Abstract
Background
MEIS1::NCOA2 is a rare fusion gene that has been recently described in a subset of spindle cell rhabdomyosarcomas and multiple low-grade undifferentiated spindle cell sarcomas predominantly arising in the genitourinary and gynecologic tracts with no specific line of differentiation. We present the first documented case of this neoplasm arising as a lung primary tumor.
Case Presentation
A 74-year-old woman with a 40-year smoking history presented with a 2.1 × 1.7 cm lung nodule discovered on computed tomography (CT) scan. A biopsy and subsequent lobe resection were performed, as well as an extensive metastatic work up, which revealed no additional masses. No specific line of differentiation was found by immunohistochemical staining, and an RNA-based fusion panel revealed a MEIS1::NCOA2 fusion, at which point a diagnosis of Low-Grade Undifferentiated Sarcoma with MEIS1::NCOA2-Rearrangement was rendered.
Conclusions
This report represents the first diagnosis of this tumor primary to the lung, and provides additional insight into the origin and localization of these rare tumors.
Similar content being viewed by others

Background
MEIS1::NCOA2 is a rare fusion gene that has been recently described in a subset of spindle cell rhabdomyosarcomas and multiple low-grade undifferentiated spindle cell sarcomas predominantly arising in the genitourinary and gynecologic tracts [1,2,3]. We present a case of a 74-year-old woman who presented with a 2.1 cm right upper lobe lung nodule. The lesion was composed of whorls and fascicles of monomorphic and infiltrative spindled cells with minimal mitotic activity and no necrosis. Immunohistochemical staining showed no specific line of differentiation, but next generation sequencing revealed an MEIS1:NCOA2 fusion. Ultimately, given a completely negative metastatic workup, a diagnosis of lung primary low-grade undifferentiated spindle cell sarcoma with MEIS1::NCOA2 fusion was rendered. To our knowledge, no other lung primary tumors of this type have been reported.
Case presentation
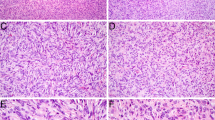
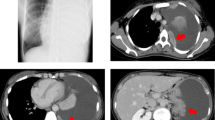
A 74-year-old woman with a 40-year smoking history was found to have a right upper lobe lung nodule that was discovered on routine surveillance computed tomography (CT) scan. The imaging studies described a mass with a dominant 2.1 × 1.7 cm solid component (Fig. 1). The patient underwent an endobronchial biopsy of the right upper lung mass which revealed a spindle cell tumor in the bronchial submucosa with minimal variability in nuclear size arranged in whorls and fascicles with very rare mitotic activity. A preliminary diagnosis of low-grade spindle cell neoplasm was provided and the patient was treated with lobectomy to obtain a negative margin. The lobe was received intact, and sectioning revealed a 1.7 × 1.5 × 1.5 cm white, bulging mass that was abutting the pleural surface (Fig. 2). Histologic sections of the entire tumor recapitulated biopsy findings, showing whorls and fascicles of primitive and monomorphic spindle cells with minimal mitotic activity (< 1 per 10 high-powered fields) and no necrosis (Fig. 3). On high-power magnification, the tumor cells showed very mild nuclear size variety and occasional overlap with ovoid to cigar-shaped nuclei, inconspicuous nucleoli, and ample eosinophilic cytoplasm with indistinct cell borders. The tumor originated in the bronchial wall and showed an infiltrative pattern surrounding bronchial cartilage and submucosal glands. Focal ulceration into the bronchial mucosa was also noted. A panel of immunohistochemical stains was performed which revealed patchy positive staining for smooth muscle actin (SMA), and negative staining for cytokeratins (CK AE1/AE3, CK8/18), S100, CD34, ALK-1, desmin, myoD1, and myogenin. The proliferative rate was relatively low, with a Ki-67 of ~ 5%. A peculiar previously undescribed finding was the presence of scattered periodic acid Schiff (PAS) positive crystalloid structures located throughout the tumor (Fig. 4). These are of unclear origin but may represent entrapped concretions of normal submucosal gland secretions or material produced by the tumor.
A) Hematoxylin and eosin stained slide showing whorls and fascicles of primitive and monomorphic spindle cells (10x); B) Hematoxylin and eosin stained slide showing adjacent respiratory cartilage (10x), C) adjacent respiratory epithelium (10x), D) entrapped salivary gland-type tissue (20x), and E) high-power showing nuclear pleomorphism (40x); F) low proliferative index highlighted by Ki-67 (10x)
Molecular testing was performed using the PGDx elio tissue complete panel (Labcorp) and the Archer FusionPlex panel (IDT) for assessment of sequence variants and rearrangements. No variants of known or possible clinical significance were found, and the tumor was shown to be microsatellite stable with a mutational burden of 4.6 mutations per megabase. The fusion panel revealed an in-frame fusion of MEIS1 (Chr2: 66,670,180) and NCOA2 (Chr8: 71,060,718) (Fig. 3) in 267 reads using genome assembly GRCh37/hg19 resulting in a fusion of MEIS1 exon 6 to NCOA2 exon 12 (MEIS1 NM_002398.3, NCOA2 NM_001321703.2) (Fig. 5). Additional imaging studies, including CT and PET scans, were performed and showed no other evidence of disease. Taken together, the imaging, histologic, immunohistochemical, and molecular findings led to a diagnosis of a primary lung low-grade undifferentiated spindle cell sarcoma with MEIS1::NCOA2 fusion. Continued follow-up from diagnosis to present (2 years) has still revealed no additional site of primary and no disease recurrence.
Discussion and conclusions
The NCOA2 gene (nuclear receptor co-activator 2) is located on chromosome band 8q13 and encodes a transcriptional coactivator for nuclear hormone receptors that include steroid, thyroid, retinoid, and vitamin D receptors [4]. NCOA2 has been described as a 3’ partner in a number of fusion-associated sarcomas including mesenchymal chondrosarcoma (HEY1::NCOA2), spindle cell rhabdomyosarcoma (VGLL2::NCOA2, SRF::NCOA2, or TEAD1::NCOA2) [5], and soft tissue angiofibroma (AHRR::NCOA2) [6, 7].In these settings, the NCOA2 fusion gene typically retains its C-terminal transcription activation domains 1 and 2, which leads to the prevailing theory that NCOA2 is targeted by a DNA-binding domain that is provided by the N-terminal partner gene [8].
The role of MEIS1 as a fusion partner in fusion-associated sarcomas is less well understood. The MEIS1 gene, located at chromosome 2p14, encodes a protein within the three amino acid loop extension (TALE) homeodomain transcription factor family which is thought to function through the activation of Hox transcription factors [9]. The MEIS1 gene is postulated to have key roles in cardiac regeneration and stem cell function, as well as potential for tumorigenesis [10, 11]. Interestingly, MEIS1 is known, in isolation, to function as both a tumor suppressor gene as well as an oncogene in several tumor types [12,13,14,15,16]. Aside from NCOA2 fusions in the current entity and a subset of spindle cell rhabdomyosarcomas, MEIS1 has not been associated with gene fusion related cancers, though overexpression has been associated with myeloid leukemias [1]. The common partners for Low-grade undifferentiated spindle cell sarcomas with MEIS1::NCOA1/2 fusions represent a recently described group of lesions initially presented in a series of two patients with primitive-appearing spindle cell sarcomas with non-specific immunohistochemical profiles found in the kidneys [1]. Moreover, a number of other reports have been published that demonstrated these tumors occurring in the kidney, uterine corpus, vagina, scrotum, and para-rectal area [2, 3]. Previous studies have noted that the broad expression of MEIS1 across numerous human tissue types seemed to be at odds with the relative consistent localization of these tumors to the genitourinary tract [1], and this case of a lung primary seems to support the potential for numerous body sites to give rise to these tumors.
The diagnosis of MEIS1::NCOA2 fused undifferentiated sarcomas can provide significant diagnostic challenges depending on the site of origin. A low-grade appearing spindle cell neoplasm in the lung raises the differential diagnosis of leiomyoma (either primary or benign metastasizing), metastatic low-grade appearing leiomyosarcoma, solitary fibrous tumors, schwannoma, and other low-grade metastatic spindle cell neoplasms. Some of this differential diagnosis can be investigated with a combination of immunohistochemical stains, diligent historical chart review, and imaging studies.
The overall behavior of these lesions is not well established, given the paucity of long-term follow up and rarity, but the current data seems to suggest a “low-grade” clinical course with rare reports of distant metastases (kidney to the lung), and local aggressiveness. More data is needed to fully characterize this lesion [3, 17]. The current case represents the first reported case of this entity in a solitary, central lung mass with no other sites of origin seen on imaging to suggest metastasis. This unique case broadens the perspective on MEIS1::NCOA2-rearranged sarcomas and further workup for this rearrangement should be considered in the appropriate setting regardless of location.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Argani P, Reuter VE, Kapur P, Brown JE, Sung YS, Zhang L, et al. Novel MEIS1-NCOA2 gene fusions define a distinct primitive spindle cell sarcoma of the kidney. Am J Surg Pathol. 2018;42(11):1562–70.
Kao YC, Bennett JA, Suurmeijer AJH, Dickson BC, Swanson D, Wanjari P, et al. Recurrent MEIS1-NCOA2/1 fusions in a subset of low-grade spindle cell sarcomas frequently involving the genitourinary and gynecologic tracts. Mod Pathol. 2021;34(6):1203–12.
Kommoss FKF, Kölsche C, Mentzel T, Schmidt D, von Deimling A, McCluggage WG, et al. Spindle cell sarcoma of the Uterine Corpus with adipose metaplasia: expanding the morphologic spectrum of Neoplasms with MEIS1-NCOA2 Gene Fusion. Int J Gynecol Pathol. 2022;41(4):417–22.
NCOA2 nuclear receptor. coactivator 2 [ Homo sapiens (human) ] 2023 [updated 2/12/2023. https://www.ncbi.nlm.nih.gov/gene/10499.
Mosquera JM, Sboner A, Zhang L, Kitabayashi N, Chen CL, Sung YS, et al. Recurrent NCOA2 gene rearrangements in congenital/infantile spindle cell rhabdomyosarcoma. Genes Chromosomes Cancer. 2013;52(6):538–50.
Panagopoulos I, Gorunova L, Viset T, Heim S. Gene fusions AHRR-NCOA2, NCOA2-ETV4, ETV4-AHRR, P4HA2-TBCK, and TBCK-P4HA2 resulting from the translocations t(5;8;17)(p15;q13;q21) and t(4;5)(q24;q31) in a soft tissue angiofibroma. Oncol Rep. 2016;36(5):2455–62.
Yamada Y, Yamamoto H, Kohashi K, Ishii T, Iura K, Maekawa A, et al. Histological spectrum of angiofibroma of soft tissue: histological and genetic analysis of 13 cases. Histopathology. 2016;69(3):459–69.
Wang L, Motoi T, Khanin R, Olshen A, Mertens F, Bridge J, et al. Identification of a novel, recurrent HEY1-NCOA2 fusion in mesenchymal chondrosarcoma based on a genome-wide screen of exon-level expression data. Genes Chromosomes Cancer. 2012;51(2):127–39.
MEIS1 Gene. - Meis Homeobox 1 [updated 1/10/2023. https://www.genecards.org/cgi-bin/carddisp.pl?gene=MEIS1.
Aksoz M, Turan RD, Albayrak E, Kocabas F. Emerging roles of Meis1 in Cardiac Regeneration, Stem cells and Cancer. Curr Drug Targets. 2018;19(2):181–90.
Blasi F, Bruckmann C, Penkov D, Dardaei L. A tale of TALE, PREP1, PBX1, and MEIS1: interconnections and competition in cancer. BioEssays. 2017;39(5).
Zhu J, Cui L, Xu A, Yin X, Li F, Gao J. MEIS1 inhibits clear cell renal cell carcinoma cells proliferation and in vitro invasion or migration. BMC Cancer. 2017;17(1):176.
Rad A, Farshchian M, Forghanifard MM, Matin MM, Bahrami AR, Geerts D, et al. Predicting the molecular role of MEIS1 in esophageal squamous cell carcinoma. Tumour Biol. 2016;37(2):1715–25.
Patel AV, Chaney KE, Choi K, Largaespada DA, Kumar AR, Ratner N. An ShRNA screen identifies MEIS1 as a driver of malignant peripheral nerve sheath tumors. EBioMedicine. 2016;9:110–9.
Jones TA, Flomen RH, Senger G, Nizetić D, Sheer D. The homeobox gene MEIS1 is amplified in IMR-32 and highly expressed in other neuroblastoma cell lines. Eur J Cancer. 2000;36(18):2368–74.
Crijns AP, de Graeff P, Geerts D, Ten Hoor KA, Hollema H, van der Sluis T, et al. MEIS and PBX homeobox proteins in ovarian cancer. Eur J Cancer. 2007;43(17):2495–505.
Quiroga-Garza GM, Lajara S, Burgess MA, John I. Distant metastatic potential in primary renal sarcoma with MEIS1–NCOA2 gene fusion. Histopathology. 2021;79(1):117–8.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ZCF performed histologic review of the tumor, immunohistochemical analysis, prepared all figures, and was a major contributor in writing the manuscript, FO performed histologic review of the tumor, immunohistochemical analysis, and was a major contributor in writing the manuscript, BC performed initial histologic review of the tumor and immunohistochemical analysis of the tumor. All authors reviewed the manuscript. MV assisted with finding details regarding specific fusion details. ZCF is the corresponding author.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was given as per institutional policy.
Consent for publication
Consent for publication was given as per institutional policy.
Author’s information
FO is associate professor of pathology at Northwestern University and is a fellowship-trained bone and soft tissue pathologist.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Coty-Fattal, Z., Carter, B., Volek, M.J. et al. Low-grade undifferentiated sarcoma with MEIS1::NCOA2-rearrangement primary to the lung: a case report. Diagn Pathol 19, 65 (2024). https://doi.org/10.1186/s13000-024-01484-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-024-01484-3