Abstract
Background
The Target Product Profile (TPP) is a tool used in industry to guide development strategies by addressing user needs and fostering effective communication among stakeholders. However, they are not frequently used in academic research, where they may be equally useful. This systematic review aims to extract the features of accessible TPPs, to identify commonalities and facilitate their integration in academic research methodology.
Methods
We searched peer-reviewed papers published in English developing TPPs for different products and health conditions in four biomedical databases. Interrater agreement, computed on random abstract and paper sets (Cohen’s Kappa; percentage agreement with zero tolerance) was > 0.91. We interviewed experts from industry contexts to gain insight on the process of TPP development, and extracted general and specific features on TPP use and structure.
Results
138 papers were eligible for data extraction. Of them, 92% (n = 128) developed a new TPP, with 41.3% (n = 57) focusing on therapeutics. The addressed disease categories were diverse; the largest (47.1%, n = 65) was infectious diseases. Only one TPP was identified for several fields, including global priorities like dementia. Our analyses found that 56.5% of papers (n = 78) was authored by academics, and 57.8% of TPPs (n = 80) featured one threshold level of product performance. The number of TPP features varied widely across and within product types (n = 3–44). Common features included purpose/context of use, shelf life for drug stability and validation aspects. Most papers did not describe the methods used to develop the TPP. We identified aspects to be taken into account to build and report TPPs, as a starting point for more focused initiatives guiding use by academics.
Discussion
TPPs are used in academic research mostly for infectious diseases and have heterogeneous features. Our extraction of key features and common structures helps to understand the tool and widen its use in academia. This is of particular relevance for areas of notable unmet needs, like dementia. Collaboration between stakeholders is key for innovation. Tools to streamline communication such as TPPs would support the development of products and services in academia as well as industry.
Similar content being viewed by others
Introduction
A Target Product Profile (TPP) is a strategic document outlining the desired characteristics of a planned product, procedure or service intended for a particular disease or use case. Its goal is to guide in addressing users’ needs, facilitating stakeholders’ communication, and making best use of resources to develop a successful product. TPPs encompass context of use features, such as the target disease and populations, and specific desired attributes of the product, procedure or service under development [1,2,3]. TPPs are widely used in industry as a planning tool to guide product development and ensure that relevant product features be aligned among stakeholders. They are therefore treated confidentially, containing sensitive information about a company’s assets, product development plans and strategies (See Table S1 for a concrete example of TPP).
Although not common practice yet, TPPs may be useful in academia as well. Like industry, academics also develop therapeutics and diagnostics. However, academic research is often slower in adopting tools for systematic development, with consequent lower efficiency of translational research [4]. For example, the field of neurodegenerative disorders is validating biomarkers for Alzheimer’s disease since 2009 [5, 6], but only in 2017 did it import a systematic validation framework [7], first published in 2001 for oncology research [8] and similar to others used well before for imaging [9] and other biomarkers [10]. Adopting good practice procedures and tools commonly used in industry settings may reduce waste of efforts and costs, and increase the efficiency of academic translational research as well. Noteworthy, the World Health Organization (WHO) recommends the use of TPPs to facilitate the communication with research project funders to align funding strategies with prioritised unmet public healthcare needs. This is now urgent for the dementia field, to strive to meet the innovation goals set by the 2017 Global Action Plan, that, despite many efforts, still remain a distant ambition [11, 12]. Facilitating the incorporation of TPPs among the methods used in this field means therefore bringing a pivotal tool to upgrade translational methods and help boost its innovation efforts. The example of neurodegenerative disorders represents well several fields with a high prevalence of unmet needs.
The effort to help researchers to adopt TPPs was already initiated with a previous systematic review, summarizing the methods currently used to develop them and the sources used for the inclusion for each feature [13]. Focused on diagnostic tests, the authors found TPPs for infectious diseases only, and identified a 3-phase process for their development: (1) identifying the unmet need, (2) initial drafting of the TPP, and (3) building consensus among stakeholders. The outcome of that systematic review provided an insightful first glimpse on TPPs applications outside the pharma industry, as well as the rudiments to adapt the method to academic research. Our review aims to expand on these results and extract key structural features of TPPs across different therapeutic areas and product types, to gain a wider understanding of the tool’s structure and development and facilitate its use by academic researchers.
Methods
This work stems from the IMI-2-funded project EPND (European Platform for Neurodegenerative Disorders – epnd.org). IMI (www.imi.europa.eu) is a collaborative initiative between the European Commission and EFPIA (European Federation of Pharmaceutical Industries and Associations), requiring the collaboration between partners from both academia and industry. EPND aims to build a platform making existing data and samples on neurodegenerative disorders FAIR (findable, accessible, interoperable and reusable). During the development of such platform, academic and industry project partners contributed to define a TPP supporting the development of the platform. As researchers, we leveraged this experience and know-how, to generate this review and try to import the tool for academic research.
We reported our methods following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14]. The PRISMA checklist is provided as supplementary material (see Supplementary material S2). The protocol for this systematic review was not registered in an open access platform. We performed the systematic review as detailed below. Then, based on the extracted data, we highlighted key features and the structure of retrieved TPPs, that we believe are useful to framework the tool.
Information sources
Publication search:
We searched relevant publications in the PubMed, Medline, CINHAL, and Scopus biomedical databases in January 2023. Additionally, we hand-searched and screened primary publications in one identified systematic review. For grey literature, a Google search using the terms “target product profile” was used to identify publicly available TPPs (e.g., WHO TPPs, FIND, PATH). These TPPs were used to guide the conceptualization of the systematic review and the development of the search strategy. We also referred to the publicly available WHO TPPs [15] to understand the typical process and the methods commonly used to draft TPPs.
Interviews:
We asked availability to experts from the network of the last author, and to 3 regulators (Dutch, German and Norwegian), known for their activity within the European Medicine Agency. Regulators reported no familiarity with the tool (Netherlands and Germany) or did not reply (Norway). Four experts (AG, MG, MR, JS) from leading medical product development or consultancy companies accepted to be interviewed and provided general information on TPP use in the industry. The interviewed experts were senior professionals with extensive expertise on multiple aspects of research and development in pharma. Here we report their initials, affiliation and role at the time of the interview, and any additional expertise particularly relevant for this review: AG: UCB, Senior Global Director; external engagement with clinical and governmental communities for early clinical development; additional experience on regulatory intelligence through activities with CIRS (Center for Innovation and Regulatory Science). MG: AbbVie, Industry Co-Director. MR: IDEA Pharma, CEO. IDEA Pharma is a consultancy company advising on the path-to-market strategy. JS: AC Immune, Chief Medical Officer with broad responsibility for all clinical development functions. No confidential material was disclosed during the interviews. The collected qualitative information guided the review process and provided insights into how to process and contextualise the results.
Search strategy
Using iterations of key terms such as “target product profile”, TPP, “quality by design” or QbD or QTTP we formulated a comprehensive search strategy applicable to all databases. The search strategy was: (“target product profile” OR TPP OR QTTP OR “quality by design” OR QdB).
Eligibility criteria of included studies for final analysis
We included papers published in English that reported the development or revision of a target product profile (TPP) or described a pre-existing TPP used for the development of products across any health field. There were no restrictions on the publication date. Publications were eligible if they provided a TPP structure in the form of a table, figure or narrative description of the TPP features.
Selection and data collection process
The first author screened all titles and abstracts to identify relevant publications using Rayyan, and then conducted a full-text screening of the included studies. A second reviewer (NL) independently screened 12% of the abstracts (n = 78) and 15% of the full-texts (n = 52). We calculated the inter-rater reliability between the two reviewers for both abstract and full-text screening with the Cohen’s Kappa and/or percentage agreement with zero tolerance using R Studio [16]. We used Zotero to manage and store references of included studies and created a data extraction tool using Excel.
Data items
The target data items to be extracted included content, product type, disease category and the specific disease, performance thresholds for each TPP feature, authors’ affiliation, a full list of TPP features, the number and type of features and categories thereof, and the methods deployed to develop the TPP. We defined the data items as follows:
Content:
Describes whether a publication reports the development of a new TPP, revises a pre-defined TPP, or only describes an existing TPP.
Product type:
Indicates whether the target product consists of therapeutics, diagnostics, vaccine, medical device, or other (e.g., app, drug delivery system, etc.).
Disease category:
Describes whether the disease for which the TPP was reported was an infectious or non-infectious disease, as well as the specific disease.
Thresholds:
Reports whether each TPP feature includes one (target), two (minimal, ideal), or three (current practice, minimum acceptable, ideal) levels of possible performance or target quality achievement.
Affiliation of publishing authors:
Classifies the affiliation of publishing authors into academic (university, research institute, independent researchers), private (industry, consultancies, or other for-profit organisations), or public-private partnership (PPP) for collaborations between academic and private organisations.
List of TPP features:
The names of all features included in each TPP were stratified by product type.
Measure of variability:
Consists of the number of TPP features in each TPP.
Categories of TPP features:
Includes the number and type of categories by which TPP features were grouped. For example, the category named “Scope” may include TPP features such as target population, intended use, and the level of health care system implementation; similarly, “Operational characteristics” typically includes features such as cost of product, shelf life, power requirements, and training needs.
Framework:
Describes which framework was utilised to structure the TPP, e.g., the WHO or the FDA TPP guidance.
Criteria for the choice of TPP features:
Reports how an initial pool of TPP features and their target levels were chosen.
Consensus approach:
Categorises which kind of consensus procedure was followed to select the final set of TPP features. The approaches were divided into formal (e.g., Delphi process or survey) and informal (e.g., discussion in virtual or in-person meetings).
Experts:
Describes which experts were involved (e.g., clinicians, researchers, relevant product manufacturers, etc.).
Patient-public involvement:
Reports whether patient populations or the public were involved in the process of developing a TPP.
Results
From the biomedical databases and hand searching, we identified 1314 records. After title and abstract screening, 337 met the eligibility criteria for full-text review, and 138 publications [3, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153] were eligible for data extraction (see Fig. 1 and Table S2 for the reasons and references of excluded studies). Raters had 100% agreement for abstract screening and Cohen’s Kappa = 0.912 (p-value < 0.001; 96.1% agreement with zero tolerance) for full-text screening.
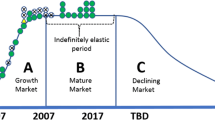
Reports of TPPs steadily increased following the publications of the FDA [1] and ICH Q8 R2 [154] guidelines (Fig. 2), most contributions being in 2020. Of the 138 papers included in our review, 92% developed a new TPP, 4% revised a predefined TPP, and 4% described an existing TPP, with no overlap among these groups. The ICH Q8 R2 [154] was the most widely used framework (54%), followed by the FIND [155] (26%), the WHO [15] (15.4%) and the FDA guidance [1] (7.7%) (Table 1, upper panel). Combinations of frameworks (e.g., WHO and FIND) were also used.
Distribution of publications on target product profiles (TPP) by year in relation to significant TPP-related events or publications by the WHO and the FDA. Panel A demonstrates the distribution of the 337 publications included after title and abstract screening. Panel B demonstrates the distribution of the 138 publications included after full text screening. Abbreviations TPP: Target product profile, FDA: Food and Drug Administration, WHO: World Health Organisation, R & D: Research and Development
Product types included mostly therapeutics (41.3%) and diagnostics (21%), and a variety of products, like apps, new technology for product development, drug delivery systems, or clinical practice guidelines (“other products”: 29.7%; Fig. 3, Table S3). TPPs were used for products targeting infectious (47.1%) and non-infectious (25.4%) diseases, and unspecified disease categories, e.g., skin diseases possibly due to either infectious or non-infectious causes (26.8%; Fig. 3, Table S4). Among non-infectious diseases, one TPP was for a drug for Alzheimer’s disease [57], and one for a drug delivery system for an unspecified disease category [118]. The number of included features (range 3–44) was mostly between 3 and 8 (44%), across product types (Fig. 4; Figures S1-3). These included target population, indication, storage conditions and shelf life (Table 2; Table S5). Among TPPs reporting performance thresholds (89.2%), 57.9% set one target threshold, 28.9% set two (“minimum acceptable” and “ideal”), and 2.2% three (“current practice”, “minimum acceptable”, and “ideal”; Table S3). In the 15% of publications grouping TPP features into categories, “Scope” was the most frequent (90%; Tables S6-S7); others included “Operational”, “Performance”, and “Test characteristics” (complete list in Table S6). Criteria to define features and target levels were clarified in 17% of papers (Table 1, lower panel). Methods to agree on the TPP features were reported in 22% of the papers: these included formal consensus (e.g., Delphi process; 46%), and combined formal and informal approaches (e.g., virtual/in-person meetings or workshops; 33.3%) (Table S8).
Most of the retrieved TPPs were published by authors from academia (56.5%), 11.6% by authors with non-academic affiliations, and 31.9% within hybrid collaborations. Twenty-seven (20%) of the papers mentioned which experts were involved, and their fields of expertise. These included academic researchers, clinicians, experts from the WHO, and stakeholders related to product development (end users, manufacturing companies, regulators) (Table S9). One group explicitly reported the involvement of civil societies representatives [93], but none reported involving patient populations or the public directly.
Based on the overall extracted data, we identified essential aspects relevant to developing a new TPP, that would be good to report to enable full understanding and replication by other groups (Table 3).
Discussion
We conducted a systematic review to extract the features and structure of published TPPs across various therapeutic areas, to facilitate the incorporation of this tool in academic research. Most papers included in our review developed a new TPP, and mostly focused on developing treatments in the field of infectious diseases. Several medical fields (e.g., poliomyelitis, rheumatic fever, or tropical diseases) had only one TPP reported for any of their products. This happened also for diseases characterized by high unmet need and global prioritization, like the case of Alzheimer’s disease [57]. We found that the methods used to develop TPPs, their specific features, and the information provided to understand their structure varied considerably also within product or disease category, most papers providing limited or no explanation of how TPPs were developed.
To our knowledge, only one other systematic review on TPPs exists [13], focusing on diagnostic tests, and uniquely retrieving contributions for infectious diseases. Like us, Cocco and colleagues found a generally poor description of the methods employed to build TPPs, although they could extract a common 3-phase structure and the distinct dimensions of “activities”, “source of input information” and “contributing stakeholders”. The authors underlined that further research is needed to improve support for researchers in understanding and adopting the tool. In our review, we extended such examination beyond diagnostic tests, and tried to extract additional dimensions in TPP development that may further help to understand its general structure and logics (Table 3). Such dimensions may not be readily applicable to any field at present. For example, as a starting step, we recommend choosing a reference framework. However, as also noted by Cocco et al. [13], existing frameworks like the FDA guidance apply to drug development. They may not be directly transferable to diagnostics, and formal guidance on developing TPPs for diagnostics is not yet available. We believe that making this gap explicit and inviting researchers to identify a reference framework anyway may elicit consequent constructive steps. In this specific example, researchers developing a new TPP for diagnostics may decide to choose, as a reference framework, the structure of a previous TPP described in greater detail for a biomarker (see for example references 26, 28, 38 and 60 in Cocco’s paper); furthermore, outlining such gap explicitly may lead methodologists or other organizations or stakeholders to produce TPP guidance specifically adapted to diagnostics.
By widening the scope of therapeutic areas and products relative to the previous review, we sought to better outline the heterogeneity of TPPs, and extract more features contributing to their structure. To this regard, we underline that the TPPs scope is meant to be heterogeneous in nature, as they serve the development of specific products that need to differentiate themselves in the market. This needed heterogeneity adds to inconsistent reporting across the few documents that can escape confidentiality, which constitutes an additional hurdle to the effort of academic researchers to adopt the tool. On the other hand, a wide representation of different TPPs is needed to extract and communicate their very structure. In their review, Cocco et al. [13] not only focused on the field of diagnostics, and uniquely retrieved TPPs for infectious diseases, but also presented a quite consistent purpose of TPPs, mainly supporting the validation of diagnostic tests within a regulatory perspective. Despite our wider focus, also our study captured a mainly regulatory perspective. Indeed, a task like product validation can easily constitute a shared goal across independent research organizations, and can therefore be retrieved relatively easily in published documents. However, we underline here that TPPs are meant to support any development perspective (e.g., ensuring marketability, competitiveness or refundability within an HTA context). These perspectives, only to a limited degree captured in our review [84], may well be in the interest of academic developments as well. In industry, these other perspectives are usually represented in separate TPPs for the same product and each indication identified. We therefore underline that the mainly regulatory perspective emerging from our, as well as from Cocco’s, review is not the only nor the main purview of TPPs. Consistently, we do not support the idea that a TPP mainly serves single unitary purposes: indeed, they rather try to serve cross-functional aims, although they may not have one standard, coherent or all-inclusive form. This complexity enables the needed flexibility in operational contexts, but also makes it more difficult to understand the tool, for those who never used it. Finally, within the aim of demonstrating product validity, Cocco et al. highlighted a considerable absence of clinical utility features in TPPs for diagnostic products [13]; consistently, we found that, regardless of product type, the development of TPPs did not directly involve patient populations or the public, whose participation is important to define clinical significance in specific settings and demonstrate impact on clinically relevant outcomes. Different from academia, it is common in industrial practices to include patients or the public directly, and from the early stages of a product development; detailing this aspect in future TPP guidance may help upgrade academic product development and help it to manage the complex task of demonstrating clinical utility.
Overall, our extensive data extraction aimed to come up with a common structure helping academics to understand and use TPPs. Along with the features previously identified by Cocco et al., the items reported in Table 3 are general enough to be considered for inclusion in most TPPs, and relevant enough to be commendable for potential reporting guidelines on TPP development. Defining guidance as well as reporting recommendations requires independent dedicated efforts. With this work, we provided additional concrete elements for further initiatives supporting TPP integration in academic research. Such efforts are particularly urgent for diseases characterized by numerous unmet needs. Among these, the field of neurodegenerative diseases leading to dementia provides a concrete and current example: the 2017 Global Action Plan set goals to tackle the global priority of dementia [12], but the global status report on the public health response to dementia anticipated that these goals will not be achieved by the 2025 deadline [156]. WHO recommended using TPPs to boost efficiency in the field of infectious disease through a blueprint [157] recently provided also for dementia [11, 158]. Indeed, the use of tools like the TPP, already constituting good industrial practice, is increasingly relevant in any academic contexts, with an increasing interest in developing products also in the pharmacology field, and would support the efficiency of developing any kind of product, including medical procedures or services, by improving communication and interactions with industry and other stakeholders. Despite major dedicated efforts, like those supported by grant frameworks like the European Innovative Health Initiative, requiring that academics be paired with industry partners for large research projects, such interactions are still difficult, and concrete initiatives like ours, focusing on importing specific translational tools, methods and procedures, are essential to enable concrete steps forward. However, this overall picture raises pivotal questions about how to increase the efficiency of translational research. Which are exactly the stakeholders, collectively represented by WHO, supposedly interested in investing to translate and validate a reference methodology to develop TPPs, and promote their use in academic contexts across disease areas? Which incentives may encourage researchers to use them? Similar questions link our effort to the need to better understand and help improve the ecosystem of current translational research [159], where communication among academia, industry and relevant stakeholders is key to overcome gaps, and deserves greater attention.
Similar to the previous review, also our results show a striking majority of TPPs published for products in infectious diseases, with an exponential increase that, from the publication of the FDA Guidance for Industry guidelines in 2007, peaked during the COVID-19 epidemic. This prevalence of TPPs in the field of infectious diseases can be explained with the urgency to act and control rapidly spreading diseases [160], and can also be attributed to the successful implementation of the WHO blueprint [157]. The fact that we could identify many more publications in this rather than any other field also highlights the main constraint of our study: TPPs are usually confidential documents that cannot be circulated beyond the company producing them. The field of infectious diseases, however, may not be the most attractive area of development for industry: microbial resistance allows only limited time and distribution for a product to be effective, the treatment duration is very limited, antimicrobials’ price is generally low, and their need is mostly felt in countries with limited budget. Along with the highly unmet need posed by infectious diseases, a great public and academic involvement pushes the production of dedicated products, which may explain the disproportionate prevalence of public TPPs in this, compared to any other medical fields (Table S4). Some of the features characterizing the field of infectious diseases, like the increasing global unmet need with major distribution in LMICs, also apply to the field of dementia; this may provide additional motivation to greater adoption of TPPs in academic research in this field. On the other hand, developing TPPs in fields with similar features as that of neurodegenerative disorders may present more complex challenges. The etiology of complex diseases is often not definitively understood; genes, as well as their variable interaction with the environment, generate for example different degrees of cerebral reserve, and a number of factors interact with clinical outcomes and treatment effects; the urgency to bring innovation to clinics may lead to overlook validation steps for products or procedures, sometimes mistakenly not expected to originate negative effects, like biomarkers. Analogous considerations and analyses may help support the adoption of TPPs also in other such medical fields, where they are not yet widely used (Table S4). Moreover, the fact that independent laboratories may not be consistently aligned on a common translational methodology could provide additional rationale for producing shared and accessible TPPs, potentially benefitting all those working at a common goal. Indeed, the confidentiality protecting property for industry can well apply to academic research as well, thus it is relevant to identify the specific areas where the use of TPPs can be shared and possibly validated, to enable academics to familiarise with the methodology and then increase their use, either open or confidential. Further research in this direction may include retrieving TPPs developed for assets that subsequently failed, or by companies that are no longer active, and extract further learnings also leveraging reasons for failure.
Our findings indicate that TPP-related publications are mostly published by academics, although this finding is biased by the nature of this study. Different from the previous review [13], we only targeted full papers in scholar communications, using grey literature only to guide our understanding and framing of the data. We did find TPPs published by private organizations or public-private partnerships, however, by definition, we could only access information that was not confidential, an issue in common with the previous review [13]. We attenuated this bias by interviewing and involving some leading experts, all from industry contexts, able to provide a wider and more representative insight into this typically industrial procedure. We did not perform a formal assessment of risk of bias, however not feasible in this type of study, and did not extract data regarding the geographic location of TPP publications, connected with potential variations in unmet needs and priorities across health conditions, and consequently the product, depending on geography. From a methodological point of view, moreover, we guaranteed reliability only by assessing reviewers’ consistence on subsets of abstracts and full papers.
Conclusion
This review highlights the heterogenous features of TPPs and their limited representation in academic literature besides the field of infectious diseases, and provides further concrete support for researchers trying to use TPPs in academic research. Our results can also feed future initiatives to adapt guidance for specific fields and to develop TPP reporting guidelines. Besides supporting researchers’ understanding and use of the tool in academic contexts, this would improve their ability to interact with regulators, HTA experts, and end users, whose contribution is needed along the whole translational continuum. Much more research is needed however to improve communication between academia and industry, stakeholder alignment, and the efficiency of academic translational research in general. Such efforts should help a wider understanding of the ecosystem and incentives structuring current translational research, and should be pursued to foster progress on global priorities.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AD:
-
Alzheimer’s disease
- FDA:
-
Food and Drug Administration
- HTA:
-
Health Technology Assessment
- ICH:
-
International Conference on Harmonisation
- NDD:
-
Neurodegenerative diseases
- PPP:
-
Public-Private Partnership
- QbD:
-
Quality by design
- TPP:
-
Target product profile
- WHO:
-
World Health Organisation
References
FDA. Guidance for Industry and Review Staff Target Product Profile — A Strategic Development Process Tool. 2007.
Organization WH. Links to TPP. https://www.who.int/observatories/global-observatory-on-health-research-and-development/analyses-and-syntheses/target-product-profile/who-target-product-profiles.
Singh G. Target Product Profile and Clinical Development Plan. Pharmaceutical Medicine and Translational Clinical Research. Elsevier; 2018. pp. 65–80.
Boccardi M. Translational process. J Transl Med. 2023;21(1):677.
Vemuri P, Wiste HJ, Weigand SD, Shaw LM, Trojanowski JQ, Weiner MW, et al. MRI and CSF biomarkers in normal, MCI, and AD subjects: predicting future clinical change. Neurology. 2009;73(4):294–301.
Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9(1):119–28.
Boccardi M, Gallo V, Yasui Y, Vineis P, Padovani A, Mosimann U, et al. The biomarker-based diagnosis of Alzheimer’s disease. 2-lessons from oncology. Neurobiol Aging. 2017;52:141–52.
Pepe MS, Etzioni R, Feng Z, Potter JD, Thompson ML, Thornquist M, et al. Phases of biomarker development for early detection of cancer. J Natl Cancer Inst. 2001;93(14):1054–61.
Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Mak. 1991;11(2):88–94.
Lijmer JG, Leeflang M, Bossuyt PMM. Proposals for a phased evaluation of medical tests. Med Decis Mak. 2009;29(5):E13–21.
Cataldi R, Chowdhary N, Seeher K, Moorthy V, Dua T. A blueprint for the worldwide research response to dementia. Lancet Neurol. 2022;21(8):690–1.
Organization WH. Global action plan on the public health response to dementia 2017–2025. 2017. https://www.who.int/publications/i/item/global-action-plan-on-the-public-health-response-to-dementia-2017---2025.
Cocco P, Ayaz-Shah A, Messenger MP, West RM, Shinkins B. Target product profiles for medical tests: a systematic review of current methods. BMC Med. 2020;18(1):119.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Organization WH. Links to WHO TPPs and PPCs. https://www.who.int/observatories/global-observatory-on-health-research-and-development/analyses-and-syntheses/target-product-profile/links-to-who-tpps-and-ppcs.
Team R, RStudio. Integrated Development for R. RStudio [Internet]. In: PBC, editor. Boston, MA2020.
Chua A, Prat I, Nuebling CM, Wood D, Moussy F. Update on Zika Diagnostic tests and WHO’s related activities. PLoS Negl Trop Dis. 2017;11(2):e0005269.
Denkinger CM, Kik SV, Cirillo DM, Casenghi M, Shinnick T, Weyer K, et al. Defining the needs for next generation assays for tuberculosis. J Infect Dis. 2015;211(suppl2):S29–38.
Ding XC, Ade MP, Baird JK, Cheng Q, Cunningham J, Dhorda M, et al. Defining the next generation of Plasmodium Vivax diagnostic tests for control and elimination: target product profiles. PLoS Negl Trop Dis. 2017;11(4):e0005516.
Donadeu M, Fahrion AS, Olliaro PL, Abela-Ridder B. Target product profiles for the diagnosis of Taenia solium taeniasis, neurocysticercosis and porcine cysticercosis. PLoS Negl Trop Dis. 2017;11(9):e0005875.
Ebels KB, Clerk C, Crudder CH, McGray S, Magnuson K, Tietje K et al. editors. Incorporating user needs into product development for improved infection detection for malaria elimination programs. 2014 IEEE Global Humanitarian Technology Conference (GHTC); 2014 2014/10//. San Jose, CA: IEEE.
Lim MD, Brooker SJ, Belizario VY, Gay-Andrieu F, Gilleard J, Levecke B, et al. Diagnostic tools for soil-transmitted helminths control and elimination programs: a pathway for diagnostic product development. PLoS Negl Trop Dis. 2018;12(3):e0006213.
Pal S, Jasper LE, Lawrence KL, Walter M, Gilliland T, Dauner AL, et al. Assessing the Dengue Diagnosis Capability Gap in the Military Health System. Mil Med. 2016;181(8):756–66.
Solomon AW, Engels D, Bailey RL, Blake IM, Brooker S, Chen J-X, et al. A Diagnostics platform for the Integrated Mapping, Monitoring, and Surveillance of Neglected Tropical diseases: Rationale and Target Product profiles. PLoS Negl Trop Dis. 2012;6(7):e1746.
Toskin I, Murtagh M, Peeling RW, Blondeel K, Cordero J, Kiarie J. Advancing prevention of sexually transmitted infections through point-of-care testing: target product profiles and landscape analysis. Sex Transm Infect. 2017;93(S4):S69–80.
Utzinger J, Becker SL, Van Lieshout L, Van Dam GJ, Knopp S. New diagnostic tools in schistosomiasis. Clin Microbiol Infect. 2015;21(6):529–42.
Abdulgader SM, Okunola AO, Ndlangalavu G, Reeve BWP, Allwood BW, Koegelenberg CFN, et al. Diagnosing tuberculosis: what do New Technologies allow us to (not). Do? Respiration. 2022;101(9):797–813.
Adepoyibi T, Lilis L, Greb H, Boyle D. Which attributes within target product profiles for tuberculosis diagnostics are the most important to focus on? int j Tuberc lung dis. 2018;22(4):425–8.
Alafeef M, Pan D. Diagnostic approaches for COVID-19: lessons learned and the path Forward. ACS Nano. 2022;16(8):11545–76.
Alonso-Padilla J, Abril M, De Alarcón B, Almeida IC, Angheben A, Araujo Jorge T, et al. Target product profile for a test for the early assessment of treatment efficacy in Chagas disease patients: an expert consensus. PLoS Negl Trop Dis. 2020;14(4):e0008035.
Amasya G, Badilli U, Aksu B, Tarimci N. Quality by design case study 1: design of 5-fluorouracil loaded lipid nanoparticles by the W/O/W double emulsion — solvent evaporation method. Eur J Pharm Sci. 2016;84:92–102.
Apolinário AC, Ferraro RB, De Oliveira CA, Pessoa A Jr, De Oliveira Rangel-Yagui C. Quality-by-Design Approach for Biological API encapsulation into Polymersomes using off-the-Shelf materials: a study on L-Asparaginase. AAPS PharmSciTech. 2019;20(6):251.
Arnold SLM. Target Product Profile and Development path for Shigellosis Treatment with antibacterials. ACS Infect Dis. 2021;7(5):948–58.
Arora D, Nanda S. Quality by design driven development of resveratrol loaded ethosomal hydrogel for improved dermatological benefits via enhanced skin permeation and retention. Int J Pharm. 2019;567:118448.
Arranja A, Gouveia LF, Gener P, Rafael DF, Pereira C, Schwartz S, et al. Self-assembly PEGylation assists SLN-paclitaxel delivery inducing cancer cell apoptosis upon internalization. Int J Pharm. 2016;501(1–2):180–9.
Awotwe-Otoo D, Agarabi C, Wu GK, Casey E, Read E, Lute S, et al. Quality by design: impact of formulation variables and their interactions on quality attributes of a lyophilized monoclonal antibody. Int J Pharm. 2012;438(1–2):167–75.
Beg S, Katare OP, Singh B. Formulation by design approach for development of ultrafine self-nanoemulsifying systems of rosuvastatin calcium containing long-chain lipophiles for hyperlipidemia management. Colloids Surf B. 2017;159:869–79.
Beg S, Saini S, Bandopadhyay S, Katare OP, Singh B. QbD-driven development and evaluation of nanostructured lipid carriers (NLCs) of Olmesartan medoxomil employing multivariate statistical techniques. Drug Dev Ind Pharm. 2018;44(3):407–20.
Beg S, Sandhu PS, Batra RS, Khurana RK, Singh B. QbD-based systematic development of novel optimized solid self-nanoemulsifying drug delivery systems (SNEDDS) of lovastatin with enhanced biopharmaceutical performance. Drug Delivery. 2015;22(6):765–84.
Bell M, Webster L, Woodland A. Research Techniques made simple: an introduction to Drug Discovery for Dermatology. J Invest Dermatology. 2019;139(11):2252–e71.
Bengtson M, Bharadwaj M, Bosch AT, Nyakundi H, Matoke-Muhia D, Dekker C, et al. Matching development of point-of-care diagnostic tests to the local context: a case study of visceral leishmaniasis in Kenya and Uganda. Glob Health Sci Pract. 2020;8(3):549–65.
Bergström F, Lindmark B. Accelerated drug discovery by rapid candidate drug identification. Drug Discovery Today. 2019;24(6):1237–41.
Bernatchez JA, Tran LT, Li J, Luan Y, Siqueira-Neto JL, Li R. Drugs for the treatment of Zika Virus infection. J Med Chem. 2020;63(2):470–89.
Burrows JN, Duparc S, Gutteridge WE, Van Hooft R, Kaszubska W, Macintyre F, et al. New developments in anti-malarial target candidate and product profiles. Malar J. 2017;16(1):26.
Burrows J, Slater H, Macintyre F, Rees S, Thomas A, Okumu F, et al. A discovery and development roadmap for new endectocidal transmission-blocking agents in malaria. Malar J. 2018;17(1):462.
Campbell A, Brieva T, Raviv L, Rowley J, Niss K, Brandwein H, et al. Concise review: process development considerations for cell therapy. Stem Cells Translational Med. 2015;4(10):1155–63.
Carballar-Lejarazú R, Ogaugwu C, Tushar T, Kelsey A, Pham TB, Murphy J, et al. Next-generation gene drive for population modification of the malaria vector mosquito, <i > Anopheles gambiae</i >. Proc Natl Acad Sci USA. 2020;117(37):22805–14.
Chang R-K, Raw A, Lionberger R, Yu L. Generic development of topical dermatologic products, part II: quality by design for Topical Semisolid products. AAPS J. 2013;15(3):674–83.
Chappidi SR, Bhargav E, Marikunte V, Chinthaginjala H, Vijaya Jyothi M, Pisay M, et al. A cost effective (QbD) Approach in the Development and Optimization of Rosiglitazone Maleate Mucoadhesive Extended Release tablets – in Vitro and Ex vivo. Adv Pharm Bull. 2019;9(2):281–8.
Charoo NA, Shamsher AAA, Zidan AS, Rahman Z. Quality by design approach for formulation development: a case study of dispersible tablets. Int J Pharm. 2012;423(2):167–78.
Chudiwal SS, Dehghan MHG. Quality by design approach for development of suspension nasal spray products: a case study on budesonide nasal suspension. Drug Dev Ind Pharm. 2016;42(10):1643–52.
Chudiwal SS, Dehghan MHG. Quality by design (QbD) approach for design and development of drug-device combination products: a case study on flunisolide nasal spray. Pharm Dev Technol. 2018;23(10):1077–87.
Chudiwal VS, Shahi S, Chudiwal S. Development of sustained release gastro-retentive tablet formulation of nicardipine hydrochloride using quality by design (QbD) approach. Drug Dev Ind Pharm. 2018;44(5):787–99.
Costa CP, Cunha S, Moreira JN, Silva R, Gil-Martins E, Silva V, et al. Quality by design (QbD) optimization of diazepam-loaded nanostructured lipid carriers (NLC) for nose-to-brain delivery: toxicological effect of surface charge on human neuronal cells. Int J Pharm. 2021;607:120933.
Crcarevska M, Dimitrovska A, Sibinovska N, Mladenovska K, Slavevska Raicki R, Glavas Dodov M. Implementation of quality by design principles in the development of microsponges as drug delivery carriers: identification and optimization of critical factors using multivariate statistical analyses and design of experiments studies. Int J Pharm. 2015;489(1–2):58–72.
Cruz I, Albertini A, Barbeitas M, Arana B, Picado A, Ruiz-Postigo JA, et al. Target Product Profile for a point-of-care diagnostic test for dermal leishmaniases. Parasite Epidemiol Control. 2019;5:e00103.
Cunha S, Costa CP, Loureiro JA, Alves J, Peixoto AF, Forbes B, et al. Double optimization of Rivastigmine-loaded nanostructured lipid carriers (NLC) for nose-to-brain delivery using the quality by Design (QbD) Approach: formulation variables and instrumental parameters. Pharmaceutics. 2020;12(7):599.
Dailey P, Osborn J, Ashley E, Baron E, Dance D, Fusco D, et al. Defining System requirements for simplified blood culture to enable widespread use in resource-limited settings. Diagnostics. 2019;9(1):10.
Dalal R, Shah J, Gorain B, Choudhury H, Jacob S, Mehta TA, et al. Development and optimization of Asenapine Sublingual Film using QbD Approach. AAPS PharmSciTech. 2021;22(7):244.
Deng Y, Zhong G, Wang Y, Wang N, Yu Q, Yu X. Quality by design approach for the preparation of fat-soluble vitamins lipid injectable emulsion. Int J Pharm. 2019;571:118717.
Denkinger CM, Dolinger D, Schito M, Wells W, Cobelens F, Pai M, et al. Target Product Profile of a Molecular Drug-Susceptibility Test for Use in Microscopy centers. J Infect Dis. 2015;211(suppl2):S39–49.
Dittrich S, Tadesse BT, Moussy F, Chua A, Zorzet A, Tängdén T, et al. Target Product Profile for a diagnostic assay to differentiate between bacterial and non-bacterial infections and reduce antimicrobial overuse in Resource-Limited settings: an Expert Consensus. PLoS ONE. 2016;11(8):e0161721.
Dormenval C, Lokras A, Cano-Garcia G, Wadhwa A, Thanki K, Rose F, et al. Identification of factors of importance for spray drying of small interfering RNA-Loaded lipidoid-polymer hybrid nanoparticles for inhalation. Pharm Res. 2019;36(10):142.
Fongwen N, Wilder-Smith A, Gubler DJ, Ooi EE, Salvana T, De Lamballerie EM. Target product profile for a dengue pre-vaccination screening test. PLoS Negl Trop Dis. 2021;15(7):e0009557.
Funk CD, Laferrière C, Ardakani A. A snapshot of the global race for vaccines targeting SARS-CoV-2 and the COVID-19 pandemic. Front Pharmacol. 2020;11:937.
Gal M, Francis NA, Hood K, Villacian J, Goossens H, Watkins A, et al. Matching diagnostics development to clinical need: target product profile development for a point of care test for community-acquired lower respiratory tract infection. PLoS ONE. 2018;13(8):e0200531.
García-Basteiro AL, DiNardo A, Saavedra B, Silva DR, Palmero D, Gegia M, et al. Point of care diagnostics for tuberculosis. Pulmonology. 2018;24(2):73–85.
Garg B, Katare OP, Beg S, Lohan S, Singh B. Systematic development of solid self-nanoemulsifying oily formulations (S-SNEOFs) for enhancing the oral bioavailability and intestinal lymphatic uptake of lopinavir. Colloids Surf B. 2016;141:611–22.
Garg S, Tambwekar KR, Vermani K, Kandarapu R, Garg A, Waller DP, et al. Development Pharmaceutics of Microbicide formulations. Part II: formulation, evaluation, and challenges. AIDS Patient Care STDs. 2003;17(8):377–99.
Gavan A, Porfire A, Marina C, Tomuta I. Formulation and pharmaceutical development of quetiapine fumarate sustained release matrix tablets using a QbD approach. Acta Pharm. 2017;67(1):53–70.
Ghaffari A, Meurant R, Ardakani A. COVID-19 point-of-Care Diagnostics that Satisfy Global Target Product profiles. Diagnostics. 2021;11(1):115.
Gurumukhi VC, Bari SB. Quality by design (QbD)–based fabrication of atazanavir-loaded nanostructured lipid carriers for lymph targeting: bioavailability enhancement using chylomicron flow block model and toxicity studies. Drug Deliv Transl Res. 2022;12(5):1230–52.
Gurumukhi VC, Bari SB. Development of ritonavir-loaded nanostructured lipid carriers employing quality by design (QbD) as a tool: characterizations, permeability, and bioavailability studies. Drug Deliv Transl Res. 2022;12(7):1753–73.
Ha J-M, Seo J-W, Kim S-H, Kim J-Y, Park C-W, Rhee Y-S, et al. Implementation of quality by design for Formulation of Rebamipide Gastro-retentive tablet. AAPS PharmSciTech. 2017;18(8):3129–39.
Hales D, Vlase L, Porav SA, Bodoki A, Barbu-Tudoran L, Achim M, et al. A quality by design (QbD) study on enoxaparin sodium loaded polymeric microspheres for colon-specific delivery. Eur J Pharm Sci. 2017;100:249–61.
Hastings IM, Hodel EM. Pharmacological considerations in the design of anti-malarial drug combination therapies – is matching half-lives enough? Malar J. 2014;13(1):62.
Heal DJ, Smith SL. Prospects for new drugs to treat binge-eating disorder: insights from psychopathology and neuropharmacology. J Psychopharmacol. 2022;36(6):680–703.
Hernandez-Morales I, Van Loock M. An industry perspective on Dengue Drug Discovery and Development. In: Hilgenfeld R, Vasudevan SG, editors. Dengue and Zika: control and antiviral treatment strategies. Volume 1062. Singapore: Springer Singapore; 2018. pp. 333–53.
Huston CD, Spangenberg T, Burrows J, Willis P, Wells TNC, Van Voorhis W. A proposed Target Product Profile and Developmental Cascade for New Cryptosporidiosis treatments. PLoS Negl Trop Dis. 2015;9(10):e0003987.
Ignjatović J, Đuriš J, Cvijić S, Dobričić V, Montepietra A, Lombardi C, et al. Development of solid lipid microparticles by melt-emulsification/spray-drying processes as carriers for pulmonary drug delivery. Eur J Pharm Sci. 2021;156:105588.
Ingvarsson PT, Yang M, Mulvad H, Nielsen HM, Rantanen J, Foged C. Engineering of an inhalable DDA/TDB liposomal adjuvant: a quality-by-design Approach towards optimization of the spray drying process. Pharm Res. 2013;30(11):2772–84.
Ivanova Reipold E, Easterbrook P, Trianni A, Panneer N, Krakower D, Ongarello S, et al. Optimising diagnosis of viraemic hepatitis C infection: the development of a target product profile. BMC Infect Dis. 2017;17(S1):707.
Jaffar-Aghaei M, Khanipour F, Maghsoudi A, Sarvestani R, Mohammadian M, Maleki M, et al. QbD-guided pharmaceutical development of Pembrolizumab biosimilar candidate PSG-024 propelled to industry meeting primary requirements of comparability to Keytruda®. Eur J Pharm Sci. 2022;173:106171.
Jambulingam T. The R&D Marketing Interface in Biopharma and MedTech. JCB. 2019;24(4).
Javed MN, Kohli K, Amin S. Risk Assessment Integrated QbD Approach for Development of Optimized Bicontinuous Mucoadhesive Limicubes for oral delivery of Rosuvastatin. AAPS PharmSciTech. 2018;19(3):1377–91.
Joshi M, Yadav KS, Prabhakar B. Quality by Design Approach for Development and Optimization of Rifampicin Loaded Bovine Serum Albumin Nanoparticles and characterization. CDD. 2021;18(9):1338–51.
Kadam R, White W, Banks N, Katz Z, Dittrich S, Kelly-Cirino C. Target Product Profile for a mobile app to read rapid diagnostic tests to strengthen infectious disease surveillance. PLoS ONE. 2020;15(1):e0228311.
Kakade P, Gite S, Patravale V. Development of Atovaquone Nanosuspension: quality by Design Approach. CDD. 2020;17(2):112–25.
Kraan H, Van Der Stel W, Kersten G, Amorij J-P. Alternative administration routes and delivery technologies for polio vaccines. Expert Rev Vaccines. 2016;15(8):1029–40.
Kuk D-H, Ha E-S, Ha D-H, Sim W-Y, Lee S-K, Jeong J-S, et al. Development of a Resveratrol Nanosuspension using the Antisolvent Precipitation Method without Solvent removal, based on a quality by Design (QbD) Approach. Pharmaceutics. 2019;11(12):688.
Lambert WJ. Considerations in developing a Target Product Profile for Parenteral Pharmaceutical products. AAPS PharmSciTech. 2010;11(3):1476–81.
Leng D, Thanki K, Fattal E, Foged C, Yang M. Engineering of budesonide-loaded lipid-polymer hybrid nanoparticles using a quality-by-design approach. Int J Pharm. 2018;548(2):740–6.
Lewin SR, Attoye T, Bansbach C, Doehle B, Dubé K, Dybul M, et al. Multi-stakeholder consensus on a target product profile for an HIV cure. Lancet HIV. 2021;8(1):e42–50.
Lokras A, Thakur A, Wadhwa A, Thanki K, Franzyk H, Foged C. Optimizing the intracellular delivery of therapeutic anti-inflammatory TNF-α siRNA to activated macrophages using lipidoid-polymer hybrid nanoparticles. Front Bioeng Biotechnol. 2021;8:601155.
Macintyre F, Ramachandruni H, Burrows JN, Holm R, Thomas A, Möhrle JJ, et al. Injectable anti-malarials revisited: discovery and development of new agents to protect against malaria. Malar J. 2018;17(1):402.
Malvolti S, Malhame M, Mantel CF, Le Rutte EA, Kaye PM. Human leishmaniasis vaccines: use cases, target population and potential global demand. PLoS Negl Trop Dis. 2021;15(9):e0009742.
Manjunatha UH, Chao AT, Leong FJ, Diagana TT. Cryptosporidiosis Drug Discovery: opportunities and challenges. ACS Infect Dis. 2016;2(8):530–7.
Martín-Escolano J, Medina-Carmona E, Martín-Escolano R. Chagas Disease: current view of an ancient and global chemotherapy challenge. ACS Infect Dis. 2020;6(11):2830–43.
Mateus D, Marto J, Trindade P, Gonçalves H, Salgado A, Machado P, et al. Improved morphine-loaded hydrogels for Wound-Related Pain Relief. Pharmaceutics. 2019;11(2):76.
Mather RG, Hopkins H, Parry CM, Dittrich S. Redefining typhoid diagnosis: what would an improved test need to look like? BMJ Glob Health. 2019;4(5):e001831.
Mercuri AM. Quality by Design Applied to Ocular solid lipid nanoparticles containing a hydrophilic peptide prepared via Hot High pressure Homogeniser. CDD. 2016;13(8):1247–60.
Mirani AG, Patankar SP, Kadam VJ. Risk-based approach for systematic development of gastroretentive drug delivery system. Drug Deliv Transl Res. 2016;6(5):579–96.
Mishra SM, Rohera BD. An integrated, quality by design (QbD) approach for design, development and optimization of orally disintegrating tablet formulation of carbamazepine. Pharm Dev Technol. 2017;22(7):889–903.
Mo AX, Colley DG. Workshop report: Schistosomiasis vaccine clinical development and product characteristics. Vaccine. 2016;34(8):995–1001.
Monath TP, Kortekaas J, Watts DM, Christofferson RC, Desiree LaBeaud A, Gowen BB et al. Theoretical risk of genetic reassortment should not impede development of live, attenuated Rift Valley fever (RVF) vaccines commentary on the draft WHO RVF Target Product Profile. Vaccine: X. 2020;5:100060.
Nakas A, Dalatsi AM, Kapourani A, Kontogiannopoulos KN, Assimopoulou AN, Barmpalexis P. Quality Risk Management and Quality by Design for the Development of Diclofenac Sodium Intra-articular Gelatin Microspheres. AAPS PharmSciTech. 2020;21(4):127.
Namjoshi S, Dabbaghi M, Roberts MS, Grice JE, Mohammed Y. Quality by design: development of the Quality Target Product Profile (QTPP) for Semisolid Topical products. Pharmaceutics. 2020;12(3):287.
Nazari K, Mehta P, Arshad MS, Ahmed S, Andriotis EG, Singh N, et al. Quality by Design Micro-engineering Optimisation of NSAID-Loaded Electrospun Fibrous patches. Pharmaceutics. 2019;12(1):2.
Neale G, Gaihre S, O’Gorman P, Price RK, Balzategi AG, Barrientos CH, et al. Review of recent innovations in portable child growth measurement devices for use in low- and middle-income countries. J Med Eng Technol. 2021;45(8):642–55.
Németh Z, Pallagi E, Dobó DG, Csóka I. A proposed methodology for a Risk Assessment-based Liposome Development process. Pharmaceutics. 2020;12(12):1164.
Nsanzabana C, Ariey F, Beck H-P, Ding XC, Kamau E, Krishna S, et al. Molecular assays for antimalarial drug resistance surveillance: a target product profile. PLoS ONE. 2018;13(9):e0204347.
Oh G-H, Park J-H, Shin H-W, Kim J-E, Park Y-J. Quality-by-design approach for the development of telmisartan potassium tablets. Drug Dev Ind Pharm. 2018;44(5):837–48.
Pallagi E, Ambrus R, Szabó-Révész P, Csóka I. Adaptation of the quality by design concept in early pharmaceutical development of an intranasal nanosized formulation. Int J Pharm. 2015;491(1–2):384–92.
Pallagi E, Jójárt-Laczkovich O, Németh Z, Szabó-Révész P, Csóka I. Application of the QbD-based approach in the early development of liposomes for nasal administration. Int J Pharm. 2019;562:11–22.
Patadia R, Vora C, Mittal K, Mashru RC. Quality by Design Empowered Development and Optimisation of Time-controlled pulsatile release platform Formulation employing Compression Coating Technology. AAPS PharmSciTech. 2017;18(4):1213–27.
Patel GM, Shelat PK, Lalwani AN. QbD based development of proliposome of lopinavir for improved oral bioavailability. Eur J Pharm Sci. 2017;108:50–61.
Patel HP, Chaudhari PS, Gandhi PA, Desai BV, Desai DT, Dedhiya PP, et al. Nose to brain delivery of tailored clozapine nanosuspension stabilized using (+)-alpha-tocopherol polyethylene glycol 1000 succinate: optimization and in vivo pharmacokinetic studies. Int J Pharm. 2021;600:120474.
Patel H, Patel K, Tiwari S, Pandey S, Shah S, Gohel M. Quality by Design (QbD) Approach for Development of Co-processed Excipient Pellets (MOMLETS) by extrusion-spheronization technique. DDF. 2016;10(3):192–206.
Pellé KG, Rambaud-Althaus C, D’Acremont V, Moran G, Sampath R, Katz Z, et al. Electronic clinical decision support algorithms incorporating point-of-care diagnostic tests in low-resource settings: a target product profile. BMJ Glob Health. 2020;5(2):e002067.
Peraman R, Bhadraya K, Reddy Y, Reddy C, Lokesh T. Analytical quality by design approach in RP-HPLC method development for the assay of etofenamate in dosage forms. Indian J Pharm Sci. 2015;77(6):751.
Perrier Q, Piquemal M, Leenhardt J, Choisnard L, Mazet R, Desruet M-D, et al. A quality by design approach for the qualification of automating compounding device for parenteral nutrition. Eur J Pharm Sci. 2022;179:106275.
Porrás AI, Yadon ZE, Altcheh J, Britto C, Chaves GC, Flevaud L, et al. Target Product Profile (TPP) for Chagas Disease Point-of-care diagnosis and Assessment of response to treatment. PLoS Negl Trop Dis. 2015;9(6):e0003697.
Reinhard-Rupp J, Klohe K. Developing a comprehensive response for treatment of children under 6 years of age with schistosomiasis: research and development of a pediatric formulation of praziquantel. Infect Dis Poverty. 2017;6(1):122.
Romano J, Manning J, Hemmerling A, McGrory E, Young Holt B. Prioritizing multipurpose prevention technology development and investments using a target product profile. Antiviral Res. 2013;100:S32–8.
Russell C, Hussain M, Huen D, Rahman AS, Mohammed AR. Profiling gene expression dynamics underpinning conventional testing approaches to better inform pre-clinical evaluation of an age appropriate spironolactone formulation. Pharm Dev Technol. 2021;26(1):101–9.
Salami K, Gsell P-S, Olayinka A, Maiga D, Formenty P, Smith PG, et al. Meeting report: WHO consultation on accelerating Lassa fever vaccine development in endemic countries, Dakar, 10–11 September 2019. Vaccine. 2020;38(26):4135–41.
Saydam M, Takka S. Development and < i > in vitro evaluation of pH-independent release matrix tablet of weakly acidic drug valsartan using quality by design tools. Drug Dev Ind Pharm. 2018;44(12):1905–17.
Simões A, Veiga F, Figueiras A, Vitorino C. A practical framework for implementing quality by design to the development of topical drug products: Nanosystem-based dosage forms. Int J Pharm. 2018;548(1):385–99.
Simões A, Veiga F, Vitorino C, Figueiras A. A Tutorial for developing a topical cream formulation based on the quality by Design Approach. J Pharm Sci. 2018;107(10):2653–62.
Singh B, Kaur A, Dhiman S, Garg B, Khurana RK, Beg S. QbD-Enabled development of Novel Stimuli-Responsive Gastroretentive systems of Acyclovir for Improved Patient Compliance and Biopharmaceutical Performance. AAPS PharmSciTech. 2016;17(2):454–65.
Staunton KM, Liu J, Townsend M, Desnoyer M, Howell P, Crawford JE, et al. Designing Aedes (Diptera: Culicidae) Mosquito traps: the evolution of the male Aedes sound trap by iterative evaluation. Insects. 2021;12(5):388.
Swindells S, Siccardi M, Barrett SE, Olsen DB, Grobler JA, Podany AT, et al. Long-acting formulations for the treatment of latent tuberculous infection: opportunities and challenges. int j Tuberc lung dis. 2018;22(2):125–32.
Sylvester B, Tefas L, Vlase L, Tomuţă I, Porfire A. A quality by design (QbD) approach to the development of a gradient high-performance liquid chromatography for the simultaneous assay of curcuminoids and doxorubicin from long-circulating liposomes. J Pharm Biomed Anal. 2018;158:395–404.
Taipale-Kovalainen K, Karttunen A-P, Ketolainen J, Korhonen O. Lubricant based determination of design space for continuously manufactured high dose Paracetamol tablets. Eur J Pharm Sci. 2018;115:1–10.
Tanaka T, Hanaoka H, Sakurai S. Optimization of the quality by design approach for gene therapy products: a case study for adeno-associated viral vectors. Eur J Pharm Biopharm. 2020;155:88–102.
Thakkar R, Ashour EA, Shukla A, Wang R, Chambliss WG, Bandari S, et al. A comparison between lab-scale and hot-melt-extruder-based anti-inflammatory Ointment Manufacturing. AAPS PharmSciTech. 2020;21(5):200.
Thanki K, Papai S, Lokras A, Rose F, Falkenberg E, Franzyk H, et al. Application of a Quality-By-Design Approach to optimise lipid-polymer hybrid nanoparticles loaded with a splice-correction antisense oligonucleotide: Maximising Loading and Intracellular Delivery. Pharm Res. 2019;36(3):37.
Thanki K, Zeng X, Justesen S, Tejlmann S, Falkenberg E, Van Driessche E, et al. Engineering of small interfering RNA-loaded lipidoid-poly(DL -lactic-co-glycolic acid) hybrid nanoparticles for highly efficient and safe gene silencing: a quality by design-based approach. Eur J Pharm Biopharm. 2017;120:22–33.
The mal ERACGoV. A Research Agenda for Malaria Eradication: vaccines. PLoS Med. 2011;8(1):e1000398.
Timpe C, Stegemann S, Barrett A, Mujumdar S. Challenges and opportunities to include patient-centric product design in industrial medicines development to improve therapeutic goals. Brit J Clin Pharma. 2020;86(10):2020–7.
Torregrosa A, Ochoa-Andrade AT, Parente ME, Vidarte A, Guarinoni G, Savio E. Development of an emulgel for the treatment of rosacea using quality by design approach. Drug Dev Ind Pharm. 2020;46(2):296–308.
Vetter B, Beran D, Boulle P, Chua A, De La Tour R, Hattingh L, et al. Development of a target product profile for a point-of-care cardiometabolic device. BMC Cardiovasc Disord. 2021;21(1):486.
Villamagna AH, Gore SJ, Lewis JS, Doggett JS. The need for antiviral drugs for pandemic coronaviruses from a Global Health Perspective. Front Med. 2020;7:596587.
Vitoria M, Rangaraj A, Ford N, Doherty M. Current and future priorities for the development of optimal HIV drugs. Curr Opin HIV AIDS. 2019;14(2):143–9.
Vliegenthart ADB, Antoine DJ, Dear JW. Target biomarker profile for the clinical management of Paracetamol overdose. Brit J Clin Pharma. 2015;80(3):351–62.
Vora C, Patadia R, Mittal K, Mashru R. Risk based approach for design and optimization of stomach specific delivery of rifampicin. Int J Pharm. 2013;455(1–2):169–81.
Waghule T, Dabholkar N, Gorantla S, Rapalli VK, Saha RN, Singhvi G. Quality by design (QbD) in the formulation and optimization of liquid crystalline nanoparticles (LCNPs): a risk based industrial approach. Biomed Pharmacother. 2021;141:111940.
Walsh J, Masini T, Huttner B, Moja L, Penazzato M, Cappello B. Assessing the appropriateness of formulations on the WHO Model list of essential Medicines for children: Development of a Paediatric Quality Target Product Profile Tool. Pharmaceutics. 2022;14(3):473.
Walsh J, Schaufelberger D, Iurian S, Klein S, Batchelor H, Turner R, et al. Path towards efficient paediatric formulation development based on partnering with clinical pharmacologists and clinicians, a conect4children expert group white paper. Brit J Clin Pharma. 2022;88(12):5034–51.
Wang Y, Müllertz A, Rantanen J. Structured approach for designing drug-loaded solid products by binder jetting 3D printing. Eur J Pharm Sci. 2022;178:106280.
Wyber R, Boyd BJ, Colquhoun S, Currie BJ, Engel M, Kado J, et al. Preliminary consultation on preferred product characteristics of benzathine penicillin G for secondary prophylaxis of rheumatic fever. Drug Deliv Transl Res. 2016;6(5):572–8.
Zhang E, Xie L, Qin P, Lu L, Xu Y, Gao W, et al. Quality by design–based Assessment for Analytical Similarity of Adalimumab Biosimilar HLX03 to Humira®. AAPS J. 2020;22(3):69.
Zidan A, Ahmed O, Aljaeid B. Nicotinamide polymeric nanoemulsified systems: a quality-by-design case study for a sustained antimicrobial activity. IJN. 2016:1501.
guideline IQRPd-S. International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use.
FIND. Target product profiles. https://www.finddx.org/tools-and-resources/rd-and-innovation/target-product-profiles/.
Organization WH. Global status report on the public health response to dementia. 2021.
Organization WH. An R&D blueprint for action to prevent epidemics. Plan Action. 2016.
Organization WH. A blueprint for dementia research. Geneva: World Health Organization; 2022.
Mahant V. Translational medicines ecosystem. J Translational Med. 2020;18(1):158.
Charnaud SCMV, Reeder J, Ross AL. WHO target product profiles to shape global research and development. Bull World Health Organ. 2023;101(5):326–30.
Acknowledgements
The authors acknowledge the contribution of Sjak Bott for providing useful information about the method. The part of the work performed under the EPND project has received funding from the Innovative Medicines Initiative 2 (www.imi.europa.eu) Joint Undertaking under grant agreement No 101034344. This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by DZNE (Deutsches Zentrum für Neurodegenerative Erkrankungen) and the EU/EFPIA Innovative Medicines Initiative Joint Undertaking (EPND, grant No 101034344).
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MB and AGa conceived the study. AI contributed to the data collection (screened abstracts and full-texts, extracted the data items, visualised results) and to the first draft of the manuscript. NL performed the random check on the abstract and full-text screening. MB and AI performed the interviews with experts and conceptualised the findings. AGa contributed information about the concept and use of TPPs in industry. AGu, JS, MG, and MR provided general information and know-how about TPPs in industry. EE worked at the revision of the paper after peer review. All authors contributed to the manuscript writing and approved the final submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. No ethics approval was required to conduct this review.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ibnidris, A., Liaskos, N., Eldem, E. et al. Facilitating the use of the target product profile in academic research: a systematic review. J Transl Med 22, 693 (2024). https://doi.org/10.1186/s12967-024-05476-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-024-05476-1