Abstract
Background
Sexually transmitted infections (STIs) during pregnancy may increase the risk of adverse pregnancy outcomes. STI syndromic management is standard of care in South Africa but has its limitations. We evaluated the impact of diagnosing and treating curable STIs during pregnancy on adverse pregnancy and birth outcomes.
Methods
We combined data from two prospective studies of pregnant women attending public sector antenatal care (ANC) clinics in Tshwane District and Cape Town, South Africa. Pregnant women were enrolled, tested and treated for STIs. We evaluated the association between any STI at the first ANC visit and a composite adverse pregnancy outcome (miscarriage, stillbirth, preterm birth, early neonatal death, or low birthweight) using modified Poisson regression models, stratifying by HIV infection and adjusting for maternal characteristics.
Results
Among 619 women, 61% (n = 380) were from Tshwane District and 39% (n = 239) from Cape Town; 79% (n = 486) were women living with HIV. The prevalence of any STI was 37% (n = 228); C. trachomatis, 26% (n = 158), T. vaginalis, 18% (n = 120) and N. gonorrhoeae, 6% (n = 40). There were 93% (n = 574) singleton live births, 5% (n = 29) miscarriages and 2% (n = 16) stillbirths. Among the live births, there were 1% (n = 3) neonatal deaths, 7% (n = 35) low birthweight in full-term babies and 10% (n = 62) preterm delivery. There were 24% (n = 146) for the composite adverse pregnancy outcome. Overall, any STI diagnosis and treatment at first ANC visit was not associated with adverse outcomes in women living with HIV (adjusted relative risk (aRR); 1.43, 95% CI: 0.95–2.16) or women without HIV (aRR; 2.11, 95% CI: 0.89–5.01). However, C. trachomatis (aRR; 1.57, 95% CI: 1.04–2.39) and N. gonorrhoeae (aRR; 1.69, 95% CI: 1.09–3.08), were each independently associated with the composite adverse outcome in women living with HIV.
Conclusion
Treated STIs at the first ANC visit were not associated with adverse pregnancy outcome overall. In women living with HIV, C. trachomatis or N. gonorrhoeae at first ANC were each independently associated with adverse pregnancy outcome. Our results highlights complex interactions between the timing of STI detection and treatment, HIV infection and pregnancy outcomes, which warrants further investigation.
Similar content being viewed by others
Background
Curable sexually transmitted infections (STIs), specifically C. trachomatis, T. vaginalis and N. gonorrhoeae during pregnancy have been associated with several adverse pregnancy and birth outcomes. Those adverse outcomes include miscarriage, stillbirth, prematurity, low birth weight and several secondary life-threatening conditions in surviving neonates [1,2,3,4]. However, there is limited consensus on the benefit of diagnosis and treatment of STIs, outside of syphilis, during pregnancy and reducing adverse pregnant outcomes. In pregnant women, untreated C. trachomatis infection has been associated with adverse obstetric outcomes such as fetal loss, premature rupture of membranes, preterm labour and preterm delivery in most but not all studies [5,6,7,8]. Maternal C. trachomatis infections can be transmitted during delivery and lead to conjunctivitis and pneumonia in newborns [5, 9, 10]. Maternal N. gonorrhoeae infection is associated with adverse pregnancy outcomes such as low birthweight [11, 12], small for gestational age (SGA) [1], preterm delivery, premature rupture of membranes and septic abortion. Newborns of mothers with N. gonorrhoeae infection can contract neonatal conjunctivitis which can lead to blindness if left untreated [13]. Maternal T. vaginalis infection can lead to low birthweight, preterm delivery, premature rupture of membranes, mental retardation, and vaginal and respiratory infections in neonates [14,15,16].
Despite the major threat to maternal and child health posed by these curable STIs, antenatal screening for C. trachomatis, N. gonorrhoeae and T. vaginalis infections is not recommended by WHO nor is part of the routine standard of care in antenatal settings in most developing countries [17]. Although symptomatic cases may be screened and offered treatment, most of these curable STIs are asymptomatic and often go without diagnosis and treatment [18, 19]. Most developing countries, introduced universal screening of syphilis in pregnant women attending antenatal clinics since 2012 [20, 21]. However, this has not been the case with other curable STIs such as C. trachomatis, N. gonorrhoeae and T. vaginalis because of the lack of laboratory infrastructure and financial resources to support aetiological screening in pregnancy [18, 19, 22]. However, point-of-care molecular tests such as GeneXpert® for C. trachomatis, N. gonorrhoeae and T. vaginalis have demonstrated high acceptability [6], feasibility and reliability [23, 24] in low- and middle-income countries, and could be scaled up to support screening for asymptomatic STIs in pregnancy.
South Africa’s antenatal HIV prevalence is one of the highest globally, reported at approximately 30% in 2017 [25]. In a recent study of pregnant women in South Africa in 2020, the prevalence and incidence of STIs was shown to be higher among women living with HIV compared to women without HIV [26]. In this high prevalence setting, more than 95% of HIV-infected pregnant women receive treatment for HIV infection in pregnancy, resulting in many newborns who are exposed to both HIV and antiviral treatment [27,28,29]. Recent studies are demonstrating that in utero fetal exposure to HIV and ARVs may be associated with adverse birth outcomes such as preterm birth and low birthweight [27,28,29,30,31]. In settings with double burden of HIV and STIs, there is a greater need to evaluate the impact of curable STIs in pregnancy on the pregnancy and birth outcome. In this study, we evaluated the impact of screening and treating STIs at first antenatal care visit on the prevalence of adverse pregnancy and birth outcomes stratifying by HIV status.
Methods
Study design and setting
We combined data from two observational prospective studies of pregnant women attending public sector antenatal clinics (ANCs) in Tshwane District and Cape Town, South Africa. Study enrolment in Tshwane District occurred between June 2016 and October 2017, and this study enrolled only women living with HIV. The study setting, eligibility criteria, data collection, and specimen collection and testing have been described elsewhere [19]. Study enrolment in Cape Town occurred between January 2018 and January 2019, and this study enrolled pregnant women living with and without HIV infection. Pregnant women with a confirmed HIV negative test result at enrolment, had repeat HIV testing at every antenatal appointment and after delivery. The study setting, eligibility criteria, data collection, and specimen collection and testing have been described elsewhere [18]. Briefly, in both studies pregnant women had to be: (i) ≥ 18 years of age, (ii) attending their first ANC visit and confirmed pregnancy using a urine pregnancy test, (iii) ≤ 35 weeks gestational age, (iv) confirmed HIV-infection status and (v) intenting to reside within the community for the duration of the pregnancy up to delivery.
Specimen collection, testing and treatment
As previously described [18, 19], women were offered aetiological testing through vulvovaginal swab specimens using Xpert® Vaginal/Endocervical Specimen Collection kits (Cepheid, Sunnyvale, CA). Specimens were tested for C. trachomatis, N. gonorrhoeae and T. vaginalis at first ANC visit and the first visit postpartum within one month (4 weeks) postpartum. Specimens were tested at the same day, and most women (94%) were given results before leaving the clinic. All women with a positive STI test result received treatment on the same day based on the Xpert® result per the choice of drugs in line with the South African National guidelines [32]. As per the national STI guidelines, women were given counselling, and provided with condoms and partner notification/referral letter [26].
Study definitions
For this analysis, pregnancy and obstetric outcomes were abstracted from obstetric records and maternity case records at delivery facilities. Birth anthropometrics were abstracted from the child Road to Health Booklets at the 7-day postpartum visit where mother-infant pairs were evaluated by study teams. Gestational age was estimated based on the date of the last menstrual period. Miscarriage was defined as noninduced pregnancy loss before 20 weeks of gestation. Stillbirth was defined as delivery of a baby with no sign of life at or after 20 weeks gestation. Early neonatal death was defined as death of a newborn between zero and seven days after birth. Preterm birth was defined as birth before completion of 37 weeks of gestation. Low birthweight was defined as an infant birthweight less than 2500 g. We used World Health Organization guidelines to categorize adverse birth outcomes [33]. The primary outcome of interest was a composite adverse outcome defined as any adverse pregnancy or birth outcome including miscarriage, stillbirth, early neonatal death, preterm birth or low birthweight. For sensitivity analysis, we excluded miscarriages (usually underestimated in outcomes of pregnancy cohorts due to left truncation as most women attend first ANC visit at gestational age after the typical period at which miscarriage occurs) in the composite adverse outcome. The exposure of interest was a positive diagnosis of a STI at first ANC visit. We also performed a sensitivity analysis by combining C. trachomatis and N. gonorrhoeae as exposure of interest excluding T. vaginalis with a different pathogenic inflammatory mechanism.
Data management
Study data were collected and managed using Research Electronic Data Capture (REDCap) platform [34]. All study participants were allocated a unique participant identifier allocated at study enrolment and all electronic communications were done through password-protected and encrypted files.
Statistical analysis
Maternal characteristics were compared using Wilcoxon test, χ2 test or Fisher exact test as appropriate. Odds Ratios are often used to approximate prevalence ratio or relative risk but can lead to overestimations for common events hence relative risk were used [35]. We fitted generalized linear models using modified Poisson regression with robust error measurements to estimate relative risk and 95% confidence interval (CI) for all association analyses. The modified Poisson regression with robust error measurements has fewer convergence problems compared to log-binomial logistic regression [35]. In stratified exploratory analysis by HIV status, we observed that women living with HIV were more likely to have composite adverse outcome compared to their counterpart women living without HIV, suggesting HIV status may be an effect modifier. Therefore, we performed several sensitivity analyses: first, exposure of interest as positive diagnosis of each STI (C. trachomatis, N. gonorrhoeae and T. vaginalis) to assess if a particular STI was associated with the composite adverse outcome. Second, we performed a sensitivity analyses with exposure of interest including C. trachomatis and N. gonorrhoeae only, third, with composite adverse outcome excluding miscarriages. Fourth, we used STIs at postnatal visit as proxy for STI status at time of delivery for women who had live births. All the models adjusted for maternal age, gestational age at enrolment, employment, marital status and gravidity.
Ethical consideration
Ethical approvals were provided by the University of Cape Town’s Faculty of Health Sciences Research Ethics Committee (UCT-HREC, reference number 454/2017), University of Pretoria’s Faculty of Health Sciences Research Ethics Committee (reference number 401/2015) and the University of California Los Angeles (reference number 15–001351). All women participating in the two studies provided informed written consent for their respective study participation.
Results
A total of 669 pregnant women were enrolled at first ANC visit and followed until the first postpartum study visit. Women excluded from this analysis have reasons listed in Fig. 1. Of the 669 pregnant women, 93% (619) of the women who had pregnancy outcomes recorded are included in this data analysis, 61% (380) were from Tshwane District and 39% (239) from Cape Town. Overall, 79% (486) were women living with HIV and 21% (133) without HIV (Table 1). The median age of participants at enrolment was 30 years (IQR 25–34 years) and the median gestational age was 18 weeks (IQR 13–24 weeks) (Table 1). At enrolment, half of the women (49%) reported being married or cohabitating with a partner and a third (34%) were formally employed. There were no differences in characteristics of women at enrolment between the Tshwane district and Cape Town cohorts as shown in supplementary material (Table S1).
Flow chart of pregnancies and outcomes included in this analysis.
CT, Chlamydia trachomatis; NG, Neisseria gonorrhoeae; TV, Trichomonas vaginalis; ANC, antenatal clinic.
Preterm, gestational age < 37 weeks; miscarriage, gestational age ≤ 20 weeks; stillbirth, gestational age > 20 weeks, LBW, low birthweight < 2500 g and neonatal death, early neonatal death of new-born between 0 and 7 days after birth
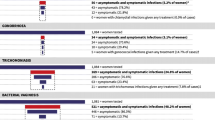
Prevalence of curable STI at first antenatal visit
At first ANC visit, 37% (228); 95% CI 33–41% were diagnosed with at least one STI. When stratified by HIV status, prevalence of any STI was 40% (192) in women living with HIV versus 27% (36) in women living without HIV. The most common infection at enrolment was C. trachomatis at 26% (158), with the infection more prevalent among women living with HIV, 27% (131) versus 20% (20) in women living without HIV, (p-value = 0.11), followed by T. vaginalis at 18% (120), with more infections among women living with HIV, 21% (106) versus 11% (14) in women living without HIV, (p-value = 0.008). N. gonorrhoeae had the lowest prevalence at enrolment with 6% (40) infected and 8% (37) in women living with HIV versus 2% (3) in women living without HIV, (p-value = 0.05). At enrolment, 12% (72) women had at least two infections of curable STIs, 13% (64) in women living with HIV versus 6% (8) in women living without HIV, (p-value = 0.02) (Table 1). At first postnatal visit, 8% (45) among women who had live births (n = 571) were diagnosed with at least one STI, 4% (21) were incident infection and 4% (24) were persistent infection. When stratified by HIV status, prevalence of any STI at first postnatal visit was 9% (45) in women living with HIV versus 3% (4) in women living without HIV. We compared the prevalence of at least one STIs in women living with HIV from Tshwane district 40% (151) versus Cape Town 39% (41). The prevalence for each STI was: C. trachomatis 29% (110) vs 20% (21), T. vaginalis 20% (77) vs 22% (23) and N. gonorrhoeae 6% (21) vs 10% (11) (Table S1). Most women (94%) were given their STI tests results before leaving the clinic and those who had a positive diagnosis received treatment on the same day in accordance with South African national guidelines.
Pregnancy and birth outcomes
Among 619 women included for this analysis (Fig. 1), 93% (574) had singleton live births with a median birthweight of 3125 g (IQR 2780–3420). Of those in this analysis, 24% (146) of the women had an adverse pregnancy outcome making up the primary outcome of interest, the composite adverse outcome 25% (123) in women living with HIV and 17% (23) in women living without HIV. Overall, 5% (29) experienced a miscarriage and 2% (16) experienced a stillbirth. Among the live birth, 1% (3) were early neonatal deaths, 10% (62) delivered a preterm baby and 7% (35) with low birth weight among the full term babies (Table 2). There was no difference observed for pregnancy losses (miscarriage and stillbirth) between women with and without STI during pregnancy by HIV status, 6% (2) vs 6% (6) in women living without HIV and 7%(13) vs 8%(24) in women living with HIV. In women who had a live birth, the preterm delivery rates were higher, but the difference is not significant, among women diagnosed with a STI during pregnancy compared to those without a STI in both women living with HIV (12% (24) vs. 10% (29)) and women living without HIV (11% (4) vs. 5% (5)). There was no difference detected for low birthweight between women with and without a curable STI during pregnancy in both women living with and without HIV (RR; 1.00, 95% CI: 0.84–1.19 and RR; 1.02, 95% CI: 0.69–1.44 respectively).
In the modified Poisson regression with robust error measurements, STI diagnosis and treatment at the first ANC visit was not associated with a composite adverse outcome in women living with HIV and women living without HIV, adjusted relative risk (aRR); 1.43, 95% CI: 0.95–2.16 and 2.11, 95% CI: 0.89–5.01, respectively, adjusting for maternal age, gestational age at enrolment, employment, marital status and gravidity (Table 3). When restricting the analysis to C. trachomatis or N. gonorrhoeae at first ANC visit we found an association with adverse pregnancy outcome in women living with HIV (aRR; 1.57, 95% CI: 1.04–2.39). When stratified by each STI, C. trachomatis and N. gonorrhoeae diagnosis and treatment at first ANC, each were significantly associated with the composite adverse outcomes in women living with HIV ((aRR; 1.57, 95% CI: 1.04–2.39) and (aRR; 1.69, 95% CI: 1.09–3.08), respectively) (Table 3). STI diagnosis at first postnatal visit (a proxy of STI positivity at time of delivery) did not elevate the risk of an adverse birth outcome in women living with HIV or in women without HIV who had live birth and returned for postnatal visit (aRR; 0.90, 95% CI: 0.44–1.82 and aRR; 0.90, 95% CI: 0.45–1.79). In the sensitivity analysis, we excluded miscarriage in the composite adverve outcome, and having diagnosis with a curable STI at first ANC did not increase the risk of having a composite adverse outcome in women living with and without HIV (Table 3).
Discussion
This prospective observational study implemented aetiological STI testing and treatment for the most common STIs (C. trachomatis, N. gonorrhoeae and T. vaginalis) as part of ANC at community health centres in two districts (Tshwane and Cape Town) in South Africa. The study shows high prevalence of curable STIs at enrolment of 37% in pregnant women living with and without HIV. STI prevalence was 1.48 times higher in women living with HIV versus women living without HIV. We observed a 78% reduction in prevalence of STIs at postnatal visit, (from 37 to 8%), which we used as proxy for STI status at time of delivery with only half of the infections incident [26].
In our study, we did not find an association between STI diagnosis and treatment at first ANC visit and composite adverse pregnancy outcome in women living with and without HIV. However, when we stratified the analysis by each STI, C. trachomatis and N. gonorrhoeae were each significantly associated with adverse pregnancy and birth outcomes among women living with HIV with a 1.57 and 1.69 fold increased risk respectively. Despite diagnosis and treatment fairly early in pregnancy, the association of STI diagnosis and composite adverse pregnancy outcome was present for C. trachomatis and N. gonorrhoeae among women living with HIV but not women living without HIV. When we excluded miscarriage from the composite adverse outcome, there was no difference in the risk of adverse pregnancy and birth outcomes among women living with and without HIV.
In our study, most women (94%) were given their STI tests results before leaving the clinic and those who had a positive diagnosis received treatment on the same day [32]. The overall finding of no association between STI diagnosis at first ANC visit and composite adverse pregnancy outcome could be a result of timely diagnosis and treatment of STIs at first ANC visit. The study provided partner referral for STI treatment, but it is not known how many men were treated for STIs. Hence, 8% of women had a STI in their postpartum visit which is a proxy for infection at delivery. More work is needed to improve partner expedited therapy and treatment, especially in pregnancy [36]. It is well documented that untreated STIs during pregnancy are associated with adverse pregnancy outcomes [1, 4, 11, 12]. However, the association found between a diagnosis with C. trachomatis and N. gonorrhoeae at first ANC visit with adverse pregnancy and birth outcomes among women living with HIV could be highlighting that there is complex interactions in STIs, HIV and pregnancy outcomes. Importantly, implementation of aetiological testing and treating of curable STIs at the first ANC visit resulted in reducation of the burden of STIs at the time of delivery. Although the optimal timing of STI management to improve pregnancy outcomes is unknown, reducing STI burden during pregnancy is likely beneficial in effort to improve maternal health during pregnancy [1, 4, 8].
In the stratified analysis by each STI, our finding of C. trachomatis and N. gonorrhoeae at first ANC visit associated with increased risk of composite adverse outcome is consistent with previous studies that have assessed this relationship [1, 5, 6, 11]. These associations were present after adjusting for maternal age, gestational age at enrolment, employment, marital status and gravidity. However, all women living with HIV in this study were on antiretroviral therapy (ART) (predominately first line efavirenz-based regimen) either prior to conception or initiated during pregnancy. It is possible that HIV and ART could have amplified the risk of having an adverse outcome as a result of in utero exposure of the foetus to HIV and or ARVs [27,28,29,30,31]. Nevertheless, the association of N. gonorrhoeae infection during pregnancy and low birthweight is biologically plausible as N. gonorrhoeae can cross the placenta, impact placental and fetal development leading to intrauterine growth restriction, which subsequently results in low birthweight [37]. C. trachomatis infection during pregnancy may infect the placenta, which may lead to preterm delivery [7, 8]. There are many possible explanations for discrepancies in findings between published studies, some showing association [1, 4,5,6,7,8, 12] and others showing no association [11, 38, 39]. Heterogeneity in studies could be due to small numbers of adverse events in underpowered studies, time of detection and treatment of the infection or inconsistency in the types of tests used for screening of STIs. The impact of STIs at different duration of pregnancy is unknown and it is not clear whether a STI in early pregnancy impacts outcomes later. C. trachomatis is associated with upper genital tract infections that result in intrauterine colonization that can occur early in gestation or preconception [40]. Therefore, timing of screening and treatment of curable STIs is an important factor to be considered when evaluating the association.
In the sensitivity analysis, we excluded miscarriage in the composite adverve outcome as the estimate of miscarriage is usually underestimated due to left truncation as women attend first ANC visit late in gestation. However, we did not find any association between STI at first ANC and adverse outcomes when we included or excluded the underestimate outcome of miscarriage in the composite adverse outcome.
This study provides important findings to suggest that universal testing of STIs at first ANC visit using diagnostic tests may be justified in routine ANC especially for pregnant women living with HIV, given the high prevalence of antenatal HIV in South Africa [25]. The integration of STI screening in routine ANC could also help reduce the risk of HIV acquisition and might help eliminate vertical HIV transmission [11].
However, the study is not without limitations. Our study over-represented women living with HIV relative to women without HIV, as the study in Tshwane District enrolled women living with HIV only. However, collating data from two geographically distinct areas increased generalizability of our study findings in South African township settings. We included an underestimate of miscarriage outcomes in our composite outcome of interest, acknowledging the limitation that most women attend for their first antenatal visit late in gestation after the typical occurrence period of miscarriage. Due to missing infant sex in our dataset, we were limited from using standardized birthweight adjusted for infant sex and gestational age to evaluate infants who were small for gestational age. Unfortunately, we could not evaluate small-for-gestational age infants as part of the composite adverse outcome. Many women were infected with STIs at first ANC and subsequent visits. However, we were not able to ascertain if women were re-infected or if it was a failure to cure. In this study, we tested for the three most common STIs (C. trachomatis, T. vaginalis and N. gonorrhoeae), but infections may co-exist and could have masked our findings. Therefore, unobserved confounding should be taken into account when interpreting our findings. Lastly, we used STI test results at postnatal visit as proxy for STI status at time of delivery which could have been biased by post-delivery selection bias whereby all women who experienced adverse pregnancy events did not return for postnatal follow up. Also, a 4 weeks window period was given for the first postnatal visit, which could have allowed for post delivery incident infection if women had resumed sexual intercourse, biasing our STI prevalence estimate at time of delivery.
Conclusion
Detecting and treating of STIs at first ANC were not associated with increased risk of having a composite adverse pregnancy outcome overall. However, in women living with HIV infection, a positive diagnosis with C. trachomatis or N. gonorrhoeae had an association with composite adverse outcome independently. Our overall finding suggest that aetiological STI testing and treating in routine ANC can provide an effective intervention urgently needed to reduce the high burden of STIs in pregnant women in South Africa, and possibly improve pregnancy outcomes. The interaction between STIs, HIV and pregnancy outcomes is complex and requires studies designed to identify clinical significance of these interations, especially in South African setting with high double burden of HIV and STIs.
Availability of data and materials
The datasets used and analysed during this current study are available from corresponding author on request.
Abbreviations
- ANC:
-
Antenatal clinic
- ARV:
-
Antiretroviral
- ART:
-
Antiretroviral therapy
- GA:
-
Gestational age
- STIs:
-
Sexually transmitted infections
References
Heumann CL, Quilter LA, Eastment MC, Heffron R, Hawes SE. Adverse birth outcomes and maternal Neisseria gonorrhoeae infection: a population-based cohort study in Washington state. Sex Transm Dis. 2017;44(5):266.
Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015;10(12):e0143304.
Reekie J, Donovan B, Guy R, Hocking JS, Kaldor JM, Mak D, et al. Risk of ectopic pregnancy and tubal infertility following gonorrhea and Chlamydia infections. Clin Infect Dis. 2019;15;69(9):1621-3.
Warr AJ, Pintye J, Kinuthia J, Drake AL, Unger JA, McClelland RS, et al. Sexually transmitted infections during pregnancy and subsequent risk of stillbirth and infant mortality in Kenya: a prospective study. Sex Transm Infect. 2019;95(1):60–6.
Adachi K, Nielsen-Saines K, Klausner JD. Chlamydia trachomatis infection in pregnancy: the global challenge of preventing adverse pregnancy and infant outcomes in sub-Saharan Africa and Asia. BioMed research international. 2016, 9315757. https://doi.org/10.1155/2016/9315757
Grant JS, Chico RM, Lee AC, Low N, Medina-Marino A, Molina RL, et al. Sexually transmitted infections in pregnancy: a narrative review of the global research gaps, challenges, and opportunities. Sex Transm Dis. 2020;47(12):779.
Rantsi T, Joki-Korpela P, Wikström E, Öhman H, Bloigu A, Lehtinen M, et al. Population-based study of prediagnostic antibodies to Chlamydia trachomatis in relation to adverse pregnancy outcome. Sex Transm Dis. 2016;43(6):382–7.
Reekie J, Roberts C, Preen D, Hocking JS, Donovan B, Ward J, et al. Chlamydia trachomatis and the risk of spontaneous preterm birth, babies who are born small for gestational age, and stillbirth: a population-based cohort study. Lancet Infect Dis. 2018;18(4):452–60.
Darville T, editor. Chlamydia trachomatis infections in neonates and young children. In Seminars in pediatric infectious diseases. WB Saunders. 2005;16(4):235-44.
Rours IG, Hammerschlag MR, Ott A, De Faber TJ, Verbrugh HA, de Groot R, et al. Chlamydia trachomatis as a cause of neonatal conjunctivitis in Dutch infants. Pediatrics. 2008;121(2):e321–e6.
Adachi K, Klausner JD, Xu J, Ank B, Bristow CC, Morgado MG, et al. Chlamydia trachomatis and Neisseria gonorrhoeae in HIV-infected pregnant women and adverse infant outcomes. Pediatr Infect Dis J. 2016;35(8):894.
Vallely LM, Egli-Gany D, Wand H, Pomat WS, Homer CS, Guy R, et al. Adverse pregnancy and neonatal outcomes associated with Neisseria gonorrhoeae: systematic review and meta-analysis. Sex Transm Infect. 2021;97(2):104–11.
World Health Organization. WHO guidelines for the treatment of Neisseria gonorrhoeae: World Health Organization; 2016. ID: who-246114
Allsworth JE, Ratner JA, Peipert JF. Trichomoniasis and other sexually transmitted infections: results from the 2001–2004 NHANES surveys. Sex Transm Dis. 2009;36(12):738.
Mann JR, McDermott S, Barnes TL, Hardin J, Bao H, Zhou L. Trichomoniasis in pregnancy and mental retardation in children. Ann Epidemiol. 2009;19(12):891–9.
Silver BJ, Guy RJ, Kaldor JM, Jamil MS, Rumbold AR. Trichomonas vaginalis as a cause of perinatal morbidity: a systematic review and meta-analysis. Sex Transm Dis. 2014;41(6):369–76.
Medline A, Joseph Davey D, Klausner JD. Lost opportunity to save newborn lives: variable national antenatal screening policies for Neisseria gonorrhoeae and Chlamydia trachomatis. Int J STD AIDS. 2017;28(7):660–6.
Davey DLJ, Nyemba DC, Gomba Y, Bekker L-G, Taleghani S, DiTullio DJ, et al. Prevalence and correlates of sexually transmitted infections in pregnancy in HIV-infected and-uninfected women in Cape Town, South Africa. PLoS One. 2019;14(7):e0218349.
Mudau M, Peters RP, De Vos L, Olivier DH, Davey DJ, Mkwanazi ES, et al. High prevalence of asymptomatic sexually transmitted infections among human immunodeficiency virus-infected pregnant women in a low-income south African community. Int J STD AIDS. 2018;29(4):324–33.
Klausner JD. The evidence that increased syphilis testing controls syphilis is compelling: what is needed to act? Clin Infect Dis. 2017;65(3):396–7.
Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiane SG, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes—estimates for 2016 and progress since 2012. PLoS One. 2019;14(2):e0211720.
Garrett NJ, Osman F, Maharaj B, Naicker N, Gibbs A, Norman E, et al. Beyond syndromic management: opportunities for diagnosis-based treatment of sexually transmitted infections in low-and middle-income countries. PLoS One. 2018;13(4):e0196209.
Morikawa E, Mudau M, Olivier D, De Vos L, Joseph Davey D, Price C, et al. Acceptability and feasibility of integrating point-of-care diagnostic testing of sexually transmitted infections into a South African antenatal care program for HIV-infected pregnant women. Infect Dis Obstet Gynecol. 2018. 3946862. https://doi.org/10.1155/2018/3946862.
Shannon CL, Bristow C, Hoff N, Wynn A, Nguyen M, Medina-Marino A, et al. Acceptability and feasibility of rapid chlamydial, Gonococcal, and Trichomonal screening and treatment in pregnant women in six Low-to-middle income countries. Sex Transm Dis. 2018;45(10):673.
Woldesenbet SA, Kufa T, Barron P, Ayalew K, Cheyip M, Chirombo BC, et al. Assessment of readiness to transition from antenatal HIV surveillance surveys to PMTCT programme data-based HIV surveillance in South Africa: the 2017 antenatal sentinel HIV survey. Int J Infect Dis. 2020;91:50–6.
Nyemba DC, Medina-Marino A, Peters RP, Klausner JD, Ngwepe P, Myer L, et al. Prevalence, incidence and associated risk factors of STIs during pregnancy in South Africa, 2021. Sex Transm Infect. 2021;97(5):375-81.
Dadabhai S, Gadama L, Chamanga R, Kawalazira R, Katumbi C, Makanani B, et al. Pregnancy outcomes in the era of universal antiretroviral treatment in sub-Saharan Africa (POISE study). J Acquir Immune Defic Syndr. 2019;80(1):7–14.
Newell M-L, Bunders MJ. Safety of antiretroviral drugs in pregnancy and breastfeeding for mother and child. Curr Opin HIV AIDS. 2013;8(5):504–10.
Santosa WB, Staines-Urias E, Tshivuila-Matala CO, Norris SA, Hemelaar J. Perinatal outcomes associated with maternal HIV and antiretroviral therapy in pregnancies with accurate gestational age in South Africa. Aids. 2019;33(10):1623–33.
Ramokolo V, Goga AE, Lombard C, Doherty T, Jackson DJ, Engebretsen IM. In utero ART exposure and birth and early growth outcomes among HIV-exposed uninfected infants attending immunization services: results from national PMTCT surveillance, South Africa. Open Forum Infect Dis. 2017;4(4):ofx187. https://doi.org/10.1093/ofid/ofx187.
Zash R, Jacobson DL, Diseko M, Mayondi G, Mmalane M, Essex M, et al. Comparative safety of antiretroviral treatment regimens in pregnancy. JAMA Pediatr. 2017;171(10):e172222–e.
South African National Department of Health. Sexually transmitted infections management guidelines, SA Health. 2018.
WHO. Maternal, newborn, child and adolescent health: Stillbirths 2020. Available at: https://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en/. Accessed 04 June 2021.
Paul A, Harris RT, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;14(2):377–81.
Zou G, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22(6):661–70.
Taleghani S, Joseph-Davey D, West SB, Klausner HJ, Wynn A, Klausner JD. Acceptability and efficacy of partner notification for curable sexually transmitted infections in sub-Saharan Africa: a systematic review. Int J STD AIDS. 2019;30(3):292–303.
De Bernabé JV, Soriano T, Albaladejo R, Juarranz M, MaE C, Martínez D, et al. Risk factors for low birth weight: a review. Eur J Obstet Gynecol Reprod Biol. 2004;116(1):3–15.
Herbst de Cortina S, Bristow CC, Joseph Davey D, Klausner JD. A systematic review of point of care testing for Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. Infect Dis Obstet Gynecol. 2016;2016. https://doi.org/10.1155/2016/4386127.
Moodley D, Sartorius B, Madurai S, Chetty V, Maman S. Pregnancy outcomes in association with STDs including genital HSV-2 shedding in a south African cohort study. Sex Transm Infect. 2017;93(7):460–6.
Folger AT. Maternal Chlamydia trachomatis infections and preterm birth: the impact of early detection and eradication during pregnancy. Matern Child Health J. 2014;18(8):1795–802.
Acknowledgements
We would like to acknowledge the participants in our studies and study staff in Tshwane and Cape Town who worked on these studies.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this research has been supported by the Eunice Kennedy Shriver Institute of Child Health and Human Development (NICHD) and National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health (NIH) under award numbers: R21HD084274-01A1 (NICHD) and R01AI149339 (NIAID) to AMM and JDK and the President’s Emergency Plan for AIDS Relief (PEPFAR) through the United States Agency for International Development under the terms of the Cooperative Agreement AID 674-A-12-00017 (AMM and PN). DJD received funding from the National Institute of Health and Fogarty International Center (K01TW011187). DJD and LM received funding from the National Institute of Mental Health (R01MH116771). We received a donation of STI Xpert® assays from Cepheid (CA, USA).
Author information
Authors and Affiliations
Contributions
DCN, DJD, RPHP and LFJ collaborated in the writing of the manuscript. DJD, RPHP and AMM designed and conducted the study and data collection. DCN performed the statistical analyses. DJD, LFJ, RPHP, AMM, JDK, LM and PN reviewed the manuscript before submission. DCN and DJD determined the hypotheses to be tested. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approvals were provided by the Institutional Review Boards at the University of Cape Town’s Faculty of Health Sciences Research Ethics Committee (UCT-HREC, reference number 454/2017), University of Pretoria’s Faculty of Health Sciences Research Ethics Committee (reference number 401/2015) and the University of California Los Angeles (reference number 15–001351). All women participating in the two studies provided informed written consent for their own participation and that of their infant’s. All methods in this study were carried out in accordance with relevant guidelines and regulations in the Helsinki Declaration as revised in 1983.
Consent for publication
Not applicable.
Competing interests
We received a donation of STI Xpert® assays from Cepheid (CA, USA).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nyemba, D.C., Peters, R.P.H., Medina-Marino, A. et al. Impact of aetiological screening of sexually transmitted infections during pregnancy on pregnancy outcomes in South Africa. BMC Pregnancy Childbirth 22, 194 (2022). https://doi.org/10.1186/s12884-022-04520-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04520-6