinician and patient experiences, health equity, and behavioral economics to optimize and de-risk our strategies and methods before trial initiation. Step 1 will send patients messages through the health system patient portal. For non-responders, step 2 will reach out to patients via text message. For non-responders, Step 3 will contact patients’ clinicians using a novel “pend and send” tool in the EHR. The primary implementation outcome is engagement with germline genetic testing for breast and ovarian cancer predisposition, defined as a scheduled genetic counseling appointment. Patient data collected through the EHR (e.g., race/ethnicity, geocoded address) will be examined as moderators of the impact of the strategies.
Discussion
This study will be one of the first to sequentially examine the effects of patient- and clinician-directed strategies informed by behavioral economics on engagement with breast and ovarian cancer genetic testing. The pragmatic and sequential design will facilitate a large and diverse patient sample, allow for the assessment of incremental gains from different implementation strategies, and permit the assessment of moderators of strategy effectiveness. The findings may help determine the impact of low-cost, highly transportable implementation strategies that can be integrated into healthcare systems to improve the use of genomic medicine.
Trial registration
ClinicalTrials.gov. NCT05721326. Registered February 10, 2023. https://www.clinicaltrials.gov/study/NCT05721326
Similar content being viewed by others
Background
Breast cancer is the most common cancer for women across the world [1,2,3]. Approximately 300,000 new breast cancer cases were estimated in the USA for 2022, accounting for roughly one-third of new cancer diagnoses among U.S. women [4, 5]. Although less common, ovarian cancer ranks as the deadliest gynecologic cancer, accounting for about 20,000 cases and 13,000 deaths per year [4, 6, 7]. Moreover, substantial health inequities exist for both cancers. Early-stage diagnosis is critical for increasing survival rates [8, 9], but Black women tend to be diagnosed at later stages than white women [7, 10], and mortality rates for both diseases are > 30% higher for Black women as compared to white women [7, 11, 12].
In the past decade, multigene panel tests have been increasingly used to analyze several genes associated with breast and ovarian cancer [13,14,15]. Genetic testing can inform risk assessment, suggest interventions for risk reduction, and change options for therapy [16]. Multiple FDA approvals for PARP inhibitors for the treatment for BRCA-associated cancer, including early-stage, high-risk breast cancer [17, 18], have changed the landscape with regard to medical intervention [19]. As such, patients [20, 21] and clinicians [20, 22, 23] are generally interested in genetic testing and the National Comprehensive Cancer Network (NCCN) recommends testing for specific groups (e.g., people with personal histories of ovarian cancer) [14]. Unfortunately, there is a clear practice gap in genetic testing uptake, with only about 35% of ovarian cancer patients undergoing testing [24,25,26,27]. In assessing two large gynecology practices in our health system, we found higher rates than average of genetic testing among patients diagnosed within the last two years with early-onset breast cancer or triple-negative breast cancer. However, we found very low rates of genetic testing in individuals who were (1) diagnosed with ovarian cancer previously, or (2) had a family history of ovarian cancer or male breast cancer. Testing rates of those with a family history (rather than a personal history) of cancer were less than 15%. Moreover, substantial health inequities exist in testing rates. Eligible Black women are much less likely to be tested than their non-Hispanic white counterparts [11, 25,26,27,28], a finding replicated in the analysis of our own data, even with similar referral rates for all patients meeting our eligibility criteria.
Barriers to genomic medicine uptake exist at the system, clinician, and patient levels. The number of available genetic tests is growing exponentially [29, 30], so it can be challenging to integrate genomic data into the electronic health record (EHR) to track genetic test results and facilitate clinical workflows [31,32,33]. Our health system has tackled this issue by using Health Level 7 (HL7) standardization with labs, genomic indicators, and a precision medicine tab within the EHR [34]. However, due to expanding and changing indications and unclear eligibility criteria [35], clinicians may face challenges in identifying those eligible for genetic testing. Also, they report barriers related to a lack of awareness or training, cost concerns, and busy schedules [33, 35,36,37,38,39], resulting in uncertainty and lower priority for referring patients to genetic counseling. Integrating genomic medicine into the EHR can mitigate some concerns by identifying appropriate patients and guiding clinicians via streamlined workflows [34, 35, 40, 41]. Still, when faced with uncertainty, people often rely on cognitive heuristics to make decisions [42], such as status quo bias, or preferring to maintain the current state over taking action to change [40]. When perceiving unclear eligibility criteria or facing a busy schedule, clinicians may opt to keep things the same to maintain simplicity. The status quo bias can be leveraged by shifting the status quo to default genetics consult orders and emphasizing the availability of EHR-based support systems and clear recommendations for genetic testing. Similarly, default orders can make the referral process easier.
Given the shared decision-making dynamics underlying the choice to pursue genetic testing, patient barriers also must be addressed, including awareness [43,44,45], access [46], cost concerns [21, 43,44,45,46,47], anxiety about the potential misuse of test results [45, 48, 49], and insurance discrimination [21, 50]. Patients’ decisions are also affected by cognitive heuristics. Omission bias, or focusing on the potential harm of action more than that of inaction [51], plays a key role. Concerns about the implications of test results for patients and their families (such as the need for family members to be tested or fear about how medical professionals or insurance companies may use test results) can trigger omission bias and lead patients to think that getting genetic testing is worse than not pursuing it [52, 53]. These concerns tend to be heightened among members of racial or ethnic minority groups who have been mistreated by the medical system [45, 48, 49]. Although clinician recommendations to pursue genetic testing are one of the strongest predictors of patient willingness to undergo testing [28, 54, 55], clinicians are significantly less likely to recommend it to Black and Hispanic women [28, 54, 56]. Increasing the use of genetic testing requires addressing barriers at multiple levels [57], many of which are salient for patients from minoritized groups. Thus, offering patients the opportunity to be involved in decision-making about genetic testing is crucial for facilitating sustainable and equitable uptake [43].
Leveraging behavioral economic theory to mitigate cognitive heuristics has been effective in promoting evidence-based care and improving patient outcomes [58,59,60,61,62]. Nudges are strategies that make it easier for clinicians and patients to make evidence-based decisions. These can include framing language and/or default options, which subtly change the environment to facilitate evidence-based decisions while still preserving people’s freedom of choice [60, 63]. For instance, emphasizing the ease of genetic testing and the harms of not taking the first steps toward an appointment could mitigate omission bias. For clinicians, nudges can incorporate accountable justification, which requires clinicians to substantiate their decisions when declining a new status quo (in the form of a default order) and can promote self-reflection and higher-value care [64, 65].
Health system nudges have the potential to encourage uptake of genetic testing. These strategies can be automated, are scalable, and could mitigate health inequities [40, 62, 66, 67]. Prior research suggests that clinicians recommend genetic testing less often for non-white patients [28, 54, 56], but sequential dissemination of strategies could expand reach. Initial messages sent via the health system patient portal (MyPennMedicine; MPM) could generate initial interest via a “low-touch” message with minimal costs. Outreach via text messaging, which is more widespread [68], will be able to mitigate inequities resulting from differential patient portal access [69] and facilitate comparisons of outreach strategies. To reduce clinician burden, clinicians will only be contacted in the final phase. Literature suggests that clinician-directed default nudges, which sit atop the nudge intervention ladder, may be the most influential in changing behavior [62, 66].
This study was designed to evaluate the effects of three sequentially delivered patient- and clinician-directed implementation strategies informed by behavioral economics on the scheduling of genetic counseling appointments for patients with breast and ovarian cancer risk. We chose a sequential study design to determine the relative effects of the three strategies. Adaptive designs are gaining in use, including in oncology [70], since they can efficiently help identify the relative benefits of adding components of an intervention in relationship to the overall resources needed to sustain them. Behavioral economics and implementation science can be integrated to maximize the impact and equity of strategies seeking to encourage patients to pursue genetic testing [63].
Methods
Study design
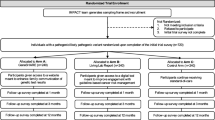
This pragmatic study will use a non-randomized, sequential adaptive design to examine the effect of patient- and clinician-directed nudges informed by behavioral economics and delivered via the EHR for promoting the use of genetic testing for the identification of breast and ovarian cancer predisposition. Sequences are detailed in Fig. 1. Before the sequences begin, we will use electronic phenotyping procedures to identify a cohort of patients receiving care through two large OB-GYN clinics who are eligible for genetic testing for breast and ovarian cancer predisposition (based on information in the EHR), but who have no documentation of testing in the EHR [71]. Next, in the first sequence, all patients will be contacted via the MyPennMedicine (MPM) patient portal. Messages will be delivered twice, one week apart. The message will include direct information on patients’ cancer risk based on their genetic history, their ability to take action to address their risk, and how to contact the study team to schedule an appointment. Patients can reply directly to the MPM message, call the Cancer Risk Evaluation Program (CREP), or use an outreach-specific email address. Patients who do not engage with the CREP within three weeks will receive the next adaptive sequence, a direct text message targeting omission bias to promote breast and ovarian cancer genetic testing. Again, patients will receive two text messages, a week apart, and will be given three weeks to schedule an appointment. The text message program will be conducted through Penn Way to Health, an evidence-based patient engagement platform [72, 73]. Finally, if patients do not engage with the genetics team, their clinicians will receive an EHR-based nudge targeting status quo bias using the “pend and send” functionality with a pended genetics consult order as a default. A final 6-month observation period will track the scheduling of genetic counseling and genetic testing results for breast and ovarian cancer predisposition following clinician strategy delivery. Patient characteristics (e.g., age, race/ethnicity, nature of genetic risk) will be ascertained from the EHR and explored as moderators of the effectiveness of each sequence to promote genetic testing. This sequential adaptive design will allow for comparisons of which strategies work best across clinics and subgroups of patients.
The primary implementation outcomes will be rates of scheduling and completion of genetic counseling appointments, stratified by factors such as referral clinic and diagnosis, with cumulative nudges representing a time-varying covariate. Decisions to undergo genetic testing in a timely manner are dependent on several factors, including patient preference. Additionally, a counseling discussion can alleviate some patient concerns about testing and may be more acceptable to patients. As such, scheduling the initial genetic counseling appointment was chosen as a primary outcome in addition to appointment completion. Process outcomes will include open rates for the two patient-directed strategies and the proportion of pended orders signed by referring clinicians. We will compare the number of appointments scheduled after each sequence and across patient-level characteristics (e.g., race and ethnicity) and site.
Study setting, population, and duration
This study will be conducted at gynecologic practices within two Penn Medicine centers: Penn Health for Women Radnor and the Helen O. Dickens Center for Women. These sites serve substantially different patient populations in terms of racial identity and insurance coverage, which may affect testing uptake. Most patients at Radnor are white (83.7% white, 6.5% Black, 3.0% Asian, 6.8% other/unknown), while the Dickens Center predominantly serves Black patients (73.7% Black, 18.9% white, 2.1% Asian, 5.3% other/unknown). Patients seen at these two sites since January 1, 2009 will be selected by an EHR-based algorithm established previously [71] using the following eligibility criteria: (1) serous ovarian cancer diagnosed more than two years prior to study contact; (2) breast cancer diagnosed at under 50 years of age more than two years prior to study contact; (3) triple-negative breast cancer diagnosed at any age more than two years prior to study contact; (4) unaffected individuals reporting a family history of ovarian cancer; (5) unaffected individuals reporting a family history of male breast cancer; and (6) at least two Penn Medicine appointments within the last three years. Utilizing electronic phenotyping in the EHR, participants who have previously received genetic counseling and testing will be excluded. Approximately, 3000 patients at these sites have been identified as eligible for genetic testing for familial high-risk breast and ovarian cancer based on these criteria, and these patients make up the target sample. The clinician sample (N = 30) will consist of gynecologists at participating practice sites associated with these patients. It is anticipated that the study will take approximately 18 months to complete. The study was approved by the University of Pennsylvania Institutional Review Board. The trial presents minimal risks to participants, and a waiver of informed consent was approved for all study aims.
Overview of rapid-cycle approaches and study procedures
The first step to increasing genetic testing is to identify patients who might benefit from it by utilizing updated tools in the EHR. Penn Medicine’s Abramson Cancer Center Electronic Phenotyping Core developed algorithms for identifying patients based on cancer registry data and family history fields in the EHR. These electronic phenotyping procedures were used to identify randomly selected patients to include in pilot testing during the rapid cycle approaches (RCAs).
As a project led by the National Cancer Institute-funded Penn Implementation Science Center in Cancer Control (Penn ISC3; P50CA244690), this study builds on strategies from the center’s prior research [74, 75]. As in prior studies, RCAs to quickly learn and innovate from pilot tests [41, 76,77,78] were used to de-risk and optimize our nudges as implementation strategies. They also helped us refine our methods based on relevant experiences from clinicians and patient partners to maximize their effect and study efficiency. This work is summarized in Table 1. RCAs involved advisory meetings with experts in behavioral economics, discussions with patient and family partners on the Basser Young Leadership Council, and meetings with clinicians with expertise in breast and ovarian cancer genetic testing. In addition, given the calls to incorporate implementation science and health equity together in genomic medicine [43, 79], experts at integrating these fields provided guidance on study design and message content. We then designed prototype messages and received feedback about content and delivery mechanisms. Finally, two template patient nudges were pilot-tested by randomizing 200 patients to one of two messages that were based on different heuristics. After patients were sent their arm’s respective pilot message via the patient portal and text message, the proportions of patients who engaged with messages, contacted the CREP scheduling staff and scheduled a genetic counseling appointment were assessed. Based on extensive review from partners and pilot test results, the nudges to be implemented in the overall study were designed as follows.
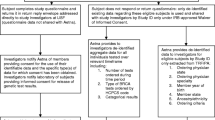
Patient nudges (patient portal and text message)
The patient-directed strategies will be delivered via two mechanisms: the patient portal and text message. Figure 2 shows both patient-directed nudges. The content of the nudges was influenced by past research documenting that patients tend to focus on the potential adverse effects of action vs. inaction [52, 53, 80] and was reviewed and modified by a group of clinicians and patient partners. Eligible patients will initially be contacted via the patient portal. This “low-touch” implementation strategy can provide information about the impact of using patient health system portals to encourage the uptake of genetic testing. If patients do not respond, or if they are identified as not having a patient portal account, they will be moved to the second implementation sequence. In this sequence, patients will be sent text messages using similar content from the first sequence, encouraging them to sign up for genetic counseling appointments. Patients who do not respond to the first two nudges will be identified for the clinician's nudge.
Clinician nudge
Our preliminary formative work involved the development of prototype messages to integrate as nudges delivered to clinicians through the EHR. As with the patient nudge, we created multiple versions of the nudges and ascertained feedback from partners about the message content and design, as well as the method and timing of delivery. Also, the study team engaged with research from another study promoting genetic testing and adapted the wording and format of a clinician nudge to design a message considered most likely to receive clinician support.
Both study sites use Epic (Epic Systems Corporation, Verona, WI) to deliver care. Recent upgrades to Penn’s Epic instance introduced the “pend and send” capability. Using this process, the research team will create a pended order for a genetics consult for eligible patients who did not respond to prior patient-directed strategies. As detailed in Fig. 3, the clinician nudge will include text leveraging status quo bias, a default order for a genetics consult, and a requirement for clinicians to provide accountable justification if they decline the order. Clinicians can efficiently sign orders in the InBasket without needing to open each encounter separately. The consults are then routed directly to the CREP scheduling team, who will contact the patient to schedule an appointment with a genetic counselor. We pilot-tested the “pend and send” mechanism in the RCAs. Clinicians have been engaged at both clinics so that they are aware of this initiative and clinician education has been provided.
Measures
The primary outcomes are the rates of contacted patients who schedule and complete a genetic counseling appointment within six months after each sequential step, collected via the EHR. As process measures, we will evaluate the proportion of patients who open MPM messages or respond to text messages within one month of receiving them, as well as the proportion of pended orders that clinicians sign within one month to refer patients for a genetics consult. Potential moderating variables will also be collected, including patient demographics (age, race, ethnicity, diagnosis, health insurance, address, and geocoded area as a proxy for neighborhood-level socioeconomic status), clinician data (practice site, years in practice), and practice-level information (community vs. hospital-based setting, urban vs. non-urban location, health insurance mix). These data will be used to describe the sample of participating patients and clinicians and to identify factors that may influence strategy effectiveness. Genetic counseling and testing rates will be evaluated after being stratified by these factors.
Sample size, power, and statistical analysis
Based on preliminary assessments via electronic phenotyping in the EHR, we have identified a target sample of around 3000 patients (clustered within approximately 30 physicians at the two Penn Medicine sites) who may benefit from genetic testing for familial high-risk breast and ovarian cancer predisposition but have not done so. We calculated power conservatively by assuming correlations of 0 to 0.2, using PASS (Power and Sample Size, NCSS Software, Kaysville, UT). We found our sample gives us 80% power to detect at least a 5% improvement in our cumulative incidence of testing using a two-sided type 1 error rate of 5%, for planned comparisons between each stage in the sequence.
We will analyze the change in the incidence of scheduling counseling appointments across the three sequences (all time to event outcomes) using Cox regression, with variances adjusted for physician clustering. The models will contain time-varying binary predictor terms for each nudge, making adjustments for time in months, and fixed effects for site. We will control for type 1 error inflation by hierarchical testing, starting with the overall model significance, followed by the effect of each strategy. Once we have fitted the main effects model, we will test for each sequence and retain terms if significant (alpha = 5%). Variability in outcomes by sequence and moderators (particularly health equity variables) will be assessed using interaction terms within Cox regression models. We will fit an adjusted Cox regression model using the same approach described in the primary analysis. Covariates of interest available through the EHR will be added to the model, including patient-level (e.g., race), clinician-level (e.g., physician type), and practice-level (e.g., community vs. hospital-based) data.
Discussion
This study will sequentially test the effects of patient-directed strategies, sent via the patient portal and text message, and EHR-based clinician-directed strategies, sent as “pend and send” default orders, on genetic counseling engagement in gynecology practices at two distinct Penn Medicine clinics. It builds upon Penn ISC3’s prior work [74, 75] implementing nudges to patients and clinicians by extending it to new populations who face additional barriers to engaging in evidence-based clinical practices. Sequential delivery mechanisms can reinforce the additive value of combining outreach via different communication channels, as well as facilitate comparisons between different patient outreach mechanisms. Additionally, the study demonstrates the value of RCAs and pilot testing strategies before implementing them at scale. By addressing barriers and heuristics that affect both patients and clinicians, this multi-level approach may help to define optimal strategies resulting in increased potential for success.
Substantial racial inequities exist in genetic testing, the timeliness of cancer diagnosis, and mortality rates. Implementing these strategies at diverse clinics in this study seeks to mitigate such inequities. While innovative treatments for BRCA-associated cancers (such as PARP inhibitors) are being approved, these innovations can exacerbate racial inequities in downstream outcomes and guideline-concordant receipt of these innovative treatments if genetic testing is not equitably implemented. In combination with existing racial inequities in clinicians’ recommendations for genetic testing, expanding inclusion criteria for genetic testing for all breast cancer patients may widen the divide in genetic testing uptake. Automated outreach via several communication channels aims to alleviate this inequity, and if successful, it can guide future outreach programs to extend health systems’ reach.
Nevertheless, researchers must be mindful of not overloading patients and clinicians with information and support tools. Co-designing strategies with patients and clinicians, switching from a BPA to a “pend and send” default order and the sequential nature of the study has helped mitigate this concern. While the clinics in this study serve diverse patient populations, results may not be generalizable to sites lacking a robust EHR network, capacity for genetic counseling, or leadership support. Finally, this is not a randomized trial. If the implementation strategies demonstrate a positive impact, study results can provide an initial model for encouraging genetic testing uptake and may lead to future large cluster randomized clinical trials focused on scaling these approaches at other Penn Medicine sites and beyond.
Availability of data and materials
Not applicable.
Abbreviations
- BPA:
-
Best Practice Alert
- BRCA:
-
Breast cancer gene
- CREP:
-
Cancer Risk Evaluation Program
- EHR:
-
Electronic Health Record
- FDA:
-
Food and Drug Administration
- HL7:
-
Health Level 7
- ISC3:
-
Implementation Science Center in Cancer Control
- MPM:
-
MyPennMedicine
- NCCN:
-
National Comprehensive Cancer Network
- NCSS:
-
Number Cruncher Statistical Systems
- OB-GYN:
-
Obstetrics and Gynecology
- PARP:
-
Poly (ADP-ribose) Polymerase
- PASS:
-
Power Analysis & Sample Size
- RCA:
-
Rapid cycle approaches
- TNBC:
-
Triple negative breast cancer
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020–2070. Nat Rev Clin Oncol. 2021;18(10):663–72.
Arnold M, Morgan E, Rumgay H, Mafra A, Singh D, Laversanne M, et al. Current and future burden of breast cancer: Global statistics for 2020 and 2040. Breast. 2022;66:15–23.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Centers for Disease Control and Prevention. Cancer Statistics At a Glance 2019 [Available from: https://gis.cdc.gov/Cancer/USCS/?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcancer%2Fdataviz%2Findex.htm#/AtAGlance/.
Srivastava SK, Ahmad A, Miree O, Patel GK, Singh S, Rocconi RP, et al. Racial health disparities in ovarian cancer: not just black and white. J Ovarian Res. 2017;10(1):58.
Collins Y, Holcomb K, Chapman-Davis E, Khabele D, Farley JH. Gynecologic cancer disparities: a report from the health disparities taskforce of the society of gynecologic oncology. Gynecol Oncol. 2014;133(2):353–61.
Menon U, Gentry-Maharaj A, Burnell M, Singh N, Ryan A, Karpinskyj C, et al. Ovarian cancer population screening and mortality after long-term follow-up in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): a randomised controlled trial. Lancet. 2021;397(10290):2182–93.
Cancer Research UK. Ovarian cancer survival 2021 [Available from: https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/survival.
Morris CR, Sands MT, Smith LH. Ovarian cancer: predictors of early-stage diagnosis. Cancer Causes Control. 2010;21(8):1203–11.
Reid S, Cadiz S, Pal T. Disparities in genetic testing and care among Black women with hereditary breast cancer. Curr Breast Cancer Rep. 2020;12(3):125–31.
Jatoi I, Sung H, Jemal A. The emergence of the racial disparity in U.S. breast-cancer mortality. N Engl J Med. 2022;386(25):2349–52.
Domchek SM, Robson ME. Update on genetic testing in gynecologic cancer. J Clin Oncol. 2019;37(27):2501–9.
Daly MB, Pal T, Berry MP, Buys SS, Dickson P, Domchek SM, et al. Genetic/familial high-risk assessment: breast, ovarian, and pancreatic, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2021;19(1):77–102.
Hu C, Hart SN, Gnanaolivu R, Huang H, Lee KY, Na J, et al. A population-based study of genes previously implicated in breast cancer. N Engl J Med. 2021;384(5):440–51.
Domchek SM, Friebel TM, Singer CF, Evans DG, Lynch HT, Isaacs C, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304(9):967–75.
Geyer CE Jr, Garber JE, Gelber RD, Yothers G, Taboada M, Ross L, et al. Overall survival in the OlympiA phase III trial of adjuvant olaparib in patients with germline pathogenic variants in BRCA1/2 and high-risk, early breast cancer. Ann Oncol. 2022;33(12):1250–68.
Tutt ANJ, Garber JE, Kaufman B, Viale G, Fumagalli D, Rastogi P, et al. Adjuvant Olaparib for patients with BRCA1- or BRCA2-mutated breast cancer. N Engl J Med. 2021;384(25):2394–405.
Yadav S, Jinna S, Pereira-Rodrigues O, Reeves A, Campian S, Sufka A, et al. Impact of preoperative BRCA1/2 testing on surgical decision making in patients with newly diagnosed breast cancer. Breast J. 2018;24(4):541–8.
Hall MJ, Forman AD, Montgomery SV, Rainey KL, Daly MB. Understanding patient and provider perceptions and expectations of genomic medicine. J Surg Oncol. 2015;111(1):9–17.
Smith-Uffen M, Bartley N, Davies G, Best M. Motivations and barriers to pursue cancer genomic testing: a systematic review. Patient Educ Couns. 2021;104(6):1325–34.
Heck PR, Meyer MN. Population whole exome screening: primary care provider attitudes about preparedness, information avoidance, and nudging. Med Clin North Am. 2019;103(6):1077–92.
de Moor JS, Gray SW, Mitchell SA, Klabunde CN, Freedman AN. Oncologist confidence in genomic testing and implications for using multimarker tumor panel tests in practice. JCO Precis Oncol. 2020;4:PO.19.00338.
McBride CM, Pathak S, Johnson CE, Alberg AJ, Bandera EV, Barnholtz-Sloan JS, et al. Psychosocial factors associated with genetic testing status among African American women with ovarian cancer: results from the African American cancer epidemiology study. Cancer. 2022;128(6):1252–9.
Lau-Min KS, McCarthy AM, Nathanson KL, Domchek SM. Nationwide trends and determinants of germline BRCA1/2 testing in patients with breast and ovarian cancer. J Natl Compr Canc Netw. 2023;21(4):351-8 e4.
Lee J, Gubernick LR, Brodsky AL, Fehniger JE, Levine DA, Gerber D, et al. Missed opportunities: genetic counseling and testing among an ethnically diverse cohort of women with endometrial cancer. Gynecol Oncol. 2018;151(1):153–8.
Kurian AW, Ward KC, Howlader N, Deapen D, Hamilton AS, Mariotto A, et al. Genetic testing and results in a population-based cohort of breast cancer patients and ovarian cancer patients. J Clin Oncol. 2019;37(15):1305–15.
McCarthy AM, Bristol M, Domchek SM, Groeneveld PW, Kim Y, Motanya UN, et al. Health care segregation, physician recommendation, and racial disparities in BRCA1/2 testing among women with breast cancer. J Clin Oncol. 2016;34(22):2610–8.
Phillips KA, Deverka PA, Hooker GW, Douglas MP. Genetic test availability and spending: where are we now? Where are we going? Health Aff (Millwood). 2018;37(5):710–6.
Dragojlovic N, Borle K, Kopac N, Ellis U, Birch P, Adam S, et al. Correction: the composition and capacity of the clinical genetics workforce in high-income countries: a scoping review. Genet Med. 2020;22(9):1570.
Williams MS, Taylor CO, Walton NA, Goehringer SR, Aronson S, Freimuth RR, et al. Genomic information for clinicians in the electronic health record: lessons learned from the clinical genome resource project and the electronic medical records and genomics network. Front Genet. 2019;10:1059.
Kho AN, Rasmussen LV, Connolly JJ, Peissig PL, Starren J, Hakonarson H, et al. Practical challenges in integrating genomic data into the electronic health record. Genet Med. 2013;15(10):772–8.
Zebrowski AM, Ellis DE, Barg FK, Sperber NR, Bernhardt BA, Denny JC, et al. Qualitative study of system-level factors related to genomic implementation. Genet Med. 2019;21(7):1534–40.
Lau-Min KS, McKenna D, Asher SB, Bardakjian T, Wollack C, Bleznuck J, et al. Impact of integrating genomic data into the electronic health record on genetics care delivery. Genet Med. 2022;24:2338.
Franck LS, Kriz RM, Rego S, Garman K, Hobbs C, Dimmock D. Implementing rapid whole-genome sequencing in critical care: a qualitative study of facilitators and barriers to new technology adoption. J Pediatr. 2021;237(237–43): e2.
Owusu Obeng A, Fei K, Levy KD, Elsey AR, Pollin TI, Ramirez AH, et al. Physician-reported benefits and barriers to clinical implementation of genomic medicine: a multi-site IGNITE-network survey. J Pers Med. 2018;8(3):24.
Jayasinghe K, Quinlan C, Mallett AJ, Kerr PG, McClaren B, Nisselle A, et al. Attitudes and practices of Australian nephrologists toward implementation of clinical genomics. Kidney Int Rep. 2021;6(2):272–83.
Birmingham WC, Agarwal N, Kohlmann W, Aspinwall LG, Wang M, Bishoff J, et al. Patient and provider attitudes toward genomic testing for prostate cancer susceptibility: a mixed method study. BMC Health Serv Res. 2013;13:279.
Lee YQ, Yoon SY, Hassan T, Padmanabhan H, Yip CH, Keng WT, et al. Attitudes and training needs of oncologists and surgeons in mainstreaming breast cancer genetic counseling in a low-to-middle income Asian country. J Genet Couns. 2022;31:1080.
Lau-Min KS, Guerra CE, Nathanson KL, Bekelman JE. From race-based to precision oncology: leveraging behavioral economics and the electronic health record to advance health equity in cancer care. JCO Precis Oncol. 2021;5:PO.20.00418.
Kukafka R, Pan S, Silverman T, Zhang T, Chung WK, Terry MB, et al. Patient and clinician decision support to increase genetic counseling for hereditary breast and ovarian cancer syndrome in primary care: a cluster randomized clinical trial. JAMA Netw Open. 2022;5(7): e2222092.
Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185(4157):1124–31.
Roberts MC, Mensah GA, Khoury MJ. Leveraging implementation science to address health disparities in genomic medicine: examples from the field. Ethn Dis. 2019;29(Suppl 1):187–92.
Gray SW, Hicks-Courant K, Lathan CS, Garraway L, Park ER, Weeks JC. Attitudes of patients with cancer about personalized medicine and somatic genetic testing. J Oncol Pract. 2012;8(6):329–35 p following 35.
Suther S, Kiros GE. Barriers to the use of genetic testing: a study of racial and ethnic disparities. Genet Med. 2009;11(9):655–62.
Steffen LE, Du R, Gammon A, Mandelblatt JS, Kohlmann WK, Lee JH, et al. Genetic testing in a population-based sample of breast and ovarian cancer survivors from the REACH randomized trial: cost barriers and moderators of counseling mode. Cancer Epidemiol Biomarkers Prev. 2017;26(12):1772–80.
Cragun D, Weidner A, Kechik J, Pal T. Genetic testing across young Hispanic and non-hispanic white breast cancer survivors: facilitators, barriers, and awareness of the genetic information nondiscrimination act. Genet Test Mol Biomarkers. 2019;23(2):75–83.
Glenn BA, Chawla N, Bastani R. Barriers to genetic testing for breast cancer risk among ethnic minority women: an exploratory study. Ethn Dis. 2012;22(3):267–73.
Hann KEJ, Freeman M, Fraser L, Waller J, Sanderson SC, Rahman B, et al. Awareness, knowledge, perceptions, and attitudes towards genetic testing for cancer risk among ethnic minority groups: a systematic review. BMC Public Health. 2017;17(1):503.
Rogith D, Yusuf RA, Hovick SR, Peterson SK, Burton-Chase AM, Li Y, et al. Attitudes regarding privacy of genomic information in personalized cancer therapy. J Am Med Inform Assoc. 2014;21(e2):e320–5.
Spranca M, Minsk E, Baron J. Omission and commission in judgment and choice. J Exp Soc Psychol. 1991;27(1):76–105.
Schneider JL, Goddard KA, Davis J, Wilfond B, Kauffman TL, Reiss JA, et al. “Is it worth knowing?” Focus group participants’ perceived utility of genomic preconception carrier screening. J Genet Couns. 2016;25(1):135–45.
Taber JM, Klein WM, Ferrer RA, Lewis KL, Harris PR, Shepperd JA, et al. Information avoidance tendencies, threat management resources, and interest in genetic sequencing feedback. Ann Behav Med. 2015;49(4):616–21.
Cragun D, Weidner A, Lewis C, Bonner D, Kim J, Vadaparampil ST, et al. Racial disparities in BRCA testing and cancer risk management across a population-based sample of young breast cancer survivors. Cancer. 2017;123(13):2497–505.
Kurian AW, Griffith KA, Hamilton AS, Ward KC, Morrow M, Katz SJ, et al. Genetic testing and counseling among patients with newly diagnosed breast cancer. JAMA. 2017;317(5):531–4.
Linfield DT, Rothberg MB, Pfoh ER, Noss R, Cassard L, Powers JC, et al. Primary care physician referral practices regarding BRCA1/2 genetic counseling in a major health system. Breast Cancer Res Treat. 2022;195(2):153–60.
Stange KC, Breslau ES, Dietrich AJ, Glasgow RE. State-of-the-art and future directions in multilevel interventions across the cancer control continuum. J Natl Cancer Inst Monogr. 2012;2012(44):20–31.
Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med. 2007;357(13):1340–4.
Patel MS, Volpp KG. Leveraging insights from behavioral economics to increase the value of health-care service provision. J Gen Intern Med. 2012;27(11):1544–7.
Patel MS, Volpp KG, Asch DA. Nudge units to improve the delivery of health care. N Engl J Med. 2018;378(3):214–6.
Yoong SL, Hall A, Stacey F, Grady A, Sutherland R, Wyse R, et al. Nudge strategies to improve healthcare providers’ implementation of evidence-based guidelines, policies and practices: a systematic review of trials included within cochrane systematic reviews. Implement Sci. 2020;15(1):50.
Last BS, Buttenheim AM, Timon CE, Mitra N, Beidas RS. Systematic review of clinician-directed nudges in healthcare contexts. BMJ Open. 2021;11(7): e048801.
Beidas RS, Buttenheim AM, Mandell DS. Transforming mental health care delivery through implementation science and behavioral economics. JAMA Psychiat. 2021;78(9):941–2.
Takvorian SU, Ladage VP, Wileyto EP, Mace DS, Beidas RS, Shulman LN, et al. Association of behavioral nudges with high-value evidence-based prescribing in oncology. JAMA Oncol. 2020;6(7):1104–6.
Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA. 2016;315(6):562–70.
Waddell KJ, Shah PD, Adusumalli S, Patel MS. Using behavioral economics and technology to improve outcomes in cardio-oncology. JACC CardioOncol. 2020;2(1):84–96.
Rendle KA, Beidas RS. Four strategic areas to advance equitable implementation of evidence-based practices in cancer care. Transl Behav Med. 2021;11(11):1980–8.
Pew Research Center. Mobile Fact Sheet 2021 [updated April 7, 2021. Available from: https://www.pewresearch.org/internet/fact-sheet/mobile/.
Richwine C, Johnson C, Patel V. Disparities in patient portal access and the role of providers in encouraging access and use. J Am Med Inform Assoc. 2023;30(2):308–17.
Mistry P, Dunn JA, Marshall A. A literature review of applied adaptive design methodology within the field of oncology in randomised controlled trials and a proposed extension to the CONSORT guidelines. BMC Med Res Methodol. 2017;17(1):108.
Verma A, Damrauer SM, Naseer N, Weaver J, Kripke CM, Guare L, et al. The penn medicine biobank: towards a genomics-enabled learning healthcare system to accelerate precision medicine in a diverse population. J Pers Med. 2022;12(12):1974.
Asch DA, Muller RW, Volpp KG. Automated hovering in health care–watching over the 5000 hours. N Engl J Med. 2012;367(1):1–3.
Asch DA, Volpp KG. On the way to health. LDI Issue Brief. 2012;17(9):1–4.
Takvorian SU, Bekelman J, Beidas RS, Schnoll R, Clifton ABW, Salam T, et al. Behavioral economic implementation strategies to improve serious illness communication between clinicians and high-risk patients with cancer: protocol for a cluster randomized pragmatic trial. Implement Sci. 2021;16(1):90.
Jenssen BP, Schnoll R, Beidas RS, Bekelman J, Bauer AM, Evers-Casey S, et al. Cluster randomized pragmatic clinical trial testing behavioral economic implementation strategies to improve tobacco treatment for patients with cancer who smoke. J Clin Oncol. 2023;41:4511 JCO2300355.
Asch DA, Rosin R. Innovation as discipline, not fad. N Engl J Med. 2015;373(7):592–4.
Last BS, Buttenheim AM, Futterer AC, Livesey C, Jaeger J, Stewart RE, et al. A pilot study of participatory and rapid implementation approaches to increase depression screening in primary care. BMC Fam Pract. 2021;22(1):228.
Lee KC, Al-Ramahi N, Hahn L, Donnell T, Schonewolf L, Khan N, et al. Operationalizing equity: a rapid-cycle innovation approach to Covid-19 vaccination in black neighborhoods. NEJM Catalyst Innov Care Deliv 2021;2(2).
Green ED, Gunter C, Biesecker LG, Di Francesco V, Easter CL, Feingold EA, et al. Strategic vision for improving human health at The forefront of genomics. Nature. 2020;586(7831):683–92.
Stevens EM, Patterson CA, Tchume-Johnson T, Antiel RM, Flake A, Smith-Whitley K, et al. Parental attitudes towards prenatal genetic testing for sickle cell disease. J Pediatr Hematol Oncol. 2019;41(8):579–85.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Cancer Institute grant P50 CA244690.
Author information
Authors and Affiliations
Contributions
HS, RS, KLN, and SMD led study design. HS, RS, RSB, DB, KAR, OMF, KLN, and SMD supported paper writing. RS, RSB, and JEB obtained the study funding. HS, DB, AB, KLN, and SMD developed the study protocol and managed the study. PG, LB, and AD lead clinical informatics. HS, PG, and LB led the design of clinician nudges. JP, JC, DBM, RR, and LC serve as genetic counselor partners. RO and EGC lead the two clinics at which the trial is being implemented, and JEB and LNS support the overall implementation lab. AMB and DAA oversaw the preparation for rapid cycle approaches. KAR, RCS, and OMF led the health equity assessment. EPW is the study biostatistician. HS and MP led the design and distribution of text messages for patients. SW developed the study database.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This trial was approved by the University of Pennsylvania Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
RSB is the principal at Implementation Science & Practice, LLC. She receives royalties from Oxford University Press, consulting fees from United Behavioral Health and OptumLabs, and serves on the advisory boards for Optum Behavioral Health, AIM Youth Mental Health Foundation, and the Klingenstein Third Generation Foundation outside of the submitted work. JEB reports grants from AstraZeneca, Emerson Collective, Loxo@Lilly, and Gilead and personal fees from Reimagine Care, Healthcare Foundry, and AstraZeneca, outside the submitted work. DBM reports having been a one-time consultant for Nest Genomics. DAA is a partner at VAL Health. KAR reports receiving grants from Pfizer and AstraZeneca paid to her institution, personal fees from Merck for serving as a scientific consultant, and honoraria and travel paid as an invited speaker from MJH Life Sciences outside the submitted work. KLN reports serving on a Scientific Advisory Board for Merck, unrelated to the current study. SMD reports consulting fees from AstraZeneca and GlaxoSmithKline.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 2.
Standards for Reporting Implementation Studies: the StaRI checklist for completion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Symecko, H., Schnoll, R., Beidas, R.S. et al. Protocol to evaluate sequential electronic health record-based strategies to increase genetic testing for breast and ovarian cancer risk across diverse patient populations in gynecology practices. Implementation Sci 18, 57 (2023). https://doi.org/10.1186/s13012-023-01308-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-023-01308-w