Abstract
Background
Although physical activity is generally protective of cardiovascular disease (CVD), less is known about how young adult physical activity relates to premature CVD events. The objective of this study was to determine the association between level and change in physical activity from young adulthood to middle age and incidence of premature CVD events before age 60.
Methods
We analyzed data collected across four urban sites from nine visits over 30 years of follow-up (1985–2016) from the Coronary Artery Risk Development in Young Adults (CARDIA) study, a prospective community-based cohort study of 5115 Black and White women and men aged 18–30 years at baseline (1985–1986). Linear mixed models were used to develop individualized moderate-to-vigorous intensity self-reported physical activity trajectories per participant. Fatal and nonfatal coronary heart disease (CHD), heart failure, and stroke outcomes were analyzed separately and as a combined CVD event outcome.
Results
Overall, physical activity declined in young adults as they progressed through middle age. Lower physical activity scores (per 100 exercise units) in 18 year-olds were associated with higher odds of premature CHD (AOR 1.14, 95% CI 1.02–1.28), heart failure (AOR 1.21, 95% CI 1.05–1.38), stroke (AOR 1.20, 95% CI 1.04–1.39), and any CVD (AOR 1.15, 95% CI 1.06–1.24) events. Each additional annual 1-unit reduction in the physical activity score was associated with a higher annual odds of incident heart failure (1.07, 95% CI 1.02–1.13), stroke (1.06, 95% CI 1.00–1.13), and CVD (1.04, 95% CI 1.01–1.07) events. Meeting the minimum (AOR 0.74, 95% CI 0.0.57–0.96) and twice the minimum (AOR 0.55, 95% CI 0.34–0.91) Department of Health and Human Services physical activity guidelines through follow up was protective of premature CVD events.
Conclusions
Given recent trends in declining physical activity with age and associated premature CVD events, the transition from young adult to midlife is an important time period to promote physical activity.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the United States (US), with over 130 million adults in the US (45.1%) projected to have CVD by 2035 [1]. Despite prior studies noting the relationship between physical activity and CVD events (hospitalizations and mortality) [2,3,4], the 2018 Department of Health and Human Services (HHS) Physical Activity Guidelines noted important research gaps of public health importance [5]. The HHS Guidelines determined that there was insufficient evidence to determine if the relationship between physical activity and CVD events vary by age. Thus, further research investigating the importance of timing of the physical activity exposure across the life course is needed [5]. For instance, little is known about how physical activity trajectories (level and annual change) from young adulthood to middle age (approximately 18 to 65 years) influence CVD events, particularly premature events prior to age 60.
Serious gaps remain in our understanding of recommended levels of physical activity during young adulthood [5]. Young adulthood is an important transition period that sets physical activity patterns for the rest of adulthood and may represent a critical window for intervention [6,7,8]. On average, physical activity declines markedly during young adulthood, when individuals often transition from high school to college or the workforce [6,7,8]. The Physical Activity Guidelines noted young adults have unique growth and developmental needs similar to adolescents [5]. However, the optimal dose of physical activity, particularly in young adulthood, to prevent CVD events, remains unknown [9, 10]. Furthermore, physical activity disparities by race and sex have been noted in young adulthood and through the adult life course [11, 12], but it is unknown if race or sex modifies the effect of physical activity and CVD events.
We sought to quantify the impact of young adult and midlife physical activity on metabolic risk factors by analyzing data from the Coronary Artery Risk Development in Young Adults (CARDIA) Study, a large prospective cohort starting in young adulthood with 30 years of follow-up. CARDIA collected repeated measures of moderate and vigorous intensity physical activity, which allow for the development of individual trajectories of physical activity from young adulthood through middle age. The objective of this study was to determine the independent associations between young adult level of physical activity and subsequent changes in physical activity through the transition to midlife and incidence of premature CVD events (coronary heart disease [CHD], heart failure, stroke). In addition, we examined if meeting the current adult aerobic physical activity guideline levels were protective of premature CVD events. We hypothesized low physical activity levels at age 18 and declines in physical activity through the adult life course will be associated with incidence of premature CVD events.
Methods
Study population
The CARDIA Study recruited Black and White young adults (N = 5115) from four urban sites (Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California). Baseline data collection occurred in 1985–1986 and participants have been followed up for more than 30 years with high retention. Retention was 91, 86, 81, 77, 74, 72, 72, and 71% at years 2, 5, 7, 10, 15, 20, 25, 30, respectively. At baseline, the cohort was designed to be approximately balanced within center by age (18–24 years and 25–30 years), race (Black and White), sex (male and female), and educational level (high school or less or higher than high school). Following the baseline examination, one participant requested to be excluded from further analyses. Additional details about the study design are described elsewhere [13]. The institutional review boards at each study site approved study procedures. All participants provided written informed consent.
Measures
Physical activity
Physical activity was ascertained by the interviewer-administered CARDIA Physical Activity History Questionnaire at each of the 9 examinations [14, 15]. Participants self-reported their frequency of participation in 13 activity categories (8 vigorous and 5 moderate intensity) within time for leisure and occupational physical activity domains over the past 12 months. Each activity’s intensity was measured as metabolic equivalents of task (METs), where 1 MET is the energy expended at rest (an approximate oxygen consumption of 3.5 mL/1 kg of body weight/minute). Vigorous intensity activities (≥6 METs) included running, swimming, heavy lifting, and vigorous exercise classes. Moderate intensity activities (3–5.9 METs) included walking, non-strenuous sports (e.g. softball), and home maintenance (e.g., raking, gardening) [16]. A frequency was assigned to each activity based on the following criteria: 1) whether it was performed for ≥1 hour or during any 1 month in the past year, 2) the number of months it was performed at that level, and 3) the number of months the activity was performed frequently. Duration thresholds (2–5 hours per week) and intensity scores (3–8 METs) were assigned to each activity. Frequent participation was defined as above these levels [15]. Frequency (number of months) of participation was multiplied by the intensity (METs) of each activity, with a weighting factor for the months of more frequent participation, to calculate the moderate-to-vigorous-intensity physical activity score [17]. All activities were summed to estimate the total activity score expressed in exercise units (EUs). For reference, a physical activity score of 300 EU approximates the HHS recommendations of approximately 150 minutes of moderate-intensity activity per week [18, 19]. Convergent validity of the CARDIA Physical Activity History questionnaire has been established using report-based measures, including physical activity diaries and detailed quantitative recall questionnaires [14, 17, 20] and accelerometers [20,21,22]. The CARDIA physical activity questionnaire demonstrated test-retest reliability of 0.77–0.84 [17], similar to other activity questionnaires [14].
CVD events
Any fatal or non-fatal CVD events, including coronary heart disease (myocardial infarction, non-myocardial infarction acute coronary syndrome), heart failure, and stroke (stroke, transient ischemic attack), were determined through participant contacts every 6 months, annual vital status searches, national death index searches every 5 years, telephone contact, and relevant medical records. Hospital records were sought for self-reported outcomes, and central adjudication was performed by trained physicians to ascertain CVD events. Two members of the CARDIA Endpoints Surveillance and Adjudication Subcommittee (ESAS) reviewed each record, applying standard outcome definitions to classify events; disagreements were resolved by the full CARDIA ESAS Committee.
Covariates
Age (years), race (Black or White), sex (male or female), smoking status (never, former, or current smoker), alcohol use (mL of alcohol consumed/day), educational attainment (highest grade of school completed), and family history of CVD (yes or no) were reported through questionnaire. Based on previous literature and causal directed acyclic graphs, these variables were considered potential confounders for the association between physical activity and CVD [11, 12]. Body mass index (BMI) was calculated based on measured height and weight at each examination. Blood pressure (hypertension) and fasting laboratory measures (glucose and cholesterol) were measured at each examination. BMI, hypertension, diabetes, and dyslipidemia were considered potential mediators for the association between physical activity and CVD based on previous literature and directed acyclic graphs [11, 12, 23].
Statistical analysis
Summarizing physical activity
Physical activity trajectories were modeled among all CARDIA participants. A linear mixed model (LMM) for repeated measures of physical activity was used to generate concise summaries of exercise patterns over time [11, 12]. The physical activity slopes consisted of all observations of the physical activity scores before CVD event onset with the goal of using as much of the data per participant as possible and to stabilize the best linear unbiased predictions. The LMM had fixed effects for a four-level categorization of sex and race, continuous age, and their interactions, as well as random effects for participant and age, with unstructured covariance. We calculated expected physical activity level at age 18 and annual change for each participant from the fixed and random effects estimates the model provided. In order to capture the associations of lower level and faster decline in physical activity with increased CVD event risk and for easy interpretation, we changed the sign of both summaries.
Modeling the association of lower physical activity with incident CVD events
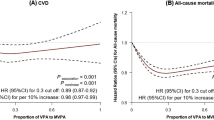
Unadjusted cumulative incidence of CVD events (coronary heart disease, congestive heart failure, and stroke) by sex and race/ethnicity was estimated using Kaplan-Meier methods [24]. We then expanded the data for each participant to include a record of each age between study entry and either metabolic disease onset, which was assumed to occur at the first visit at which it was detected, or at censoring by the end of the study of loss to follow-up. We used three sets of pooled logistic models to estimate the independent associations of the expected physical activity at age 18 and ensuing annual change with incidence of premature CVD events: adjusting for age (Model 1); adjusting for potential confounders including sex, race, family history of CVD, income, years of education, smoking status, and alcohol use (Model 2) [15]; and adjusting for all confounders in Model 2, as well as potential mediators, including BMI, hypertension, diabetes, and dyslipidemia (Model 3) [23]. Given the importance of age as a confounder for physical activity and CVD, we did not present unadjusted models. Smoking status, alcohol use, BMI, hypertension, diabetes, and dyslipidemia were time varying, with the last observation carried forward. We tested if sex and race modified the effect of physical activity (level and change) on incident premature CVD events. Pooled logistic models estimated the associations of various physical activity guideline thresholds (exceeding 2x minimum guidelines [> 600 EU], 1-2x minimum guidelines [300–600 EU], or below guidelines [< 300 EU]) at age 18 and through follow-up with onset of CVD events. We used Stata 16.0 (Statacorp, College Station, TX) for all analyses. Sensitivity analyses are listed in the Supplemental Appendix.
Results
Baseline demographic and health characteristic data of the 5114 participants (51.6% Black and 45.5% male) included in the sample are displayed in Table 1. Figure 1 portrays the decline in average physical activity from young adulthood in all race and sex groups. Supplemental Figs. 1-4 show the cumulative incidence of premature CVD events by race and sex.
Pooled logistic regression model estimates for the associations between premature CVD event incidence and the two physical activity summaries (physical activity level at age 18 and subsequent declines in physical activity) are shown in Table 2. Model 1 adjusted for age only whereas Model 2 adjusted for race, sex, education, income, family history of CVD, smoking status, and alcohol in addition to age. Model 2, the fully adjusted model, indicates the association between lower physical activity score (per 100 units) at age 18 and the higher odds of incident CHD (14%), heart failure (21%), stroke (20%), and any CVD (15%). Each additional annual 1 EU reduction in the physical activity score was associated with a higher annual odds of incident heart failure (7%), stroke (6%), and any CVD (4%). Sex and race categories did not modify the effect of physical activity (level and change) on incident CVD events (all p > 0.05). Sensitivity analyses are shown in the Supplemental Appendix.
In models including potential mediators such as BMI, hypertension, diabetes, and dyslipidemia (Table 2, Model 3), the association between physical activity and incident CVD events was attenuated. In particular, these factors mediated 41% of the total effect of physical activity at age 18 and 59% of the total effect of the annual reduction in physical activity on incident CVD events. When adding each potential mediator (BMI, hypertension, diabetes, and dyslipidemia) to the model separately (Appendix D), diabetes accounted for the highest percent of the total effect mediated (24% for physical activity at age 18 and 38% for annual reduction in physical activity).
Table 3 shows associations with various physical activity guideline thresholds (> 600 EU or 300–600 EU vs < 300 EU) at age 18 and through follow-up with onset of CVD events. Meeting the minimum HHS physical activity guidelines (300–600 EU, OR 0.69) and twice the minimum HHS guidelines (> 600 EU, OR 0.60) at age 18 was associated with lower odds of any premature CVD events compared to not meeting the minimum HHS guidelines. Meeting the minimum HHS physical activity guidelines (OR 0.74) and twice the minimum HHS guidelines (OR 0.55) from young adulthood to middle age (estimated physical activity level from linear mixed model was always above the threshold over the 30-year follow-up period) was associated with lower odds of any premature CVD events compared to not meeting the minimum HHS guidelines.
Discussion
In this prospective cohort study with 30-years of follow-up, we found that a high level of physical activity during young adulthood is a crucial starting point for preventing premature CVD events before age 60. Physical activity in young adults is associated with lower incidence of premature CVD events, specifically heart failure and stroke events, independent of physical activity later in adulthood. In addition, for any given young adult physical activity set-point, decline in physical activity through the adult life course is also associated with incident premature heart failure and stroke events. Thus, it is important to maintain high levels of physical activity throughout the adult life course. While meeting the minimum HHS physical activity guidelines of 150 minutes of moderate-intensity physical activity per week at age 18 and through the adult life course was protective of premature CVD events, meeting twice the minimum HHS guidelines was even more protective of premature CVD events.
Our study builds upon prior research linking physical activity to subsequent CVD events [2,3,4], but expands on this literature by examining trajectories with 30-years of follow-up from young to middle adulthood and also examining premature CVD events prior to age 60. The 2018 HHS Physical Activity Guidelines Scientific Advisory Committee concluded there was insufficient evidence that the association between physical activity and CVD events varied by age group, with a particular evidence gap for young adults [5]. We found physical activity levels in young adulthood are protective of premature heart failure and stroke events. Examining the various guideline thresholds, we found meeting both the current recommended minimum levels and twice the recommended minimum levels of moderate physical activity at age 18 and through midlife were protective of premature CVD events before age 60.
Several potential mechanisms may explain the link between physical activity and fewer premature CVD events. We found, collectively, that diabetes, BMI, hypertension, and dyslipidemia mediate 41–59% of the association between physical activity and CVD events, with diabetes as the largest contributor. Physical activity may improve inflammatory and metabolic factors which could protect from premature CVD [23]. High levels of physical activity in young and middle adulthood are protective of incident hypertension [11], which could be particularly implicated in the prevention of stroke events. It is notable that both physical activity level and slope were independently associated with premature heart failure and stroke event onset, even after adjusting for several potential sociodemographic and behavioral confounders.
Our findings indicate that young adult physical activity levels provide protection from subsequent premature CVD events, independent of physical activity levels up through midlife. Therefore, young adults may be an important target for interventions to ensure adequate physical activity levels. We find that physical activity declines, on average, during young adulthood in all race and sex groups, consistent with previous literature [6,7,8]. Educational, economic, and social transitions such as starting college, entering the workforce, or becoming parents during young adulthood may lead to fewer opportunities for organized or leisure time physical activity [25, 26].
Disparities in physical activity and premature CVD events across race and sex are noteworthy over the 30-year follow-up period. Black women reported the lowest physical activity levels from young adulthood through midlife. While young men start with high average physical activity levels, these levels persistently decline through young adulthood, with further declines among Black men through midlife, similar to previously reported patterns [21, 27]. In terms of disparities in premature CVD events, we found that Black populations had the highest incidence of premature heart failure and stroke events while men had the highest incidence of premature CHD events, similar to known race disparities in CVD including CHD and stroke [1, 28, 29]. Despite these disparities, we did not find evidence of effect modification by race or sex in the association between physical activity and premature CVD events. This finding of no effect modification by race or sex also contributes to an HHS-articulated gap for the Physical Activity Guidelines for Americans Scientific Report [5]. The benefits of physical activity to prevent premature CVD do not differ by race or sex which indicates that disparities in premature CVD events are likely due to other factors such as social determinants of health.
Clinical perspectives
Clinicians should assess for and promote physical activity at health maintenance visits. Despite evidence of the feasibility, validity, and effectiveness of assessing and promoting physical activity in clinical settings, physical activity is less routinely assessed in clinical practice compared to smoking, obesity, blood pressure, glucose, and lipid profiles [30], though CVD risk associated with physical inactivity is comparable to smoking [31]. Messaging promoting optimizing health, rather than the need to avoid risk, may better evoke responses from young adults [32]. Young adults may be more prone to taking on immediate risks (e.g. not being physically active) if they believe the outcome related to the counseling is far in the future; this is an instance of the concept referred to as temporal discounting [33]. The urgency of high levels of physical activity in young adulthood is emphasized by our finding that physical activity may prevent premature CVD events, including death before age 60.
Physical activity interventions at universities [34], workplaces [35], community organizations [36, 37], and faith-based organizations [38] may promote physical activity among young and middle-aged adults. Digital interventions including social media, text messages, e-mails, games, and multicomponent interventions, may hold future promise for promoting physical activity especially among young adults [39]; however, further research on and development of digital interventions for promoting physical activity is required.
Limitations and strengths
The CARDIA Physical Activity History does not directly quantify duration and frequency within activity categories and was based on self-reported data, which may be subject to information bias, including recall (12-month recall) and prevarication bias. Social desirability bias may lead to inflation of the self-reported physical activity and limit generalizability. Nonetheless, repeated measures of the same physical activity measure were collected in 2–5-year intervals across the 30-year follow-up period, which is a unique strength. The sampling design of CARDIA was not representative of all races or ethnicities in the US, which may limit generalizability; however the study specifically focused on participants identifying as Black or White race [13]. While we adjusted for several potential confounders including age, sex, race, education, family history, smoking status, and alcohol, there is the possibility of unmeasured confounders. Given the small proportion of the sample with premature CVD events by age 60, we may have been underpowered to detect associations with some of the individual premature CVD event outcomes, particularly with the guideline threshold analyses. Future research examining these outcomes later in adulthood, when CVD event outcomes become more common, may have greater power to inform various guideline level thresholds.
Conclusion
In conclusion, low physical activity levels in young adulthood and declining physical activity in later adulthood are each significantly and independently associated with premature CVD events before age 60. Clinicians and public health programs should emphasize, prioritize, and develop interventions to promote physical activity across the lifespan, including young adulthood, which is an important time when individuals establish physical activity lifestyle behaviors for the rest of their life course. Regardless of young adult physical activity level, sustained or increased physical activity later in midlife can also prevent premature CVD events and death.
Availability of data and materials
Data from the Coronary Artery Risk Development in Young Adults Study may be accessed through a manuscript proposal or ancillary study proposal (details at https://www.cardia.dopm.uab.edu/invitation-to-new-investigators).
Abbreviations
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
- CVD:
-
Cardiovascular disease
- CARDIA:
-
Coronary Artery Risk Development in Young Adults Study
- EU:
-
Exercise units
- HHS:
-
Department of Health and Human Services
- LMM:
-
Linear mixed model
- MET:
-
Metabolic equivalent
- US:
-
United States
References
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–596.
Arem H, Moore SC, Patel A, Hartge P, de Gonzalez AB, Visvanathan K, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015;175:959–67.
Shah RV, Murthy VL, Colangelo LA, Reis J, Venkatesh BA, Sharma R, et al. Association of fitness in young adulthood with survival and cardiovascular risk: the coronary artery risk development in Young adults (CARDIA) study. JAMA Intern Med. 2016;176:87–95.
White DK, Gabriel KP, Kim Y, Lewis CE, Sternfeld B. Do short spurts of physical activity benefit cardiovascular health? The CARDIA study. Med Sci Sports Exerc. 2015;47:2353–8.
2018 Physical Activity Guidelines Advisory Committee. 2018 physical activity guidelines advisory committee scientific report. Washington, DC: U.S. Department of Health and Human Services; 2018.
Schmitz KH Jr, DRJ, Leon AS, Schreiner PJ, Sternfeld B. Physical activity and body weight: associations over ten years in the CARDIA study. Coronary artery risk development in Young adults. Int J Obes Relat Metab Disord. 2000;24:1475–87.
Li K, Haynie D, Lipsky L, Iannotti RJ, Pratt C, Simons-Morton B. Changes in moderate-to-vigorous physical activity among older adolescents. Pediatrics. 2016;138:e20161372.
Kwon S, Janz KF, Letuchy EM, Burns TL, Levy SM. Developmental trajectories of physical activity, sports, and television viewing during childhood to young adulthood: Iowa bone development study. JAMA Pediatr. 2015;169:666–72.
Eijsvogels TM, Thompson PD. Exercise is medicine: at any dose? Jama. 2015;314:1915–6.
Eijsvogels TM, Thompson PD. Are there clinical cardiac complications from too much exercise? Curr Sports Med Rep. 2017;16:9–11.
Nagata JM, Vittinghoff E, Pettee Gabriel K, Garber AK, Moran AE, Sidney S, et al. Physical activity and hypertension from Young adulthood to middle age. Am J Prev Med. 2021;60:757–65.
Nagata JM, Vittinghoff E, Gabriel KP, Garber AK, Moran AE, Rana JS, et al. Moderate-to-vigorous intensity physical activity from young adulthood to middle age and metabolic disease: a 30-year population-based cohort study. Br J Sports Med. 2022;56(15):847–53.
Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, et al. Cardia: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–16.
Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, et al. A collection of physical activity questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 Suppl):1.
Laddu DR, Rana JS, Murillo R, Sorel ME, Quesenberry CP Jr, Allen NB, et al. 25-year physical activity trajectories and development of subclinical coronary artery disease as measured by coronary artery calcium: the coronary artery risk development in Young adults (CARDIA) study. Mayo Clin Proc. 2017;92:1660–70.
Sidney S, Jacobs DR, Haskell WL, Armstrong MA, Dimicco A, Oberman A, et al. Comparison of two methods of assessing physical activity in the coronary artery risk development in young adults (CARDIA) study. Am J Epidemiol. 1991;133:1231–45.
Jacobs DR, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and reliability of short physical activity history: CARDIA and the Minnesota heart health program. J Cardpulm Rehabil. 1989;9:448–59.
U.S. Department of Health and Human Services. Physical activity guidelines for Americans, 2nd Edition. 2018.
Gabriel KP, Sidney S, Jacobs DR, Quesenberry CP, Reis JP, Jiang S-F, et al. Convergent validity of a brief self-reported physical activity questionnaire. Med Sci Sports Exerc. 2014;46:1570–7.
Jacobs DR, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25:81–91.
Gabriel KP, Sidney S, Jacobs DR, Whitaker KM, Carnethon MR, Lewis CE, et al. 10-year changes in accelerometer-based physical activity and sedentary time during midlife: CARDIA study. Am J Epidemiol. 2018;187:2145–50.
Sternfeld B, Gabriel KP, Jiang S-F, Whitaker KM, Jacobs DR, Quesenberry CP, et al. Risk estimates for diabetes and hypertension with different physical activity methods. Med Sci Sports Exerc. 2019;51:2498–505.
Hamer M, Stamatakis E. Physical activity and risk of cardiovascular disease events: inflammatory and metabolic mechanisms. Med Sci Sports Exerc. 2009;41:1206–11.
Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Regression methods in biostatistics: linear, logistic, survival, and repeated measures models. 2nd ed. New York: Springer-Verlag; 2012.
Kwan MY, Cairney J, Faulkner GE, Pullenayegum EE. Physical activity and other health-risk behaviors during the transition into early adulthood: a longitudinal cohort study. Am J Prev Med. 2012;42:14–20.
Bellows-Riecken KH, Rhodes RE. A birth of inactivity? A review of physical activity and parenthood. Prev Med. 2008;46:99–110.
Armstrong S, Wong CA, Perrin E, Page S, Sibley L, Skinner A. Association of Physical Activity with Income, race/ethnicity, and sex among adolescents and Young adults in the United States: findings from the National Health and nutrition examination survey, 2007-2016. JAMA Pediatr. 2018;172:732–80.
Gerber Y, Rana JS, Jacobs DR, Yano Y, Levine DA, Nguyen-Huynh MN, et al. Blood pressure levels in Young adulthood and midlife stroke incidence in a diverse cohort. Hypertension. 2021;77:1683–93.
Shah NS, Molsberry R, Rana JS, Sidney S, Capewell S, O’Flaherty M, et al. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999-2018: observational analysis of vital statistics. BMJ. 2020;370.
Lobelo F, Rohm Young D, Sallis R, Garber MD, Billinger SA, Duperly J, et al. Routine assessment and promotion of physical activity in healthcare settings: a scientific statement from the American Heart Association. Circulation. 2018;137:e495–522.
Rana JS, Liu JY, Moffet HH, Karter AJ, Nasir K, Solomon MD, et al. Risk of atherosclerotic cardiovascular disease by cardiovascular health metric categories in approximately 1 million patients. Eur J Prev Cardiol. 2021;28:e29–32.
Gooding HC, Milliren C, Shay CM, Richmond TK, Field AE, Gillman MW. Achieving cardiovascular health in young adulthood-which adolescent factors matter? J Adolesc Health. 2016;58:119–21.
de Water E, AHN C, Scheres A. Distinct age-related differences in temporal discounting and risk taking in adolescents and young adults. Child Dev. 2014;85:1881–97.
Brown DMY, Bray SR, Beatty KR, Kwan MYW. Healthy active living: a residence community-based intervention to increase physical activity and healthy eating during the transition to first-year university. J Am Coll Heal. 2014;62:234–42.
Jirathananuwat A, Pongpirul K. Promoting physical activity in the workplace: a systematic meta-review. J Occup Health. 2017;59:385–93.
Garbers S, Hunersen K, Nechitilo M, Fisch M, Bell DL, Byrne MW, et al. Healthy weight and cardiovascular health promotion interventions for adolescent and Young adult males of color: a systematic review. Am J Mens Health. 2018;12:1328–51.
Deatrick JA, Klusaritz H, Atkins R, Bolick A, Bowman C, Lado J, et al. Engaging with the community to promote physical activity in urban neighborhoods. Am J Health Promot. 2019;33:718–26.
Lemacks JL, James RE, Abbott L, Choi H, Parker A, Bryant A, et al. The church bridge project: an academic–community perspective of a church-based weight management pilot intervention among young adult African Americans. Prog Comm Heal Partnerships Res Educ Action. 2018;12(1S):23–34.
Rose T, Barker M, Maria Jacob C, Morrison L, Lawrence W, Strömmer S, et al. A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. J Adolesc Health. 2017;61:669–77.
Acknowledgements
The authors thank Samuel Benabou, Sanya Dhama, Ananya Rupanagunta, and Anthony Kung for editorial assistance. The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I & HHSN268201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). This manuscript has been reviewed by CARDIA for scientific content. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Institutes of Health or the U.S. Department of Health and Human Services.
Funding
JMN is supported by the National Institutes of Health (K08HL159350) and the American Heart Association (CDA34760281). KBD is supported by the National Institutes of Health (K24DK103992).
Role of the Funding Bodies: The funders had no role in the design of the study, analysis, interpretation of data, or decision to submit the results.
Author information
Authors and Affiliations
Contributions
JMN conducted the literature search, interpreted findings, and wrote, revised, and edited the manuscript. EV conceptualized the study, analyzed data and edited the manuscript. KPG, SS, AKG, KBD conceptualized the study, interpreted the data and provided critical revisions on the manuscript. AEM, JSR, CEL and JPR provided critical revisions on the manuscript. All authors approved the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review boards at each study site (Kaiser Permanente [CN-98SSidn-03-H], Northwestern University [STU00024971-MOD0007], University of Minnesota [8304 M00575], and University of Alabama at Birmingham [F990825030]) approved study procedures. All participants provided written informed consent. The institutional review board at the University of California, San Francisco deemed this secondary data analysis project exempt (IRB 18–26523).
Consent for publication
Not applicable.
Competing interests
The authors declare that they do not have conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nagata, J.M., Vittinghoff, E., Gabriel, K.P. et al. Physical activity from young adulthood to middle age and premature cardiovascular disease events: a 30-year population-based cohort study. Int J Behav Nutr Phys Act 19, 123 (2022). https://doi.org/10.1186/s12966-022-01357-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-022-01357-2