Abstract
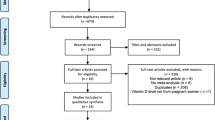
Docosahexaenoic acid (DHA) supplementation is recommended for women during pregnancy because of its neurological, visual, and cognitive effects. Previous studies have suggested that DHA supplementation during pregnancy may prevent and treat certain pregnancy complications. However, there are contradictions in the current related studies, and the specific mechanism by which DHA acts remains unclear. This review summarizes the research on the relationship between DHA intake during pregnancy and preeclampsia, gestational diabetes mellitus, preterm birth, intrauterine growth restriction, and postpartum depression. Furthermore, we explore the impact of DHA intake during pregnancy on the prediction, prevention, and treatment of pregnancy complications as well as its impact on offspring neurodevelopment. Our results suggest that there is limited and controversial evidence for the protective effect of DHA intake on pregnancy complications, with the exception of preterm birth and gestational diabetes mellitus. However, additional DHA supplementation may improve long-term neurodevelopmental outcomes in the offspring of women with pregnancy complications.
Similar content being viewed by others
Introduction
Today, the world is experiencing a demographic transition towards long-term subreplacement fertility [1]. The low fertility rate is undoubtedly an important reason for the rapidly aging worldwide population [2], and this aging brings along a series of complex social problems [3]. Some countries have implemented policies to encourage childbearing, but these policies have resulted in an increase in advanced maternal age and the resultant high risk of pregnancy complications [4]. Therefore, increased attention to perinatal care, reduction in pregnancy complications, and improvement in adverse neonatal outcomes are the current goals of obstetricians and are essential for promoting social health and economic development.
To maintain normal physiological health, the body must intake various nutritional elements from food, especially glucose, fat and protein. Fat is the second-largest source of dietary energy for human beings [5], and fatty acids (FAs), which are obtained through the metabolism of fat, not only serve as energy sources but also play an important role in maintaining normal cellular physiology. Deficiencies or abnormal increases in FAs are associated with cardiovascular and neurodevelopmental diseases [6]. N-3 long-chain polyunsaturated fatty acids (n-3 PUFAs) are believed to play a central role in brain function and neuronal membrane structure, and are also necessary for the development of the myelin sheath and retina [7]. Approximately 90% of n-3 PUFAs in the brain are composed of docosahexaenoic acid (DHA) [8], suggesting the importance of DHA in maintaining brain function. In recent years, increasing epidemiological and clinical evidence has proven the preventive or therapeutic effects of DHA in Alzheimer’s disease [9], attention deficit and hyperactivity disorder [10], breast cancer [11], coronary heart disease [12] and some other diseases.
The importance of DHA is evident early in life. DHA is rapidly integrated into retinal and brain neural tissue during the last three months of pregnancy [13] and plays a significant role in early fetal neurodevelopment. Remarkably, the fetus and placenta rarely synthesize DHA autonomously [14]. Therefore, maternal DHA intake and placental transport function are critical for fetal DHA acquisition [15]. However, in some pregnancy complications, low maternal DHA levels [16, 17] or dysfunction in placental fatty acid transport [18, 19] leads to DHA deficiency in the offspring, which may lead to long-term neurological disorders. Thus, women with pregnancy complications may benefit from DHA supplementation. Additionally, healthy pregnant women and fetuses may also benefit from DHA supplementation due to its potential effects on neurodevelopment and its preventive effect on a variety of diseases [20]. However, there remain contradictions in the current relevant clinical studies. For example, Colombo et al. found that prenatal DHA may positively affect infants’ attention and regulation [21], whereas Gould et al. observed no benefit of prenatal DHA supplementation on child behavior; on the contrary, the results of Gould et al. suggest an adverse effect of DHA on behavioral functioning [22]. Clarifying the mechanism of action of DHA can help guide supplementation during pregnancy [23].
This review summarizes the research on the relationship between DHA intake during pregnancy and five common pregnancy complications: preeclampsia (PE), gestational diabetes mellitus (GDM), preterm birth (PT), intrauterine growth restriction (IUGR), and postpartum depression (PPD). Additionally, we discuss the impact of DHA intake during pregnancy on the prediction, prevention and treatment of the aforementioned pregnancy complications. Furthermore, we explore the role of DHA in offspring neurodevelopment. Finally, because DHA is the most important n-3 PUFA, this review also summarizes the relationship between n-3 PUFAs and the aforementioned pregnancy complications.
Preeclampsia (PE)
Maternal plasma DHA levels are significantly altered in patients with PE. Dangat et al. collected peripheral blood from PE patients (n = 45) and normal pregnant women (n = 85) at the time of delivery and found that maternal plasma DHA concentrations were significantly reduced in PE patients [16], and similar results were reported in other studies [17]. In addition, women with the lowest n-3 PUFA levels in red blood cells were 7.6 times more prone to suffer from PE than those with the highest levels [24], but this conclusion may be confounded by causality. In fact, the decrease in plasma DHA levels in PE patients does not occur until the third trimester. A cross-sectional study suggested that the decrease in DHA in PE patients was already present at 16–20 weeks of gestation [18]. These results suggest that early maternal DHA levels may be potentially predictive of PE.
Previous studies have not found any difference in seafood intake between PE patients and normal pregnant women, suggesting that the decrease in plasma DHA content in PE patients is not caused by the decrease in maternal dietary intake. Mackay et al. proposed that the metabolic pattern of PE patients includes high nonesterified fatty acid (NEFA) concentrations [25]. Increased NEFA flux is associated with mitochondrial dysfunction and may cause ectopic lipid accumulation in the liver and other tissues, which interferes with PUFA synthesis [26]. Another explanation for the decrease in plasma DHA content in PE patients is oxidative stress in the placenta [27]. Reactive oxygen species attack the double bonds of PUFAs and initiate a chain reaction leading to the formation of lipid peroxides. There is a deficiency of antioxidants in PE, and the increased peroxidative reactions further promote the decomposition of PUFAs. Notably, Roy et al. found that maternal plasma DHA levels were lower in PE women who gave birth to male infants than in normal control pregnant women who gave birth to male infants, but this same relationship was not observed between PE and normal pregnant women who gave birth to female infants [28]. Taken together with in utero exposure to PE as an environmental risk factor for various neurodevelopmental disorders [29] and the role of DHA in neurodevelopment, this result suggests that male infants born to mothers with PE may be at higher risk for neurodevelopmental disorders than female infants.
In addition to maternal plasma, the DHA content in the cord blood of PE patients is also lower than that of normal pregnant women [18, 25, 30]. The decrease in cord blood DHA levels may be due to the following three reasons: (1) PE patients are in a low PUFA environment, which leads to a decrease in maternal plasma DHA content and a subsequent decrease in cord blood DHA content. (2) Increased oxidative stress in the placental tissues of patients with PE may lead to peroxidation of cord blood lipids. In addition, oxidative stress can also lead to the dysregulation of angiogenic factors, resulting in an increase in sFlt-1, which by itself has been shown to induce oxidative stress, leading to further decreases in the level of DHA in cord blood [30]. (3) Placental tissues of PE patients have been confirmed to have decreased mRNA levels of Δ5 desaturase and fatty acid transport protein 1/4 (FATP1/4) [18]. Unfortunately, Δ5 and Δ6 desaturases are the rate-limiting enzymes for PUFA conversion and are recognized as the primary determinants of PUFA levels, and the transport of DHA from mother to offspring is primarily carried out by FATP1/4 [31]. The decreased expression of FATP1/4 is a sign of impaired fatty acid transport in the placenta and a possible cause of decreased DHA content in cord blood. (4) Lipidomic analysis of placentas from patients with preeclampsia reveals higher lipid content than placentas from healthy patients [32]. Although the mechanism remains unclear, the presence of ectopic fat in the placenta suggests that DHA becomes trapped in the placenta and is not transferred to the fetus; thus, the amount of DHA in cord blood is low. The fatty acid transport family primarily includes fatty acid transport proteins (FATPs), fatty acid-binding proteins (FABPs) and fatty acid translocases (FAT/CD36) [33]. In human placental tissue, FABPs are predominantly located on the maternal-facing placental membranes, whereas FATPs and FAT are distributed across both maternal and fetal membranes [34]. FABP4 is essential for trophoblast lipid accumulation. Inhibition of FABP4 expression in primary human trophoblasts blocked their uptake of exogenous fatty acids [35]. In addition, Biron-Shental et al. found that human primary trophoblasts exhibited increased expression of FABP1, FABP3 and FABP4 under inflammatory and hypoxic conditions [36], and FABP4 expression was increased in both the serum and placenta of PE patients [37, 38]. Increased expression of FABPs located on the maternal surface and decreased expression of FATPs, which are primarily responsible for the transport of free fatty acids to the fetus, may be the cause of placental ectopic fat in patients with eclampsia. These results suggest that alterations in polyunsaturated fatty acid metabolism and transport in different regions of the preeclamptic placenta may contribute to the pathological features of preeclampsia.
However, the decrease in cord blood DHA levels due to these three potential causes appears to be partially ameliorated by DHA supplementation during pregnancy. First, the low maternal plasma level of DHA in PE patients can be improved by exogenous DHA supplementation. Second, DHA can exert antioxidant effects by promoting mitochondrial function and biogenesis [39], which is speculated to antagonize oxidative stress in PE patients. Third, FATPs and FABPs are regulated by peroxisome proliferator-activated receptor γ (PPAR-γ) [40], whose natural ligand is primarily derived from dietary n-3 PUFAs, with DHA being the main component [41]. Therefore, DHA is expected to ameliorate the decreased expression of FATP1 and FATP4 in placental tissues of PE patients through the PPAR-γ pathway, subsequently promoting DHA transport, forming a process similar to “positive feedback” mechanism (Fig. 1). However, most of the current studies are observational studies, and no study has investigated the effects of DHA supplementation in PE patients on cord blood DHA content and long-term neurodevelopment in offspring. Future studies could use this as an entry point to explore the clinical value of DHA supplementation.
Interestingly, despite the decrease in maternal plasma DHA content in PE patients, the postpartum DHA content in breast milk increases [16, 42]. It is possible that when global PUFA levels are low in PE patients, there are adaptive mechanisms in the mammary gland to synthesize PUFAs by increasing sterol regulatory element binding proteins (SREBP-1), and the increase in SREBP-1 expression may ameliorate the expression of Δ5 and Δ6 desaturase [43]. This study seems to provide guidance for breastfeeding in PE patients. However, because there are few studies on this topic, further mechanistic studies and animal models are needed to explore the clinical significance.
A large number of epidemiological studies support the positive effects of n-3 PUFAs on cardiovascular events, including hypertension [44], which may be attributed to the antioxidant effect of n-3 PUFAs. The n-3 PUFAs can improve vascular endothelial function and antagonize the proinflammatory response in hypertension [45]. Meanwhile, n-3 PUFAs have also been shown to possess vasodilator effects [46]. Similar to hypertension patients, PE patients exhibit pathologic oxidative stress, inflammation and vasoconstriction. Therefore, n-3 PUFAs are also expected to improve the symptoms of PE patients. However, studies have reported conflicting results. A Cochrane study reported that PE may be reduced with omega-3 LCPUFAs (RR 0.84, 95% CI 0.69–1.01; 20 trials, 8306 participants; low-quality evidence) [47], whereas another RCT suggested that DHA supplementation of 800 mg/d in the second half of pregnancy does not reduce the risk of PE [48]. In contrast, Li et al. found that maternal DHA intake was inversely associated with the risk of PE, and dietary n-3 PUFA intake may protect pregnant women from the development of PE [49]. A Danish cohort study involving 65,220 pregnant women with singleton pregnancies suggested that although EPA + DHA 250 mg/d did not improve the overall risk of PE, supplementation reduced the risk of severe preeclampsia (RR = 0.77, 95% CI 0.60–0.99) [50]. In view of the current controversy about the risk and therapeutic effect of DHA on PE in pregnant women, we look forward to more large-scale RCTs on maternal DHA intake and PE risk to provide guidance on maternal DHA supplementation. Current studies primarily focus on whether the use of DHA in normal pregnant women can prevent PE and whether DHA supplementation in PE patients can improve abnormal blood pressure. Few studies have focused on the relationship between DHA supplementation in PE patients and long-term neurodevelopment in offspring. Future research could focus on this relationship.
In conclusion, PE patients exhibit lower plasma DHA concentrations, which have been observed as early as 16–20 weeks of gestation. Low plasma DHA levels, placental oxidative stress, the absence of fatty acid transporters, and ectopic fat in the placenta are potential reasons for the reduction in cord blood DHA concentrations in PE offspring. Whether supplementation with DHA during pregnancy can improve the reduction in cord blood DHA in eclamptic patients and the neurodevelopment of the offspring remains largely unknown and necessitates future research.
Gestational diabetes mellitus (GDM)
In contrast to the decrease in maternal plasma DHA levels in PE patients, a cross-sectional study suggested that GDM did not affect the activities of Δ5 and Δ6 desaturases, and maternal plasma DHA levels were not decreased when GDM was diagnosed in the second trimester [51]. In a meta-analysis of 24 observational studies, plasma DHA levels were even elevated in GDM patients [52]. However, a high maternal DHA environment did not increase the DHA content in cord blood. Léveillé et al. did not identify any difference in DHA levels in cord blood between GDM patients and normal pregnant women [53], and even in most studies, DHA levels in the cord blood of GDM patients were found to be significantly lower than those of pregnant women with normal blood glucose [52, 54]. These results suggest that the ability of the GDM placenta to transport n-3 PUFAs like DHA is decreased.
Gázquez et al. found that DHA supplementation during pregnancy in normal pregnant women increased both maternal DHA levels and cord blood DHA levels simultaneously, but DHA supplementation in GDM mothers did not improve cord blood DHA levels [55, 56]. Studies of fatty acid placental transfer in vivo using stable isotope tracers have also confirmed the impairment of fatty acid transport in GDM placentas [19]. Previous studies have found that the expression of FATP1, FATP4, the Major Family Super Domain 2a (MFSD2a) and endothelial lipase in placental tissues of GDM patients is significantly decreased [57, 58], resulting in placental fatty acid transport disorders. MFSD2a is associated with the selective transportation of DHA as lysophospholipids. The expression of the DHA membrane transporter MFSD2a is lower in GDM placentas, which could affect maternal-fetal DHA transport. Therefore, the level of MFSD2a in the maternal blood of GDM mothers could be used as a potential biomarker for the early detection of disturbances in MFSD2a expression during pregnancy and the subsequent consequences on offspring neurodevelopment [57]. The fatty acid transport disorder in GDM placental tissue may be caused by environmental stimulation of high glucose and insulin resistance [59]. When GDM patients exhibit good blood glucose control, cord blood DHA levels are positively correlated with maternal DHA levels [60]. This result also explains why Léveillé et al. did not observe a reduction in DHA levels in the cord blood of GDM patients; the case group selected in this study was GDM patients with good blood glucose control by diet or insulin [53]. Therefore, controlling blood glucose levels through diet, exercise, and medications in GDM patients may facilitate placental fatty acid transport.
Decreased cord blood DHA levels in GDM patients may lead to decreased plasma DHA levels in GDM newborns [61, 62], and this result has been shown to affect neurodevelopment at 6 months after birth [63]. Because previous studies suggest that additional DHA supplementation did not significantly increase the DHA levels in cord blood [55, 56], how to improve GDM placental fatty acid transport disorders has become the focus of preventing neurodevelopmental disorders in GDM offspring. As mentioned previously, improving blood glucose by diet, exercise or medication may help restore normal fatty acid transport in the placenta. In addition, similar to the reduced expression of FATP1 and FATP4 in the placenta of PE patients, DHA is also expected to improve FATP1 and FATP4 expression and promote fatty acid transport through the PPAR-γ pathway in GDM (Fig. 1). Although DHA supplementation at 600 mg/d during pregnancy in GDM patients did not improve the status of fetal DHA [56], this dose was within the physiological recommended intake range, and the effects of higher doses of DHA supplementation on placental fatty acid transport function and umbilical cord blood DHA content cannot be determined. Given that n-3 PUFAs have been used at a dose of 2.4 g/d in overweight school-age children with metabolic syndrome [64] and have not been associated with adverse pregnancy outcomes including excessive weight gain in overweight pregnant women [65], future studies should evaluate the effect of higher doses of n-3 PUFAs on cord blood DHA levels in GDM patients under conditions of safety.
DHA levels in vivo are negatively correlated with several markers of insulin resistance [66]. Animal models have suggested that n-3 PUFAs may reduce the secretion of inflammatory cytokines and reverse glucose intolerance [67, 68]. Meanwhile, n-3 PUFAs can also improve pancreatic fatty infiltration in the offspring of GDM mice [69]. Therefore, DHA may also have some preventive and therapeutic effects on GDM. However, RCTs and cohort studies have demonstrated that supplementation of DHA-rich fish oil during pregnancy did not prevent the development of GDM in normal pregnant women [48, 66, 70], but pregnant women who have been diagnosed with GDM can reduce the levels of blood glucose, blood lipids, high-sensitivity C-reactive protein and insulin resistance by intake of cod liver oil [71]. Combined supplementation of vitamin D and n-3 PUFAs for 6 weeks in GDM patients has also been shown to have beneficial effects on fasting blood glucose, serum triglycerides, very low-density lipoprotein cholesterol, and insulin-related indicators [72]. Therefore, DHA plays a more therapeutic role than a preventive role in GDM patients. Patients with GDM during pregnancy may benefit from DHA supplementation, and DHA supplementation can be considered in the management of GDM patients during pregnancy. The clinical benefits of this initiative, such as whether it can control blood glucose levels in GDM patients and improve neurodevelopment in GDM offspring, remain to be evaluated in large-scale clinical trials.
In summary, although the plasma DHA level of GDM patients is unchanged or even increased, the umbilical cord blood DHA level is significantly decreased. These results suggest that placental transport dysfunction in GDM, which has been verified in many other studies, may be the primary cause of reduced DHA uptake in GDM offspring. High-dose DHA may improve the reduction in cord blood DHA in GDM patients. In addition, according to existing studies, although DHA supplementation during pregnancy does not seem to prevent GDM, pregnant women with GDM may benefit from DHA supplementation during pregnancy.
Preterm birth (PT)
A case‒control design nested in the Danish National Birth Cohort measured the percentage of plasma DHA + EPA in total fatty acids at 9 and 25 weeks of gestation in 376 pregnant women with early preterm birth (< 34 weeks, ePT) and 348 pregnant women with term pregnancy [73]. Compared with women with DHA + EPA concentrations ≥ 1.8%, women with concentrations < 1.6% had a 10.27-fold increased risk of ePT. This result suggests that low plasma DHA and EPA concentrations during pregnancy may be a strong risk factor for preterm birth. A cross-sectional study in 2021 also suggested that the plasma DHA levels of PT pregnant women at delivery were significantly lower than those of full-term pregnant women [17]. However, this study did not compare the plasma DHA levels of PT pregnant women at delivery with the plasma DHA levels of full-term pregnant women at the corresponding gestational weeks, and there is no study to dynamically monitor the changes in plasma DHA levels of pregnant women throughout the whole pregnancy, so it is not possible to confirm whether the results are caused by different gestational weeks. In general, the low plasma DHA levels during pregnancy seem suggestive of a relationship with PT [74], and some scholars have advocated monitoring the plasma concentration of DHA + EPA during pregnancy to predict PT [75].
The mechanism by which DHA levels contribute to PT remains unclear, although several have been suggested: (1) The initiation of labor is associated with increased expression of uterotonic proteins, activation of specific ion channels, and increased connexin 43 [76]. These factors promote electrical synchronization and coordination of contractions in the myometrium. Upon activation of contractile protein receptors, the uterus can be stimulated to contract by oxytocin and the stimulatory prostaglandins E2 and F2α. As one of the n-3 PUFAs, the physical properties of the lipid membrane of DHA may affect the activity of contractile protein receptors [77]. In addition, DHA regulates connexin 43 expression [78] and reduces PGE2 and F2α levels [79]. (2) The infiltration of white blood cells and the release of cytokines are the triggers for the initiation of labor, and this maternal inflammatory response provides a protective effect for mother and baby [80, 81]. However, abnormal inflammation is considered the cause of PT [82], and DHA can reduce inflammation by regulating the interaction between ligands and receptors on the cell surface [83]. The lack of DHA in the third trimester of pregnancy may lead to abnormal activation of the inflammatory response and subsequent PT. This theory has been supported by clinical studies in which DHA supplementation during pregnancy contributes to the prolongation of gestational age [84]. (3) Defective deep placentation, a failure of invasion and transformation of the spiral arteries by the trophoblast, may cause uteroplacental ischemia, which is one of the causes of PT [85]. Studies of fatty acids on trophoblast cells have demonstrated that DHA has a proangiogenic effect, stimulating the production of proangiogenic factors [86] and improving the development of capillary buds [87]. Therefore, DHA may reduce the incidence of preterm birth by improving deep placental dysfunction.
Considering the above three reasons, it is speculated that DHA supplementation during pregnancy is a potential way to prevent PT. In 2018, the Cochrane study included 70 RCTs to analyze the association between n-3 PUFA supplementation during pregnancy and pregnancy outcomes, and found that pregnant women with n-3 PUFA supplementation during pregnancy exhibited reduced incidences of PT and ePT compared with those without DHA supplementation [47]. Three RCTs since 2018 have also suggested that DHA supplementation during pregnancy can reduce the risk of PT [88,89,90]. Among them, Carlson et al. found that daily supplementation with 1000 mg DHA was more effective in preventing ePT than daily supplementation with 200 mg DHA, and the effect was more significant in pregnant women with low baseline DHA levels [89]. Although these studies suggest the preventive significance of DHA supplementation during pregnancy for PT, further studies are needed to explore the relationship between maternal DHA levels and appropriate DHA intake; women with higher n-3 PUFA levels content have a lower risk of PT, and it is possible that additional supplementation with n-3 PUFAs may actually increase the risk of PT [91].
Moreover, the accumulation of fetal n-3 PUFAs primarily occurs during the last trimester of pregnancy [92], with the efficiency of n-3 PUFA transport from mother to fetus reaching a peak of 42–75 mg/d at 35–40 weeks of gestation [93]. Due to the early end of this period, preterm infants are especially prone to lack DHA in the critical window period of neurodevelopment [94], which is more likely to cause adverse outcomes, including long-term neurodevelopmental disorders in ePT [95]. Therefore, it is important and difficult to improve the low n-3 PUFA status of preterm infants. Human milk is the preferred source of nutrition for premature infants when they are able to receive enteral feeding, but the DHA content in breast milk is generally low due to the changes in modern dietary structure and the decrease in fish consumption [94, 96]. Adding to the problem, Vizzari et al. found that DHA content in breast milk appears to be related to gestational age, with breastmilk from preterm women having lower DHA content than that from full-term women [97]. These studies suggest that preterm infants who do not absorb enough DHA in the third trimester may benefit from DHA supplementation of the infants and their nursing mothers. Therefore, many scholars have advocated increasing the content of DHA in formula milk powder or food for preterm infants [97,98,99]. However, there is significant heterogeneity in related studies on this topic, and whether preterm infants can benefit from DHA supplementation is still inconclusive. Regarding offspring neurodevelopment, Hewawasam et al. found that DHA supplementation in preterm infants did not improve the attention of the offspring at 18 months [100], and the Cochrane analysis of the relationship between preterm infants and fatty acid supplementation did not find long-term benefits or harms in preterm infants receiving n-3 PUFA formula milk powder [101]. However, the study by Westerberg et al. suggested that early DHA supplementation in very low birth weight newborns had a positive effect on the attention ability of offspring at 20 months of age [102]. Moreover, DHA supplementation in preterm infants may reduce the risk of hay fever [103], necrotizing enterocolitis [104], and intraventricular hemorrhage [105].
In general, low plasma DHA levels during pregnancy seem to be suggestive of PT risk, and DHA supplementation during pregnancy has a preventive effect on PT and ePT. Premature infants have insufficient intake of DHA due to the early termination of pregnancy. There is considerable controversy regarding whether preterm infants benefit from postnatal DHA supplementation. RCTs with large sample sizes are needed to determine the clinical significance of DHA supplementation in preterm infants.
Intrauterine growth retardation (IUGR)
Although DHA has been shown to be closely related to fetal neurodevelopment, there are few studies on the relationship between DHA and IUGR. A previous study found that DHA levels in maternal plasma and umbilical cord blood of pregnant women with IUGR fetuses decreased during pregnancy, whereas the placental expression of lipoprotein lipase, FABP1/3 and FATP1/2/4 increased [106]. The increase in placental fatty acid transporters may be a compensatory response, but this compensation did not improve the DHA deficiency of IUGR fetuses. It is not known whether the decrease in maternal DHA levels is a cause or consequence of IUGR. Although placental disorders are also predisposing factor for IUGR (see preterm birth section) [85], a meta-analysis suggested that n-3 PUFA supplementation during pregnancy did not reduce the risk of IUGR [47].
Given that the major site of action of DHA in the fetal period is the brain, two studies have evaluated the relationship between DHA supplementation during pregnancy and fetal head circumference [107, 108]. However, the two studies differed in their results, despite using the same DHA dose and similar start and end times. A Mexican study demonstrated that maternal intake of 400 mg/d DHA starting at 20 weeks of gestation was associated with a larger head circumference at birth [108], whereas another study suggested that intake of 400 mg/d DHA starting before 20 weeks of gestation until delivery did not increase the head circumference [107]. Gamboa et al. found that inactivating mutations in MFSD2A, required for n-3 PUFA transport in the brain, cause lethal microcephaly syndrome [109]. This result suggests that DHA deficiency may contribute to microcephaly. If clinical studies confirm this theory, DHA supplementation may be a potential treatment for women with microcephaly or small head circumference detected by ultrasound during pregnancy.
Notably, some animal models suggest that offspring with IUGR may benefit from maternal DHA supplementation, such as enhanced lung function [110, 111] and prevention of impaired oligodendrogenesis [112]. In addition, DHA supplementation in the offspring of IUGR model rats can improve cognition [113].
In conclusion, plasma and cord blood DHA levels are decreased in IUGR patients. DHA supplementation during pregnancy may have a protective effect on fetal microcephaly and small head circumference. Despite the demonstrated benefits of maternal and offspring DHA supplementation for IUGR infants in animal models, there are substantial gaps in relevant clinical studies, which should be the focus of future research.
Postpartum depression (PPD)
Previous studies have suggested that EPA, DHA and total n-3 PUFA levels are lower in patients with depression, suggesting their role in the pathogenesis of depression [114, 115]. Related RCTs and meta-analyses also suggest that n-3 PUFAs may exhibit preventive and therapeutic effects on depression [116,117,118] through their role in anti-inflammatory, antioxidant, and neurotrophic processes in the brain [119]. Similar to depression, patients who develop PPD have been shown to exhibit low levels of DHA in the postpartum period [120], which may occur in the third trimester [121] or even the first trimester [122]. Epidemiological evidence suggests that both higher DHA concentrations in breast milk and higher seafood consumption predict a lower prevalence of PPD [123], and greater seafood consumption and n-3 PUFA intake may be protective against PPD [124]. This evidence suggests the potential predictive, preventive and therapeutic effects of n-3 PUFAs in PPD.
However, the results of RCTs have been more divergent. A large RCT involving 2399 pregnant women suggested that DHA supplementation at 800 mg daily starting at 21 weeks of gestation did not reduce maternal PPD risk [125]. Other studies have reached similar conclusions [126,127,128,129,130]. For pregnant women with low DHA levels during pregnancy, additional DHA supplementation did not seem to prevent PPD [131]. DHA supplementation of 1.9 g/d for 8 weeks also did not exhibit a significant therapeutic effect on women who already developed PPD [130], and the result of Mendelian randomization did not demonstrate a causal relationship between n-3 PUFA intake and PPD [132]. In contrast, several recent studies have suggested an association between maternal DHA levels and PPD [133], as well as the preventive or therapeutic effects of DHA supplementation on PPD [134, 135]. We compared the differences between different studies and found that the year of study was the most significant factor explaining the differences in conclusions. Most of the negative studies [125,126,127,128,129,130,131,132] were conducted relatively early, with even the most recent negative studies [126, 127] published in 2017. However, most of the positive studies [133,134,135] were conducted in recent years, all of which were performed after 2020. The specific effect of study years on this outcome is not clear. Changes in social environment and dietary structure may be potential causes, but more clinical studies are needed to verify the results. The two recently published meta-analyses [136, 137] were limited by the lack of comprehensiveness of the included studies, and the conclusions were inconsistent, which had limited the creation of clinical guidelines. Although Cochrane did not conclude a protective effect of n-3 PUFAs against PPD [138], this meta-analysis is a decade old. Therefore, it is necessary to conduct a systematic, comprehensive and rigorous analysis of the studies on the association between n-3 PUFA intake and PPD.
In addition, because one-third of women with PPD experience the onset of depressive symptoms during pregnancy [139], we also summarized the effects of DHA intake on depression during pregnancy. Epidemiology suggests an association between low omega-3 intake from seafood and increased risk of elevated depressive symptoms during pregnancy [140], and the intake of fish and DHA has a protective effect on depression during pregnancy [141]. Rees et al. found that women with depression during pregnancy have lower blood DHA levels in the third trimester [142]. After adjustment for confounding factors, those with high DHA levels still had significantly lower odds of depression. Another prospective cohort also found that lower DHA serum concentrations, regardless of the pregnancy trimester in which levels were measured, were associated with higher odds of depressive symptoms throughout pregnancy [143]. Depressive symptoms in early pregnancy, even in the subclinical range, were inversely associated with breast milk DHA levels [144], which may have some impact on the offspring. Given that DHA appears to have a protective effect on depression during pregnancy [145], women with depressive symptoms may benefit from DHA supplementation during pregnancy, both for themselves and their offspring.
In summary, similar to patients with depression, DHA levels were decreased in PPD patients. Epidemiological evidence suggests that DHA supplementation has a potential role in the prediction, prevention and treatment of PPD. There is a large variation in clinical studies, and the year of study, which may reflect social development, dietary structure improvements and changes in the preparation of DHA, may be the main reason for this variation. In addition, DHA may also have a protective effect on depression during pregnancy.
Conclusions and future perspectives
Although significant evidence suggests that DHA supplementation during pregnancy may aid in the prevention of PT and may represent a treatment for GDM, in the data is less clear with respect to the prevention or treatment of other pregnancy complications. In view of the suggestive role of maternal DHA levels in these diseases, and the finding that only pregnant women with low maternal DHA levels could benefit from additional DHA supplementation in some studies, we suggest that the measurement of maternal DHA levels during pregnancy may have a positive effect on maternal perinatal management.
Studies suggest that a daily intake of 200 mg DHA can decrease the likelihood of preterm birth [146], and the recommended daily intake of DHA for pregnant women in many countries meets this requirement [89, 147]. Although studies suggest that 1000 mg/d DHA is more effective than 200 mg/d DHA in preventing ePT [89], there are few studies on the dose, and this relationship seems to be influenced by maternal DHA levels [91]. Therefore, we do not recommend DHA supplementation in healthy pregnant women beyond the doses recommended in the dietary guidelines because it does not appear to provide additional benefit. Unfortunately, in modern diets, the intake of fish containing high levels of n-3 PUFAs is limited [83]. In the United States, the average adult daily intake of DHA + EPA is approximately 100 mg [148], well below the recommended daily intake of DHA during pregnancy. Therefore, when normal pregnant women are unable to meet the appropriate intake of DHA, additional supplementation with DHA capsule preparations has a positive effect on pregnancy outcomes and fetal development.
Whether DHA supplementation should be added to the recommended intake of 200 mg/d for pregnant women with comorbidities remains questionable. The prevention and treatment effects of DHA for pregnancy complications are controversial, and there is a lack of related studies on the long-term neurodevelopment of offspring of women with complications. Previous animal studies have found that the water maze performance of healthy young mice fed DHA until adulthood is not different from that of healthy mice fed without DHA supplementation [149]. However, in animal models such as Alzheimer’s disease [150], traumatic brain injury [151], n-3 PUFA deficiency [152, 153] and offspring exposed to general anesthesia with propofol during early pregnancy [154], water maze related performances were significantly improved after DHA supplementation. In view of this phenomenon, we believe that the effects of DHA on nerve development and wound repair may only be reflected in pathological conditions. For women with normal pregnancies who have normal levels of DHA and meet the daily requirements for DHA intake, additional DHA supplementation may not confer benefit in the offspring. However, for mothers with certain pregnancy complications, even if their DHA levels are normal or they consume the recommended amount of DHA daily, the offspring may still be exposed to low DHA levels due to placental transport disorders, which may lead to long-term neurodevelopmental disorders. In such cases, although high-dose DHA supplementation may not play a role in the treatment of complications, it may improve DHA deficiency in offspring by increasing maternal DHA levels, improving placental fatty acid transport, and preventing the long-term neurodevelopmental disorders caused by some pregnancy complications.
Current studies on DHA and offspring neurodevelopment primarily focus on healthy pregnant women without complications. We hope that future studies can explore the effects of DHA supplementation on the long-term neurodevelopment of offspring in complicated pregnancies, and provide new guidance for the necessity of DHA supplementation in women with complicated pregnancies.
Availability of data and materials
Not applicable.
References
Lesthaeghe R. The second demographic transition, 1986–2020: sub-replacement fertility and rising cohabitation—a global update[J]. Genus. 2020;76(1):10.
Oura P. Sociodemographic indicators of birth rate in a low fertility Country-a nationwide study of 310 finnish municipalities covering > 5,000,000 inhabitants[J]. Front Public Health. 2021;9:643561.
Ogura S, Jakovljevic MM, Editorial. Global population aging - health care, social and economic consequences[J]. Front Public Health. 2018;6:335.
Attali E, Yogev Y. The impact of advanced maternal age on pregnancy outcome[J]. Best Pract Res Clin Obstet Gynaecol. 2021;70:2–9.
Hawkesworth S, Dangour AD, Johnston D, et al. Feeding the world healthily: the challenge of measuring the effects of agriculture on health[J]. Philos Trans R Soc Lond B Biol Sci. 2010;365(1554):3083–97.
Kimura I, Ichimura A, Ohue-Kitano R, et al. Free fatty acid receptors in health and disease[J]. Physiol Rev. 2020;100(1):171–210.
van Elst K, Bruining H, Birtoli B, et al. Food for thought: dietary changes in essential fatty acid ratios and the increase in autism spectrum disorders[J]. Neurosci Biobehav Rev. 2014;45:369–78.
Weiser MJ, Mucha B, Denheyer H, et al. Dietary docosahexaenoic acid alleviates autistic-like behaviors resulting from maternal immune activation in mice[J]. Prostaglandins Leukot Essent Fatty Acids. 2016;106:27–37.
Patrick RP. Role of phosphatidylcholine-DHA in preventing APOE4-associated Alzheimer’s disease[J]. FASEB J. 2019;33(2):1554–64.
Chang JP, Su KP, Mondelli V, et al. Omega-3 polyunsaturated fatty acids in youths with attention deficit hyperactivity disorder: a systematic review and meta-analysis of clinical trials and biological studies[J]. Neuropsychopharmacology. 2018;43(3):534–45.
Fabian CJ, Kimler BF, Hursting SD. Omega-3 fatty acids for breast cancer prevention and survivorship[J]. Breast Cancer Res. 2015;17(1):62.
Innes JK, Calder PC. Marine omega-3 (N-3) fatty acids for cardiovascular health: an update for 2020[J]. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21041362.
Cardoso C, Afonso C, Bandarra NM. Dietary DHA, bioaccessibility, and neurobehavioral development in children[J]. Crit Rev Food Sci Nutr. 2018;58(15):2617–31.
Gil-Sanchez A, Demmelmair H, Parrilla JJ, et al. Mechanisms involved in the selective transfer of long chain polyunsaturated fatty acids to the fetus[J]. Front Genet. 2011;2:57.
Larque E, Gil-Sanchez A, Prieto-Sanchez MT, et al. Omega 3 fatty acids, gestation and pregnancy outcomes[J]. Br J Nutr. 2012;107(Suppl 2):77–84.
Dangat KD, Mehendale SS, Yadav HR, et al. Long-chain polyunsaturated fatty acid composition of breast milk in pre-eclamptic mothers[J]. Neonatology. 2010;97(3):190–4.
Irwinda R, Hiksas R, Siregar AA, et al. Long-chain polyunsaturated fatty acid (LC-PUFA) status in severe preeclampsia and preterm birth: a cross sectional study[J]. Sci Rep. 2021;11(1):14701.
Wadhwani N, Patil V, Pisal H, et al. Altered maternal proportions of long chain polyunsaturated fatty acids and their transport leads to disturbed fetal stores in preeclampsia[J]. Prostaglandins Leukot Essent Fatty Acids. 2014;91(1–2):21–30.
Pagan A, Prieto-Sanchez MT, Blanco-Carnero JE, et al. Materno-fetal transfer of docosahexaenoic acid is impaired by gestational diabetes mellitus[J]. Am J Physiol Endocrinol Metab. 2013;305(7):E826–833.
Morgese MG, Trabace L. Maternal malnutrition in the etiopathogenesis of psychiatric diseases: role of polyunsaturated fatty acids[J]. Brain Sci. 2016. https://doi.org/10.3390/brainsci6030024.
Colombo J, Gustafson KM, Gajewski BJ, et al. Prenatal DHA supplementation and infant attention[J]. Pediatr Res. 2016;80(5):656–62.
Gould JF, Anderson PJ, Yelland LN, et al. The influence of prenatal DHA supplementation on individual domains of behavioral functioning in school-aged children: follow-up of a randomized controlled trial[J]. Nutrients. 2021. https://doi.org/10.3390/nu13092996.
Heath RJ, Wood TR. Why have the benefits of DHA not been borne out in the treatment and prevention of Alzheimer’s disease? A narrative review focused on DHA metabolism and adipose Tissue[J]. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms222111826.
Williams MA, Zingheim RW, King IB, et al. Omega-3 fatty acids in maternal erythrocytes and risk of preeclampsia[J]. Epidemiology. 1995;6(3):232–7.
Mackay VA, Huda SS, Stewart FM, et al. Preeclampsia is associated with compromised maternal synthesis of long-chain polyunsaturated fatty acids, leading to offspring deficiency[J]. Hypertension. 2012;60(4):1078–85.
Jarvie E, Hauguel-de-Mouzon S, Nelson SM, et al. Lipotoxicity in obese pregnancy and its potential role in adverse pregnancy outcome and obesity in the offspring[J]. Clin Sci (Lond). 2010;119(3):123–9.
Mehendale S, Kilari A, Dangat K, et al. Fatty acids, antioxidants, and oxidative stress in pre-eclampsia[J]. Int J Gynaecol Obstet. 2008;100(3):234–8.
Roy S, Dhobale M, Dangat K, et al. Differential levels of long chain polyunsaturated fatty acids in women with preeclampsia delivering male and female babies[J]. Prostaglandins Leukot Essent Fatty Acids. 2014;91(5):227–32.
Barron A, McCarthy CM, O’Keeffe GW. Preeclampsia and neurodevelopmental outcomes: potential pathogenic roles for inflammation and oxidative stress?[J]. Mol Neurobiol. 2021;58(6):2734–56.
Kulkarni AV, Mehendale SS, Yadav HR, et al. Circulating angiogenic factors and their association with birth outcomes in preeclampsia[J]. Hypertens Res. 2010;33(6):561–7.
Larque E, Demmelmair H, Klingler M, et al. Expression pattern of fatty acid transport protein-1 (FATP-1), FATP-4 and heart-fatty acid binding protein (H-FABP) genes in human term placenta[J]. Early Hum Dev. 2006;82(10):697–701.
Brown SH, Eather SR, Freeman DJ, et al. A lipidomic analysis of placenta in preeclampsia: evidence for lipid storage[J]. PLoS ONE. 2016;11(9):e0163972.
Hu M, Li J, Baker PN, et al. Revisiting preeclampsia: a metabolic disorder of the placenta[J]. FEBS J. 2022;289(2):336–54.
Campbell FM, Bush PG, Veerkamp JH, et al. Detection and cellular localization of plasma membrane-associated and cytoplasmic fatty acid-binding proteins in human placenta[J]. Placenta. 1998;19(5–6):409–15.
Scifres CM, Chen B, Nelson DM, et al. Fatty acid binding protein 4 regulates intracellular lipid accumulation in human trophoblasts[J]. J Clin Endocrinol Metab. 2011;96(7):E1083–1091.
Biron-Shental T, Schaiff WT, Ratajczak CK, et al. Hypoxia regulates the expression of fatty acid-binding proteins in primary term human trophoblasts[J]. Am J Obstet Gynecol. 2007;197(5):516e511–516.
Yan Y, Peng H, Wang P, et al. Increased expression of fatty acid binding protein 4 in preeclamptic placenta and its relevance to preeclampsia[J]. Placenta. 2016;39:94–100.
Scifres CM, Catov JM, Simhan H. Maternal serum fatty acid binding protein 4 (FABP4) and the development of preeclampsia[J]. J Clin Endocrinol Metab. 2012;97(3):E349–356.
Li G, Li Y, Xiao B, et al. Antioxidant activity of docosahexaenoic acid (DHA) and its regulatory roles in mitochondria[J]. J Agric Food Chem. 2021;69(5):1647–55.
Giaginis C, Spanopoulou E, Theocharis S. PPAR-gamma signaling pathway in placental development and function: a potential therapeutic target in the treatment of gestational diseases[J]. Expert Opin Ther Targets. 2008;12(8):1049–63.
Liu Y, Tian Y, Cai W, et al. DHA/EPA-enriched phosphatidylcholine suppresses tumor growth and metastasis via activating peroxisome proliferator-activated receptor gamma in lewis lung cancer mice[J]. J Agric Food Chem. 2021;69(2):676–85.
Dangat K, Kilari A, Mehendale S, et al. Preeclampsia alters milk neurotrophins and long chain polyunsaturated fatty acids[J]. Int J Dev Neurosci. 2014;33:115–21.
Rodriguez-Cruz M, Tovar AR, Palacios-Gonzalez B, et al. Synthesis of long-chain polyunsaturated fatty acids in lactating mammary gland: role of Delta5 and Delta6 desaturases, SREBP-1, PPARalpha, and PGC-1[J]. J Lipid Res. 2006;47(3):553–60.
Yang B, Shi MQ, Li ZH, et al. Fish, long-chain n-3 PUFA and incidence of elevated blood pressure: a meta-analysis of prospective cohort studies[J]. Nutrients. 2016. https://doi.org/10.3390/nu8010058.
Liao J, Xiong Q, Yin Y, et al. The effects of fish oil on cardiovascular diseases: systematical evaluation and recent advance[J]. Front Cardiovasc Med. 2021;8:802306.
Bercea CI, Cottrell GS, Tamagnini F, et al. Omega-3 polyunsaturated fatty acids and hypertension: a review of vasodilatory mechanisms of docosahexaenoic acid and eicosapentaenoic acid[J]. Br J Pharmacol. 2021;178(4):860–77.
Middleton P, Gomersall JC, Gould JF, et al. Omega-3 fatty acid addition during pregnancy[J]. Cochrane Database Syst Rev. 2018;11(11):CD003402.
Zhou SJ, Yelland L, McPhee AJ, et al. Fish-oil supplementation in pregnancy does not reduce the risk of gestational diabetes or preeclampsia[J]. Am J Clin Nutr. 2012;95(6):1378–84.
Li SN, Liu YH, Luo ZY, et al. The association between dietary fatty acid intake and the risk of developing preeclampsia: a matched case-control study[J]. Sci Rep. 2021;11(1):4048.
Arvizu M, Afeiche MC, Hansen S, et al. Fat intake during pregnancy and risk of preeclampsia: a prospective cohort study in Denmark[J]. Eur J Clin Nutr. 2019;73(7):1040–8.
Thomas B, Ghebremeskel K, Lowy C, et al. Plasma AA and DHA levels are not compromised in newly diagnosed gestational diabetic women[J]. Eur J Clin Nutr. 2004;58(11):1492–7.
Hai-Tao Y, Zhi-Heng G, Yi-Ru C, et al. Gestational diabetes mellitus decreased umbilical cord blood polyunsaturated fatty acids: a meta-analysis of observational studies[J]. Prostaglandins Leukot Essent Fatty Acids. 2021;171:102318.
Leveille P, Ardilouze JL, Pasquier JC, et al. Fatty acid profile in cord blood of neonates born to optimally controlled gestational diabetes mellitus[J]. Prostaglandins Leukot Essent Fatty Acids. 2016;115:48–52.
Devarshi PP, Grant RW, Ikonte CJ, et al. Maternal omega-3 nutrition, placental transfer and fetal brain development in gestational diabetes and preeclampsia[J]. Nutrients. 2019. https://doi.org/10.3390/nu11051107.
Gazquez A, Gimenez-Banon MJ, Prieto-Sanchez MT, et al. Self-reported DHA supplementation during pregnancy and its association with obesity or gestational diabetes in relation to DHA concentration in cord and maternal plasma: results from NELA, a prospective mother-offspring cohort[J]. Nutrients. 2021. https://doi.org/10.3390/nu13030843.
Min Y, Djahanbakhch O, Hutchinson J, et al. Efficacy of docosahexaenoic acid-enriched formula to enhance maternal and fetal blood docosahexaenoic acid levels: randomized double-blinded placebo-controlled trial of pregnant women with gestational diabetes mellitus[J]. Clin Nutr. 2016;35(3):608–14.
Sanchez-Campillo M, Ruiz-Palacios M, Ruiz-Alcaraz AJ, et al. Child head circumference and placental MFSD2a expression are associated to the level of MFSD2a in maternal blood during pregnancy[J]. Front Endocrinol. 2020;11:38.
Segura MT, Demmelmair H, Krauss-Etschmann S, et al. Maternal BMI and gestational diabetes alter placental lipid transporters and fatty acid composition[J]. Placenta. 2017;57:144–51.
Mishra JS, Zhao H, Hattis S, et al. Elevated glucose and insulin levels decrease DHA transfer across human trophoblasts via SIRT1-dependent mechanism[J]. Nutrients. 2020. https://doi.org/10.3390/nu12051271.
Ortega-Senovilla H, Schaefer-Graf U, Herrera E. Pregnant women with gestational diabetes and with well controlled glucose levels have decreased concentrations of individual fatty acids in maternal and cord serum[J]. Diabetologia. 2020;63(4):864–74.
Thomas BA, Ghebremeskel K, Lowy C, et al. Plasma fatty acids of neonates born to mothers with and without gestational diabetes[J]. Prostaglandins Leukot Essent Fatty Acids. 2005;72(5):335–41.
Ortega-Senovilla H, Alvino G, Taricco E, et al. Gestational diabetes mellitus upsets the proportion of fatty acids in umbilical arterial but not venous plasma[J]. Diabetes Care. 2009;32(1):120–2.
Zornoza-Moreno M, Fuentes-Hernandez S, Carrion V, et al. Is low docosahexaenoic acid associated with disturbed rhythms and neurodevelopment in offsprings of diabetic mothers?[J]. Eur J Clin Nutr. 2014;68(8):931–7.
Garcia-Lopez S, Villanueva Arriaga RE, Najera Medina O, et al. One month of omega-3 fatty acid supplementation improves lipid profiles, glucose levels and blood pressure in overweight schoolchildren with metabolic syndrome[J]. J Pediatr Endocrinol Metab. 2016;29(10):1143–50.
Pellonpera O, Vahlberg T, Mokkala K, et al. Weight gain and body composition during pregnancy: a randomised pilot trial with probiotics and/or fish oil[J]. Br J Nutr. 2021;126(4):541–51.
Zhu Y, Li M, Rahman ML, et al. Plasma phospholipid n-3 and n-6 polyunsaturated fatty acids in relation to cardiometabolic markers and gestational diabetes: a longitudinal study within the prospective NICHD fetal growth studies[J]. PLoS Med. 2019;16(9):e1002910.
Lamping KG, Nuno DW, Coppey LJ, et al. Modification of high saturated fat diet with n-3 polyunsaturated fat improves glucose intolerance and vascular dysfunction[J]. Diabetes Obes Metab. 2013;15(2):144–52.
Pahlavani M, Ramalho T, Koboziev I, et al. Adipose tissue inflammation in insulin resistance: review of mechanisms mediating anti-inflammatory effects of omega-3 polyunsaturated fatty acids[J]. J Investig Med. 2017;65(7):1021–7.
Gao J, Huang T, Li J, et al. Beneficial effects of n-3 polyunsaturated fatty acids on offspring’s pancreas of gestational diabetes rats[J]. J Agric Food Chem. 2019;67(48):13269–81.
Gholami N, Abotorabi S, Lalooha F, et al. Effects of fish oil supplementation on pregnancy outcomes in pregnant women referred to Kosar hospital[J]. Iran J Pharm Res. 2020;19(3):241–7.
Yang S, Lin R, Si L, et al. Cod-liver oil improves metabolic indices and hs-CRP levels in gestational diabetes mellitus patients: a double-blind randomized controlled trial[J]. J Diabetes Res. 2019. https://doi.org/10.1155/2019/7074042.
Jamilian M, Samimi M, Ebrahimi FA, et al. The effects of vitamin D and omega-3 fatty acid co-supplementation on glycemic control and lipid concentrations in patients with gestational diabetes[J]. J Clin Lipidol. 2017;11(2):459–68.
Olsen SF, Halldorsson TI, Thorne-Lyman AL, et al. Plasma concentrations of long chain N-3 fatty acids in early and mid-pregnancy and risk of early preterm birth[J]. EBioMedicine. 2018;35:325–33.
Jackson KH, Harris WS. A prenatal DHA test to help identify women at increased risk for early preterm birth: a proposal[J]. Nutrients. 2018. https://doi.org/10.3390/nu10121933.
Lauterbach R. EPA + DHA in prevention of early preterm birth—do we know how to apply it?[J]. EBioMedicine. 2018;35:16–7.
Norwitz ER, Robinson JN, Challis JR. The control of labor[J]. N Engl J Med. 1999;341(9):660–6.
Shaikh SR, Kinnun JJ, Leng X, et al. How polyunsaturated fatty acids modify molecular organization in membranes: insight from NMR studies of model systems[J]. Biochim Biophys Acta. 2015;1848(1 Pt B):211–9.
Radosinska J, Kurahara LH, Hiraishi K, et al. Modulation of cardiac connexin-43 by omega-3 fatty acid ethyl-ester supplementation demonstrated in spontaneously diabetic rats[J]. Physiol Res. 2015;64(6):795–806.
Gabbs M, Leng S, Devassy JG, et al. Advances in our understanding of oxylipins derived from dietary PUFAs[J]. Adv Nutr. 2015;6(5):513–40.
Romero R, Espinoza J, Kusanovic JP, et al. The preterm parturition syndrome[J]. BJOG. 2006;113(Suppl 3):17–42.
Prairie E, Cote F, Tsakpinoglou M, et al. The determinant role of IL-6 in the establishment of inflammation leading to spontaneous preterm birth[J]. Cytokine Growth Factor Rev. 2021;59:118–30.
Goldenberg RL, Culhane JF, Iams JD, et al. Epidemiology and causes of preterm birth[J]. Lancet. 2008;371(9606):75–84.
Rogers LK, Valentine CJ, Keim SA. DHA supplementation: current implications in pregnancy and childhood[J]. Pharmacol Res. 2013;70(1):13–9.
Carlson SE, Colombo J, Gajewski BJ, et al. DHA supplementation and pregnancy outcomes[J]. Am J Clin Nutr. 2013;97(4):808–15.
Carvajal JA. Docosahexaenoic acid supplementation early in pregnancy may prevent deep placentation disorders[J]. Biomed Res Int. 2014;2014:526895.
Basak S, Duttaroy AK. cis-9,trans-11 conjugated linoleic acid stimulates expression of angiopoietin like-4 in the placental extravillous trophoblast cells[J]. Biochim Biophys Acta. 2013;1831(4):834–43.
Basak S, Duttaroy AK. Effects of fatty acids on angiogenic activity in the placental extravillious trophoblast cells[J]. Prostaglandins Leukot Essent Fatty Acids. 2013;88(2):155–62.
Valentine CJ, Khan AQ, Brown AR, et al. Higher-dose DHA supplementation modulates immune responses in pregnancy and is associated with decreased preterm birth[J]. Nutrients. 2021. https://doi.org/10.3390/nu13124248.
Carlson SE, Gajewski BJ, Valentine CJ, et al. Higher dose docosahexaenoic acid supplementation during pregnancy and early preterm birth: a randomised, double-blind, adaptive-design superiority trial[J]. EClinicalMedicine. 2021;36:100905.
Colombo J, Shaddy DJ, Gustafson K, et al. The Kansas University DHA outcomes study (KUDOS) clinical trial: long-term behavioral follow-up of the effects of prenatal DHA supplementation[J]. Am J Clin Nutr. 2019;109(5):1380–92.
Simmonds LA, Sullivan TR, Skubisz M, et al. Omega-3 fatty acid supplementation in pregnancy-baseline omega-3 status and early preterm birth: exploratory analysis of a randomised controlled trial[J]. BJOG. 2020;127(8):975–81.
Kuipers RS, Luxwolda MF, Offringa PJ, et al. Fetal intrauterine whole body linoleic, arachidonic and docosahexaenoic acid contents and accretion rates[J]. Prostaglandins Leukot Essent Fatty Acids. 2012;86(1–2):13–20.
Baack ML, Puumala SE, Messier SE, et al. Daily enteral DHA supplementation alleviates deficiency in premature infants[J]. Lipids. 2016;51(4):423–33.
Valentine CJ. Maternal dietary DHA supplementation to improve inflammatory outcomes in the preterm infant[J]. Adv Nutr. 2012;3(3):370–6.
Martin CR, Dasilva DA, Cluette-Brown JE, et al. Decreased postnatal docosahexaenoic and arachidonic acid blood levels in premature infants are associated with neonatal morbidities[J]. J Pediatr. 2011;159(5):743–9. e741-742.
Valentine CJ, Morrow G, Fernandez S, et al. Docosahexaenoic acid and amino acid contents in pasteurized donor milk are low for preterm infants[J]. J Pediatr. 2010;157(6):906–10.
Vizzari G, Morniroli D, Alessandretti F, et al. Comparative analysis of docosahexaenoic acid (DHA) content in mother’s milk of term and preterm mothers[J]. Nutrients. 2022. https://doi.org/10.3390/nu14214595.
Heath RJ, Klevebro S, Wood TR. Maternal and neonatal polyunsaturated fatty acid intake and risk of neurodevelopmental impairment in premature infants[J]. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23020700.
Castillo F, Castillo-Ferrer FJ, Cordobilla B, et al. Inadequate content of docosahexaenoic acid (DHA) of donor human milk for feeding preterm infants: a comparison with mother’s own milk at different stages of lactation[J]. Nutrients. 2021. https://doi.org/10.3390/nu13041300.
Hewawasam E, Collins CT, Muhlhausler BS, et al. DHA supplementation in infants born preterm and the effect on attention at 18 months’ corrected age: follow-up of a subset of the N3RO randomised controlled trial[J]. Br J Nutr. 2021;125(4):420–31.
Moon K, Rao SC, Schulzke SM, et al. Longchain polyunsaturated fatty acid supplementation in preterm infants[J]. Cochrane Database Syst Rev. 2016;12(12):CD000375.
Westerberg AC, Schei R, Henriksen C, et al. Attention among very low birth weight infants following early supplementation with docosahexaenoic and arachidonic acid[J]. Acta Paediatr. 2011;100(1):47–52.
Manley BJ, Makrides M, Collins CT, et al. High-dose docosahexaenoic acid supplementation of preterm infants: respiratory and allergy outcomes[J]. Pediatrics. 2011;128(1):e71–77.
Bernabe-Garcia M, Calder PC, Villegas-Silva R, et al. Efficacy of docosahexaenoic acid for the prevention of necrotizing enterocolitis in preterm infants: a randomized clinical Trial[J]. Nutrients. 2021. https://doi.org/10.3390/nu13020648.
Tam EW, Chau V, Barkovich AJ, et al. Early postnatal docosahexaenoic acid levels and improved preterm brain development[J]. Pediatr Res. 2016;79(5):723–30.
Assumpcao RP, Mucci DB, Fonseca FCP, et al. Fatty acid profile of maternal and fetal erythrocytes and placental expression of fatty acid transport proteins in normal and intrauterine growth restriction pregnancies[J]. Prostaglandins Leukot Essent Fatty Acids. 2017;125:24–31.
Khandelwal S, Kondal D, Chaudhry M, et al. Prenatal maternal docosahexaenoic acid (DHA) supplementation and newborn anthropometry in India: findings from DHANI[J]. Nutrients. 2021. https://doi.org/10.3390/nu13030730.
Ramakrishnan U, Stein AD, Parra-Cabrera S, et al. Effects of docosahexaenoic acid supplementation during pregnancy on gestational age and size at birth: randomized, double-blind, placebo-controlled trial in Mexico[J]. Food Nutr Bull. 2010;31(2 Suppl):108–16.
Guemez-Gamboa A, Nguyen LN, Yang H, et al. Inactivating mutations in MFSD2A, required for omega-3 fatty acid transport in brain, cause a lethal microcephaly syndrome[J]. Nat Genet. 2015;47(7):809–13.
Velten M, Britt RD Jr, Heyob KM, et al. Maternal dietary docosahexaenoic acid supplementation attenuates fetal growth restriction and enhances pulmonary function in a newborn mouse model of perinatal inflammation[J]. J Nutr. 2014;144(3):258–66.
Joss-Moore LA, Wang Y, Baack ML, et al. IUGR decreases PPARgamma and SETD8 expression in neonatal rat lung and these effects are ameliorated by maternal DHA supplementation[J]. Early Hum Dev. 2010;86(12):785–91.
Kuhne BA, Vazquez-Aristizabal P, Fuentes-Amell M, et al. Docosahexaenoic acid and melatonin prevent impaired oligodendrogenesis induced by intrauterine growth restriction (IUGR)[J]. Biomedicines. 2022. https://doi.org/10.3390/biomedicines10051205.
Wan L, He X, He M, et al. Docosahexaenoic acid improves cognition and hippocampal pyroptosis in rats with intrauterine growth restriction[J]. Heliyon. 2023;9(2):e12920.
Hibbeln JR. Fish consumption and major depression[J]. Lancet. 1998;351(9110):1213.
Lin PY, Huang SY, Su KP. A meta-analytic review of polyunsaturated fatty acid compositions in patients with depression[J]. Biol Psychiatry. 2010;68(2):140–7.
Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder[J]. Am J Psychiatry. 2002;159(3):477–9.
Su KP, Huang SY, Chiu CC, et al. Omega-3 fatty acids in major depressive disorder. A preliminary double-blind, placebo-controlled trial[J]. Eur Neuropsychopharmacol. 2003;13(4):267–71.
Guu TW, Mischoulon D, Sarris J, et al. International society for nutritional psychiatry research practice guidelinesfor omega-3 fatty acids in the treatment of major depressive disorder. Psychother Psychosom. 2019;88(5):263–73.
Song C, Shieh CH, Wu YS, et al. The role of omega-3 polyunsaturated fatty acids eicosapentaenoic and docosahexaenoic acids in the treatment of major depression and Alzheimer’s disease: acting separately or synergistically?[J]. Prog Lipid Res. 2016;62:41–54.
Otto SJ, de Groot RH, Hornstra G. Increased risk of postpartum depressive symptoms is associated with slower normalization after pregnancy of the functional docosahexaenoic acid status[J]. Prostaglandins Leukot Essent Fatty Acids. 2003;69(4):237–43.
Markhus MW, Skotheim S, Graff IE, et al. Low omega-3 index in pregnancy is a possible biological risk factor for postpartum depression[J]. PLoS ONE. 2013;8(7):e67617.
Hoge A, Tabar V, Donneau AF, et al. Imbalance between omega-6 and omega-3 polyunsaturated fatty acids in early pregnancy is predictive of postpartum depression in a belgian cohort[J]. Nutrients. 2019. https://doi.org/10.3390/nu11040876.
Hibbeln JR. Seafood consumption, the DHA content of mothers’ milk and prevalence rates of postpartum depression: a cross-national, ecological analysis[J]. J Affect Disord. 2002;69(1–3):15–29.
Zhao XH, Zhang ZH. Risk factors for postpartum depression: an evidence-based systematic review of systematic reviews and meta-analyses[J]. Asian J Psychiatr. 2020;53:102353.
Makrides M, Gibson RA, McPhee AJ, et al. Effect of DHA supplementation during pregnancy on maternal depression and neurodevelopment of young children: a randomized controlled trial[J]. JAMA. 2010;304(15):1675–83.
Vaz JDS, Farias DR, Adegboye ARA, et al. Omega-3 supplementation from pregnancy to postpartum to prevent depressive symptoms: a randomized placebo-controlled trial[J]. BMC Pregnancy Childbirth. 2017;17(1):180.
Kobayashi M, Ogawa K, Morisaki N, et al. Dietary n-3 polyunsaturated fatty acids in late pregnancy and pcite figure.ostpartum depressive symptom among Japanese women[J]. Front Psychiatry. 2017;8:241.
Mozurkewich EL, Clinton CM, Chilimigras JL, et al. The mothers, Omega-3, and Mental Health Study: a double-blind, randomized controlled trial[J]. Am J Obstet Gynecol. 2013;208(4):313e311–319.
Rees AM, Austin MP, Parker GB. Omega-3 fatty acids as a treatment for perinatal depression: randomized double-blind placebo-controlled trial[J]. Aust N Z J Psychiatry. 2008;42(3):199–205.
Freeman MP, Davis M, Sinha P, et al. Omega-3 fatty acids and supportive psychotherapy for perinatal depression: a randomized placebo-controlled study[J]. J Affect Disord. 2008;110(1–2):142–8.
Doornbos B, van Goor SA, Dijck-Brouwer DA, et al. Supplementation of a low dose of DHA or DHA + AA does not prevent peripartum depressive symptoms in a small population based sample[J]. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(1):49–52.
Sallis H, Steer C, Paternoster L, et al. Perinatal depression and omega-3 fatty acids: a mendelian randomisation study[J]. J Affect Disord. 2014;166(100):124–31.
Urech C, Eussen S, Alder J, et al. Levels of n-3 and n-6 fatty acids in maternal erythrocytes during pregnancy and in human milk and its association with perinatal mental health[J]. Nutrients. 2020. https://doi.org/10.3390/nu12092773.
Cao Y, Wei Q, Zou L, et al. Postpartum dietary intake, depression and the concentration of docosahexaenoic acid in mature breast milk in Wuhan, China[J]. Food Funct. 2023. https://doi.org/10.1039/d2fo03129a.
Osuna E, Symington EA, Malan L, et al. Higher n-3 polyunsaturated fatty acid status during early pregnancy is associated with lower risk for depression at 12 months postpartum: the NuPED study[J]. Prostaglandins Leukot Essent Fatty Acids. 2023;190:102528.
Suradom C, Suttajit S, Oon-Arom A, et al. Omega-3 polyunsaturated fatty acid (n-3 PUFA) supplementation for prevention and treatment of perinatal depression: a systematic review and meta-analysis of randomized-controlled trials[J]. Nord J Psychiatry. 2021;75(4):239–46.
Zhang MM, Zou Y, Li SM, et al. The efficacy and safety of omega-3 fatty acids on depressive symptoms in perinatal women: a meta-analysis of randomized placebo-controlled trials[J]. Transl Psychiatry. 2020;10(1):193.
Miller BJ, Murray L, Beckmann MM, et al. Dietary supplements for preventing postnatal depression[J]. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD009104.pub2.
Wisner KL, Sit DK, McShea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings[J]. JAMA Psychiatry. 2013;70(5):490–8.
Golding J, Steer C, Emmett P, et al. High levels of depressive symptoms in pregnancy with low omega-3 fatty acid intake from fish[J]. Epidemiology. 2009;20(4):598–603.
Sontrop J, Avison WR, Evers SE, et al. Depressive symptoms during pregnancy in relation to fish consumption and intake of n-3 polyunsaturated fatty acids[J]. Paediatr Perinat Epidemiol. 2008;22(4):389–99.
Rees AM, Austin MP, Owen C, et al. Omega-3 deficiency associated with perinatal depression: case control study[J]. Psychiatry Res. 2009;166(2–3):254–9.
Pinto TJ, Vilela AA, Farias DR, et al. Serum n-3 polyunsaturated fatty acids are inversely associated with longitudinal changes in depressive symptoms during pregnancy[J]. Epidemiol Psychiatr Sci. 2017;26(2):157–68.
Keim SA, Daniels JL, Siega-Riz AM, et al. Depressive symptoms during pregnancy and the concentration of fatty acids in breast milk[J]. J Hum Lact. 2012;28(2):189–95.
Hsu MC, Tung CY, Chen HE. Omega-3 polyunsaturated fatty acid supplementation in prevention and treatment of maternal depression: putative mechanism and recommendation[J]. J Affect Disord. 2018;238:47–61.
Le Donne M, Alibrandi A, Vita R, et al. Does eating oily fish improve gestational and neonatal outcomes? Findings from a sicilian study[J]. Women Birth. 2016;29(3):e50–57.
Authority EFS. Dietary reference values for nutrients summary report[J]. EFSA Support Publ. 2017;14(12):e15121E.
Ervin RB, Wang CY, Wright JD, et al. Dietary intake of selected minerals for the United States population: 1999–2000[J]. Adv Data. 2004;341:1–5.
Wainwright PE, Xing HC, Ward GR, et al. Water maze performance is unaffected in artificially reared rats fed diets supplemented with arachidonic acid and docosahexaenoic acid[J]. J Nutr. 1999;129(5):1079–89.
Xiao M, Xiang W, Chen Y, et al. DHA ameliorates cognitive ability, reduces amyloid deposition, and nerve fiber production in Alzheimer’s disease[J]. Front Nutr. 2022;9:852433.
Zhu W, Ding Y, Kong W, et al. Docosahexaenoic acid (DHA) provides neuroprotection in traumatic brain injury models via activating Nrf2-ARE signaling[J]. Inflammation. 2018;41(4):1182–93.
Wainwright PE, Xing HC, Girard T, et al. Effects of dietary n-3 fatty acid deficiency on morris water-maze performance and amphetamine-induced conditioned place preference in rats[J]. Nutr Neurosci. 1998;1(4):281–93.
Wen M, Zhao Y, Shi H, et al. Short-term supplementation of DHA as phospholipids rather than triglycerides improve cognitive deficits induced by maternal omega-3 PUFA deficiency during the late postnatal stage[J]. Food Funct. 2021;12(2):564–72.
Yu X, Ma F, Cao X, et al. Effects of the application of general anesthesia with propofol during the early stage of pregnancy on brain development and function of SD rat offspring and the intervention of DHA[J]. Neurol Res. 2019;41(11):1008–14.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Key Research and Development Program of China (2021YFC2701502).
Author information
Authors and Affiliations
Contributions
Conceptualization, YJ; writing—original draft preparation, YJ, LJW, HTZ, YTC; writing—review and editing, XZ, SLZ, YYD and RS; resources, CYF, JYZ, WCD and LF; funding acquisition, LF. All authors read and approved the final the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, Y., Chen, Y., Wei, L. et al. DHA supplementation and pregnancy complications. J Transl Med 21, 394 (2023). https://doi.org/10.1186/s12967-023-04239-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-023-04239-8