Abstract
Backgrounds
Mycoplasma pneumoniae (M. pneumoniae) is a common pathogen causing respiratory diseases in children. This study aimed to characterize epidemiological and disease severity shifts of M. pneumoniae: infections in Guangzhou, China during and after the coronavirus disease 2019 (COVID-19) pandemic.
Methods
Throat swab samples were obtained from 5405 hospitalized patients with symptoms of acute respiratory infections to detect M. pneumoniae. Differences in epidemiological and clinical characteristics of M. pneumoniae: infections were investigated during 2020–2022 and after COVID-19 pandemic (2023).
Results
M. pneumoniae were detected in 849 (15.6%, 849/5405) patients. The highest annual positive rate was 29.4% (754/2570) in 2023, followed by 5.3% (72/1367) in 2022, 1.2% (12/1015) in 2021, and 2.0% (11/553) in 2020, with significantly increasing annual prevalence from 2020 to 2023. M. pneumoniae incidence peaked between July and December post-COVID-19 pandemic in 2023, with the highest monthly positive rate (56.4%, 165/293). Clinical characteristics and outcomes of patients with M. pneumoniae did not vary between periods during and after COVID-19 pandemic except that patients with M. pneumoniae post-COVID-19 pandemic were more likely to develop fever. Patients with severe M. pneumoniae pneumonia (SMPP) were more likely to develop respiratory complications, myocardial damage, and gastrointestinal dysfunction than those with non-SMPP. Patients with SMPP had lower lymphocytes, CD3+ T cells, CD4+ T cells, CD8+ T cells, B cells, and higher IL-4, IL-6, IL-10 levels than those with non-SMPP. Bronchoalveolar lavage fluid specimens from infected patients were obtained to identify macrolide resistance mutations. Macrolide-resistant M. pneumoniae (MRMP) proportion in 2023 was 91.1% (215/236).
Conclusion
Outbreaks of M. pneumoniae: occurred in Guangzhou, China in 2023 upon Non-pharmaceutical interventions easing. Despite the increasing incidence of M. pneumoniae, the disease severity remained similar during and after the COVID-19 pandemic.
Similar content being viewed by others
Introduction
Mycoplasma pneumoniae (M. pneumoniae), which is the smallest self-living and cell-wall-less bacterium, commonly causes upper and lower respiratory tract infections, particularly in children and young adults [1,2,3]. M. pneumoniae infections contribute significantly to the disease burden in children, accounting for 10–30% of community-acquired pneumonia (CAP) cases [4, 5]. M. pneumonia infections may induce extrapulmonary complications, such as myocardial injury, abnormal liver function, kidney damage, encephalitis, gastrointestinal dysfunction, Stevens-Johnson syndrome, and arthritis [6,7,8].
During COVID-19 pandemic, the widespread adoption of non-pharmaceutical interventions (NPIs), such as mask wearing, hand hygiene, social distancing, travel restrictions, and school closure reduced the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and altered the prevalence patterns of other common respiratory pathogens [9]. Globally, M. pneumonia infections occur in regional outbreaks every three to seven years, each lasting for 1–2 years. A nationwide retrospective cohort study revealed that two epidemics of M. pneumonia (2011 and 2015) took place in South Korea [10]. Previous studies showed that there was an M. pneumoniae epidemic from 2015 to 2016 in Beijing [11]. Moreover, outbreaks of M. pneumoniae occurred in Southern Taiwan in 2019–2020, with the peak case numbers occurring between July 2019 and January 2020 [12]. Cheng et al. reported a M. pneumoniae outbreak in Beijing, China, in the summer of 2019, while M. pneumoniae activity notably reduced during the COVID-19 pandemic (2020–2021) [13]. Previous studies have shown significantly reduced M. pneumoniae positive rates in 2020 compared to 2012 and 2016 in Japan and Finland [14, 15]. Previous global M. pneumoniae surveillance studies revealed that the most recent M. pneumoniae epidemic occurred in late 2019-early 2020 simultaneously across multiple nations, predominantly in Europe and Asia; however, after the NPIs, M. pneumoniae positive rates dramatically dropped in 20 countries across Asia, Oceania, the Americas, and Europe during the COVID-19 pandemic in 2020–2022 [16, 17].
For most respiratory pathogens, a reduction was observed in the early phase of COVID-19 pandemic [18]. However, resurgence of respiratory pathogens was observed when NPIs eased [19]. Previous studies have reported a marked resurgence of respiratory syncytial virus(RSV) in England and Australia, which was associated with the relaxation of COVID-19 measures [20, 21]. Previous studies have reported an unusual resurgence of human metapneumovirus in South Korea and Western Australia after the COVID-19 pandemic [22, 23]. Global prospective surveillance data in previous study showed the re-emergence of M. pneumoniae in Europe and Asia in 2023 [24]. Changes in epidemiological, macrolide resistance, and clinical characteristics caused by M. pneumoniae infections when measures to restrict SARS-CoV-2 transmission were relaxed in Guangzhou, China remain unclear.
This study investigated the epidemiological, macrolide-resistant, and clinical characteristics of M. pneumoniae infections in two distinct periods, January 2020 to December 2022 and January 2023 to December 2023, encompassing the periods during and after the COVID-19 pandemic.
Materials and methods
Study population
From 1 January 2020 to 31 December 2023, hospitalized children under 14 years of age who were diagnosed with acute respiratory tract infections (ARTIs) at the First Affiliated Hospital of Guangzhou Medical University were enrolled. Diagnosis of pediatric M. pneumoniae pneumonia (MPP) was performed by attending physicians according to the Guidelines for Diagnosis and Treatment of M. pneumoniae pneumonia in Children as follows: (i) fever, or acute respiratory symptoms (cough, tachypnea, difficulty breathing) or both; (ii) low breathing or dry, wet rales; (iii) chest film findings characterized by lung portal lymph node and lung gate shadow, bronchopneumonia, interstitial pneumonia, and large and high-density shadow; (iv) children with positive polymerase chain reaction (PCR) results or M. pneumoniae antibody titer ≥ 1:160. SMPP was defined as MPP with one of the following: (i) disturbance of consciousness; (ii) hypoxemia, consisting of respiratory rate (RR) ≥ 70/min (infant), RR ≥ 50/min (over 1 year old), assisted breathing (groan, nasal fan, three concave sign), intermittent apnea, and oxygen saturation < 92%; (iii) persistent high fever for more than 5 days; (iv) dehydration; (v) chest X-ray showed that multiple lobes were involved or complicated with pleural effusion; and (vi) serious extrapulmonary complications, according to the guideline for diagnosis and treatment of CAP in children (2019 version) [25].
Specimen detection
Throat swab samples were collected within 24 h after admission for M. pneumoniae screening following established clinical protocols. Real-time polymerase chain reaction (RT-PCR) testing was performed to M. pneumoniae using a commercial kit (Daan Gene Co., Ltd., Guangzhou, China) based on the recommended protocol. Amplifications were performed using an Applied Biosystems 7500 Real-Time PCR system (Applied Biosystems, Foster City, USA).
Lymphocyte subset detection
Ethylene diamine tetra acetic acid anticoagulated whole blood samples (2 mL) were collected from patients with SMPP (n = 108) and non-SMPP (n = 281) within 24 h after admission. Briefly, CD3+T cells, CD3+CD4+T cells, CD3+CD8+T cells, CD19+B cells, and CD16+CD56+NK cells were measured using multi-color flow cytometry with panels 1 and 2. Panel 1 included CD3-FITC, CD4-APC, CD8-PE, and CD45-PerCP. Panel 2 comprised CD3-FITC, CD19-APC, CD16-PE, CD56-PE and CD45-PerCP (Agilent Multitest). Cells were acquired on a NovoCyte D3000 flow cytometer (Agilent Technologies, Palo Alto, USA) following the manufacturer’s instructions. All flow cytometry data were acquired and analyzed using Agilent NovoExpress software.
Cytokine assays
The serum samples from patients with SMPP (n = 142) and non-SMPP (n = 323) were collected within 24 h after admission. The serum levels of interleukin-1β (IL-1β), IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12P70, IL-17 A, interferon-α (IFN-α), IFN-γ, and tumor necrosis factor-α (TNF-α) were detected according to the 12 cytokine detection kit manufacturer’s instructions (Jiangxi Saiji Biotechnology Limited Company) on a MateCyte 2L6C flow cytometer (Challen Biotechnology Co., Ltd., Hunan, China). The FCAP Array™ v 3.0.1 software returned data as Median Fluorescence Intensity and concentration (pg/ml).
Data collections
Demographic information, age, sex, clinical symptoms and signs, extrapulmonary complications, treatment and length of hospital stay were collected retrospectively from patient records. Laboratory findings including white blood cell (WBC) counts, neutrophil counts, lymphocyte counts, erythrocyte counts, hemoglobin (Hb), platelet (PLT), K+, Na+, Cl-, total protein (TP), albumin (ALB), total biliary acid (TBA), gamma-glutamyl transferase (GGT), alanine transaminase (ALT), aspartate transaminase (AST), creatine kinase (CK), lactate dehydrogenase (LDH), procalcitonin (PCT), C-reactive protein (CRP), prothrombin time (PT), Fibrinogen (FIB), Activated partial thromboplastin time (APPT), D-dimer, Ceruloplasmin, immunoglobulin (Ig)G, IgM, and IgA were conducted within 24 h after admission.
Macrolide-resistant mutations of M. pneumoniae
The main indications of bronchoalveolar lavage fluid (BALF) were as follows: (i) diagnosis of infection: persistent infection symptoms despite empirical treatment, necessitating clarification of the etiology, suspected infections involving unusual pathogens, mixed pathogens, or drug-resistant bacteria, and severe pneumonia requiring mechanical ventilation; (ii) therapeutic removal of airways materials; (iii) diagnosis of noninfectious lung diseases; (iv) evaluation of alveolar inflammatory processes [26]. Among the 754 cases of M. pneumoniae infection in 2023, 236 BALF samples from infected patients were obtained and transferred by an uninterrupted cold-chain transportation to KingMed, Guangzhou, China for tNGS detection to identify pathogens and macrolide-resistance mutation. Nucleic acid extraction was performed using the MetaPure DNA & RNA Extraction Kit (KingCreate, Guangzhou, China), and library preparation was performed using the RP100™ Respiratory Pathogen Microorganisms Multiplex Testing Kit (KingCreate, Guangzhou, China). Sequencing was carried out on Illumina MiniSeq Platform using the MiniSeq Rapid Reagent Kit (Illumina, CA, USA) as previously described [27]. The sequencing data generated was analyzed using a customized bioinformatics workflow. Fastp v0.20.1 was used for adaptor trimming and low-quality filtering, and Bowtie2 v2.4.1 was utilized to map the reads of each sample against tNGS special authoritatively classified database in very-sensitive mode. If the best alignment of the reads dropped into one target amplicon region, the reads were counted. The count number of each target amplicon was summed and normalized to 100,000. The number of reads per 100,000 (RPhK) was calculated for species or genus level. and subsequently indicated as the target pathogen result (RPhK ≥ 10). Macrolide-resistance mutations of M. pneumoniae including 23 S rRNA: A2063G, A2064G, A2067G, and A2617G, were calling using samtools mpileup [28]. The mutation rate was obtained by calculating the ratio of the depth of the mutation at the site to the total depth. The threshold for mutation calling was 10%.
Statistical analysis
All analyses were performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA). Normally distributed data were presented as mean ± standard deviation. Categorical variables were summarized as frequencies and proportions. An unpaired t-test was used to compare the normally distributed parameters of the two groups, and all tests were two-tailed. The Chi‐square or Fisher’s exact test was utilized for classified variables. Linear regression models with gamma values were used to assess changes in prevalence over the calendar year. P < 0.05 was considered statistically significant.
Results
Study population and detection of M. pneumoniae
As shown in Table 1, from January 2020 to December 2023, 5405 hospitalized children with ARTI were enrolled, including 553 patients in 2020, 1015 patients in 2021, 1267 patients in 2022 (during the COVID-19 pandemic); and 2570 patients in 2023 (after the COVID-19 pandemic). A total of 849 (15.6%, 849/5405) cases were caused by M. pneumoniae. The highest annual positive rate was 29.4% (754/2570) in 2023, followed by 5.3% (72/1367) in 2022, 1.2% (12/1015) in 2021, and 2.0% (11/553) in 2020. The annual prevalence of M. pneumoniae showed an obvious increasing trend from 2020 to 2023 (P < 0.001).
Temporal distribution of M. pneumoniae
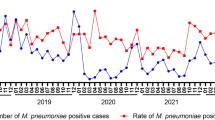
The monthly distributions of M. pneumoniae in 2020–2023 are illustrated in Fig. 1. During the COVID-19 pandemic, M. pneumoniae infections rarely occurred in 2020–2022, coinciding with the implementation of NPIs against COVID-19. Interestingly, M. pneumoniae notably increased since June and showed peaks between July and December after the COVID-19 pandemic in 2023, especially the highest monthly positive rate (56.4%, 165/293).
Macrolide-resistant M. pneumoniae (MRMP)
Among the 754 cases of M. pneumoniae infection in 2023, 236 BALF samples from patients infected with M. pneumoniae were obtained for tNGS detection to identify macrolide -resistance mutations. Of 236 clinical M. pneumoniae strains, 215 carried macrolide resistance mutations in the 23 S rRNA gene. All macrolide resistance mutations were A2063G transitions, and MRMP proportion was 91.1% (215/236) in 2023.
Clinical characteristics and laboratory findings of hospitalized patients infected with M. pneumoniae during and after the COVID-19 pandemic
We compared the clinical characteristics of hospitalized patients infected with M. pneumoniae during (2020 and 2022) and after the COVID-19 pandemic (2023) to investigate whether the clinical characteristics of M. pneumoniae infection changed during the post-pandemic period (Table 2). Patients with M. pneumoniae were older after the COVID-19 pandemic than during the COVID-19 pandemic (P < 0.001). A total of 754 patients with M. pneumoniae after the COVID-19 pandemic were categorized into four age groups, including 30 patients in age ≤ 1 years old group, 81 patients in age 1–3 years old group, 261 patients in 3–6 years old group, 382 patients in > 6 years old group, respectively. Most patients with M. pneumoniae after the COVID-19 pandemic were > 3 years old (85.4%). The most common symptoms were cough, fever, and pharyngodynia. Clinical characteristics, extra-pulmonary manifestations and outcomes of M. pneumoniae-infected patients did not vary between the periods during and after the COVID-19 pandemic, except that patients with M. pneumoniae after the COVID-19 pandemic were more likely to have fever (P = 0.001). Patients infected with M. pneumoniae after the COVID-19 pandemic had a higher rate of co-infection with respiratory viruses than those during the COVID-19 pandemic (P = 0.03) (Table 3).
The laboratory findings of hospitalized patients with M. pneumoniae between the periods during and after the COVID-19 pandemic are summarized in Table S1. Fibrinogen levels and neutrophil counts for these patients were higher after the COVID-19 pandemic than during the COVID-19 pandemic (P < 0.001 and P = 0.007, respectively). The lymphocyte counts in patients with M. pneumoniae after the COVID-19 pandemic were lower than those during the COVID-19 pandemic (P < 0.001).
Clinical characteristics and laboratory findings of patients with non-SMPP and SMPP
Among the 849 cases of M. pneumoniae infection, 639 (75.3%) and 201 (23.7%) were diagnosed with non-SMPP and SMPP, respectively, and the clinical characteristics of patients diagnosed with non-SMPP and SMPP were compared (Table 4). No significant differences in sex or age were observed between the non-SMPP and SMPP groups (P > 0.05). No significant differences in the rate of MRMP were observed between the non-SMPP and SMPP groups (P > 0.05). Patients with SMPP were more likely to have fever, wheezing, shortness of breath, three concave signs, hypoxemia, and pleural effusion compared to those with non-SMPP (P < 0.05). Patients with SMPP were more susceptible to myocardial damage, gastrointestinal dysfunction, and electrolyte disturbances than those with non-SMPP (P < 0.05). Patients with SMPP received bronchoscopy therapy (P < 0.001), and oxygen therapy (P < 0.001) more often than those with non-SMPP. Patients with SMPP were more likely to have longer length of hospital stay, compared to those with non-SMPP (P < 0.001). Patients infected with SMPP had a higher rate of coinfection with viruses and bacteria than those with non-SMPP (P = 0.007 and P = 0.032, respectively). Patients with SMPP were more likely to be coinfected with rhinovirus and Streptococcus pneumoniae than those with non-SMPP (P = 0.016 and P = 0.009, respectively) (Table 3).
Laboratory findings of patients with non-SMPP and SMPP were analyzed (Table S2). Patients with SMPP had significantly higher neutrophil and lower lymphocyte counts than those with non-SMPP. CRP, PCT, D-dimer, AST, CK, and LDH levels were significantly higher in patients with SMPP than those with non-SMPP. Hemoglobin, TP, ALB, Na+, and Cl- levels were significantly lower in patients with SMPP than those with non-SMPP. As shown in Fig. 2, CD3+ T cells, CD4+ T cells CD8+ T cells, and B cells were significantly lower in patients with SMPP than those with non-SMPP. As shown in Fig. 3, there were no statistically significant differences in the serum levels of IL-1β, IL-2, IL-5, IL-8, IL-12P70, TNF-α, IFN-α, IFN-γ and IL-17 A between patients with non-SMPP and SMPP. Serum levels of IL-4, IL-6, and IL-10 were significantly higher in patients with SMPP than those with non-SMPP.
Discussion
In this study, we systematically compared the epidemiology, and clinical characteristics of M. pneumoniae among hospitalized children in Guangzhou, China, during and after the COVID-19 pandemic. Our study revealed a notable reduction in M. pneumoniae activity during the COVID-19 pandemic (2020–2022), coinciding with the implementation of NPIs. These findings are in line with several reports [13, 29,30,31], suggesting that COVID-19 restrictive measures had effectively reduced M. pneumoniae transmission. We further observed that outbreaks of M. pneumoniae occurred in Guangzhou, China in 2023, following the relaxation of measures to restrict SARS-CoV-2 transmission. Recently, Gong et al. reported that the increase in incidence of respiratory diseases among children in Beijing between September and November 2023 coincided with an increased positivity rate of common respiratory pathogens, predominantly M. pneumoniae [32]. Additionally, since late October 2023, an epidemic of M. pneumoniae has occurred in Denmark [33]. As for explanations, the extraordinary absence of M. pneumoniae during the COVID-19 pandemic (2020–2022) probably resulted in young children without natural immunity to M. pneumoniae, thereby causing M. pneumoniae infection outbreaks upon NPIs easing. Additionally, we found that there was an M. pneumoniae epidemic in Guangzhou, China in 2019 (Figure S1). Therefore, the M. pneumoniae outbreaks in 2023 might be a return of the cyclical M. pneumoniae outbreaks witnessed prior to the COVID-19 pandemic, since M. pneumoniae epidemics typically occur every three to seven years. We found that M. pneumoniae revealed peaks between July and December in Southern China after the COVID-19 pandemic in 2023, which was largely consistent with other reports [34].
We further compared the clinical characteristics and laboratory findings of hospitalized patients infected with M. pneumoniae during (2020 and 2022) and after the COVID-19 pandemic (2023). Our results suggest that patients with M. pneumoniae after the COVID-19 pandemic (2023) had a higher rate of coinfection with respiratory viruses than those during the COVID-19 pandemic. Previous studies revealed that resurgence of respiratory pathogens was observed after NPIs easing, such as influenza A, influenza B, RSV, and human metapneumovirus [19]. Our data revealed that patients with M. pneumoniae were older in 2023 than those in 2020–2022. Maison et al. presented a shift in the average age of influenza A and RSV infection to older children upon NPIs easing in Germany [35]. One possible explanation is the accumulation of a susceptible population and subsequent decline in population immunity due to NPIs implemented during the COVID-19 pandemic. Meanwhile, with the lifting of NPIs, school-aged children attended school, leading to a widespread trend. Hence, some researchers have speculated whether a large outbreak and more severe pulmonary and extrapulmonary symptoms will be caused by M. pneumoniae infection [17]. In our study, no significant differences were found in the clinical characteristics and outcomes of patients with M. pneumoniae during and after the COVID-19 pandemic, except that patients with M. pneumoniae after the COVID-19 pandemic were more likely to have fever.
In recent years, severe M. pneumoniae pneumonia had been reported worldwide, resulting in a significant disease burden on children. In our study, 201 (23.7%, 201/849) cases were diagnosed with SMPP. We found that patients with SMPP were more likely to have fever, wheezing, shortness of breath, three concave sign, hypoxemia, and pleural effusion than those with non-SMPP. Our results also indicated that patients with SMPP were more likely to show myocardial damage and gastrointestinal dysfunction, consistent with previous reports [36, 37].
Patients with SMPP were more likely to be coinfected with rhinovirus and Streptococcus pneumoniae than those with non-SMPP in this study, which was largely consistent with other reports [34]. Innate and adaptive immune responses play critical roles in the defense against pathogen infection and disease progression. In this study, M. pneumoniae infections resulted in a broad reduction in immune cells, including lymphocytes, CD3+ T cells, CD4+ T cells, CD8+ T cells and B cells in patients with SMPP. Our results suggest that decreases in lymphocyte, CD3+ T cell, CD4+ T cell, CD8+ T cell and B cell counts were correlated with disease severity in patients with M. pneumoniae. Previous studies revealed that CD4+ effector memory T cells form the major population of the pathogen-specific IFN-γ response in children with MPP and that the presence of these cells in peripheral blood correlates with pulmonary disease severity [38]. Similar to bacterial or viral infection, M. pneumoniae infection can also stimulate a variety of immunoactive cells to produce hyperactive cytokine-mediated inflammatory response, leading to body damage. Previous reports revealed that compared to healthy controls, serum levels of PCT, IL-6, IL-8, TNF-α, and IL-10 were significantly higher in patients with M. pneumoniae [39]. We further found that the serum levels of IL-4, IL-6, and IL-10 were higher in patients with SMPP than those with non-SMPP. Deng et al. reported that patients with SMPP had significantly higher levels of TNF-α, IL-6, and IL-10 in their BALF than those with non-SMPP [40]. Collectively, these findings imply that elevated levels of IL-6 and IL-10 are indicative of the severity of inflammation and pneumonia.
Macrolides are first-line agents for treating M. pneumoniae infections. Understanding the prevalence of MRMP is crucial due to limited number of alternative therapies available to children. The global prevalence of MRMP infection, especially in Asian regions, is increasing rapidly. We found a high rate of MRMP (91.1%, 215/236) among children with M. pneumoniae in Guangzhou, China in 2023. No significant differences in the rate of MRMP were observed between the non-SMPP and SMPP groups in this study, which was largely consistent with other reports [41]. In total, 36 (63%, 36/57) strains were classified as MRMP with mutations in A2063G in Shenzhen, China in 2010–2011 [42]. A multicenter population-based epidemiological study revealed that the total MRMP proportion in patients with ARTI from 35 sentinel hospitals in Beijing from 2018 to 2020 was 84.7% (402/474), with 74.4% in 2018, 90.6% in 2019, and 93.9% in 2020 [43]. Wu et al. reported that the total proportion of MRMP in Taiwan from 2017 to 2019 was 38.4% (53/138), with 10.6% in 2017, 47.5% in 2018, and 62.5% in 2019 [44]. In 2015, the rate of MRMP was 87.2% (82/94) in children with M. pneumoniae pneumonia in Korea [45]. These findings revealed that the increase in MRMP in many regions is due to the selective antibiotic pressure on children during periods of extensive macrolide use. Therefore, continuous monitoring of occurrence and antimicrobial susceptibility of MRMP is necessitated to control its spread and establish strategies for treating second-line antibiotic resistant M. pneumoniae infections.
This study has several limitations. First, this was a single-center retrospective study, not a multicenter retrospective study. Second, the study population included hospitalized pediatric patients with M. pneumoniae and did not include outpatients. Third, M. pneumoniae strains were exclusively screened for gene mutations associated with macrolide resistance; however, a phenotypic assessment of drug resistance was not conducted. Fourth, some hospitalized patients with M. pneumoniae were coinfected with other bacteria or viruses.
In conclusion, this study revealed that the COVID-19 restrictive measures had effectively reduced the transmission of M. pneumoniae during the COVID-19 pandemic (2020–2022). There were outbreaks of M. pneumoniae in Guangzhou, China in 2023, following the easing of NPIs. The rate of MRMP was 91.1% (215/236) among children with M. pneumoniae in Guangzhou, China in 2023. Clinical characteristics and outcomes of patients with M. pneumoniae did not vary during and after the COVID-19 pandemic. Patients with SMPP were more likely to develop respiratory complications, myocardial damage, electrolyte disturbance and gastrointestinal dysfunction than those with non-SMPP. This study comprehensively analyzed the changes in M. pneumoniae during and after the COVID-19 pandemic in terms of incidence, temporal distribution, prevalence of macrolide resistance, and clinical features, providing invaluable data for monitoring, infection prevention, control, and treatment of M. pneumoniae in the post-pandemic.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ARTIs:
-
Acute respiratory tract infections
- CAP:
-
Community-acquired pneumoniae
- COVID-19:
-
Coronavirus disease 2019
- M. pneumoniae :
-
Mycoplasma pneumoniae
- MPP:
-
M. pneumoniae pneumonia
- MRMP:
-
Macrolide-resistant Mycoplasma pneumoniae
- NPIs:
-
Non-pharmaceutical interventions
- RSV:
-
Respiratory syncytial virus
- SMPP:
-
Severe M. pneumoniae pneumonia
- tNGS:
-
Targeted next-generation sequencing
References
Atkinson TP, Balish MF, Waites KB. Epidemiology, clinical manifestations, pathogenesis and laboratory detection ofMycoplasma pneumoniaeinfections. FEMS Microbiol Rev. 2008;32:956–73.
Song Z, Jia G, Luo G, Han C, Zhang B, Wang X. Global research trends of Mycoplasma pneumoniae pneumonia in children: a bibliometric analysis. Front Pead. 2023;11:1306234.
Kumar S, Kumar S. Mycoplasma pneumoniae: among the smallest bacterial pathogens with great clinical significance in children. Ind J Med Microbiol. 2023;46:100480.
Kutty PK, Jain S, Taylor TH, Bramley AM, Diaz MH, Ampofo K, et al. Mycoplasma pneumoniae among children hospitalized with community-acquired pneumonia. Clin Infect Dis. 2019;68:5–12.
Zhu Y, Tang X, Lu Y, Zhang J, Qu J. Contemporary situation of community-acquired pneumonia in China: a systematic review. J Translational Intern Med. 2018;6:26–31.
Zheng Y, Hua L, Zhao Q, Li M, Huang M, Zhou Y, et al. The level of D-Dimer is positively correlated with the severity of Mycoplasma pneumoniae pneumonia in children. Front Cell Infect Microbiol. 2021;11:100807.
Poddighe D. Extra-pulmonary diseases related to Mycoplasma pneumoniae in children: recent insights into the pathogenesis. Curr Opin Rheumatol. 2018;30:380–7.
Xu M, Li Y, Shi Y, Liu H, Tong X, Ma L, et al. Molecular epidemiology of Mycoplasma pneumoniae pneumonia in children, Wuhan, 2020–2022. BMC Microbiol. 2024;24:23.
Li ZJ, Yu LJ, Zhang HY, Shan CX, Lu QB, Zhang XA, et al. Broad impacts of Coronavirus disease 2019 (COVID-19) pandemic on acute respiratory infections in China: an observational study. Clin Infect Dis. 2022;75:e1054–62.
Lee E, Kim CH, Lee YJ, Kim HB, Kim BS, Kim HY, et al. Annual and seasonal patterns in etiologies of pediatric community-acquired pneumonia due to respiratory viruses and Mycoplasma pneumoniae requiring hospitalization in South Korea. BMC Infect Dis. 2020;20:e1054–62.
Yan C, Sun H, Zhao H, Onderdonk AB. Latest surveillance data on Mycoplasma pneumoniae infections in children, suggesting a new epidemic occurring in Beijing. J Clin Microbiol. 2016;54:1400–1.
Kuo C, Tsai W, Lee H, Ho T, Huang L, Shen C, et al. The epidemiology, clinical characteristics, and macrolide susceptibility of Mycoplasma pneumoniae pneumonia in children in Southern Taiwan, 2019–2020. J Microbiol Immunol Infect. 2022;55:611–9.
Cheng Y, Cheng Y, Dai S, Hou D, Ge M, Zhang Y, et al. The prevalence of Mycoplasma Pneumoniae among children in Beijing before and during the COVID-19 pandemic. Front Cell Infect Microbiol. 2022;12:854505.
Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children – A nationwide register study in Finland. EClinicalMedicine. 2021;34:100807.
Fujita J. Mycoplasma pneumoniae pneumonia and respiratory syncytial virus infection in Japan during the severe acute respiratory syndrome coronavirus 2 pandemic. Respiratory Invest. 2021;59:5–7.
Meyer Sauteur PM, Beeton ML, Uldum SA, Bossuyt N, Vermeulen M, Loens K, et al. Mycoplasma pneumoniae detections before and during the COVID-19 pandemic: results of a global survey, 2017 to 2021. Euro Surveill. 2022;27:2100746.
Sauteur PMM, Chalker VJ, Berger C, Nir Paz R, Beeton ML, Pereyre S, et al. Mycoplasma pneumoniae beyond the COVID-19 pandemic: where is it? Lancet Microbe. 2022;3:e897.
Principi N, Autore G, Ramundo G, Esposito S. Epidemiology of respiratory infections during the COVID-19 pandemic. Viruses. 2023;15:1160.
Burrell R, Saravanos G, Britton PN. Unintended impacts of COVID-19 on the epidemiology and burden of paediatric respiratory infections. Paediatric Respiratory Reviews. 2023:S1526-0542(23)00044–1.
Bardsley M, Morbey RA, Hughes HE, Beck CR, Watson CH, Zhao H, et al. Epidemiology of respiratory syncytial virus in children younger than 5 years in England during the COVID-19 pandemic, measured by laboratory, clinical, and syndromic surveillance: a retrospective observational study. Lancet Infect Dis. 2023;23:56–66.
Eden JS, Sikazwe C, Xie R, Deng YM, Sullivan SG, Michie A, et al. Off-season RSV epidemics in Australia after easing of COVID-19 restrictions. Nat Commun. 2022;13:2884.
Cho SJ, Kim SH, Lee H, Lee YU, Mun J, Park S, et al. Re-emergence of HMPV in Gwangju, South Korea, after the COVID-19 pandemic. Pathogens. 2023;12:1218.
Foley DA, Sikazwe CT, Minney Smith CA, Ernst T, Moore HC, Nicol MP, et al. An unusual resurgence of human metapneumovirus in Western Australia following the reduction of non-pharmaceutical interventions to prevent SARS-CoV-2 transmission. Viruses. 2022;14:2135.
Meyer Sauteur PM, Beeton ML. Mycoplasma pneumoniae: delayed re-emergence after COVID-19 pandemic restrictions. Lancet Microbe. 2024;5:e100–1.
National Health Commission of the People’s Republic of China, State Administration of Traditional Chinese Medicine. Guideline for diagnosis and treatment of community-acquired pneumonia in children (2019 version). Chin J Clin Infect Dis. 2019;12:6–13.
De Blic J, Midulla F, Barbato A, Clement A, Dab I, Eber E, et al. Bronchoalveolar lavage in children. ERS Task Force on bronchoalveolar lavage in children. Eur Respiratory Soc Eur Respir J. 2000;15:217–31.
Deng Z, Li C, Wang Y, Wu F, Liang C, Deng W, et al. Targeted next-generation sequencing for pulmonary infection diagnosis in patients unsuitable for bronchoalveolar lavage. Front Med. 2023;10:1321515.
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The sequence alignment/map format and SAMtools. Bioinformatics. 2009;25:2078–9.
Wang H, Zheng Y, de Jonge MI, Wang R, Verhagen LM, Chen Y, et al. Lockdown measures during the COVID-19 pandemic strongly impacted the circulation of respiratory pathogens in Southern China. Sci Rep. 2022;12:16926.
Hirae K, Hoshina T, Koga H. Impact of the COVID-19 pandemic on the epidemiology of other communicable diseases in Japan. Int J Infect Dis. 2023;128:265–71.
Oster Y, Abu Ahmad W, Michael-Gayego A, Rivkin M, Levinzon L, Wolf D, et al. Viral and bacterial respiratory pathogens during the COVID-19 pandemic in Israel. Microorganisms. 2023;11:166.
Gong C, Huang F, Suo L, Guan X, Kang L, Xie H, et al. Increase of respiratory illnesses among children in Beijing, China, during the autumn and winter of 2023. Eurosurveillance. 2024;29:2300704.
Nordholm AC, Søborg B, Jokelainen P, Lauenborg Møller K, Flink Sørensen L, Grove Krause T, et al. Mycoplasma pneumoniae epidemic in Denmark, October to December, 2023. Euro Surveill. 2024;29:2300707.
Zhang XB, He W, Gui YH, Lu Q, Yin Y, Zhang JH et al. Current Mycoplasma pneumoniae epidemic among children in Shanghai: unusual pneumonia caused by usual pathogen. World J Pediatr. 2024;20:5–10.
Maison N, Omony J, Rinderknecht S, Kolberg L, Meyer-Bühn M, von Mutius E, et al. Old foes following news ways?-Pandemic-related changes in the epidemiology of viral respiratory tract infections. Infection. 2024;52:209–18.
Yusuf SO, Chen P. Clinical characteristics of community-acquired pneumonia in children caused by mycoplasma pneumoniae with or without myocardial damage: a single-center retrospective study. World J Clin Pediatr. 2023;12:115–24.
Zhou Y, Shan Y, Cui Y, Shi J, Wang F, Miao H, et al. Characteristics and outcome of severe Mycoplasma pneumoniae pneumonia admitted to PICU in Shanghai: a retrospective cohort study. Crit Care Explorations. 2021;3:e0366.
Pánisová E, Unger WWJ, Berger C, Meyer Sauteur PM. Mycoplasma pneumoniae-specific IFN-γ-producing CD4(+) effector-memory T cells correlate with pulmonary disease. Am J Respir Cell Mol Biol. 2021;64:143–6.
Liu B, Chang X, Yan N. Clinical analysis of the epidemiology and changes in inflammatory indexes of Mycoplasma pneumonia in acute and recovery stage pediatric patients. Translational Pediatr. 2022;11:1645–55.
Deng F, Cao H, Liang X, Li Q, Yang Y, Zhao Z, et al. Analysis of cytokine levels, cytological findings, and MP-DNA level in bronchoalveolar lavage fluid of children with Mycoplasma pneumoniae pneumonia. Immun Inflamm Dis. 2023;11:e849.
Jiang TT, Sun L, Wang TY, Qi H, Tang H, Wang YC, et al. The clinical significance of macrolide resistance in pediatric Mycoplasma pneumoniae infection during COVID-19 pandemic. Front Cell Infect Microbiol. 2023;12:131181402.
Ma Z, Zheng Y, Deng J, Ma X, Liu H. Characterization of macrolide resistance of Mycoplasma pneumoniae in children in Shenzhen, China. Pediatr Pulmonol. 2014;49:695–700.
Wang X, Li M, Luo M, Luo Q, Kang L, Xie H, et al. Mycoplasma pneumoniae triggers pneumonia epidemic in autumn and winter in Beijing: a multicentre, population-based epidemiological study between 2015 and 2020. Emerg Microbes Infections. 2022;11:1508–17.
Wu TH, Wang NM, Liu FC, Pan HH, Huang FL, Fang YP, et al. Macrolide resistance, clinical features, and Cytokine profiles in Taiwanese children with Mycoplasma pneumoniae infection. Open Forum Infect Dis. 2021;8:ofab416.
Lee E, Cho HJ, Hong SJ, Lee J, Sung H, Yu J. Prevalence and clinical manifestations of macrolide resistant Mycoplasma pneumoniae pneumonia in Korean children. Korean J Pediatr. 2017;60:151–7.
Acknowledgements
Not applicable.
Funding
This work was supported by the Guangzhou Science and Technology Project [grant numbers: 202201020484 and 2023A03J0357], the Plan on enhancing scientific research in GMU [grant number:2024SRP055] and the Sanming Project of Medicine in Shenzhen [grant number: SZSM202311002].
Author information
Authors and Affiliations
Contributions
Y.L., M.-Z.W., and Y.L. contributed equally to this manuscript. Q.-G. C., Y. L., and Y.-P.L. contributed to conceptualization, writing of the original draft, review and editing, and resources. Q.-G.C., Y.L., M.-Z.W., Y.L., Y.-H.Y., W.-Y.G., Y.-Z.D., T.W., C.-W.T., C.L., and F.-F.L. contributed to methodology, investigation, formal analysis, and data curation. Q.-G. C. contributed to project administration. All authors have reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University. The approval date is 16/09/2022, and the approval number is 2022121.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Y., Wu, M., Liang, Y. et al. Mycoplasma pneumoniae infection outbreak in Guangzhou, China after COVID-19 pandemic. Virol J 21, 183 (2024). https://doi.org/10.1186/s12985-024-02458-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-024-02458-z