Abstract
Degenerative cervical myelopathy (DCM) is the most prevalent cause of spinal cord dysfunction in the aging population. Significant neurological deficits may result from a delayed diagnosis as well as inadequate neurological recovery following surgical decompression. Here, we review the pathophysiology of DCM with an emphasis on how blood-spinal cord barrier (BSCB) disruption is a critical yet neglected pathological feature affecting prognosis. In patients suffering from DCM, compromise of the BSCB is evidenced by elevated cerebrospinal fluid (CSF) to serum protein ratios and abnormal contrast-enhancement upon magnetic resonance imaging (MRI). In animal model correlates, there is histological evidence of increased extravasation of tissue dyes and serum contents, and pathological changes to the neurovascular unit. BSCB dysfunction is the likely culprit for ischemia–reperfusion injury following surgical decompression, which can result in devastating neurological sequelae. As there are currently no therapeutic approaches specifically targeting BSCB reconstitution, we conclude the review by discussing potential interventions harnessed for this purpose.
Similar content being viewed by others
Introduction
Degenerative cervical myelopathy (DCM) is the commonest cause of spinal cord dysfunction in developed countries due to age-related changes within the cervical spinal canal [1, 2]. Chronic mechanical compression of the spinal cord results from encroachment by surrounding structures. Neurological manifestations include sensory impairment, decline in hand dexterity, limb weakness, gait instability, and even tetraplegia if left untreated [3, 4]. Average age at diagnosis is estimated to be 65 and the disease classically exhibits a steady, stepwise deterioration with stable intervening periods [5,6,7,8]. There remains inadequate awareness of DCM amongst the public as well as primary health care providers, resulting in delay in diagnosis or misdiagnosis [1, 9]. Although operative treatment via cervical decompression is effective, full recovery is uncommon whilst non-operative treatment modalities show limited clinical efficacy [10,11,12]. As a disease with a substantial and increasing global burden, understanding the mechanisms contributing to disease pathology is essential to advancing diagnosis, treatment, and recovery. In this review, we delve into the significance of blood-spinal cord barrier (BSCB) disruption to DCM pathophysiology, whilst proposing novel BSCB-based treatment strategies that may be beneficial to management.
The blood-spinal cord barrier in health and disease
BSCB architecture
The BSCB is generally considered to be an extension of the blood brain barrier (BBB). They share the same ultrastructural arrangement, although differences in morphology and function do exist as will be discussed in the following section. The BSCB is comprised of capillary endothelial cells and its accompanying basement membrane, pericytes, and astrocytic end-feet. Endothelia over the BSCB are distinct in being non-fenestrated. They form tight junctions (TJs) with adjacent cells [13,14,15,16], and compared to the endothelia of other tissues possess a low density of pinocytic vacuoles and a high number of cytosolic mitochondria [17, 18]. The basement membrane is composed of laminins, collagen IV isoforms, nidogens, and heparan sulphate proteoglycans (HSPGs) to form a three-dimensional matrix [19, 20] and is maintained by endothelial cells as well as embedded pericytes [21, 22]. Astrocytes encircle endothelia, contributing to the basement membrane, and enwrap neuronal synapses to enable neurovascular coupling [19, 20, 23]. This arrangement allows for neurohumoral regulation of blood flow, controlling the inflow and efflux of nutrients, energy stores, metabolites, and toxins within the neurovascular unit (NVU) [24,25,26,27]. The spinal cord perivascular space is continuous with the subarachnoid space [16]. At the capillary level, the basal lamina of endothelial cells is in direct contact with the glia limitans. Upon inflammation, basal lamina may separate into two layers, forming a transient perivascular space or “loop” that facilitates leukocyte infiltration [15, 20].
BSCB vs BBB
Animal studies indicate that the BSCB has increased permeability to serum biomolecules, cytokines, and growth factors, such as mannitol, inulin, interferon (IFN) α/γ, and nerve growth factor (NGF) compared to the BBB [28,29,30]. This may be explained by lower expression of tight and adherent junction proteins in spinal cord endothelial cells compared to brain endothelial cells, which is associated with increased paracellular transport [31,32,33]. Mouse pericyte number and coverage within the BSCB is reduced in comparison to the BBB, which is associated with increased endothelial transcytosis and barrier permeability [34, 35]. Genes associated with astrogliosis i.e. GFAP, IL-6, and STAT3, are expressed at higher levels in mouse spinal cord astrocytes compared to astrocytes in the brain. Enhanced GFAP expression may help the spinal cord to withstand bending and torque [36], allowing the BSCB to tolerate mechanical stresses associated with vertebral movement. Significantly higher mitochondria content was observed in rat spinal cord endothelial cells compared to endothelial cells of the cerebral cortex and cerebellum, which may indicate more robust active transport systems and diminished vesicular transport [17, 37].
BSCB disruption in traumatic spinal cord injury
In acute spinal cord injury (SCI), primary injury causes immediate physical disruption of the BSCB [38, 39]. Edema of spinal cord parenchyma is an early macroscopic manifestation of barrier disruption that is correlated with contusion force [40,41,42,43]. Hemolysates from extravasated erythrocytes and serum macromolecules such as serine proteases perpetuate neuroinflammation as well as oxidative stress [43, 44]. Even after filtration of high molecular weight proteins (> 10 kDa), serum contents cause apoptosis of cultured spinal cord neurons, likely due to the presence of neurotoxic depolarizing agents such as glutamate [41, 42]. Animal models have revealed that cord edema peaks at Day 5 post-injury [38], whilst permeability to large serum macromolecules resolves around 2 weeks post-SCI. Nevertheless, permeability to smaller molecules persists especially in areas with microglial aggregates, implying lasting alterations to BSCB permeability [45, 46]. There is evidence indicating that BSCB alteration is a key factor in the pathogenesis of post-SCI syringomyelia, which is characterized by the formation of cystic cavities over the lesion epicentre [46,47,48].
BSCB disruption in neurodegenerative and autoimmune diseases
BSCB disruption is also a key factor contributing to the pathogenesis of amyotrophic lateral sclerosis (ALS), a progressive and fatal neurodegenerative disorder affecting upper and lower motor neurons located in the brain and spinal cord [49, 50]. In necropsy specimens of spinal cords obtained from ALS patients, there was evidence of cytotoxic lipofuscin deposits within the capillaries, decreased endothelial expression of TJs, and increased infiltration by leucocytes, erythrocytes, and serum macromolecules [51,52,53,54]. Pericyte and astrocyte end-feet degeneration were also observed at sites corresponding to vessel rupture [49, 55, 56]. Likewise, in the SOD1 mouse ALS model, impaired BSCB function and vascular pathology preceded motor neuron degeneration, which was evidenced by vascular leakage and loss of TJs throughout the spinal cord [52, 57]. Histological and imaging studies on experimental autoimmune encephalomyelitis (EAE) animal models of multiple sclerosis (MS) showed evidence of BSCB disruption during early disease, sometimes preceding neurological manifestations [58,59,60,61]. However, clinical studies on the impact of BSCB disruption in MS pathogenesis is lacking. BSCB disruption in DCM, traumatic SCI, and neurodegenerative disease (using ALS as an example) is compared in Table 1.
Pathophysiology of degenerative cervical myelopathy
Animal models of DCM
In addition to necropsy specimens, animal model correlates of DCM have been invaluable to understanding disease pathophysiology, and in highlighting differences from acute traumatic SCI [66]. Acute traumatic SCI models result in immediate neurological deterioration (i.e. via cord contusion, distraction, and transection) [67], whilst animal models mimicking DCM cause progressive neurological compromise following chronic compression. Murine models are most frequently utilized. Twy/twy mice possess an autosomal recessive, non-sense mutation at the Npps (nucleotide pyrophosphatase) gene locus [68]. Failure of the Npps enzyme to produce inorganic phosphatase, a major inhibitor of calcification, causes progressive soft-tissue calcification and bone mineralization to compromise the cervical canal [69]. Limitations to this model exist, in that the site of maximal compression is within the upper cervical spine which is atypical for DCM, and decompression of the ossified spinal canal is technically infeasible. In rats, implantation of expandable polymers dorsal to the spinal cord following a laminectomy is a common experimental setup, and decompression may be modelled via polymer removal. Implant positioning, size, and swell rate are important variables to control [70]. The rate and region of cervical compression is better controlled in larger animal models following polymer implantation, and there are means to mimic ventral compression for example via screw insertion from the anterior vertebral body, although larger animals are costly, may not be readily available, and present more ethical concerns [70,71,72,73,74,75,76].
Mechanical compression
DCM is a multifactorial disorder instigated by static and dynamic mechanical compression of the cervical spinal cord. Causes for static compression include degenerative disc disease (DDD) and congenital cervical stenosis. DDD also results in cervical microinstability, and over time this causes secondary spondylotic changes such as cervical facet and posterior longitudinal ligament hypertrophy to further mechanical compression [77]. Dynamic factors, for example in occupations requiring prolonged and exaggerated movement of the cervical spine, may further mechanical insult [78, 79]. Biological processes resulting from chronic compression include tissue ischemia, BSCB disruption, and neuroinflammation, culminating in the loss of neurons and glia. These have been summarized in Fig. 1 and will be discussed in further detail below.
Blood spinal cord barrier disruption during and after cervical decompression in degenerative cervical myelopathy. Spinal cord perfusion is maintained by the anterior spinal artery, left/right posterior spinal arteries, and their associated veins. Chronic cervical cord compression (schematically represented as anterior compression alone) causes pathological changes to these supplying vessels and disrupts the BSCB. Spinal cord tissues remain hypoperfused despite vascular remodeling. Following surgical decompression, there is sudden restoration in blood flow but the BSCB remains hyperpermeable. This predisposes the cord to reperfusion injury and impairs neurological recovery, although the underlying mechanical compression has been relieved. Bright red and blue colors denote healthy blood vessels, while dark red and blue colors indicate blood vessels with compromised blood supply. Pink-shaded regions indicate mildly hypoxic regions, while darker pink-shaded regions indicate ischemic regions with severe ischemia
Ischemia
Spinal cord perfusion is compromised in DCM as evidenced by distorted anterior spinal and radicular arteries upon necropsy specimens [78]. Cord perfusion may be further compromised by vessel wall thickening and hyalinization [80,81,82]. Evidence of ischemic injury is manifest early in medial grey and white matter tracts, which are supplied by terminal branches of the anterior spinal artery [80]. Corresponding to this topography, the lateral corticospinal tract is first to be affected in DCM [83,84,85,86]. In the polymer-implanted rat DCM model, a significant reduction in the number of blood vessels in white and grey matter of the cervical spinal cord was observed [75]. Ischemic injury precipitates apoptosis and inflammation, which can proceed to necroptosis as cord compression worsens [66, 87].
BSCB disruption
It remains uncertain whether mechanical compression is an independent factor for BSCB disruption, or whether its effects are exerted secondary to compression-induced ischemia. Regarding pathophysiology of the latter, spinal cord ischemia causes pericytes located at the BSCB to express hypoxia inducible factor-1 (HIF-1). HIF-1 dilates blood vessels and disrupts endothelial TJs, thereby increasing BSCB permeability [88]. Mild chronic spinal cord hypoxia in mice was sufficient to induce vascular leakage, resulting in extravasation of neurotoxic serum macromolecules and activation of microglia [89]. Another mechanism for BSCB breakdown is the upregulation of matrix metallopeptidase 9 (MMP-9) within the spinal cord of DCM patients and animal model correlates [90,91,92]. MMP9 is a proteolytic enzyme which is expressed in neutrophils and endothelial cells, and by degrading the basement membrane, compromises BSCB integrity [91]. BSCB disruption causes an influx of inflammatory cells [87], exposes the spinal cord to neurotoxic serum contents, impairs clearance of metabolic waste, and result in the accumulation of protein aggregates which generate oxidative stress [93, 94]. This instigates further injury to the BSCB, forming a vicious cycle.
Inflammation
Inflammation in DCM occurs consequent to chronic ischemia and BSCB disruption [77]. In animal models, CNS hypoxia induces neuroglia to release proinflammatory cytokines such as IL-1β, IL-6, IL-8, FasL, and TNF-α [90, 95,96,97]. These cytokines, together with nuclear factor kappa B (NF-κB), MMP-2, and urokinase-type plasminogen activator (u-PA) are also detected in DCM necropsy specimens [92, 98]. Proinflammatory cytokines increase macrophage recruitment, infiltration, and activation, as evidenced by a 12-fold increase in Iba1 expression in DCM spinal cords compared to controls [75]. In the experimental hyperostotic (twy/twy) DCM mouse model, macrophages within the cord parenchyma are predominantly of the cytotoxic M1 phenotype [99].
Apoptosis
There are multiple disease processes leading to cellular apoptosis in DCM. Firstly, proinflammatory cytokines and neurotoxins can directly bind to cell death receptors upon neurons and glia [41, 100,101,102,103,104]. Secondly, loss of cellular homeostasis from ischemia can activate apoptotic pathways in neural cells by causing membrane depolarization, Ca2+ influx, and glutamate release [105]. Lastly, mechanical compression can cause cytoskeletal degradation and result in calponin-mediated neuronal apoptosis [106]. Evidence for activation of TNF-α, MAPK, and FasL mediated apoptotic pathways have been demonstrated in both animal models and human specimens. In the twy/twy mouse, TNF-α signaling mediated oligodendrocyte apoptosis [107], as did mitogen-activated protein kinase (MAPK) pathways involving ASK1, JNK, and p38 [108]. In a necropsy study, FasL-mediated apoptosis was implicated in mediating neuronal and oligodendrocyte apoptosis, and FasL neutralization led to increased cell survival and improvement in functional recovery in the animal model correlate [90].
BSCB dysfunction during different phases of DCM
Ongoing mechanical compression
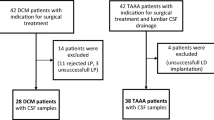
Literature indicates that the extent of BSCB dysfunction is correlated with DCM disease severity. CSF/serum ratios of albumin and IgG in mild-to-moderate DCM patients are only marginally increased compared to normal patients [109]. A systematic review on the disease progression of DCM patients concluded that 38–80% of patients with mild DCM and managed non-operatively improved neurologically or remained unchanged, suggesting that an equilibrium or reconstitution of BSCB function can occur within this patient subset [110]. In severe DCM, CSF/serum ratios of albumin and IgG are over two-fold higher when compared to normal controls, indicating significant barrier compromise [109]. An imaging correlate of BSCB breakdown is T1-weighted hyperintensity with Gd-DTPA enhancement, which indicates spinal cord edema [111,112,113,114,115]. In the rat insertable polymer DCM model, BSCB histopathology was characterised by swollen endothelial cells filled with caveolae-like vesicles, abnormal TJs with large gaps, pericyte enlargement, swollen perivascular astrocytes with disrupted mitochondria, and thickened basement membrane [74, 116, 117]. Rat disease models also exhibit increased extravasation of serum Evans Blue, markedly impaired angiogenesis, and decreased endothelial barrier protein (EBA) immunopositivity [74, 75].
BSCB function following surgical decompression
Patients with severe or rapidly progressive DCM are prone to exhibit poor neurological recovery [118,119,120]. A particular disastrous manifestation following surgery is known as White Cord Syndrome (WCS). WCS is so-named due to the de novo appearance of white T2 hyperintense lesions upon post-operative MRI images that accompany neurological deterioration with onset typically within 24-h of decompression [121, 122]. It is hypothesized that WCS occurs due to reperfusion injury to the spinal cord, which initiates inflammatory and apoptotic cascades [123, 124]. Whilst WCS only affects 0.3% of patients, the recovery trajectory of many more is likely affected by a leaky BSCB.
Is the BSCB reconstituted following surgical decompression?
Clinical evidence suggests that BSCB function is largely intact in mild DCM [109]. Additionally, a cohort with an averaged JOA score of moderate severity demonstrated barrier reconstitution at 3-months post-decompression, with JOA improvement correlating with the extent of barrier recovery [125]. In severe DCM, chronic BSCB disruption is suggested by T1-weighted hyperintensity with Gd-DTPA enhancement persisting for months, even after the onset of neurological recovery [112, 126, 127]. In the insertable polymer rat model, hypervascularization of spinal cord regions adjacent to the compression region was observed with a concomitant increase in Evans Blue dye extravasation [74]. Therefore, neovascularization and altered blood flow in response to chronic ischemia may attenuate capacity for vascular remodelling following decompression [74, 80, 82, 128, 129]. Figure 2 is a schematic diagram postulating the status of the blood spinal cord barrier and spinal cord vasculature during compression and decompression, when the BSCB fails to be reconstituted.
Components of the blood spinal cord barrier (BSCB) and therapeutic strategies for BSCB reconstitution in degenerative cervical myelopathy (DCM). Left panel—At the BSCB, the presence of non-fenestrated endothelial cells establishes tight junctions that heavily restrict paracellular transport. At the capillary level, the basement membrane is closely associated with astrocyte end-feet, resulting in the elimination of the perivascular space. Pericytes, embedded within the basement membrane, assume a crucial role in facilitating endothelial cell maturation, supporting the basement membrane, and potentially modulating blood flow. Disruption of the BSCB integrity is characterized by the thickening or swelling of the basement membrane, endothelial cells, pericytes, and astrocytes. Deterioration of the tight junctions leads to the leakage of serum contents into the surrounding tissues. Inflammation leads to the transient formation of the perivascular space at the capillary level, thereby enabling leukocytes infiltration into the spinal cord parenchyma. Right panel—The treatment modalities mentioned in this figure are elaborated in the main text
Potential therapeutic strategies to ameliorate BSCB Disruption
An overview of DCM management at present
At present, patients with radiological cervical canal stenosis and moderate to severe neurological impairment, often defined as having a JOA score of 13/17 or less, are recommended to receive surgery. Improvement in neurological function has been reported after surgery for over 70% of patients, most notably over the upper limb, followed by the lower limb and sphincters [130]. Nevertheless, patients with severe DCM often report residual sensory deficits or limb spasticity and incoordination [131]. Factors most strongly predictive of neurological outcomes following surgery include preoperative neurological severity and duration of symptoms [132]. Late-onset neurological deterioration may also occur despite adequate mechanical decompression [133, 134]. There is insufficient evidence to support the long-term efficacy of non-operative management approaches for DCM such as physiotherapy, nutritional supplementation, use of analgesics and non-steroidal anti-inflammatory drugs (NSAIDs), cervical steroid injections (CSIs), traction, and acupuncture [10, 135,136,137]. Few DCM-related therapeutics have undergone clinical testing. Of note, a Phase III trial on the safety and efficacy of peri-operative riluzole has been recently completed for DCM patients undergoing decompression [138]. Riluzole is a neuroprotective agent approved for clinical use in ALS, which acts by mitigating glutamate-induced excitotoxicity in the CNS [139, 140]. Although riluzole did not improve neurological outcomes, reduction in neck pain was observed. There remains a clinical necessity to identity adjuncts to surgical decompression especially amongst patient groups with i) mild disease yet to require surgery, ii) non-recovery / deterioration after surgery, and iii) at-risk groups for poor surgical outcomes. As summarised in Table 2 and Fig. 3, we subsequently discuss potential strategies to promote BSCB reconstitution in DCM.
Cell therapy
Delivery of cells such as mesenchymal stem cells (MSCs) or neural stem cells (NSCs) into the spinal cord parenchyma may facilitate BSCB recovery via direct engraftment, trophic support, and immunomodulation [141,142,143]. NSCs and MSCs express PDGF which is a key marker delineating capillary pericytes [144,145,146,147,148]. Transplanted NSCs have been demonstrated to engraft into the perivascular niche and differentiate into PDGFRβ + CNS pericytes, and in doing facilitate angiogenesis, suppress neuroinflammation, and induce NVU maturation [141, 149,150,151,152]. Pericytes are descended from the neuroectoderm during development, as are a subpopulation of MSCs [153], thereby explaining their emergence from transplanted progenitors [144, 154, 155]. Exosomes provide an alternative to whole cells in facilitating BSCB reconstitution. As an example, bone marrow MSC-derived exosomes significantly increased TJ expression, promoted remyelination, and decreased production of MMP-9 [156] in a diabetic stroke model. Future cell-based studies focusing on BSCB pathology and reconstitution are essential to establish preclinical efficacy.
Growth factors and mitogenic agents
Growth factors and mitogenic agents can support the BSCB by inducing proliferation and maturation of cells composing the BSCB, such as pericytes, astrocytes, and endothelium, thereby facilitating reconstitution [157,158,159,160]. Such restorative factors include platelet derived-growth factor-BB (PDGF-BB), fibroblast growth factors (FGF), epidermal growth factor (EGFs), and adropin [161,162,163,164,165,166,167,168,169,170,171,172,173]. Despite promising results from preclinical studies and early clinical trials, translation of bFGF therapy into spinal cord diseases has been slow [159]. Translational research into EGF and PDGF-BB for spinal cord disorders is nascent, with a few preclinical studies conducted demonstrating its efficacy [168, 169]. Since growth and mitogenic factors have diverse biological effects, further in vivo studies are required to characterize their effect on the BSCB.
Gene therapy
Studies utilizing gene therapy-based approaches to treat diseases affecting the spinal cord have aimed to replenish neuroglial populations and replace absent or dysfunctional genes [174,175,176]. These have provided indirect evidence for the potential of gene therapy to facilitate restoration of the BSCB. In the context of acute SCI, AAV delivery of combined growth factors (FGF, EGF, and GDNF) to the lesion core resulted in an increase in basement membrane-associated laminin expression [177]. Chondroitinase ABC (ChABC) is an enzyme known for its ability to induce axonal sprouting in SCI by degrading chondroitin sulphate proteoglycans (CSPGs). ChABC has also been shown to promote vascular remodelling and attenuate secondary injury from neuroinflammation thereby presenting a candidate for gene therapy [178]. Several other siRNA-based therapies aimed at reducing neuroinflammation may also prevent or ameliorate BSCB injury [179,180,181,182]. Key mediators of proinflammatory cascades such as P2X-purinogenic receptors or toll-like receptor 4 (TLR-4) are ideal targets for siRNA-mediated silencing that could protect the BSCB and improve neurological recovery [180, 183,184,185,186].
Molecular inhibitors and neutralizing antibodies
Inhibitors to BSCB-destabilizing factors and ER stress-induced apoptosis are amongst promising therapeutic agents that have been shown to reduce BBB / BSCB damage. One such agent is anti-Nogo-A neutralizing antibody. Nogo-A is a myelin-associated inhibitor that may be neutralized with an antibody to improve neurite outgrowth following spinal cord injury [187,188,189]. Interestingly, Nogo-A signalling via S1PR2 receptor activation and downstream RhoA/ROCK activation compromised vascular integrity by causing internalization of TJs and loosening of the endothelial lining [190,191,192]. Thus, anti-Nogo antibodies may also be effective in protecting the BSCB. Another drug candidate is imatinib, a receptor tyrosine kinase (RTK) inhibitor commonly used in cancer treatment and known to suppress PDGF-CC signalling, which plays a key role in BSCB disruption mediated by inflammation and oxidative stress [193, 194]. Other therapeutic candidates acting via inhibition of endoplasmic reticulum (ER) stress include 4-phenylbutyric acid (PBA) and salubrinal, which preserved endothelial cell survival and TJ integrity in mice subject to traumatic SCI [195,196,197,198].
Immune modulators
Inflammation is a pathophysiological feature of DCM that results in cytotoxicity and compromises BSCB function. There are many clinical studies regarding the perioperative use of dexamethasone to reduce neurological complications in cervical spine surgery [199,200,201] but not BSCB disruption per se. Inhibiting proinflammatory cascades via attenuation of TNFα signaling and calpain with infliximab and calpastatin respectively restored BBB permeability and promoted endothelial cell survival and TJ expression in mouse models of subarachnoid hemorrhage (SAH) and traumatic brain injury (TBI) [202,203,204]. Compounds derived from natural herbs that possess anti-inflammatory or antioxidant activity, such as shikonin, curcumin, and salvianolic acid B have also demonstrated efficacy in rat models of SCI [205,206,207,208]. Arachidonic acid pathway attenuation [209,210,211], monoacylglycerol lipase (MAGL) inhibition [212, 213], and inhibition of complement C5a [214,215,216] are also potential pharmacological targets as alternatives to more established anti-inflammatory agents such as corticosteroids, riluzole, and NSAIDs.
Other approaches
Studies on the BBB have demonstrated that nutritional remedies such as vitamins B and D [217, 218], omega-3 fatty acids [219, 220], and antioxidants such as glutathione and polyphenols [221,222,223] have a positive effect on barrier health. Gut microbiota is increasing being recognized as a key regulator of BBB function [224]. Dysfunction of gut microbiota can lead to the disruption of the gut-vascular barrier (GVB), leading to infiltration of bacteria and toxic metabolites into the bloodstream that induces chronic inflammation and NVU hyperpermeability [225, 226]. Lack of diversity in gut microbiome can also negatively impact BBB health, potentially due to reduced short-chain fatty acids (SCFAs) and production of beneficial microbes, which protect the NVU from oxidative stress [226]. Although these studies have only focused on the BBB, the same therapeutic principles apply to the BSCB, especially in patients with a dysregulated gut-brain axis [227,228,229,230].
Photobiomodulation (PBM), also referred to as transcranial low-level laser therapy (LLLT), is an experimental light therapy that has undergone clinical trials for stroke, TBI, and neurodegenerative disorders such as Alzheimer’s disease and Parkinson’s disease [231]. The mechanism of PBM is attributed to be via cytochrome C oxidase, a photoreceptor in the mitochondria that upon activation can promote proliferation and maturation of cells composing the BSCB [232]. Recently, PBM has been shown to increase pericyte mobilization and to support the BBB in stroke models [233, 234].
Conclusion
BSCB disruption is increasingly recognized as a cause for neurological decline in disease affecting the spinal cord. Our review highlights the preclinical and clinical evidence for BSCB breakdown in DCM and identifies therapeutic strategies that may facilitate neurological recovery by means of BSCB reconstitution. Future studies should be performed upon representative animal models to characterise BSCB breakdown in moderate to severe DCM, and thereafter, to evaluate the efficacy of the aforementioned treatment modalities. Protection and regeneration of the dysfunctional BSCB in DCM provides a promising direction for future study as neurological and functional deficits often remain despite best available treatment.
Availability of data and materials
Not applicable.
References
Milligan J, et al. Degenerative cervical myelopathy: diagnosis and management in primary care. Can Fam Physician. 2019;65(9):619–24.
Nouri A, et al. Degenerative cervical myelopathy: a brief review of past perspectives, present developments, and future directions. J Clin Med. 2020;9(2):535.
Tetreault LA, et al. The natural history of degenerative cervical myelopathy and the rate of hospitalization following spinal cord injury: an updated systematic review. Global Spine J. 2017;7(3 Suppl):28S-34S.
The Lancet N. A focus on patient outcomes in cervical myelopathy. Lancet Neurol. 2019;18(7):615.
Kane SF, Abadie KV, Willson A. Degenerative cervical myelopathy: recognition and management. Am Fam Physician. 2020;102(12):740–50.
Lannon M, Kachur E. Degenerative cervical myelopathy: clinical presentation, assessment, and natural history. J Clin Med. 2021;10(16):3626.
Northover JR, et al. The epidemiology of cervical spondylotic myelopathy. Skeletal Radiol. 2012;41(12):1543–6.
Matz PG, et al. The natural history of cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11(2):104–11.
Behrbalk E, et al. Delayed diagnosis of cervical spondylotic myelopathy by primary care physicians. Neurosurg Focus. 2013;35(1):E1.
Fehlings MG, et al. A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global Spine J. 2017;7(3 Suppl):70S-83S.
Youssef JA, et al. Outcomes of posterior cervical fusion and decompression: a systematic review and meta-analysis. Spine J. 2019;19(10):1714–29.
Schuermans VNE, et al. A systematic review on neurological outcomes for cervical degenerative myelopathy after anterior decompression surgery: motion preservation vs fusion. Int J Spine Surg. 2022. https://doi.org/10.14444/8320.
Bartanusz V, et al. The blood-spinal cord barrier: morphology and clinical implications. Ann Neurol. 2011;70(2):194–206.
Reinhold AK, Rittner HL. Barrier function in the peripheral and central nervous system-a review. Pflugers Arch. 2017;469(1):123–34.
Garbuzova-Davis S, et al. Ultrastructure of blood-brain barrier and blood-spinal cord barrier in SOD1 mice modeling ALS. Brain Res. 2007;1157:126–37.
Lam MA, et al. The ultrastructure of spinal cord perivascular spaces: implications for the circulation of cerebrospinal fluid. Sci Rep. 2017;7(1):12924.
Oldendorf WH, Cornford ME, Brown WJ. The large apparent work capability of the blood-brain barrier: a study of the mitochondrial content of capillary endothelial cells in brain and other tissues of the rat. Ann Neurol. 1977;1(5):409–17.
Bernacki J, et al. Physiology and pharmacological role of the blood-brain barrier. Pharmacol Rep. 2008;60(5):600–22.
Nguyen B, Bix G, Yao Y. Basal lamina changes in neurodegenerative disorders. Mol Neurodegener. 2021;16(1):81.
Takigawa T, et al. Separation of the perivascular basement membrane provides a conduit for inflammatory cells in a mouse spinal cord injury model. J Neurotrauma. 2010;27(4):739–51.
Nakazawa E, Ishikawa H. Ultrastructural observations of astrocyte end-feet in the rat central nervous system. J Neurocytol. 1998;27(6):431–40.
Rash JE, et al. Direct immunogold labeling of aquaporin-4 in square arrays of astrocyte and ependymocyte plasma membranes in rat brain and spinal cord. Proc Natl Acad Sci U S A. 1998;95(20):11981–6.
Paquette T, Piche M, Leblond H. Contribution of astrocytes to neurovascular coupling in the spinal cord of the rat. J Physiol Sci. 2021;71(1):16.
McConnell HL, et al. The translational significance of the neurovascular unit. J Biol Chem. 2017;292(3):762–70.
Li Y, et al. Pericytes impair capillary blood flow and motor function after chronic spinal cord injury. Nat Med. 2017;23(6):733–41.
Winkler EA, et al. Blood-spinal cord barrier pericyte reductions contribute to increased capillary permeability. J Cereb Blood Flow Metab. 2012;32(10):1841–52.
Hamilton NB, Attwell D, Hall CN. Pericyte-mediated regulation of capillary diameter: a component of neurovascular coupling in health and disease. Front Neuroenergetics. 2010. https://doi.org/10.3389/fnene.2010.00005.
Prockop LD, et al. Selective permeability of [3H]-D-mannitol and [14C]-carboxyl-inulin across the blood-brain barrier and blood-spinal cord barrier in the rabbit. J Spinal Cord Med. 1995;18(4):221–6.
Pan W, Banks WA, Kastin AJ. Permeability of the blood-brain and blood-spinal cord barriers to interferons. J Neuroimmunol. 1997;76(1–2):105–11.
Pan W, Kastin AJ. Penetration of neurotrophins and cytokines across the blood-brain/blood-spinal cord barrier. Adv Drug Deliv Rev. 1999;36(2–3):291–8.
Ge S, Pachter JS. Isolation and culture of microvascular endothelial cells from murine spinal cord. J Neuroimmunol. 2006;177(1–2):209–14.
Uchida Y, et al. Comparison of absolute protein abundances of transporters and receptors among blood-brain barriers at different cerebral regions and the blood-spinal cord barrier in humans and rats. Mol Pharm. 2020;17(6):2006–20.
Sawada N. Tight junction-related human diseases. Pathol Int. 2013;63(1):1–12.
Winkler EA, et al. Blood-spinal cord barrier pericyte reductions contribute to increased capillary permeability. J Cereb Blood Flow Metab. 2012;32(10):1841–52.
Sun Z, et al. Reduction in pericyte coverage leads to blood-brain barrier dysfunction via endothelial transcytosis following chronic cerebral hypoperfusion. Fluids Barriers CNS. 2021;18(1):21.
Yoon H, et al. Astrocyte heterogeneity across the brain and spinal cord occurs developmentally, in adulthood and in response to demyelination. PLoS ONE. 2017;12(7):e0180697.
Claudio L, et al. Increased vesicular transport and decreased mitochondrial content in blood-brain barrier endothelial cells during experimental autoimmune encephalomyelitis. Am J Pathol. 1989;135(6):1157–68.
Yashon D, et al. Edema of the spinal cord following experimental impact trauma. J Neurosurg. 1973;38(6):693–7.
Bilgen M, et al. Spatial and temporal evolution of hemorrhage in the hyperacute phase of experimental spinal cord injury: in vivo magnetic resonance imaging. Magn Reson Med. 2000;43(4):594–600.
Kadry H, Noorani B, Cucullo L. A blood-brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS. 2020;17(1):69.
Schramm M, Eimerl S, Costa E. Serum and depolarizing agents cause acute neurotoxicity in cultured cerebellar granule cells: role of the glutamate receptor responsive to N-methyl-D-aspartate. Proc Natl Acad Sci U S A. 1990;87(3):1193–7.
Garcia JE Jr, et al. Neurotoxic components in normal serum. Exp Neurol. 1992;118(3):309–16.
Stokum JA, et al. When the blood hits your brain: the neurotoxicity of extravasated blood. Int J Mol Sci. 2021;22(10):5132.
Anwar MA, Al Shehabi TS, Eid AH. Inflammogenesis of secondary spinal cord injury. Front Cell Neurosci. 2016;10:98.
Popovich PG, et al. A quantitative spatial analysis of the blood-spinal cord barrier. I. Permeability changes after experimental spinal contusion injury. Exp Neurol. 1996;142(2):258–75.
Jin LY, et al. Blood-spinal cord barrier in spinal cord injury: a review. J Neurotrauma. 2021;38(9):1203–24.
Hemley SJ, Tu J, Stoodley MA. Role of the blood-spinal cord barrier in posttraumatic syringomyelia. J Neurosurg Spine. 2009;11(6):696–704.
Berliner J, et al. Abnormalities in spinal cord ultrastructure in a rat model of post-traumatic syringomyelia. Fluids Barriers CNS. 2020;17(1):11.
Steinruecke M, et al. Blood-CNS barrier dysfunction in amyotrophic lateral sclerosis: proposed mechanisms and clinical implications. J Cereb Blood Flow Metab. 2023;43(5):642–54.
Chio A, et al. Prognostic factors in ALS: a critical review. Amyotroph Lateral Scler. 2009;10(5–6):310–23.
Sasaki S. Alterations of the blood-spinal cord barrier in sporadic amyotrophic lateral sclerosis. Neuropathology. 2015;35(6):518–28.
Zhong Z, et al. ALS-causing SOD1 mutants generate vascular changes prior to motor neuron degeneration. Nat Neurosci. 2008;11(4):420–2.
Winkler EA, et al. Blood-spinal cord barrier breakdown and pericyte reductions in amyotrophic lateral sclerosis. Acta Neuropathol. 2013;125(1):111–20.
Engelhardt JI, Tajti J, Appel SH. Lymphocytic infiltrates in the spinal cord in amyotrophic lateral sclerosis. Arch Neurol. 1993;50(1):30–6.
Garbuzova-Davis S, et al. Impaired blood-brain/spinal cord barrier in ALS patients. Brain Res. 2012;1469:114–28.
Armulik A, et al. Pericytes regulate the blood-brain barrier. Nature. 2010;468(7323):557–61.
Garbuzova-Davis S, et al. Evidence of compromised blood-spinal cord barrier in early and late symptomatic SOD1 mice modeling ALS. PLoS ONE. 2007;2(11):e1205.
Schellenberg AE, et al. Magnetic resonance imaging of blood-spinal cord barrier disruption in mice with experimental autoimmune encephalomyelitis. Magn Reson Med. 2007;58(2):298–305.
Juhler M, et al. Blood-brain and blood-spinal cord barrier permeability during the course of experimental allergic encephalomyelitis in the rat. Brain Res. 1984;302(2):347–55.
Hawkins CP, et al. Patterns of blood-brain barrier breakdown in inflammatory demyelination. Brain. 1991;114(Pt 2):801–10.
Hawkins CP, et al. Duration and selectivity of blood-brain barrier breakdown in chronic relapsing experimental allergic encephalomyelitis studied by gadolinium-DTPA and protein markers. Brain. 1990;113(Pt 2):365–78.
Bonfield CM, et al. Surgical management of post-traumatic syringomyelia. Spine (Phila Pa 1976). 2010;35(21 Suppl):S245-58.
Bhagavathula Venkata SS, et al. Syringomyelia secondary to cervical spondylosis: case report and review of literature. J Neurosci Rural Pract. 2014;5(Suppl 1):S78-82.
Niida-Kawaguchi M, et al. Soluble iron accumulation induces microglial glutamate release in the spinal cord of sporadic amyotrophic lateral sclerosis. Neuropathology. 2020;40(2):152–66.
Kwan JY, et al. Iron accumulation in deep cortical layers accounts for MRI signal abnormalities in ALS: correlating 7 tesla MRI and pathology. PLoS ONE. 2012;7(4):e35241.
Shea GKH, et al. Prospects of cell replacement therapy for the treatment of degenerative cervical myelopathy. Rev Neurosci. 2021;32(3):275–87.
Cheriyan T, et al. Spinal cord injury models: a review. Spinal Cord. 2014;52(8):588–95.
Okawa A, et al. Mapping of a gene responsible for twy (tip-toe walking Yoshimura), a mouse model of ossification of the posterior longitudinal ligament of the spine (OPLL). Mamm Genome. 1998;9(2):155–6.
Okawa A, et al. Mutation in Npps in a mouse model of ossification of the posterior longitudinal ligament of the spine. Nat Genet. 1998;19(3):271–3.
Ijima Y, et al. Experimental rat model for cervical compressive myelopathy. NeuroReport. 2017;28(18):1239–45.
Kanbara S, et al. Zonisamide ameliorates progression of cervical spondylotic myelopathy in a rat model. Sci Rep. 2020;10(1):13138.
Long HQ, et al. Is the speed of chronic compression an important factor for chronic spinal cord injury rat model? Neurosci Lett. 2013;545:75–80.
Klironomos G, et al. New experimental rabbit animal model for cervical spondylotic myelopathy. Spinal Cord. 2011;49(11):1097–102.
Li GS, et al. Neurovascular unit compensation from adjacent level may contribute to spontaneous functional recovery in experimental cervical spondylotic myelopathy. Int J Mol Sci. 2023;24(4):3408.
Karadimas SK, et al. A novel experimental model of cervical spondylotic myelopathy (CSM) to facilitate translational research. Neurobiol Dis. 2013;54:43–58.
Kim P, et al. Delayed myelopathy induced by chronic compression in the rat spinal cord. Ann Neurol. 2004;55(4):503–11.
Badhiwala JH, et al. Degenerative cervical myelopathy—update and future directions. Nat Rev Neurol. 2020;16(2):108–24.
Breig A, Turnbull I, Hassler O. Effects of mechanical stresses on the spinal cord in cervical spondylosis. A study on fresh cadaver material. J Neurosurg. 1966;25(1):45–56.
Shi R, Pryor JD. Pathological changes of isolated spinal cord axons in response to mechanical stretch. Neuroscience. 2002;110(4):765–77.
Mair WG, Druckman R. The pathology of spinal cord lesions and their relation to the clinical features in protrusion of cervical intervertebral discs; a report of four cases. Brain. 1953;76(1):70–91.
Blume C, et al. Decreased angiogenesis as a possible pathomechanism in cervical degenerative myelopathy. Sci Rep. 2021;11(1):2497.
Brain WR, Knight GC, Bull JW. Discussion of rupture of the intervertebral disc in the cervical region. Proc R Soc Med. 1948;41(8):509–16.
Gooding MR, Wilson CB, Hoff JT. Experimental cervical myelopathy. Effects of ischemia and compression of the canine cervical spinal cord. J Neurosurg. 1975;43(1):9–17.
Lo YL. The role of electrophysiology in the diagnosis and management of cervical spondylotic myelopathy. Ann Acad Med Singap. 2007;36(11):886–93.
Tetreault L, et al. The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J. 2017;26(1):78–84.
Bernhardt M, et al. Cervical spondylotic myelopathy. J Bone Joint Surg Am. 1993;75(1):119–28.
Karadimas SK, Gatzounis G, Fehlings MG. Pathobiology of cervical spondylotic myelopathy. Eur Spine J. 2015;24(Suppl 2):132–8.
Tsao CC, et al. Pericyte hypoxia-inducible factor-1 (HIF-1) drives blood-brain barrier disruption and impacts acute ischemic stroke outcome. Angiogenesis. 2021;24(4):823–42.
Halder SK, Milner R. Mild hypoxia triggers transient blood-brain barrier disruption: a fundamental protective role for microglia. Acta Neuropathol Commun. 2020;8(1):175.
Yu WR, et al. Human neuropathological and animal model evidence supporting a role for Fas-mediated apoptosis and inflammation in cervical spondylotic myelopathy. Brain. 2011;134(Pt 5):1277–92.
Noble LJ, et al. Matrix metalloproteinases limit functional recovery after spinal cord injury by modulation of early vascular events. J Neurosci. 2002;22(17):7526–35.
Karadimas SK, et al. Immunohistochemical profile of NF-kappaB/p50, NF-kappaB/p65, MMP-9, MMP-2, and u-PA in experimental cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2013;38(1):4–10.
Winkler EA, et al. Blood-spinal cord barrier disruption contributes to early motor-neuron degeneration in ALS-model mice. Proc Natl Acad Sci U S A. 2014;111(11):E1035–42.
Xiao M, et al. Blood-brain barrier: more contributor to disruption of central nervous system homeostasis than victim in neurological disorders. Front Neurosci. 2020;14:764.
Wang J, et al. Ischemia-induced neuronal cell death is mediated by chemokine receptor CX3CR1. Sci Rep. 2018;8(1):556.
Mukandala G, et al. The effects of hypoxia and inflammation on synaptic signaling in the CNS. Brain Sci. 2016;6(1):6.
Harrison JK, et al. Role for neuronally derived fractalkine in mediating interactions between neurons and CX3CR1-expressing microglia. Proc Natl Acad Sci U S A. 1998;95(18):10896–901.
Yu WR, Karadimas S, Fehlings MG. The role of CX3CR1 in promoting inflammation and neural degeneration in cervical spondylotic myelopathy. Society for Neuroscience, 2012. 722.01.
Hirai T, et al. The prevalence and phenotype of activated microglia/macrophages within the spinal cord of the hyperostotic mouse (twy/twy) changes in response to chronic progressive spinal cord compression: implications for human cervical compressive myelopathy. PLoS ONE. 2013;8(5):e64528.
Alvarez S, et al. TNF-alpha contributes to caspase-3 independent apoptosis in neuroblastoma cells: role of NFAT. PLoS ONE. 2011;6(1):e16100.
Kaufmann T, Strasser A, Jost PJ. Fas death receptor signalling: roles of Bid and XIAP. Cell Death Differ. 2012;19(1):42–50.
Nesic O, et al. IL-1 receptor antagonist prevents apoptosis and caspase-3 activation after spinal cord injury. J Neurotrauma. 2001;18(9):947–56.
Radulovic M, et al. Targeting the thrombin receptor modulates inflammation and astrogliosis to improve recovery after spinal cord injury. Neurobiol Dis. 2016;93:226–42.
Donovan FM, et al. Thrombin induces apoptosis in cultured neurons and astrocytes via a pathway requiring tyrosine kinase and RhoA activities. J Neurosci. 1997;17(14):5316–26.
Broughton BR, Reutens DC, Sobey CG. Apoptotic mechanisms after cerebral ischemia. Stroke. 2009;40(5):e331–9.
Ye Z, et al. Effects of mechanical force on cytoskeleton structure and calpain-induced apoptosis in rat dorsal root ganglion neurons in vitro. PLoS ONE. 2012;7(12):e52183.
Inukai T, et al. Tumor necrosis factor-alpha and its receptors contribute to apoptosis of oligodendrocytes in the spinal cord of spinal hyperostotic mouse (twy/twy) sustaining chronic mechanical compression. Spine (Phila Pa 1976). 2009;34(26):2848–57.
Takenouchi T, et al. Expression of apoptosis signal-regulating kinase 1 in mouse spinal cord under chronic mechanical compression: possible involvement of the stress-activated mitogen-activated protein kinase pathways in spinal cord cell apoptosis. Spine (Phila Pa 1976). 2008;33(18):1943–50.
Blume C, et al. Patients with degenerative cervical myelopathy have signs of blood spinal cord barrier disruption, and its magnitude correlates with myelopathy severity: a prospective comparative cohort study. Eur Spine J. 2020;29(5):986–93.
Karadimas SK, et al. Pathophysiology and natural history of cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2013;38(22 Suppl 1):S21-36.
Tachibana N, et al. Spinal cord swelling in patients with cervical compression myelopathy. BMC Musculoskelet Disord. 2019;20(1):284.
Ozawa H, et al. Clinical significance of intramedullary Gd-DTPA enhancement in cervical myelopathy. Spinal Cord. 2010;48(5):415–22.
Sasamori T, et al. Spinal cord swelling with abnormal gadolinium-enhancement mimicking intramedullary tumors in cervical spondylosis patients: Three case reports and review of the literature. Asian J Neurosurg. 2010;5(2):1–9.
Xu Y, et al. Surgical approaches and outcomes for cervical myelopathy with increased signal intensity on T2-weighted MRI: a meta-analysis. J Orthop Surg Res. 2019;14(1):224.
Vedantam A, Rajshekhar V. Does the type of T2-weighted hyperintensity influence surgical outcome in patients with cervical spondylotic myelopathy? A review. Eur Spine J. 2013;22(1):96–106.
Xu L, Nirwane A, Yao Y. Basement membrane and blood-brain barrier. Stroke Vasc Neurol. 2019;4(2):78–82.
Li G-S, et al. Ultrastructural destruction of neurovascular unit in experimental cervical spondylotic myelopathy. Front Neurosci. 2022. https://doi.org/10.3389/fnins.2022.1031180.
Pandita N, et al. Neurological recovery pattern in cervical spondylotic myelopathy after anterior surgery: a prospective study with literature review. Asian Spine J. 2019;13(3):423–31.
Yamazaki T, et al. Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery. 2003;52(1):122–6.
Vidal PM, et al. Delayed decompression exacerbates ischemia-reperfusion injury in cervical compressive myelopathy. JCI Insight. 2017. https://doi.org/10.1172/jci.insight.92512.
Papaioannou I, et al. Late-onset “white cord syndrome” in an elderly patient after posterior cervical decompression and fusion: a case report. Spinal Cord Ser Cases. 2019;5:28.
Malinovic M, Walker J, Lee F. Ischemia-reperfusion injury after posterior cervical laminectomy. Cureus. 2021;13(9):e18298.
Tu J, et al. Degenerative cervical myelopathy: insights into its pathobiology and molecular mechanisms. J Clin Med. 2021;10(6):1214.
Hu J, et al. Targeting the blood-spinal cord barrier: a therapeutic approach to spinal cord protection against ischemia-reperfusion injury. Life Sci. 2016;158:1–6.
Schmidt TP, Jütten K, Bertram U, Brandenburg LO, Pufe T, Delev D, Gombert A, Mueller CA, Clusmann H, Blume C. Blood spinal cord barrier disruption recovers in patients with degenerative cervical myelopathy after surgical decompression: a prospective cohort study. Sci Rep. 2023;13(1):7389. https://doi.org/10.1038/s41598-023-34004-2.
Lee J, et al. Spinal cord edema: unusual magnetic resonance imaging findings in cervical spondylosis. J Neurosurg. 2003;99(1 Suppl):8–13.
Gkasdaris G, et al. Spinal cord edema with contrast enhancement mimicking intramedullary tumor in patient with cervical myelopathy: a case report and a brief literature review. Surg Neurol Int. 2017;8:111.
Shingu H, et al. Microangiographic study of spinal cord injury and myelopathy. Paraplegia. 1989;27(3):182–9.
Murakami N, Muroga T, Sobue I. Cervical myelopathy due to ossification of the posterior longitudinal ligament: a clinicopathologic study. Arch Neurol. 1978;35(1):33–6.
Cheung WY, et al. Neurological recovery after surgical decompression in patients with cervical spondylotic myelopathy—a prospective study. Int Orthop. 2008;32(2):273–8.
Fehlings MG, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am. 2013;95(18):1651–8.
Tetreault LA, Karpova A, Fehlings MG. Predictors of outcome in patients with degenerative cervical spondylotic myelopathy undergoing surgical treatment: results of a systematic review. Eur Spine J. 2015;24(2):236–51.
Haft GF. Are functional gains durable after decompressive surgery for cervical myelopathy? Commentary on an article by Victor Hin Ting Yick, MBBS, et al.: “neurological survivorship following surgery for degenerative cervical myelopathy. A longitudinal study on 195 patients.” J Bone Joint Surg Am. 2023;105(3):e11.
Ting Yick VH, et al. Neurological survivorship following surgery for degenerative cervical myelopathy: a longitudinal study on 195 Patients. J Bone Joint Surg Am. 2023;105(3):181–90.
Rhee J, et al. Nonoperative versus operative management for the treatment degenerative cervical myelopathy: an updated systematic review. Global Spine J. 2017;7(3 Suppl):35S-41S.
Hirpara KM, et al. Nonoperative modalities to treat symptomatic cervical spondylosis. Adv Orthop. 2012;2012:294857.
Manzur MK, et al. Cervical steroid injections are not effective for prevention of surgical treatment of degenerative cervical myelopathy. Global Spine J. 2021. https://doi.org/10.1177/21925682211024573.
Fehlings MG, et al. Safety and efficacy of riluzole in patients undergoing decompressive surgery for degenerative cervical myelopathy (CSM-Protect): a multicentre, double-blind, placebo-controlled, randomised, phase 3 trial. Lancet Neurol. 2021;20(2):98–106.
Doble A. The pharmacology and mechanism of action of riluzole. Neurology. 1996;47(6 Suppl 4):S233–41.
Dharmadasa T, Kiernan MC. Riluzole, disease stage and survival in ALS. Lancet Neurol. 2018;17(5):385–6.
Horie N, et al. Transplanted stem cell-secreted vascular endothelial growth factor effects poststroke recovery, inflammation, and vascular repair. Stem Cells. 2011;29(2):274–85.
Suzuki H, Sakai T. Current concepts of stem cell therapy for chronic spinal cord injury. Int J Mol Sci. 2021;22(14):7435.
Guo W, et al. The roles and applications of neural stem cells in spinal cord injury repair. Front Bioeng Biotechnol. 2022;10:966866.
Funa K, Sasahara M. The roles of PDGF in development and during neurogenesis in the normal and diseased nervous system. J Neuroimmune Pharmacol. 2014;9(2):168–81.
Sato H, et al. PDGFR-beta plays a key role in the ectopic migration of neuroblasts in cerebral stroke. Stem Cells. 2016;34(3):685–98.
Ishii Y, et al. Characterization of neuroprogenitor cells expressing the PDGF beta-receptor within the subventricular zone of postnatal mice. Mol Cell Neurosci. 2008;37(3):507–18.
Xu G, et al. Functional analysis of platelet-derived growth factor receptor-beta in neural stem/progenitor cells. Neuroscience. 2013;238:195–208.
Wang S, et al. Platelet-derived growth factor receptor beta identifies mesenchymal stem cells with enhanced engraftment to tissue injury and pro-angiogenic property. Cell Mol Life Sci. 2018;75(3):547–61.
Menezes K, et al. Human mesenchymal stromal/stem cells recruit resident pericytes and induce blood vessels maturation to repair experimental spinal cord injury in rats. Sci Rep. 2020;10(1):19604.
Vidal M, et al. Adult DRG stem/progenitor cells generate pericytes in the presence of Central Nervous System (CNS) developmental cues, and Schwann cells in response to CNS demyelination. Stem Cells. 2015;33(6):2011–24.
Pluchino S, et al. Neurosphere-derived multipotent precursors promote neuroprotection by an immunomodulatory mechanism. Nature. 2005;436(7048):266–71.
Tiklova K, et al. Single cell transcriptomics identifies stem cell-derived graft composition in a model of Parkinson’s disease. Nat Commun. 2020;11(1):2434.
Takashima Y, et al. Neuroepithelial cells supply an initial transient wave of MSC differentiation. Cell. 2007;129(7):1377–88.
Etchevers HC, et al. The cephalic neural crest provides pericytes and smooth muscle cells to all blood vessels of the face and forebrain. Development. 2001;128(7):1059–68.
Korn J, Christ B, Kurz H. Neuroectodermal origin of brain pericytes and vascular smooth muscle cells. J Comp Neurol. 2002;442(1):78–88.
Venkat P, et al. Exosomes derived from bone marrow mesenchymal stem cells harvested from type two diabetes rats promotes neurorestorative effects after stroke in type two diabetes rats. Exp Neurol. 2020;334: 113456.
Shen J, et al. PDGFR-beta restores blood-brain barrier functions in a mouse model of focal cerebral ischemia. J Cereb Blood Flow Metab. 2019;39(8):1501–15.
Smyth LCD, et al. Characterisation of PDGF-BB:PDGFRbeta signalling pathways in human brain pericytes: evidence of disruption in Alzheimer’s disease. Commun Biol. 2022;5(1):235.
Zhou Y, et al. Fibroblast growth factors in the management of spinal cord injury. J Cell Mol Med. 2018;22(1):25–37.
Mushala BAS, Scott I. Adropin: a hepatokine modulator of vascular function and cardiac fuel metabolism. Am J Physiol Heart Circ Physiol. 2021;320(1):H238–44.
Ye LB, et al. Regulation of Caveolin-1 and junction proteins by bFGF contributes to the integrity of blood-spinal cord barrier and functional recovery. Neurotherapeutics. 2016;13(4):844–58.
Zhang R, et al. ALG-bFGF hydrogel inhibiting autophagy contributes to protection of blood-spinal cord barrier integrity via PI3K/Akt/FOXO1/KLF4 pathway after SCI. Front Pharmacol. 2022;13:828896.
Zhang HY, et al. Regulation of autophagy and ubiquitinated protein accumulation by bFGF promotes functional recovery and neural protection in a rat model of spinal cord injury. Mol Neurobiol. 2013;48(3):452–64.
Rabchevsky AG, et al. Basic fibroblast growth factor (bFGF) enhances functional recovery following severe spinal cord injury to the rat. Exp Neurol. 2000;164(2):280–91.
Sun D, et al. Basic fibroblast growth factor-enhanced neurogenesis contributes to cognitive recovery in rats following traumatic brain injury. Exp Neurol. 2009;216(1):56–65.
Wang ZG, et al. bFGF protects against blood-brain barrier damage through junction protein regulation via PI3K-Akt-Rac1 pathway following traumatic brain injury. Mol Neurobiol. 2016;53(10):7298–311.
Padel T, et al. Platelet-derived growth factor-BB has neurorestorative effects and modulates the pericyte response in a partial 6-hydroxydopamine lesion mouse model of Parkinson’s disease. Neurobiol Dis. 2016;94:95–105.
Ye LX, et al. Exogenous platelet-derived growth factor improves neurovascular unit recovery after spinal cord injury. Neural Regen Res. 2021;16(4):765–71.
Zheng B, et al. Epidermal growth factor attenuates blood-spinal cord barrier disruption via PI3K/Akt/Rac1 pathway after acute spinal cord injury. J Cell Mol Med. 2016;20(6):1062–75.
Kojima A, Tator CH. Intrathecal administration of epidermal growth factor and fibroblast growth factor 2 promotes ependymal proliferation and functional recovery after spinal cord injury in adult rats. J Neurotrauma. 2002;19(2):223–38.
Ozturk AM, et al. Epidermal growth factor regulates apoptosis and oxidative stress in a rat model of spinal cord injury. Injury. 2018;49(6):1038–45.
Dodd WS, et al. Adropin decreases endothelial monolayer permeability after cell-free hemoglobin exposure and reduces MCP-1-induced macrophage transmigration. Biochem Biophys Res Commun. 2021;582:105–10.
Yu L, et al. Adropin preserves the blood-brain barrier through a Notch1/Hes1 pathway after intracerebral hemorrhage in mice. J Neurochem. 2017;143(6):750–60.
Fang T, et al. Gene therapy in amyotrophic lateral sclerosis. Cells. 2022;11(13):2066.
Zavvarian MM, et al. Novel innovations in cell and gene therapies for spinal cord injury. F1000Res. 2020;9:279.
Cunningham CJ, et al. The potential of gene therapies for spinal cord injury repair: a systematic review and meta-analysis of pre-clinical studies. Neural Regen Res. 2023;18(2):299–305.
Anderson MA, et al. Required growth facilitators propel axon regeneration across complete spinal cord injury. Nature. 2018;561(7723):396–400.
Milbreta U, et al. Astrocytic and vascular remodeling in the injured adult rat spinal cord after chondroitinase ABC treatment. J Neurotrauma. 2014;31(9):803–18.
Huang W, et al. SiRNA in MSC-derived exosomes silences CTGF gene for locomotor recovery in spinal cord injury rats. Stem Cell Res Ther. 2021;12(1):334.
Almarghalani DA, Shah ZA. Progress on siRNA-based gene therapy targeting secondary injury after intracerebral hemorrhage. Gene Ther. 2023;30(1–2):1–7.
Gu Y, et al. Repair of spinal cord injury by inhibition of PLK4 expression through local delivery of siRNA-loaded nanoparticles. J Mol Neurosci. 2022;72(3):544–54.
Chan WH, et al. Intrathecal IGF2 siRNA injection provides long-lasting anti-allodynic effect in a spared nerve injury rat model of neuropathic pain. PLoS ONE. 2021;16(12):e0260887.
Feng L, et al. P2X7R blockade prevents NLRP3 inflammasome activation and brain injury in a rat model of intracerebral hemorrhage: involvement of peroxynitrite. J Neuroinflammation. 2015;12:190.
Dorn G, et al. siRNA relieves chronic neuropathic pain. Nucleic Acids Res. 2004;32(5):e49.
Wu FX, et al. Intrathecal siRNA against Toll-like receptor 4 reduces nociception in a rat model of neuropathic pain. Int J Med Sci. 2010;7(5):251–9.
Chen ZQ, et al. Negative regulation of glial Tim-3 inhibits the secretion of inflammatory factors and modulates microglia to antiinflammatory phenotype after experimental intracerebral hemorrhage in rats. CNS Neurosci Ther. 2019;25(6):674–84.
Mohammed R, et al. Evaluating the effectiveness of anti-Nogo treatment in spinal cord injuries. Neural Dev. 2020;15(1):1.
Rust R, et al. Anti-Nogo-A antibodies prevent vascular leakage and act as pro-angiogenic factors following stroke. Sci Rep. 2019;9(1):20040.
Zorner B, Schwab ME. Anti-Nogo on the go: from animal models to a clinical trial. Ann N Y Acad Sci. 2010;1198(Suppl 1):E22-34.
Kim GS, et al. Critical role of sphingosine-1-phosphate receptor-2 in the disruption of cerebrovascular integrity in experimental stroke. Nat Commun. 2015;6:7893.
Kempf A, et al. The sphingolipid receptor S1PR2 is a receptor for Nogo-a repressing synaptic plasticity. PLoS Biol. 2014;12(1):e1001763.
Rust R, et al. Nogo-A targeted therapy promotes vascular repair and functional recovery following stroke. Proc Natl Acad Sci U S A. 2019;116(28):14270–9.
Liu L, et al. Imatinib inhibits oxidative stress response in spinal cord injury rats by activating Nrf2/HO-1 signaling pathway. Exp Ther Med. 2020;19(1):597–602.
Abrams MB, et al. Imatinib enhances functional outcome after spinal cord injury. PLoS ONE. 2012;7(6):e38760.
Zhou Y, et al. Phenylbutyrate prevents disruption of blood-spinal cord barrier by inhibiting endoplasmic reticulum stress after spinal cord injury. Am J Transl Res. 2016;8(4):1864–75.
He Z, et al. Inhibition of endoplasmic reticulum stress preserves the integrity of blood-spinal cord barrier in diabetic rats subjected to spinal cord injury. Sci Rep. 2017;7(1):7661.
Barreda-Manso MA, et al. Neuroprotection and blood-brain barrier restoration by salubrinal after a cortical stab injury. J Cell Physiol. 2017;232(6):1501–10.
Ohri SS, Hetman M, Whittemore SR. Restoring endoplasmic reticulum homeostasis improves functional recovery after spinal cord injury. Neurobiol Dis. 2013;58:29–37.
Jeyamohan SB, et al. Effect of steroid use in anterior cervical discectomy and fusion: a randomized controlled trial. J Neurosurg Spine. 2015;23(2):137–43.
Cui S, et al. The effects of perioperative corticosteroids on dysphagia following surgical procedures involving the anterior cervical spine: a prospective, randomized, controlled, double-blinded clinical trial. J Bone Joint Surg Am. 2019;101(22):2007–14.
Dombrowski ME, et al. Prophylactic perioperative dexamethasone decreases the incidence of postoperative C5 palsies after a posterior cervical laminectomy and fusion. The Spine Journal. 2019;19(2):253–60.
Chen AQ, et al. Microglia-derived TNF-alpha mediates endothelial necroptosis aggravating blood brain-barrier disruption after ischemic stroke. Cell Death Dis. 2019;10(7):487.
Alluri H, et al. Attenuation of blood-brain barrier breakdown and hyperpermeability by calpain inhibition. J Biol Chem. 2016;291(53):26958–69.
Teng F, et al. Calpastatin peptide attenuates early brain injury following experimental subarachnoid hemorrhage. Exp Ther Med. 2020;19(4):2433–40.
Bi Y, et al. Effect of Shikonin on spinal cord injury in rats via regulation of HMGB1/TLR4/NF-kB signaling pathway. Cell Physiol Biochem. 2017;43(2):481–91.
Yao M, et al. Shikonin inhibits neuronal apoptosis via regulating endoplasmic reticulum stress in the rat model of double-level chronic cervical cord compression. Cell Biol Toxicol. 2022. https://doi.org/10.1007/s10565-021-09648-3.
Yu DS, et al. Curcumin improves the integrity of blood-spinal cord barrier after compressive spinal cord injury in rats. J Neurol Sci. 2014;346(1–2):51–9.
Fu J, et al. Salvianolic acid B attenuates spinal cord ischemia-reperfusion-induced neuronal injury and oxidative stress by activating the extracellular signal-regulated kinase pathway in rats. J Surg Res. 2014;188(1):222–30.
Arevalo-Martin A, et al. Early endogenous activation of CB1 and CB2 receptors after spinal cord injury is a protective response involved in spontaneous recovery. PLoS ONE. 2012;7(11):e49057.
Kendall DA, Yudowski GA. Cannabinoid receptors in the central nervous system: their signaling and roles in disease. Front Cell Neurosci. 2016;10:294.
Huo J, et al. Inhibiting a spinal cord signaling pathway protects against ischemia injury in rats. J Thorac Cardiovasc Surg. 2019;157(2):494–503.
Zanfirescu A, et al. Targeting monoacylglycerol lipase in pursuit of therapies for neurological and neurodegenerative diseases. Molecules. 2021;26(18):5668.
Piro JR, et al. Inhibition of 2-AG hydrolysis differentially regulates blood brain barrier permeability after injury. J Neuroinflammation. 2018;15(1):142.
Dong Q, et al. Expression of C5a and its receptor following spinal cord ischemia reperfusion injury in the rat. Spinal Cord. 2015;53(8):581–4.
Flierl MA, et al. Inhibition of complement C5a prevents breakdown of the blood-brain barrier and pituitary dysfunction in experimental sepsis. Crit Care. 2009;13(1):R12.
Carpanini SM, Torvell M, Morgan BP. Therapeutic inhibition of the complement system in diseases of the central nervous system. Front Immunol. 2019;10:362.
Lehmann M, et al. Vitamin B12-B6-folate treatment improves blood-brain barrier function in patients with hyperhomocysteinaemia and mild cognitive impairment. Dement Geriatr Cogn Disord. 2003;16(3):145–50.
Won S, et al. Vitamin D prevents hypoxia/reoxygenation-induced blood-brain barrier disruption via vitamin D receptor-mediated NF-kB signaling pathways. PLoS ONE. 2015;10(3):e0122821.
Zhang W, et al. Omega-3 polyunsaturated fatty acids mitigate blood-brain barrier disruption after hypoxic-ischemic brain injury. Neurobiol Dis. 2016;91:37–46.
Barnes S, et al. Omega-3 fatty acids are associated with blood-brain barrier integrity in a healthy aging population. Brain Behav. 2021;11(8):e2273.
Bains M, Hall ED. Antioxidant therapies in traumatic brain and spinal cord injury. Biochim Biophys Acta. 2012;1822(5):675–84.
Agarwal R, Shukla GS. Potential role of cerebral glutathione in the maintenance of blood-brain barrier integrity in rat. Neurochem Res. 1999;24(12):1507–14.
Kim Y, et al. Effects of natural polyphenols on oxidative stress-mediated blood-brain barrier dysfunction. Antioxidants (Basel). 2022;11(2):197.
Braniste V, et al. The gut microbiota influences blood-brain barrier permeability in mice. Sci Transl Med. 2014;6(263):263ra158.
Brescia P, Rescigno M. The gut vascular barrier: a new player in the gut-liver-brain axis. Trends Mol Med. 2021;27(9):844–55.
Tang W, et al. The impact of gut microbiota disorders on the blood-brain barrier. Infect Drug Resist. 2020;13:3351–63.
Dhaliwal J, et al. Lactobacillus plantarum MTCC 9510 supplementation protects from chronic unpredictable and sleep deprivation-induced behaviour, biochemical and selected gut microbial aberrations in mice. J Appl Microbiol. 2018;125(1):257–69.
Hoyles L, et al. Regulation of blood-brain barrier integrity by microbiome-associated methylamines and cognition by trimethylamine N-oxide. Microbiome. 2021;9(1):235.
Bloemendaal M, et al. Probiotics-induced changes in gut microbial composition and its effects on cognitive performance after stress: exploratory analyses. Transl Psychiatry. 2021;11(1):300.
Yang X, et al. Probiotics modulate the microbiota-gut-brain axis and improve memory deficits in aged SAMP8 mice. Acta Pharm Sin B. 2020;10(3):475–87.
Salehpour F, et al. Brain photobiomodulation therapy: a narrative review. Mol Neurobiol. 2018;55(8):6601–36.
de Freitas LF, Hamblin MR. Proposed mechanisms of photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron. 2016;22(3):348.
do Valle IB, et al. Photobiomodulation drives pericyte mobilization towards skin regeneration. Sci Rep. 2020;10(1):19257.
Lee HI, et al. Pre-conditioning with transcranial low-level light therapy reduces neuroinflammation and protects blood-brain barrier after focal cerebral ischemia in mice. Restor Neurol Neurosci. 2016;34(2):201–14.
Liao W, et al. Therapeutic effect of human umbilical cord multipotent mesenchymal stromal cells in a rat model of stroke. Transplantation. 2009;87(3):350–9.
Wei N, et al. Delayed intranasal delivery of hypoxic-preconditioned bone marrow mesenchymal stem cells enhanced cell homing and therapeutic benefits after ischemic stroke in mice. Cell Transplant. 2013;22(6):977–91.
Cheng Z, et al. Mesenchymal stem cells attenuate blood-brain barrier leakage after cerebral ischemia in mice. J Neuroinflammation. 2018;15(1):135.
Do PT, et al. Mesenchymal stem/stromal cell therapy in blood-brain barrier preservation following ischemia: molecular mechanisms and prospects. Int J Mol Sci. 2021;22(18):10045.
Park HJ, et al. Mesenchymal stem cells stabilize the blood-brain barrier through regulation of astrocytes. Stem Cell Res Ther. 2015;6:187.
Zhang Y, et al. Adipose-derived mesenchymal stem cells stereotactic transplantation alleviate brain edema from intracerebral hemorrhage. J Cell Biochem. 2019;120(9):14372–82.
Boese AC, et al. Human neural stem cells improve early stage stroke outcome in delayed tissue plasminogen activator-treated aged stroke brains. Exp Neurol. 2020;329:113275.
Yuan X, et al. Exosomes derived from pericytes improve microcirculation and protect blood-spinal cord barrier after spinal cord injury in mice. Front Neurosci. 2019;13:319.
Yi H, Wang Y. A meta-analysis of exosome in the treatment of spinal cord injury. Open Med (Wars). 2021;16(1):1043–60.
Feng J, et al. Emerging exosomes and exosomal mirnas in spinal cord injury. Front Cell Dev Biol. 2021;9:703989.
Zhang C, et al. Therapeutic effect of exosomes derived from stem cells in spinal cord injury: a systematic review based on animal studies. Front Neurol. 2022;13:847444.
Williams AM, et al. Early single-dose treatment with exosomes provides neuroprotection and improves blood-brain barrier integrity in swine model of traumatic brain injury and hemorrhagic shock. J Trauma Acute Care Surg. 2020;88(2):207–18.
Lee MJ, et al. A transcriptomic analysis of cerebral microvessels reveals the involvement of Notch1 signaling in endothelial mitochondrial-dysfunction-dependent BBB disruption. Fluids Barriers CNS. 2022;19(1):64.
Kjell J, Olson L. Repositioning imatinib for spinal cord injury. Neural Regen Res. 2015;10(10):1591–3.
Zhan Y, et al. Imatinib preserves blood-brain barrier integrity following experimental subarachnoid hemorrhage in rats. J Neurosci Res. 2015;93(1):94–103.
Adzemovic MV, et al. Imatinib ameliorates neuroinflammation in a rat model of multiple sclerosis by enhancing blood-brain barrier integrity and by modulating the peripheral immune response. PLoS ONE. 2013;8(2):e56586.
Zhou Y, et al. The cross-talk between autophagy and endoplasmic reticulum stress in blood-spinal cord barrier disruption after spinal cord injury. Oncotarget. 2017;8(1):1688–702.
Romero-Ramirez L, Nieto-Sampedro M, Barreda-Manso MA. All roads go to Salubrinal: endoplasmic reticulum stress, neuroprotection and glial scar formation. Neural Regen Res. 2015;10(12):1926–7.
Melloni E, Salamino F, Sparatore B. The calpain-calpastatin system in mammalian cells: properties and possible functions. Biochimie. 1992;74(3):217–23.
Alok A, et al. Curcumin—pharmacological actions and its role in oral submucous fibrosis: a review. J Clin Diagn Res. 2015;9(10):ZE01-3.
Xiao Z, et al. Pharmacological effects of salvianolic acid b against oxidative damage. Front Pharmacol. 2020;11:572373.
Fan ZK, et al. The protective effect of salvianolic acid B on blood-spinal cord barrier after compression spinal cord injury in rats. J Mol Neurosci. 2013;51(3):986–93.
El-Mezayen NS, Abd El Moneim RA, El-Rewini SH. Vitamin B12 as a cholinergic system modulator and blood brain barrier integrity restorer in Alzheimer’s disease. Eur J Pharm Sci. 2022;174:106201.
Xie Y, et al. Fish oil protects the blood-brain barrier integrity in a mouse model of Alzheimer’s disease. Chin Med. 2020;15:29.
Yang T, et al. Protective effects of omega-3 fatty acids in a blood-brain barrier-on-chip model and on postoperative delirium-like behaviour in mice. Br J Anaesth. 2022. https://doi.org/10.1016/j.bja.2022.05.025.
Hong SH, et al. Docosahexaenoic acid improves behavior and attenuates blood-brain barrier injury induced by focal cerebral ischemia in rats. Exp Transl Stroke Med. 2015;7(1):3.
Cheng Y, et al. Photobiomodulation inhibits long-term structural and functional lesions of diabetic retinopathy. Diabetes. 2018;67(2):291–8.
Chao LL. Effects of home photobiomodulation treatments on cognitive and behavioral function, cerebral perfusion, and resting-state functional connectivity in patients with dementia: a pilot trial. Photobiomodul Photomed Laser Surg. 2019;37(3):133–41.
Acknowledgements
Not applicable.
Funding
Get Up and Walk Campaign’ awarded to GK Shea.
Author information
Authors and Affiliations
Contributions
HWK, HY and GKS wrote the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, H.W., Yong, H. & Shea, G.K.H. Blood-spinal cord barrier disruption in degenerative cervical myelopathy. Fluids Barriers CNS 20, 68 (2023). https://doi.org/10.1186/s12987-023-00463-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12987-023-00463-y