Abstract
Background
While previous population studies have shown that higher triglyceride-glucose (TyG) index values are associated with an increased risk of congestive heart failure (CHF), the relationship between TyG and CHF in patients with abnormal glucose metabolism remains understudied. This study aimed to evaluate the association between TyG and CHF in individuals with diabetes and prediabetes.
Methods
The study population was derived from the National Health and Nutrition Examination Survey (NHANES) spanning from 1999 to 2018. The exposure variable, TyG, was calculated based on triglyceride and fasting blood glucose levels, while the outcome of interest was CHF. A multivariate logistic regression analysis was employed to assess the association between TyG and CHF.
Results
A total of 13,644 patients with diabetes and prediabetes were included in this study. The results from the fitting curve analysis demonstrated a non-linear U-shaped correlation between TyG and CHF. Additionally, linear logistic regression analysis showed that each additional unit of TyG was associated with a non-significant odds ratio (OR) of 1.03 (95%CI: 0.88–1.22, P = 0.697) for the prevalence of CHF. A two-piecewise logistic regression model was used to calculate the threshold effect of the TyG. The log likelihood ratio test (p < 0.05) indicated that the two-piecewise logistic regression model was superior to the single-line logistic regression model. The TyG tangent point was observed at 8.60, and on the left side of this point, there existed a negative correlation between TyG and CHF (OR: 0.54, 95%CI: 0.36–0.81). Conversely, on the right side of the inflection point, a significant 28% increase in the prevalence of CHF was observed per unit increment in TyG (OR: 1.28, 95%CI: 1.04–1.56).
Conclusions
The findings from this study suggest a U-shaped correlation between TyG and CHF, indicating that both elevated and reduced levels of TyG are associated with an increased prevalence of CHF.
Similar content being viewed by others
Introduction
Congestive heart failure (CHF), as the terminal stage of various cardiac diseases, has emerged as a significant public health concern impacting residents’ well-being. In the United States alone, CHF affects six million adults over the age of 20 [1, 2], and its mortality rate is rapidly increasing worldwide, imposing a significant social and economic burden on human society [2]. Therefore, to mitigate the incidence and progression of heart failure, it is imperative to concentrate on high-risk cohorts for CHF, such as patients with diabetes and prediabetes.
Diabetes mellitus (DM) constitutes a primary risk factor for cardiovascular outcomes, encompassing HF [3,4,5,6,7,8,9]. The prevalence of heart failure among patients with type 2 diabetes in the United States is estimated to be as high as 22% [10]. Furthermore, research has demonstrated that even individuals with pre-diabetes are at an increased risk for developing HF. The pathophysiological basis of diabetes and pre-diabetes is intricately linked to the dysregulation of glucose metabolism and insulin resistance (IR), thus underscoring the paramount importance of identifying pertinent biomarkers. The triglyceride-glucose (TyG) index is widely employed as a surrogate marker for IR in population-based studies due to its ease of acquisition and has been substantiated by numerous investigations [11,12,13]. Previous studies have established a direct correlation between elevated TyG and structural as well as functional impairment of the left ventricle (LV), accompanied by myocardial fibrosis, consequently increasing the risk of HF [14,15,16,17]. However, the aforementioned research has primarily focused on the general population or patients with coronary heart disease, Even in diabetic patients, only a positive correlation between TyG and HF is found, and most diabetic patients are also complicated with coronary heart disease, cardiac insufficiency and other cardiovascular diseases [18,19,20]. In fact, patients with impaired glucose metabolism and uncomplicated diabetes mellitus represent high-risk populations for heart failure, necessitating increased attention and research efforts. Simultaneously, monitoring TyG levels can serve as a valuable tool to observe disease progression in this cohort, enabling early intervention strategies and improved prognostic outcomes.
To address the research gap concerning the interplay between metabolic factors and heart failure, we leveraged the comprehensive National Health and Nutrition Examination Survey Database, which encompasses a substantial sample size within the US. Our study aimed to investigate the association between the TyG index and CHF among patients with abnormal glucose metabolism.
Methods
Study design and population
The data for this cross-sectional survey was obtained from the ongoing National Health and Nutrition Examination Survey (NHANES) project conducted by the National Center for Health Statistics in the United States. This survey aims to assess the nutritional status and health of the general population in a complex, multi-stage sampling design that combines face-to-face interviews surveys with physical examinations [21]. The research plan of NHANES was approved by the Ethics Review Committee of the National Center for Health Statistics. Since 1999, NHANES has evolved into a continuous cross-sectional survey, wherein nationally representative data from continuous NHANES are collected and published biennially. All participants who participated in the research project provided informed consent by signing a document.
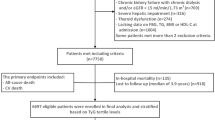
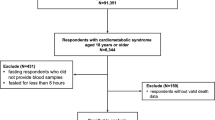
A total of 13,644 individuals were included in the cross-sectional dataset utilized for this analysis. The inclusion criteria encompassed: (1) Participants aged over 18 years between 1999 and 2018; (2) Availability of complete triglyceride and fasting blood glucose data; (3) Presence of comprehensive questionnaire data on CHF; (4) All participants exhibited impaired glucose tolerance or diabetes (Fig. 1).
Definition of the TyG and CHF
The exposure variable, TyG, is derived from the combination of triglyceride and fasting blood glucose levels. The specific details are outlined as follows: TyG = ln [TG (mg/dL)*fasting blood glucose (mg/dL)/2]. The outcome variable, congestive heart failure (CHF), is assessed using a face-to-face questionnaire administered by a trained healthcare professional. Specifically, participants who responded affirmatively to the question “Have doctors or other health professionals ever diagnosed you with CHF?” were considered as having chronic heart failure [22].The final event has received extensive validation in previous scholarly literature [23, 24].
Potential covariates
The covariates considered in this cross-sectional analysis encompass continuous variables, including age, body mass index (BMI), poverty income ratio, glycosylated hemoglobin (HBA1C), estimated glomerular filtration rate (eGFR). Additionally, classified variables such as sex, race, smoking status are also taken into account along with hypertension and hyperlipidemia conditions. Furthermore, the usage of antihypertensive drugs and lipid-lowering drugs is included. The eGFR is calculated using the CKD-EPI formula among the variables considered [25]. BMI can be obtained by dividing weight (kg) by the square of height (m). Prediabetes was defined according to the 2013 American Diabetes Association guidelines as meeting any one of the following criteria: HbA1c between 5.7% and 6.4%, fasting plasma glucose (FPG) between 5.6 mmol/L and 6.9 mmol/L, or a 2-hour plasma glucose value between 7.8 mmol/L and 11.0 mmol/L during an oral glucose tolerance test (OGTT) [26]. Diabetes was defined as a self-reported physician diagnosis of diabetes or having an HbA1c level ≥ 6.5%, FPG level ≥ 7.0 mmol/L, or a 2-hour OGTT plasma glucose level ≥ 11.1 mmol/L.
Statistical analysis
Continuous variables are represented by the mean ± standard deviation (SD), while categorical variables are presented using frequency and percentage. Following quartile of baseline TyG for describing demographic characteristics, we employed chi-square tests to compare differences among categorical variables and conducted variance (ANOVA) analysis for comparing continuous variables. Logistic regression analysis was employed to calculate the odds ratios (ORs) and 95% confidence interval (CI), enabling evaluation of the independent relationship between TyG and CHF. To this end, we have constructed two models.Model 1 was adjusted for age, sex, race, poverty income ratio, BMI, HbA1c. Model 2 was adjusted for age, sex, race, poverty income ratio, BMI, current smoking, HbA1c, eGFR, serum albumin, hypertension, Hyperlipidemia, antihypertensive drugs, lipoprotein-lowering drugs. Additionally, a generalized additive model and the penalty spline method for fitting smooth curves were used to explore the dose-response relationship between the above-mentioned variables. In the event of detecting nonlinearity, we initially employ a recursive algorithm to compute the inflection point and subsequently construct two two-piecewise logistic models on either side of this inflection point. As an additional exploratory analysis, we conducted subgroup analyses and interaction tests to investigate potential effect modifiers of TyG’s impact on the prevalence of CHF. These subgroups included sex (male vs. female), age(< 65 vs. ≥65), BMI (< 25 vs. ≥25), poverty income ratio (< 2.48 vs. ≥2.48), smoking status (never vs. former vs. now), hypertension (no vs. yes), and hyperlipidemia (no vs.yes).
The significance tests were conducted using bilateral approaches, with a predetermined significance level of 0.05. Empower (R; www.empowerstats.com; X&Y Solutions, Inc., Boston, MA, USA) and the R software package (http://www.R-project.org, The R Foundation) were employed for statistical analysis.
Results
Study participants and baseline characteristics
A total of 13,644 participants with impaired glucose tolerance were included in this cross-sectional analysis. The mean age (standard deviation: SD) was 55.83 (16.55) years old, and the average TyG index level (SD) was 8.86 (0.69). Among them, CHF accounted for 4.81% (656 individuals), prediabetes accounted for 6.98% (9,139 individuals), and diabetes accounted for 33.02% (4,505 individuals).
Furthermore, based on the baseline description of the research population in the fourth TyG group, we observed that compared to individuals in the lowest TyG group, those in the highest TyG group exhibited a higher age and a greater proportion of non-hispanic white males and current smokers. Additionally, they demonstrated higher levels of BMI and HBA1C, along with a higher prevalence of hypertension and hyperlipidemia. Moreover, this group displayed increased utilization rates of antihypertensive drugs and lipid-lowering drugs; however, they had lower poverty-income ratios and eGFR levels (Table 1).
Associations between TyG and CHF
The multivariate logistic regression analysis in Table 2 demonstrates the association between TyG and CHF. In fully adjusted model 2, each additional unit of TyG is associated with a non-significant odds ratio (OR) of 1.03 (95%CI: 0.88–1.22, P = 0.697) for prevelance of CHF. We further stratified TyG into categorized variables. In comparison to the participants in the Q1 group (TyG < 8.40), the ORs for CHF prevalence in the Q2 (8.40 < TyG < 8.81), Q3 (8.81 < TyG < 9.25), and Q4 (TyG ≥ 9.25) groups were 0.82 (95% CI: 0.62–1.09), 0.78 (95% CI: 0.59–1.04), and 0.98 (95% CI: 0.73–1.04), respectively. The trend P test > 0.05 suggests the presence of a potential nonlinear correlation between TyG and CHF. Figure 2 visually demonstrates a U-shaped association between TyG and CHF, providing direct evidence for this association. Hence, the utilization of a piecewise logistic regression model is employed to assess the association between TyG and CHF. Two-piecewise logistic-regression model was used to calculate the threshold effect of the TyG (Table 3). If the log likelihood ratio test < 0.05, it means the two-piecewise logistic regression model is superior to the single-line logistic regression model. We observed that the TyG tangent point was 8.60, and on the left side of this point, there existed a negative correlation between TyG and CHF (OR:0.54, 95%CI:0.36–0.81). Conversely, On the right side of the inflection point, we observed a significant 28% increase in the prevalence of CHF per unit increment in TyG (OR:1.28, 95%CI:1.04–1.56 ).
Association between TyG and the prevalence of CHF. A nonlinear association between TyG and the prevalence of CHF was found (P < 0.05). The solid line and dashed line represent the estimated values and their corresponding 95% confidence interval. Adjustment factors included age, sex, race, poverty income ratio, BMI, current smoking, HbA1c, eGFR, serum albumin, hypertension, Hyperlipidemia, antihypertensive drugs, lipoprotein-lowering drugs
Subgroup analyses
In order to validate the robustness of our findings, we conducted subgroup analysis and interaction testing (Fig. 3). Considering the U-shaped association between TyG and CHF, we initially stratified the study population into two groups based on the inflection point of TyG at 8.60, followed by a comprehensive evaluation of the continuous relationship between TyG and CHF within different subgroups. The subgroups examined in this study encompassed sex (male vs. female), age(< 65 vs. ≥65), BMI (< 25 vs. ≥25), poverty income ratio (< 2.48 vs. ≥2.48), smoking status (never vs. former vs. now), hypertension (no vs. yes), and hyperlipidemia (no vs.yes); however, none of these subgroups exhibited any significant interaction with TyG (P for interaction > 0.05 ).
Stratified Analyses by Potential Modifiers of the Association between TyG and the prevalence of CHF * (A) TyG < 8.6 (B) TyG ≥ 8.6. *Each subgroup analysis adjusted for age, sex, race, poverty income ratio, BMI, current smoking, HbA1c, eGFR, serum albumin, hypertension, Hyperlipidemia, antihypertensive drugs, lipoprotein-lowering drugs. except for the stratifying variable
Discussion
In this comprehensive cross-sectional analysis, we have identified, for the first time, a nonlinear relationship between the TyG index and CHF. Specifically, our findings indicate that among patients with impaired glucose tolerance, both excessively low and high TyG index values are associated with an increased prevalence of CHF. This relationship has been found to be consistent across various subgroups.
The majority of prior population-based investigations examining the relationship between the TyG index and HF have indicated that individuals with the highest TyG index values are at an elevated risk of developing HF [14, 15, 17, 27,28,29]. Khalaji et al [29]. conducted a comprehensive systematic evaluation on the association between TyG index and HF events, encompassing 772,809 participants from 30 longitudinal cohort studies. The findings revealed a significant positive correlation between elevated TyG levels and increased prevalence of HF in both diabetic patients and those with coronary heart disease. Given that HF represents the advanced stage of numerous cardiovascular diseases, several clinics have demonstrated that TyG, an independent predictor of cardiovascular diseases such as coronary heart disease, stroke, myocardial infarction, and atrial fibrillation, can effectively monitor the progression and prognosis of these conditions [30,31,32,33].The aforementioned research enhances the impact of the TyG index on occurrences of HFevents.
The subsequent report presents a comprehensive analysis of the association between TyG and occurrences of HF events. Huang et al. reported that the group with the highest quartile of the TyG index (TyG Q4, with a mean value of 9.5) exhibited a significantly higher risk of developing heart failure compared to the group with the lowest quartile of the TyG index (TyG Q1, with a mean value of 8.0) [14]. Signifcantly, two independent reports also confrmed these results. Xu and coworkers demonstrated that in a population-based cohort of 138,620 participants, Q4 of TyG (9.00-11.65) was signifcantly associated with a higher HF incidence compared with Q1 (6.77–8.16) (P < 0.05). Analogously, Zeng et al. reported that in a total of 4992 participants enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) investigation [from 1985 to 1986 (year 0)], only those participants in the Q4 of TyG (8.3–8.7) were at an increased risk of HF events than those in the Q1 (7.1–7.4) throughout the clinical monitoring timeframe (log-rank test, P < 0.001). Remarkably, findings from two separate studies have provided validation for the association between the TyG index and HF incidence.
Xu et al. [15]. conducted a population-based cohort study encompassing 138,620 individuals, revealing that participants within the highest quartile of the TyG index (Q4; range: 9.00-11.65) exhibited a significantly elevated risk of heart failure compared to those in the lowest quartile (Q1; range: 6.77–8.16), with a P-value less than 0.05. In a parallel vein, Zeng and colleagues [27], through their analysis of 4,992 participants from the Coronary Artery Risk Development in Young Adults (CARDIA) study, initiated between 1985 and 1986, identified that individuals in the highest TyG quartile (Q4; range: 8.3–8.7) faced a heightened risk of heart failure events relative to those in the lowest quartile (Q1; range: 7.1–7.4) over the course of clinical follow-up, as evidenced by a log-rank test with a P-value less than 0.001. A study conducted in a Chinese population cohort revealed that HF events gradually increased in accordance with the escalation of the TyG index, whether it was considered as a continuous variable or a categorical variable [17]. Conversely, a study in an American population cohort demonstrated that there was a statistically significant difference in the increase of HF events when TyG was treated as a continuous variable. However, when TyG was classified as a categorical variable, the risk of HF events in the Q4 group (TyG ≥ 9) significantly surpassed that of the Q1-Q3 group (TyG < 9) [28] .
However, it is noteworthy that some studies have also demonstrated a lack of association between the TyG index and the incidence of HF [34,35,36]. Muhammad et al. conducted their study utilizing the Malmö Diet and Cancer Study-Cardiovascular Cohort (MDCS-CV) and The Malmö Preventive Project (MPP) cohorts. They discovered that the increase in the TyG index, when adjusted for potential confounding factors, did not significantly elevate the risk of HF events [35]. Si et al. [36]and their colleagues reported that the TyG index did not exhibit a significant association with HF events in the general population across Europe. Likewise, Jung et al. [34]found that there was no discernible difference in the risk of HF events among cancer survivors, as indicated by a p value greater than 0.05.
Our study represents the first to establish a U-shaped nonlinear correlation between the TyG index and HF in patients with diabetes and pre-diabetes. This finding extends beyond the observation that a higher TyG level significantly increases the prevalence of HF. It also provides an explanation for the phenomenon that TyG and HF have been reported to be unrelated in certain research populations. However, it is noteworthy that the nonlinear correlation between TyG and HF was not further evaluated in our study.The observed non-linear correlation between the TyG index and HF may be attributable to the heterogeneity of diseases across different research populations. Consequently, the TyG index may represent the variability in the body’s response to insulin resistance among diverse study groups. In patients with abnormal glucose metabolism, a lower TyG level may elicit a sudden and intense physiological reaction. However, as the TyG level gradually increases, the body may initiate a compensatory process, resulting in a relatively low prevalence of HF. Nonetheless, with a continuous escalation of the TyG level, the ability to compensate for IR may become progressively compromised. To elucidate the specific mechanism underlying the deleterious effect of low TyG levels on myocardial cells in the context of abnormal glucose metabolism, further basic research investigations are warranted.
The development of heart failure associated with high TyG levels may be attributed to the following mechanisms: Hyperglycemia and elevated triglyceride levels can lead to dysregulation of cardiac energy metabolism, thereby increasing the workload on the heart and promoting the progression of HF [37]. Furthermore, insulin resistance can augment the levels of inflammatory mediators, such as tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6), which may exacerbate inflammatory processes within cardiac tissues and impair heart function [38]. Additionally, IR can induce structural alterations in the heart, including myocardial fibrosis [39, 40].
Advantages and limitations
The TyG index offers several advantages over the traditional gold standard HOMA-IR for detecting insulin resistance markers in population cohorts, including its simplicity of measurement, repeatability, high sensitivity, and cost-effectiveness. Several limitations of our study warrant acknowledgment. Firstly, due to the inherent nature of cross-sectional studies, we cannot establish a causal relationship between the TyG index and HF. Secondly, although we adjusted for relevant covariates, the possibility of unmeasured confounding factors cannot be entirely excluded. Finally, our research population comprised a representative sample of patients with abnormal glucose metabolism in the United States; therefore, the generalizability of our findings to other populations may be limited.
Future directions
The findings of this study serve as a cautionary signal for patients with abnormal glucose metabolism. Both excessively high and excessively low levels of the triglyceride-glucose (TyG) index warrant attention, as our results suggest that the TyG index may exert biological effects beyond its association with IR. However, the underlying mechanisms require further elucidation through basic research investigations and large-scale randomized controlled trials (RCTs).
Conclusions
It is imperative to note that the observed U-shaped correlation between the TyG index and HF prevalence highlights the importance of maintaining optimal levels of this index in patients with dysregulated glucose metabolism. Deviations from the optimal range, either towards higher or lower values, may confer an increased prevalence of HF.
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
References
Chen J, Aronowitz P. Congestive heart failure. Med Clin North Am. 2022;;106:447–58. .
Heidenreich PA, Bozkurt B, Aguilar D. 2022 AHA/ACC/HFSA Guideline for the management of Heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation. 2022;;145:e895–8951032. .
Lehrke M, Marx N. Diabetes Mellitus and Heart failure. Am J Cardiol. 2017;;120:S37–3747. .
Shah AD, Langenberg C, Rapsomaniki E. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1·9 million people. Lancet Diabetes Endocrinol. 2015;;3:105–13. .
Rao Kondapally Seshasai S, Kaptoge S, Thompson A. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;;364:829–41. .
Aune D, Schlesinger S, Neuenschwander M. Diabetes mellitus, blood glucose and the risk of heart failure: a systematic review and meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis. 2018;;28:1081–91. .
Lehrke M, Marx N. Diabetes Mellitus and Heart failure. Am J Med. 2017;;130:S40–4050. .
Jankauskas SS, Kansakar U, Varzideh F. Heart failure in diabetes. Metabolism. 2021;;125:154910. .
Pandey A, Khan MS, Patel KV. Predicting and preventing heart failure in type 2 diabetes. Lancet Diabetes Endocrinol. 2023;;11:607–24. .
Dunlay SM, Givertz MM, Aguilar D. Type 2 diabetes Mellitus and Heart failure: a Scientific Statement from the American Heart Association and the Heart Failure Society of America: this statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation. 2019;;140:e294–294324. .
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;;95:3347–51. .
Ramdas Nayak VK, Satheesh P, Shenoy MT. Triglyceride glucose (TyG) index: a surrogate biomarker of insulin resistance. J Pak Med Assoc. 2022;;72:986–8. .
Rodríguez-Morán M, Simental-Mendía LE, Guerrero-Romero F. The triglyceride and glucose index is useful for recognising insulin resistance in children. Acta Paediatr. 2017;;106:979–83. .
Huang R, Lin Y, Ye X. Triglyceride-glucose index in the development of heart failure and left ventricular dysfunction: analysis of the ARIC study. Eur J Prev Cardiol. 2022;;29:1531–41. .
Xu L, Wu M, Chen S. Triglyceride-glucose index associates with incident heart failure: a cohort study. Diabetes Metab. 2022;;48:101365. .
Yang S, Du Y, Liu Z. Triglyceride-glucose index and extracellular volume fraction in patients with heart failure. Front Cardiovasc Med. 2021;;8:704462. .
Li X, Chan J, Guan B. Triglyceride-glucose index and the risk of heart failure: evidence from two large cohorts and a mendelian randomization analysis. Cardiovasc Diabetol. 2022;;21:229. .
Chen Y, Fu J, Wang Y. Association between triglyceride glucose index and subclinical left ventricular systolic dysfunction in patients with type 2 diabetes. Lipids Health Dis. 2023;;22:35. .
Sun QC, Liu J, Meng R. Association of the triglyceride-glucose index with subclinical left ventricular dysfunction in type 2 diabetes mellitus patients: a retrospective cross-sectional study. J Diabetes Investig. 2023;;14:953–60. .
Tai S, Fu L, Zhang N. Impact of baseline and trajectory of triglyceride-glucose Index on Cardiovascular outcomes in patients with type 2 diabetes Mellitus. Front Endocrinol (Lausanne). 2022;;13:858209. .
Johnson CL, Paulose-Ram R, Ogden CL. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat. 2013:;2:1–24. .
Abdalla SM, Yu S, Galea S. Trends in Cardiovascular Disease Prevalence by Income Level in the United States. JAMA Netw Open. 2020;;3:e2018150. .
Wu Z, Tian T, Ma W. Higher urinary nitrate was associated with lower prevalence of congestive heart failure: results from NHANES. BMC Cardiovasc Disord. 2020;;20:498. .
Zhan X, Liu Y, Chen T. The association between serum testosterone level and congestive heart failure in US male adults: data from National Health and Nutrition Examination Survey (NHANES) 2011–2016. Reprod Biol Endocrinol. 2024;;22:4. .
Levey AS, Stevens LA, Schmid CH. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;;150:604–12. .
Standards of medical care in diabetes–2013. Diabetes Care. 2013;;36(Suppl 1):S11–66.
Zeng X, Han D, Zhou H. Triglyceride-glucose index and Homeostasis Model Assessment-Insulin Resistance in Young Adulthood and Risk of Incident Congestive Heart failure in midlife: the coronary artery risk development in young adults study. Front Cardiovasc Med. 2022;;9:944258. .
Li X, Wang J, Niu L. Prevalence estimates of the insulin resistance and associated prevalence of heart failure among United Status adults. BMC Cardiovasc Disord. 2023;;23:294. .
Khalaji A, Behnoush AH, Khanmohammadi S. Triglyceride-glucose index and heart failure: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;;22:244. .
Yang Y, Huang X, Wang Y. The impact of triglyceride-glucose index on ischemic stroke: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;;22:2. .
Liang S, Wang C, Zhang J. Triglyceride-glucose index and coronary artery disease: a systematic review and meta-analysis of risk, severity, and prognosis. Cardiovasc Diabetol. 2023;;22:170. .
Azarboo A, Behnoush AH, Vaziri Z. Assessing the association between triglyceride-glucose index and atrial fibrillation: a systematic review and meta-analysis. Eur J Med Res. 2024;;29:118. .
Liu X, Tan Z, Huang Y. Relationship between the triglyceride-glucose index and risk of cardiovascular diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;;21:124. .
Jung MH, Yi SW, An SJ. Associations between the triglyceride-glucose index and cardiovascular disease in over 150,000 cancer survivors: a population-based cohort study. Cardiovasc Diabetol. 2022;;21:52. .
Muhammad IF, Bao X, Nilsson PM. Triglyceride-glucose (TyG) index is a predictor of arterial stiffness, incidence of diabetes, cardiovascular disease, and all-cause and cardiovascular mortality: a longitudinal two-cohort analysis. Front Cardiovasc Med. 2022;;9:1035105. .
Si S, Li J, Li Y. Causal effect of the triglyceride-glucose index and the joint exposure of higher glucose and triglyceride with extensive cardio-cerebrovascular metabolic outcomes in the UK Biobank: a mendelian randomization study. Front Cardiovasc Med. 2020;;7:583473. .
Shah MS, Brownlee M. Molecular and Cellular mechanisms of Cardiovascular disorders in Diabetes. Circ Res. 2016;;118:1808–29. .
Pickup JC, Crook MA. Is type II diabetes mellitus a disease of the innate immune system. Diabetologia. 1998;;41:1241–8. .
Spinale FG. Myocardial matrix remodeling and the matrix metalloproteinases: influence on cardiac form and function. Physiol Rev. 2007;;87:1285–342. .
Wu QQ, Xiao Y, Yuan Y. Mechanisms contributing to cardiac remodelling. Clin Sci (Lond). 2017;;131:2319–45. .
Acknowledgements
A special thanks to all of the NHANES participants who freely gave their time to make this and other studies possible.
Funding
This work was supported by the Cultivation of backup projects for National Science and Technology Awards(20223AEI91007), Jiangxi Science and Technology Innovation Base Plan - Jiangxi Clinical Medical Research Center(20223BCG74012), Jiangxi Provincial Natural Science Foundation (20232BAB206140), Fund project of the Second Affiliated Hospital of Nanchang University(2021efyA01).
Author information
Authors and Affiliations
Contributions
YMS participated in literature search, study design, data collection, data analysis, data interpretation, and wrote the manuscript.YMS and CY conceived of the study, and participated in its design, coordination, data collection and analysis. CY participated in study design and provided the critical revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were following the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, Y., Yu, C. U shape association between triglyceride glucose index and congestive heart failure in patients with diabetes and prediabetes. Nutr Metab (Lond) 21, 42 (2024). https://doi.org/10.1186/s12986-024-00819-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-024-00819-7