Abstract
Since the twenty-first century, the development of technological advances in anesthesia and surgery has brought benefits to human health. However, the adverse neurological effects of perioperative-related factors (e.g., surgical trauma, anesthesia, etc.) as stressors cannot be ignored as well. The nervous system appears to be more “fragile” and vulnerable to damage in developing and aging individuals. Ferroptosis is a novel form of programmed cell death proposed in 2012. In recent years, the regulation of ferroptosis to treat cancer, immune system disorders, and neurodegenerative diseases have seen an unprecedented surge of interest. The association of ferroptosis with perioperative neurocognitive disorders has also received much attention. Cognitive impairment can not only affect the individual’s quality of life, but also impose a burden on the family and society. Therefore, the search for effective preventive and therapeutic methods to alleviate cognitive impairment caused by perioperative-related factors is a challenge that needs to be urgently addressed. In our review, we first briefly describe the connection between iron accumulation in neurons and impairment of brain function during development and aging. It is followed by a review of the pathways of ferroptosis, mainly including iron metabolism, amino acid metabolism, and lipid metabolism pathway. Furthermore, we analyze the connection between ferroptosis and perioperative-related factors. The surgery itself, general anesthetic drugs, and many other relevant factors in the perioperative period may affect neuronal iron homeostasis. Finally, we summarize the experimental evidence for ameliorating developmental and degenerative neurotoxicity by modulating ferroptosis. The suppression of ferroptosis seems to provide the possibility to prevent and improve perioperative neurocognitive impairment.
Similar content being viewed by others
Introduction
With health issues intensifying around the world, worldwide surgical procedures are increasing dramatically and surgery has become one of the predominant means of curing disease. Global surgical volume statistics published by the World Health Organization (WHO) have shown that the global surgical volume is up to 320 million each year and is gradually growing [1]. With the dual effect of improved surgical techniques and safety, surgical treatment has made contributions to human health. However, brain dysfunction caused by perioperative-related factors should not be neglected equally. Perioperative neurocognitive disorders (PND) are a common postoperative complication of the central nervous system, mainly including postoperative cognitive dysfunction (POCD) and postoperative delirium. It is usually characterized by confusion, anxiety, personality changes, and memory impairment [2]. Currently, the pathogenesis of PND is unclear and may be the result of a combination of factors. Oxidative stress, apoptosis, neuroinflammation, changes in synaptic properties, and abnormal accumulation of amyloid β (Aβ) may all be involved in the pathological development of PND [3, 4]. Compared to other age groups, elderly patients have a lower resistance to stress and a relatively lower tolerance to surgery, resulting in a higher incidence of PND [5]. It is important to note that PND is not a harmless disease. Not only does it lead to longer hospital length of stay, higher costs, and increased readmission rates, but it may also increase 5-year mortality after surgery [6, 7]. In addition, postoperative delirium may accelerate the deterioration of cognitive function in elderly patients and is associated with a decline in neurocognitive function in the distant postoperative period [8, 9]. Cognitive impairment not only leads to a reduced level of quality of life for the individual, but may also place a heavy burden on the family and society. Aging-induced neurological degeneration increases susceptibility to perioperative cognitive impairment, and the developing brain is likewise more vulnerable to multiple factors such as anesthetics and surgical trauma. Experimental animal studies have found that some anesthetics (e.g., isoflurane, sevoflurane, ketamine, sodium thiopental, and others) are neurotoxic to the developing brain [10, 11], and general anesthesia in infancy may also be associated with impaired recall memory in childhood [12]. Therefore, effective prevention and mitigation of anesthetic developmental neurotoxicity and perioperative neurocognitive impairment have become urgent issues to be addressed.
Ferroptosis is a novel iron-dependent form of programmed cell death proposed in 2012 [13], which is characterized by the generation of lipid peroxides by highly expressed unsaturated fatty acids in the cell membrane and the accumulation of lipid peroxides to lethal levels catalyzed by divalent iron or ester oxygenases, thereby inducing cell death [14, 15]. Iron is an essential trace element in the human body, involved in regulating energy metabolism, transporting oxygen, DNA synthesis, and improving immunity. In nerve cells, iron is not only engaged in mitochondrial respiration, but also plays a significant role in the synthesis of neurotransmitters and myelin sheaths, which is an indispensable part of maintaining normal physiological functions of the brain [16]. Elevated iron levels in the brain can damage nerve cells by inducing lipid peroxidation, mitochondrial inactivation, and neuroinflammation. Current research has demonstrated that iron overload can be linked to a variety of neurodegenerative diseases such as Alzheimer's disease, Parkinson’s disease, and epilepsy [17, 18]. And the mechanisms of general anesthetic neurotoxicity have similarities with neurodegenerative diseases. Ferroptosis, a form of cell death, may inevitably disrupt nerve cell function. However, this is not the only cause of the cognitive decline. Inhibition of neuronal activity can also affect cellular function. The intensity of perioperative stimuli and the susceptibility of neurons may lead to different outcomes for individual perioperative cognitive decline. Some individuals can return to normal quickly, while others take 6 months to 1 year, or even longer. Emerging insights suggest that ferroptosis is possibly involved in the pathogenesis of PND. Our review provides an update on the targeted modulation of ferroptosis to attenuate cognitive impairment attributed to perioperative-related factors.
Mechanisms of ferroptosis
Ferroptosis is a novel form of cell death that differs from apoptosis, autophagy, and necrosis, as proposed by Dixon et al. in 2012 [13]. It can be evoked by endogenous and exogenous pathways, with the endogenous pathway generally referring to the suppression of intracellular antioxidant enzyme activation, while the exogenous pathway is through the regulation of membrane transport proteins, mainly including the inhibition of System Xc− and activation of transferrin [19]. Increased iron accumulation and lipid peroxidation are critical signals for the induction of ferroptosis, and disruption of the balance between cellular regulation of oxidative damage and antioxidant defense will trigger cellular death. Currently, the precise mechanism of ferroptosis is still unclear and potentially closely interrelated with a variety of biological pathways, the main ones widely recognized being iron, lipid, and amino acid metabolic pathways [20] (Fig. 1).
Iron metabolism
Iron is an essential micro-element with two oxidation states, Fe2+ and Fe3+. Fe3+ binds to transferrin (TF) and eventually flows into the cells via the transferrin cycle. The principal processes include the binding of Tf–Fe3+ to transferrin high-affinity receptor 1 (TfR1) on the cell membrane and its entry into the cell to form an endosome by endocytosis. The acidic nuclear endosomal environment separates Fe3+ from TF, while the metal reductase STEAP3 reduces Fe3+ to Fe2+ [21]. Fe2+ can be subsequently assisted by the divalent metal transporter 1(DMT1) or the zinc transporter protein ZIP14 (ZRT/IRT-like protein14) to flow to the cytoplasmic labile iron pool(LIP) [22]. TF and TfR1, which have released Fe3+, can be reintroduced to the cell surface by cytosolic action. In this process, Tf and TfR1 can be recycled and reused in the next cycle of cellular iron uptake. Ferroportin 1(FPN1) is the unique protein in humans that transports intracellular iron efflux. Intracellular Fe2+ can be oxidized to Fe3+ by hephaestin and bound to ferroportin 1, which in turn are transferred out of the cell. Hepcidin can regulate FPN1 levels by binding to FPN1 and triggering its internalization, ubiquitination, and degradation. Iron response element (IRE) is a highly conserved RNA stem–loop structure present at the 5′ end or 3′ end of the non-coding region of iron metabolism-related protein genes (e.g., TFR1, DMT1, ferritin, FPN1, etc.) [23]. Iron regulatory proteins 1 and 2 (IRP1 and IRP2) can act as sensors to control intracellular iron metabolic homeostasis, recognizing and binding IRE in a structure and sequence-specific manner, and thereby regulating iron uptake, storage, and export [24]. When intracellular iron is at relatively low levels, IRP/IRE can increase iron uptake and inhibit iron export by upregulating the expression of TFR1 and DMT1 and downregulating FPN and ferritin [25].
Ferritinophagy is a type of selective cellular autophagy. Nuclear receptor co-activator 4 (NCOA4) has been identified as a crucial regulator of ferritinophagy, which binds to ferritin through the C-terminal helix domain and is delivered to the lysosome for degradation and release of free iron [26]. The regulation of NCOA4 expression by iron content has a negative feedback inhibition mechanism. In iron-sufficient cells, NCOA4 is degraded by the ubiquitin–proteasome system, increasing iron storage in the form of ferritin [27]. In addition, NCOA4 is regulated by hypoxia-inducible factor (HIF), and cells with increased activity of HIF1α or HIF2α will increase the expression level of NCOA4 [28]. Moderate ferritinophagy is essential in maintaining stable intracellular iron content. However, NCOA4 overexpression may excessively activate ferritinophagy and increase intracellular free iron, which might trigger ferroptosis [29].
Amino acid metabolism
System Xc− is a reverse transporter protein located in the cell membrane, consisting of a light chain subunit SLC7A11 and a heavy chain subunit SLC3A2 linked by a covalent disulfide bond, mediating the exchange of extracellular cystine and intracellular glutamate in a ratio of 1:1. The one that performs the amino acid transport function is SLC7A11, while SLC3A2 is responsible for enhancing protein stability [30]. Intracellular cystine can be converted into L-cysteine in a reducing environment, which can be utilized as a raw material for the synthesis of glutathione (GSH) [31]. Glutathione peroxidase 4 (GPX4), a member of the selenium-containing GPX family, is an essential peroxide-degrading enzyme in the body. The antioxidant process can catalyze the conversion of toxic peroxides to non-toxic hydroxyl compounds by using GSH as a reducing agent [15]. Therefore, GPX4 is an important factor in the negative regulation of ferroptosis.
Lipid metabolism
Lipid peroxidation is usually the process by which free radicals seize electrons from lipids leading to the accumulation of lipid peroxyl radicals and hydroperoxides, which is an essential point in initiating ferroptosis. The process usually affects polyunsaturated fatty acids (PUFAs), especially arachidonic acid (AA) and adrenoic acid (AdA) [32]. Free AA or AdA is successively generated by the action of Acyl-CoA synthetase long-chain family member4 (ACSL4) and lysophosphatidylcholine acyltransferase 3 (LPCAT3) to form AA/AdA-phosphatidyl ethanolamine (PE), and the whole process can be summarized as the production of CoA derivatives of PUFA and their binding to phospholipids [33]. Subsequently, under the regulation of lipoxygenases (LOXs), PUFA-PE is peroxidized to PUFA-PE-OOH. The accumulation of lipid peroxides destroys cell membranes and other structures, which exacerbates the development of ferroptosis [34, 35].
Other signals involved in the regulation of ferroptosis
Hypoxia-inducible factors (HIFs) are essential factors that regulate oxygen homeostasis at the level of gene transcription and are involved in the regulation of many iron metabolism-related proteins. Hydroxylation by prolyl hydroxylases (PHDs) can lead to the degradation of HIF-α, and iron ions can play an auxiliary role in this process. HIFs-PHDs are involved in the regulation of several iron metabolism-related proteins, and HIF-1 can activate the transcription of TFR by binding to hypoxia response elements [36]. In astrocytes, upregulation of HIF-1α and HIF-2α expression significantly increases DMT1 and FPN1 expression [37]. Grx3 and Grx4 in the glutaredoxin system can bind Fe–S proteins together with GSH to form a complex that functions in antioxidation and maintenance of iron homeostasis [38]. Depletion of GSH can increase free iron in the cytoplasm, which in turn is deployed to iron-dependent PHDs, promoting the expression of ATF4 in the cytoplasm and ultimately inducing the occurrence of ferroptosis. New insights propose that HIF-PHDs are oxygen sensors associated with neuronal survival and that iron chelators prevent heme-induced neuronal ferroptosis in an in vitro model of cerebral hemorrhage by targeting and regulating HIF-PHDs, an iron-dependent enzyme, rather than by inhibiting the Fenton response [39]. Coenzyme Q10 is a lipid-soluble antioxidant and its reduced form can resist free radicals that mediate the process of lipid peroxidation. Ferroptosis suppressor protein 1 (FSP1), tetrahydrobiopterin (BH4), and dihydroorotate dehydrogenase (DHODH) are involved in regulating the production of panthenol and perform an effect in the process of cellular antioxidation. The FSP1/CoQ10/NAD(P)H signaling pathway is an antioxidant pathway that parallels the GPX4 system and strongly synergizes with GPX4 to inhibit phospholipid peroxidation. FSP1 can decrease the accumulation of lipid peroxides by converting ubiquinone (CoQ) to the antioxidant dihydroubiquinone (CoQH2) [40]. BH4 is a critical enzyme in the synthesis of CoQ precursors. Normal expression of the BH4/dihydrofolate reductase (DHFR) pathway serves an essential function in promoting the production of CoQ [41]. New research suggests that DHODH, a flavin-dependent enzyme in mitochondria, can also promote CoQH2 production and thus mitigate lipid peroxidation damage in mitochondria [42].
GSH is a crucial antioxidant in the body, and the System Xc−-mediated uptake of cysteine is an important source of GSH synthesis. Both tumor suppressor p53 and nuclear factor erythroid 2-related factor (Nrf2) can be involved in regulating System Xc− function, but their roles are distinct. p53 interferes with cystine uptake by inhibiting SLC7A11 expression, which in turn promotes cellular ferroptosis [43]. In contrast, Nrf2 can translocate to the nucleus after stimulation by oxidative stress to promote the expression of antioxidant molecules SLC7A11 and HO-1, and consequently inhibit cellular ferroptosis [44].
Iron metabolism in different types of neuronal cells
The blood–brain barrier is a material exchange-limiting structure composed of capillary endothelial cells, basement membrane, and astrocytes, which makes it impossible for iron ions from peripheral blood to enter the brain directly, but requires a special transport process [45]. Iron transport involves two transmembrane processes, located on both sides of the vascular endothelium: the parietal membrane on the blood side and the basement membrane on the brain side. Iron in cerebrospinal fluid exists mainly in the form of transferrin-bound iron (TBI) and non-transferrin-bound iron (NTBI) [46]. Most of the iron flows into the cells by binding to TF and TFR1, which is highly expressed on the luminal side of the vascular endothelium. A small fraction enters via a NTBI pathway, probably involving the iron transporter in the parietal membrane [47]. Intracellular iron flows out of the basal plane via Fpn1 or other transporters. The iron being released outside the cell may bind to transferrin or complex with citric acid, ATP, etc., to form low molecular weight complexes, which are subsequently taken up by other cells [48]. Iron is capable of moving between different neurons and glial cells, but the exact mechanism is not yet fully clarified [49].
Different glial cells mainly express different iron regulatory proteins, such as astrocytes mainly express Fpn1, oligodendrocytes mainly express TFR1, and microglia mainly express ferritin [50]. Although all nerve cells can take up non-transferrin-bound iron, different nerve cells have different capacities to store iron. In an in vitro study comparing the ability of neurons, astrocytes, and microglia to accumulate iron, it was found that the ability of neuroglia (especially microglia) was stronger than that of neurons [51]. However, brain astrocytes in vivo express less ferritin and have a poor capacity to store iron [52]. As a major component of the blood–brain barrier, astrocytes serve a critical role in regulating iron homeostasis in the central nervous system. The presence of ferrous iron-converting enzymes on astrocytes can reduce Fe3+ to Fe2+, which is then transported into the cells via DMT1 [53]. Fpn1, hepcidin, and ceruloplasmin expressed in the terminal peduncle are all involved in regulating the transport of Fe2+ to the extracellular compartment in astrocytes [54, 55]. In addition, astrocytes appear to be more resistant to iron overload-induced neurotoxicity than other neuronal cells, which may be associated with the presence of their antioxidant system [52].
Microglia are neuroimmune cells with both anti-inflammatory and pro-inflammatory effects. The different effects depend mainly on the subpopulation into which they are activated: typically activated microglia (M1 type) and alternatively activated microglia (M2 type). M1 type is capable of producing pro-inflammatory cytokines such as IL-1, TNF-α, and IL-β, which in turn trigger cell damage [56]. Conversely, M2 secretes anti-inflammatory cytokines such as IL-10 and neurotrophic factors, which can exert anti-inflammatory and pro-neural tissue repair effects [57]. There are also differences in the regulation of iron transport in different states of microglia. The expression of DMT1 is upregulated in the M1 state, where it takes up more NTBI at the cell surface as a result of increased extracellular acidification [58]. In addition, the increase in extracellular acidification and the decrease in intracellular hemoglobin levels are changes that exacerbate the increase in intracellular labile iron. In the M2 state, the expression of TFR1 and ferritin increased, the cellular uptake of transferrin-bound iron increased, and the iron ions entering the cells could bind to ferritin to form stable complexes [59]. This avoids cell damage caused by elevated free iron outside the nerve cells. Iron metabolism in microglia is not deeply examined, and it is generally believed that iron uptake increases and output decrease after activation [60]. Iron in oligodendrocytes is mainly in the form of ferritin and transferrin [61]. Oligodendrocytes and choroid plexus are the main cells that synthesize transferrin, and iron in nerve cells is mainly delivered by transferrin. Therefore, the concentration of transferrin in cerebrospinal fluid can reflect the availability of iron in the brain [48]. In addition, oligodendrocytes can provide large amounts of iron for axonal myelin formation [62].
Interaction of ferroptosis, neuroinflammation, and PND
Although the etiology of perioperative neurocognitive disorders remained unclear, neuroinflammation has been characterized as one of the major causes, especially in elderly patients. In addition, there is a complex link between ferroptosis and enzymes involved in inflammation, and ferroptosis inhibitors have demonstrated benefits in certain diseases due to their anti-inflammatory activity. Microglia perform an instrumental role in neuroinflammation as major mediators of the innate immune response, and their iron metabolism has been characterized as previously described. Iron overload is strongly associated with neuroinflammation. Elevated intracellular iron levels promote M1 polarization in microglia and facilitate a switch from M2 to M1 phenotype [63]. PUFAs and their metabolites are essential regulators of inflammation production and regression [64]. Arachidonic acid (AA) can produce leukotrienes (LT) via the lipoxygenases (LOXs) pathway and prostaglandins(PG) via the cyclooxygenases (COXs) pathway [65]. Ferroptosis appears to be linked to inflammation through regulation of the activity of LOXs and COXs. Lipid peroxidation is an important driver of ferroptotic cell death, and it has been identified in early studies that endogenous peroxisomal tension can regulate cellular lipoxygenase activity [66]. COX, as the rate limiting enzyme that catalyzes the conversion of AA to PG, has two isozymes, COX-1 and COX-2. Among them, COX-2 is an inducible enzyme encoded by PTGS2, which can activate inflammatory cells and thus trigger subsequent inflammatory responses. The emerging research has revealed that iron death can directly upregulate the expression of PTGS2 and thus promote the secretion of inflammatory mediators [67]. Elevated pro-inflammatory cytokines function in both the innate immune system and the adaptive immune system. Prostaglandin E promotes the differentiation of helper T cells and the secretion of TNF in dendritic cells, which in turn activates T cells [68]. Neuroinflammation is also capable of further exacerbating iron accumulation. Nuclear factor-kappa B (NF-κB) is a transcription factor that mediates the immune response and its activation contributes to iron accumulation in dopaminergic neurons [69]. Both neuroinflammation and ferroptosis exacerbate the disruption of neuronal cell function, which subsequently leads to cognitive dysfunction. Numerous studies have found that the application of iron chelators in mouse models of perioperative neurocognitive impairment suppresses neuroinflammation and enhances behavioral and cognitive performance.
Association of ferroptosis with perioperative neurocognitive disorders
Surgical trauma-induced changes in iron homeostasis of nerve cells
In research exploring the pathogenesis of POCD, there were significant differences in iron homeostasis in the hippocampus of splenectomized animals on the first and third postoperative days, but no significant changes were observed in the control and anesthesia-only groups. Iron accumulation was accompanied by increased oxidative stress, mainly in the form of increased malondialdehyde, a product of lipid peroxidation, and decreased levels of superoxide dismutase activity. The investigators proposed that postoperative cognitive decline might be principally attributed to surgical trauma rather than anesthesia and that changes in neuronal iron homeostasis and oxidative stress damage caused by surgical procedures were significant factors in cognitive decline [70]. Similarly, in another study using an abdominal surgery model to assess the effects of surgical trauma on hippocampal iron homeostasis, surgery resulted in altered levels of iron content and expression of proteins related to iron metabolism for up to 14 days, with increases in hippocampal iron content, ferritin, and DMT1, and a significant decrease in Fpn-1 levels, compared to controls and sham surgery [71]. In addition, surgical procedures inevitably lead to increased production of reactive oxygen species (ROS) in the body, and large amounts of ROS can result in a disruption of the intracellular oxidative and antioxidant balance [72]. The reaction between ROS and PUFA of the cell membrane promoted the production of lipid peroxides, which eventually caused ferroptosis in the cells. Reactive lipid species (RLS) can be regarded as a product of the non-enzymatic and enzymatic lipid peroxidation of PUFAs. Large intracellular accumulation of iron content and oxidative stress damage may promote ferroptosis and thus lead to decreased cellular function.
The mechanism by which general anesthetics affect ferroptosis
General anesthetics affect iron metabolism
The neurotoxicity of general anesthetics has been a topical issue in the field of anesthesia. Repeated and prolonged exposure not only affects the neurodevelopment of infants and children, but also may accelerate the neurological degeneration of elderly patients [5, 73]. Elevated iron in the brain is associated with neuronal dysfunction. Current opinion suggests that general anesthetics may induce cognitive deficits by exacerbating iron overload in neuronal cells. This can be obtained by the detection of intracellular iron and iron metabolism-related protein levels. In a study using developing pups and aged rats, both ketamine and sevoflurane exposure was found to cause cytoplasmic and mitochondrial iron accumulation in hippocampal neurons. Reduced IRP2 and TfR1 expressions and increased ferritin expression further indicated that general anesthetics interfered with the balance of iron metabolism in neuronal cells [74]. Wang et al. discovered that sevoflurane significantly upregulated the expression of H-ferritin and, l-ferritin and iron export protein in the hippocampus and cortex of aged mice, but the expression of the input-related protein TfR1 was significantly decreased. In contrast to the previous findings, the expression level of IRP2 did not change significantly, and the investigators suggested that IRP2 may not be involved in sevoflurane-induced disorders of iron metabolism [75]. Fe–S protein is a component of the mitochondrial respiratory chain and plays a key role in biological activities as an important electron carrier. Anesthetics may affect mitochondrial function by causing disturbances in iron metabolism. Interestingly, maternal sevoflurane anesthetic exposure during pregnancy reduced brain iron levels and inhibited myelin production in offspring mice leading to cognitive impairment, while iron supplementation therapy improved impaired cognitive performance [76]. Therefore, the impact of sevoflurane on iron metabolism in mice of different ages may not be identical.
It is widely accepted that anesthetics indeed induce an imbalance of iron homeostasis in neuronal cells by affecting iron metabolism, but the exact molecular mechanism is not clear. One of the main mechanisms by which general anesthetics act may be through inhibition of excitatory synapses and enhancement of inhibitory synaptic transmission, specifically by affecting the function of ligand-gated ion channels, such as glutamate receptors/GABA receptors and glycine receptor ion channels [77]. N-Methyl-d-aspartic acid receptor (NMDAR) is a subtype of the ionotropic glutamate receptor, and it has been proposed that NMDAR may be the crucial link between anesthetics and cellular iron overload [74, 78]. Prolonged exposure of developing neurons to general anesthetics such as sevoflurane and ketamine may be responsible for a compensatory increase in NMDAR expression [79, 80]. Dexras1, also known as RASD1, is a Ras family small G protein, and activation of NMDAR can regulate iron transport in neurons through Dexras1 [81]. Dexras1 complexed with DMT1 not only promotes the transmembrane uptake of extracellular iron, but also increases the release of iron from lysosomes [82,83,84]. Wu et al. further confirm that NMDAR/RASD1/DMT1 signaling may be one of the molecular mechanisms by which general anesthetics disrupt the balance of iron metabolism in hippocampal neurons [74].
General anesthetics affect amino acid metabolism and lipid metabolism
It was found that isoflurane exposure did not alter the expression levels of genes related to iron metabolism and transport, suggesting that other alternative iron metabolic pathways were involved in inducing cellular ferroptosis [85]. The System Xc−/GSH/GPX4 regulatory axis is an important pathway that negatively regulates ferroptosis, and a decrease in glutathione-dependent antioxidant defense may be an essential trigger for ferroptosis [67, 86]. SLC7A11 is the predominant subunit in System Xc− that functions as an amino acid transporter. Beclin1 is a protein that can exert a vital regulatory role in cellular autophagy, and new insights suggest that it is not only involved in autophagy regulation, but also interacts with different protein partners to regulate multiple cellular processes in a non-autophagy-dependent manner [87, 88]. AMPK-mediated phosphorylation of BECN1 promotes BECN1–SLC7A11 complex formation and thus blocks System Xc− activity to induce cellular ferroptosis [89]. In an isoflurane-treated human neuroblastoma cell line, the expression level of phosphorylated Beclin1 protein was found to be significantly upregulated and mediated the inhibition of System Xc− function by binding to SLC7A11 in a complex. Isoflurane resulted in GSH depletion in neuronal cells in a concentration-dependent manner, ultimately inducing the development of ferroptosis [85]. Similarly, in Liu et al.’s study, SLC7A11 and GSH levels in the hippocampus decreased significantly after 6 h of 1.5% isoflurane exposure, but GPX4 levels did not change significantly, suggesting that isoflurane exposure may induce ferroptosis by affecting System Xc− and cystine uptake but not GPX4 [90]. However, it was controversial whether isoflurane affects ferroptosis by modulating GPX4 levels. Another study revealed a significant decrease in GPX 4 mRNA and protein expression levels in primary cortical neuronal cultures from mice treated with 2% isoflurane [91]. Lipid peroxidation is an influential part of ferroptosis, which usually refers to the process of oxidation of cell membrane by ROS and thus damage to cell structure and function. Malondialdehyde (MDA) and 4-hydroxynonenal (HNE) are common lipid peroxidation products. The brain is highly sensitive to lipid peroxidation due to its high oxygen consumption and the fact that nerve cell membranes are usually rich in polyunsaturated fatty acids [92]. A possible mechanism for omega-3 polyunsaturated fatty acids to improve postoperative cognitive dysfunction is that their components can replace arachidonic acid in cell membrane phospholipids to compete for cyclooxygenase and lipoxygenase and reduce RLS-induced cellular damage [93]. It is found that exposure of in vitro cultured cortical neurons to isoflurane significantly increases cellular ROS levels, impairs mitochondrial membrane potential, and ultimately induces cell death [91]. When the intracellular balance between oxidation and antioxidation is disturbed, more ROS reacting with lipids is an important factor leading to a decrease in cell viability.
Impact of other relevant factors in the perioperative period
Ferroptosis is a cell death process that catalyzes lipid peroxidation of cell membranes in the presence of divalent iron or lipoxygenase, thereby destroying structure and function. Surgical trauma and anesthetic drugs may be the main factors contributing to postoperative cognitive decline. However, many other relevant factors in the perioperative period deserve equal attention. Decreased cerebral oxygen levels, inadequate cerebral perfusion due to prolonged hypotension, excessive blood loss, duration of surgery, clinical history of cerebrovascular disease, and postoperative pain are all risk factors for the development of POCD [94, 95]. These factors may differentially stimulate the release of cellular inflammatory factors and exacerbate oxidative stress damage. It is worth noting that cellular ferroptosis does not exist independently, but is interconnected with oxidative stress, energy stress, endoplasmic reticulum response, lysosomal and mitochondrial functions, etc. [15, 96,97,98]. Currently, studies exploring ferroptosis and POCD are still in their infancy, and more studies are expected to explore the effects of perioperative-related factors on iron metabolism in neuronal cells.
Evidence for attenuation of developmental and degenerative neurotoxicity through modulation of ferroptosis
It is estimated that more than 300 million people worldwide will undergo surgical treatment each year. However, the stimulation of multiple factors such as surgery and anesthesia may inevitably lead to neurocognitive impairment in the body. The developing and aging brain appears to be more susceptible to damage in the perioperative period. Developmental neurotoxicity usually refers to abnormal changes in the structure and function of the nervous system caused by exposure of the brain to certain toxic substances during development, and there is an age-related susceptibility to such toxicity, ranging from 1 to 2 weeks after birth in rodents such as mice and from mid-conception to 3 years after birth in humans [99]. However, it has been proposed that the period of susceptibility to developmental neurotoxicity is determined by the cycle of division and differentiation in which neurons are present. Since neurons in the dentate gyrus and olfactory bulb regions have the capacity for continuous regeneration, some brain regions in adult life forms remain vulnerable to anesthetic-induced neurotoxicity [100]. In addition, the degenerative neurological changes associated with aging make the elderly more susceptible to multifactorial stimulation of cognitive decline in the perioperative period, which can also be considered degenerative neurotoxicity. New insights suggest that ferroptosis is involved in the pathology of postoperative cognitive dysfunction [101, 102]. The evidence from experimental studies to date is summarized in Table 1.
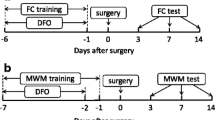
Iron accumulation can affect cognitive performance in mice by inducing multiple pathways including mitochondrial dysfunction, increased lethality of ROS, dendritic reduction, β-amyloid accumulation, and tau hyperphosphorylation [103]. In Wang et al.’s study, a low-iron diet appeared to improve sevoflurane-induced cognitive deficits [75]. In recent years, it has been widely investigated whether the regulation of ferroptosis by several treatments can prevent or improve POCD. The three main approaches of inhibiting ferroptosis include the following: iron chelation, prevention of lipid peroxidation, and scavenging of lipid peroxides [104]. Currently, iron chelators and lipophilic antioxidants are widely accepted methods to inhibit ferroptosis. Deferoxamine (DFO) is a high-affinity iron chelator that is capable of binding Fe3+ and exerts neuroprotective effects through suppression of LPS-induced increases in iron levels and neuroinflammation [105]. In Li et al.'s study, DFO pretreatment not only improved surgically induced changes in iron homeostasis, but also effectively reduced reactive microglia activation and inhibited oxidative stress and neuroinflammation. The mechanisms involved may include downregulation of gp91phox levels to inhibit oxidative stress signaling and suppression of p38 MAPK activation to reduce the release of inflammatory factors [71]. Pan et al. concluded similarly that preoperative administration of 100 mg/kg DFO improved iron accumulation in the hippocampus, inhibited microglial activation, and thus improved postoperative spatial memory in aged rats [106]. However, it is worth noting that the presence of the blood–brain barrier may not allow much DFO to actually enter the neuronal cells [107]. Deferiprone (DFP) is another metal chelator used to address iron overload and has the potential to treat a variety of diseases associated with iron accumulation. Its shuttle properties allow it to cross the blood–brain barrier and bind iron at multiple intracellular sites [108]. It was found that deferiprone pretreatment improved cognitive impairment induced by sevoflurane or ketamine, and behavioral testing ability was significantly improved in both adolescent and aged rats [74]. Cognitive impairment is strongly associated with iron overload and neuroinflammation, and DMT1 has been implicated as a key link between iron signaling and immunity [109]. DMT1-specific inhibitor (DMT1i) may attenuate GA-induced neurotoxicity by inhibiting iron uptake and counteracting compensatory upregulation of NMDAR [74]. Unlike the iron chelators mentioned above, ferrostatin-1 (Fer-1) is an inhibitor for ferroptosis with a lipophilic antioxidant effect. It could attenuate RLS generation, cell death, and mitochondrial dysfunction induced by isoflurane exposure [91]. Isoflurane can affect system Xc− function and mitochondrial electron respiratory chain activity in a time-dependent and dose-dependent manner, and cysteine deprivation-induced hippocampal ferroptosis is an essential contributor to isoflurane-induced developmental neurotoxicity. Both ferroptosis inhibitor (ferrostatin-1) and mitochondria activator (dimethyl fumarate) modulate ferroptosis induced by isoflurane exposure, except that dimethyl fumarate (DMF) pretreatment decreases the activity of the complex IV in mitochondrial ETCs, but ferrostatin-1 does not have the effect [90]. Notably, the primary target of DMF is Nrf2, a key regulator of redox reactions. However, significant off-target effects of DMF have been found in studies of CNS diseases, which may limit the further application of DMF. The ability of iron chelators and lipophilic antioxidants to exert neuroprotective effects by inhibiting ferroptosis has also been demonstrated with human in vitro experiments. Furthermore, it was proposed that silencing of ACSL4 attenuated sevoflurane-induced ferroptosis by activating the AMPK/mTOR signaling pathway. Transfection of si-ACSL4 eliminated the inhibition of SH-SY5Y cell viability by sevoflurane [102]. In recent years, it was suggested that the E3 ubiquitin-protein ligase Mind bomb-2 (MIB2) could be involved in regulating neuronal function. In a sevoflurane-induced POCD model, knockdown of MIB2 enhanced the stability of GPX4 and reduced its ubiquitination, consequently reducing hippocampal ferroptosis [101]. The silencing of ACSL4 and MIB2 has enriched the approaches to inhibit ferroptosis in neuronal cells, and these findings provide new directions for the application of related drugs or strategies such as anti-ACSL4 and anti-MIB2 for the treatment of POCD.
Conclusion and perspectives
Ferroptosis is a novel form of programmed cell death that is dependent on the accumulation of intracellular iron, resulting in inadequate antioxidant protection of the cellular lipid membrane. Ferroptosis is fundamentally different from apoptosis. The key to the apoptotic process is caspases, whose activation is achieved mainly through the death receptor pathway and the mitochondrial pathway. While a large body of literature in the past has emphasized apoptosis as a key cell death mechanism in the perioperative period after surgical or anesthetic exposure, emerging evidence supports the possible involvement of ferroptosis in mediating the pathogenesis of perioperative neurocognitive impairment. This implies that therapeutic measures related to the inhibition of ferroptosis may be promising agents for improving cognitive decline.
Iron is an essential trace element for the vital activity of human cells, however, the overload of iron ions can cause impairment in neuronal function. Experimental animal studies have found that ferroptosis is involved in the pathology of perioperative neurocognitive disorders. The current investigation showed that retreatment with the iron chelators deferiprone and deferoxamine together with the lipophilic antioxidant ferrostatin-1 all inhibited the ferroptosis process in neuronal cells and improved the cognitive behavior of experimental animals. Downregulation of ACSL4 and MIB2 can both independently inhibit sevoflurane-induced ferroptotic cell death. However, the presence of the blood–brain barrier may reduce the amount of iron chelator that actually enters the nervous system, and the binding of iron to iron chelator in cells at non-lesioned sites may also bring about many side effects. Discovering effective techniques for delivering biological agents to the central nervous system is a challenge in treating almost all neurological disorders. Studies to inhibit ferroptosis to improve perioperative neurocognitive impairment are still in their infancy, and the reproducibility and accuracy of experimental findings remain to be further validated. In addition, most of these current experiments have been conducted in mice. Provided that the ethics of animal experimentation are met, further experiments could be considered in primates that are more closely related to humans to obtain data more compatible with human clinical trials. Overall, there are relatively few studies in this area and more high-quality studies are warranted in the future to explore the possibility of inhibiting ferroptosis to improve cognitive impairment. Drugs that can treat cognitive dysfunction-related disorders by regulating ferroptosis deserve further development and exploration.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
References
Weiser TG, Haynes AB, Molina G, et al. Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet. 2015;385(Suppl 2):S11.
Evered L, Silbert B, Knopman DS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br J Anaesth. 2018;121(5):1005–12.
Needham MJ, Webb CE, Bryden DC. Postoperative cognitive dysfunction and dementia: what we need to know and do. Br J Anaesth. 2017;119(suppl_1):i115–25.
Lin X, Chen Y, Zhang P, Chen G, Zhou Y, Yu X. The potential mechanism of postoperative cognitive dysfunction in older people. Exp Gerontol. 2020;130: 110791.
Jungwirth B, Zieglgänsberger W, Kochs E, Rammes G. Anesthesia and postoperative cognitive dysfunction (POCD). Mini Rev Med Chem. 2009;9(14):1568–79.
Migirov A, Chahar P, Maheshwari K. Postoperative delirium and neurocognitive disorders. Curr Opin Crit Care. 2021;27(6):686–93.
Relander K, Hietanen M, Nuotio K, et al. Cognitive dysfunction and mortality after carotid endarterectomy. Front Neurol. 2020;11: 593719.
Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367(1):30–9.
Cavallari M, Fong TG, Touroutoglou A, et al. Assessment of potential selection bias in neuroimaging studies of postoperative delirium and cognitive decline: lessons from the SAGES study. Brain Imaging Behav. 2022;16:1732.
Lei X, Guo Q, Zhang J. Mechanistic insights into neurotoxicity induced by anesthetics in the developing brain. Int J Mol Sci. 2012;13(6):6772–99.
Altay O, Suzuki H, Altay BN, Calisir V, Tang J, Zhang JH. Isoflurane versus sevoflurane for early brain injury and expression of sphingosine kinase 1 after experimental subarachnoid hemorrhage. Neurosci Lett. 2020;733: 135142.
Stratmann G, Lee J, Sall JW, et al. Effect of general anesthesia in infancy on long-term recognition memory in humans and rats. Neuropsychopharmacology. 2014;39(10):2275–87.
Dixon SJ, Lemberg KM, Lamprecht MR, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–72.
Angeli J, Shah R, Pratt DA, Conrad M. Ferroptosis inhibition: mechanisms and opportunities. Trends Pharmacol Sci. 2017;38(5):489–98.
Stockwell BR, Friedmann Angeli JP, Bayir H, et al. Ferroptosis: a regulated cell death nexus linking metabolism, redox biology, and disease. Cell. 2017;171(2):273–85.
Singh N, Haldar S, Tripathi AK, et al. Brain iron homeostasis: from molecular mechanisms to clinical significance and therapeutic opportunities. Antioxid Redox Signal. 2014;20(8):1324–63.
Cheng R, Dhorajia VV, Kim J, Kim Y. Mitochondrial iron metabolism and neurodegenerative diseases. Neurotoxicology. 2022;88:88–101.
Wang F, Wang J, Shen Y, Li H, Rausch WD, Huang X. Iron Dyshomeostasis and Ferroptosis: a new Alzheimer’s disease hypothesis. Front Aging Neurosci. 2022;14: 830569.
Chen X, Kang R, Kroemer G, Tang D. Broadening horizons: the role of ferroptosis in cancer. Nat Rev Clin Oncol. 2021;18(5):280–96.
Wu JR, Tuo QZ, Lei P. Ferroptosis, a recent defined form of critical cell death in neurological disorders. J Mol Neurosci. 2018;66(2):197–206.
Mou Y, Wang J, Wu J, et al. Ferroptosis, a new form of cell death: opportunities and challenges in cancer. J Hematol Oncol. 2019;12(1):34.
Gao M, Monian P, Quadri N, Ramasamy R, Jiang X. Glutaminolysis and Transferrin Regulate Ferroptosis. Mol Cell. 2015;59(2):298–308.
Kühn LC. Iron regulatory proteins and their role in controlling iron metabolism. Metallomics. 2015;7(2):232–43.
Gao G, Li J, Zhang Y, Chang YZ. Cellular iron metabolism and regulation. Adv Exp Med Biol. 2019;1173:21–32.
Li H, Liu Y, Shang L, et al. Iron regulatory protein 2 modulates the switch from aerobic glycolysis to oxidative phosphorylation in mouse embryonic fibroblasts. Proc Natl Acad Sci U S A. 2019;116(20):9871–6.
Fujimaki M, Furuya N, Saiki S, Amo T, Imamichi Y, Hattori N. Iron supply via NCOA4-mediated ferritin degradation maintains mitochondrial functions. Mol Cell Biol. 2019; 39(14).
Ajoolabady A, Aslkhodapasandhokmabad H, Libby P, et al. Ferritinophagy and ferroptosis in the management of metabolic diseases. Trends Endocrinol Metab. 2021;32(7):444–62.
Philpott CC. Iron on the move: mobilizing liver iron via NCOA4. Blood. 2020;136(23):2604–5.
Gao M, Monian P, Pan Q, Zhang W, Xiang J, Jiang X. Ferroptosis is an autophagic cell death process. Cell Res. 2016;26(9):1021–32.
Lin W, Wang C, Liu G, et al. SLC7A11/xCT in cancer: biological functions and therapeutic implications. Am J Cancer Res. 2020;10(10):3106–26.
Piani D, Fontana A. Involvement of the cystine transport system xc- in the macrophage-induced glutamate-dependent cytotoxicity to neurons. J Immunol. 1994;152(7):3578–85.
Yang WS, Kim KJ, Gaschler MM, Patel M, Shchepinov MS, Stockwell BR. Peroxidation of polyunsaturated fatty acids by lipoxygenases drives ferroptosis. Proc Natl Acad Sci U S A. 2016;113(34):E4966–75.
Doll S, Proneth B, Tyurina YY, et al. ACSL4 dictates ferroptosis sensitivity by shaping cellular lipid composition. Nat Chem Biol. 2017;13(1):91–8.
Kagan VE, Mao G, Qu F, et al. Oxidized arachidonic and adrenic PEs navigate cells to ferroptosis. Nat Chem Biol. 2017;13(1):81–90.
Kuang F, Liu J, Tang D, Kang R. Oxidative damage and antioxidant defense in ferroptosis. Front Cell Dev Biol. 2020;8: 586578.
Tacchini L, Bianchi L, Bernelli-Zazzera A, Cairo G. Transferrin receptor induction by hypoxia. HIF-1-mediated transcriptional activation and cell-specific post-transcriptional regulation. J Biol Chem. 1999;274(34):24142–6.
Yang L, Fan M, Du F, et al. Hypoxic preconditioning increases iron transport rate in astrocytes. Biochim Biophys Acta. 2012;1822(4):500–8.
Li H, Mapolelo DT, Dingra NN, et al. The yeast iron regulatory proteins Grx3/4 and Fra2 form heterodimeric complexes containing a [2Fe-2S] cluster with cysteinyl and histidyl ligation. Biochemistry. 2009;48(40):9569–81.
Karuppagounder SS, Alim I, Khim SJ, et al. Therapeutic targeting of oxygen-sensing prolyl hydroxylases abrogates ATF4-dependent neuronal death and improves outcomes after brain hemorrhage in several rodent models. Sci Transl Med. 2016;8(328):328–9.
Doll S, Freitas FP, Shah R, et al. FSP1 is a glutathione-independent ferroptosis suppressor. Nature. 2019;575(7784):693–8.
Kraft V, Bezjian CT, Pfeiffer S, et al. GTP cyclohydrolase 1/tetrahydrobiopterin counteract ferroptosis through lipid remodeling. ACS Cent Sci. 2020;6(1):41–53.
Mao C, Liu X, Zhang Y, et al. DHODH-mediated ferroptosis defence is a targetable vulnerability in cancer. Nature. 2021;593(7860):586–90.
Huang C, Yang M, Deng J, Li P, Su W, Jiang R. Upregulation and activation of p53 by erastin-induced reactive oxygen species contribute to cytotoxic and cytostatic effects in A549 lung cancer cells. Oncol Rep. 2018;40(4):2363–70.
Dong H, Qiang Z, Chai D, et al. Nrf2 inhibits ferroptosis and protects against acute lung injury due to intestinal ischemia reperfusion via regulating SLC7A11 and HO-1. Aging (Albany NY). 2020;12(13):12943–59.
Chiou B, Neal EH, Bowman AB, Lippmann ES, Simpson IA, Connor JR. Endothelial cells are critical regulators of iron transport in a model of the human blood-brain barrier. J Cereb Blood Flow Metab. 2019;39(11):2117–31.
Gaasch JA, Lockman PR, Geldenhuys WJ, Allen DD, Van der Schyf CJ. Brain iron toxicity: differential responses of astrocytes, neurons, and endothelial cells. Neurochem Res. 2007;32(7):1196–208.
Khan AI, Liu J, Dutta P. Iron transport kinetics through blood-brain barrier endothelial cells. Biochim Biophys Acta Gen Subj. 2018;1862(5):1168–79.
Leitner DF, Connor JR. Functional roles of transferrin in the brain. Biochim Biophys Acta. 2012;1820(3):393–402.
Ward RJ, Zucca FA, Duyn JH, Crichton RR, Zecca L. The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol. 2014;13(10):1045–60.
Zhang X, Gou YJ, Zhang Y, et al. Hepcidin overexpression in astrocytes alters brain iron metabolism and protects against amyloid-β induced brain damage in mice. Cell Death Discov. 2020;6(1):113.
Bishop GM, Dang TN, Dringen R, Robinson SR. Accumulation of non-transferrin-bound iron by neurons, astrocytes, and microglia. Neurotox Res. 2011;19(3):443–51.
Xu Y, Zhang Y, Zhang JH, et al. Astrocyte hepcidin ameliorates neuronal loss through attenuating brain iron deposition and oxidative stress in APP/PS1 mice. Free Radic Biol Med. 2020;158:84–95.
Xu J, Ling EA. Studies of the ultrastructure and permeability of the blood-brain barrier in the developing corpus callosum in postnatal rat brain using electron dense tracers. J Anat. 1994;184(Pt 2):227–37.
Wu LJ, Leenders AG, Cooperman S, et al. Expression of the iron transporter ferroportin in synaptic vesicles and the blood-brain barrier. Brain Res. 2004;1001(1–2):108–17.
Chen Z, Jiang R, Chen M, et al. Multi-copper ferroxidase deficiency leads to iron accumulation and oxidative damage in astrocytes and oligodendrocytes. Sci Rep. 2019;9(1):9437.
Dresselhaus EC, Meffert MK. Cellular specificity of NF-κB function in the nervous system. Front Immunol. 2019;10:1043.
Michell-Robinson MA, Touil H, Healy LM, et al. Roles of microglia in brain development, tissue maintenance and repair. Brain. 2015;138(Pt 5):1138–59.
McCarthy RC, Sosa JC, Gardeck AM, Baez AS, Lee CH, Wessling-Resnick M. Inflammation-induced iron transport and metabolism by brain microglia. J Biol Chem. 2018;293(20):7853–63.
Santiago González DA, Cheli VT, Wan R, Paez PM. Iron Metabolism in the peripheral nervous system: the role of DMT1, ferritin, and transferrin receptor in schwann cell maturation and myelination. J Neurosci. 2019;39(50):9940–53.
Rathore KI, Redensek A, David S. Iron homeostasis in astrocytes and microglia is differentially regulated by TNF-α and TGF-β1. Glia. 2012;60(5):738–50.
Connor JR, Menzies SL, St Martin SM, Mufson EJ. Cellular distribution of transferrin, ferritin, and iron in normal and aged human brains. J Neurosci Res. 1990;27(4):595–611.
Badaracco ME, Siri MV, Pasquini JM. Oligodendrogenesis: the role of iron. BioFactors. 2010;36(2):98–102.
Kroner A, Greenhalgh AD, Zarruk JG, Passos Dos Santos R, Gaestel M, David S. TNF and increased intracellular iron alter macrophage polarization to a detrimental M1 phenotype in the injured spinal cord. Neuron. 2014;83(5):1098–116.
Çolakoğlu M, Tunçer S, Banerjee S. Emerging cellular functions of the lipid metabolizing enzyme 15-Lipoxygenase-1. Cell Prolif. 2018;51(5): e12472.
Yang W, Wang X, Xu L, Li H, Wang R. LOX inhibitor HOEC interfered arachidonic acid metabolic flux in collagen-induced arthritis rats. Am J Transl Res. 2018;10(8):2542–54.
Weitzel F, Wendel A. Selenoenzymes regulate the activity of leukocyte 5-lipoxygenase via the peroxide tone. J Biol Chem. 1993;268(9):6288–92.
Yang WS, SriRamaratnam R, Welsch ME, et al. Regulation of ferroptotic cancer cell death by GPX4. Cell. 2014;156(1–2):317–31.
Sato N, Yako Y, Maruyama T, et al. The COX-2/PGE(2) pathway suppresses apical elimination of RasV12-transformed cells from epithelia. Commun Biol. 2020;3(1):132.
Hunot S, Brugg B, Ricard D, et al. Nuclear translocation of NF-kappaB is increased in dopaminergic neurons of patients with parkinson disease. Proc Natl Acad Sci U S A. 1997;94(14):7531–6.
An LN, Yue Y, Guo WZ, et al. Surgical trauma induces iron accumulation and oxidative stress in a rodent model of postoperative cognitive dysfunction. Biol Trace Elem Res. 2013;151(2):277–83.
Li Y, Pan K, Chen L, et al. Deferoxamine regulates neuroinflammation and iron homeostasis in a mouse model of postoperative cognitive dysfunction. J Neuroinflammation. 2016;13(1):268.
Rosenfeldt F, Wilson M, Lee G, et al. Oxidative stress in surgery in an ageing population: pathophysiology and therapy. Exp Gerontol. 2013;48(1):45–54.
Baxter MG, Fehr T. Developmental exposure to general anaesthesia: missed connections. Br J Anaesth. 2021;126(4):756–8.
Wu J, Yang JJ, Cao Y, et al. Iron overload contributes to general anaesthesia-induced neurotoxicity and cognitive deficits. J Neuroinflammation. 2020;17(1):110.
Wang M, Zuo Y, Li X, et al. Effect of sevoflurane on iron homeostasis and toxicity in the brain of mice. Brain Res. 2021;1757: 147328.
Zuo Y, Li B, Xie J, et al. Sevoflurane anesthesia during pregnancy in mice induces cognitive impairment in the offspring by causing iron deficiency and inhibiting myelinogenesis. Neurochem Int. 2020;135: 104693.
Hemmings HC Jr, Riegelhaupt PM, Kelz MB, et al. Towards a comprehensive understanding of anesthetic mechanisms of action: a decade of discovery. Trends Pharmacol Sci. 2019;40(7):464–81.
Xu H, Jiang H, Xie J. New insights into the crosstalk between NMDARs and iron: implications for understanding pathology of neurological diseases. Front Mol Neurosci. 2017;10:71.
Wang C, Liu F, Patterson TA, Paule MG, Slikker W Jr. Relationship between ketamine-induced developmental neurotoxicity and NMDA receptor-mediated calcium influx in neural stem cell-derived neurons. Neurotoxicology. 2017;60:254–9.
Zhang X, Shen F, Xu D, Zhao X. A lasting effect of postnatal sevoflurane anesthesia on the composition of NMDA receptor subunits in rat prefrontal cortex. Int J Dev Neurosci. 2016;54:62–9.
Chen Y, Khan RS, Cwanger A, et al. Dexras1, a small GTPase, is required for glutamate-NMDA neurotoxicity. J Neurosci. 2013;33(8):3582–7.
Garrick MD. Human iron transporters. Genes Nutr. 2011;6(1):45–54.
White RS, Bhattacharya AK, Chen Y, et al. Lysosomal iron modulates NMDA receptor-mediated excitation via small GTPase, Dexras1. Mol Brain. 2016;9:38.
Cheah JH, Kim SF, Hester LD, et al. NMDA receptor-nitric oxide transmission mediates neuronal iron homeostasis via the GTPase Dexras1. Neuron. 2006;51(4):431–40.
Liu R, Li X, Zhao G. Beclin1-mediated ferroptosis activation is associated with isoflurane-induced toxicity in SH-SY5Y neuroblastoma cells. Acta Biochim Biophys Sin (Shanghai). 2019;51(11):1134–41.
Fujii J, Homma T, Kobayashi S. Ferroptosis caused by cysteine insufficiency and oxidative insult. Free Radic Res. 2020;54(11–12):969–80.
Kang R, Zeh HJ, Lotze MT, Tang D. The Beclin 1 network regulates autophagy and apoptosis. Cell Death Differ. 2011;18(4):571–80.
Wirawan E, Lippens S, Vanden Berghe T, et al. Beclin1: a role in membrane dynamics and beyond. Autophagy. 2012;8(1):6–17.
Song X, Zhu S, Chen P, et al. AMPK-mediated BECN1 phosphorylation promotes ferroptosis by directly blocking system X(c)(-) activity. Curr Biol. 2018;28(15):2388-2399.e5.
Liu P, Yuan J, Feng Y, Chen X, Wang G, Zhao L. Ferroptosis contributes to isoflurane-induced neurotoxicity and learning and memory impairment. Cell Death Discov. 2021;7(1):72.
Xia Y, Sun X, Luo Y, Stary CM. Ferroptosis contributes to isoflurane neurotoxicity. Front Mol Neurosci. 2018;11:486.
Shichiri M. The role of lipid peroxidation in neurological disorders. J Clin Biochem Nutr. 2014;54(3):151–60.
Guo Y, Ping F, Cao Y, et al. Effects of omega-3 polyunsaturated fatty acids on cognitive function after splenectomy in rats. Biomed Res Int. 2021;2021:5513886.
Bhushan S, Li Y, Huang X, Cheng H, Gao K, Xiao Z. Progress of research in postoperative cognitive dysfunction in cardiac surgery patients: a review article. Int J Surg. 2021;95: 106163.
Liu B, Huang D, Guo Y, et al. Recent advances and perspectives of postoperative neurological disorders in the elderly surgical patients. CNS Neurosci Ther. 2022;28(4):470–83.
Lee H, Zandkarimi F, Zhang Y, et al. Energy-stress-mediated AMPK activation inhibits ferroptosis. Nat Cell Biol. 2020;22(2):225–34.
Li L, Sun S, Tan L, et al. Correction to “Polystyrene nanoparticles reduced ROS and inhibited ferroptosis by triggering lysosome stress and TFEB nucleus translocation in a size-dependent manner.” Nano Lett. 2019;19(12):9170.
Ge X, Zuo Y, Xie J, et al. A new mechanism of POCD caused by sevoflurane in mice: cognitive impairment induced by cross-dysfunction of iron and glucose metabolism. Aging (Albany NY). 2021;13(18):22375–89.
Yon JH, Daniel-Johnson J, Carter LB, Jevtovic-Todorovic V. Anesthesia induces neuronal cell death in the developing rat brain via the intrinsic and extrinsic apoptotic pathways. Neuroscience. 2005;135(3):815–27.
Hofacer RD, Deng M, Ward CG, et al. Cell age-specific vulnerability of neurons to anesthetic toxicity. Ann Neurol. 2013;73(6):695–704.
Zhao L, Gong H, Huang H, Tuerhong G, Xia H. Participation of mind bomb-2 in sevoflurane anesthesia induces cognitive impairment in aged mice via modulating ferroptosis. ACS Chem Neurosci. 2021;12(13):2399–408.
Cheng L, Zhu X, Liu Y, Zhu K, Lin K, Li F. ACSL4 contributes to sevoflurane-induced ferroptotic neuronal death in SH-SY5Y cells via the 5’ AMP-activated protein kinase/mammalian target of rapamycin pathway. Ann Transl Med. 2021;9(18):1454.
Sripetchwandee J, Wongjaikam S, Krintratun W, Chattipakorn N, Chattipakorn SC. A combination of an iron chelator with an antioxidant effectively diminishes the dendritic loss, tau-hyperphosphorylation, amyloids-β accumulation and brain mitochondrial dynamic disruption in rats with chronic iron-overload. Neuroscience. 2016;332:191–202.
Chen J, Li X, Ge C, Min J, Wang F. The multifaceted role of ferroptosis in liver disease. Cell Death Differ. 2022;29(3):467–80.
Zhang XY, Cao JB, Zhang LM, Li YF, Mi WD. Deferoxamine attenuates lipopolysaccharide-induced neuroinflammation and memory impairment in mice. J Neuroinflammation. 2015;12:20.
Pan K, Li X, Chen Y, et al. Deferoxamine pre-treatment protects against postoperative cognitive dysfunction of aged rats by depressing microglial activation via ameliorating iron accumulation in hippocampus. Neuropharmacology. 2016;111:180–94.
Shachar DB, Kahana N, Kampel V, Warshawsky A, Youdim MB. Neuroprotection by a novel brain permeable iron chelator, VK-28, against 6-hydroxydopamine lesion in rats. Neuropharmacology. 2004;46(2):254–63.
Sohn YS, Breuer W, Munnich A, Cabantchik ZI. Redistribution of accumulated cell iron: a modality of chelation with therapeutic implications. Blood. 2008;111(3):1690–9.
Hansen JB, Tonnesen MF, Madsen AN, et al. Divalent metal transporter 1 regulates iron-mediated ROS and pancreatic β cell fate in response to cytokines. Cell Metab. 2012;16(4):449–61.
Acknowledgements
We sincerely appreciate the support of the National Natural Science Foundation of China and the Outstanding Scientific Fund of Shengjing Hospital for this study.
Funding
This work was supported by the National Nature Science Foundation of China (No. 81870838 to Ping Zhao; No. 82001154 to Ziyi Wu) and the Outstanding Scientific Fund of Shengjing Hospital (No. 201708 to Ping Zhao).
Author information
Authors and Affiliations
Contributions
SY wrote the main manuscript text, and WZ revised the structure and content of the article. XH provided help on the creation of tables and pictures in the article. The whole process was finished under the supervision and assistance of PZ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not involved.
Consent for publication
All authors have seen the manuscript and approved its publication.
Competing interests
The authors declare that there is no conflict of interest regarding the publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, Y., Wu, Z., Xue, H. et al. Ferroptosis is involved in regulating perioperative neurocognitive disorders: emerging perspectives. J Neuroinflammation 19, 219 (2022). https://doi.org/10.1186/s12974-022-02570-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-022-02570-3