Abstract
Background
Mucinous cystadenocarcinoma (MCA) is a very rare form of breast cancer that was first described in 1998. Only 33 cases of primary MCA, including our present case, have been reported thus far. As a consequence, its molecular features, prognosis and treatment regimen are poorly known. Here, we describe a less common presentation of MCA, detail its molecular features, discuss the major differential diagnosis, and provide a brief review of the literature.
Case presentation
A 59-year-old woman presented with a breast lump in which mammography showed a well-defined nodule. Core needle biopsy (CNB) revealed several lesions lined by tall columnar cells with stratification and abundant mucinous secretion; excision was recommended for final diagnosis. The resected specimens showed cavities of different sizes without surrounding myoepithelial cells. The cavities were rich in mucus, and the nuclei were located at the base of the cells, containing intracellular mucus. Immunohistochemical analysis revealed that it was triple-negative breast cancer (TNBC). Next-generation sequencing (NGS) revealed pathogenic mutations in the PIK3CA, KRAS, MAP2K4, RB1, KDR, PKHD1, TERT, and TP53 genes. A diagnosis of MCA was rendered. The patient has been followed up for 108 months to date and showed no signs of recurrence or metastasis.
Conclusion
Our study presents the gene profile of an MCA case with no recurrence or metastatic tendency after 108 months of follow-up, and a review of the literature helps us better understand the clinical, pathologic, and molecular features of this tumor.
Similar content being viewed by others
Introduction
Mucinous cystadenocarcinoma (MCA) is an exceptionally rare variant of primary breast cancer that was first described by Tavassoli et al. in 1998, with approximately 30 cases reported in the English literature [1, 2]. MCAs are characterized by high columnal cells that are rich in intracellular mucin, and the lumen contains a large amount of extracellular mucin. The diagnostic process is challenging in some cases due to overlapping histological characteristics with other lesions. Accurate morphological recognition, understanding the immunohistochemical and molecular features of such diseases, and avoiding improper management are essential.
In the current limited studies, MCAs typically occurred in postmenopausal females with a median age of 61 years [1]. Patients were followed up from 3 to 96 months and had a relatively good prognosis without distant metastasis [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. The entity is usually triple-negative breast cancer (TNBC), which is negative for estrogen receptor (ER), progestogen receptor (PR) and human epidermal growth factor receptor 2 (HER2) expression [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Due to its rarity, the pathogenesis and prognosis of this disease remain poorly characterized. Additionally, a standard treatment regimen is still lacking.
Herein, we report a case of MCA in a 59-year-old woman without evidence of recurrence or metastasis at 108 months after surgery. Genomic profiling was performed, providing evidence for a better understanding of this rare tumor.
Case presentation
A 59-year-old postmenopausal female presented herself to our hospital with a mass on her right breast for 2 weeks. The patient had no history of hormonal treatment or family history of cancer. Clinical examination confirmed a nodule in the right breast, situated at 5 o’clock. Mammography revealed a spherical, well-defined nodule of 3.2*3*2.3 cm (Fig. 1).
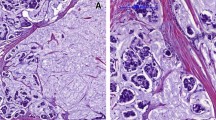
Core needle biopsy (CNB) revealed multiple lesions lined with layered columnar cells and abundant mucous secretion, and the diagnosis of invasive breast cancer with abundant mucous secretion was made. Then, a right lumpectomy along with ipsilateral axillary lymph node dissection was performed. Under macroscopic observation, the tumor was a well-circumscribed mass 3*3*2 cm in size. The cross-section was grayish-white with a moderate myxoid appearance. Microscopically, the tumor consisted of mucus-filled cavities of varying sizes lined with columnar cells (Fig. 2a, b). Tall columnar cells were rich in mucous and had nuclei at the base of the cell. Cells in some areas appeared stratified, protruding into the lumen and even forming branched papillary structures. Nests or papillary cell masses floated in the intracavity mucous lake accompanied by necrosis and inflammatory cell infiltration (Fig. 2c, d). Microscopically, no distinct myoepithelial layer was observed, and subsequent immunohistochemical results also confirmed the absence of myoepithelium (Fig. 3d, e). The cells had mild atypia, and mitotic figures were rare. No common ductal carcinoma in situ (DCIS) existed, and ipsilateral axillary lymph nodes showed no metastasis. The Nottingham grade was 1 (tubule formation = 3, nuclear pleomorphism = 1, and mitotic count = 1), and the pathological stage was T2N0Mx.
a The low-power view illustrates that the surgical specimen was a well-circumscribed tumor. b, c, d The tumor consisted of mucus-filled cavities of varying sizes lined with columnar cells (b, low-power). Tall columnar cells were rich in mucous and had nuclei at the base of the cell. Some areas were stratified, protruding into the lumen and even forming branched papillary structures. Nests or papillary cell masses floated in the intracavity mucous lake accompanied by inflammatory cell infiltration (c, d high-power)
Immunohistochemical features of the lesion. a Cytokeratin 7 was strongly and diffusely positive for neoplastic cells. b The Ki-67 index of the tumor cells. c Overexpression of p53 protein. d Myoepithelial markers were absent (p63). e Myoepithelial markers were absent (calponin). f Focal positive expression of PD-L1 in immune cells within the tumor
Based on these morphological features, a wide range of differential diagnoses included metastatic tumors from the ovaries or pancreas, mucinous carcinoma, mucoceloid lesions, encapsulated papillary carcinoma (EPC) and invasive papillary carcinoma. A broad immunohistochemical panel was performed to narrow the differential diagnosis. The neoplastic cells showed diffuse immunoreactivity for cytokeratin 7 (CK7) (Fig. 3a) and a high Ki-67 index of up to 40% (Fig. 3b). There was no immunoreactivity for ER, PR, HER2, cytokeratin 20 (CK20), CA19-9, CDX-2, Villin, PAX8, GATA3, SOX10, GCDFP-15, mammaglobin, p63 or calponin. Positive immunoreactivity for CK7, negative immunoreactivity for CK20, CA19-9, CDX-2, and Villin, and metastasis from the ovary, pancreas or intestine were excluded. Positron emission tomography (PET)/computed tomography (CT) was performed on the patient, and no other lesions were found, confirming nonmetastatic lesions. A triple-negative immunophenotype and a relatively high Ki-67 index ruled out mucinous carcinoma and EPC, which typically express ER and PR. Mucoceloid lesions of the breast are benign lesions in which myoepithelium is present around the lumen. The absence of myoepithelium also ruled out this diagnosis (Fig. 3d, e). Invasive papillary carcinoma is composed of mildly dilated ducts and microcysts containing a papillary formation without intracellular and extracellular mucus. These cases are usually non-triple-negative phenotypes. Eventually, we favored the diagnosis of MCA based on the morphological and immunohistochemical findings.
Furthermore, 425 genes were sequenced using formalin-fixed and paraffin-embedded (FFPE) tissues and next-generation sequencing (NGS) technology. Recurrent mutations in PIK3CA, KRAS, MAP2K4, RB1, KDR, PKHD1, TERT, and TP53 were identified and are summarized in Table 1. The tumor mutation burden (TMB) was 9.27, and microsatellite instability high (MSI-H) was not detected. P53, RB1 and PD-L1 protein were stained according to the sequencing results. Immunohistochemistry confirmed the overexpression of p53 protein (Fig. 3c) and loss of RB1 protein expression. PD-L1 (sp142) was focally positive in immune cells, and the positive rate was approximately 7% (Fig. 3f). The patient received 6 cycles of adjuvant chemotherapy and was followed up for 108 months, with no signs of recurrence or metastasis.
Discussion
Table 2 summarizes the features of MCAs previously described and our present case [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. To date, only 33 cases, including our present case, have been reported in the English literature [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Overall, MCA predominantly affected perimenopausal or postmenopausal women aged 41 to 96 years [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. The tumor size ranged from 0.8 cm to 19 cm, and there were two cases with multiple nodes [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Metastatic lymph nodes were seen in 5 cases, with no more than 3 lymph nodes involved [2, 4, 13, 20, 21].
The morphological spectrum of MCA ranges from pure MCA and MCA with DCIS to MCA with both DCIS and invasive ductal carcinoma (IDC) [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. The diagnosis of MCA without DCIS is challenging because overlapping morphological features are not uncommon among the entities, suggesting the use of broad immunohistochemical biomarkers. The combination of clinical history, morphology, and immunohistochemistry is helpful to confirm the diagnosis. The immunohistochemical staining of our present case showed that only CK7 was positive. To exclude ovarian or pancreatic metastatic cancer, we added markers of ovarian and pancreatic origin, including CK20, CA19-9, CDX-2, Villin and PAX8, all of which were negative. In terms of the immunohistochemical phenotype, ovarian and pancreatic mucinous adenocarcinomas are usually CK7 + /CK20 + , while MCA of the breast is usually CK7 + and CK20– [24]. Therefore, a group of biomarkers is recommended for differential diagnosis, in which CK7 + /CK20- may assist in the diagnosis of the primary breast lesion, but a detailed clinical evaluation is required [24]. Additionally, various primary breast lesions are considered for the differential diagnosis of MCAs, including mucoceloid lesions, mucinous carcinoma, EPC and invasive papillary carcinoma [10, 13, 30,31,32]. The presence of mucinous cells, invasive growth behavior, and loss of myoepithelial expression are the first characteristics used to rule out mucinous cyst lesions [31]. The presence of intracellular and extracellular mucus and a triple-negative phenotype exclude the diagnosis of invasive papillary carcinoma [30, 33]. Additionally, the triple-negative phenotype and a relatively high Ki-67 index help to exclude mucinous carcinoma and EPC [10, 13, 30,31,32].
For the molecular subtype, two hormone receptor-positive, twenty-two triple-negative and four HER2 overexpression cases were among the known molecular phenotypes [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. The Ki-67 index ranged from 3 to 99%, with most cases having a Ki-67 index higher than 30% [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Only one case recurred eight years after surgery, and no cases of metastasis have been reported [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. One reason is that such tumors may be indolent tumors. However, unlike that in other low-grade indolent TNBCs, Ki-67 in most MCAs is relatively high. The other reason is that only three cases were followed up for more than five years, and the follow-up times of the remaining cases were approximately 1–2 years [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. The biological behavior of the tumor was not fully demonstrated during the short follow-up period. MCAs may have a long-term risk of local recurrence, and whether they have metastatic potential requires more accumulated cases. Many clinicopathological parameters, including ER, PR, HER2, Ki-67, tumor size, tumor grade, lymph node status, and vascular invasion, have prognostic significance in breast cancer [34]. For TNBC, the prognostic value of parameters such as tumor grade, tumor size and lymph node status are still questionable; in contrast, high expression of Ki-67 and overexpression of p53 protein may contribute to poor prognosis in such tumors [35, 36]. Our case was a TNBC with high expression of the Ki-67 index and overexpression of p53 protein, suggesting that the patient had some adverse prognostic factors. The only reported recurrent case was a microinvasive breast cancer with the triple-negative phenotype and a small tumor size, but the expression of Ki-67 and p53 protein was unknown [21]. Therefore, more long-term follow-up cases are needed to verify the prognostic factors of MCAs.
Surgical resection was performed for all cases, and chemotherapy and radiotherapy were performed in a few cases [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Hormone therapy and HER2 targeted therapy have been reported for hormone receptor-positive and HER2 + cases [14, 19, 24]. In the only recurrent case, which was mostly DCIS with only a 5 mm invasive MCA, mastectomy and axillary lymph node dissection were performed without adjunct therapy [21]. Despite the small size of the tumor and the presence of isolated tumor cells in a sentinel lymph node at the time of diagnosis, the tumor recurred 8 years later [21]. Our patient underwent six cycles of chemotherapy and showed no recurrence or metastatic potential thus far. Individualized treatment regimens are still lacking.
Table 1 shows the genomes of only two cases at present. Common genetic variants were TP53 and RB1, which suggests that alterations in tumor suppressor genes, particularly those involved in regulating the cell cycle and chromatin remodeling, are associated with the occurrence of this tumor [18]. In a large NGS project involving more than 10,000 patients with metastatic cancer, TP53, KRAS, RB1 and PIK3CA were among the top 10 most commonly mutated genes in 62 major solid tumor entities [37]. TP53 mutations lead to abnormal protein function, and immunohistochemistry showed that p53 protein was overexpressed in our case, which may affect downstream signaling pathways and participate in tumor development [38]. RB1 mutation may lead to loss of the tumor suppressor function of the RB1 protein, thus promoting excessive cell proliferation, avoiding apoptosis, delaying cell senescence, and participating in the occurrence and development of tumors [39]. Immunohistochemical staining also confirmed RB1 protein loss in our case. Missense mutation in PIK3CA (c.3140A > G, p. H1047R), which is located in the phosphatidylinositol 3/4 kinase domain, is a common activation mutation of the PIK3CA gene in breast cancer. By enhancing PI3K lipid kinase activity, the PI3K/AKT signaling pathway can be activated to promote the invasion and metastasis of cancer cells and participate in the occurrence and development of tumors [40]. The mutation site (c.35G > T, p.G12V) is the hot spot mutation site of the KRAS gene, which has been reported in a variety of tumors, including breast cancer. This mutation can cause impairment of the GP-mediated hydrolytic function of GTP, resulting in increased intracellular RAS-GTP levels, thereby activating the RAS pathway [41]. In addition to mutations in MAP2K4, mutations in KDR, PKHD1 and TERT may also participate in tumorigenesis. The MAP2K4 (c.257_258del, p. R86Tfs*7) mutation may reduce the function of MKK4 protein, enhance its mediated cell invasion and participate in the occurrence and development of tumors by promoting the expression of PPARγ [39]. The significance of the other mutated genes is unclear, and they may be related to tumor formation. The gene profile of our case is closer to that of TNBC, especially high-grade TNBC, in which PIK3CA, TP53, KRAS and RB1 mutations are commonly present [42]. Similarly, this case had a relatively high TMB value of 9.27. According to the immune and gene phenotypes, we further detected PD-L1 (sp142) in this case, and the results showed that the expression rate of PD-L1 (sp142) in immune cells was more than 1%. The tumor genome provided us with other therapeutic clues, such as PIK3CA and KRAS, which have corresponding targeted inhibitors.
Conclusion
Mucinous cystadenocarcinoma (MCA) is a rare breast cancer, with only approximately 30 cases reported. Here, we present the gene profile of an MCA case with no recurrence or metastatic tendency after 108 months of follow-up, and a review of the literature helps us better understand the clinical, pathologic, and molecular features of this tumor. A wide panel of immunohistochemical biomarkers should be applied to achieve a correct diagnosis. The genomic characteristics of this tumor are similar to those of common TNBC, in which PIK3CA, TP53, KRAS and RB1 mutations are commonly present. A better understanding of the genomic characteristics of such tumors could help predict prognosis and guide treatment.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Abbreviations
- MCA:
-
Mucinous cystadenocarcinoma
- CNB:
-
Core needle biopsy
- NGS:
-
Next-generation sequencing
- TNBC:
-
Triple-negative breast cancer
- EPC:
-
Encapsulated papillary carcinoma
- CK7:
-
Cytokeratin 7
- CK20:
-
Cytokeratin 20
- PET/CT:
-
Positron emission tomography/computed tomography
- FFPE:
-
Formalin-fixed and paraffin-embedded
- TMB:
-
Tumor mutation burden
References
Rakha EA, Reisilho JS, Sasano H, Wu Y. Breast tumours. In: WHO classifcation of tumours series. 5th ed. 2019.
Koenig C, Tavassoli FA.Mucinous Cystadenocarcinoma of the breast. Am J Surg Pathol. 1998;22(6):698–703.
Coyne JD, Irion L. Mammary mucinous cystadenocarcinoma. Histopathology. 2006;49(6):659–60.
Deng Y, Xue D, Wang X, Xu S, Ao Q, Hu Z, Wang G. Mucinous cystadenocarcinoma of the breast with a basal-like immunophenotype. Pathol Int. 2012;62(6):429–32.
Gulwani H, Bhalla S. Mucinous cystadenocarcinoma: a rare primary malignant tumor of the breast. Indian J Pathol Microbiol. 2010;53(1):200–2.
Domoto H, Terahata S, Yamazaki T, Sato K, Takeo H, Tamai S. Mucinous cystadenocarcinoma of the breast showing sulfomucin production. Histopathol. 2000;26(6):567–9.
Hu Y, Tian C, Zhang X, Wei Q, Bian Y. 18F-FDG PET/CT Findings in a Patient With Primary Mucinous Cystadenocarcinoma of the Breast. Clin Nucl Med. 2020;45(2):159–60.
Jain E, Kumar A, Jain R, Sharma S. Primary Mucinous Cystadenocarcinoma of the Breast: A Rare Case Report With Review of Literature. Int J Surg Pathol. 2021;29(7):740–6.
Kamrani G, Nikbakhsh N, Hosseini A, Ghorbani H, Arefisigaroudi N, Davarian A. Mucinous cystadenocarcinoma of breast in a 69-year-old woman with positive hormone receptors, the first case reported. Caspian J Intern Med. 2021;12(Suppl 2):S444–6.
Kaur K, Shah A, Gandhi J, Trivedi P.Mucinous cystadenocarcinoma of the breast: a new entity with broad differentials—a case report. J Egypt Natl Canc Inst. 2022;34(2):9.
Kaur M, Tiwana KK, Singla N. Rare Breast Malignancy Subtypes: A Cytological, Histological, and Immunohistochemical Correlation. Niger J Surg. 2019;25(1):70–5.
Kim SE, Park JH, Hong S, Koo JS, Jeong J, Jung WH. Primary Mucinous Cystadenocarcinoma of the Breast: Cytologic Finding and Expression of MUC5 Are Different from Mucinous Carcinoma. Korean J Pathol. 2012;46(6):611–6.
Koufopoulos N, Goudeli C, Syrios J, Filopoulos E, Khaldi L. Mucinous cystadenocarcinoma of the breast: the challenge of diagnosing a rare entity. Rare Tumors. 2017;9(3):7016.
Kucukzeybek BB, Yigit S, Sari AA, Rezanko T, Durak E, Sadullahoglu C. Primary mucinous cystadenocarcinoma of the breast with amplification of the HER2 gene confirmed by FISH - case report and review of the literature. Pol J Pathol. 2014;65(1):70–3.
Lee SH, Chaung CR. Mucinous metaplasia of breast carcinoma with macrocystic transformation resembling ovarian mucinous cystadenocarcinoma in a case of synchronous bilateral infiltrating ductal carcinoma. Pathol Int. 2008;58(9):601–5.
Li X, Peng J, Zhang Z, Zhang Y. Mammary mucinous cystadenocarcinoma. Breast J. 2012;18(3):282–3.
Lin DL, Hu JL, Shao SH, Sun DM, Wang JG. Primary mucinous cystadenocarcinoma of the breast with endocervical-like mucinous epithelium. Breast Care (Basel). 2013;8(6):445–7.
Lin LH, Hernandez O, Zhu K, Guth A, Cotzia P, Darvishian F. Genetic profile of primary mucinous cystadenocarcinoma of the breast-A case report. Breast J. 2021;27(9):731–4.
Sun M, Su ST, Liu QP, Li QL, Wang KS: Mammary synchronous mucinous cystadenocarcinoma and columnar cell mucinous carcinoma: a case report. Int J Clin Exp Pathol. 2020;13(9):2381–6.
Honma N, Sakamoto G, Ikenaga M, Kuroiwa K, Younes M, Takubo K. Mucinous cystadenocarcinoma of the breast: a case report and review of the literature. Arch Pathol Lab Med. 2003;127(8):1031–3.
Nayak A, Bleiweiss IJ, Dumoff K, Bhuiya TA. Mucinous Cystadenocarcinoma of the Breast: Report of 2 Cases Including One With Long-Term Local Recurrence. Int J Surg Pathol. 2018;26(8):749–57.
Rosen PP, Scott M. Cystic Hypersecretory Duct Carcinoma of the Breast. Am J Surg Pathol. 1984;8(1):31–41.
Petersson F, Pang B, Thamboo TP, Putti TC. Mucinous cystadenocarcinoma of the breast with amplification of the HER2-gene confirmed by FISH: The first case reported. Hum Pathol. 2010;41(6):910–3.
Rakici S, Gönüllü G, Gürsel SB, Yildiz L, Bayrak IK, Yücel I. Mucinous Cystadenocarcinoma of the Breast with Estrogen Receptor Expression: A Case Report and Review of the Literature. Case Rep Oncol. 2009;2(3):210–6.
Sentani K, Tashiro T, Uraoka N, Aosaki Y, Yano S, Takaeko F, Yasui W. Primary mammary mucinous cystadenocarcinoma: cytological and histological findings. Diagn Cytopathol. 2012;40(7):624–8.
Seong MJ, Ko EY, Han BK, Cho SY, Cho EY, Lee SK, Lee JE. Radiologic Findings of Primary Mucinous Cystadenocarcinoma of the Breast: A Report of Two Cases and a Literature Review. J Breast Cancer. 2016;19(3):330–3.
Chen WY, Chen CS, Chen HC, Hung YJ, Chu JS. Mucinous cystadenocarcinoma of the breast coexisting with infiltrating ductal carcinoma. Pathol Int. 2004;54(10):781–6.
Witherspoon LE, Oxenhandler RW. A rare tumor: mucinous cystadenocarcinoma of the breast. Am Surg. 2015;81(3):E106-108.
Wang X, Li YJ, Zhao P, Jia HQ, Dong XN, Zhang LX, Wang CQ. Primary mucinous cystadenocarcinoma of the breast: a clinicopathologic analysis of one case and review of the literature. Int J Clin Exp Pathol. 2020;13(10):2562–8.
Tay TKY, Tan PH. Papillary neoplasms of the breast-reviewing the spectrum. Mod Pathol. 2021;34(6):1044–61.
Ginter PS, Tang X, Shin SJ. A review of mucinous lesions of the breast. Breast J. 2020;26(6):1168–78.
Chen SJ, Wang J, Yang L, Ji M, Chen S. Comparative analysis of clinicopathologic characteristics and molecular subtypes of invasive papillary carcinoma of the breast and invasive ductal carcinoma: results from SEER database. J BUON. 2021;26(5):1991–2002.
Tsoukalas N, Kiakou M, Tolia M, Kostakis ID, Galanopoulos M, Nakos G, Tryfonopoulos D, Kyrgias G, Koumakis G. Mucinous breast carcinoma with tall columnar cells. Ann R Coll Surg Engl. 2018;100(5):e132–5.
Oshiro C, Yamasaki M, Noda Y, Nishimae A, Takahashi H, Inaji H. Comparative evaluation of nuclear and histological grades as prognostic factors for invasive breast cancer. Breast Cancer. 2020;27(5):947–53.
Kumar P, Aggarwal R. An overview of triple-negative breast cancer. Arch Gynecol Obstet. 2015;293(2):247–69.
Aleskandarany MA, Green AR, Benhasouna AA, Barros FF, Neal K, Reis-Filho JS, Ellis IO, Rakha EA. Prognostic value of proliferation assay in the luminal, HER2-positive, and triple-negative biologic classes of breast cancer. Breast Cancer Res. 2012;14(1):R3.
Zehir A, Benayed R, Shah RH, Syed A, Middha S, Kim HR, Srinivasan P, Gao J, Chakravarty D, Devlin SM, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23(6):703–13.
Kato S, Han SY, Liu W, Otsuka K, Shibata H, Kanamaru R, Ishioka C. Understanding the function-structure and function-mutation relationships of p53 tumor suppressor protein by high-resolution missense mutation analysis. Proc Natl Acad Sci U S A. 2003;100(14):8424–9.
Hollestelle A, Nagel JH, Smid M, Lam S, Elstrodt F, Wasielewski M, Ng SS, French PJ, Peeters JK, Rozendaal MJ, et al. Distinct gene mutation profiles among luminal-type and basal-type breast cancer cell lines. Breast Cancer Res Treat. 2010;121(1):53–64.
Janku F, Wheler JJ, Naing A, Falchook GS, Hong DS, Stepanek VM, Fu SQ, Piha-Paul SA, Lee JJ, Luthra R, et al. PIK3CA mutation H1047R is associated with response to PI3K/AKT/mTOR signaling pathway inhibitors in early-phase clinical trials. Cancer Res. 2013;73(1):276–84.
Modest DP, Camaj P, Heinemann V, Schwarz B, Jung A, Laubender RP, Gamba S, Haertl C, Stintzing S, Primo S, Bruns CJ. KRAS allel-specific activity of sunitinib in an isogenic disease model of colorectal cancer. J Cancer Res Clin Oncol. 2013;139(6):953–61.
Geyer FC, Pareja F, Weigelt B, Rakha E, Ellis IO, Schnitt SJ, Reis-Filho JS. The Spectrum of Triple-Negative Breast Disease: High- and Low-Grade Lesions. Am J Pathol. 2017;187(10):2139–51.
Funding
The study was supported by Changzhou Science and Technology Project (QN202114), a project funded by Changzhou Health Commission.
Author information
Authors and Affiliations
Contributions
All authors contributed in the writing of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved the Third Affiliated Hospital of Soochow University Institutional Review Board.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lei, T., Shi, Y.Q. & Chen, T.B. Mammary mucinous cystadenocarcinoma with long-term follow-up: molecular information and literature review. Diagn Pathol 18, 13 (2023). https://doi.org/10.1186/s13000-023-01302-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-023-01302-2