Abstract
Background
Antenatal screening for HIV, syphilis and HBV has been successfully implemented in The Netherlands, but data on other STI among pregnant women or male partners are limited. Our objectives: (i) to assess the prevalence of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG) and Trichomonas vaginalis (TV) among pregnant women and male partners, (ii) to identify risk factors for these STI during pregnancy, and (iii) to identify adverse perinatal outcomes (APO) associated with STI.
Methods
Cross-sectional study. Pregnant women aged ≤ 30 years (n = 548) and male partners (n = 425) were included at 30 midwifery practices during 2012–2016. Participants provided a self-collected vaginal swab (women) or urine sample (men) and completed a questionnaire. Perinatal data were derived from pregnancy cards. APO was defined as premature rupture of membranes, preterm delivery, low birthweight, stillbirth, neonatal conjunctival and respiratory infections. Data were analysed by logistic regression.
Results
STI were present in 2.4% of pregnant women (CT 1.8%, NG 0.4%, TV 0.4%), and in 2.2% of male partners (CT 2.2%, NG 0.2%, TV 0%). Of young women (≤ 20 years), 12.5% had a CT infection. Prevalent STI during pregnancy was associated with female young age (≤ 20 years vs ≥ 21 years) (adjusted OR 6.52, CI 95%: 1.11–38.33), male non-Western vs Western background (aOR 9.34, CI 2.34–37.21), and female with ≥ 2 sex partners < 12 months vs 0–1 (aOR 9.88, CI 2.08–46.91). APO was not associated with STI, but was associated with female low education (aOR 3.36, CI 1.12–10.09), complications with previous newborn (aOR 10.49, CI 3.21–34.25 vs no complications) and short duration (0–4 years) of relationship (aOR 2.75, CI 1.41–5.39 vs ≥ 5 years). Small-for-gestational-age was not associated with STI, but was associated with female low education (aOR 7.81, 2.01–30.27), female non-Western background (aOR 4.41, 1.74–11.17), and both parents smoking during pregnancy (aOR 2.94, 1.01–8.84 vs both non-smoking).
Conclusions
Prevalence of STI was low among pregnant women and male partners in midwifery practices, except for CT among young women. The study could not confirm previously observed associations between STI and APO, which is probably due to low prevalence of STI, small study sample, and presumed treatment for STI.
Plain language summary
Antenatal screening for HIV, syphilis and HBV has been successfully implemented in The Netherlands, but data on other STI among pregnant women or male partners are limited. Our objectives were: (i) to assess the prevalence of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG) and Trichomonas vaginalis (TV) among pregnant women and male partners, (ii) to identify risk factors for these STI during pregnancy, and (iii) to identify adverse perinatal outcomes (APO) associated with STI.
Pregnant women aged ≤ 30 years and male partners were included at 30 midwifery practices. Women provided a vaginal swab, partners a urine sample; both completed a questionnaire. Perinatal data were derived from midwives.
STI were present in 2.4% of pregnant women (CT 1.8%, NG 0.4%, TV 0.4%), and in 2.2% of male partners (CT 2.2%, NG 0.2%, TV 0%). Of women ≤ 20 years, 12.5% had a CT infection. Prevalent STI during pregnancy was associated with female young age, male non-Western background, and female with ≥ 2 sex partners < 12 months. APO was not associated with STI, but was associated with female low education, complications with previous newborn, and short duration of the relationship. Small-for-gestational-age was not associated with STI, but was associated with female low education, female non-Western background, and both parents smoking during pregnancy.
Prevalence of STI was low among pregnant women and male partners in midwifery practices, except for CT among young women. The study could not confirm previously observed associations between STI and APO. Probably due to low prevalence of STI, small study sample, and presumed treatment for STI.
Similar content being viewed by others
Background
In the Netherlands, pregnant women are screened for HIV, syphilis and hepatitis B [1, 2], but not for other sexually transmitted infections (STI). Hence, limited data are available on STI such as Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG) or Trichomonas vaginalis (TV) among pregnant women and their male partners. The World Health Organization (WHO) estimated for 2012 that among women of reproductive age (15–49 years) in the European region the prevalence of CT was 2.2% (95% uncertainty interval (UI): 1.6–2.9%), NG was 0.3% (0.2–0.5%), and TV was 1.0% (0.8–1.3%). For men, these prevalence rates were 1.5% (0.9–2.6%), 0.3% (0.2–0.5%), and 0.1% (0.1–0.2%) respectively [3].
An accurate detection and effective management of these STI are particularly relevant to women in their reproductive age as most infections are asymptomatic and may affect reproductive health [4, 5]. Untreated infections with CT, NG or TV in women can result in pelvic inflammatory disease (PID), which can cause chronic pelvic pain, infertility, and ectopic pregnancies [6,7,8]. During pregnancy, these STI have been associated with adverse perinatal outcomes (APO) including premature rupture of membranes (PROM), preterm delivery, low birthweight [9,10,11,12,13,14,15,16,17,18,19], stillbirth, and neonatal conjunctival and respiratory infections [20,21,22,23]. The effect of these STI on newborns who are born small for gestational age (SGA) is less evident [23, 24].
Although having STI during pregnancy is considered a risk factor for APO [15, 16, 23], data regarding STI prevalence rates in pregnant women together with their male partners, and factors associated with STI in pregnancy or its associations with APO are limited when taking into account sociodemographic and lifestyle factors [12, 25,26,27,28]. Also, findings from observational and cohort studies are inconclusive about the strengths of the associations between STI and reproductive outcomes [23, 24].
In many countries CT, NG and TV infections in pregnant women are still identified and treated by syndromic management [29]. Antenatal screening, especially for NG and TV, is often limited to resource-limited regions [30,31,32,33], where prevalence rates and incidence rates are much higher compared to high-income regions [29, 34, 35]. Although international guidelines recommend antenatal screening for CT of all women under 25 years of age and of older women at increased (sexual) risk [7], in the Netherlands these recommendations are not followed.
A previous study among pregnant women in Rotterdam showed an overall CT prevalence of 3.9% (including women up to ≥ 30 years of age). Women who tested positive for CT had higher adjusted odds ratios (aORs) for preterm delivery at 32 weeks (aOR 4.3, 95%CI 1.3–3.5) and 35 weeks (aOR 2.7, 95% CI 1.1–6.5) of pregnancy compared to CT negative women [36]. For the Netherlands CT screening of all pregnant women is considered cost-saving [37], based on the prevalence of 3.9% from the Rotterdam study [36]. Cost-effectiveness studies on screening for NG and TV infections among pregnant women in the Netherlands or other high-income regions are greatly lacking, and more insight is needed in these prevalence rates among pregnant women and their partners.
To inform recommendations about antenatal screening for these STI, we conducted a national cross-sectional study with the following aims: (i) to assess the CT-, NG-, and TV prevalence rates among pregnant women aged ≤ 30 years and their male partners who present to midwifery practices, (ii) to explore risk factors associated with these STI during pregnancy, and (iii) to explore the association between STI during pregnancy and adverse perinatal outcomes, with special focus on CT infection.
Methods
Study participants
The design of this multicentre observational study that included thirty midwifery practices across the Netherlands is described in detail elsewhere [38, 39]. The practices included covered approximately 5.0% of the pregnant women in the Netherlands (Supplementary file). In brief, pregnant women between 18 and 30 years of age were enrolled by their midwives if they could understand Dutch. There were no restrictions to the gestational age at inclusion. Male partners were included without an age limit, if they were present at the time of their partners’ enrolment and could understand Dutch. Both, women and partners signed an Informed Consent (IC) form for participation including follow-up data collection on perinatal outcomes through their midwives (pregnancy cards). Subsequently, they received a test package including home sampling devices, an information flyer, and a questionnaire for the woman and partner.
Sample and data collection
Pregnant women filled in a questionnaire including sociodemographic characteristics (age, migration background, education, religion, marital status, postal code), obstetric characteristics (duration of pregnancy, parity, gravity, complaints, early and late miscarriages, abortions, complications with last pregnancy or previous newborn including delivery at ≤ 37 weeks, premature contractions, PROM, birthweight ≤ 2500 g, previous newborn with pneumonia or eye inflammation), biometric measures (weight, length, body mass index (BMI)), lifestyle factors (smoking, drug and alcohol use), antibiotic use ≤ 3 months before study inclusion, CT related knowledge (infection, transmission routes), attitude questions on CT screening for women and partners (how did they experience the test offer in terms of feeling satisfied, surprised, stigmatized or ashamed), and sexual risk behaviour including age of sexual debut, history of STI, having a new partner in the last 3 months, number of partners in the last 12 months, sex in exchange for money, and condom use. Partners filled in a questionnaire with the same questions on sociodemographic characteristics, lifestyle factors (except alcohol use), antibiotic use, CT related knowledge and attitude questions, sexual risk behaviour, complaints, and history of STI.
Migration background was measured as country of birth of both the woman and her partner and both their parents, and subsequently recoded in Western or non-Western (1st and 2nd generation) migration background. A Western background included Western Europe, North America, Australia and New Zealand. All other regions were defined as non-Western background. Data on socioeconomic status (SES) and urbanity for postal code areas were added to the database. SES status scores were obtained from the Netherlands Institute for Social Research (available at: www.scp.nl). This score takes into account the average income per household in a given postal code area as well as the percentage of households with low income, without paid work, and with low education level. The level of urbanity by postal code area was obtained from Statistics Netherlands (www.cbs.nl).
Women provided vaginal swabs and men provided urine specimens. CT, NG and TV DNA was detected in a two-step approach: first human and microbial DNA was isolated using the High Pure PCR Template Preparation Kit (Roche), and secondly the isolated DNA was used in a PCR system based on the CE-IVD certified PRESTO CT-NG test and the CE-IVD PRESTO TV kit (Goffin Molecular Diagnostics, Beesd, the Netherlands). The assays were performed following the instructions for use of the manufacturer. PCR Cp value’s of 40 and higher were considered negative. The Isolation and Amplification Control (IAC) needs to be positive to consider the sample PCR result reliable. In case the sample is positive for CT, NG or TV the IAC might become negative due to competition, in that case the result is reliable.
Test results were provided by mail in closed envelopes and separately for women and partners, leaving the decision to share test results open. Midwives received the test results for their female clients only. Women and partners who tested positive for CT, NG or TV received an information brochure on the diagnosed STI and a referral letter for their general practitioner (GP) to get treatment.
After birth, pregnancy and neonatal outcomes were collected through pregnancy cards obtained from midwives that included gynaecological information, weeks of gestation, birth weight of the newborn, congenital defects, single or multiple birth(s), medication, preeclampsia, drug use, herpes simplex virus (HSV) infections among women or partners, and STI history of the mother.
Data analysis
To evaluate the representativeness of the participating midwifery practices, the demographic characteristics of pregnant women from the participating practices were compared to non-participating practices while using aggregated data from Perined (the Dutch national perinatal registry) for the same period. This dataset includes characteristics of pregnant women such as age, ethnicity, weeks of gestation, single or multiple birth(s), and birth weight of the newborn. Descriptive statistics with Chi-square tests were used to compare demographic and obstetric characteristics between (sub)groups.
Knowledge scores were calculated based on twelve questions about CT infection and transmission risks that could be answered with “true”, “false”, or “I don’t know”. Scores were calculated by giving each correct answer a value of 1, and an incorrect answer or ‘I don’t know’ a value of 0. The knowledge sum score could vary between 0 and 12. The knowledge score was included as covariate in the multivariable models in case statistically significant univariably. Exploratory factor analyses were used for the 5-item CT attitude scales to obtain theoretical constructs (factors) for ‘Attitude towards CT screening’ for inclusion as covariate in the multivariable models if relevant. Factors with a Cronbach’s alpha ≥ 0.7 were chosen. For women, the 6 attitude questions resulted in 2 attitude factors of which only one factor (‘negative emotions with the test offer’) was reliable with a Cronbach’s alpha of 0.74 and included two 5-scale (strongly agree to disagree entirely) questions (“I felt ‘stigmatized’ when I was asked to take the Chlamydia test”, “I was embarrassed when I was asked to take the Chlamydia test”). For partners, the same factor was obtained with a Cronbach’s alpha of 0.72.
Univariable and multivariable logistic regression analyses were used to explore risk factors for STI during pregnancy, with the combined STI endpoint of having any of the CT-, NG-, and/or TV-infection(s), due to small numbers of infections. Analyses were repeated for a single CT infection as endpoint, as this was the most common STI and the focus of the study. Multivariable models were adjusted for all covariates as listed with p < 0.20 (Wald test) in univariable analyses using backwards stepwise selection (as listed in footnotes of Tables 2, 3, 4). Highly correlated variables (Spearman correlation coefficients) were not included in the model together; the strongest associated variables were selected or variables were combined into new variables (e.g. combined female and male variables for smoking). Variables were considered statistically significant when p < 0.05 for the likelihood ratio test.
Procedures were repeated for the dichotomous outcome variables of any adverse perinatal outcome (APO) and separately for small-for-gestational-age (SGA). APO was defined as ‘Yes’ if one or more of the variables of preterm birth (< 37 weeks), low birthweight (< 2500 g), premature rupture of membranes (PROM), stillbirth or neonatal conjunctival and respiratory infections were reported. The outcome SGA (birthweight for gestational age < 10th percentile) was calculated according to the Dutch standards [40]. Independent variables of pregnant women and partners included age, migration background, SES, urbanity, religion, education, (history of) STI, drug use, smoking, and antibiotic use. Independent variables for women only included marital status, duration of relationship, body mass index (BMI kg/m2), alcohol use, gravity, parity, gestational age at discovery of pregnancy, and gestational age at study inclusion. By including this last variable in the model, we could examine a potential effect of (treated) STI on perinatal outcomes. As previous pregnancies may influence subsequent pregnancy outcomes, sub-analyses of nulliparous women were performed to examine associations between STI and APO in more detail. Analyses were done in SPSS 24.0 (SPSS inc, Chicago, IL).
Results
Midwifery practices
The characteristics of pregnant women from the participating practices and non-participating practices were very similar. The percentage of pregnant women of Dutch origin was 72.3% and 73.2% respectively. A small but significant difference was observed for low SES; 39.8% percent versus 38.2% respectively (P < 0.05). Obstetric characteristics including gestational age, prematurity, and neonatal birthweight did not differ significantly between the two groups (Additional file 1: Table S1).
Demographic characteristics
In total, 856 pregnant women and 575 male partners were registered as being approached for study participation of whom 83 women and 19 partners returned a non-participation form. Reasons for non-participation among women were: not interested (32.5%), recently tested for STI (25.3%), ‘not at risk’ (13.2%), too much on their mind (7.2%), first partner (6.0%), not willing to take a sample (3.6%), and other/unknown reasons (12.0%). Reasons for non-participation among males were often the same as for females (a ‘couple decision’) and were therefore not presented.
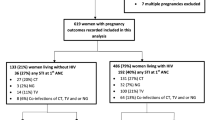
All 773 women (90.3%) gave informed consent of whom 548 returned the questionnaire and a vaginal swab (70.9%). These women and their 425 partners (73.9%) were included in the analyses. For 457 women (83.4%), perinatal outcome data from pregnancy cards were available (Table 1). No multiple births were reported.
The median age at enrolment for women was 27 years [interquartile range (IR): 25–29 years] and 29 years [IR: 27–32] for their partners. Most participants had a Dutch or other Western background (75.2% of women, 78.4% of men), and half of the participants had a high-level education (49.6% of women and 53.4% of men). Most women were married or living together but unmarried (83.9%). Thirty-six percent of the women had a religion of whom the majority was Catholic or had another Christian religion, and 4.9% were Muslim.
Lifestyle factors
During pregnancy 21.9% of the women smoked of whom 64.2% stopped after the pregnancy became known and 7.8% smoked during the entire pregnancy (Table 1). Of their partners, 25.4% smoked during the pregnancy, but only 12.0% stopped when the pregnancy was known. Alcohol use by women was 67%, but 97% stopped when the pregnancy was discovered. Any drug use among women was 4.2% of whom 73.9% used soft drugs and 26.1% used hard drugs. One woman (0.2%) continued to use soft drugs during pregnancy; none were using hard drugs. Of the partners, 11.1% used drugs during the pregnancy and 9.4% continued to use drugs during pregnancy (55.0% soft drugs, 45.0% hard drugs or combination of both).
STI positivity during pregnancy
The pooled STI positivity (CT, NG and TV) was 2.4% (95%CI 1.3–4.0%) for the women and 2.2% (CI 1.0–4.0) for their partners. Among the women, 1.8% (CI 0.9–3.3) was infected with CT, 0.4% (CI 0.0–1.3) with NG and 0.4% (CI 0.0–1.3) with TV (Table 1); among men CT positivity was 2.2% (CI 1.0–4.0), NG positivity 0.2% (CI 0.0–1.3), and no TV infections were identified. CT positivity was 12.5% (CI 3.5–29.0) among women aged ≤ 20 years of age, 3.1% (CI 0.8–7.6) among women < 25 years, and 1.4% (CI 0.3–3.5) among women of 20–25 years of age.
Discordant CT test results within couples were as follows: 14% of the male partners were CT negative while the female was CT positive, and among CT positive male partners, 40% of the women were CT negative.
Women had slightly more knowledge on CT infection and transmission risks than the partners: 13.4% of the women answered all questions correct compared to 10.4% of the men (Table 1).
Univariable logistic regression analyses showed that an STI diagnosis during pregnancy was associated with various demographic, behavioural, and lifestyle variables (Table 2). Adjusted for covariates, three variables remained in the model: young age at inclusion (≤ 20 years versus ≥ 21 years, adjusted OR (aOR) 6.62, CI 95%: 1.11–38.33), having a partner of non-Western background vs Western background (aOR 9.34, CI 2.34–37.21), and having two or more sex partners in the past 12 months (aOR 9.88, CI 2.08–46.91).
The same model was run for CT infection as outcome variable. Results were the same, but confidence intervals were wider due to smaller numbers: age ≤ 20 years at inclusion (aOR 11.45, CI 1.80–72.90), having a non-Western partner (aOR 9.45, CI 1.84–49.50) and having two or more sex partners in the past 12 months (aOR 9.62, CI 1.54–60.25) (model not shown).
Adverse perinatal outcomes
Of the pregnant women 10.9% had one or more adverse perinatal outcome(s) (APO), including preterm birth (< 37 weeks, 7.0%), premature rupture of membranes (PROM, 3.9%), low birthweight (< 2500 g, 4.2%), stillbirth (n = 1, 0.22%), and neonatal conjunctival infection (n = 1, 0.22%). No neonatal respiratory infections were reported.
Having an STI during pregnancy, having had a history of STI diagnoses, and/or having a partner with a current STI diagnosis were not associated with APO (Table 3). CT infection during pregnancy was also not associated with APO (not shown).
However, other factors that were associated with APO were complications with the previous newborn (preterm birth and/or low birthweight) (aOR 10.49, CI 3.21–34.25 vs no complications), short duration of the relationship (aOR for 0–4 years: 2.75, CI 1.41–5.39 vs ≥ 5 years) and female low education (aOR 3.36, CI 1.12–10.09).
As a substantial proportion of the pregnant women had previous deliveries (26.6%) that may influence subsequent pregnancy outcomes, the same analyses were done for nulliparous women. The APO model for nulliparous women showed that none of the STI-variables were associated with APO. However, short duration of the relationship was still associated with APO (aOR for 0–4 years: 3.52, CI 1.47–8.43 vs ≥ 5 years), and an additional risk factor was obesity (BMI ≥ 30, aOR 4.46, CI 1.21–16.47 vs BMI 18.5–25, Additional file 1: Table S2).
Of the newborns, 28 (6.3%) were small for gestational age (SGA). The univariable models for SGA showed that female and male non-Western migration background, female low education level, province, female and male smoking, and having had an STI in the past (female) were associated with SGA (Table 4). Having an STI (or CT only) in the current pregnancy was not associated with SGA univariably and was not included in the adjusted model. Factors that remained associated in the adjusted model were: female low education (aOR 7.81, CI 2.01–30.27), female non-Western background (aOR 4.41, CI 1.74–11.17), and both female and male smoking during pregnancy (aOR 2.94, CI 1.01–8.84).
Discussion
The pooled prevalence of STI (CT, NG and TV) was 2.4% among pregnant women ≤ 30 years of age and 2.2% among their male partners in Dutch midwifery practices. Risk factors for STI during pregnancy were female young age (≤ 20 years), male non-Western background, and having had two or more sex partners in the past 12 months (female). Of the women, 10.9% had one or more adverse perinatal outcomes (APO) and 6.3% of the newborns were small for gestational age (SGA). However, having an STI during pregnancy was not associated with APO nor with SGA in our study population. We did identify other risk factors for APO (low female education, previous newborn with preterm birth, short duration of the current relationship, obesity) and for SGA (low female education, female non-Western background, combined female and male smoking during pregnancy).
The strength of our study is the inclusion of samples and epidemiological information of both pregnant women and their male partners. However, our study also has some limitations. First, the study sample of 548 women of whom 457 had perinatal outcome data is rather small. Together with the low prevalence of STI, this may have caused a lack of statistical power to identify STI associated determinants with small effects that are known for these STI and APO [41, 42]. Second, women were included at various stages of pregnancy. Most (65.1%) women were included in the second or third trimester, which may have attenuated underlying associations with STI due to foetal development and treatment. Prior studies showed that associations between STI during pregnancy and APO are strongest during the first trimester [42]; the stage in which vital organs develop. Third, our study may not be fully representative for all pregnant women in the Netherlands, although we assume no major selection bias in midwifery practices since the baseline characteristics of pregnant women and perinatal outcomes were comparable between participating and non-participating practices. However, our study sample only includes women who understand Dutch. Therefore, percentages of STI as well as APO may have been underestimated, assuming that having a non-Western background is associated with a higher STI prevalence [43, 44]. Finally, we cannot rule out response bias from women and partners due to stigma or social desirability, which could understate exposure to sexual risks or other lifestyle factors during pregnancy.
Previous research, including meta-analyses, showed small but increased odds of APO due to infections with CT and NG during pregnancy, such as preterm delivery and low birthweight [16, 36, 41, 45]. We could not confirm these associations, probably due to the small study sample and low STI prevalence. Also, we assume that most women who were diagnosed with an STI received treatment that may have mitigated any effect of STI on APO. Unfortunately, follow-up information on treatment by general practitioners was not collected. However, we identified other risk factors than STI for APO and SGA newborns, such as low female education. These associations confirm previous findings [46]. Women with low education might be less capable to adopt healthy behaviours before conception or during pregnancy [13, 14, 47]. Education on healthy behaviour before conception and during pregnancy is relevant to reduce APO, especially for women with obesity, which was also associated with APO among nulliparous women [48]. Further, having a previous newborn with low birthweight or preterm birth was a risk factor for APO, confirming earlier studies showing that previous preterm birth was a risk factor for current preterm birth and premature rupture of membranes [49, 50]. Of the lifestyle factors, a small effect of combined male and female smoking was identified for SGA newborns, but other lifestyle factors were not significant. Likely, most women stop smoking or drinking alcohol after finding out about the pregnancy [51, 52]. The role of relationship duration in APO could be the result of underlying factors. A short duration of the relationship could be associated to changing sexual partners that increases the risk of STI or could be related to other risk factors for APO that we could not identify.
The CT prevalence among pregnant women in our study was 1.8% and among women ≤ 20 years of age it was 12.5%. Young age is one of the most important risk factors for CT among women [44, 53]. The Rotterdam study among pregnant women showed an overall CT prevalence of 3.9% (including women up to ≥ 30 years of age), and a prevalence of 13.5% among women ≤ 20 years. Besides young age, Antillean ethnicity, and not being married were independent risk factors for CT infection during pregnancy in the Rotterdam study [36]. In our study, having a non-Western partner and having two or more sex partners in the past 12 months were risk factors for CT infection. The partners’ non-Western background was stronger associated than the female non-Western background, although the two are interrelated [54]. This relationship between migration background of the partner and CT infections among women has been previously described [44, 53]. In our study, the group of people with a non-Western background also included men and women with an Antillean or Surinamese background. In the Rotterdam study, CT prevalences among Antillean women and Surinamese women were 16.2%, and 9.1% respectively. Prevalence rates among these subgroups in our study were not shown due to small numbers. Therefore, we used the variable Western and non-Western background. Small numbers could also be the reason that female migration background was not significant in the regression models.
We also showed that male partners can be a critical source of transmission to pregnant women who tested negative for CT. Among CT infected male partners, 40% of the women tested CT negative. These women are at risk of transmission during their pregnancy or in the post-delivery phase. Although this proportion may not accurately reflect discordant rates due to small numbers, male involvement in CT testing has been recognized internationally as an important aspect of prevention of mother-to-child transmission [7, 55]. In general, CT testing during pregnancy is well accepted by women and their partners [39].
International guidelines recommend antenatal screening for CT of all women under 25 years of age and of older women at increased (sexual) risk [7]. These guidelines are not followed in the Netherlands. A previous study showed that Dutch midwives base their decisions to offer CT testing to pregnant women on symptoms rather than on risk profiles [38]. Hence, since up to 80% of CT infections in women and 50% in men remain asymptomatic [7], most pregnant women will remain undetected with the current prenatal Dutch standard. Subsequently, CT infected women are left untreated with a risk for postpartum PID for themselves, a risk for transmission to their offspring with possible neonatal conjunctivitis and pneumonia, and a risk for transmission to their partner. The high CT prevalence (12.5%) we found among women ≤ 20 years in this study coincides with the high 13.5% prevalence in the same age group in the Rotterdam study. These findings would support the implementation of the international guidelines. Also, CT screening of this group of young pregnant women (≤ 20 years) was shown to be particularly cost-saving based on the results from the Rotterdam study [36, 37]. Based on this study, screening of women age < 25 years would also be cost-effective; the prevalence in this age group was 3.1% compared to 6.7% in the Rotterdam study. However, to decide on a national CT screening program for all pregnant women in the Netherlands, more research might be needed on its (cost)-effectiveness [37, 56,57,58].
In conclusion, the prevalence of STI among pregnant women, and their male partners, in Dutch midwifery practices was low, except for a high prevalence of CT infection among young women. Important female and male risk factors for STI and for CT infection during pregnancy were identified as young age, having had two or more sex partners in the past 12 months, and having a male partner with a non-Western background. Previously observed associations between STI and APO could not be confirmed. In the absence of a national screening program midwives and obstetricians should be aware of the high prevalence of CT among women under the age of 20 and with multiple sexual partners.
Availability of data and materials
The dataset presented in this article is not publicly available because statistical information or data for research purposes can be requested by submitting a research proposal. Requests to access the dataset should be directed to the corresponding author.
Abbreviations
- STI:
-
Sexually transmitted infection
- CT:
-
Chlamydia trachomatis
- NG:
-
Neisseria gonorrhoeae
- TV:
-
Trichomonas vaginalis
- HIV:
-
Human immunodeficiency virus
- HBV:
-
Hepatitis B virus
- HSV:
-
Herpes simplex virus
- APO:
-
Adverse perinatal outcomes
- SGA:
-
Small for gestational age
- PROM:
-
Premature rupture of membranes
- PID:
-
Pelvic inflammatory disease
- BMI:
-
Body mass index
- IC:
-
Informed consent
- GP:
-
General practitioner
- SES:
-
Socio economic status
- WHO:
-
World Health Organization
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- DNA:
-
Deoxyribonucleic acid
- PCR:
-
Polymerase chain reaction
- IAC:
-
Isolation and amplification control
- CE-IVD:
-
European Community marking for in vitro diagnostic devices
References
Op de Coul EL, Hahne S, van Weert YW, Oomen P, Smit C, van der Ploeg KP, et al. Antenatal screening for HIV, hepatitis B and syphilis in the Netherlands is effective. BMC Infect Dis. 2011;11:185.
Visser M, Van der Ploeg CPB, Smit C, Hukkelhoven CWPM, Abbink F, Van Benthem BH, et al. Evaluating progress towards triple elimination of mother-to-child transmission of HIV, syphilis and hepatitis B in the Netherlands. BMC Public Health. 2019. https://doi.org/10.1186/s12889-019-6668-6.
Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS ONE. 2015;10(12): e0143304.
Sutton M, Sternberg M, Koumans EH, McQuillan G, Berman S, Markowitz L. The prevalence of Trichomonas vaginalis infection among reproductive-age women in the United States, 2001–2004. Clin Infect Dis. 2007;45(10):1319–26.
Workowski KA, Berman SM. Centers for disease control and prevention sexually transmitted disease treatment guidelines. Clin Infect Dis. 2011;53(Suppl 3):S59-63.
CDC. Chlamydia screening among sexually active young female enrollees of health plans—United States, 1999–2001. MMWR Morb Mortal Wkly Rep. 2009;42(53):983–5.
CDC. STDs during pregnancy CDC; 2016. https://www.cdc.gov/std/pregnancy/stdfact-pregnancy-detailed.htm.
Ahmadi MH, Mirsalehian A, Bahador A. Association of Chlamydia trachomatis with infertility and clinical manifestations: a systematic review and meta-analysis of case-control studies. Infect Dis (London, England). 2016;48(7):517–23.
Bonsel GJ BE, Denktaş S, Poeran J, Steegers EAP. Lijnen in de perinatale sterfte. Signalementstudie 'Zwangerschap en Geboorte'. Erasmus MC, Rotterdam; 2010 2010.
Caughey AB, Robinson JN, Norwitz ER. Contemporary diagnosis and management of preterm premature rupture of membranes. Rev Obstet Gynecol. 2008;1(1):11–22.
RIVM. Welke factoren beïnvloeden de sterfte rond de geboorte? Volksgezondheid Toekomst Verkenning, Nationaal Kompas Volksgezondheid.: RIVM; 2013.
Lang JM, Lieberman E, Cohen A. A comparison of risk factors for preterm labor and term small-for-gestational-age birth. Epidemiology. 1996;7(4):369–76.
Karlberg J, Albertsson-Wikland K. Growth in full-term small-for-gestational-age infants: from birth to final height. Pediatr Res. 1995;38(5):733–9.
Thompson JM, Clark PM, Robinson E, Becroft DM, Pattison NS, Glavish N, et al. Risk factors for small-for-gestational-age babies: The Auckland Birthweight Collaborative Study. J Paediatr Child Health. 2001;37(4):369–75.
Moodley P, Sturm AW. Sexually transmitted infections, adverse pregnancy outcome and neonatal infection. Semin Neonatol. 2000;5(3):255–69.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84.
Watts DH, Eschenbach DA. Sexually transmitted diseases in pregnancy. Infect Dis Clin North Am. 1987;1(1):253–75.
Donders GG, Desmyter J, De Wet DH, Van Assche FA. The association of gonorrhoea and syphilis with premature birth and low birthweight. Genitourin Med. 1993;69(2):98–101.
Cotch MF, Pastorek JG 2nd, Nugent RP, Hillier SL, Gibbs RS, Martin DH, et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. The vaginal infections and prematurity study group. Sex Transm Dis. 1997;24(6):353–60.
Allaire AD, Huddleston JF, Graves WL, Nathan L. Initial and repeat screening for Chlamydia trachomatis during pregnancy. Infect Dis Obstet Gynecol. 1998;6(3):116–22.
Rours IG, Hammerschlag MR, Ott A, De Faber TJ, Verbrugh HA, de Groot R, et al. Chlamydia trachomatis as a cause of neonatal conjunctivitis in Dutch infants. Pediatrics. 2008;121(2):e321–6.
Rours GI, Hammerschlag MR, Van Doornum GJ, Hop WC, de Groot R, Willemse HF, et al. Chlamydia trachomatis respiratory infection in Dutch infants. Arch Dis Child. 2009;94(9):705–7.
Tang W, Mao J, Li KT, Walker JS, Chou R, Fu R, et al. Pregnancy and fertility-related adverse outcomes associated with Chlamydia trachomatis infection: a global systematic review and meta-analysis. Sex Transm Infect. 2020;96(5):322–9.
Reekie J, Roberts C, Preen D, Hocking JS, Donovan B, Ward J, Mak DB, Liu B, on behalf of the Chlamydia and Reproductive Health Outcome Investigators. Chlamydia trachomatis and the risk of spontaneous preterm birth, babies who are born small for gestational age, and stillbirth: a population-based cohort study. Lancet Infect Dis. 2018;18:452–60.
McFarlane J, Parker B, Soeken K. Physical abuse, smoking, and substance use during pregnancy: prevalence, interrelationships, and effects on birth weight. J Obstet Gynecol Neonatal Nurs. 1996;25(4):313–20.
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88(1):31–8.
Tucker J, McGuire W. Epidemiology of preterm birth. BMJ (Clinical research ed). 2004;329(7467):675–8.
Cheong JL, Doyle LW. Increasing rates of prematurity and epidemiology of late preterm birth. J Paediatr Child Health. 2012;48(9):784–8.
WHO. Report on global sexually transmitted infection surveillance, 2018.
Bristow CC, Mathelier P, Ocheretina O, Benoit D, Pape JW, Wynn A, et al. Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis screening and treatment of pregnant women in Port-au-Prince, Haiti. Int J STD AIDS. 2017;28(11):1130–4.
Shannon CL, Bristow C, Hoff N, Wynn A, Nguyen M, Medina-Marino A, et al. Acceptability and feasibility of rapid Chlamydial, Gonococcal, and Trichomonal screening and treatment in pregnant women in 6 low- to middle-income countries. Sex Transm Dis. 2018;45(10):673–6.
Yeganeh N, Kreitchmann R, Leng M, Nielsen-Saines K, Gorbach PM, Klausner J. High prevalence of sexually transmitted infections in pregnant women living in southern Brazil. Sex Transm Dis. 2020. https://doi.org/10.1097/OLQ.0000000000001276.
Joseph Davey DL, Shull HI, Billings JD, Wang D, Adachi K, Klausner JD. Prevalence of curable sexually transmitted infections in pregnant women in low- and middle-income countries from 2010 to 2015: a systematic review. Sex Transm Dis. 2016;43(7):450–8.
Rowley J, Vander Hoorn S, Korenromp E, Low N, Unemo M, Abu-Raddad LJ, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97(8):548–62.
Teasdale CA, Abrams EJ, Chiasson MA, Justman J, Blanchard K, Jones HE. Incidence of sexually transmitted infections during pregnancy. PLoS ONE. 2018;13(5): e0197696.
Rours GI, Duijts L, Moll HA, Arends LR, de Groot R, Jaddoe VW, et al. Chlamydia trachomatis infection during pregnancy associated with preterm delivery: a population-based prospective cohort study. Eur J Epidemiol. 2011;26(6):493–502.
Rours GI, Smith-Norowitz TA, Ditkowsky J, Hammerschlag MR, Verkooyen RP, de Groot R, et al. Cost-effectiveness analysis of Chlamydia trachomatis screening in Dutch pregnant women. Pathog Glob Health. 2016;110(7–8):292–302.
Pereboom MT, Mannien J, Rours GI, Spelten ER, Hutton EK, Schellevis FG. Chlamydia trachomatis infection during pregnancy: knowledge, test practices, and attitudes of Dutch midwives. Scand J Infect Dis. 2014;46(2):107–13.
Pereboom MT, Spelten ER, Mannien J, Rours GI, Morre SA, Schellevis FG, et al. Knowledge and acceptability of Chlamydia trachomatis screening among pregnant women and their partners; a cross-sectional study. BMC Public Health. 2014;14:704.
Hoftiezer L, Hof MHP, Dijs-Elsinga J, Hogeveen M, Hukkelhoven C, van Lingen RA. From population reference to national standard: new and improved birthweight charts. Am J Obstet Gynecol. 2019;220(4):383 e1-e17.
Olson-Chen C, Balaram K, Hackney DN. Chlamydia trachomatis and adverse pregnancy outcomes: meta-analysis of patients with and without infection. Matern Child Health J. 2018;22(6):812–21.
Heumann CL, Quilter LA, Eastment MC, Heffron R, Hawes SE. Adverse birth outcomes and maternal Neisseria gonorrhoeae infection: a population-based cohort study in Washington State. Sex Transm Dis. 2017;44(5):266–71.
Noordt M van der, Eysink PED, Van Aar F. Chlamydia samengevat. Volksgezondheid Toekomst Verkenning, Nationaal Kompas Volksgezondheid. 2014. http://www.nationaalkompas.nl/gezondheid-en-ziekte/ziekten-en-aandoeningen/infectieziekten-en-parasitaire-ziekten/soa/chlamydia/chlamydia-samengevat/.
Op de Coul EL, Götz HM, van Bergen JE, Fennema JS, Hoebe CJ, Koekenbier RH, et al. Who participates in the Dutch Chlamydia screening? A study on demographic and behavioral correlates of participation and positivity. Sex Transm Dis. 2012;39(2):97–103.
Rours GI, de Krijger RR, Ott A, Willemse HF, de Groot R, Zimmermann LJ, et al. Chlamydia trachomatis and placental inflammation in early preterm delivery. Eur J Epidemiol. 2011;26(5):421–8.
Luo ZC, Wilkins R, Kramer MS, Fetal, Infant Health Study Group of the Canadian Perinatal Surveillance S. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. CMAJ. 2006;174(10):1415–20.
Goossens J, Beeckman D, Van Hecke A, Delbaere I, Verhaeghe S. Preconception lifestyle changes in women with planned pregnancies. Midwifery. 2018;56:112–20.
Melchor I, Burgos J, Del Campo A, Aiartzaguena A, Gutierrez J, Melchor JC. Effect of maternal obesity on pregnancy outcomes in women delivering singleton babies: a historical cohort study. J Perinat Med. 2019;47(6):625–30.
Panaretto K, Lee H, Mitchell M, Larkins S, Manessis V, Buettner P, et al. Risk factors for preterm, low birth weight and small for gestational age birth in urban Aboriginal and Torres Strait Islander women in Townsville. Aust N Z J Public Health. 2006;30(2):163–70.
Harger JH, Hsing AW, Tuomala RE, Gibbs RS, Mead PB, Eschenbach DA, et al. Risk factors for preterm premature rupture of fetal membranes: a multicenter case-control study. Am J Obstet Gynecol. 1990;163(1 Pt 1):130–7.
Crone MR, Luurssen-Masurel N, Bruinsma-van Zwicht BS, van Lith JMM, Rijnders MEB. Pregnant women at increased risk of adverse perinatal outcomes: a combination of less healthy behaviors and adverse psychosocial and socio-economic circumstances. Prev Med. 2019;127:105817.
Project. EP. European perinatal health report. Core indicators of the health and care of pregnant women and babies in Europe in 2015. https://www.europeristat.com/index.php/reports/european-perinatal-health-report-2015.html. Accessed 11 Oct 2020.
Visser M, Van Aar F, Op de Coul ELM, Slurink IAL, van Wees DA, Hoenderboom BM, et al. Sexually transmitted infections in the Netherlands in 2017. RIVM report number 2018-0012. 2018.
Ford K, Lepkowski JM. Characteristics of sexual partners and STD infection among American adolescents. Int J STD AIDS. 2004;15(4):260–5.
Dhairyawan R, Creighton S, Sivyour L, Anderson J. Testing the fathers: carrying out HIV and STI tests on partners of pregnant women. Sex Transm Infect. 2012;88(3):184–6.
Ditkowsky J, Shah KH, Hammerschlag MR, Kohlhoff S, Smith-Norowitz TA. Cost-benefit analysis of Chlamydia trachomatis screening in pregnant women in a high burden setting in the United States. BMC Infect Dis. 2017;17(1):155.
Ong JJ, Chen M, Hocking J, Fairley CK, Carter R, Bulfone L, et al. Chlamydia screening for pregnant women aged 16–25 years attending an antenatal service: a cost-effectiveness study. BJOG. 2016;123(7):1194–202.
Norman JE, Wu O, Twaddle S, Macmillan S, McMillan L, Templeton A, et al. An evaluation of economics and acceptability of screening for Chlamydia trachomatis infection, in women attending antenatal, abortion, colposcopy and family planning clinics in Scotland, UK. BJOG. 2004;111(11):1261–8.
Acknowledgements
This study was performed in collaboration with the AVAG (Academy of Obstetrics) in Groningen and the VU medical centre in Amsterdam. The authors thank Maiza Campos Ponce (VU University), and Sanne Hofstraat and Susan van den Hof from the RIVM for their inputs on the manuscript. The authors also thank all participating midwifery practices, as well as all pregnant women and their partners who participated in this study.
Funding
This study was funded by the Academy of Midwifery Amsterdam & Groningen (AVAG), and the Ministry of Health, Welfare and Sports in the Netherlands.
Author information
Authors and Affiliations
Contributions
MP and EC designed and conducted the study. DP and EC analysed the data and wrote the manuscript. SM was involved in laboratory analyses and interpretation of test results. CH contributed data. YW was involved in the logistics. All authors provided input on the manuscript read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Medical Ethics Committee of the VU University Medical Center in Amsterdam approved the study. All participants gave written informed consent for study participation. Data from consent forms, questionnaires, STI test results and postnatal pregnancy outcomes were linked using anonymised identification numbers.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Characteristics of pregnant women at participating and non-participating midwifery practices in the Netherlands (Source: Perined). Table S2. Factors associated with adverse perinatal outcomes (APO), nulliparous women.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Op de Coul, E.L.M., Peek, D., van Weert, Y.W.M. et al. Chlamydia trachomatis, Neisseria gonorrhoea, and Trichomonas vaginalis infections among pregnant women and male partners in Dutch midwifery practices: prevalence, risk factors, and perinatal outcomes. Reprod Health 18, 132 (2021). https://doi.org/10.1186/s12978-021-01179-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-021-01179-8