Abstract
Background
Nonpharmaceutical interventions (NPIs) implemented to reduce the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have suppressed the spread of other respiratory viruses during the coronavirus disease 2019 (COVID-19) pandemic. This study aimed to explore the epidemiological trends and clinical characteristics of Mycoplasma pneumoniae (MP) infection among inpatient children with lower respiratory tract infection (LRTI) before and during the COVID-19 pandemic, and investigate the long-term effects of China’s NPIs against COVID-19 on the epidemiology of MP among inpatient children with LRTI.
Methods
Children hospitalised for LRTI at the Department of Pulmonology, The Children’s Hospital, Zhejiang University School of Medicine (Hangzhou, China) between January 2019 and December 2022 were tested for common respiratory pathogens, including Mycoplasma pneumoniae (MP), Chlamydia trachomatis (CT) and other bacteria. Clinical data on age, sex, season of onset, disease spectrum, and combined infection in children with MP-induced LRTI in the past 4 years were collected and analysed.
Results
Overall, 15909 patients were enrolled, and MP-positive cases were 1971 (34.0%), 73 (2.4%), 176 (5.8%), and 952 (20.6%) in 2019, 2020, 2021, and 2022, respectively, with a significant statistical difference in the MP-positive rate over the 4 years (p <0.001). The median age of these children was preschool age (3–6 years), except for 2022, when they were school age (7–12 years), with statistical differences. Comparing the positive rates of different age groups, the school-age children (7–12 years) had the highest positive rate, followed by the preschoolers (3–6 years) in each of the 4 years. Compared among different seasons, the positive rate of MP in children with LRTI was higher in summer and autumn, whereas in 2020, it was highest in spring. The monthly positive rate peaked in July 2019, remained low from 2020 to 2021, and rebounded until 2022. Regarding the disease spectrum, severe pneumonia accounted for the highest proportion (46.3%) pre-pandemic and lowest (0%) in 2020.
Conclusion
Trends in MP detection in children with LRTIs suggest a possible correlation between COVID-19 NPIs and significantly reduced detection rates. The positivity rate of MP gradually rose after 2 years. The epidemic season showed some differences, but school-age children were more susceptible to MP before and during the COVID-19 pandemic.
Similar content being viewed by others
Background
Mycoplasma pneumoniae (MP) can be transmitted via respiratory droplets, causing respiratory tract infections [1]. It stands as one of the most prevalent pathogens causing respiratory diseases in children, accounting for up to 40% of community-acquired pneumonia cases in the paediatric population [2]. This percentage tends to increase during epidemics. While MP infections are generally self-limiting, they can lead to refractory pneumonia and extrapulmonary injury, resulting in severe complications and even death. The MP epidemic has had a serious impact on children, society, and medical resources. The periodic occurrence of MP epidemic, with intervals of 3–7 years and durations of up to 2 years, has been observed. It was estimated that 2019–2020 would be another year of MP epidemic [3]. The coronavirus disease 2019 (COVID-19) pandemic has significantly altered the epidemiology of other viral respiratory infections [4, 5]. Investigating the impact of the COVID-19 pandemic on the prevalence of MP is crucial.
During the COVID-19 pandemic, non-pharmaceutical interventions (NPIs) were proposed to mitigate the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [6]. Since the onset of the pandemic, the Chinese government had implemented extensive and strict NPIs, including mask-wearing, social distancing, home-based work, and school closures. In the first half of 2020, most cities in China, including Hangzhou in Zhejiang Province, enforced strict NPIs. Hangzhou, being the first province to initiate a “first-level emergency plan” on 23 January, responded with a comprehensive set of measures for a significant public health emergency. These measures included working from home, closing public cultural or entertainment places, and implementing work from home policies until gradual reopening of classes at the end of April. From then until the end of December 2022, “relaxed NPIs”, including mask-wearing and physical-distancing, were mandated in public areas. If SARS-CoV-2 positive cases were reported during this period, the specific location was considered high-risk, triggering the enforcement of strict NPIs. Temporary suppression of influenza epidemics and other viral respiratory diseases, including the respiratory syncytial virus (RSV), has been associated with the global implementation of NPIs [7,8,9]. The three-year comprehensive control measures implemented in China differ significantly from those in other countries, warranting a study on their impact on the epidemic trend of respiratory pathogens.
Recent studies have focused on MP trends before and during the pandemic in China [10, 11]; however, these results were obtained using pre-pandemic data, and lacked data from the later stages of the epidemic. In the present study, we conducted a retrospective epidemiologic analysis of MP prevalence during the last four years to explore the characteristics of inpatient children with MP in Hangzhou, and to investigate the effect of the COVID-19 pandemic on the prevalence of MP.
Methods
Study design
Data were retrospectively analysed for paediatric in-patients between 1 month and 18 years of age with LRTI who were admitted to the respiratory ward of the Children’s Hospital of Zhejiang University School of Medicine between 1 January 2019 and 31 December 2022. All children were diagnosed with LRTI, manifesting fever and/or lower respiratory tract symptoms, such as tachypnoea, non-productive cough, wheezing, and increased breath sounds. Additionally, each in-patient exhibited at least one of the following conditions indicative of LRTI: rales or wheezes, or chest imaging findings, encompassing diagnoses such as pneumonia, bronchitis, bronchiolitis, and prolonged pneumonia. Respiratory pathogens were analysed in all enrolled patients. Furthermore, the prevalence trends of other pathogens, including RSV [12], were analysed using similar methods. The clinical data of MP-positive children, including age, sex, length of stay (LOS), seasonal distribution, co-infecting pathogens, and diagnosis, were comprehensively analysed to evaluate the impact of the pandemic. A comparison of data for four consecutive years from 2019 to 2022 reflected the epidemiological trend of MP detection after the COVID-19 outbreak.
Measurement
Respiratory specimens (pharyngeal swabs or nasopharyngeal aspirates) were collected from the enrolled in-patients with LRTI by trained staff in accordance with the standard operating procedures. All specimens were tested by direct immunofluorescence (DIF) test for RSV, influenza virus A (Flu A), influenza virus B (Flu B), adenovirus (ADV), para-influenza virus 1 (PIV-1), para-influenza virus 2 (PIV-2), para-influenza virus 3 (PIV-3). MP and Chlamydia trachomatis (CT) were tested for by polymerase chain reaction (PCR), and cultures were grown to detect bacteria. If MP was detected, the patient was enrolled for further analysis. Co-infection was evaluated according to the test results for other pathogens.
Data processing and statistical analyses
Categorical variables were expressed as ratios or numbers (%). The age and LOS of the patients were expressed as medians and interquartile ranges (IQR) as they were not normally distributed. χ2 and rank-sum tests were used when comparing respective groups. A p value below 0.05 was considered statistically significant. All data were analysed using the SPSS software package (version 24.0, IBM, Armonk, NY, USA).
Results
Patient characteristics
Between January 2019 and December 2022, 15909 children were admitted to the pulmonary department due to LRTI: 5271 cases in 2019, 3006 cases in 2020, 3013 cases in 2021, and 4619 cases in 2022. Among all the enrolled patients, MP-positive cases and proportions were 1791 (34.0%), 73 (2.4%), 176 (5.8%), and 952 (20.6 %) in 2019, 2020, 2021, and 2022, respectively, with a significant statistical difference in the MP-positive rate over the 4 years (p <0.001) and between every 2 years. The monthly positive rate of children with MP and LRTI peaked in July 2019 (61.7%), while the highest monthly positive rate annually from 2020 to 2022 was in April (9.2%), August (16.9%), and November (31.4%), respectively. The characteristics of LRTI with MP detection between 2019 and 2022 are shown in Table 1. No significant difference was observed in the sex ratio of MP detected over 4 years (p = 0.488). The median age of patients in the preschool or school-age group was 55, 61, 54, and 84 months in 2019, 2020, 2021, and 2022, respectively, and the median age in 2022 was higher than that in the other 3 years (p <0.001). The median LOS in 2022 (5 d) was shorter than that in the other 3 years (p <0.001). Co-detection proportion in 4 years was 10.2–16.4%, with no statistical difference (p = 0.219). Regarding the disease spectrum, all children with LRTI and MP were classified as having acute pneumonia or acute bronchopneumonia, acute bronchitis, prolonged pneumonia, bronchiolitis, and severe pneumonia. Within 4 years, a statistically significant difference was observed in the distribution of each disease (p <0.001). In 2019, pre-COVID-19 pandemic, the proportion of severe pneumonia was the highest, with statistical differences compared to the other 3 years, and lowest in 2020, which was also statistically different from the other 3 years. The number of cases of co-detection with other pathogens was 282 (15.7%), 15 (20.5%), 18 (10.2%), and 87 (8.9%) in 2019, 2020, 2021, and 2022, respectively, with a statistically significant difference (p <0.001). Statistical analysis was performed to determine whether MP-positive cases were combined with the other seven respiratory viruses and CT and whether the bacterial culture was positive. The proportion of co-detections with other pathogens in 2019 and 2020 was relatively high, whereas that in 2022 was relatively low. Post hoc analysis revealed statistically significant differences between 2019 and 2022, 2020 and 2021, and 2020 and 2022. Among the co-infecting pathogens, ADV accounted for the most significant proportion in 2019 and 2022, whereas RSV and bacteria were most common in 2020 and 2021, respectively.
Age stratification
The patients were divided into four groups according to age: infants (1–2 years), pre-schoolers (3–6 years), school-aged children (7–12 years), and adolescents (13–18 years). The MP positive rates and the number of MP positive cases in different age groups from 2019 to 2022 are shown in Table 2 and Fig. 1. The positive rates of the various groups showed that school-age children had the highest positive rate annually, followed by the preschoolers. Except in 2020, MP was not detected in adolescents, and the lowest MP-positive rate was observed in infants in the other 3 years. The positive rates of the different age groups annually and those of various years in each age group were significantly different (p <0.001).
Seasonal distribution
Patients were categorized into four admission periods based on their admission dates: Winter, Spring, Summer, and Autumn. Winter was defined as December to February, spring as March to May, summer as June to August, and autumn as September to November. The positivity rates of MP stratified by season in children with LRTI are shown in Table 3 and Fig. 2. Comparison of the MP-positive rates of different seasons in 4 years revealed a statistically significant difference (p <0.001). The incidence was highest in summer, followed by autumn in 2019 and 2021, while it was highest in spring at the beginning of the COVID-19 pandemic in 2020, and in 2022, the incidence was highest in autumn, followed by summer, with statistical differences compared with the distribution in 2019, the year prior to the pandemic.
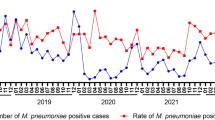
Based on the monthly distribution of MP-positive cases over 4 years, the number of cases gradually increased from the beginning of 2019, peaked in August, remained high during the summer, then gradually decreased, and remained low from 2020 to 2021. By 2022, the number of cases will rebound and peak by the end of 2022. This epidemiological trend of MP can also be seen in the monthly positive rate over the 4 years (Fig. 3).
Discussion
This study investigated the clinical features and epidemiological trends of MP infections before and during the COVID-19 pandemic. Additionally, the analysis of 4-year clinical data showed an epidemiological trend under various preventive and control measures. Epidemic prevention strategies vary across nations and areas and may affect MP prevalence differently. Our findings indicated the impact of these strategies on MP prevalence in Southeast China. Mitigating the transmission of SARS-CoV-2 requires drastic adjustments to population-level community behaviour, affecting the spread of endemic respiratory diseases [13]. Both stringent and relaxed NPIs may have reduced the spread of respiratory viruses, including SARS-CoV-2, RSV, and the influenza virus [13, 14]. However, studies have also indicated that viral respiratory infections have been common during the COVID-19 pandemic. For instance, our previous research revealed that RSV was the primary causative agent of LRTI during the pandemic, and variations in the trends of susceptible populations and epidemic seasons were observed before and during the pandemic [12].
Different pathogens transmitted via respiratory droplets may exhibit different trends in prevalence during the COVID-19 pandemic. As the primary causative pathogen of community-acquired pneumonia in children, MP remains a concern for pediatricians. This study aimed to understand the prevalence and clinical characteristics of hospitalized children with MP infection during the pandemic. This large sample study of 4 consecutive years summarizes the changes in the seasonal distribution of epidemics. It clarifies the demographic characteristics and disease severity in hospitalized children with MP-induced LRTI. Our study comprehensively investigated MP infection’s prevalence and clinical characteristics in children before and during the pandemic. It provided information for prevention and treatment strategies for the future mitigation of MP infection in children.
Our study found that among hospitalized children with LRTI, the detection rate of MP was highest in 2019, decreased to the lowest in 2020, and recovered to 20.6% by 2022, with statistical differences. This reflects the epidemiological trend of MP detection for four consecutive years before and during the COVID-19 pandemic. According to the seasonal and monthly MP-positivity rates, a peak was observed in the summer of 2019, similar to previous studies [10, 11]. Based on past trends, a recent MP outbreak was predicted to extend from the summer and fall of 2019 to the winter or spring of 2021 [15]. However, compared to 2019, the positive instances of MP in 2020 and 2021 were significantly lower. Our findings also indicated a significant decline in MP detection starting in February 2020, which was maintained at a low level with slight oscillations. The number of positive cases steadily increased until April 2022 and persisted until the conclusion of the investigation. Effective COVID-19 pandemic control strategies have the potential to significantly lower MP prevalence in closed or semi-closed populations, including hospitals, schools, religious centers, and military bases [16,17,18]. The significant decline in the MP-positivity rate observed in 2020 is consistent with previous research [19], and investigations conducted in Finland and Japan showed that MP prevalence was significantly lower in 2020 than in 2012 and 2016 [20, 21]. Stringent protocols to mitigate the spread of SARS-CoV-2 might have affected the spread of other respiratory viruses with similar transmission modes. NPIs such as obligatory facemasks, social isolation, stay-at-home orders, and hand hygiene were primary global initiatives. All these measures aided in reducing the spread of MP via droplets and contact with unclean hands and feet. Our research also found that although it was during the COVID-19 pandemic, MP-positive cases gradually increased until 2022. By the end of 2022, the number of positive instances exceeded the level of the same period in 2019. This may be related to the implementation of relaxed NPIs in Hangzhou in 2022, where children attend school and participate in activities normally; However, after 2 years of low infection proportion with MP, the population lacks immune protection and is generally susceptible to MP, resulting in a gradual increase in the number of positive cases.
From the perspective of age stratification, most positive cases were observed among preschool and school-aged children, consistent with the characteristics of MP infections in children [14]. Although the annual positivity rate varied greatly from the perspective of age distribution, the positivity rate of school-age children was the highest both before and during COVID-19. In 2022, the MP-positivity rate of school-aged children reached 54.3%, and the median age was higher than that of the other 3 years, indicating statistical differences. In 2022, the first year during the epidemic in which the infection rate of MP had gradually increased after a sustained low level of infection, most cases were among school-age children, suggesting that school-age children are more susceptible to MP infection in a population with a generally decreased immune protection against it. Compared with infants, the safety of school-aged children is easily neglected, rendering them more susceptible to MP infection. However, this requires further investigation.
Regarding disease spectrum and severity, acute pneumonia dominated, accounting for 50.2–68.5% of MP-positive cases; moreover, the proportion of severe pneumonia was high. Except for 2020, a year with a meagre MP detection rate, the proportion of severe pneumonia in other years was above 30%; suggesting that MP is an important pathogen of community-acquired pneumonia in children and an important pathogen that causes severe pneumonia in children. In our study, 8.9–20.5% of children were co-detected with other pathogens within 4 years. The co-detection rate was relatively low in 2021 and 2022, possibly related to the selection of pathogens detected in this study. Common respiratory viruses, such as rhinovirus, coronavirus, and metapneumovirus, were not detected. The co-detection rate was also related to the prevalence of other viruses. For instance, more mixed adenovirus infections in 2019 were associated with the prevalence of adenoviruses in 2019 [22].
Compared with previous studies [10, 15], the nucleic acid test was performed to investigate the MP-positivity rate in our research, which was more reliable than specific IgM antibodies for diagnosing MP infection, as the time and duration of antibody production may influence IgM antibody test results. In addition, our study period, which lasted from before the end of the pandemic, was meaningful for a comprehensive understanding of MP prevalence during the entire epidemic period. Our study has some limitations. First, in the first 2 years of the pandemic, especially in early 2020, when the NPIs were strictly implemented, the total number of cases of LRTI for admission was low, which may have been related to delays in patients’ visits to hospital emergency emergencies and face-to-face outpatient clinics, which may have created a selection bias. Second, this was a single-center study, and it would have been more convincing if the data had been obtained from different centers. In addition, our research should have covered the period after China implemented prevention and control measures for category A infectious diseases against SARS-CoV-2 infection. Therefore, it is not yet possible to determine MP prevalence after the end of the pandemic. Further research is required to determine whether MP prevalence will return to pre-COVID-19 levels by the end of the pandemic.
Conclusion
Through a study on MP prevalence during NPI enforcement during the COVID-19 pandemic, we compared the data before and during the epidemic for four consecutive years. We found that MP-positive cases sharply decreased at the beginning of the COVID-19 outbreak and gradually rebounded after 2 years, indicating a possible correlation between COVID-19 NPIs and significantly reduced detection numbers. By comparing the seasonal and age distribution of MP-positive rates, it was concluded that MP-positive cases gradually recovered after 2 years of NPI implementation or relaxed NPIs, and the epidemic season showed some differences, while school-age children were all more susceptible to MP both before and during the COVID-19 pandemic.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NPIs:
-
Non-pharmaceutical interventions
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- MP:
-
Mycoplasma pneumonia
- COVID-19:
-
The coronavirus disease 2019
- LRTI:
-
Lower respiratory tract infection
- CT:
-
Chlamydia trachomatis
- RSV:
-
Respiratory syncytial virus
- LOS:
-
Length of stay
- DIF:
-
Direct immunofluorescence
- Flu A:
-
Influenza virus A
- Flu B:
-
Influenza virus B
- ADV:
-
Adenovirus
- PIV-1:
-
Para-influenza virus 1
- PIV-2:
-
Para-influenza virus 2
- PIV-3:
-
Para-influenza virus 3
- PCR:
-
Polymerase chain reaction
- IQR:
-
Interquartile ranges
References
Waites KB, Xiao L, Liu Y, Balish MF, Atkinson TP. Mycoplasma pneumoniae from the Respiratory Tract and Beyond. Clin Microbiol Rev. 2017;30(3):747–809. https://doi.org/10.1128/CMR.00114-16.
Atkinson TP, Waites KB. Mycoplasma pneumoniae Infections in Childhood. Pediatr Infect Dis J. 2014;33(1):92–4. https://doi.org/10.1097/INF.0000000000000171.
Yan C, Sun H, Zhao H. Latest Surveillance Dataon Mycoplasma Pneumoniae Infections in Children, Suggesting a New Epidemic Occurring in Beijing. J Clin Microbiol. 2016;54(5):1400–1. https://doi.org/10.1128/JCM.00184-16.
Oster Y, Michael-Gayego A, Rivkin M, Levinson L, Wolf DG, Nir-Paz R. Decreased prevalence rate of respiratory pathogens in hospitalized patients during the COVID-19 pandemic: possible role for public health containment measures? Clin Microbiol Infect. 2021;27(5):811–2. https://doi.org/10.1016/j.cmi.2020.12.007.
Huang QS, Wood T, Jelley L, Jennings T, Jefferies S, Daniells K, et al. Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand. Nat Commun. 2021;12(1):1001. https://doi.org/10.1038/s41467-021-21157-9.
Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279-88. https://doi.org/10.1016/S2468-2667(20)30090-6.
Emborg HD, Carnahan A, Bragstad K, Trebbien R, Brytting M, Hungnes O, et al. Abrupt termination of the 2019/20 influenza season following preventive measures against COVID-19 in Denmark, Norway and Sweden. Euro Surveill. 2021;26(22):2001160. https://doi.org/10.2807/1560-7917.ES.2021.26.22.2001160.
Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children-A nationwide register study in Finland. EClinicalMedicine. 2021;34:100807. https://doi.org/10.1016/j.eclinm.2021.100807.
Wan WY, Thoon KC, Loo LH, Chan KS, Oon LLE, Ramasamy A, et al. Trends in respiratory virus infections during the COVID-19 pandemic in Singapore, 2020. JAMA Netw Open. 2021;4(6):e2115973. https://doi.org/10.1001/jamanetworkopen.2021.15973.
Cheng Y, Cheng YJ, Dai SH, Hou DQ, Ge ML, Zhang Y, et al. The Prevalence of Mycoplasma Pneumoniae Among Children in Beijing Before and During the COVID-19 Pandemic. Front Cell Infect Microbiol. 2022;12:854505. https://doi.org/10.3389/fcimb.2022.854505.
Zhang Y, Huang YJ, Ai T, Luo J, Liu HM. Effect of COVID-19 on childhood Mycoplasma pneumoniae infection in Chengdu, China. BMC Pediatr. 2021;21(1):202. https://doi.org/10.1186/s12887-021-02679-z.
Qiu WL, Zheng C, Huang SM, Zhang YY, Chen ZM. Epidemiological trend of RSV infection before and during COVID-19 pandemic: A three-year consecutive study in China. Infect Drug Resist. 2022;15:6829–37. https://doi.org/10.2147/IDR.S388231.
Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses. Euro Surveill. 2020;25(47):2001847. https://doi.org/10.2807/1560-7917.ES.2020.25.47.2001847.
Liu PC, Xu MH, Lu LJ, Cao LF, Su LY, Dong NN, et al. The changing pattern of common respiratory and enteric viruses among outpatient children in Shanghai, China: Two years of the COVID-19 pandemic. J Med Virol. 2022;94(10):4696–703. https://doi.org/10.1002/jmv.27896.
Cai FQ, Shou XY, Ye Q. Epidemiological study on Mycoplasma pneumoniae and Chlamydia pneumoniae infection of hospitalized children in a single center during the COVID-19 pandemic. Front Cell Infect Microbiol. 2022;12:843463. https://doi.org/10.3389/fcimb.2022.843463.
Suzuki Y, Seto J, Shimotai Y, Itagak T, Katsushima Y, Katsushima F, et al. Polyclonal spread of multiple Genotypes of Mycoplasma Pneumoniae in semi-closed settings in Yamagata Japan. J Med Microbiol. 2019;68(5):785–90. https://doi.org/10.1099/jmm.0.000969.
Zhang WZ, Zhang SJ, Wang QY, Li YD, Jing HB, Hu GY, et al. Outbreak of Macrolide-Resistant Mycoplasma Pneumoniae in a primary school in Beijing, China in 2018. BMC Infect Dis. 2019;19(1):871. https://doi.org/10.1186/s12879-019-4473-6.
Zhang X, Han MN, Dong JH, Li XX, Hu XY, Wang Z, et al. Outbreak of Mycoplasma Pneumoniae at a Military Academy. Mil Med Res. 2020;7(1):60. https://doi.org/10.1186/s40779-020-00289-x.
Meyer Sauteur PM, Beeton ML, Uldum SA, Bossuyt N, Vermeulen M, Loens K, et al. Mycoplasma pneumoniae detections before and during the COVID-19 pandemic: results of a global survey, 2017 to 2021. Euro Surveill. 2022;27(19):2100746. https://doi.org/10.2807/1560-7917.ES.2022.27.19.2100746.
Fujita J. Mycoplasma Pneumoniae Pneumonia and respiratory syncytial virus infection in Japan during the severe acute respiratory syndrome Coronavirus 2 Pandemic. Respir Investig. 2021;59(1):5–7. https://doi.org/10.1016/j.resinv.2020.11.002.
Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the Re-opening of schools and day Cares on the Epidemiology of SARS-CoV-2 and other respiratory infections in children - A nationwide register study in Finland. EClinicalMedicine. 2021;34:100807. https://doi.org/10.1016/j.eclinm.2021.100807.
Chen Y, Lin T, Wang CB, Liang WL, Lian GW, Zanin M, et al. Human adenovirus (HAdV) infection in children with acute respiratory tract infections in Guangzhou, China, 2010–2021: a molecular epidemiology study. World J Pediatr. 2022;18(8):545–52. https://doi.org/10.1007/s12519-022-00590-w.
Acknowledgements
The authors thank the National Clinical Research Center for Child Health and the Natural Science Foundation of Zhejiang province for sponsoring the study, and the participating children and their parents. The funding body had no role in the design of the study, or the collection, analysis, and interpretation of data, or in writing the manuscript.
Funding
This work was supported by the grant from the Key Program of the Independent Design Project of National Clinical Research Center for Child Health (G20B0003) , and the grant from the Natural Science Foundation of Zhejiang province (LY22H100007).
Author information
Authors and Affiliations
Contributions
WQ, YZ, and ZC conceived and designed the study. WQ, HZ, SH, ZH, ML collected the clinical information, and analyzed the data. WQ, JD drafted the article and YZ, ZC revised it critically for important. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Children’s Hospital, Zhejiang University School of Medicine in accordance with the Declaration of Helsinki (2021-IRB-325).It was a retrospective study, and all the patients’ data were anonymously reported in this study. Based on the guidelines of the Ethics Committee of the Capital Institute of Pediatrics, informed consent was not sought from patients. The need for written informed consent was waived by the Ethics Committee of Children’s Hospital, Zhejiang University School of Medicine due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qiu, W., Ding, J., Zhang, H. et al. Mycoplasma pneumoniae detections in children with lower respiratory infection before and during the COVID-19 pandemic: a large sample study in China from 2019 to 2022. BMC Infect Dis 24, 549 (2024). https://doi.org/10.1186/s12879-024-09438-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09438-2