Abstract
Cumulative evidence has established that Interferon (IFN)-γ has both pathogenic and protective roles in Multiple Sclerosis and the animal model, Experimental Autoimmune Encephalomyelitis (EAE). However, the underlying mechanisms to the beneficial effects of IFN-γ are not well understood. In this study, we found that IFN-γ exerts therapeutic effects on chronic, relapsing-remitting, and chronic progressive EAE models. The frequency of regulatory T (Treg) cells in spinal cords from chronic EAE mice treated with IFN-γ was significantly increased with no effect on Th1 and Th17 cells. Consistently, depletion of FOXP3-expressing cells blocked the protective effects of IFN-γ, indicating that the therapeutic effect of IFN-γ depends on the presence of Treg cells. However, IFN-γ did not trigger direct in vitro differentiation of Treg cells. In vivo administration of blocking antibodies against either interleukin (IL)-10, transforming growth factor (TGF)-β or program death (PD)-1, revealed that the protective effects of IFN-γ in EAE were also dependent on TGF-β and PD-1, but not on IL-10, suggesting that IFN-γ might have an indirect role on Treg cells acting through antigen-presenting cells. Indeed, IFN-γ treatment increased the frequency of a subset of splenic CD11b+ myeloid cells expressing TGF-β-Latency Associated Peptide (LAP) and program death ligand 1 (PD-L1) in a signal transducer and activator of transcription (STAT)-1-dependent manner. Furthermore, splenic CD11b+ cells from EAE mice preconditioned in vitro with IFN-γ and myelin oligodendrocyte glycoprotein (MOG) peptide exhibited a tolerogenic phenotype with the capability to induce conversion of naïve CD4+ T cells mediated by secretion of TGF-β. Remarkably, adoptive transfer of splenic CD11b+ cells from IFN-γ-treated EAE mice into untreated recipient mice ameliorated clinical symptoms of EAE and limited central nervous system infiltration of mononuclear cells and effector helper T cells. These results reveal a novel cellular and molecular mechanism whereby IFN-γ promotes beneficial effects in EAE by endowing splenic CD11b+ myeloid cells with tolerogenic and therapeutic activities.
Similar content being viewed by others
Introduction
Multiple Sclerosis (MS) is a chronic autoimmune disease of the central nervous system (CNS), characterized by demyelination and axonal damage mediated by myelin-specific T cells [1]. Although the etiology of MS remains unknown, both genetic and environmental factors are involved in breaking self-tolerance [2, 3]. MS is classified into two main clinical forms: relapsing-remitting (RR)-MS, characterized by episodes of acute neuroinflammation followed by variable recovery periods, and progressive MS, consisting of chronic and irreversible neurological disability [4, 5]. Our understanding of the immunopathogenesis of MS and the development of therapies for this disease is largely based on the study of an animal model, experimental autoimmune encephalomyelitis (EAE) [6,7,8,9]. EAE is actively induced by immunization with myelin-derived antigens associated with adjuvant and consists of an induction phase and an effector phase. During the inductive phase of EAE, peripheral myeloid antigen-presenting cells (APC) process and present myelin antigens to naïve CD4+ T cells inducing differentiation of encephalitogenic interferon (IFN)-γ-producing Th1 and IL-17-producing Th17 cells [10, 11]. Next, during the early effector phase, innate and adaptive immune cells, including Th1 and Th17 cells, migrate from the periphery into the CNS generating a rapid and acute progression of disease leading to chronic demyelination and axonal damage [12]. Therefore, myeloid APC play a critical role in MS and EAE activating encephalitogenic T cells and perpetuating the neuroinflammatory process. However, APC also have the capability to induce activation of Forkhead box p3 (FOXP3+) regulatory T (Treg) cells through the secretion of several molecules such as interleukin (IL)-10 and tumor growth factor (TGF)-β, and the interaction of co-inhibitory molecules such as those belonging to the program death-1 (PD-1)/program-death ligands (PD-Ls) system [13,14,15,16,17]. In turn, Treg cells develop a key protective role in EAE and MS, exerting immunosuppressive activities on effector T cells and regulating disease onset and progression [18,19,20,21,22,23]. Indeed, a functional impairment of Treg cells has been related with MS pathogenesis [24,25,26,27].
IFN-γ is an essential cytokine that plays an important role in both innate and adaptive immune response. Its receptor (IFN-γR) is ubiquitously expressed on all nucleated cells in the body [28], primarily signaling through the transcription factor signal transducers and activators of transcription (STAT)-1 [29], to induce expression of multiple interferon-stimulated genes (ISGs) [30, 31]. Historically, IFN-γ is thought to have a pro-inflammatory role in MS and EAE [32,33,34]. However, several studies have paradoxically shown that IFN-γ can also mediate protective functions in EAE and MS (reviewed in [35, 36]). In MS, induction of endogenous IFN production in progressive-MS patients showed that some patients with improving symptoms had high levels of serum IFN-γ, while worsening clinical symptoms was related to low serum IFN-γ levels [37]. In EAE, cumulative evidence has demonstrated that IFN-γ signaling is necessary to suppress EAE, and that IFN-γ treatment has anti-inflammatory and tolerogenic effects on disease progression [38,39,40]. Moreover, it has been reported that the therapeutic activity of IFN-β, an extensively used therapy in RRMS patients, depends on IFN-γ signaling because IFN-β treatment has no effect on the development of disease in IFN-γR-deficient mice [41]. Also, we have shown that IFN-γ has a dual role depending on the phase of EAE: playing a pathogenic role during the inductive phase and a protective during the acute effector phase of disease [42]. Similar results have been found using neutralizing antibodies against IFN-γ in EAE mice [43]. Recently, we have reported that IFN-γ administered at the peak of EAE results in amelioration of clinical symptoms and attenuation of neuroinflammation, in a STAT-1-dependent manner. Histological analyses showed that spinal cord sections from IFN-γ-treated EAE mice exhibit significantly less infiltration of inflammatory cells and fewer demyelinated areas compared to control-treated EAE mice. Besides, IFN-γ treatment promoted a shift from activated microglia (MG) to resting MG and the induction of a subset of CX3CR1highPD-L1low MG characterized by a homeostatic and anti-inflammatory transcriptional signature [44]. Therefore, accumulative evidence has demonstrated a beneficial role of IFN-γ in EAE and MS. However, after 30 years of study, the mechanisms underlying the protective effects of IFN-γ in these pathologies remain largely unknown. Because EAE and MS are diseases mainly mediated by myelin-specific T cells, in this study we addressed the impact of IFN-γ treatment on peripheral and CNS infiltrating CD4+ T cell subpopulations, including Th1, Th17, and Treg cells, in EAE. We found that the therapeutic effect of IFN-γ requires the presence of functional FOXP3+ Treg cells, although IFN-γ does not directly regulate Treg cell differentiation. Instead, IFN-γ acts directly on splenic CD11b+ cells inducing a tolerogenic phenotype in a STAT-1-dependent manner. Interestingly, IFN-γ-stimulated splenic CD11b+ cells induce in vitro conversion of naïve CD4+ T cells to Treg cells mediated by secretion of tumor growth factor (TGF)-β. Furthermore, adoptive transfer of splenic CD11b+ cells from IFN-γ-treated EAE mice to untreated EAE mice induces disease amelioration by reducing CNS infiltration of effector helper T cells.
Materials and methods
Mice
C57BL/6 (CD45.1, CD45.2, and Stat-1−/−) mice, non-obese diabetic (NOD) mice, and SJL/J mice were purchased from The Jackson Laboratory (US). The C57BL/6-FOXP3GFP − DTR (FOXP3-DTR) mice were kindly provided by Dr. Pablo Penaloza-MacMaster (Northwestern University, US). Mice were maintained and bred at the animal core facility of Faculty of Medicine-Universidad de Chile or Center for Comparative Medicine-Northwestern University and treated in accordance with the Institutional Animal Care and Use guidelines (IACUC) of the Universidad de Chile and Northwestern University.
EAE induction, clinical scoring, and treatments
Mice 8 to 12-weeks-old were induced with different types of EAE. Chronic EAE was induced by subcutaneous (s.c.) immunization of C57BL/6 male mice with 150 µg MOG33 − 55 peptide (CPC Scientific, California, US) and 500 µg Mycobacterium tuberculosis (MT) H37Ra (BD Difco, Detroit, US) in incomplete Freund’s adjuvant (BD Difco, Detroit, US) followed by an intraperitoneal (i.p.) injection with 200 ng pertussis toxin (PTx) (Calbiochem, Campbell, US) on days 0 and 2 post-immunization (p.i.). RR-EAE was induced by s.c. immunization of SJL female mice with 150 µg PLP139 − 151 peptide. Chronic progressive EAE was induced in NOD female mice by s.c. immunization with 150 µg MOG33 − 55 peptide, 400 µg MT, and a single i.v. injection of 200 ng PTx on day 0. For treatment with IFN-γ, 1 µg/day of recombinant murine IFN-γ (Biolegend, San Diego, US) was administered i.p. for 5 days in chronic and RR-EAE or for 10 days in progressive EAE. For in vivo neutralization of PD-1, mice received two i.p. doses of 500 µg of anti-PD-1 (clone RMP1-14) or isotype Ig control (rat IgG2a, clone 2 A) at day − 2 and 0 of IFN-γ treatment. For in vivo cytokine neutralization, three doses of 100 µg anti-TGF-β (clone 1D11.16.18) and anti-IL-10 (clone JES5-2A5), or their isotype Ig control (mouse anti-IgG1, clone MOPC-2, or rat anti-IgG1, clone HRPN, respectively), were administered i.p. at days 0, 2, and 4 after IFN-γ treatment. All neutralizing antibodies and isotype controls were purchased to BioXcell (Lebanon, US). To deplete FOXP3+ Treg cells, FOXP3-DTR mice were i.p. treated with one dose of 2.5 µg of diphtheria toxin (Sigma-Aldrich, Saint Louis, Missouri, USA) at day − 2 and 0 before starting IFN-γ treatment. EAE symptoms were scored using a 0–5 scale as follows: 0, no symptoms; 1, loss of tail tone; 2. flaccid tail; 3, partial paralysis of lower extremities; 4, complete paralysis of lower extremities; 5, moribund/death (animals are humanely euthanized).
CD4+ T cell and APC phenotyping
Mice were perfused intracardially with PBS and brains and spinal cords were isolated and incubated with DNAse (10 units/mL) (New England Biolabs, Ipswich, US) and collagenase D (0.5 mg/mL) (Roche, Manheim, Germany) for 1 h at 37 °C. Then, tissues were disaggregated and centrifuged. Mononuclear cells were obtained using a discontinuous Percoll gradient (Amersham, Piscataway, US). Draining cervical/axillary lymph nodes (LN) and spleens were screened to yield single cell suspensions and splenocytes were treated with red blood lysis buffer (155mM NH4Cl, 10mM KHCO3, y 1mM EDTA, pH 7.3). For T cell flow cytometry analysis, cells were first stimulated with PMA (50 ng/mL)/ionomycin (500 ng/mL) (Sigma-Aldrich, Saint Louis, US) and Brefeldin A (5 µg/mL) (Sigma-Aldrich, Saint Louis, US) for 4 h. Then, cells were stained with LIVE/DEAD™ Fixable dye-Dead Cell Stain Kit (Thermofisher, Carlsbad, US) to determine viability, blocked with Fc Block (Biolegend, San Diego, US) and fixed/permeabilized with FOXP3/transcription factor staining buffer set (eBioscience, San Diego, US) for intracellular staining. A T-cell staining panel consisting of the following markers was used: CD45, CD3, CD4, CD25, FOXP3, IFN-y and IL-17 A. The APC staining panel included the following markers: CD45, CD11b, TGF-β-Latency Associated Peptide (LAP), PD-L1, PD-L2, CD80, CD86 and MHC-II. All antibodies were purchased from Biolegend (San Diego, California, US). Samples were acquired with FACS LSR Fortessa at University of Chile or FACS Celesta (BD bioscience, New Jersey, US) at Northwestern University and analyzed with Flowjo X v10.7 software (Tree Star, Ashland, Oregon, US). Gating flow cytometry strategies are represented in Supplementary Fig. 1.
Cell purification
CD4+CD25− and CD4+CD25+ T cells were isolated by immunomagnetic selection using the EasySep™ mouse CD4+CD25+ regulatory T cell isolation kit II (> 90% purity). CD4+CD62L+CD44low naïve CD4+ T cells were isolated using the EasySep™ mouse CD4+ T cell isolation kit (> 95% purity). CD11b+ cells were purified using the EasySep™ mouse CD11b positive selection kit II (> 87% purity). All purification kits were from Stem Cell (Vancouver, Canada).
Treg cell induction by IFN-γ
CD4+CD25− and CD4+CD25+ T cells isolated from the spleen and LN of mice at the peak of the disease (day 12–15 p.i.) were cultured with serum-free X-VIVO 20 medium (Lonza, Basel, Switzerland) in the presence of 2 µg/mL of plate-bound anti-CD3 antibody and 1 µg/mL of soluble anti-CD28 antibody (both from Biolegend, San Diego, California, US), with or without IFN-γ, at 37 °C for 3 days. Different concentrations of IFN-γ (1, 10, 25, 50, and 100 ng/mL) were tested (Supplementary Fig. 3B) to select the final concentration of 25 ng/mL, which was previously described to induce Treg cells in similar conditions [45]. Controls with 5 µg/mL anti-IFN-γ antibody or isotype control antibody were used. Similar experiments were also performed in the presence of TGF-β (2 ng/mL) and IL-2 (10 ng/mL) (both from Thermofisher, Waltham, Massachusetts, US) to induce differentiation of Treg cells (iTreg conditions). Cell culture supernatants were collected and stored frozen for further cytokine analysis. The frequency of FOXP3+ Treg cells and the expression of CTLA-4, LAG-3, HELIOS, and TGF-β-LAP were determined by flow cytometry.
Treg cell induction by IFN-γ-stimulated CD11b+ cells
CD11b+ cells isolated from the spleen of EAE mice at the peak of the disease (day 12–15 p.i.) were cultured in the presence of 10 µg/mL MOG33 − 55 peptide and stimulated with 25 ng/mL IFN-γ for 24–72 h. The expression of TGF-β-LAP, PD-L1, PD-L2, CD80, CD86, and MHC-II was determined by flow cytometry. Cell culture supernatants were collected to determine TGF-β levels. In other assays, CD11b+ purified cells from the spleen of EAE mice were preconditioned with 10 µg/mL MOG33 − 55 peptide and 25 ng/mL IFN-γ for 24 h, washed, and co-cultured with naïve CD4+ T cells (ratio 1:1) from non-immunized mice in the presence of 1 µg/mL soluble anti-CD3 antibody (Biolegend, San Diego, California, US) and with either 5 µg/mL anti-TGF-β antibody (BioXcell, Lebanon, US) or anti-PD-L1 antibody (Thermofisher, Carlsbad, US), and their isotype control antibodies. After 72 h, the frequency of Treg (CD4+CD25+FOXP3+) cells was determined by flow cytometry.
Adoptive transfer of splenic CD11b+ cells from IFN-γ-treated EAE mice into recipient EAE mice
CD11b+ cells (1 × 106) were purified from spleens of CD45.1+ EAE mice treated with IFN-γ or PBS for 5 days and i.v. transferred into untreated CD45.2+ EAE mice at the peak of disease. After 3 days, splenocytes and mononuclear cells from spinal cords of recipient EAE mice were isolated and absolute cell number and frequencies of mononuclear cells, CD45.2+ cells, CD45.1+CD11b+ cells, CD3+ T cells, CD3+CD4+ T cells, CD3+CD4− T cells, CD3+CD4+CD25+FOXP3− T cells, and Treg cells (CD3+CD4+CD25+FOXP3+) were determined by flow cytometry.
Cytokine measurements
Cell culture supernatants were used to determine the levels of TGF-β1, IL-10, IL-27, Granzyme B, and sFASL by MILLIPLEX® Multiplex Assay kits (Millipore-Sigma, Saint Louis, US) and quantitated using the Luminex® 200™ System (Northbrook, Illinois, US).
Statistical analysis
Results were analyzed using a Mann–Whitney U test or Kruskal-Wallis test. For comparison of EAE scores between two or multiple groups, we conducted two-way ANOVA or one-way ANOVA followed by multiple comparisons with Bonferroni post-hoc test. Statistical analyses were performed with GraphPad Prism v.9.0 software (San Diego, California, US). All data are presented as mean ± SEM. Values were considered statistically significant when p < 0.05.
Results
Therapeutic effect of IFN-γ is dependent on FOXP3+ Treg cells in EAE
First, we confirmed that treatment of C57BL/6 mice developing chronic EAE with IFN-γ for 5 days starting at peak of disease induced a significant suppression of clinical symptoms. After cessation of treatment, disease severity slowly returned to levels similar to control EAE mice (Fig. 1A). Next, we asked whether IFN-γ might have beneficial effects in two other clinically distinct EAE models mimicking RRMS (SJL/J mice) and chronic progressive MS (NOD mice). The results showed that IFN-γ administered at the peak of the first flare of RR-EAE (SJL mice) induced a significant attenuation of clinical symptoms and prevention of further relapses compared to PBS-treated mice (Fig. 1B). In addition, IFN-γ treatment promoted significant suppression of disease in chronic progressive EAE mice (NOD mice) after 10 days of treatment (Fig. 1C).
Therapeutic administration of IFN-γ ameliorates clinical severity in chronic, relapsing-remitting, and chronic progressive-EAE. (A) Two groups of C57BL/6 mice were induced with chronic EAE (n = 9/group) and daily treated with 1 µg IFN-γ (empty black circles) or PBS (solid black circles) at peak of disease for 5 days. (B) SJL mice were induced with relapsing-remitting (RR)-EAE (n = 6/group) and daily treated with 1 µg IFN-γ (empty black circles) or PBS (solid black circles) at peak of the first flare for 5 days. (C) Chronic progressive-EAE was induced in NOD mice (n = 13/group) and treated with 1 µg IFN-γ (empty black circles) or PBS (solid black circles) during the chronic phase of the disease (starting at 45 days post-immunization) for 10 days. Clinical symptoms were monitored daily using the standard scoring scale. Results are shown as the mean ± SEM. Data were analyzed using two-way ANOVA followed by Bonferroni post-hoc test. *p < 0.05, **p < 0.01
Next, we investigated the impact of IFN-γ treatment on peripheral and CNS-infiltrating CD4+ T cell subpopulations in chronic MOG35 − 55 peptide EAE in B6 mice. Spinal cords isolated from EAE mice treated with IFN-γ for 5 days (Fig. 2A) exhibited a significant reduction in the number of mononuclear cells (MNC) and infiltrating CD45+ cells compared with those from PBS-treated EAE mice (Fig. 2B). There was no statistical difference in the absolute number of MNC and CD45+ cells in brains from IFN-γ and PBS-treated EAE mice and similar numbers of cells were found in spleen and LN from both groups of EAE mice (Supplementary Fig. 2A). Lower absolute numbers of CD3+ T cells were observed in IFN-γ-treated EAE mice compared to PBS-treated EAE mice, but this difference did not reach statistical significance (Fig. 2B). Analysis of the impact of IFN-γ on different subpopulations of CD4+ T lymphocytes (Supplementary Fig. 1A and B) showed a lower absolute number of CD4+ T cells and Th1 cells in spinal cords from IFN-γ-treated EAE mice than in control EAE mice, but these differences were not significant. The number of Th17 and Treg cells was similar between both groups of mice (Fig. 2C). The absence of impact on Th17 and Treg cell number led us to determine if the frequencies might be modulated by IFN-γ treatment. Similar frequencies of CD4+ T cells and Th1 cells and a slight but not significant increase of Th17 cells were determined in spinal cords from IFN-γ and PBS-treated EAE mice. Notably, a significantly higher frequency of Treg cells was found in spinal cords from IFN-γ-treated EAE mice (Fig. 2D). No significant differences in numbers or frequencies of CD4+ T cell subpopulations were observed in the brain and secondary lymphoid organs (cervical/axillary draining LN and spleen); although the absolute number of Treg cells tended to be higher in brains and spleens of IFN-γ-treated EAE mice (Supplementary Fig. 2B). These results led us to examine the functional requirement of Treg cells in mediating the protective effect of IFN-γ in EAE. To do that, we used the transgenic FOXP3-DTR mouse model, which allows the conditional depletion of FOXP3+ Treg cells after systemic administration of diphtheria toxin (Supplementary Fig. 2C). Consistent with a previous study [21], depletion of FOXP3+ Treg cells at the peak of EAE induced a more severe disease over time. Interestingly, EAE mice depleted of Treg cells were refractory to the protective effects of IFN-γ, suggesting that functional Treg cells are required at the time of IFN-γ treatment for effective therapeutic regulation of EAE (Fig. 2E).
Therapeutic effect of IFN-γ depends on the presence of FOXP3+ Treg cells in EAE. (A) Mice induced with chronic EAE were treated daily with 1 µg IFN-γ (empty black circles) or PBS (solid black circles) at the peak of disease for five days (n = 10/group, mean of three independent experiment). (B-D) At the end of treatment, spinal cords were isolated and the absolute number of (B) mononuclear cells (MNC), CD45+ cells, and CD3+ cells, and (C) the absolute number and (D) frequency of CD4+ T cells, Th1, Th17 and Treg cells were determined by flow cytometry. (E) Wild type (n = 13/group) and FOXP3-DTR mice (n = 5/group) were induced with EAE and treated with 1 µg IFN-γ (empty black and red circles) or PBS (solid black and red circles) at the peak of disease for five days. To deplete FOXP3+ Treg cells, FOXP3-DTR mice were i.p. treated with one dose 2.5 µg of diphtheria toxin (DTx) two days before starting IFN-γ treatment and with another similar dose two days later. Three independent experiments were pooled. Results are shown as the mean ± SEM. Data were analyzed using two-way ANOVA followed by Bonferroni post-hoc test (A), Mann–Whitney U test (B-D), or one-way ANOVA followed by Bonferroni post-hoc test (E). *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001
IFN-γ does not exert a direct effect on Treg cell differentiation
In order to determine whether IFN-γ might directly trigger the conversion of CD4+CD25− T cells into Treg cells, CD4+CD25− T cells were purified from spleen and draining LN of EAE mice at the peak of the disease (> 90% purity, Supplementary Fig. 3A) and in vitro activated with anti-CD3 and anti-CD28 antibodies with IFN-γ or anti-IFN-γ antibody for 72 h. Different concentrations of IFN-γ (range between 1 and 100 ng/ml) did not induce conversion of CD4+CD25− T cells isolated from spleen or LN of EAE mice into Treg cells (Fig. 3A and Supplementary Fig. 3B). Next, we analyzed whether IFN-γ might have a direct effect on the generation of inducible Treg cells (iTreg) promoted by TGF-β and IL-2. The results showed that addition of IFN-γ did not change the frequency of iTreg cells starting from CD4+CD25− T cells isolated from spleens or LN (Fig. 3B). Moreover, addition of blocking antibodies to IFN-γ led to significantly higher generation of iTreg cells compared to untreated and IFN-γ-stimulated CD4+CD25− T cells (Fig. 3B). We also determined whether IFN-γ might have a direct effect on the fraction of CD4+CD25+ T cells obtained during the purification of CD4+CD25− T cells (> 89% of total FOXP3+ cells - Supplementary Fig. 3A). IFN-γ treatment did not affect the expression of regulatory markers associated with Treg cells such as FOXP3, CTLA-4, HELIOS, LAG-3, and TGF-β-LAP (Fig. 3C) or the secretion of IL-10, Granzyme B, and soluble FAS ligand (Fig. 3D) in CD4+CD25+ T cells in vitro activated with anti-CD3 and anti-CD28 antibodies. Taken together, these results indicate that IFN-γ does not directly promote the generation of Treg cells, but does, in fact, inhibits the differentiation of iTreg cells.
IFN-γ does not exert a direct effect on Treg cell differentiation. (A) CD4+CD25− T cells isolated (purity > 90%) from spleen or draining lymph nodes (LN) of EAE mice at the peak of disease were stimulated for 3 days with 2 µg/mL plate-bound anti-CD3 and 1 µg/mL soluble anti-CD28 in the absence (control) or presence of either 25 ng/mL IFN-γ, 5 µg/mL anti-IFN-γ antibody or 5 µg/mL isotype control antibody. (B) Similar assay as described in (A) in the presence of 2 ng/mL TGF-β and 10 ng/mL IL-2 to promote differentiation of inducible Treg cells (iTregs). The frequency of Treg cells (CD3+CD4+CD25+FOXP3+) was determined by flow cytometry. (C) Purified fraction of CD4+CD25+ cells (containing > 82% of Treg cells) obtained during the purification of CD4+CD25− T cells were stimulated with 2 µg/mL plate-bound anti-CD3 and 1 µg/mL soluble anti-CD28 for 3 days in the absence (control, solid gray bars) or presence of 25 ng/mL IFN-γ (empty gray bars). The expression of regulatory markers FOXP3, HELIOS, CTLA-4, LAG-3 and TGF-β-LAP was determined as median fluorescence intensity (MFI) by flow cytometry. (D) Secretion of IL-10, Granzyme B and sFASL in cell culture supernatants was assessed by multiplex assay. Results are shown as the mean ± SEM (n = 4). Data were analyzed using Mann–Whitney U test. *p < 0.05
Therapeutic effect of IFN-γ is dependent on TGF-β and PD-1
Because IFN-γ has no direct effect on the induction of Treg cells, we asked if this cytokine might modulate regulatory molecules involved in the differentiation and activity of FOXP3+ Treg cells, such as TGF-β [46], IL-10 [47], and PD-1 [16]. As expected, in vivo blockade of either TGF-β or IL-10 in untreated (without IFN-γ) EAE mice slightly exacerbated disease severity compared to control groups. Interestingly, neutralization of TGF-β, but not IL-10, interfered with the protective effects of IFN-γ on EAE (Fig. 4A and B). Similarly, disease amelioration induced by IFN-γ was prevented when EAE mice were administered blocking antibodies to PD-1 (Fig. 4C). Based on these results, we hypothesized that IFN-γ might have an indirect role on FOXP3+ Treg cells regulating the expression of TGF-β and ligands of PD-1 in APC.
Therapeutic effect of IFN-γ is dependent on TGF-β and PD-1. EAE mice were treated at the peak of disease for 5 days with 1 µg/day IFN-γ alone (empty black circles) or along with (A) 100 µg of neutralizing antibody against TGF-β (solid blue circles, n = 6) or (B) IL-10 (solid blue circles, n = 7) administered at days 0, 2 and 4 after IFN-γ treatment, or with (C) 500 µg neutralizing anti-PD-1 antibody (solid blue circles, n = 8) administered two days before starting IFN-γ treatment and at the same time of IFN-γ treatment. Control EAE mice were treated with PBS (vehicle, solid black circles) or corresponding isotype antibody alone (empty red circles) or along with IFN-y (empty blue circles). Two independent experiments were pooled. Results are shown as the mean ± SEM. Data were analyzed using one-way ANOVA followed by the Bonferroni post-hoc test. *p < 0.05, **p < 0.01
IFN-γ/STAT1 axis induces a subset of splenic CD11b+ myeloid cells expressing PD-L1 and TGF-β in EAE mice
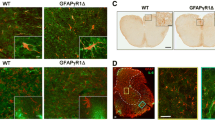
To address the above hypothesis, we determined the impact of IFN-γ on myeloid APC in EAE by analyzing the frequency of CD11b+ myeloid cells expressing PD-L1 and TGF-β-LAP in brain, spinal cord, spleen, and LN from EAE mice. The results showed that the frequency of CD11b+ cells expressing PD-L1 and TGF-β-LAP was significantly higher in the spleen from IFN-γ-treated EAE mice than in those from PBS-treated EAE mice. There was no difference in other organs (Fig. 5A).
IFN-γ/STAT-1 axis induces splenic CD11b+ myeloid cells expressing PD-L1 and TGF-β-LAP. (A) Frequency of PD-L1+ and TGF-β-LAP+ CD11b+ cells in brain, spinal cord (SC), draining lymph nodes (LN) and spleen from EAE mice treated at the peak of disease with IFN-γ (empty gray bars, n = 4) or PBS (solid gray bars, n = 5) for 5 days was determined by flow cytometry. (B) Frequency of CD11b+PD-L1+ cells and (C) CD11b+TGF-β-LAP+ cells were determined by flow cytometry in spleen from wild-type mice (solid and empty gray bars, n = 6) and STAT-1 deficient mice (solid and empty red bars, n = 6) induced with EAE and treated at the peak of disease with IFN-γ (empty bars) or PBS (vehicle, solid bars) for 5 days. Three independent experiments were pooled. Results are shown as the mean ± SEM. Data were analyzed using Mann–Whitney U or Kruskal-Wallis test. *p < 0.05, **p < 0.01
The biological activity of IFN-γ is mainly mediated through STAT-1, thus we determined whether the in vivo modulation of splenic CD11b+ myeloid cells by IFN-γ is also dependent on STAT-1. We found that the enhanced frequency of CD11b+ cells expressing PD-L1 and TGF-β-LAP induced by IFN-γ was significantly reversed in EAE mice lacking STAT-1 (Fig. 5B and C). Therefore, these results indicate that the IFN-γ-STAT-1 axis mediates protective effects in EAE via inducing a subset of splenic CD11b+ myeloid cells expressing PD-L1 and TGF-β-LAP.
IFN-γ acts directly on splenic CD11b+ cells inducing a tolerogenic phenotype and function
Next, we wanted to determine whether IFN-γ might directly regulate the expression of PD-L1, TGF-β-LAP, and other molecules involved in T cell activation on CD11b+ myeloid cells. CD11b+ cells isolated from spleen (> 87% purity, Supplementary Fig. 4) at peak EAE were stimulated with IFN-γ and MOG35 − 55 peptide for 24–72 h and the expression of TGF-β-LAP, co-inhibitory molecules (PD-L1 and PD-L2), co-stimulatory molecules (CD80 and CD86), and MHC-II molecules was evaluated by flow cytometry. The levels of secreted TGF-β were assessed in the cell culture supernatant by multiplex assay. The results showed that CD11b+ cells treated with IFN-γ for 24 h presented a significantly lower expression of TGF-β-LAP on the cell surface, as measured by mean fluorescence intensity (MFI), which was associated with a higher secretion of TGF-β1 compared to unstimulated cells (Fig. 6A and C); suggesting an enhanced processing and secretion of TGF-β in response to IFN-γ in these cells. After 72 h, IFN-γ-treated CD11b+ cells showed a significantly higher expression of TGF-β-LAP+ on the cell surface but a similar secretion of TGF-β than untreated CD11b+ cells (Fig. 6B and C). Given that it has been reported that IL-27, a cytokine induced by IFN-γ, is involved in antigen-specific immune tolerance in EAE by inducing PD-L1 expression in dendritic cells and production of IL-10 in CD4+ T cells [48, 49], we also determined the levels of IL-27 and IL-10 in the cell culture supernatant. The results showed that splenic CD11b+ cells from EAE mice secreted low levels of IL-27 and IL-10 and that they were not induced by IFN-γ after 24 and 72 h of treatment (Supplementary Fig. 5A). Remarkably, stimulation with IFN-γ for 24 h and 72 h induced a significantly higher frequency of CD11b+ cells expressing PD-L1 as well as a higher expression of PD-L1 compared to untreated CD11b+ cells (Fig. 6A and B). The expression of PD-L2 on CD11b+ cells was significantly lower in IFN-γ-treated CD11b+ cells than untreated cells at 24 h, and the frequency of CD11b+ cells expressing PD-L2 was also significantly reduced after 72 h.
IFN-γ directly induces a tolerogenic phenotype and function in splenic CD11b+ cells from EAE mice. Splenic CD11b+ cells isolated from EAE mice were in vitro stimulated with 25 ng/mL IFN-γ (empty gray bars) or left untreated (UN, solid gray bars) for (A) 24 and (B) 72 h in the presence of 10 µg/mL MOG33 − 55 peptide. Frequency and median fluorescence intensity (MFI) of TGF-β-LAP, PD-L1, PD-L2, CD80, CD86 and MHC-II were analyzed by flow cytometry (n = 4). (C) Cell culture supernatants were collected at 24 and 72 h and concentration of TGF-β1 was measured by multiplex assay (n = 8). (D) Splenic CD11b+ cells from EAE mice were preconditioned with 10 µg/mL MOG33 − 55 peptide and 25 ng/mL IFN-γ for 24 h, washed, and co-cultured with naïve CD4+ T cells (ratio 1:1) from healthy mice in the presence of 1 µg/mL soluble anti-CD3 antibody and with either anti-TGF-β antibody (solid blue bar), anti-PD-L1 antibody (solid red bar), or corresponding isotype control antibodies (empty blue and red bars). After 72 h, the frequency of Treg cells (CD4+CD25+FOXP3+) was determined by flow cytometry. Results are shown as the mean ± SEM. Data were analyzed using Mann–Whitney U test. *p < 0.05, **p < 0.01
The frequency of CD11b+ cells expressing CD80 and CD86 was initially increased at 24 h by IFN-γ but decreased to control levels after 72 h. The expression of CD80 was significantly lower in response to IFN-γ after 72 h (Fig. 6A and B). Although there was no difference in the frequency of CD11b+ cells expressing MHC-II molecules, CD11b+ cells stimulated with IFN-γ showed significantly lower expression of MHC-II molecules at 24 h compared to untreated CD11b+ cells (Fig. 6A). After 72 h, IFN-γ induced a significantly higher frequency of CD11b+MHC-II+ cells but with a similar level of expression of MHC-II molecules than control cells (Fig. 6B). Taken together, these results suggest that IFN-γ acts directly on CD11b+ cells regulating the expression of molecules involved in immune tolerance resulting in an early secretion of TGF-β1, enhanced expression of PD-L1 and CD86, and decreased expression of MHC-II molecules, followed by an increased expression of TGF-β-LAP and PD-L1, and a reduced expression of CD80.
Therefore, we next investigated the capability of IFN-γ-treated CD11b+ cells to induce differentiation of Treg cells. CD11b+ cells isolated from spleen at peak EAE were cultured in the presence of IFN-γ and MOG35 − 55 peptide for 24 h, washed, and then co-cultured with naïve CD4+ T cells from healthy mice (1:1 ratio) and soluble anti-CD3 antibody for 72 h. The expression of FOXP3+ (MFI) in CD4+ T cells and the frequency of Treg cells (CD4+CD25+FOXP3+) was significantly higher in naïve CD4+ T cells co-cultured with IFN-γ-stimulated CD11b+ cells than with untreated CD11b+ cells (Fig. 6D and Supplementary Fig. 5B). Interestingly, neutralization of TGF-β, but not of PD-L1, significantly decreased the expression of FOXP3+ in CD4+ T cells and the frequency of Treg cells to a similar level of untreated cells. These results indicate that IFN-γ induces tolerogenic splenic CD11b+ cells with the capability to convert naïve CD4+ T cells into Treg cells.
Transfer of CD11b+ myeloid cells from IFN-γ-treated EAE mice to untreated EAE mice induces disease amelioration by reducing CNS-infiltrating helper T cells
To demonstrate the therapeutic and tolerogenic potential of splenic CD11b+ myeloid cells induced by IFN-γ, these cells were isolated from IFN-γ or PBS-treated EAE mice (CD45.1) and transferred to untreated EAE mice (CD45.2) at the peak of EAE. EAE mice receiving a single injection of splenic CD11b+ myeloid cells from IFN-γ-treated EAE mice exhibited a significant and rapid amelioration of clinical symptoms followed by a relapse of disease compared to control EAE mice receiving CD11b+ cells from PBS-treated EAE mice (Fig. 7A). After three days of transfer, the total number of mononuclear cells and CD45.2+ cells were significantly lower in spinal cord from EAE mice receiving splenic CD11b+ cells from IFN-γ-treated EAE mice than those receiving splenic CD11b+ myeloid cells from PBS-treated EAE mice (Fig. 7B). Instead, the absolute cell number and frequency of CD45.1+CD11b+ cells in spinal cord were not significantly different between both groups of recipients EAE mice (Fig. 7B). There was also no difference in the absolute cell number and frequency of CD45.2+ cells and CD45.1+CD11b+ cells in the spleen from both groups of recipients EAE mice (Supplementary Fig. 6A). Interestingly, spinal cords from EAE mice receiving CD11b+ myeloid cells from IFN-γ-treated EAE mice exhibited a significantly lower absolute number of CD3+ T cells, CD3+CD4+ T helper cells, CD3+CD4− cells, and CD25+FOXP3− cells compared to spinal cords from EAE mice receiving CD11b+ myeloid cells from PBS-treated EAE mice. Likewise, the absolute number of Treg cells was lower in EAE mice receiving CD11b+ myeloid cells from IFN-γ-treated EAE mice; but it did not reach statistical significance (Fig. 7C). Although reduction in all these cell populations might be influenced by the lower absolute numbers of total mononuclear cells observed in spinal cord from EAE mice receiving CD11b+ myeloid cells from IFN-γ-treated EAE mice (Fig. 7B), the frequency of CD3+ T cells and CD3+CD4+ helper T cells was also significantly lower in recipients of CD11b+ myeloid cells from IFN-γ-treated EAE mice (Fig. 7C). There was no difference in the absolute cell number and frequency of all T cell subpopulations analyzed in spleen from both groups of recipients EAE mice (Supplementary Fig. 6B). Taken together, these results indicate that adoptive transfer of splenic CD11b+ myeloid cells from IFN-γ-treated EAE mice to recipient (untreated) EAE mice suppresses disease progression by limiting CNS-infiltrating effector helper T cells.
Adoptive transfer of splenic CD11b+ cells from IFN-γ-treated EAE mice into recipient EAE mice suppresses disease progression. (A) Splenic CD11b+ cells (106) from CD45.1 EAE mice treated for 5 days with IFN-γ (empty black circles) or PBS (solid black circles) were i.v. transferred into CD45.2 EAE mice at the peak of disease (n = 15). Clinical symptoms were monitored daily. Four independent experiments were pooled. (B-C) After three days of transfer, mononuclear cells from spinal cords of recipient EAE mice receiving CD45.1+CD11b+ cells from EAE mice treated with IFN-γ (empty gray bars, n = 8) or PBS (solid gray bars, n = 8) were isolated and absolute number and frequencies of (B) mononuclear cells (MNC), CD45.2+ cells, and CD45.1+CD11b+ cells, and (C) CD3+ T cells, CD3+CD4+ T cells, CD3+CD4− T cells, CD3+CD4+CD25+FOXP3− T cells, and Treg cells (CD3+CD4+CD25+FOXP3+), were determined by flow cytometry (n = 8, two different experiments were pooled). Results are shown as the mean ± SEM. Data were analyzed using two-way ANOVA followed by the Bonferroni post-hoc test (A) or Mann–Whitney U test (B-C). *p < 0.05, **p < 0.01, ***p < 0.001
Discussion
IFN-γ is primarily considered a pro-inflammatory cytokine based on its key role against infections and tumors as well as the promotion of Th1 cell-driven inflammation. However, cumulative evidence has revealed that IFN-γ also exerts protective effects in EAE (reviewed in [35, 36, 42, 44]). Here, we provide further support for these findings, demonstrating that IFN-γ limits the magnitude of new relapses in RR-EAE and slows clinical course in chronic progressive EAE. Also, beneficial effects of IFN-γ have been reported in other murine models of transplantation, asthma, and autoimmune diseases such as collagen-induced arthritis (CIA), experimental autoimmune uveitis (EAU), autoimmune nephritis, and autoimmune myocarditis [50,51,52,53,54,55,56,57,58]. More recently, we have shown that IFN-γ is essential for maintaining immune tolerance to aquaporin-4 (AQP4) antigen and that its absence leads to autoimmune inflammation and severe clinical disease resembling AQP4-IgG+ neuromyelitis optica spectrum disorders (NMOSD) [59].
Treg cells play a critical role in maintaining immune tolerance in EAE and MS [60]. Indeed, FOXP3+-depleted EAE mice exhibit worsening of disease associated with a significant increase in CNS-infiltrating CD4+ T effector cells [21]. In addition, several reports have shown that there is a dysregulation in the Treg cell population in both MS and EAE due to either a reduction in their frequency [61, 62], or in their functionality [18, 25, 63]. In this study, we found that although the therapeutic activity of IFN-γ in EAE is dependent on the presence of functional Treg cells, IFN-γ does not trigger direct differentiation of FOPX3+ Treg cells and; on the contrary, in vitro neutralization of IFN-γ induces an increase in their cell number. Consistent with our findings, several studies have shown that IFN-γ inhibits the in vitro and in vivo development of Treg cells and that the neutralization of IFN-γ markedly promotes the differentiation and suppressive function of iTregs [64,65,66,67]. Furthermore, some reports have included antibodies against IFN-γ to improve in vitro differentiation of iTreg cells [65, 68]. In contrast, Wang et al., reported that IFN-γ can directly induce in vitro FOXP3 expression in murine TCR-stimulated CD4+CD25− T cells and that their transfer to EAE recipient mice reduced clinical symptoms. Furthermore, IFN-γ induced, in a dose-dependent manner, increased expression of FOXP3 in CD4+CD25− T cells from healthy individuals and the resulting Treg cells inhibited autologous T cell proliferation [45]. Similarly, IFN-γ promoted a significant increase in the conversion of TCR-stimulated CD4+CD25− T cells to suppressive CD4+CD25+FOXP3+ T cells in patients with Guillain-Barré syndrome or myasthenia gravis [69, 70]. Another study showed that differentiation of iTreg cells starting from healthy human CD4+CD45RA+ T cells in the presence of IFN-γ exhibited higher expression of FOXP3 than iTreg cells differentiated only with TGF-β and both TGF-β-induced iTreg cells and IFN-γ-boosted iTreg cells had similar suppressive activity [71]. Therefore, the role of IFN-γ in the conversion of CD4+CD25− T cells to Treg cells is controversial. The difference between these results might be explained by the microenvironment from which CD4+ T cells were isolated. Wang et al. [45], generated FOXP3+ Treg cells from CD4+CD25− T cells obtained from the spleen of unprimed (without EAE) mice. In this study, we used CD4+CD25− T cells obtained from LN and spleens of EAE mice. In addition, the conversion rate of CD4+CD25− T cells into CD4+CD25+FOXP3+ T cells was significantly higher in healthy individuals than in patients with Guillain-Barré syndrome or myasthenia gravis [69, 70]. Therefore, the response of CD4+CD25− T cells to IFN-γ may differ between patients and healthy subjects and between patients in different stages of disease. In the same way, the inflammatory microenvironment might also affect the responsiveness of Treg cells to signals promoting suppressive activity, such as IFN-γ. Supporting this notion, it has been reported that FOXP3+ Treg cells readily accumulate in the CNS of EAE mice, but they are unable to inhibit MOG35 − 55 peptide-specific effector T cells derived from the CNS at the peak of inflammation due to their production of IL-6 and TNF [18, 72].
It has been reported that RRMS patients exhibit a significantly higher percentage of Treg cells producing IFN-γ than healthy individuals. Furthermore, the in vitro suppressive activity of IFN-γ+FOXP3+ Treg cells from RRMS patients was significantly lower than that from healthy controls. Besides, blocking IFN-γ significantly increased the suppressive activity of IFN-γ+FOXP3+ Treg cells from RRMS patients, but not to the same level of suppressive activity as IFN-γ+FOXP3+ Treg cells from healthy subjects [66]. Therefore, these results suggest that the dual role of IFN-γ on the differentiation and tolerogenic function of Treg cells might be determined by the conditions of the particular inflammatory microenvironment. Indeed, we and other investigators have found that the opposite roles of IFN-γ in EAE are dependent on the stage of disease: pathogenic during the induction phase of EAE, but beneficial during the early and chronic effector phases [39, 42,43,44, 73].
Our results show that the therapeutic activity of IFN-γ in EAE also depends on TGF-β and PD-1. PD-1 is a co-inhibitory surface receptor that plays a pivotal role in regulating T cell activation. The interaction between PD-1 and its ligands PD-L1 and PD-L2 regulates peripheral CD4+ and CD8+ T cell tolerance attenuating self-reactive T cell response and promoting Treg cell differentiation and function [16]. In particular, expression of PD-L1 is regulated by IFN-γ and this ligand has a critical regulatory role in EAE [16, 74,75,76,77,78]. In turn, TGF-β has been described as one of the most essential cytokines involved in Treg cell development and function as well as a key factor regulating EAE development [46, 79,80,81]. Interestingly, Treg cell conversion induced by splenic DCs in a tumor microenvironment is dependent on TGF-β and PD-L1 signaling [82]. In addition, Casella et al. [49], have described that antigen-specific tolerance induction by intravenous injection of high doses of autoantigen halts EAE progression by inducing PD-L1 expression in CNS monocyte-derived DCs via IFN-γ/IL-27-dependent mechanism. Based on this evidence, we hypothesized that IFN-γ might have an indirect role on FOXP3+ Treg cells by inducing expression of TGF-β and ligands of PD-1 in APC. In line with our hypothesis, we found that IFN-γ induces an increased frequency of a subset of splenic CD11b+ cells expressing PD-L1 and TGF-β-LAP+ in EAE. Furthermore, our ex vivo assays show that IFN-γ acts directly on CD11b+ cells inducing a tolerogenic phenotype characterized by an early secretion of TGF-β1, enhanced expression of PD-L1, and decreased expression of MHC-II molecules, followed by an increased expression of TGF-β-LAP and PD-L1, and a reduced expression of CD80. IL-27 and IL-10 are not induced by IFN-γ and they would not be involved in the tolerogenic mechanism mediated by IFN-γ. Consistently, in vivo neutralization of IL-10 does not interfere with the protective effects of IFN-γ on EAE. Notably, IFN-γ-treated CD11b+ cells promote antigen-specific conversion of CD4+ T cells into Treg cells through the secretion of TGF-β. Because PD-L1 was not involved in this process, it is not ruled out that the role of PD-1 in EAE is partially independent of Treg induction. In this case, it is plausible that the role of PD-1 is rather related with attenuation of self-reactive T cell response [16]. Supporting our results showing that the beneficial activity of IFN-γ is dependent on TGF-β, we have recently found that primary myeloid cells/microglia cultures obtained from spinal cord of IFN-γ-treated EAE mice that were ex vivo re-stimulated with low dose (1 ng/ml) IFN-γ and MOG35 − 55 peptide showed significantly enhanced tolerogenic activity, promoting induction of CD4+ Treg cells associated with increased TGF-β secretion [44]. Additionally, it has been reported that IFN-γ signaling is required for tolerogenic function of DCs mediated by TGF-β in EAE [83], and that IFN-γ along with TNF-α produced by T cells in combination with TGF-β and B7 molecules expressed by neurons are critical in the generation of neuron-induced Treg cells in the CNS of EAE mice [84]. Collectively, this evidence supports the ability of IFN-γ to endow different cell types with tolerogenic properties.
Remarkably, splenic CD11b+ myeloid cells from IFN-γ-treated EAE mice showed a significant therapeutic potential in that intravenous injection of these cells in untreated EAE mice induced a rapid and significant amelioration of clinical symptoms. Disease attenuation induced by adoptive transfer of splenic CD11b+ myeloid cells from IFN-γ-treated EAE mice was associated with lower CNS infiltration of mononuclear cells and effector CD3+CD4+ helper T cells. Although there was no significant difference in Treg cells at the time of evaluation (3 days after injection), it does not rule out the possibility that Treg cells are induced by splenic CD11b+ myeloid cells earlier and/or transitorily. Further experiments will be necessary to identify which type of APC mediates the therapeutic effects of splenic CD11b+ myeloid cells. A possible cellular target of IFN-γ might be DCs because transfer of healthy splenic DC ex vivo stimulated with IFN-γ significantly suppressed clinical symptoms of EAE and prevented diabetes onset in NOD mice [49, 85, 86].
We found that that the induction of splenic CD11b+ myeloid cells expressing PD-L1 and LAP-TGF-β depends on STAT-1, an essential transcriptional factor involved in the maintenance of immunological self-tolerance and function of Treg cells in EAE [87, 88]. Interestingly, we have recently reported that amelioration of EAE symptoms and induction of homeostatic microglia by IFN-γ is also dependent on STAT-1. Therefore, our previous and current results reveal a novel role of the IFN-γ/STAT-1 axis in the induction of tolerogenic microglia and splenic CD11b+ myeloid cells involved in the suppression of EAE development and shed light on the protective mechanism of IFN-γ showing that it induces tolerogenic activity in EAE targeting both peripheral and CNS-resident APC.
Conclusions
Collectively, our results show that the protective mechanisms of IFN-γ in EAE depend on the presence of FOXP3+ Treg cells. However, IFN-γ does not exert a direct effect on Treg cells but rather induces a subset of splenic CD11b+ myeloid cells with tolerogenic phenotype and function able to induce conversion of naïve CD4+ T cells into Treg cells signaling through STAT-1 and promoting TGF-β secretion. Furthermore, IFN-γ-induced splenic CD11b+ myeloid cells exert therapeutic activity in recipient EAE mice limiting CNS infiltration of mononuclear cells and helper T cells. Therefore, our findings reveal a previously unknown protective mechanism of IFN-γ in a neuroinflammatory context and contribute to clarifying its paradoxical role in EAE and MS.
Data availability
The data supporting the findings of this work are available upon reasonable request.
Abbreviations
- APC:
-
antigen presenting cells
- CD:
-
cluster of differentiation
- CNS:
-
central nervous system
- CTLA:
-
Cytotoxic T-lymphocyte antigen
- DNAse:
-
deoxyribonuclease
- DTR:
-
diphtheria toxin receptor
- DTx:
-
diphtheria toxin
- EAE:
-
experimental autoimmune encephalomyelitis
- FOXP3:
-
Forkhead box p3
- IFN:
-
interferon
- IFN-γR:
-
interferon-γ receptor
- IL:
-
interleukin
- i.p.:
-
intra peritoneal
- LAG:
-
Lymphocyte-activation gene
- LAP:
-
Latency associated peptide: LN, lymph node
- MFI:
-
mean fluorescence intensity
- MHC:
-
major histocompatibility complex
- MNC:
-
mononuclear cells
- MOG:
-
myelin oligodendrocyte glycoprotein
- MS:
-
Multiple Sclerosis
- MT:
-
mycobacterium tuberculosis
- PBS:
-
phosphate-buffered saline
- PD:
-
Program-death
- PD-L:
-
Program-death Ligand
- p.i.:
-
post-immunization
- PLP:
-
proteolipid protein
- PMA:
-
phorbol myristate acetate
- PTx:
-
pertussis toxin
- RR:
-
relapsing-remitting
- s.c.:
-
subcutaneous
- SC:
-
spinal cord
- STAT:
-
Signal Transducers and Activators of Transcription
- Th:
-
T helper cells
- TGF:
-
Tumor growth factor
- Treg:
-
regulatory T
- WT:
-
wild type
References
Dendrou CA, Fugger L, Friese MA. Immunopathology of multiple sclerosis. Nat Rev Immunol. 2015;15:545–58.
Yadav SK, Mindur JE, Ito K, Dhib-Jalbut S. Advances in the immunopathogenesis of multiple sclerosis. Curr Opin Neurol. 2015;28:206–19.
Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502–17.
Mahad DH, Trapp BD, Lassmann H. Pathological mechanisms in progressive multiple sclerosis. Lancet Neurol. 2015;14:183–93.
Confavreux C, Vukusic S. The clinical course of multiple sclerosis. Handb Clin Neurol. 2014;122:343–69.
Robinson AP, Harp CT, Noronha A, Miller SD. The experimental autoimmune encephalomyelitis (EAE) model of MS: utility for understanding disease pathophysiology and treatment. Handb Clin Neurol. 2014;122:173–89.
Lovett-Racke AE. Contribution of EAE to understanding and treating multiple sclerosis. J Neuroimmunol. 2017;304:40–2.
Constantinescu CS, Farooqi N, O’Brien K, Gran B. Experimental autoimmune encephalomyelitis (EAE) as a model for multiple sclerosis (MS). Br J Pharmacol. 2011;164:1079–106.
Lassmann H, Bradl M. Multiple sclerosis: experimental models and reality. Acta Neuropathol. 2017;133:223–44.
Domingues HS, Mues M, Lassmann H, Wekerle H, Krishnamoorthy G. Functional and pathogenic differences of Th1 and Th17 cells in experimental autoimmune encephalomyelitis. PLoS ONE. 2010;5:e15531.
Arellano G, Acuña E, Reyes LI, Ottum PA, De Sarno P, Villarroel L, Ciampi E, Uribe-San Martín R, Cárcamo C, Naves R. Th1 and Th17 cells and Associated cytokines discriminate among clinically isolated syndrome and multiple sclerosis phenotypes. Front Immunol. 2017;8:753.
Miller SD, Karpus WJ. Experimental autoimmune encephalomyelitis in the mouse. Curr Protoc Immunol 2007, Chap. 15:Unit 15.11.
Wasser B, Pramanik G, Hess M, Klein M, Luessi F, Dornmair K, Bopp T, Zipp F, Witsch E. Increase of alternatively activated Antigen presenting cells in active experimental autoimmune encephalomyelitis. J Neuroimmune Pharmacol. 2016;11:721–32.
Rawji KS, Yong VW. The benefits and detriments of macrophages/microglia in models of multiple sclerosis. Clin Dev Immunol. 2013;2013:948976.
Jiang Z, Jiang JX, Zhang GX. Macrophages: a double-edged sword in experimental autoimmune encephalomyelitis. Immunol Lett. 2014;160:17–22.
Ibañez-Vega J, Vilchez C, Jimenez K, Guevara C, Burgos PI, Naves R. Cellular and molecular regulation of the programmed death-1/programmed death ligand system and its role in multiple sclerosis and other autoimmune diseases. J Autoimmun. 2021;123:102702.
Wang L, Li Z, Ciric B, Safavi F, Zhang GX, Rostami A. Selective depletion of CD11c(+) CD11b(+) dendritic cells partially abrogates tolerogenic effects of intravenous MOG in murine EAE. Eur J Immunol. 2016;46:2454–66.
Korn T, Reddy J, Gao W, Bettelli E, Awasthi A, Petersen TR, Bäckström BT, Sobel RA, Wucherpfennig KW, Strom TB, et al. Myelin-specific regulatory T cells accumulate in the CNS but fail to control autoimmune inflammation. Nat Med. 2007;13:423–31.
McGeachy MJ, Stephens LA, Anderton SM. Natural recovery and protection from autoimmune encephalomyelitis: contribution of CD4 + CD25 + regulatory cells within the central nervous system. J Immunol. 2005;175:3025–32.
Ma A, Xiong Z, Hu Y, Qi S, Song L, Dun H, Zhang L, Lou D, Yang P, Zhao Z, et al. Dysfunction of IL-10-producing type 1 regulatory T cells and CD4(+)CD25(+) regulatory T cells in a mimic model of human multiple sclerosis in Cynomolgus monkeys. Int Immunopharmacol. 2009;9:599–608.
Koutrolos M, Berer K, Kawakami N, Wekerle H, Krishnamoorthy G. Treg cells mediate recovery from EAE by controlling effector T cell proliferation and motility in the CNS. Acta Neuropathol Commun. 2014;2:163.
Oh U, Blevins G, Griffith C, Richert N, Maric D, Lee CR, McFarland H, Jacobson S. Regulatory T cells are reduced during anti-CD25 antibody treatment of multiple sclerosis. Arch Neurol. 2009;66:471–9.
Kohm AP, Carpentier PA, Anger HA, Miller SD. Cutting edge: CD4 + CD25 + regulatory T cells suppress antigen-specific autoreactive immune responses and central nervous system inflammation during active experimental autoimmune encephalomyelitis. J Immunol. 2002;169:4712–6.
Danikowski KM, Jayaraman S, Prabhakar BS. Regulatory T cells in multiple sclerosis and myasthenia gravis. J Neuroinflammation. 2017;14:117.
Frisullo G, Nociti V, Iorio R, Patanella AK, Caggiula M, Marti A, Sancricca C, Angelucci F, Mirabella M, Tonali PA, Batocchi AP. Regulatory T cells fail to suppress CD4T+-bet + T cells in relapsing multiple sclerosis patients. Immunology. 2009;127:418–28.
Haas J, Hug A, Viehöver A, Fritzsching B, Falk CS, Filser A, Vetter T, Milkova L, Korporal M, Fritz B, et al. Reduced suppressive effect of CD4 + CD25high regulatory T cells on the T cell immune response against myelin oligodendrocyte glycoprotein in patients with multiple sclerosis. Eur J Immunol. 2005;35:3343–52.
Venken K, Hellings N, Broekmans T, Hensen K, Rummens JL, Stinissen P. Natural naive CD4 + CD25 + CD127low regulatory T cell (Treg) development and function are disturbed in multiple sclerosis patients: recovery of memory Treg homeostasis during disease progression. J Immunol. 2008;180:6411–20.
Valente G, Ozmen L, Novelli F, Geuna M, Palestro G, Forni G, Garotta G. Distribution of interferon-gamma receptor in human tissues. Eur J Immunol. 1992;22:2403–12.
Hu X, Ivashkiv LB. Cross-regulation of signaling pathways by interferon-gamma: implications for immune responses and autoimmune diseases. Immunity. 2009;31:539–50.
Bhat MY, Solanki HS, Advani J, Khan AA, Keshava Prasad TS, Gowda H, Thiyagarajan S, Chatterjee A. Comprehensive network map of interferon gamma signaling. J Cell Commun Signal. 2018;12:745–51.
Schroder K, Hertzog PJ, Ravasi T, Hume DA. Interferon-gamma: an overview of signals, mechanisms and functions. J Leukoc Biol. 2004;75:163–89.
Skurkovich S, Boiko A, Beliaeva I, Buglak A, Alekseeva T, Smirnova N, Kulakova O, Tchechonin V, Gurova O, Deomina T, et al. Randomized study of antibodies to IFN-gamma and TNF-alpha in secondary progressive multiple sclerosis. Mult Scler. 2001;7:277–84.
Panitch HS, Hirsch RL, Haley AS, Johnson KP. Exacerbations of multiple sclerosis in patients treated with gamma interferon. Lancet. 1987;1:893–5.
Panitch HS, Hirsch RL, Schindler J, Johnson KP. Treatment of multiple sclerosis with gamma interferon: exacerbations associated with activation of the immune system. Neurology. 1987;37:1097–102.
Arellano G, Ottum PA, Reyes LI, Burgos PI, Naves R. Stage-specific role of Interferon-Gamma in Experimental Autoimmune encephalomyelitis and multiple sclerosis. Front Immunol. 2015;6:492.
Ottum PA, Arellano G, Reyes LI, Iruretagoyena M, Naves R. Opposing roles of Interferon-Gamma on cells of the Central Nervous System in Autoimmune Neuroinflammation. Front Immunol 2015, 6.
Bever CT, Panitch HS, Levy HB, McFarlin DE, Johnson KP. Gamma-interferon induction in patients with chronic progressive MS. Neurology. 1991;41:1124–1124.
Sabatino JJ Jr., Shires J, Altman JD, Ford ML, Evavold BD. Loss of IFN-gamma enables the expansion of autoreactive CD4 + T cells to induce experimental autoimmune encephalomyelitis by a nonencephalitogenic myelin variant antigen. J Immunol. 2008;180:4451–7.
Furlan R, Brambilla E, Ruffini F, Poliani PL, Bergami A, Marconi PC, Franciotta DM, Penna G, Comi G, Adorini L, Martino G. Intrathecal delivery of IFN-gamma protects C57BL/6 mice from chronic-progressive experimental autoimmune encephalomyelitis by increasing apoptosis of central nervous system-infiltrating lymphocytes. J Immunol. 2001;167:1821–9.
Billiau A, Heremans H, Vandekerckhove F, Dijkmans R, Sobis H, Meulepas E, Carton H. Enhancement of experimental allergic encephalomyelitis in mice by antibodies against IFN-gamma. J Immunol. 1988;140:1506–10.
Axtell RC, de Jong BA, Boniface K, van der Voort LF, Bhat R, De Sarno P, Naves R, Han M, Zhong F, Castellanos JG, et al. T helper type 1 and 17 cells determine efficacy of interferon-beta in multiple sclerosis and experimental encephalomyelitis. Nat Med. 2010;16:406–12.
Naves R, Singh SP, Cashman KS, Rowse AL, Axtell RC, Steinman L, Mountz JD, Steele C, De Sarno P, Raman C. The interdependent, overlapping, and differential roles of type I and II IFNs in the pathogenesis of experimental autoimmune encephalomyelitis. J Immunol. 2013;191:2967–77.
Dungan LS, McGuinness NC, Boon L, Lynch MA, Mills KH. Innate IFN-γ promotes development of experimental autoimmune encephalomyelitis: a role for NK cells and M1 macrophages. Eur J Immunol. 2014;44:2903–17.
Tichauer JE, Arellano G, Acuña E, González LF, Kannaiyan NR, Murgas P, Panadero-Medianero C, Ibañez-Vega J, Burgos PI, Loda E, et al. Interferon-gamma ameliorates experimental autoimmune encephalomyelitis by inducing homeostatic adaptation of microglia. Front Immunol. 2023;14:1191838.
Wang Z, Hong J, Sun W, Xu G, Li N, Chen X, Liu A, Xu L, Sun B, Zhang JZ. Role of IFN-gamma in induction of Foxp3 and conversion of CD4 + CD25- T cells to CD4 + Tregs. J Clin Invest. 2006;116:2434–41.
Horwitz DA, Zheng SG, Wang J, Gray JD. Critical role of IL-2 and TGF-beta in generation, function and stabilization of Foxp3 + CD4 + Treg. Eur J Immunol. 2008;38:912–5.
Hsu P, Santner-Nanan B, Hu M, Skarratt K, Lee CH, Stormon M, Wong M, Fuller SJ, Nanan R. IL-10 Potentiates Differentiation of Human Induced Regulatory T Cells via STAT3 and Foxo1. J Immunol. 2015;195:3665–74.
Thomé R, Moore JN, Mari ER, Rasouli J, Hwang D, Yoshimura S, Ciric B, Zhang GX, Rostami AM. Induction of Peripheral Tolerance in Ongoing Autoimmune inflammation requires interleukin 27 signaling in dendritic cells. Front Immunol. 2017;8:1392.
Casella G, Rasouli J, Thome R, Descamps HC, Vattikonda A, Ishikawa L, Boehm A, Hwang D, Zhang W, Xiao D, et al. Interferon-γ/Interleukin-27 Axis induces programmed death Ligand 1 expression in monocyte-derived dendritic cells and restores Immune Tolerance in Central Nervous System Autoimmunity. Front Immunol. 2020;11:576752–576752.
Konieczny BT, Dai Z, Elwood ET, Saleem S, Linsley PS, Baddoura FK, Larsen CP, Pearson TC, Lakkis FG. IFN-gamma is critical for long-term allograft survival induced by blocking the CD28 and CD40 ligand T cell costimulation pathways. J Immunol. 1998;160:2059–64.
Hassan AT, Dai Z, Konieczny BT, Ring GH, Baddoura FK, Abou-Dahab LH, El-Sayed AA, Lakkis FG. Regulation of alloantigen-mediated T-cell proliferation by endogenous interferon-gamma: implications for long-term allograft acceptance. Transplantation. 1999;68:124–9.
Yu XZ, Albert MH, Martin PJ, Anasetti C. CD28 ligation induces transplantation tolerance by IFN-gamma-dependent depletion of T cells that recognize alloantigens. J Clin Invest. 2004;113:1624–30.
Jones LS, Rizzo LV, Agarwal RK, Tarrant TK, Chan CC, Wiggert B, Caspi RR. IFN-gamma-deficient mice develop experimental autoimmune uveitis in the context of a deviant effector response. J Immunol. 1997;158:5997–6005.
Caspi RR, Chan CC, Grubbs BG, Silver PB, Wiggert B, Parsa CF, Bahmanyar S, Billiau A, Heremans H. Endogenous systemic IFN-gamma has a protective role against ocular autoimmunity in mice. J Immunol. 1994;152:890–9.
Ring GH, Dai Z, Saleem S, Baddoura FK, Lakkis FG. Increased susceptibility to immunologically mediated glomerulonephritis in IFN-gamma-deficient mice. J Immunol. 1999;163:2243–8.
Eriksson U, Kurrer MO, Sebald W, Brombacher F, Kopf M. Dual role of the IL-12/IFN-gamma axis in the development of autoimmune myocarditis: induction by IL-12 and protection by IFN-gamma. J Immunol. 2001;167:5464–9.
Flaishon L, Topilski I, Shoseyov D, Hershkoviz R, Fireman E, Levo Y, Marmor S, Shachar I. Cutting edge: anti-inflammatory properties of low levels of IFN-gamma. J Immunol. 2002;168:3707–11.
Kitching AR, Turner AL, Semple T, Li M, Edgtton KL, Wilson GR, Timoshanko JR, Hudson BG, Holdsworth SR. Experimental autoimmune anti-glomerular basement membrane glomerulonephritis: a protective role for IFN-gamma. J Am Soc Nephrol. 2004;15:1764–74.
Arellano G, Loda E, Chen Y, Neef T, Cogswell AC, Primer G, Joy G, Kaschke K, Wills S, Podojil JR, et al. Interferon-γ controls aquaporin 4-specific Th17 and B cells in neuromyelitis optica spectrum disorder. Brain. 2024;147:1344–61.
Jadidi-Niaragh F, Mirshafiey A. Regulatory T-cell as orchestra leader in immunosuppression process of multiple sclerosis. Immunopharmacol Immunotoxicol. 2011;33:545–67.
Huan J, Culbertson N, Spencer L, Bartholomew R, Burrows GG, Chou YK, Bourdette D, Ziegler SF, Offner H, Vandenbark AA. Decreased FOXP3 levels in multiple sclerosis patients. J Neurosci Res. 2005;81:45–52.
Venken K, Hellings N, Thewissen M, Somers V, Hensen K, Rummens JL, Medaer R, Hupperts R, Stinissen P. Compromised CD4 + CD25(high) regulatory T-cell function in patients with relapsing-remitting multiple sclerosis is correlated with a reduced frequency of FOXP3-positive cells and reduced FOXP3 expression at the single-cell level. Immunology. 2008;123:79–89.
Kumar M, Putzki N, Limmroth V, Remus R, Lindemann M, Knop D, Mueller N, Hardt C, Kreuzfelder E, Grosse-Wilde H. CD4 + CD25 + FoxP3 + T lymphocytes fail to suppress myelin basic protein-induced proliferation in patients with multiple sclerosis. J Neuroimmunol. 2006;180:178–84.
Caretto D, Katzman SD, Villarino AV, Gallo E, Abbas AK. Cutting edge: the Th1 response inhibits the generation of peripheral regulatory T cells. J Immunol. 2010;184:30–4.
Tao X, Ma J, Zhang Y, Yu J, Cai L, Wang J, Zheng SG. Neutralization of IL-4 and IFN-γ facilitates inducing TGF-β-induced CD4(+)Foxp3(+) Regulatory cells. Int J Biomed Sci. 2008;4:52–7.
Dominguez-Villar M, Baecher-Allan CM, Hafler DA. Identification of T helper type 1-like, Foxp3 + regulatory T cells in human autoimmune disease. Nat Med. 2011;17:673–5.
Chang JH, Kim YJ, Han SH, Kang CY. IFN-gamma-STAT1 signal regulates the differentiation of inducible Treg: potential role for ROS-mediated apoptosis. Eur J Immunol. 2009;39:1241–51.
Wei J, Duramad O, Perng OA, Reiner SL, Liu YJ, Qin FX. Antagonistic nature of T helper 1/2 developmental programs in opposing peripheral induction of Foxp3 + regulatory T cells. Proc Natl Acad Sci U S A. 2007;104:18169–74.
Huang S, Li L, Liang S, Wang W. Conversion of peripheral CD4(+)CD25(-) T cells to CD4(+)CD25(+) regulatory T cells by IFN-gamma in patients with Guillain-Barré syndrome. J Neuroimmunol. 2009;217:80–4.
Huang S, Wang W, Chi L. Feasibility of up-regulating CD4(+)CD25(+) Tregs by IFN-γ in myasthenia gravis patients. BMC Neurol. 2015;15:163.
Ouaked N, Mantel PY, Bassin C, Burgler S, Siegmund K, Akdis CA, Schmidt-Weber CB. Regulation of the foxp3 gene by the Th1 cytokines: the role of IL-27-induced STAT1. J Immunol. 2009;182:1041–9.
Korn T, Muschaweckh A. Stability and maintenance of Foxp3 + Treg cells in non-lymphoid microenvironments. Front Immunol 2019, 10.
Tanuma N, Shin T, Kogure K, Matsumoto Y. Differential role of TNF-alpha and IFN-gamma in the brain of rats with chronic relapsing autoimmune encephalomyelitis. J Neuroimmunol. 1999;96:73–9.
Cheng X, Zhao Z, Ventura E, Gran B, Shindler KS, Rostami A. The PD-1/PD-L pathway is up-regulated during IL-12-induced suppression of EAE mediated by IFN-gamma. J Neuroimmunol. 2007;185:75–86.
Liang SC, Latchman YE, Buhlmann JE, Tomczak MF, Horwitz BH, Freeman GJ, Sharpe AH. Regulation of PD-1, PD-L1, and PD-L2 expression during normal and autoimmune responses. Eur J Immunol. 2003;33:2706–16.
Sun C, Mezzadra R, Schumacher TN. Regulation and function of the PD-L1 checkpoint. Immunity. 2018;48:434–52.
Brown JA, Dorfman DM, Ma FR, Sullivan EL, Munoz O, Wood CR, Greenfield EA, Freeman GJ. Blockade of programmed death-1 ligands on dendritic cells enhances T cell activation and cytokine production. J Immunol. 2003;170:1257–66.
Schreiner B, Bailey SL, Shin T, Chen L, Miller SD. PD-1 ligands expressed on myeloid-derived APC in the CNS regulate T-cell responses in EAE. Eur J Immunol. 2008;38:2706–17.
Zhang X, Reddy J, Ochi H, Frenkel D, Kuchroo VK, Weiner HL. Recovery from experimental allergic encephalomyelitis is TGF-beta dependent and associated with increases in CD4 + LAP + and CD4 + CD25 + T cells. Int Immunol. 2006;18:495–503.
Johns LD, Sriram S. Experimental allergic encephalomyelitis: neutralizing antibody to TGF beta 1 enhances the clinical severity of the disease. J Neuroimmunol. 1993;47:1–7.
Zhang H, Podojil JR, Chang J, Luo X, Miller SD. TGF-beta-induced myelin peptide-specific regulatory T cells mediate antigen-specific suppression of induction of experimental autoimmune encephalomyelitis. J Immunol. 2010;184:6629–36.
Wang L, Pino-Lagos K, de Vries VC, Guleria I, Sayegh MH, Noelle RJ. Programmed death 1 ligand signaling regulates the generation of adaptive Foxp3 + CD4 + regulatory T cells. Proc Natl Acad Sci U S A. 2008;105:9331–6.
Lukas D, Yogev N, Kel JM, Regen T, Mufazalov IA, Tang Y, Wanke F, Reizis B, Müller W, Kurschus FC, et al. TGF-β inhibitor Smad7 regulates dendritic cell-induced autoimmunity. Proc Natl Acad Sci U S A. 2017;114:E1480–9.
Liu Y, Teige I, Birnir B, Issazadeh-Navikas S. Neuron-mediated generation of regulatory T cells from encephalitogenic T cells suppresses EAE. Nat Med. 2006;12:518–25.
Xiao BG, Wu XC, Yang JS, Xu LY, Liu X, Huang YM, Bjelke B, Link H. Therapeutic potential of IFN-gamma-modified dendritic cells in acute and chronic experimental allergic encephalomyelitis. Int Immunol. 2004;16:13–22.
Shinomiya M, Fazle Akbar SM, Shinomiya H, Onji M. Transfer of dendritic cells (DC) ex vivo stimulated with interferon-gamma (IFN-gamma) down-modulates autoimmune diabetes in non-obese diabetic (NOD) mice. Clin Exp Immunol. 1999;117:38–43.
Nishibori T, Tanabe Y, Su L, David M. Impaired development of CD4 + CD25 + regulatory T cells in the absence of STAT1: increased susceptibility to autoimmune disease. J Exp Med. 2004;199:25–34.
Bettelli E, Sullivan B, Szabo SJ, Sobel RA, Glimcher LH, Kuchroo VK. Loss of T-bet, but not STAT1, prevents the development of experimental autoimmune encephalomyelitis. J Exp Med. 2004;200:79–87.
Acknowledgements
We thank the members of Naves and Miller labs for their helpful suggestions and discussions.
Funding
This work was supported by the National Doctoral scholarship CONICYT-CHILE 21130452 and MECESUP UCH 1304 (GA). FONDECYT/ANID 1140049 (RN), 1141211 (PB), 1191874 (RN), 1231672 (RN), and FONDECYT/ANID postdoc 3150133 (JT). MED.UCHILE-FACS Laboratory is supported by CONICYT-CHILE through grants FONDEQUIP140032 (BD LSR Fortessa X-20, Special Order) and AIC-08 (BD FACSAria III) and by the Institute of Biomedical Sciences (ICBM), School of Medicine, Universidad de Chile, Chile. Some of this work was supported with grant from the National Institute on Drug Abuse (NIDA, DP2DA051912) (PPM). Supported by gifts from the Johnnie Walkers MS Foundation, the Amy and David Fulton Foundation, the Crammer Family Foundation, the Thomas and Deige McLaughlin Foundation, and the Rottering Family Foundation (SDM).
Author information
Authors and Affiliations
Contributions
R.N. and G.A. conceived the study, designed experiments, analyzed data, and wrote the manuscript. E.A., E.L., L.M., J.E.T., C.C., and F.V. performed experiments and analyzed data. P.I.B., P.P.M., and S.D.M. provided resources, analyzed and discussed results, and revised the manuscript. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All animal experiments and procedures were conducted in accordance with the Institutional Animal Care and Use guidelines (IACUC) of the Universidad de Chile and Northwestern University.
Competing interests
SDM is a co-founder, paid consultant, scientific advisory board member, and grantee of COUR Pharmaceuticals. SDM is also a consultant for NextCure and Takeda Pharmaceuticals. The other authors have declared that no conflicts of interest exist.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Arellano, G., Acuña, E., Loda, E. et al. Therapeutic role of interferon-γ in experimental autoimmune encephalomyelitis is mediated through a tolerogenic subset of splenic CD11b+ myeloid cells. J Neuroinflammation 21, 144 (2024). https://doi.org/10.1186/s12974-024-03126-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-024-03126-3