Abstract
Nicotinamide adenine dinucleotide (NAD+), a crucial coenzyme in cellular redox reactions, is closely associated with age-related functional degeneration and metabolic diseases. NAD exerts direct and indirect influences on many crucial cellular functions, including metabolic pathways, DNA repair, chromatin remodeling, cellular senescence, and immune cell functionality. These cellular processes and functions are essential for maintaining tissue and metabolic homeostasis, as well as healthy aging. Causality has been elucidated between a decline in NAD levels and multiple age-related diseases, which has been confirmed by various strategies aimed at increasing NAD levels in the preclinical setting. Ovarian aging is recognized as a natural process characterized by a decline in follicle number and function, resulting in decreased estrogen production and menopause. In this regard, it is necessary to address the many factors involved in this complicated procedure, which could improve fertility in women of advanced maternal age. Concerning the decrease in NAD+ levels as ovarian aging progresses, promising and exciting results are presented for strategies using NAD+ precursors to promote NAD+ biosynthesis, which could substantially improve oocyte quality and alleviate ovarian aging. Hence, to acquire further insights into NAD+ metabolism and biology, this review aims to probe the factors affecting ovarian aging, the characteristics of NAD+ precursors, and the current research status of NAD+ supplementation in ovarian aging. Specifically, by gaining a comprehensive understanding of these aspects, we are optimistic about the prominent progress that will be made in both research and therapy related to ovarian aging.
Similar content being viewed by others
Introduction
Ongoing advancements in NAD+ biology research continue to elucidate the mechanisms underlying age-related diseases. NAD+ , the reduced form of NAD, is an omnipresent coenzyme found in all human cells. It plays a crucial role in maintaining energy and redox homeostasis, regulating a vast network of systems across diverse cellular compartments and tissues [1,2,3]. In addition to its role in energy metabolism, NAD+ is recognized as a crucial signaling molecule and serves as the limiting substrate for numerous enzymes involved in DNA repair, epigenetic regulation, posttranslational modification, and metabolic adaptation [4]. The decline in NAD+ levels with aging has been thoroughly documented [5], and supplementation with NAD+ precursors have been shown to have the potential to elevate NAD+ levels, both in vitro and in vivo, serving as a promising strategy to combat age-related dysfunction and disease.
The association between NAD+ levels and health was initially established nearly a century ago by Elvehjem and his colleagues. In 1937, they discovered that pellagra resulted from a dietary insufficiency of niacin, resulting in reduced NAD+ levels [6]. Subsequent studies have demonstrated the correlation between low NAD+ levels and various disease conditions, such as metabolic disorders, neurodegenerative diseases, and aging [7,8,9,10]. Consequently, there is considerable interest in comprehending the influence of NAD+ metabolism on the initiation of diseases, particularly age-related conditions. In recent times, the restoration of NAD+ levels through the supplementation of NAD+ precursors has emerged as a promising therapeutic approach for age-related diseases [11,12,13], as evidenced by the beneficial effects observed in rodent models.
Ovarian aging, characterized by a decrease in both the quantity and quality of oocytes, along with an overall reduction in ovarian activity [14,15,16], poses a significant challenge to female reproductive health. Despite ongoing efforts, the molecular mechanisms responsible for ovarian aging and longevity remain largely unexplored, and the correlation between various factors and ovarian health necessitates further investigation. At birth, women have approximately 2 million oocytes, which diminish to a mere 1000 primordial follicles by menopause [17]. Delaying parenthood can lead to fertility issues for women of advanced maternal age, as their diminished ovarian reserve is linked to higher rates of aneuploidy and suboptimal outcomes in embryonic development and maturation following both natural conception and assisted reproductive technology [18, 19]. Recently, there has been a rapid increase in studies exploring various aspects of ovarian aging, including stress, genetics, diseases, dietary habits, and lifestyle. Obtaining a comprehensive understanding of these factors and their mechanisms is crucial for extending reproductive longevity and enhancing women’s health.
Strategies focused on decelerating ovarian aging and enhancing the quality and quantity of oocytes have made significant progress in recent decades [20,21,22]. Given that mitochondrial dysfunction and oxidative stress are pivotal factors in ovarian aging, the identification of drugs capable of mitigating ovarian disorders can play a crucial role in combating ovarian aging. These drugs can function as antioxidants or as molecules that modulate cellular signaling pathways to safeguard ovarian cells against oxidative stress. Examples of antioxidants include melatonin [23,24,25,26], coenzyme Q10 [27,28,29,30], folic acid [31], resveratrol [32, 33], and vitamins C and E [34, 35]. Although growth hormone (GH) is not classified as an antioxidant, it has the ability to impact the cellular-level oxidative stress signaling pathway [36, 37]. Employing small molecules or procedures involving mitochondrial transfer/replacement to enhance mitochondrial function has exhibited effectiveness in reducing oxidative damage to the ovaries [38].
In recent years, NAD has emerged as a promising regulator in mitigating age-related functional decline and diseases. In addition to improving mitochondrial function, this molecule enhances various other cellular processes and functions associated with antiaging effects. Encouragingly, certain studies have shown the potential of NAD precursors as a method of supplementing the body’s NAD levels. Moreover, the relationship between NAD+ levels and ovarian aging has gradually become clearer, with studies indicating that strategies to boost NAD+ can effectively alleviate ovarian aging, improve oocyte quality, and enhance fertility. Nevertheless, the specific mechanisms responsible for these effects remain unclear and necessitate further investigation and clarification [8, 39, 40]. This review offers a comprehensive overview of the current understanding of NAD+ biology and metabolism, the factors affecting ovarian aging, the NAD+ precursors, and the therapeutic potential of NAD+ boosting in countering ovarian aging.
Factors affecting ovarian aging
Mitochondrial dysfunction and oxidative stress
The mitochondrion is a pivotal organelle in oocytes, playing a critical role in energy production and determining cell fate [41,42,43,44]. Being a semiautonomous structure with its DNA, the harmonious interaction between the nuclear and mitochondrial DNA is crucial for the proper functioning of the mitochondrion [45]. Impaired mitochondria, characterized by the accumulation of mtDNA mutations, reduced oxidative phosphorylation (OXPHOS) activity, increased oxidative damage, altered mitochondrial quality control, decreased biogenesis and clearance efficiency, and disrupted mitochondrial dynamics, have been linked to ovarian aging [46,47,48,49] (Fig. 1).
According to the free radical theory, oxidative stress, resulting from elevated levels of intracellular reactive oxygen species (ROS), is a crucial factor contributing to mammalian cell senescence, including female reproductive aging [50,51,52,53]. ROS encompass both free and nonfree radicals, primarily generated as byproducts during the metabolic processes of eukaryotes [54]. Moderate levels of ROS are known to be involved in cell signaling and can promote cell survival, proliferation, and differentiation [55, 56]. However, when ROS levels surpass a cell’s oxidation resistance and repair capabilities, they induce oxidative stress, causing direct oxidative damage to biological molecules in the cell environment and leading to aging and disease development [57, 58]. Due to the positive correlation between the levels of ROS in the ovary and a woman’s age [59,60,61], human oocytes, which remain dormant in the ovary for decades, are particularly vulnerable to oxidative stress. Endogenous antioxidants, such as superoxide dismutase and catalase, present in the ovarian environment are crucial for ROS clearance. However, their levels decrease with age, weakening the ovary’s ability to remove ROS [62,63,64,65]. A recent study using single-cell transcriptomics in nonhuman primates suggested that oxidative damage is a critical factor contributing to the age-related decline in ovarian function [66]. ROS accumulation in the ovary reduces communication between oocytes and GCs, triggering GC apoptosis [67,68,69], accelerating corpus luteum degeneration [70, 71], hindering oocyte maturation before ovulation [72, 73], and ultimately leading to ovarian aging. The well-established correlation between telomere length in CCs and oocyte and embryo quality [74] highlights that ovarian oxidative stress can cause telomere shortening [75, 76]. NAD plays a critical role in cellular redox reactions, and the decrease in NAD content is closely associated with mitochondrial dysfunction and the generation of oxidative damage.
mtDNA disorders
Mitochondria play a critical role in synthesizing the energy-rich molecule adenosine triphosphate (ATP) through OXPHOS, providing energy to sustain cell activities [42, 77]. Electron leakage from the mitochondrial respiratory chain is a significant cause of intracellular ROS production. This susceptibility arises from the absence of protective histones or DNA-binding proteins in mtDNA, which is located within mitochondria, making it prone to ROS-induced damage [78,79,80]. ROS generation and mtDNA damage are closely intertwined, with the former often overlapping with the latter. As a consequence of ROS generation, mitochondrial fission, and mtDNA damage increase, primarily affecting the stromal side of the inner mitochondrial membrane [81, 82]. The gradual impairment in respiratory chain function resulting from mtDNA damage and mutations leads to an exponential increase in oxidative stress, especially with age. Female mice experience a shortened lifespan and exacerbated ovarian senescence due to the accumulation of mtDNA mutations in the germline [83, 84] (Fig. 1). Furthermore, younger women exhibit a higher mtDNA copy count per oocyte than that of elderly women, indicating reduced mtDNA in the ovary during aging [85]. Studies have demonstrated that autologous or allogeneic mitochondrial transplantation improves oocyte quality and in vitro fertilization outcomes in both human and other animal species [86, 87].
Epigenetic changes
Epigenetic modifications are linked to the decline in oocyte quality with ovarian aging [88] (Fig. 1). The expression of DNA methyltransferases and histone acetyltransferases, which impact epigenetic modification in oocytes, changes with age [89, 90]. For instance, decreased expression levels of DNA methyltransferases in 35- to 40-week-old mouse oocytes and preimplantation embryos result in low DNA methylation levels [91]. Additionally, aging affects histone methylation in mouse germinal vesicle oocytes [92], while older women exhibit a lack of certain histone marks compared to those of younger women. The transcription of histone deacetylase is downregulated in aging mouse oocytes, while histones remain acetylated in 10-month-old female mouse oocytes [93]. This finding suggests that histone modification in aging oocytes before ovulation may be impacted, potentially leading to embryonic death during development. The mRNA expression profile of human second meiotic division oocytes is related to aging and has a greater negative impact on histone acetylation as the mother ages (van den [94]. There is growing evidence that microRNAs play a crucial role in regulating oocyte DNA methylation and follicle development across various species [95,96,97,98]. Disruptions in microRNA expression also contribute to the development of ovarian aging [99, 100]. Decreased cellular NAD levels lead to impaired function of NAD-dependent and NAD-consuming enzymes involved in DNA repair and genome integrity, potentially contributing to aging-related DNA mutations and epigenetic changes.
Apoptosis
The ovary is a complex and heterogeneous organ composed of diverse cell types, with cumulus cells (CCs), playing a crucial role in the aging process. CCs, derived from granulosa cells (GCs), have been implicated in age-related elevations in oocyte apoptosis [101,102,103] (Fig. 1). The soluble molecules produced by CCs can adversely affect aging oocytes, leading to the acceleration of oocyte aging and impaired oocyte development and maturation potential [104, 105]. In vitro animal studies have demonstrated that coculture with CCs can improve oocyte maturation [106], while oocytes from older females have a marked decrease in the survival rate compared to that of oocytes from younger mice [107]. Studies in human patients have also revealed that GCs from young patients exhibit significantly lower levels of apoptosis than those from aged patients [108]. Moreover, animal experiments have shown that increased apoptosis levels in GCs result in a sharp decline in ovulation and fertility [109]. B-cell lymphoma-2 (BCL2), a key antiapoptotic factor, was found to be significantly upregulated in mature oocytes compared to immature oocytes, further reinforcing the role of CCs in accelerating the apoptosis in oocytes and aging of the ovary [110]. Recent research suggests that apoptosis and autophagy in aging cells contribute to the decline in NAD levels in the organism [111, 112].
Inflammation
Recent research highlights inflammation as a hallmark of ovarian aging [113, 114] (Fig. 1). Inflammatory aging refers to a chronic, low-grade proinflammatory state that accompanies aging and impacts various aspects of ovarian aging, such as oocyte maturation [115, 116], ovulation [117, 118], implantation [119], and delivery [120]. Animal studies have revealed an increase in gene expression related to chronic inflammation with age [121,122,123]. During the aging process, researchers have observed an increase in the populations of CD4 + cells, B cells, and macrophages in the ovary, as well as serum concentrations and intraovarian mRNA levels of specific proinflammatory cytokines such as IL-1α/β, IL-6, and TNF-α and inflammasome genes such as ASC and NLRP3 [113]. Activation of the NLRP3 inflammasome is linked to age-related inflammation and dysfunction in various organs. Studies knocking out the NLRP3 and ASC genes showed a decrease in intraovarian proinflammatory cytokine expression and a significant increase in follicle numbers, indicating that inflammation contributes to the age-related decline in ovarian reserve and that anti-inflammation may prevent ovarian insufficiency [124,125,126]. Recent studies suggest that therapeutic approaches aimed at elevating cellular NAD levels during the aging process can effectively reduce inflammation and the burden of senescent cells [127].
Telomeres length and telomerase activity
Telomeres are dynamic nucleoprotein-DNA structures located at the ends of eukaryotic chromosomes, crucial for maintaining genome integrity and chromosomal stability [128, 129]. Their length gradually shortens with each cell division. Telomerase is a reverse transcriptase enzyme that assists in elongating the highly repetitive DNA sequences of telomeres [130]. Studies have revealed that excessive telomere shortening contributes to cellular aging and is closely associated with reproductive lifespan and overall life expectancy [131, 132]. Research has found that in leukocytes of postmenopausal women, telomeres are shorter compared to age-matched women still experiencing menstruation. Additionally, women with longer telomeres tend to enter menopause at a later stage, indicating that telomere length serves as a significant marker of reproductive aging [133]. Investigations into human granulosa cells have linked telomere shortening and reduced or absent telomerase activity to latent ovarian insufficiency and primary ovarian insufficiency [134, 135].
Further research in assisted reproductive technology has shown that immature oocytes have significantly reduced telomere length compared to mature oocytes [136]. The length of telomeres in follicular cells exhibits a positive correlation with oocyte and embryo quality, and decreased telomere length may be associated with oocyte and early embryo aneuploidy [74, 137]. Oxidative stress is considered a major cause of telomere shortening [75]. With age, the levels of reactive oxygen species (ROS) increase in aging ovaries, making them more susceptible to telomeric oxidative damage and leading to a decline in oocyte developmental competence. The use of antioxidants can inhibit telomere shortening, fusion, DNA damage, and chromosomal instability in oocytes, thereby alleviating ROS-mediated damage and maintaining the quality of aging oocytes and follicles [138, 139].
NAD+ biology and metabolism
An introduction to NAD+
NAD+ was first discovered in 1906 by Harden and Young as a low-molecular-weight substance that accelerates the fermentation of yeast extracts [140]. In 1930, its chemical composition was reported to be an adenine, a phosphate, and reducing sugar groups [141]. NAD+ was discovered in 1936 to possess the capability of hydride transfer between molecules, rendering it a crucial coenzyme in redox reactions and an indispensable constituent of the energy metabolism of all organisms [142]. NAD+ plays a regulatory role in the activity of dehydrogenases engaged in diverse catabolic pathways, including glycolysis, glutamine degradation, and fatty acid oxidation. Apart from its involvement in energy metabolism, NAD+ acts as a cofactor for nonredox NAD+ -dependent enzymes, including sirtuins, CD38, SARM1, poly(ADP-ribose) polymerases (PARPs), ADP-ribosyltransferases (ARTs), and RNA polymerases [143]. These enzymes are crucial in maintaining intracellular homeostasis [112, 144, 145]. Reactions utilizing NAD+ as a substrate or cofactor generate nicotinamide (NMA) as a byproduct, which is significant to numerous metabolic pathways and cellular processes. Extensive studies have revealed the intricate and dynamic nature of NAD+ metabolism, transport, and function, rendering it an area of continuous research [146,147,148]. NAD+ compartmentalization within cells is a complex phenomenon involving three primary NAD+ subcellular pools in the cytoplasm, mitochondria, and nucleus (Fig. 2). The exchangeability of NAD+ between the cytosolic and nuclear pools is well established, with these two pools consistently exhibiting comparable NAD+ concentrations [149,150,151]. However, the interchangeability of the mitochondrial NAD+ pool with the nucleocytosolic NAD+ pool remains a topic of debate in the scientific community. Evidence from yeast suggests the presence of mitochondrial NAD+ transporters [152], while studies in mammals indicate that mitochondria can take up NAD+ precursors and intact NAD(H) [153,154,155]. These findings imply that mitochondrial NAD+ pools can indeed exchange with other NAD+ pools. The proportion and regulation of these NAD+ pools can vary greatly depending on the organelle, tissue, cell type, and individual’s age, with enzymes related to NAD+ biosynthesis and degradation being highly compartmentalized and independently regulated [2, 149, 156].
Overview of NAD+ metabolism pathway. NA: nicotinic acid, NAM: nicotinamide, QA: quinolinic acid, NMN: nicotinamide mononucleotide, NR: nicotinamide riboside, IDO, indoleamine 2,3-dioxygenase, TDO, tryptophan 2,3-dioxygenase, KMO, 3-hydroxykynurenine (3-HK) by kynurenine 3-monooxygenase, KYNU, tryptophan 2,3-dioxygenase, 3HAO. 3-hydroxyanthranilic acid oxygenase, ETC, NAMN: nicotinic acid mononucleotide, NAD: Nicotinamide adenine dinucleotide, NADH: reduced form of NAD, NADP: Nicotinamide adenine dinucleotide phosphate, NADPH: reduced form of NADP, NAAD: nicotinic acid adenine dinucleotide, NAMPT: nicotinamide phosphoribosyltransferase, NMNAT: nicotinamide mononucleotide adenylyltransferase, QPRT: quinolinic acid phosphoribosyltransferase, NaPRT: nicotinic acid phosphoribosyltransferase, Nrk: nicotinamide riboside kinase, NADS: NAD synthase, PARP: poly (ADP-ribose) polymerase, TCA, tricarboxylic acid, ETC, electron transport chain
Synthesis of NAD+
In mammals, with neurons being the exception, NAD+ cannot be imported into cells [157]. Thus, NAD+ synthesis occurs through either the de novo pathway using tryptophan or the Preiss-Handler pathway involving vitamin B3 derivatives such as nicotinic acid (NA) (Fig. 2). The enzyme responsible for de novo NAD synthesis is predominantly expressed in the liver and kidney [158,159,160,161]. De novo synthesis is also called the kynurenine pathway, which begins with complex reactions converting tryptophan into quinolinic acid (QA) and then producing nicotinic acid mononucleotide (NAMN) from QA and 5-phosphoribosyl-1-pyrophosphate (PRPP) via the catalytic action of quinolinic acid phosphoribosyltransferase (QaPRT) [162]. NAMN can also be synthesized via the Preiss-Handler pathway, which utilizes vitamin B3 [163]. This molecule is converted into nicotinic acid adenine dinucleotide (NAAD) by nicotinamide mononucleotide adenylyl transferase (NMNAT). Subsequently, NAD+ synthase deamidates NAAD, leading to the formation of NAD+ [164].
To maintain intracellular NAD+ levels, the salvage pathway is the primary source of newly synthesized NAD+ , utilizing nicotinamide (NAM), nicotinamide riboside (NR), and nicotinamide mononucleotide (NMN). NAM can be obtained from food or produced by NAD+ -consuming enzymes [165]. It undergoes two reactions: first, NAM is catalytically converted into NMN via the catalytic action of nicotinamide phosphoribosyltransferase (NAMPT) and PRPP [166]. Then, NMN is converted into NAD+ by conjugating the adenylyl moiety of ATP, catalyzed by NMNAT [167]. NAMPT is widely distributed in all NAD+ -related cellular compartments and exhibits dynamic levels [168, 169]. This enables it to regulate the body’s response to nutritional status, stress, exercise, and circadian rhythm, all of which are relevant to the functions of NAD+ [170,171,172]. Therefore, NAM is widely regarded as a common NAD+ precursor in cells. Mammalian cells possess three NMNAT isoenzymes localized in different subcellular locations: NMNAT1 in the nucleus [173, 174], NMNAT2 in the cytoplasm and Golgi apparatus [167], and NMNAT3 in mitochondria [169, 175]. Conversely, NR is phosphorylated into NMN through nicotinamide riboside kinase (Nrk) phosphorylation before undergoing conversion into NAD+ by NAMPT [176].
Degradation of NAD+
The sirtuin enzyme family is critical in regulating a wide range of biological processes, including metabolism, stress, circadian rhythm, and aging [177, 178]. These enzymes function as NAD+ -dependent deacetylases, utilizing NAD+ as a cosubstrate to remove acyl groups from their substrates and generating 2-O-acyl-ADP-ribose and NAM. In mammals, the sirtuin gene and protein family comprises seven members (SIRT1-SIRT7), each exhibiting distinct cellular localizations and functions [179, 180]. SIRT1 and SIRT6 reside in the nucleus, where they perform crucial roles in DNA repair and genome stability. In contrast, SIRT7 is specifically localized in the nucleolus. In mitochondria, SIRT3, SIRT4, and SIRT5 are responsible for regulating mitochondrial homeostasis. In the cytoplasm, SIRT1, SIRT2, and SIRT5 perform significant roles in circadian rhythm and gene expression. Based on their distinct Km values for NAD+ , sirtuins can be categorized into two groups: sirtuins with a Km value below the physiological range of NAD, such as SIRT2, SIRT4, SIRT5, and SIRT6, and sirtuins whose activity is highly dependent on the availability of NAD, including SIRT1 and SIRT3. Sirtuins are of great importance due to their ability to influence cell homeostasis through NAD+ levels, making them promising targets for antiaging therapy.
The PARP protein family serves as an essential consumer of NAD+ . This family consists of 17 members in humans and 16 members in mice, and it plays a pivotal role in DNA repair and genome integrity preservation. PARPs facilitate the cleavage of NAD+ to produce NAM and ADP-ribose. This ADP-ribose is subsequently attached to PARP and other receptor proteins, forming a polymer bond in a process referred to as poly(ADP-ribosyl) acylation (PAR acylation). PAR acylation is a dynamic, posttranscriptional modification that plays a crucial role in maintaining DNA repair and genome stability [181, 182]. Of the PARPs, PARP1, PARP2, and PARP3 are localized in the nucleus and consume a significant amount of NAD+ . As we age, both DNA damage and PARP activity increase. Among all PARPs, only PARP1, PARP2, and PARP3 are located within the nucleus. Of these, PARP1 and PARP2 are the primary consumers of NAD+ . Upon DNA damage, PARP1 is the sole contributor to approximately 90% of PARP activity [181]. Because of the fact that the Km value of PARPs is significantly lower than the physiological range of NAD, PARPs have a greater advantage in competing for the limited NAD resources than sirtuins [183, 184].
The cyclic ADP-ribose (cADPR) synthases constitute another group of NAD+ consumers, with CD38 and CD157 being the most prominent in cells. They possess both glycohydrolase and ADP-ribosyl cyclase activities, breaking down NAD+ into NAM and adenosine ADP-ribose and then producing cADPR [185]. Acting as an intercellular messenger, cADPR impacts calcium signal transduction, ROS production, and apoptosis [186]. In addition to NAD+ , CD38, and CD157 can also employ NMN and NR as alternative substrates, respectively [187,188,189]. Therefore, inhibitors of CD38 and CD157 hold the potential in restoring NAD+ levels in aging individuals and treating metabolic disorders and aging-related diseases [190]. The aging process causes an elevation in the levels of CD38 and CD157, leading to increased utilization of NAD+ [188, 191]. This phenomenon contributes to the decreased NAD+ levels observed in aged mice compared to young mice. Studies have demonstrated that CD38 deficiency in mice eliminates the reduction in NAD+ during aging [192], thereby indicating its potential role in aging-related diseases [112, 193].
SARM1, primarily expressed in neurons, is classified as an NAD+ glycohydrolase and cyclase, and its degradation of NAD+ is closely tied to axonal destruction [194, 195]. NAD+ is additionally involved in the formation of NAD+ RNA caps,however, its physiological relevance remains to be elucidated [196, 197].
Function of NAD+
Metabolism
NAD+ is an indispensable coenzyme intricately involved in cellular redox reactions, assuming an important role in cellular energy metabolism. It is engaged in diverse catabolic pathways, such as glycolysis, amino acid degradation, and fatty acid oxidation. Within these biochemical processes, NAD+ is reduced by accepting hydride ions, forming NADH. Subsequently, NADH transfers the acquired electrons to the electron transport chain, culminating in the production of ATP. Beyond its fundamental role in redox reactions, NAD+ exhibits versatility by undergoing phosphorylation to yield NADP. This phosphorylated form acts as a hydrogen acceptor, giving rise to NADPH, a pivotal participant in antioxidant defense and synthetic metabolic pathways.
Emerging evidence suggests that strategies aimed at modulating NAD+ degradation pathways or enhancing NAD+ levels may offer therapeutic benefits for metabolic disorders and aging [2]. Maintaining the balance of NAD+ is essential for the optimal functioning of diverse metabolic tissues [198]. Changes or disruptions in metabolic states, such as high-fat diets, postpartum weight loss, and circadian rhythm disturbances [154, 199,200,201], may lead to a decline in NAD+ levels, affecting NAD+ -dependent cellular processes. Conversely, increasing cellular NAD+ levels through exercise, caloric restriction, and healthy dietary interventions have been shown to reduce stress and promote metabolic normalization [202].
Knocking out PARP1 or CD38 or using PARP and CD38 inhibitors in mice leads to supraphysiological levels of NAD+ in vivo. This change enhances metabolic rates in mice during high-fat diet feeding and aging, and glucose metabolism remains relatively normal, demonstrating favorable effects in preventing obesity [188, 203, 204]. In mice subjected to a high-fat diet, reduced expression of NAMPT, a key enzyme in the NAD+ salvage pathway, leads to decreased activity in this pathway, which may be a potential mechanism underlying the decline in NAD+ levels during obesity. Additionally, in mice with adipocyte-specific NAMPT deficiency, NAD+ levels decrease, insulin resistance increases, and metabolic dysfunction worsens in adipose tissue [205], further supporting the significance of NAD + homeostasis in normal metabolic activities. The longevity protein SIRT2 has been found to promote lifespan in an NAD+ -dependent manner [177, 206]. Higher NAD+ levels also enhance the activity of nuclear SIRT1 and mitochondrial SIRT3, thereby regulating mitochondrial function and preventing diet-induced metabolic disorders [207, 208].
Inflammation and immunity
The relationship between chronic inflammation, immune cells, and metabolic cells is complex [209]. Targeting macrophage immune metabolic pathways by modulating NAD+ biosynthesis or degradation is of significant importance in regulating the inflammatory state and alleviating diseases [210]. Recent studies have indicated that NAD+ is a crucial regulatory factor for macrophage function, and pro-inflammatory M1-like macrophages may serve as the primary source of pro-inflammatory cytokines in aging tissues. Enhanced CD38 expression in macrophages leads to increased NAD + consumption, resulting in pro-inflammatory (M1) macrophage polarization. Blocking NAMPT can impede glycolytic switching in M1 macrophages, limit pro-inflammatory responses in vitro, and reduce systemic inflammation in vivo. Conversely, increased NAMPT function leading to elevated NAD + levels promotes anti-inflammatory (M2) macrophage polarization [112].
During the aging process, elevated CD38 expression and increased NADase activity in the liver and adipose tissues contribute to declining NAD + levels and accumulation of pro-inflammatory M1-like macrophages [111, 211]. Impaired de novo NAD + synthesis in aging macrophages also affects their functionality during aging [212]. The enhanced expression of pro-inflammatory cytokines may drive a vicious cycle of inflammation, exacerbating tissue and DNA damage, and further activating major NAD + consumers such as CD38 and PARP, accelerating age-related physiological decline.
On the other hand, NAD + has been implicated in inducing cell death in specific T cell subsets [213], and it can also influence T cell polarization [214, 215], showing the dual role of NAD + in immune regulation. The precise role of NAD + in adaptive immune function remains unclear and requires further investigation.
DNA repair, transcriptional regulation and epigenetics
As discussed in the section “Degradation of NAD + ” above, the PARP protein family, a crucial NAD + consumer, plays a central role in DNA repair and genome integrity. PARP accumulates at sites of single-strand breaks in cellular DNA and initiates the DNA repair process by utilizing NAD + for auto-ADP-ribosylation. Therefore, PARP is also considered a major consumer of NAD + during the aging process. Overactivation of PARP can be observed during aging or after DNA damage [216, 217], and this excessive activation may contribute to age-dependent NAD + depletion. Pharmacological inhibition or genetic deficiency of PARP1 prevents the decline in NAD + levels during aging and nutrient stress [217, 218]. NADP, acting as an endogenous inhibitor of PARP in mammalian cells, has been shown to be a negative regulator of PARylation and DNA damage repair in cancer cells [219]. Supplementing NAD + precursors can reduce DNA damage observed in hippocampal neurons of Alzheimer’s disease mouse models [220]. Apart from its role in DNA repair, PARP also functions as a chromatin modifier, a co-regulator of DNA-binding transcription factors, and a regulator of DNA methylation during the process of protein transcription [221,222,223,224]. Striking a balance between promoting and inhibiting PARP activity to achieve DNA repair and protein transcription regulation is crucial for inhibiting aging.
The sirtuin enzyme family, as another major NAD + consumer, is not only involved in DNA damage repair processes but also associated with epigenetic modifications related to aging. Sirtuins prevent DNA damage by inhibiting ROS production in mitochondria and activating ROS scavenging enzymes [225, 226]. They also promote DNA damage repair through mechanisms such as PARP activation [227], glutamine anaplerosis [228], and homologous recombination-mediated double-strand DNA break repair [229, 230]. The most notable role of sirtuins in epigenetics is their deacetylation function on histones. Deacetylation of histones H4K16, H3K9, and H3K56 by sirtuins contributes to lifespan extension [231,232,233]. Sirtuins can also activate histone methyltransferases and promote histone methylation processes [234].
Cellular senescence
As NAD + levels decline, senescent cells continue to accumulate in aging tissues. However, there have been no studies to establish a direct relationship between the accumulation of inflammatory senescent cells and NAD + levels during the aging process. The specific mechanism by which NAD + influences cellular aging remains unclear. Some studies have reported that NAD + levels affect the aging-related secretory phenotype (SASP) of senescent cells [235]. Supplementation with NAD + precursor substances enhances SASP, leading to increased chronic inflammation. CD38 is considered the primary enzyme responsible for NAD + consumption [188, 204], causing NAD + levels to decline during aging. As age increases, CD38 levels also rise, although the underlying mechanism is not well understood.
It has been observed that senescent cells and their SASPs activate CD38 expression in macrophages, promoting CD38-dependent NADase activity [111, 211]. Moreover, CD38 expression is increased in macrophages co-cultured with senescent cells or exposed to conditioned medium [112], suggesting that macrophages may represent the primary cell population responding to SASP with reduced NAD + levels. Another study revealed that cells with dysfunctional mitochondria initiate pro-inflammatory programs by secreting pro-inflammatory cytokines. However, supplementation with NAD + precursors partially ameliorates this situation, in part by reducing inflammation and the burden of senescent cells [127].
Regulatory mechanism of NAD + metabolism in ovarian aging
Modifying the properties of enzymes involved in NAD + biosynthesis or degradation
In aging mouse oocytes, the mRNA expression levels of enzymes related to NAD + biosynthesis, such as NAMPT, NaPRT, Nrk1/2, and NMNAT1/3, show no significant changes compared to young oocytes. However, the mRNA and protein expression levels of NMNAT2 significantly decrease [236]. Further investigations revealed that knocking down NMNAT2 in oocytes leads to a reduction in NAD + levels, disrupts the assembly of the meiotic spindle, and perturbs metabolic activities. Rescuing the aging phenotype of oocytes in which NMNAT2 is knocked down through SIRT1 overexpression suggests that NMNAT2 may regulate the oxidative-redox homeostasis of aging oocytes by modulating NAD + levels, thereby suppressing the aging phenotype of oocytes. Additionally, NMNAT2 downregulation can protect cells from p53-dependent cell death in response to DNA damage [237].
Sirtuins, PARPs, and cADPR are the major NAD + -consuming enzymes in cells. Sirtuins have been shown to impact oocyte quality by modulating redox states. In mouse oocytes, the expression of all sirtuins is observed, and their levels gradually decrease until the blastocyst stage. Studies have reported that SIRT1 in GV oocytes can counteract oxidative stress through the Fox3-MnSod axis under in vitro culture conditions [238]. Inhibiting SIRT1 activity in in vitro-cultured oocytes increases the likelihood of spindle and chromosomal abnormalities. SIRT1, FOXO3a, and NRF-1 may form a complex on the SIRT6 promoter, collectively participating in the regulation of ovarian follicle development [239]. P53 protein is expressed in arrested follicles, and SIRT1 can regulate p53 acetylation and p53-dependent apoptosis. SIRT1 activation leads to a reduction in p53 expression, potentially preserving oocytes that would otherwise be lost [240, 241]. Oocyte-specific overexpression of SIRT1 in mice continuously activates FOXO3a and suppresses mTOR, resulting in increased ovarian reserves, extended ovarian lifespan, and enhanced reproductive capacity [242]. Epigenetic inhibitors or RNAi targeting SIRT1 reduce oocyte survival by lowering H4K16ac levels, implying a connection between SIRT1 suppression and the establishment of oocyte follicle development [243]. SIRT3, a mitochondrial sirtuin [244], exhibits reduced expression in aging ovaries, leading to mitochondrial dysfunction and abnormal spindle assembly. Studies have reported that SIRT3 inactivation in in vitro fertilized and cultured embryos increases mitochondrial ROS production, subsequently upregulating p53, resulting in developmental arrest [245]. This indicates a protective role of SIRT3 against oxidative stress-induced developmental arrest in preimplantation embryos cultured in vitro.
PARPs maintain chromosome stability during meiosis and play a crucial role in DNA repair [246]. While there is literature suggesting that regulating ovarian NAD + metabolism can reduce DNA damage and maintain genome stability [39, 40, 247], the specific role and mechanisms of PARPs in this context remain unclear. CD38, a representative enzyme for cADPR, can influence cellular calcium signaling, ROS production, and apoptosis. CD38 is not expressed in ovarian follicles but is mainly present in ovarian immune cells, showing an age-dependent increase in expression. CD38 deficiency results in increased NAD + levels in the ovaries, reduced NAM and ADPR levels, and positive regulation of ovarian NAD + metabolism. CD38 deficiency enhances ovarian reserves and reproductive capacity in young female animals, and it can alleviate ovarian inflammation in aging animals by reducing multinucleated macrophage giant cells postreproduction. These beneficial changes are associated with increased ovarian NAD + levels [248] (Fig. 3).
Mechanism of NAD + metabolism in ovarian aging. Modulating the properties of enzymes involved in NAD + biosynthesis or degradation, providing NAD + precursors, and altering lifestyle collectively govern cellular NAD + metabolism. In the context of ovarian aging, NAD + metabolism predominantly exerts a beneficial influence on granulosa cells, oocytes, and embryonic development through alterations in the redox state and the activities of NAD + -dependent enzymes. This ultimately manifests as the reversal of ovarian aging
Supplementing NAD + precursors
In the oocytes of aging mice, protein acetylation levels are abnormally regulated. Sirtuins, a family of NAD + -dependent class III histone deacetylases, also target many nonhistone substrates. NAM is a product of NAD + -dependent enzymes such as sirtuins, PARPs, and CD38, as well as a precursor for NMN and NAD + synthesis. NAM supplementation can increase cellular NAD + levels and noncompetitively inhibit the deacetylase activity of sirtuins. Currently, NAM is known to inhibit the activity of SIRT1 and SIRT2. SIRT1 regulates p53 acetylation and p53-dependent apoptosis in response to DNA damage and oxidative stress [249]. SIRT2 plays a role in microtubule protein deacetylation [250]. Compared to class I and II histone deacetylase inhibitors, NAM can regulate the acetylation and deacetylation of α-tubulin proteins in aging oocytes at lower levels, significantly inhibiting the generation of abnormal microtubule structures during aging and affecting aging-related phenotypes associated with oocyte maturation [251].
Furthermore, NAM treatment significantly reduces the efficiency of GVBD, which produces similar effects to the use of SIRT2-specific inhibitors. However, subsequent events during meiosis I, including spindle assembly and chromosome alignment, remain unaffected. Oocytes treated with NAM show high expression of the anaphase-promoting complex-Cdc20 during meiosis I exit, which is associated with a decrease in cyclin B1 levels and an increase in inhibitory phosphorylation of Cdk1, expected to lead to Cdk1 inactivation and establish a mid-meiotic arrest in meiosis II [252]. Higher concentrations of NMN result in beneficial effects rather than harmful effects in ovulated mouse eggs [251] (Fig. 3).
NMN is a product of the NAMPT reaction and a crucial intermediate in NAD + homeostasis. Supplementing NMN in mice can increase NAD + levels, reverse the aging phenotype of oocytes in aging mice, and mitigate the adverse effects of aging on development when NMN is supplemented in embryo culture medium [8]. However, the exact mechanisms of action remain unclear. SIRT2, through deacetylation and stabilization of BubR1, plays a role in maintaining microtubule-kinetochore attachments, ensuring chromosome separation fidelity. The benefits of NMN for oocytes in aging animals are largely achieved through overexpression of SIRT2. Supplementing NMN can also enhance the fertilization capacity of oocytes by maintaining the dynamics of the cortical granule component ovastacin [39]. Long-term NMN treatment upregulates the expression of PGC-1α, a protein related to mitochondrial function, to a certain extent, reversing damage to granulosa cells in ovarian follicles [253].
Research has shown that NR supplementation can increase NAD + levels in mouse ovarian cells, reversing the ovarian aging phenotype. NR significantly upregulates the expression of genes related to mitochondrial dynamics, such as OPA1, MFN1/2, DRP1, and FIS1, which decrease with ovarian aging. Intermediate metabolites involved in energy metabolism, such as citrate, isocitrate, D-fructose1, and NAD + , are also upregulated, leading to increased ATP production. Mitochondrial biogenesis increases, and the expression of the mitochondrial autophagy-related genes PINK and LC3 is upregulated. NR treatment enhances mitochondrial autophagy and improves mitochondrial dynamics and mitochondrial function in aging oocytes, ultimately improving oocyte quality [40]. Another study reported that NR treatment can mitigate the decline in oocyte quality postovulation and lead to better clinical outcomes in assisted reproductive technology. In this study, the mRNA expression of core proteins of the mitochondrial oxidative phosphorylation chain was studied, and it was found that NR treatment increases the expression of Sdhb, Uqcrc2, and Atp5a1 [247], which helps prevent age-related mitochondrial dysfunction (Fig. 3).
Therapeutic potential of NAD + in ovarian aging
Pharmacological NAD + boosting
The levels of NAD + in the body are regulated by a delicate balance between its synthesis and degradation, which is influenced by the aging process [2, 254,255,256,257]. The concentration of NAD + in various tissues can be modified through diet, lifestyle, and pharmacological interventions, potentially yielding therapeutic benefits in certain cases. Currently, there are three main strategies for increasing NAD + levels through pharmacology: 1) improving the activity of enzymes involved in NAD + biosynthesis, particularly those that are critical in the rate-limiting steps of both the de novo synthesis and salvage pathways, such as α-amino-β-carboxymuconate-ε-semialdehyde decarboxylase (ACMSD) and NAMPT,2) inhibiting enzymes responsible for NAD + degradation, such as PARPs and CD38; and 3) supplementing the diet with NAD + precursors to support NAD + synthesis through the salvage pathway. Studies conducted in C. elegans [217], flies [258], rodents [259], and humans [260, 261] have revealed the feasibility of increasing NAD + levels by supplying NAD + precursors (Fig. 4).
Therapeutic potential of NAD + in ovarian aging. Previous studies conducted in multiple model animals and humans have revealed the feasibility of increasing NAD + levels by supplying NAD + precursors, and the NAD + metabolomic pathway can enhance mitochondrial function, enhance autophagy levels, and maintain protein homeostasis in mitochondria and lysosomes, consequently decelerating the progression of ovarian aging
Characteristics of NAD + precursors
To date, the identified NAD precursors include tryptophan, NA, NAM, NR, and NMN. These precursors have garnered significant attention as NAD + precursors due to their role in NAD + synthesis, which has been increasingly recognized [260, 262, 263]. Published research has not yet identified any specific preference of ovarian tissue for any of the mentioned NAD precursors. NA and NAM have a long history of being linked to pellagra [264], a disease that is preventable by consuming a diet rich in these precursors [265]. Recently, NR and NMN have gained attention as NAD + precursors due to their comparatively lower side effects compared to NA and NAM. These precursors enter cells through various mechanisms: NA directly passes through cells with the help of membrane carriers (SLC5A8 or SLC22A13) [266, 267], while NR enters cells through equilibrative nucleoside transporters (ENTs). NAM can enter cells either directly or can be converted into NMN via NAMPT. NMN enters cells through specific transporters (the Slc12a8 gene) [268], by conversion into NAM or NR via CD38 or CD73, or through ENTs [159, 188].
In terms of pharmacokinetics, NAD + precursors exhibit distinct properties. Tryptophan, NAM, and NA in plasma present the highest concentrations, surpassing 0.1 μM, with the concentration of NAM being ten times higher than that of NA in plasma. Moreover, under basal conditions, NR and NMN are almost nonexistent in plasma. That is, the liver is the main provider of circulating NAM, accounting for more than 95% of tryptophan-NAM production. The absorption, production, and consumption of NAM and NAD vary significantly among organs, correlating with the expression of enzymes involved in NAD synthesis and consumption. Administration of high doses of NA leads to elevated levels of NAM, which possesses a longer half-life than NA [269]. Although NAM has a stronger ability to raise NAD + levels, excessive NAM concentrations can result in adverse effects, such as nausea and vomiting [270], and may also negatively impact NAD + -consuming enzymes such as PARPs and sirtuins [261]. Clinical studies have shown the effectiveness of NA in raising blood and muscle NAD + levels, thereby alleviating systemic NAD + deficiency in patients with mitochondrial myopathy and improving muscle performance [271].
Likewise, oral intake of NAM can quickly elevate both NAM and NAD + levels in the blood [272]. Research has also shown that NMN can significantly increase NAD + levels in peripheral tissues and can even traverse the blood–brain barrier to increase NAD + in the brain [273, 274]. Upon oral administration, NMN is rapidly absorbed into the bloodstream from the intestine within a short span of 2–3 min, swiftly distributing to diverse tissues through circulation within 15 min. After 15 min, the plasma NMN level returns to baseline, while increased concentrations of NAD + can be detected in the liver, skeletal muscle, and cerebral cortex [275]. Additionally, clinical trials have demonstrated that a single oral dose of NMN can substantially increase the levels of NMN and NAD + metabolites in the plasma [276]. Similarly, oral intake of NR increases NAD + levels in blood cells, displaying 2–3 times greater potency at raising ADPR compared to NAM [261].
NAD + boosting in vitro
Notably, the potential benefits of supplementation with NAD + precursors in preventing and treating age-related diseases have gained increasing attention. Nevertheless, the impact of NAD + precursor supplementation on ovarian aging remains insufficiently investigated. A few studies have explored the role of NAD + precursors in ovarian aging (Table 1). For instance, a study in 2013 demonstrated that supplying ovulated aging oocytes with NAM could inhibit the formation of abnormal spindles and reduce cell fragmentation [251], implying a potential delay in the aging process. Furthermore, boosting NAD + biosynthesis with NA was found to prevent oxidative stress and meiotic defects in old oocytes, effectively delaying the aging process of oocytes in aged mice [236]. However, conflicting results have been observed in other studies. Specifically, one study found that NAM disrupted the regulation of Cdk1 in ovulated oocytes, impairing entry into meiosis I and the establishment of metaphase II arrest [252]. A recent study revealed the efficacy of NR supplementation in maintaining the quality of postovulatory oocytes [247]. NR effectively curbs the decline in NAD + levels, counteracts mitochondrial dysfunction, preserves spindle and chromosome structure, and decreases ROS levels and DNA damage, thereby improving oocyte quality and embryonic development potential and potentially enhancing the success rate of assisted reproductive technology. The precise molecular mechanism underlying the numerous benefits of NR supplementation remains unclear. Similarly, a separate study found that NMN treatment in embryo culture reverses the negative impact of aging on development [8].
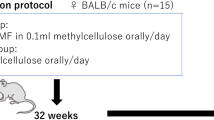
NAD + boosting in vivo
The impact of NAD + precursor supplementation on ovarian aging has been explored in vivo (Table 1). The results have shown that NMN supplementation in vivo can enhance the oocyte quality, ovulation rate, and fertility in aged mice [8]. Studies have found that a 4-week preovulation treatment of NMN can restore oocyte spindle assembly and reduce the occurrence of aneuploidy, improving oocyte quality. Additionally, the mechanisms underlying the improvement in the ovulation rate with NMN treatment may be related to the NAD + metabolome and the effects of other tissues on follicle development. Low-dose NMN supplementation has been found to increase the pregnancy rate and the number of live births in aged mice, suggesting an optimal concentration for promoting fertility. Furthermore, NMN treatment can also ensure normal dynamics of cortical granules, improve sperm binding, and enhance the fertilization capacity of aged oocytes [39]. The benefits of NMN treatment are mainly attributed to the enhancement of energy metabolism in oocytes, although a similar effect was observed in aged mice with transgenic overexpression of SIRT2. Nevertheless, the results from SIRT2 knockout mice indicate that SIRT2 protein may not play a crucial role in oocyte function [277, 278]. Consequently, further research is necessary to ascertain the participation of other members of the sirtuin family in mediating the effects of NMN.
A separate study observed similar outcomes when utilizing NMN to boost NAD + biosynthesis in aged mice [39]. The research team discovered that NMN supplementation led to an increase in antral follicles and ovulated oocytes while decreasing the occurrence of mature oocytes with fragmentation. NMN treatment improved the maturation of the nucleus and cytoplasm in aged oocytes, thus boosting the maturation rate of oocytes. Through the implementation of single-cell transcriptome profiling, the researchers investigated the potential effectors of NMN and discovered that the impact of NMN on aged oocytes may be due to its effects on mitochondrial function. Specifically, the benefits of NMN appear to stem from the restoration of mitochondrial function, reduction in the accumulation of ROS, and suppression of apoptosis (Fig. 4). Some studies suggest that administering NMN to 40-week-old mice for 20 weeks can enhance mitochondrial function, enhance autophagy levels, and maintain protein homeostasis in mitochondria and lysosomes, consequently decelerating the progression of ovarian aging [253]. Additionally, prolonged supplementation with NMN was also found to lower the expression of the ovarian aging marker P16 and increase the expression levels of mitochondrial function-related proteins. Furthermore, supplementation with NR was found to restore mitochondrial function and enhance mitochondrial energy metabolism, leading to improved ovarian reserve, increased ovulation potential, and a higher live-birth rate in aged mice [40, 279]. However, currently, there is a lack of available literature that describes clinical studies investigating the use of NAD precursors in research on ovarian aging.
Therapeutic potential of NAD + in clinical trials on aging-related conditions
Most preclinical rodent studies have revealed the promising translational potential of NAD + boosting therapy. Some clinical trials have already investigated the use of NAD + precursors for aging-related conditions (Table 2). The NAD + precursors used in clinical trials are mainly NR and NMN [276, 280], neither of which has been reported to cause adverse reactions [281], while the use of NA can cause flushing and pain [282]. Clinical trials evaluating the pharmacokinetics and toxicology of NAD + precursors have yielded preliminary evidence supporting the safety of NAD + boosting therapy [283,284,285,286]. Nonetheless, translating the promising therapeutic effects observed in preclinical animal models to humans has proven challenging due to the mild and occasionally contradictory nature of the beneficial effects of NAD + precursors.
Positive results have been seen in clinical studies, indicating that NMN supplementation can increase muscle insulin sensitivity in overweight or obese prediabetic women, thereby improving insulin signaling and remodeling [286]. In another clinical investigation of the antiaging effects of NMN, it was observed that NMN can significantly increase NAD levels in the serum of healthy subjects. Furthermore, NMN supplementation leads to increased insulin sensitivity, as evidenced by the substantially reduced HOMA scores compared to those of the control group, highlighting the antiaging effects of NMN [287]. However, a clinical study employing a dose-dependent regimen showed that NMN supplementation did not impact insulin sensitivity, although statistically significant improvements were observed in the health status of the participants [285]. Studies have reported that short-term use of NR has some beneficial effects on healthy older adults [13]. Moreover, long-term supplementation with the NAD + precursor NR exhibits good tolerability and effectively stimulates NAD metabolism in healthy middle-aged and older adults, resulting in reduced levels of circulating inflammatory cytokines [260, 284]. Some studies conducted with older adults have indicated that supplementation with NAD + precursors through L-tryptophan, niacin, and nicotinamide does not improve mitochondrial or skeletal muscle function [283]. Additionally, supplementing NR in older obese men has little effect [280, 288]. Interestingly, a study has reported that NA can rectify systemic NAD deficiency, leading to enhanced muscle performance in patients with mitochondrial myopathy [271].
The reasons behind the absence of beneficial effects in human trials of NAD + boosting therapy thus remain unclear. This could potentially be attributed to the inability of NAD + precursors to increase NAD levels in specific tissues of the human body [260, 263, 289]. Moreover, the duration of the studies may have been inadequate to attain clinical benefits, and the experimental designs primarily concentrated on healthy subjects with normal baseline NAD levels. Therefore, further human clinical trials are imperative to ascertain suitable dosage regimens, treatment periods, and long-term toxicological outcomes. These trials should account for participant diversity to effectively tackle the translational challenges associated with NAD + promotion strategies.
Perspective
The significance of NAD + in various disease models, including cancer, neurodegeneration, organ disease, and aging, has gained widespread recognition and has received extensive research attention [7, 198, 260, 290, 291]. This is attributed to the essential role of NAD + as a cofactor in redox reactions, as well as its involvement in vital processes such as energy metabolism, cellular homeostasis, posttranslational modification, epigenetic changes, and RNA stability [144, 292,293,294]. Studies on NAD + boosting by supplementing NAD + precursors in the context of ovarian aging are gaining momentum. Animal models of ovarian aging have demonstrated that supplementation with NAD + precursors improves oocyte quality, alleviates ovarian aging, and enhances fertility.
However, the molecular mechanism behind NAD + precursors remains unclear. Numerous questions have arisen, encompassing the transportation of NAD + and its precursors to ovarian cells and organelles, the preference of ovarian cells for certain NAD + precursors, the effect of specific NAD + metabolic pathways on NAD + flux in healthy and aging ovaries, and the repair mechanism for toxic metabolites produced by NAD + metabolism. Currently, the beneficial effects of NAD + boosting therapy in human trials are highly limited, leaving numerous questions unanswered. Notwithstanding these uncertainties, although much research is required to comprehensively elucidate the biological and therapeutic potential of NAD + in this context, NAD + boosting therapy still holds promise for addressing ovarian aging.
Availability of data and materials
Not applicable.
References
Rajman L, Chwalek K, Sinclair DA. Therapeutic potential of NAD-boosting molecules: the in vivo evidence. Cell Metab. 2018;27:529–47.
Verdin E. NAD(+) in aging, metabolism, and neurodegeneration. Science. 2015;350:1208–13.
Yaku K, Okabe K, Nakagawa T. NAD metabolism: Implications in aging and longevity. Ageing Res Rev. 2018;47:1–17.
Chini CCS, Zeidler JD, Kashyap S, Warner G, Chini EN. Evolving concepts in NAD(+) metabolism. Cell Metab. 2021;33:1076–87.
Schultz MB, Sinclair DA. Why NAD(+) declines during aging: it’s destroyed. Cell Metab. 2016;23:965–6.
Koehn CJ, Elvehjem CA. Further studies on the concentration of the antipellagra factor. J Biol Chem. 1937;118:693–9.
Abdellatif M, Sedej S, Kroemer G. NAD(+) metabolism in cardiac health, aging, and disease. Circulation. 2021a;144:1795–817.
Bertoldo MJ, Listijono DR, Ho WJ, Riepsamen AH, Goss DM, Richani D, Jin XL, Mahbub S, Campbell JM, Habibalahi A, et al. NAD(+) repletion rescues female fertility during reproductive aging. Cell Rep. 2020;30:1670-1681 e1677.
Hikosaka K, Yaku K, Okabe K, Nakagawa T. Implications of NAD metabolism in pathophysiology and therapeutics for neurodegenerative diseases. Nutr Neurosci. 2021;24:371–83.
Romani M, Sorrentino V, Oh CM, Li H, de Lima TI, Zhang H, Shong M, Auwerx J. NAD(+) boosting reduces age-associated amyloidosis and restores mitochondrial homeostasis in muscle. Cell Rep. 2021;34:108660.
Braidy N, Liu Y. NAD+ therapy in age-related degenerative disorders: a benefit/risk analysis. Exp Gerontol. 2020;132:110831.
Hou Y, Wei Y, Lautrup S, Yang B, Wang Y, Cordonnier S, Mattson MP, Croteau DL, Bohr VA. NAD(+) supplementation reduces neuroinflammation and cell senescence in a transgenic mouse model of Alzheimer’s disease via cGAS-STING. Proc Natl Acad Sci U S A. 2021;118:e2011226118.
Martens CR, Denman BA, Mazzo MR, Armstrong ML, Reisdorph N, McQueen MB, Chonchol M, Seals DR. Chronic nicotinamide riboside supplementation is well-tolerated and elevates NAD(+) in healthy middle-aged and older adults. Nat Commun. 2018;9:1286.
ASRM. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril. 2020;114:1151–7.
McGee EA, Hsueh AJ. Initial and cyclic recruitment of ovarian follicles. Endocr Rev. 2000;21:200–14.
Tal R, Seifer DB. Ovarian reserve testing: a user’s guide. Am J Obstet Gynecol. 2017;217:129–40.
Hansen KR, Knowlton NS, Thyer AC, Charleston JS, Soules MR, Klein NA. A new model of reproductive aging: the decline in ovarian non-growing follicle number from birth to menopause. Hum Reprod. 2008;23:699–708.
Demko ZP, Simon AL, McCoy RC, Petrov DA, Rabinowitz M. Effects of maternal age on euploidy rates in a large cohort of embryos analyzed with 24-chromosome single-nucleotide polymorphism-based preimplantation genetic screening. Fertil Steril. 2016;105:1307–13.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, Scott RT Jr. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101:656-663 e651.
Chiang JL, Shukla P, Pagidas K, Ahmed NS, Karri S, Gunn DD, Hurd WW, Singh KK. Mitochondria in ovarian aging and reproductive longevity. Ageing Res Rev. 2020;63:101168.
Liu Y, Gao J. Reproductive aging: biological pathways and potential interventive strategies. J Genet Genomics. 2023;50:141–50.
Tamura H, Kawamoto M, Sato S, Tamura I, Maekawa R, Taketani T, Aasada H, Takaki E, Nakai A, Reiter RJ, et al. Long-term melatonin treatment delays ovarian aging. J Pineal Res. 2017;62:e12381.
He C, Wang J, Zhang Z, Yang M, Li Y, Tian X, Ma T, Tao J, Zhu K, Song Y, et al. Mitochondria synthesize melatonin to ameliorate its function and improve mice oocyte’s quality under in vitro conditions. Int J Mol Sci. 2016;17:939.
Tamura H, Jozaki M, Tanabe M, Shirafuta Y, Mihara Y, Shinagawa M, Tamura I, Maekawa R, Sato S, Taketani T, et al. Importance of melatonin in assisted reproductive technology and ovarian aging. Int J Mol Sci. 2020;21:1135.
Zhang H, Li C, Wen D, Li R, Lu S, Xu R, Tang Y, Sun Y, Zhao X, Pan M, et al. Melatonin improves the quality of maternally aged oocytes by maintaining intercellular communication and antioxidant metabolite supply. Redox Biol. 2022;49:102215.
Zheng B, Meng J, Zhu Y, Ding M, Zhang Y, Zhou J. Melatonin enhances SIRT1 to ameliorate mitochondrial membrane damage by activating PDK1/Akt in granulosa cells of PCOS. J Ovarian Res. 2021;14:152.
Budani MC, Tiboni GM. Effects of supplementation with natural antioxidants on oocytes and preimplantation embryos. Antioxidants (Basel). 2020;9:612.
Darabi Z, Basir Z, Tabandeh MR, Ghotbeddin Z. Coenzyme Q10 improves ovarian histology and attenuates the expression of angiogenesis-associated proteins in the ovary of rats with experimental hyperstimulation syndrome. Iran J Basic Med Sci. 2022;25:989–96.
Ozcan P, Ficicioglu C, Kizilkale O, Yesiladali M, Tok OE, Ozkan F, Esrefoglu M. Can Coenzyme Q10 supplementation protect the ovarian reserve against oxidative damage? J Assist Reprod Genet. 2016;33:1223–30.
Xu Y, Nisenblat V, Lu C, Li R, Qiao J, Zhen X, Wang S. Pretreatment with coenzyme Q10 improves ovarian response and embryo quality in low-prognosis young women with decreased ovarian reserve: a randomized controlled trial. Reprod Biol Endocrinol. 2018;16:29.
Liao K, Wang Y, Zheng L, Lu D, Wu J, Wu B, Wu Z, Jiang Z. Effect of folic acid supplementation on diminished ovarian reserve: study protocol of a single-centre, open-label, randomised, placebo-controlled clinical trial. BMJ Open. 2022;12:e057689.
Ozatik FY, Ozatik O, Yigitaslan S, Kaygisiz B, Erol K. Do Resveratrol and dehydroepiandrosterone increase diminished ovarian reserve? Eurasian J Med. 2020;52:6–11.
Pasquariello R, Verdile N, Brevini TAL, Gandolfi F, Boiti C, Zerani M, Maranesi M. The role of resveratrol in mammalian reproduction. Molecules. 2020;25:4554.
Barim-Oz O, Sahin H. The influence of dietary antioxidant on ovarian eggs and levels of vitamin E, C, A, astaxanthin, beta-carotene and oxidative stres in tissues of Astacus leptodactylus (Eschscholtz) during reproduction. Cell Mol Biol (Noisy-le-grand). 2016;62:1–10.
Gai HF, An JX, Qian XY, Wei YJ, Williams JP, Gao GL. Ovarian damages produced by aerosolized fine particulate matter (PM(2.5)) pollution in mice: possible protective medications and mechanisms. Chin Med J (Engl). 2017;130:1400–10.
Hart RJ. Use of growth hormone in the IVF treatment of women with poor ovarian reserve. Front Endocrinol (Lausanne). 2019;10:500.
Tesarik J, Galan-Lazaro M, Conde-Lopez C, Chiara-Rapisarda AM, Mendoza-Tesarik R. The effect of GH administration on oocyte and zygote quality in young women with repeated implantation failure after IVF. Front Endocrinol (Lausanne). 2020;11:519572.
Tachibana M, Kuno T, Yaegashi N. Mitochondrial replacement therapy and assisted reproductive technology: a paradigm shift toward treatment of genetic diseases in gametes or in early embryos. Reprod Med Biol. 2018;17:421–33.
Miao Y, Cui Z, Gao Q, Rui R, Xiong B. Nicotinamide mononucleotide supplementation reverses the declining quality of maternally aged oocytes. Cell Rep. 2020;32:107987.
Yang Q, Cong L, Wang Y, Luo X, Li H, Wang H, Zhu J, Dai S, Jin H, Yao G, et al. Increasing ovarian NAD(+) levels improve mitochondrial functions and reverse ovarian aging. Free Radic Biol Med. 2020;156:1–10.
Danial NN, Korsmeyer SJ. Cell death: critical control points. Cell. 2004;116:205–19.
Friedman JR, Nunnari J. Mitochondrial form and function. Nature. 2014;505:335–43.
Perez GI, Trbovich AM, Gosden RG, Tilly JL. Mitochondria and the death of oocytes. Nature. 2000;403:500–1.
Wang X. The expanding role of mitochondria in apoptosis. Genes Dev. 2001;15:2922–33.
McBride HM, Neuspiel M, Wasiak S. Mitochondria: more than just a powerhouse. Curr Biol. 2006;16:R551-560.
Gougeon A. The biological aspects of risks of infertility due to age: the female side. Rev Epidemiol Sante Publique. 2005;53 Spec No 2:2S37-45.
Ottolenghi C, Uda M, Hamatani T, Crisponi L, Garcia JE, Ko M, Pilia G, Sforza C, Schlessinger D, Forabosco A. Aging of oocyte, ovary, and human reproduction. Ann N Y Acad Sci. 2004;1034:117–31.
Ruman J, Klein J, Sauer MV. Understanding the effects of age on female fertility. Minerva Ginecol. 2003;55:117–27.
Wang T, Zhang M, Jiang Z, Seli E. Mitochondrial dysfunction and ovarian aging. Am J Reprod Immunol. 2017;77:e12651.
Liochev SI. Reactive oxygen species and the free radical theory of aging. Free Radic Biol Med. 2013;60:1–4.
Nejabati HR, Schmeisser K, Shahnazi V, Samimifar D, Faridvand Y, Bahrami-Asl Z, Fathi-Maroufi N, Nikanfar S, Nouri M. N1-methylnicotinamide: an anti-ovarian aging hormetin? Ageing Res Rev. 2020;62:101131.
Timoteo-Ferreira F, Abreu D, Mendes S, Matos L, Rodrigues AR, Almeida H, Silva E. Redox imbalance in age-related ovarian dysfunction and perspectives for its prevention. Ageing Res Rev. 2021;68:101345.
Zhang H, Davies KJA, Forman HJ. Oxidative stress response and Nrf2 signaling in aging. Free Radic Biol Med. 2015;88:314–36.
Liguori I, Russo G, Curcio F, Bulli G, Aran L, Della-Morte D, Gargiulo G, Testa G, Cacciatore F, Bonaduce D, et al. Oxidative stress, aging, and diseases. Clin Interv Aging. 2018;13:757–72.
Lu J, Wang Z, Cao J, Chen Y, Dong Y. A novel and compact review on the role of oxidative stress in female reproduction. Reprod Biol Endocrinol. 2018;16:80.
Rizzo A, Roscino MT, Binetti F, Sciorsci RL. Roles of reactive oxygen species in female reproduction. Reprod Domest Anim. 2012;47:344–52.
Dizdaroglu M, Jaruga P. Mechanisms of free radical-induced damage to DNA. Free Radic Res. 2012;46:382–419.
Kamat PK, Kalani A, Rai S, Swarnkar S, Tota S, Nath C, Tyagi N. Mechanism of oxidative stress and synapse dysfunction in the pathogenesis of Alzheimer’s disease: understanding the therapeutics strategies. Mol Neurobiol. 2016;53:648–61.
Peters AE, Mihalas BP, Bromfield EG, Roman SD, Nixon B, Sutherland JM. Autophagy in female fertility: a role in oxidative stress and aging. Antioxid Redox Signal. 2020;32:550–68.
Sasaki H, Hamatani T, Kamijo S, Iwai M, Kobanawa M, Ogawa S, Miyado K, Tanaka M. Impact of oxidative stress on age-associated decline in oocyte developmental competence. Front Endocrinol (Lausanne). 2019;10:811.
Takeo S, Kimura K, Shirasuna K, Kuwayama T, Iwata H. Age-associated deterioration in follicular fluid induces a decline in bovine oocyte quality. Reprod Fertil Dev. 2017;29:759–67.
Carbone MC, Tatone C, Delle Monache S, Marci R, Caserta D, Colonna R, Amicarelli F. Antioxidant enzymatic defences in human follicular fluid: characterization and age-dependent changes. Mol Hum Reprod. 2003;9:639–43.
Fridovich I. Biological effects of the superoxide radical. Arch Biochem Biophys. 1986;247:1–11.
Scandalios JG. Oxidative stress: molecular perception and transduction of signals triggering antioxidant gene defenses. Braz J Med Biol Res. 2005;38:995–1014.
Zelko IN, Mariani TJ, Folz RJ. Superoxide dismutase multigene family: a comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free Radic Biol Med. 2002;33:337–49.
Wang S, Zheng Y, Li J, Yu Y, Zhang W, Song M, Liu Z, Min Z, Hu H, Jing Y, et al. Single-cell transcriptomic Atlas of primate ovarian aging. Cell. 2020;180:585-600 e519.
Prasad S, Tiwari M, Pandey AN, Shrivastav TG, Chaube SK. Impact of stress on oocyte quality and reproductive outcome. J Biomed Sci. 2016;23:36.
Sohel MMH, Akyuz B, Konca Y, Arslan K, Sariozkan S, Cinar MU. Oxidative stress modulates the expression of apoptosis-associated microRNAs in bovine granulosa cells in vitro. Cell Tissue Res. 2019;376:295–308.
Yang H, Xie Y, Yang D, Ren D. Oxidative stress-induced apoptosis in granulosa cells involves JNK, p53 and Puma. Oncotarget. 2017;8:25310–22.
Tang Z, Chen J, Zhang Z, Bi J, Xu R, Lin Q, Wang Z. HIF-1alpha activation promotes luteolysis by enhancing ROS levels in the corpus luteum of pseudopregnant rats. Oxid Med Cell Longev. 2021;2021:1764929.
Vu HV, Lee S, Acosta TJ, Yoshioka S, Abe H, Okuda K. Roles of prostaglandin F2alpha and hydrogen peroxide in the regulation of Copper/Zinc superoxide dismutase in bovine corpus luteum and luteal endothelial cells. Reprod Biol Endocrinol. 2012;10:87.
Cajas YN, Canon-Beltran K, Ladron de Guevara M, Millan de la Blanca MG, Ramos-Ibeas P, Gutierrez-Adan A, Rizos D, Gonzalez EM. Antioxidant nobiletin enhances oocyte maturation and subsequent embryo development and quality. Int J Mol Sci. 2020;21:5340.
Yong W, Ma H, Na M, Gao T, Zhang Y, Hao L, Yu H, Yang H, Deng X. Roles of melatonin in the field of reproductive medicine. Biomed Pharmacother. 2021;144:112001.
Cheng EH, Chen SU, Lee TH, Pai YP, Huang LS, Huang CC, Lee MS. Evaluation of telomere length in cumulus cells as a potential biomarker of oocyte and embryo quality. Hum Reprod. 2013;28:929–36.
Erusalimsky JD. Oxidative stress, telomeres and cellular senescence: what non-drug interventions might break the link? Free Radic Biol Med. 2020;150:87–95.
Yamada-Fukunaga T, Yamada M, Hamatani T, Chikazawa N, Ogawa S, Akutsu H, Miura T, Miyado K, Tarin JJ, Kuji N, et al. Age-associated telomere shortening in mouse oocytes. Reprod Biol Endocrinol. 2013;11:108.
Perkins GA, Frey TG. Recent structural insight into mitochondria gained by microscopy. Micron. 2000;31:97–111.
Kaarniranta K, Pawlowska E, Szczepanska J, Jablkowska A, Blasiak J. Role of mitochondrial DNA damage in ROS-mediated pathogenesis of Age-Related Macular Degeneration (AMD). Int J Mol Sci. 2019;20:2374.
Kauppila TES, Kauppila JHK, Larsson NG. Mammalian mitochondria and aging: an update. Cell Metab. 2017;25:57–71.
Scialo F, Fernandez-Ayala DJ, Sanz A. Role of mitochondrial reverse electron transport in ROS signaling: potential roles in health and disease. Front Physiol. 2017;8:428.
Caston RA, Demple B. Risky repair: DNA-protein crosslinks formed by mitochondrial base excision DNA repair enzymes acting on free radical lesions. Free Radic Biol Med. 2017;107:146–50.
Yang SG, Park HJ, Kim JW, Jung JM, Kim MJ, Jegal HG, Kim IS, Kang MJ, Wee G, Yang HY, et al. Mito-TEMPO improves development competence by reducing superoxide in preimplantation porcine embryos. Sci Rep. 2018;8:10130.
Ross JM, Coppotelli G, Hoffer BJ, Olson L. Maternally transmitted mitochondrial DNA mutations can reduce lifespan. Sci Rep. 2014;4:6569.
Yang L, Lin X, Tang H, Fan Y, Zeng S, Jia L, Li Y, Shi Y, He S, Wang H, et al. Mitochondrial DNA mutation exacerbates female reproductive aging via impairment of the NADH/NAD(+) redox. Aging Cell. 2020;19:e13206.
Pasquariello R, Ermisch AF, Silva E, McCormick S, Logsdon D, Barfield JP, Schoolcraft WB, Krisher RL. Alterations in oocyte mitochondrial number and function are related to spindle defects and occur with maternal aging in mice and humansdagger. Biol Reprod. 2019;100:971–81.
Oktay K, Baltaci V, Sonmezer M, Turan V, Unsal E, Baltaci A, Aktuna S, Moy F. Oogonial precursor cell-derived autologous mitochondria injection to improve outcomes in women with multiple IVF failures due to low oocyte quality: a clinical translation. Reprod Sci. 2015;22:1612–7.
Srirattana K, St John JC. Additional mitochondrial DNA influences the interactions between the nuclear and mitochondrial genomes in a bovine embryo model of nuclear transfer. Sci Rep. 2018;8:7246.
Ge ZJ, Zhang CL, Schatten H, Sun QY. Maternal diabetes mellitus and the origin of non-communicable diseases in offspring: the role of epigenetics. Biol Reprod. 2014;90:139.
Hamatani T, Falco G, Carter MG, Akutsu H, Stagg CA, Sharov AA, Dudekula DB, VanBuren V, Ko MS. Age-associated alteration of gene expression patterns in mouse oocytes. Hum Mol Genet. 2004;13:2263–78.
Uysal F, Ozturk S. The loss of global DNA methylation due to decreased DNMT expression in the postnatal mouse ovaries may associate with infertility emerging during ovarian aging. Histochem Cell Biol. 2020;154:301–14.
Yue MX, Fu XW, Zhou GB, Hou YP, Du M, Wang L, Zhu SE. Abnormal DNA methylation in oocytes could be associated with a decrease in reproductive potential in old mice. J Assist Reprod Genet. 2012;29:643–50.
Manosalva I, Gonzalez A. Aging changes the chromatin configuration and histone methylation of mouse oocytes at germinal vesicle stage. Theriogenology. 2010;74:1539–47.
Akiyama T, Nagata M, Aoki F. Inadequate histone deacetylation during oocyte meiosis causes aneuploidy and embryo death in mice. Proc Natl Acad Sci U S A. 2006;103:7339–44.
van den Berg IM, Eleveld C, van der Hoeven M, Birnie E, Steegers EA, Galjaard RJ, Laven JS, van Doorninck JH. Defective deacetylation of histone 4 K12 in human oocytes is associated with advanced maternal age and chromosome misalignment. Hum Reprod. 2011;26:1181–90.
Abramov R, Fu G, Zhang Y, Peng C. Expression and regulation of miR-17a and miR-430b in zebrafish ovarian follicles. Gen Comp Endocrinol. 2013;188:309–15.
Sohel MM, Hoelker M, Noferesti SS, Salilew-Wondim D, Tholen E, Looft C, Rings F, Uddin MJ, Spencer TE, Schellander K, et al. Exosomal and non-exosomal transport of extra-cellular microRNAs in follicular fluid: implications for bovine oocyte developmental competence. PLoS One. 2013;8:e78505.
Yang S, Wang S, Luo A, Ding T, Lai Z, Shen W, Ma X, Cao C, Shi L, Jiang J, et al. Expression patterns and regulatory functions of microRNAs during the initiation of primordial follicle development in the neonatal mouse ovary. Biol Reprod. 2013;89:126.
Zhang H, Jiang X, Zhang Y, Xu B, Hua J, Ma T, Zheng W, Sun R, Shen W, Cooke HJ, et al. microRNA 376a regulates follicle assembly by targeting Pcna in fetal and neonatal mouse ovaries. Reproduction. 2014;148:43–54.
Dhahbi JM, Chen JW, Bhupathy S, Atamna H, Cavalcante MB, Saccon TD, Nunes ADC, Mason JB, Schneider A, Masternak MM. Specific PIWI-interacting RNAs and related small noncoding RNAs are associated with ovarian aging in ames dwarf (df/df) mice. J Gerontol A Biol Sci Med Sci. 2021;76:1561–70.
Zhang D, Lv J, Tang R, Feng Y, Zhao Y, Fei X, Chian R, Xie Q. Association of exosomal microRNAs in human ovarian follicular fluid with oocyte quality. Biochem Biophys Res Commun. 2021;534:468–73.
Kujjo LL, Perez GI. Ceramide and mitochondrial function in aging oocytes: joggling a new hypothesis and old players. Reproduction. 2012;143:1–10.
Perez GI, Jurisicova A, Matikainen T, Moriyama T, Kim MR, Takai Y, Pru JK, Kolesnick RN, Tilly JL. A central role for ceramide in the age-related acceleration of apoptosis in the female germline. FASEB J. 2005;19:860–2.
Perez GI, Tilly JL. Cumulus cells are required for the increased apoptotic potential in oocytes of aged mice. Hum Reprod. 1997;12:2781–3.
Zhu J, Lin FH, Zhang J, Lin J, Li H, Li YW, Tan XW, Tan JH. The signaling pathways by which the Fas/FasL system accelerates oocyte aging. Aging (Albany NY). 2016;8:291–303.
Zhu J, Zhang J, Li H, Wang TY, Zhang CX, Luo MJ, Tan JH. Cumulus cells accelerate oocyte aging by releasing soluble Fas ligand in mice. Sci Rep. 2015;5:8683.
Vanderhyden BC, Armstrong DT. Role of cumulus cells and serum on the in vitro maturation, fertilization, and subsequent development of rat oocytes. Biol Reprod. 1989;40:720–8.
Fujino Y, Ozaki K, Yamamasu S, Ito F, Matsuoka I, Hayashi E, Nakamura H, Ogita S, Sato E, Inoue M. DNA fragmentation of oocytes in aged mice. Hum Reprod. 1996;11:1480–3.
Corn CM, Hauser-Kronberger C, Moser M, Tews G, Ebner T. Predictive value of cumulus cell apoptosis with regard to blastocyst development of corresponding gametes. Fertil Steril. 2005;84:627–33.
Arcos A, de Paola M, Gianetti D, Acuna D, Velasquez ZD, Miro MP, Toro G, Hinrichsen B, Munoz RI, Lin Y, et al. alpha-SNAP is expressed in mouse ovarian granulosa cells and plays a key role in folliculogenesis and female fertility. Sci Rep. 2017;7:11765.
Filali M, Frydman N, Belot MP, Hesters L, Gaudin F, Tachdjian G, Emilie D, Frydman R, Machelon V. Oocyte in-vitro maturation: BCL2 mRNA content in cumulus cells reflects oocyte competency. Reprod Biomed Online. 2009;19 Suppl 4:4309.
Chini CCS, Peclat TR, Warner GM, Kashyap S, Espindola-Netto JM, de Oliveira GC, Gomez LS, Hogan KA, Tarrago MG, Puranik AS, et al. CD38 ecto-enzyme in immune cells is induced during aging and regulates NAD(+) and NMN levels. Nat Metab. 2020;2:1284–304.
Covarrubias AJ, Kale A, Perrone R, Lopez-Dominguez JA, Pisco AO, Kasler HG, Schmidt MS, Heckenbach I, Kwok R, Wiley CD, et al. Senescent cells promote tissue NAD(+) decline during ageing via the activation of CD38(+) macrophages. Nat Metab. 2020;2:1265–83.
Lliberos C, Liew SH, Zareie P, La Gruta NL, Mansell A, Hutt K. Evaluation of inflammation and follicle depletion during ovarian ageing in mice. Sci Rep. 2021;11:278.
Navarro-Pando JM, Alcocer-Gomez E, Castejon-Vega B, Navarro-Villaran E, Condes-Hervas M, Mundi-Roldan M, Muntane J, Perez-Pulido AJ, Bullon P, Wang C, et al. Inhibition of the NLRP3 inflammasome prevents ovarian aging. Sci Adv. 2021;7:eabc7409.
Snider AP, Wood JR. Obesity induces ovarian inflammation and reduces oocyte quality. Reproduction. 2019;158:R79–90.
Yang Z, Tang Z, Cao X, Xie Q, Hu C, Zhong Z, Tan J, Zheng Y. Controlling chronic low-grade inflammation to improve follicle development and survival. Am J Reprod Immunol. 2020;84:e13265.
Duffy DM, Ko C, Jo M, Brannstrom M, Curry TE. Ovulation: parallels with inflammatory processes. Endocr Rev. 2019;40:369–416.
Huang Y, Hu C, Ye H, Luo R, Fu X, Li X, Huang J, Chen W, Zheng Y. Inflamm-aging: a new mechanism affecting premature ovarian insufficiency. J Immunol Res. 2019;2019:8069898.
Madkour A, Bouamoud N, Louanjli N, Kaarouch I, Copin H, Benkhalifa M, Sefrioui O. Intrauterine insemination of cultured peripheral blood mononuclear cells prior to embryo transfer improves clinical outcome for patients with repeated implantation failures. Zygote. 2016;24:58–69.
Allanson B, Jennings B, Jacques A, Charles AK, Keil AD, Dickinson JE. Infection and fetal loss in the mid-second trimester of pregnancy. Aust N Z J Obstet Gynaecol. 2010;50:221–5.
Briley SM, Jasti S, McCracken JM, Hornick JE, Fegley B, Pritchard MT, Duncan FE. Reproductive age-associated fibrosis in the stroma of the mammalian ovary. Reproduction. 2016;152:245–60.
Foley KG, Pritchard MT, Duncan FE. Macrophage-derived multinucleated giant cells: hallmarks of the aging ovary. Reproduction. 2021;161:V5–9.
Zhang Z, Schlamp F, Huang L, Clark H, Brayboy L. Inflammaging is associated with shifted macrophage ontogeny and polarization in the aging mouse ovary. Reproduction. 2020;159:325–37.
He L, Ling L, Wei T, Wang Y, Xiong Z. Ginsenoside Rg1 improves fertility and reduces ovarian pathological damages in premature ovarian failure model of mice. Exp Biol Med (Maywood). 2017;242:683–91.
Lliberos C, Liew SH, Mansell A, Hutt KJ. The inflammasome contributes to depletion of the ovarian reserve during aging in mice. Front Cell Dev Biol. 2020;8:628473.
Said RS, El-Demerdash E, Nada AS, Kamal MM. Resveratrol inhibits inflammatory signaling implicated in ionizing radiation-induced premature ovarian failure through antagonistic crosstalk between silencing information regulator 1 (SIRT1) and poly(ADP-ribose) polymerase 1 (PARP-1). Biochem Pharmacol. 2016;103:140–50.
Desdin-Mico G, Soto-Heredero G, Aranda JF, Oller J, Carrasco E, Gabande-Rodriguez E, Blanco EM, Alfranca A, Cusso L, Desco M, et al. T cells with dysfunctional mitochondria induce multimorbidity and premature senescence. Science. 2020;368:1371–6.
Venkatesan S, Khaw AK, Hande MP. Telomere biology-insights into an intriguing phenomenon. Cells. 2017;6:15.
Zhang Y, Wang C, Jin Y, Yang Q, Meng Q, Liu Q, Dai Y, Cai L, Liu Z, Liu K, et al. Activating the PGC-1alpha/TERT pathway by catalpol ameliorates atherosclerosis via modulating ROS production, DNA damage, and telomere function: implications on mitochondria and telomere link. Oxid Med Cell Longev. 2018;2018:2876350.
Keefe D, Kumar M, Kalmbach K. Oocyte competency is the key to embryo potential. Fertil Steril. 2015;103:317–22.
Smith EM, Pendlebury DF, Nandakumar J. Structural biology of telomeres and telomerase. Cell Mol Life Sci. 2020;77:61–79.
Whittemore K, Vera E, Martinez-Nevado E, Sanpera C, Blasco MA. Telomere shortening rate predicts species life span. Proc Natl Acad Sci U S A. 2019;116:15122–7.
Greene AD, Patounakis G, Segars JH. Genetic associations with diminished ovarian reserve: a systematic review of the literature. J Assist Reprod Genet. 2014;31:935–46.
Butts S, Riethman H, Ratcliffe S, Shaunik A, Coutifaris C, Barnhart K. Correlation of telomere length and telomerase activity with occult ovarian insufficiency. J Clin Endocrinol Metab. 2009;94:4835–43.
Xu X, Chen X, Zhang X, Liu Y, Wang Z, Wang P, Du Y, Qin Y, Chen ZJ. Impaired telomere length and telomerase activity in peripheral blood leukocytes and granulosa cells in patients with biochemical primary ovarian insufficiency. Hum Reprod. 2017;32:201–7.
Turner S, Hartshorne GM. Telomere lengths in human pronuclei, oocytes and spermatozoa. Mol Hum Reprod. 2013;19:510–8.
Treff NR, Su J, Taylor D, Scott RT Jr. Telomere DNA deficiency is associated with development of human embryonic aneuploidy. PLoS Genet. 2011;7:e1002161.
Huang J, Okuka M, McLean M, Keefe DL, Liu L. Telomere susceptibility to cigarette smoke-induced oxidative damage and chromosomal instability of mouse embryos in vitro. Free Radic Biol Med. 2010;48:1663–76.
Liu J, Liu M, Ye X, Liu K, Huang J, Wang L, Ji G, Liu N, Tang X, Baltz JM, et al. Delay in oocyte aging in mice by the antioxidant N-acetyl-L-cysteine (NAC). Hum Reprod. 2012;27:1411–20.
Harden A, Young WJ. The alcoholic ferment of yeast-juice. Proc R Soc London Ser B Contain Papers Biol Charact. 1906;77:405–20.
von Euler H, Myrbäck K. Co-Zymase. XVII. Biol Chem. 1930;190(3–6):93–100.
Warburg O, Christian W. Pyridin, der wasserstoffübertragende Bestandteil von Gärungsfermenten. Helv Chim Acta. 1936;19:E79–88.
Sahar S, Nin V, Barbosa MT, Chini EN, Sassone-Corsi P. Altered behavioral and metabolic circadian rhythms in mice with disrupted NAD+ oscillation. Aging (Albany NY). 2011;3:794–802.
Coleman MP, Hoke A. Programmed axon degeneration: from mouse to mechanism to medicine. Nat Rev Neurosci. 2020;21:183–96.
Zhan T, Xiong H, Pang J, Zhang W, Ye Y, Liang Z, Huang X, He F, Jian B, He W, et al. Modulation of NAD(+) biosynthesis activates SIRT1 and resists cisplatin-induced ototoxicity. Toxicol Lett. 2021;349:115–23.
Hogan KA, Chini CCS, Chini EN. The multi-faceted ecto-enzyme CD38: roles in immunomodulation, cancer, aging, and metabolic diseases. Front Immunol. 2019;10:1187.
Piedra-Quintero ZL, Wilson Z, Nava P, Guerau-de-Arellano M. CD38: an immunomodulatory molecule in inflammation and autoimmunity. Front Immunol. 2020;11:597959.
Xu C, Wang L, Fozouni P, Evjen G, Chandra V, Jiang J, Lu C, Nicastri M, Bretz C, Winkler JD, et al. SIRT1 is downregulated by autophagy in senescence and ageing. Nat Cell Biol. 2020;22:1170–9.
Cambronne XA, Stewart ML, Kim D, Jones-Brunette AM, Morgan RK, Farrens DL, Cohen MS, Goodman RH. Biosensor reveals multiple sources for mitochondrial NAD(+). Science. 2016;352:1474–7.
Houtkooper RH, Canto C, Wanders RJ, Auwerx J. The secret life of NAD+: an old metabolite controlling new metabolic signaling pathways. Endocr Rev. 2010;31:194–223.
Menzies KJ, Zhang H, Katsyuba E, Auwerx J. Protein acetylation in metabolism - metabolites and cofactors. Nat Rev Endocrinol. 2016;12:43–60.
Davila A, Liu L, Chellappa K, Redpath P, Nakamaru-Ogiso E, Paolella LM, Zhang Z, Migaud ME, Rabinowitz JD, Baur JA. Nicotinamide adenine dinucleotide is transported into mammalian mitochondria. Elife. 2018;7:e33246.
Brown K, Xie S, Qiu X, Mohrin M, Shin J, Liu Y, Zhang D, Scadden DT, Chen D. SIRT3 reverses aging-associated degeneration. Cell Rep. 2013;3:319–27.
Canto C, Houtkooper RH, Pirinen E, Youn DY, Oosterveer MH, Cen Y, Fernandez-Marcos PJ, Yamamoto H, Andreux PA, Cettour-Rose P, et al. The NAD(+) precursor nicotinamide riboside enhances oxidative metabolism and protects against high-fat diet-induced obesity. Cell Metab. 2012;15:838–47.
Nikiforov A, Dolle C, Niere M, Ziegler M. Pathways and subcellular compartmentation of NAD biosynthesis in human cells: from entry of extracellular precursors to mitochondrial NAD generation. J Biol Chem. 2011;286:21767–78.
Cambronne XA, Kraus WL. Location, location, location: compartmentalization of NAD(+) synthesis and functions in mammalian cells. Trends Biochem Sci. 2020;45:858–73.
Araki T, Sasaki Y, Milbrandt J. Increased nuclear NAD biosynthesis and SIRT1 activation prevent axonal degeneration. Science. 2004;305:1010–3.
Dobrovolsky VN, Bowyer JF, Pabarcus MK, Heflich RH, Williams LD, Doerge DR, Arvidsson B, Bergquist J, Casida JE. Effect of arylformamidase (kynurenine formamidase) gene inactivation in mice on enzymatic activity, kynurenine pathway metabolites and phenotype. Biochim Biophys Acta. 2005;1724:163–72.
Fletcher RS, Ratajczak J, Doig CL, Oakey LA, Callingham R, Da Silva Xavier G, Garten A, Elhassan YS, Redpath P, Migaud ME, et al. Nicotinamide riboside kinases display redundancy in mediating nicotinamide mononucleotide and nicotinamide riboside metabolism in skeletal muscle cells. Mol Metab. 2017;6:819–32.
Mori V, Amici A, Mazzola F, Di Stefano M, Conforti L, Magni G, Ruggieri S, Raffaelli N, Orsomando G. Metabolic profiling of alternative NAD biosynthetic routes in mouse tissues. PLoS One. 2014;9:e113939.
Pucci L, Perozzi S, Cimadamore F, Orsomando G, Raffaelli N. Tissue expression and biochemical characterization of human 2-amino 3-carboxymuconate 6-semialdehyde decarboxylase, a key enzyme in tryptophan catabolism. FEBS J. 2007;274:827–40.
Krishnaswamy K, Bapurao S. Effect of leucine at different levels of pyridoxine on hepatic quinolinate phosphoribosyl transferase (EC 2.4.2.19) and leucine aminotransferase (EC 2.6.1.6) in rats. Br J Nutr. 1978;39:61–4.
de Figueiredo LF, Gossmann TI, Ziegler M, Schuster S. Pathway analysis of NAD+ metabolism. Biochem J. 2011;439:341–8.
Zalkin H. NAD synthetase. Methods Enzymol. 1985;113:297–302.
Trammell SA, Yu L, Redpath P, Migaud ME, Brenner C. Nicotinamide riboside is a major NAD+ precursor vitamin in cow milk. J Nutr. 2016;146:957–63.
Revollo JR, Grimm AA, Imai S. The NAD biosynthesis pathway mediated by nicotinamide phosphoribosyltransferase regulates Sir2 activity in mammalian cells. J Biol Chem. 2004;279:50754–63.
Berger F, Lau C, Dahlmann M, Ziegler M. Subcellular compartmentation and differential catalytic properties of the three human nicotinamide mononucleotide adenylyltransferase isoforms. J Biol Chem. 2005;280:36334–41.
Kitani T, Okuno S, Fujisawa H. Growth phase-dependent changes in the subcellular localization of pre-B-cell colony-enhancing factor. FEBS Lett. 2003;544:74–8.
Yang H, Yang T, Baur JA, Perez E, Matsui T, Carmona JJ, Lamming DW, Souza-Pinto NC, Bohr VA, Rosenzweig A, et al. Nutrient-sensitive mitochondrial NAD+ levels dictate cell survival. Cell. 2007;130:1095–107.
Masri S, Rigor P, Cervantes M, Ceglia N, Sebastian C, Xiao C, Roqueta-Rivera M, Deng C, Osborne TF, Mostoslavsky R, et al. Partitioning circadian transcription by SIRT6 leads to segregated control of cellular metabolism. Cell. 2014;158:659–72.
Ramsey KM, Yoshino J, Brace CS, Abrassart D, Kobayashi Y, Marcheva B, Hong HK, Chong JL, Buhr ED, Lee C, et al. Circadian clock feedback cycle through NAMPT-mediated NAD+ biosynthesis. Science. 2009;324:651–4.
Rappou E, Jukarainen S, Rinnankoski-Tuikka R, Kaye S, Heinonen S, Hakkarainen A, Lundbom J, Lundbom N, Saunavaara V, Rissanen A, et al. Weight loss is associated with increased NAD(+)/SIRT1 expression but reduced PARP activity in white adipose tissue. J Clin Endocrinol Metab. 2016;101:1263–73.
Emanuelli M, Carnevali F, Saccucci F, Pierella F, Amici A, Raffaelli N, Magni G. Molecular cloning, chromosomal localization, tissue mRNA levels, bacterial expression, and enzymatic properties of human NMN adenylyltransferase. J Biol Chem. 2001;276:406–12.
Yalowitz JA, Xiao S, Biju MP, Antony AC, Cummings OW, Deeg MA, Jayaram HN. Characterization of human brain nicotinamide 5’-mononucleotide adenylyltransferase-2 and expression in human pancreas. Biochem J. 2004;377:317–26.
Zhang X, Kurnasov OV, Karthikeyan S, Grishin NV, Osterman AL, Zhang H. Structural characterization of a human cytosolic NMN/NaMN adenylyltransferase and implication in human NAD biosynthesis. J Biol Chem. 2003;278:13503–11.
Bieganowski P, Brenner C. Discoveries of nicotinamide riboside as a nutrient and conserved NRK genes establish a Preiss-Handler independent route to NAD+ in fungi and humans. Cell. 2004;117:495–502.
Imai S, Armstrong CM, Kaeberlein M, Guarente L. Transcriptional silencing and longevity protein Sir2 is an NAD-dependent histone deacetylase. Nature. 2000;403:795–800.
Landry J, Sutton A, Tafrov ST, Heller RC, Stebbins J, Pillus L, Sternglanz R. The silencing protein SIR2 and its homologs are NAD-dependent protein deacetylases. Proc Natl Acad Sci U S A. 2000;97:5807–11.
Houtkooper RH, Pirinen E, Auwerx J. Sirtuins as regulators of metabolism and healthspan. Nat Rev Mol Cell Biol. 2012;13:225–38.
Kim W, Deik A, Gonzalez C, Gonzalez ME, Fu F, Ferrari M, Churchhouse CL, Florez JC, Jacobs SBR, Clish CB, et al. Polyunsaturated fatty acid desaturation is a mechanism for glycolytic NAD(+) recycling. Cell Metab. 2019;29:856-870 e857.
Bai P, Canto C. The role of PARP-1 and PARP-2 enzymes in metabolic regulation and disease. Cell Metab. 2012;16:290–5.
Boehler C, Gauthier LR, Mortusewicz O, Biard DS, Saliou JM, Bresson A, Sanglier-Cianferani S, Smith S, Schreiber V, Boussin F, et al. Poly(ADP-ribose) polymerase 3 (PARP3), a newcomer in cellular response to DNA damage and mitotic progression. Proc Natl Acad Sci U S A. 2011;108:2783–8.
Ame JC, Rolli V, Schreiber V, Niedergang C, Apiou F, Decker P, Muller S, Hoger T, Menissier-de Murcia J, de Murcia G. PARP-2, A novel mammalian DNA damage-dependent poly(ADP-ribose) polymerase. J Biol Chem. 1999;274:17860–8.
Mendoza-Alvarez H, Alvarez-Gonzalez R. Poly(ADP-ribose) polymerase is a catalytic dimer and the automodification reaction is intermolecular. J Biol Chem. 1993;268:22575–80.
Malavasi F, Deaglio S, Funaro A, Ferrero E, Horenstein AL, Ortolan E, Vaisitti T, Aydin S. Evolution and function of the ADP ribosyl cyclase/CD38 gene family in physiology and pathology. Physiol Rev. 2008;88:841–86.
Yang D, Elner SG, Chen X, Field MG, Petty HR, Elner VM. MCP-1-activated monocytes induce apoptosis in human retinal pigment epithelium. Invest Ophthalmol Vis Sci. 2011;52:6026–34.
Aomatsu E, Takahashi N, Sawada S, Okubo N, Hasegawa T, Taira M, Miura H, Ishisaki A, Chosa N. Novel SCRG1/BST1 axis regulates self-renewal, migration, and osteogenic differentiation potential in mesenchymal stem cells. Sci Rep. 2014;4:3652.
Camacho-Pereira J, Tarrago MG, Chini CCS, Nin V, Escande C, Warner GM, Puranik AS, Schoon RA, Reid JM, Galina A, et al. CD38 dictates age-related NAD decline and mitochondrial dysfunction through an SIRT3-dependent mechanism. Cell Metab. 2016;23:1127–39.
Preugschat F, Carter LH, Boros EE, Porter DJ, Stewart EL, Shewchuk LM. A pre-steady state and steady state kinetic analysis of the N-ribosyl hydrolase activity of hCD157. Arch Biochem Biophys. 2014;564:156–63.
Chillemi A, Zaccarello G, Quarona V, Ferracin M, Ghimenti C, Massaia M, Horenstein AL, Malavasi F. Anti-CD38 antibody therapy: windows of opportunity yielded by the functional characteristics of the target molecule. Mol Med. 2013;19:99–108.
Aksoy P, Escande C, White TA, Thompson M, Soares S, Benech JC, Chini EN. Regulation of SIRT 1 mediated NAD dependent deacetylation: a novel role for the multifunctional enzyme CD38. Biochem Biophys Res Commun. 2006;349:353–9.
Escande C, Nin V, Price NL, Capellini V, Gomes AP, Barbosa MT, O’Neil L, White TA, Sinclair DA, Chini EN. Flavonoid apigenin is an inhibitor of the NAD+ ase CD38: implications for cellular NAD+ metabolism, protein acetylation, and treatment of metabolic syndrome. Diabetes. 2013;62:1084–93.
Ortolan E, Augeri S, Fissolo G, Musso I, Funaro A. CD157: From immunoregulatory protein to potential therapeutic target. Immunol Lett. 2019;205:59–64.
Figley MD, Gu W, Nanson JD, Shi Y, Sasaki Y, Cunnea K, Malde AK, Jia X, Luo Z, Saikot FK, et al. SARM1 is a metabolic sensor activated by an increased NMN/NAD(+) ratio to trigger axon degeneration. Neuron. 2021;109:1118-1136 e1111.
Gerdts J, Brace EJ, Sasaki Y, DiAntonio A, Milbrandt J. SARM1 activation triggers axon degeneration locally via NAD(+) destruction. Science. 2015;348:453–7.
Jiao X, Doamekpor SK, Bird JG, Nickels BE, Tong L, Hart RP, Kiledjian M. 5’ end nicotinamide adenine dinucleotide cap in human cells promotes RNA decay through DXO-mediated deNADding. Cell. 2017;168:1015-1027 e1010.
Niu K, Zhang J, Ge S, Li D, Sun K, You Y, et al. ONE-seq: epitranscriptome and gene-specific profiling of NAD-capped RNA. Nucleic Acids Res. 2023;51(2):e12.
Katsyuba E, Romani M, Hofer D, Auwerx J. NAD(+) homeostasis in health and disease. Nat Metab. 2020;2:9–31.
Ear PH, Chadda A, Gumusoglu SB, Schmidt MS, Vogeler S, Malicoat J, Kadel J, Moore MM, Migaud ME, Stevens HE, et al. Maternal nicotinamide riboside enhances postpartum weight loss, juvenile offspring development, and neurogenesis of adult offspring. Cell Rep. 2019;26:969-983 e964.
Liu Y, Zhong W, Li X, Shen F, Ma X, Yang Q, Hong S, Sun Y. Diets, gut microbiota and metabolites. Phenomics. 2023;3:268–84.
Yoshino J, Mills KF, Yoon MJ, Imai S. Nicotinamide mononucleotide, a key NAD(+) intermediate, treats the pathophysiology of diet- and age-induced diabetes in mice. Cell Metab. 2011;14:528–36.
Goodman RP, Markhard AL, Shah H, Sharma R, Skinner OS, Clish CB, Deik A, Patgiri A, Hsu YH, Masia R, et al. Hepatic NADH reductive stress underlies common variation in metabolic traits. Nature. 2020;583:122–6.
Szanto M, Bai P. The role of ADP-ribose metabolism in metabolic regulation, adipose tissue differentiation, and metabolism. Genes Dev. 2020;34:321–40.
Tarrago MG, Chini CCS, Kanamori KS, Warner GM, Caride A, de Oliveira GC, Rud M, Samani A, Hein KZ, Huang R, et al. A potent and specific CD38 inhibitor ameliorates age-related metabolic dysfunction by reversing tissue NAD(+) decline. Cell Metab. 2018;27:1081-1095 e1010.
Stromsdorfer KL, Yamaguchi S, Yoon MJ, Moseley AC, Franczyk MP, Kelly SC, Qi N, Imai S, Yoshino J. NAMPT-mediated NAD(+) biosynthesis in adipocytes regulates adipose tissue function and multi-organ insulin sensitivity in mice. Cell Rep. 2016;16:1851–60.
Smith JS, Brachmann CB, Celic I, Kenna MA, Muhammad S, Starai VJ, Avalos JL, Escalante-Semerena JC, Grubmeyer C, Wolberger C, et al. A phylogenetically conserved NAD+-dependent protein deacetylase activity in the Sir2 protein family. Proc Natl Acad Sci U S A. 2000;97:6658–63.
Hirschey MD, Shimazu T, Goetzman E, Jing E, Schwer B, Lombard DB, Grueter CA, Harris C, Biddinger S, Ilkayeva OR, et al. SIRT3 regulates mitochondrial fatty-acid oxidation by reversible enzyme deacetylation. Nature. 2010;464:121–5.
Lagouge M, Argmann C, Gerhart-Hines Z, Meziane H, Lerin C, Daussin F, Messadeq N, Milne J, Lambert P, Elliott P, et al. Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1alpha. Cell. 2006;127:1109–22.
Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017;542:177–85.
Pathria P, Louis TL, Varner JA. Targeting tumor-associated macrophages in cancer. Trends Immunol. 2019;40:310–27.
Chini C, Hogan KA, Warner GM, Tarrago MG, Peclat TR, Tchkonia T, Kirkland JL, Chini E. The NADase CD38 is induced by factors secreted from senescent cells providing a potential link between senescence and age-related cellular NAD(+) decline. Biochem Biophys Res Commun. 2019;513:486–93.
Minhas PS, Liu L, Moon PK, Joshi AU, Dove C, Mhatre S, Contrepois K, Wang Q, Lee BA, Coronado M, et al. Macrophage de novo NAD(+) synthesis specifies immune function in aging and inflammation. Nat Immunol. 2019;20:50–63.
Hubert S, Rissiek B, Klages K, Huehn J, Sparwasser T, Haag F, Koch-Nolte F, Boyer O, Seman M, Adriouch S. Extracellular NAD+ shapes the Foxp3+ regulatory T cell compartment through the ART2-P2X7 pathway. J Exp Med. 2010;207:2561–8.
Elkhal A, Rodriguez Cetina Biefer H, Heinbokel T, Uehara H, Quante M, Seyda M, Schuitenmaker JM, Krenzien F, Camacho V, de la Fuente MA, et al. NAD(+) regulates Treg cell fate and promotes allograft survival via a systemic IL-10 production that is CD4(+) CD25(+) Foxp3(+) T cells independent. Sci Rep. 2016;6:22325.
Tullius SG, Biefer HR, Li S, Trachtenberg AJ, Edtinger K, Quante M, Krenzien F, Uehara H, Yang X, Kissick HT, et al. NAD+ protects against EAE by regulating CD4+ T-cell differentiation. Nat Commun. 2014;5:5101.
Berger NA. Poly(ADP-ribose) in the cellular response to DNA damage. Radiat Res. 1985;101:4–15.
Mouchiroud L, Houtkooper RH, Moullan N, Katsyuba E, Ryu D, Canto C, Mottis A, Jo YS, Viswanathan M, Schoonjans K, et al. The NAD(+)/Sirtuin pathway modulates longevity through activation of mitochondrial UPR and FOXO signaling. Cell. 2013;154:430–41.
Bai P, Canto C, Oudart H, Brunyanszki A, Cen Y, Thomas C, Yamamoto H, Huber A, Kiss B, Houtkooper RH, et al. PARP-1 inhibition increases mitochondrial metabolism through SIRT1 activation. Cell Metab. 2011;13:461–8.
Bian C, Zhang C, Luo T, Vyas A, Chen SH, Liu C, Kassab MA, Yang Y, Kong M, Yu X. NADP(+) is an endogenous PARP inhibitor in DNA damage response and tumor suppression. Nat Commun. 2019;10:693.
Hou Y, Lautrup S, Cordonnier S, Wang Y, Croteau DL, Zavala E, Zhang Y, Moritoh K, O’Connell JF, Baptiste BA, et al. NAD(+) supplementation normalizes key Alzheimer’s features and DNA damage responses in a new AD mouse model with introduced DNA repair deficiency. Proc Natl Acad Sci U S A. 2018;115:E1876–85.
Kraus WL. Transcriptional control by PARP-1: chromatin modulation, enhancer-binding, coregulation, and insulation. Curr Opin Cell Biol. 2008;20:294–302.
Lee MH, Na H, Kim EJ, Lee HW, Lee MO. Poly(ADP-ribosyl)ation of p53 induces gene-specific transcriptional repression of MTA1. Oncogene. 2012;31:5099–107.
Schiewer MJ, Knudsen KE. Transcriptional roles of PARP1 in cancer. Mol Cancer Res. 2014;12:1069–80.
Stanisavljevic J, Porta-de-la-Riva M, Batlle R, de Herreros AG, Baulida J. The p65 subunit of NF-kappaB and PARP1 assist Snail1 in activating fibronectin transcription. J Cell Sci. 2011;124:4161–71.
Haigis MC, Deng CX, Finley LW, Kim HS, Gius D. SIRT3 is a mitochondrial tumor suppressor: a scientific tale that connects aberrant cellular ROS, the Warburg effect, and carcinogenesis. Cancer Res. 2012;72:2468–72.
Tao R, Coleman MC, Pennington JD, Ozden O, Park SH, Jiang H, Kim HS, Flynn CR, Hill S, Hayes McDonald W, et al. Sirt3-mediated deacetylation of evolutionarily conserved lysine 122 regulates MnSOD activity in response to stress. Mol Cell. 2010;40:893–904.
Mao Z, Hine C, Tian X, Van Meter M, Au M, Vaidya A, Seluanov A, Gorbunova V. SIRT6 promotes DNA repair under stress by activating PARP1. Science. 2011;332:1443–6.
Jeong SM, Xiao C, Finley LW, Lahusen T, Souza AL, Pierce K, Li YH, Wang X, Laurent G, German NJ, et al. SIRT4 has tumor-suppressive activity and regulates the cellular metabolic response to DNA damage by inhibiting mitochondrial glutamine metabolism. Cancer Cell. 2013;23:450–63.
Huertas P. DNA resection in eukaryotes: deciding how to fix the break. Nat Struct Mol Biol. 2010;17:11–6.
Kaidi A, Weinert BT, Choudhary C, Jackson SP. Human SIRT6 promotes DNA end resection through CtIP deacetylation. Science. 2010;329:1348–53.
Das C, Lucia MS, Hansen KC, Tyler JK. CBP/p300-mediated acetylation of histone H3 on lysine 56. Nature. 2009;459:113–7.
Jing H, Lin H. Sirtuins in epigenetic regulation. Chem Rev. 2015;115:2350–75.
Kanfi Y, Naiman S, Amir G, Peshti V, Zinman G, Nahum L, Bar-Joseph Z, Cohen HY. The sirtuin SIRT6 regulates lifespan in male mice. Nature. 2012;483:218–21.
Peng L, Yuan Z, Ling H, Fukasawa K, Robertson K, Olashaw N, Koomen J, Chen J, Lane WS, Seto E. SIRT1 deacetylates the DNA methyltransferase 1 (DNMT1) protein and alters its activities. Mol Cell Biol. 2011;31:4720–34.
Nacarelli T, Lau L, Fukumoto T, Zundell J, Fatkhutdinov N, Wu S, Aird KM, Iwasaki O, Kossenkov AV, Schultz D, et al. NAD(+) metabolism governs the proinflammatory senescence-associated secretome. Nat Cell Biol. 2019;21:397–407.
Wu X, Hu F, Zeng J, Han L, Qiu D, Wang H, Ge J, Ying X, Wang Q. NMNAT2-mediated NAD(+) generation is essential for quality control of aged oocytes. Aging Cell. 2019;18:e12955.
Pan LZ, Ahn DG, Sharif T, Clements D, Gujar SA, Lee PW. The NAD+ synthesizing enzyme nicotinamide mononucleotide adenylyltransferase 2 (NMNAT-2) is a p53 downstream target. Cell Cycle. 2014;13:1041–8.
Di Emidio G, Falone S, Vitti M, D’Alessandro AM, Vento M, Di Pietro C, Amicarelli F, Tatone C. SIRT1 signalling protects mouse oocytes against oxidative stress and is deregulated during aging. Hum Reprod. 2014;29:2006–17.
Liu WJ, Zhang XM, Wang N, Zhou XL, Fu YC, Luo LL. Calorie restriction inhibits ovarian follicle development and follicle loss through activating SIRT1 signaling in mice. Eur J Med Res. 2015;20:22.
Ghafari F, Pelengaris S, Walters E, Hartshorne GM. Influence of p53 and genetic background on prenatal oogenesis and oocyte attrition in mice. Hum Reprod. 2009;24:1460–72.
Kim JM, Yoon YD, Tsang BK. Involvement of the Fas/Fas ligand system in p53-mediated granulosa cell apoptosis during follicular development and atresia. Endocrinology. 1999;140:2307–17.
Long GY, Yang JY, Xu JJ, Ni YH, Zhou XL, Ma JY, Fu YC, Luo LL. SIRT1 knock-in mice preserve ovarian reserve resembling caloric restriction. Gene. 2019;686:194–202.
Sun YC, Wang YY, Sun XF, Cheng SF, Li L, Zhao Y, Shen W, Chen H. The role of autophagy during murine primordial follicle assembly. Aging (Albany NY). 2018;10:197–211.
Ji Z, Liu GH, Qu J. Mitochondrial sirtuins, metabolism, and aging. J Genet Genomics. 2022;49:287–98.
Kawamura Y, Uchijima Y, Horike N, Tonami K, Nishiyama K, Amano T, Asano T, Kurihara Y, Kurihara H. Sirt3 protects in vitro-fertilized mouse preimplantation embryos against oxidative stress-induced p53-mediated developmental arrest. J Clin Invest. 2010;120:2817–28.
Yang F, Baumann C, De La Fuente R. Persistence of histone H2AX phosphorylation after meiotic chromosome synapsis and abnormal centromere cohesion in poly (ADP-ribose) polymerase (Parp-1) null oocytes. Dev Biol. 2009;331:326–38.
Li H, Wang H, Xu J, Zeng X, Sun Y, Yang Q. Nicotinamide riboside supplementation ameliorated post-ovulatory oocyte quality decline. Reproduction. 2023;165:103–11.
Perrone R, Ashok Kumaar PV, Haky L, Hahn C, Riley R, Balough J, Zaza G, Soygur B, Hung K, Prado L, et al. CD38 regulates ovarian function and fecundity via NAD(+) metabolism. iScience. 2023;26:107949.
Cheng HL, Mostoslavsky R, Saito S, Manis JP, Gu Y, Patel P, Bronson R, Appella E, Alt FW, Chua KF. Developmental defects and p53 hyperacetylation in Sir2 homolog (SIRT1)-deficient mice. Proc Natl Acad Sci U S A. 2003;100:10794–9.
North BJ, Marshall BL, Borra MT, Denu JM, Verdin E. The human Sir2 ortholog, SIRT2, is an NAD+-dependent tubulin deacetylase. Mol Cell. 2003;11:437–44.
Lee AR, Kishigami S, Amano T, Matsumoto K, Wakayama T, Hosoi Y. Nicotinamide: a class III HDACi delays in vitro aging of mouse oocytes. J Reprod Dev. 2013;59:238–44.
Riepsamen A, Wu L, Lau L, Listijono D, Ledger W, Sinclair D, Homer H. Nicotinamide impairs entry into and exit from meiosis I in mouse oocytes. PLoS One. 2015;10:e0126194.
Huang P, Zhou Y, Tang W, Ren C, Jiang A, Wang X, Qian X, Zhou Z, Gong A. Long-term treatment of Nicotinamide mononucleotide improved age-related diminished ovary reserve through enhancing the mitophagy level of granulosa cells in mice. J Nutr Biochem. 2022;101:108911.
Chaleckis R, Murakami I, Takada J, Kondoh H, Yanagida M. Individual variability in human blood metabolites identifies age-related differences. Proc Natl Acad Sci U S A. 2016;113:4252–9.
Yaku K, Okabe K, Nakagawa T. Simultaneous measurement of NAD metabolome in aged mice tissue using liquid chromatography tandem-mass spectrometry. Biomed Chromatogr. 2018;32:e4205.
Yoshino J, Baur JA, Imai SI. NAD(+) Intermediates: the biology and therapeutic potential of NMN and NR. Cell Metab. 2018;27:513–28.
Zhang H, Ryu D, Wu Y, Gariani K, Wang X, Luan P, D’Amico D, Ropelle ER, Lutolf MP, Aebersold R, et al. NAD(+) repletion improves mitochondrial and stem cell function and enhances life span in mice. Science. 2016;352:1436–43.
Schondorf DC, Ivanyuk D, Baden P, Sanchez-Martinez A, De Cicco S, Yu C, Giunta I, Schwarz LK, Di Napoli G, Panagiotakopoulou V, et al. The NAD+ precursor nicotinamide riboside rescues mitochondrial defects and neuronal loss in iPSC and Fly models of Parkinson’s disease. Cell Rep. 2018;23:2976–88.
Imai SI, Guarente L. It takes two to tango: NAD(+) and sirtuins in aging/longevity control. NPJ Aging Mech Dis. 2016;2:16017.
Elhassan YS, Kluckova K, Fletcher RS, Schmidt MS, Garten A, Doig CL, Cartwright DM, Oakey L, Burley CV, Jenkinson N, et al. Nicotinamide riboside augments the aged human skeletal muscle NAD(+) metabolome and induces transcriptomic and anti-inflammatory signatures. Cell Rep. 2019;28:1717-1728 e1716.
Trammell SA, Schmidt MS, Weidemann BJ, Redpath P, Jaksch F, Dellinger RW, Li Z, Abel ED, Migaud ME, Brenner C. Nicotinamide riboside is uniquely and orally bioavailable in mice and humans. Nat Commun. 2016;7:12948.
Lautrup S, Sinclair DA, Mattson MP, Fang EF. NAD(+) in brain aging and neurodegenerative disorders. Cell Metab. 2019;30:630–55.
Remie CME, Roumans KHM, Moonen MPB, Connell NJ, Havekes B, Mevenkamp J, Lindeboom L, de Wit VHW, van de Weijer T, Aarts S, et al. Nicotinamide riboside supplementation alters body composition and skeletal muscle acetylcarnitine concentrations in healthy obese humans. Am J Clin Nutr. 2020;112:413–26.
Chaudhuri RN, Chakravarti H. An outbreak of pellegra syndrome in a rural area of Bengal. Ind Med Gaz. 1947;82:657–60.
Goldberger J. Public Health Reports, June 26, 1914. The etiology of pellagra. The significance of certain epidemiological observations with respect thereto. Public Health Rep. 1975;90:373–5.
Nabokina SM, Kashyap ML, Said HM. Mechanism and regulation of human intestinal niacin uptake. Am J Physiol Cell Physiol. 2005;289:C97-103.
Said HM, Nabokina SM, Balamurugan K, Mohammed ZM, Urbina C, Kashyap ML. Mechanism of nicotinic acid transport in human liver cells: experiments with HepG2 cells and primary hepatocytes. Am J Physiol Cell Physiol. 2007;293:C1773-1778.
Grozio A, Mills KF, Yoshino J, Bruzzone S, Sociali G, Tokizane K, Lei HC, Cunningham R, Sasaki Y, Migaud ME, et al. Slc12a8 is a nicotinamide mononucleotide transporter. Nat Metab. 2019;1:47–57.
Menon RM, Gonzalez MA, Adams MH, Tolbert DS, Leu JH, Cefali EA. Effect of the rate of niacin administration on the plasma and urine pharmacokinetics of niacin and its metabolites. J Clin Pharmacol. 2007;47:681–8.
Dragovic J, Kim SH, Brown SL, Kim JH. Nicotinamide pharmacokinetics in patients. Radiother Oncol. 1995;36:225–8.
Pirinen E, Auranen M, Khan NA, Brilhante V, Urho N, Pessia A, Hakkarainen A, Kuula J, Heinonen U, Schmidt MS, et al. Niacin cures systemic NAD(+) deficiency and improves muscle performance in adult-onset mitochondrial myopathy. Cell Metab. 2020;31:1078-1090 e1075.
Ito TK, Sato T, Hakamata A, Onoda Y, Setou MJ. A nonrandomized study of single oral supplementation within the daily tolerable upper level of nicotinamide affects blood nicotinamide and NAD+ levels in healthy subjects. Transl Med Aging. 2020;4:45–54.
Stein LR, Imai S. Specific ablation of Nampt in adult neural stem cells recapitulates their functional defects during aging. EMBO J. 2014;33:1321–40.
Yoon MJ, Yoshida M, Johnson S, Takikawa A, Usui I, Tobe K, Nakagawa T, Yoshino J, Imai S. SIRT1-mediated eNAMPT secretion from adipose tissue regulates hypothalamic NAD+ and function in mice. Cell Metab. 2015;21:706–17.
Mills KF, Yoshida S, Stein LR, Grozio A, Kubota S, Sasaki Y, Redpath P, Migaud ME, Apte RS, Uchida K, et al. Long-Term administration of nicotinamide mononucleotide mitigates age-associated physiological decline in mice. Cell Metab. 2016;24:795–806.
Irie J, Inagaki E, Fujita M, Nakaya H, Mitsuishi M, Yamaguchi S, Yamashita K, Shigaki S, Ono T, Yukioka H, et al. Effect of oral administration of nicotinamide mononucleotide on clinical parameters and nicotinamide metabolite levels in healthy Japanese men. Endocr J. 2020;67:153–60.
Tatone C, Di Emidio G, Barbonetti A, Carta G, Luciano AM, Falone S, Amicarelli F. Sirtuins in gamete biology and reproductive physiology: emerging roles and therapeutic potential in female and male infertility. Hum Reprod Update. 2018;24:267–89.
Zhang J, Fang L, Lu Z, Xiong J, Wu M, Shi L, Luo A, Wang S. Are sirtuins markers of ovarian aging? Gene. 2016;575:680–6.
Fang EF, Hou Y, Lautrup S, Jensen MB, Yang B, SenGupta T, Caponio D, Khezri R, Demarest TG, Aman Y, et al. NAD(+) augmentation restores mitophagy and limits accelerated aging in Werner syndrome. Nat Commun. 2019;10:5284.
Dollerup OL, Christensen B, Svart M, Schmidt MS, Sulek K, Ringgaard S, Stodkilde-Jorgensen H, Moller N, Brenner C, Treebak JT, et al. A randomized placebo-controlled clinical trial of nicotinamide riboside in obese men: safety, insulin-sensitivity, and lipid-mobilizing effects. Am J Clin Nutr. 2018;108:343–53.
Conze D, Brenner C, Kruger CL. Safety and metabolism of long-term administration of NIAGEN (Nicotinamide Riboside Chloride) in a randomized, double-blind, placebo-controlled clinical trial of healthy overweight adults. Sci Rep. 2019;9:9772.
Benyo Z, Gille A, Kero J, Csiky M, Suchankova MC, Nusing RM, Moers A, Pfeffer K, Offermanns S. GPR109A (PUMA-G/HM74A) mediates nicotinic acid-induced flushing. J Clin Invest. 2005;115:3634–40.
Connell NJ, Grevendonk L, Fealy CE, Moonen-Kornips E, Bruls YMH, Schrauwen-Hinderling VB, de Vogel J, Hageman R, Geurts J, Zapata-Perez R, et al. NAD+-precursor supplementation with L-tryptophan, nicotinic acid, and nicotinamide does not affect mitochondrial function or skeletal muscle function in physically compromised older adults. J Nutr. 2021;151:2917–31.
Vreones M, Mustapic M, Moaddel R, Pucha KA, Lovett J, Seals DR, Kapogiannis D, Martens CR. Oral nicotinamide riboside raises NAD+ and lowers biomarkers of neurodegenerative pathology in plasma extracellular vesicles enriched for neuronal origin. Aging Cell. 2023;22:e13754.
Yi L, Maier AB, Tao R, Lin Z, Vaidya A, Pendse S, Thasma S, Andhalkar N, Avhad G, Kumbhar V. The efficacy and safety of beta-nicotinamide mononucleotide (NMN) supplementation in healthy middle-aged adults: a randomized, multicenter, double-blind, placebo-controlled, parallel-group, dose-dependent clinical trial. Geroscience. 2023;45:29–43.
Yoshino M, Yoshino J, Kayser BD, Patti GJ, Franczyk MP, Mills KF, Sindelar M, Pietka T, Patterson BW, Imai SI, et al. Nicotinamide mononucleotide increases muscle insulin sensitivity in prediabetic women. Science. 2021;372:1224–9.
Huang H. A multicentre, randomised, double blind, parallel design, placebo controlled study to evaluate the efficacy and safety of Uthever (NMN Supplement), an orally administered supplementation in middle aged and older adults. Front Aging. 2022;3:851698.
Dollerup OL, Trammell SAJ, Hartmann B, Holst JJ, Christensen B, Moller N, Gillum MP, Treebak JT, Jessen N. Effects of nicotinamide riboside on endocrine pancreatic function and incretin hormones in nondiabetic men with obesity. J Clin Endocrinol Metab. 2019;104:5703–14.
Dollerup OL, Chubanava S, Agerholm M, Sondergard SD, Altintas A, Moller AB, Hoyer KF, Ringgaard S, Stodkilde-Jorgensen H, Lavery GG, et al. Nicotinamide riboside does not alter mitochondrial respiration, content or morphology in skeletal muscle from obese and insulin-resistant men. J Physiol. 2020;598:731–54.
Abdellatif M, Trummer-Herbst V, Koser F, Durand S, Adao R, Vasques-Novoa F, Freundt JK, Voglhuber J, Pricolo MR, Kasa M, et al. Nicotinamide for the treatment of heart failure with preserved ejection fraction. Sci Transl Med. 2021b;13:eabd7064.
Ralto KM, Rhee EP, Parikh SM. NAD(+) homeostasis in renal health and disease. Nat Rev Nephrol. 2020;16:99–111.
Brachs S, Polack J, Brachs M, Jahn-Hofmann K, Elvert R, Pfenninger A, Barenz F, Margerie D, Mai K, Spranger J, et al. Genetic Nicotinamide N-Methyltransferase (Nnmt) deficiency in male mice improves insulin sensitivity in diet-induced obesity but does not affect glucose tolerance. Diabetes. 2019;68:527–42.
Covarrubias AJ, Perrone R, Grozio A, Verdin E. NAD(+) metabolism and its roles in cellular processes during ageing. Nat Rev Mol Cell Biol. 2021;22:119–41.
Eckert MA, Coscia F, Chryplewicz A, Chang JW, Hernandez KM, Pan S, Tienda SM, Nahotko DA, Li G, Blazenovic I, et al. Proteomics reveals NNMT as a master metabolic regulator of cancer-associated fibroblasts. Nature. 2019;569:723–8.
Disclosure of potential conflicts of interest
The authors declare no conflicts of interest.
Funding
This work was supported by (1) the National Natural Science Foundation of China (81871141 and 82201781); (2) the National High-Level Hospital Clinical Research Funding (2022-PUMCH-B-123); (3) the National Key Research and Development Program (2018YFC1004801).
Author information
Authors and Affiliations
Contributions
J.L. wrote the main manuscript text with the help of F.H., and Z.S. prepared figures with the help of R.T., P.Z., and R.C. supervised the project. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liang, J., Huang, F., Song, Z. et al. Impact of NAD+ metabolism on ovarian aging. Immun Ageing 20, 70 (2023). https://doi.org/10.1186/s12979-023-00398-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12979-023-00398-w