Abstract
Prostate cancer, as one of the most prevalent malignancies in males, exhibits an approximate 5-year survival rate of 95% in advanced stages. A myriad of molecular events and mutations, including the accumulation of oncometabolites, underpin the genesis and progression of this cancer type. Despite growing research demonstrating the pivotal role of oncometabolites in supporting various cancers, including prostate cancer, the root causes of their accumulation, especially in the absence of enzymatic mutations, remain elusive. Consequently, identifying a tangible therapeutic target poses a formidable challenge. In this review, we aim to delve deeper into the implications of oncometabolite accumulation in prostate cancer. We center our focus on the consequential epigenetic alterations and impacts on cancer stem cells, with the ultimate goal of outlining novel therapeutic strategies.
Graphical Abstract

Similar content being viewed by others
Oncometabolites and their impact on the epigenetic landscapes of prostate cancer
Overview of prostate cancer
The prostate is the largest accessory gland in the male reproductive system, consisting of tubulo-alveolar glands. It comprises a glandular epithelium of variable height and a stroma containing connective tissue and smooth muscle. In the adult male, the prostate is divided into four zones with different relative content in epithelial and stromal cells. Only 25% of the surface in the central zone comprises epithelial glands, while the peripheral zone contains more than 70% of epithelial tissue. The transitional and periurethral zone have few secretory tissues although they undergo extensive proliferation in older individuals [1]. Prostate cancer (PC) is a significant global health concern, predominantly affecting the older male population. It develops in the prostate, a small walnut-shaped gland in men that produces seminal fluid to nourish and transport sperm. The cancer usually grows slowly and initially remains confined to the prostate gland, where it may not cause serious harm [2]. While some types are slow-growing and may need minimal or even no treatment, other types are aggressive and can spread rapidly [3].
The most common type of PC is adenocarcinoma, making up about 99% of cases. Other subtypes include ductal adenocarcinoma, transitional cell (or urothelial) cancer, neuroendocrine cancer, and small cell prostate cancer [4]. Castration-resistant prostate cancer (CRPC) is a highly aggressive form of the disease that grows despite the level of male hormones (androgens) being suppressed to very low or undetectable levels in the body. It usually signifies that the cancer is resistant to traditional hormone therapy (also known as androgen deprivation therapy), making it significantly more challenging to manage [5,6,7].
The genetic underpinnings of prostate cancer are complex and multifactorial. Mutations in the BRCA1 and BRCA2 genes, often associated with breast and ovarian cancer risks, have been found to increase the likelihood of prostate cancer as well [8]. Prostate cancer pathogenesis is also influenced by the roles of specific oncogenes and epigenetic regulators, including ERG (ETS-related gene), which is a member of the ETS family of transcription factors, known for roles in development and various cancers, including prostate cancer [9] and EZH2 (Enhancer of Zeste Homolog 2), which is a part of the Polycomb group of proteins, functioning as a histone methyltransferase and playing a crucial role in gene silencing and epigenetic regulation [10]. Their interaction significantly impacts prostate cancer progression. Zoma et al. found that EZH2 methylates ERG at K362, enhancing transcription and, combined with PTEN loss, leads to invasive adenocarcinomas and CRPC progression [11]. Similarly, Xu et al. identified that EZH2 in CRPC acts as a coactivator for key transcription factors and this function is phosphorylation-dependent and necessitates an intact methyltransferase domain [12]. The TMPRSS2-ERG gene fusion event is another common genetic abnormality observed in a significant proportion of PC cases, [13]. This fusion product disrupts androgen receptor signaling and induces repressive epigenetic programs through the direct activation of EZH2 [14]. This molecular interplay between ERG and EZH2 underscores their importance in cancer progression and as targets for new therapies.
Epidemiologically, prostate cancer is the second most common cancer and the fifth leading cause of cancer-related death among men, with an estimated 1.41 million new cases and 375,000 deaths worldwide in 2019, according to the World Health Organization [4]. The prevalence is higher in developed countries, attributed largely to routine screening using prostate-specific antigen (PSA) tests [15]. Age, family history of the disease, and race are well-established risk factors for PC. Men of African descent are at a higher risk of developing prostate cancer compared to other races, and the disease is generally more aggressive in these men [16].
The progression of prostate cancer, similarly to many other types of cancer, is influenced by metabolic alterations in the tumor cells [17]. These changes allow cancer cells to adapt to their environment and to the availability of nutrients, enabling their survival and proliferation even under adverse conditions. Among the metabolic alterations seen in cancers, the accumulation of specific metabolites, referred to as 'oncometabolites', has emerged as a significant contributor to tumor progression [18]. This leads us to a deeper understanding of how prostate cancer develops and evolves, which we will explore in the next section, focusing specifically on the role of oncometabolites in tumor progression.
The understanding and management of prostate cancer have evolved significantly over the years. Today, due to enhanced screening methods and more effective treatments, survival rates for prostate cancer are generally high, particularly for localized forms of the disease [19, 20]. However, aggressive and late-stage forms, such as CRPC, present ongoing challenges that researchers are striving to address. The future of prostate cancer research involves a multidimensional approach, focusing on risk stratification, personalizing treatments, and continually developing novel therapies.
Role of oncometabolites in tumor progression
As mentioned above, among the hallmarks of cancers, metabolic alterations are emerging as one of the most intriguing and complex therapeutic targets [21, 22] due to the strict connections of the different metabolic pathways and the capacity of cancer cells to adapt their energetic requirements on nutrient availability and microenvironmental changes. Alterations of energetic metabolism are connected with several downstream pathways and regulatory mechanisms, including protein post-translational modifications, epigenetic variations, and intercellular crosstalk, corroborating the necessity to identify metabolic targets to specifically hit cancer cells, still keeping into consideration their plastic ability to change their energetic sources. In different tumor types, the accumulation of specific metabolites (called oncometabolites) has been reported, especially concerning three intermediates derived from the Krebs cycle, i.e., 2-hydroxyglutarate (2-HG), succinate, and fumarate. Historically, 2-HG has been the first identified oncometabolite; it is mainly produced by the mutated form of the enzyme isocitrate dehydrogenase (mutIDH1/2) [23] and it is structurally similar to α-ketoglutarate (α-KG), the physiological product of the wild-type IDH. Gain-of-function mutations of IDH have been identified in different tumor types, including gliomas, leukemia, chondrosarcoma, colon cancer, and prostate carcinoma [24]. Interestingly, 2-HG can be derived also from the promiscuous activity of some key metabolic enzymes, including malate dehydrogenase (MDH), lactate dehydrogenase (LDH) [25], and phosphoglycerate dehydrogenase (PHGDH) [26], and can accumulate in cancer cells in both its enantiomeric forms (i.e., D- and L-2HG). It has been reported that D-2HG is released by malignant cells and accumulated in the extracellular space, then it is taken up by T lymphocytes, limiting their capacity to mediate antitumoral immune response (Fig. 1) [27]. In addition to 2-HG, also high levels of succinate and fumarate have been shown to sustain cancer growth. For both, the cause is connected to alterations of the functionality of the relative enzymes, such as succinate dehydrogenase (SDH) and fumarate hydratase (FH), respectively, that include loss-of-function mutations, transcript degradation by miRNAs, post-translational modifications, and protein degradation. Concerning SDH, its loss-of-function mutations have been detected mainly in two rare tumors, such as paraganglioma and pheochromocytoma [24], and are generally frequent on the two subunits SDHB and SDHC, whereas only few mutations affect the other subunits (SDHA and SDHD) [28]. This enzyme is localized into mitochondria and acts in two crucial pathways of the energetic metabolism, such as the Krebs cycle and the electron transport chain, by converting succinate into fumarate, together with the reduction of flavin adenine dinucleotide (FAD) into FADH2. A blockage of SDH activity causes an accumulation of succinate, which then acts as an oncometabolite by activating signaling pathways, DNA hypermethylation, increase of reactive oxygen species (ROS) production, epithelial-to-mesenchymal transition (EMT), hypoxia-inducible factor (HIF)-1α stabilization, protein modification (such as succinylation) to sustain cancer progression (Fig. 1) [28]. Similarly, the accumulation of fumarate is generally caused by loss-of-function mutations of the relative enzyme FH, which converts fumarate into malate, and these mutations have been evidenced mainly in neuroblastoma and glioblastoma [24]. In addition, FH expression can be decreased by miRNA-378*. The results of the low activity of FH determine the increased level of fumarate supporting cancer spread through metabolic reprograming, post-translational modifications (succination), DNA fragmentation and hypermethylation, increase of ROS levels and EMT (Fig. 1) [28].
Otto Warburg won the Nobel Prize in 1931 for his discovery of the increased glycolytic rate of cancer cells accompanied by high levels of lactate production, even in presence of oxygen. Recently, due to its abundance in tumor specimens and to its capacity to influence cancer cell metabolism, lactate has also been categorized as an oncometabolite. Indeed, environmental lactate not only acts as a metabolic by-product, but it can be uploaded by lung, prostate, and pancreatic cancer cells in order to support metabolic pathways, including fatty acid metabolism [29,30,31]. In uveal melanoma, it has been demonstrated that lactate supplementation to in vitro cultured cells increases the mRNA expression of factors involved in mitochondria biogenesis and activity, suggesting a metabolic shift towards an oxidative metabolism [32]. In addition, in the same paper, the authors showed that the expression of monocarboxylate transporter (MCT), such as MCT1 and MCT4, are increased by lactate, along with a boost in oxidative phosphorylation (OXPHOS) activity, supporting a quiescent state and a reduced proliferation. However, other data are necessary to further corroborate this mechanism. A crucial role of lactate accumulation in cancer cells has been demonstrated regarding its ability to induce expression of anti-inflammatory and proangiogenic genes, together with the modification of histones through a process called “lactylation”, where a lactyl-CoA is added to lysine residues present in the tails of histones [33]. This epigenetic alteration results in cancer progression, drug resistance [34], metastasis and stemness induction [35, 36], metabolic alterations by affecting enzymes involved in the tricarboxylic acid cycle (TCA), and carbohydrate, amino acid, fatty acid, and nucleotide metabolism [35], hence opening the way to the generation of novel therapeutic strategies against lysine lactylation, not only regarding histones (Fig. 1) [36]. Finally, it is worth noting that other metabolic intermadiates or biochemical molecules may accumulate in cancer cells [37], thus emerging as other possible oncometabolites, hence maintaing open the inclusion in this class of pro-cancer molecules.
Role of oncometabolites in modulating the epigenetic landscape of cancer cells
Concerning the epigenetic alterations associated with oncometabolites, it has been shown that D-2HG accumulation, an event that is coupled with α-KG depletion, inhibits histone lysine demethylases (KDMs), giving rise to histone hypermethylation, epigenetic programming, and acquisition of additional mutations [27]. Furthermore, since 2-HG is structurally similar to α-KG, it competitively inhibits some α-KG-dependent dioxygenases, including the ten eleven translocation enzymes (TETs) and the Jumonji family of histone lysine demethylases, giving rise to DNA and histone hypermethylation [38, 39]. Some evidence about the capacity of succinate to regulate the epigenetic pattern of cancer cells have also been reported. Indeed, it has been shown that the acetylation of SDHA causes its deactivation, which in turn leads to activation of H3K4me3 activation, accompanied by change in tumor-specific gene expression [40]. In addition, other authors showed epigenetic inactivation of tumor suppressor genes, specifically HIC1, DcR1, DcR2 and CASPS8, due to succinate accumulation in SDH-mutated head and neck paragangliomas [41]. Concerning fumarate, instead, it has been reported a connection between it and chromatin remodeling factor lymphoid-specific helicase (LSH) in patients with nasopharyngeal carcinoma (NPC). Indeed, the authors showed that the subsequent chromatin modification has a key role in the determination of epithelial–mesenchymal transition, by conferring potent metastatic potential to cancer cells [42]. Interestingly, it has been recently demonstrated that also lactate accumulation influences the epigenetic pattern of cancer cells, in particular prostate cancer. Indeed, it has been shown that the inhibition of both the lactate transporter MCT1 and the key enzyme at the basis of lipid biosynthesis, i.e., the ATP citrate lyase (ACLY), strongly reduce the intracellular levels of acetyl-CoA, bringing the authors to the suggestion that lactate produced by cancer-associated fibroblasts (CAFs) represents the main source of acetyl-CoA in lipid-reprogrammed prostate cancer cells. Since lipid-derived Acetyl-CoA is one of the major sources of carbons for histone acetylation, the authors also showed that exogenous lactate induces increased levels of specific histones acetylation (in particular H3K9 and H3K27) that correlate with an open state of the chromatin, suggesting an active gene transcription. These interesting results are further supported by the evidence that lactate derived from CAFs enters inside cancer cells and activates this epigenetic process, highlighting that the interplay between CAFs and cancer cells is crucial and that CAFs act as key players in the dysregulation of metabolite accumulation [29].
Impact of oncometabolites on prostate cancer progression and prognosis
Due to the impact of oncometabolites in cancers, different studies have been focused on their role in prostate cancer (Table 1). Starting from one of the first studies on this topic, it has been demonstrated that missense mutations on codon 132 in IDH1 gene are present in different tumor types diverse than glioblastoma multiforme or gliomas, including prostate carcinomas [43], opening the way to the investigation of the role of 2-HG also in this tumor type. Indeed, thereafter, many papers showed the effect of IDH mutation, and thus 2-HG production, on prostate cancer cells. Among these, it has been demonstrated that the TET family of α-KG dioxygenases catalyzes the oxidation of 5-methylcytosine to 5-hydroxymethylcytosine correlating with DNA demethylation. Interestingly, TET2 is considered as a tumor suppressor gene and its enzymatic activity is inhibited in IDH-mutated tumors by the accumulation of 2-HG; this is further connected with the low levels of 5-methylcytosine oxidation that sustains cancer development, including prostate [44]. Another interesting evidence has been reported about the link of IDH mutation on codon 132 or of 2-HG high levels and the higher cell invasion capacity of prostate cancer cells negative for the androgen receptor (AR); indeed, the authors showed that when AR is expressed it reverses the pro-tumorigenic effect of 2-HG via transforming growth factor (TGF)β1 and circRNA-51217 [45].
Concerning succinate, a lower number of studies are present in the literature. In one of these, the authors reported that after the therapeutic inhibition of AR, there is a metabolic shift in the regulation of energy metabolism, highlighted by lower levels of SDH activity, correlating with succinate accumulation. Hence in this scenario, a therapeutic approach could also have a negative loop effect by causing an accumulation of a molecule that could work oppositely respect to the beneficial effect of the drug [46]. Moreover, also the anti-oxidant enzyme superoxide dismutase 2 (SOD2) has been shown to be indirectly involved also in the sustainment of succinate accumulation through a decreased activity of SDH and, intriguingly, an enhanced expression of Glut1 and glucose uptake in prostate cancer models [47], however these evidence need further validations in other biological systems. In this frame, CAFs and succinate accumulation has been reported play a key role in the context of prostate cancer. Indeed, CAFs establish a metabolic connection with prostate cancer cells, through lactate shuttle and thus contributing to cancer aggressiveness. Specifically, it has been shown that lactate uptake by cancer cells alters the NAD+/NADH ratio, followed by sirtuin (SIRT)1-dependent peroxisome proliferator-activated receptor gamma coactivator (PGC)-1α activation and subsequent increase of mitochondrial mass and activity. This scenario is then reflected on the deregulation of Krebs cycle, accumulation of oncometabolites, downregulation of complexes II-III, and accumulation of ROS. In addition, the authors also showed that CAFs stimulated prostate cancer cells to invade and that CAFs conditioned media significantly enhanced malate, citrate, fumarate and succinate levels (not 2-HG) [48].
Three other types of metabolic alterations have been demonstrated in prostate cancer cells: i) increased levels of urea cycle intermediates, including arginine-succinate, arginine, and fumarate in prostate cancer cells in comparison to benign controls [49]; ii) overproduction of γ-aminobutyric acid (GABA) suggesting that the GABA shunt, particularly glutamate decarboxylase (GAD)65, may represents a molecular target in the treatment of castrate-resistant prostate cancer [50]; iii) the accumulation of a derivate of the amino acid glycine, i.e. N-methyl-glycine, also called sarcosine, which has been shown to accumulate in prostate neoplastic cells acting as an apoptotic inhibitor [51] and as an epigenetic modifier [52], thus representing a potential biomarker for the diagnosis of this cancer in the early stage [53]. Finally, in a pilot study it has been shown that, by analyzing the urine of 101 patients with prostate cancer, the concentration of sarcosine, together with ethanolamine, kynurenine, b-alanine, and isoleucine, is significantly different respect 52 control individuals, representing new potential markers for cancer detection and prognosis [54]. This aligns with the findings that activation of the PTEN-PI3K-mTORC1 pathway in prostate cancer leads to metabolic alterations in polyamine synthesis and decarboxylated S-adenosylmethionine (dcSAM) production, further underscoring the potential of metabolic markers in cancer detection and evaluation [37].
Oncometabolites and epigenetic regulation in cancer stem cells (CSCs) and EMT
Cancer stem cells in the context of prostate cancer
Despite prostate cancer usually grows slowly without spreading outside the gland, there are also more aggressive forms, in which cancer cells rapidly invade the surrounding tissues and can additionally spread to other organs. Some studies have therefore focused on the investigation of this particular and delicate clinical condition, until the discovery in 2005 by Collins and colleagues of prostate cancer stem cells (PCSCs) [55] insights into the understanding and nature of these cells have followed since then. Cancer stem cells are extremely rare within the tumor, indeed they represent only the 0.1–1% of the bulk of the malignant mass and possess specific peculiarities. Among these, they show self-renew capacity and are able to differentiate into non-CSC progeny; they have high tumor-initiation capacity and display a strong resistance to chemo- and radio-therapy. In fact, standard therapies generally kill differentiated cancer cells, whereas cancer stem cells survive giving rise to metastasis. All these elements determine a worse clinical outcome for cancer pathology. As a matter of fact, it is now commonplace to think that the portion of patients with prostate cancer who are in a metastatic stage and who, above all, do not respond to hormonal therapy (considered a gold standard) are distinguished precisely by the presence of cancer stem cells [56]. This makes them one of the main targets in the development of new possible therapies for the treatment of patients to whom it is not possible to apply the classic treatment strategies nowadays. The cure and complete healing of prostate cancer still remains an incomplete success, but one that can be resolved by unmasking the intrinsic properties of PCSCs [56].
There are several types of cells in the prostate, each of which can transform and become cancerous; it therefore agrees that one of the main characteristics of this type of tumor is the relevant heterogeneity, which manifests itself in a range of different stadial degrees named Gleason grade and metastatic states [57]. In order to identify and analyze prostate cancer stem cells, specific markers have been established over the years that allow their isolation; among them, CD44, CD133, aldehyde dehydrogenase (ALDH), and androgen receptors are noteworthy but not the only ones. The origin of PCSCs is not yet well clear, although emerging data suggest the idea that they derive from prostate stem cells that undergo epigenetic modifications due to the presence of singular molecules released in the tumor microenvironment (TME) [58].
Role of EMT in prostate cancer progression and metastasis
One of the main traits for cancer cells is their attitude to undergo epithelial-to-mesenchymal transition, a well-recognized pathway implicated in the formation of CSCs. During this physiological event, cells decrease the expression of specific epithelial proteins and instead increase the expression of other mesenchymal specific proteins. This leads cells to lose tight and adherent junctions and detach from the basement membrane, consequently disrupting cell polarity; then, they migrate throughout the bloodstream and extravasate, colonizing secondary organs [59]. To do this, cells must undergo the opposite mechanism, which is the mesenchymal-to-epithelial transition (MET). Over last years, many papers demonstrated that also prostate cancer cells possess the propensity to undergo EMT program, endowing tumor with invasive traits that facilitate metastasis and variation in therapeutic responses [60]. In particular, it is emerging that androgen-independent metastatic phenotype, advanced prostate cancer and resistant immuno-phenotype patients are associated with the presence of PCSCs [61].
During the normal process of prostate formation, which occurs at embryonic level, it is normal to witness a dynamic plasticity between EMT and MET that allows the formation of the endodermal and mesodermal structures [62]. However, when some of the crucial signaling pathways that regulate these processes are significantly altered, patients undergo prostate tumorigenesis. First of all, the Wnt pathway, that generally affects cell survival, and in particular the Wnt family member 3 (Wnt3) seems to be involved in the increased expression of some typical stem markers like CD133 and CD44 [63,64,65]. The Hedgehog signaling pathway orchestrates cell renewal and survival, and its abnormal regulation has been found in prostate cancer cells and in PCSCs [66, 67], correlating with poor survival because of high grade of metastasis. Interestingly, also Notch pathway is regulated in prostate cancer; indeed, recent data show that it alters the correct signaling of both phosphoinositide 3-kinase (PI3K)/Akt pathway and AR pathway, which coordinate carcinogenesis [68], EMT, metastasis and cancer progression in this tumor type [69,70,71,72]. A final pathway that is altered in prostate cancer is nuclear factor kB (NF-kB) signaling pathway, which is correlated with a complex clinical case since it appears to have an important role in the regulation of progression, in the formation of metastases, and also in resistance to therapies [73, 74]. Further studies need to be performed to deeply investigate this topic which appears to be as crucial and equally important as those previously mentioned.
Since important pathways are significantly altered during EMT, one of the approaches that is emerging recently is the search for specific markers involved in the aforementioned pathways in order to use them as targets not only in patient screening, to better understand in which tumor stage are classified, but also as therapeutic targets to improve life expectancy even for those patients who are resistant to therapies and/or show relapses [75]. Moreover, in last years, in-depth studies on animal models have also been performed to further understand the effects that EMT and CSCs can have on prostate cancer [76], identifying eligible markers for possible future patient-specific treatments, in a historical moment in which the precision medicine seems to be the new frontier in the fight against cancer.
Influence of oncometabolites and epigenetic changes on CSCs and EMT
As previously stated, the complexity of tumors often lies in the high heterogeneity that characterizes it and which, among others, is due to the coexistence of cancer cells and cancer stem cells. In addition to this, the sophisticated molecular and metabolic plasticity that CSCs undergo makes the clinical profile more complex. The mechanisms underlying this fluidity can be traced back to epigenetic alterations that provide a reversible and rapid switch in gene expression, in response to developmental and microenvironmental signals, as well as to hypoxic conditions [77,78,79]. These events trigger the alteration of specific oncogenes; these genes can be functional and active during physiological conditions, producing normal amounts of metabolites. Their upregulation, as a consequence of epigenetic modifications, can result in an overabundance of key metabolites, known as oncometabolites, and lead to tumorigenesis. In fact, in addition to acting as signal molecules in TME, they also act on signaling pathways which in turn orchestrate both the expression of stem traits and their intracellular abundance in a metabolic loop. This metaboloepigenetic rewiring is called “metabostemness” [80]. In detail, epigenetic modifications lead to mutations on enzymes involved in metabolic pathways (among which the best noted are SDH, FH, and IDH) which in turn cause the accumulation of oncometabolites (as mentioned before, succinate, fumarate, and 2-hydroxyglutarate) that stimulates alterations in DNA and histone modifications [28]. Each of the above oncometabolites regulates certain signaling pathways, including those regulating stemness and the EMT program. For example, succinate and fumarate inhibit TETs, important methylcytosine dioxygenases that not only demethylate DNA but also suppress specific microRNAs that usually inhibit EMT program [81]; this interference causes a constant activation of epithelial-to-mesenchymal transition and an increased expression of Zeb1, which has been identified as a potential risk factor for recurrence and poor prognosis in several types of cancers [82, 83]. In the case of 2-hydroxyglutarate instead, it seems to induce an abnormal activity of telomerase reverse transcriptase (TERT), which in turn upregulates the transcription of important genes involved in stemness and tumorigenicity, including CD117, Oct4, and Sox2 [84, 85].
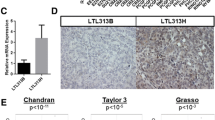
This complexity is further elucidated in a recent study by Giafaglione et al., which demonstrates that prostate epithelial cells, specifically basal and luminal types, possess unique metabolomes and nutrient patterns, fundamentally impacting their differentiation and response to treatment. These findings highlight the significant role of metabolic signaling in the regulation of prostate cancer progression, especially in the context of treatment resistance and lineage identity [86].
In recent years there have also been studies on possible link between some mutations found in patients with therapy-resistant prostate cancer, and a higher level of expression of genes involved in stemness, EMT and invasiveness [61]. These data are alarming but, at the same time, they also leave a glimmer of hope for the identification of markers and/or therapeutic targets that can help in the fight against this type of cancer (Table 2).
The impact of oncometabolites on the tumor microenvironment in prostate cancer
Elucidating the composition and metabolic function of the prostate cancer tumor microenvironment
The stroma of the human prostate is a dense connective tissue rich in smooth muscular cells with fibroblast, blood vessels, and nerves. There is no adipose tissue in the stroma, though the periprostatic adipose tissue of the prostate plays a fundamental role in the biology of the gland. In the mouse, the fibromuscular stroma is less prominent, and the epithelial tissue occupies most of the gland area [87].
Stromal cells are responsible for the growth and homeostasis of the epithelia. Also, they are responsible for extracellular matrix synthesis and turnover. The importance of the stroma in the normal gland functioning is obvious. Growth factors travel around and are stacked into the fibrous component of the extracellular matrix, the communication between stroma and epithelia is also relevant in the aging process of the gland. Aging changes matrix components and is characterized by increased pro-inflammatory cytokines that can contribute to age-associated pathologies such as benign prostate hyperplasia, prostatitis, and even prostate carcinoma [88]. In fact, cancer progression involves signals and interaction with other cell types different from tumor cells found in the neighboring tissue that embrace the tumor. In the prostate, epithelial cancerous tissues are surrounded by cells that produce factors that communicate and even regulate tumor cells [89].
The importance of TME in PC has made the number of studies focused on the metabolic crosstalk between cancer cells and the TME rapidly increase in the last few years. The TME maintains the metabolic requirements of PC cells in different ways: (1) by the production of many cytokines; (2) by secreting lactate; (3) by ensuring intracellular alkalinization of tumoral cells through bicarbonate secretion via carbonic anhydrase IX (CAIX) [90].
The unique metabolism of PC entails that the relevant oncometabolites in the TME differ from other carcinomas. In normal prostate, glycolysis is favored because of the inhibition of aconitase in the TCA cycle by zinc accumulation [91]. On the other hand, in the first steps of prostate carcinogenesis, tumor cells become citrate-dependent, increasing OXPHOS and lipogenesis. In the CRPC, choline, amino acid, and glycolytic metabolism are promoted more than OXPHOS [92]. Thus, the different metabolic requirements along PC progression alter the TME, being the mitochondria at the center of the crosstalk.
In PC, most published studies are based on the interaction of tumor cells with CAFs to promote cancer progression and aggressiveness. In healthy prostate stroma, fibroblasts play a fundamental role in the maintenance of the extracellular matrix (ECM), but acquire an activated state with tumor progression that resembles its role during the repair response in injured tissues. CAFs increase the production of EMC components and secrete growth factors and cytokines [93]. In the prostate stroma, they increase proliferation and begin to express α smooth muscle actin (α-SMA), a classical marker of myofibroblast [94]. CAFs are found in premalignant prostatic intraepithelial neoplasia (PIN), but they are significantly increased along with tumor progression [95, 96]. They express high levels of EMC proteins and show high mobility and a high proliferation rate similar to fibroblast during wound healing, but the main difference is that CAFs remain in the stroma of the TME [97]. This situation maintains oncogenic signals, including soluble factors produced by themselves or by modifying the availability of oncogenic molecules bound to the ECM components. The origin of CAFs remains unclear, and some propose that they derive from the activation of resident fibroblast [98, 99], from recruited bone marrow progenitors [100], or the transdifferentiation from endothelial [101, 102] or epithelial to mesenchymal [103].
CAFs show a secretory phenotype that enhances the proliferation and invasion of prostate cancer cells in vitro. However, though in vivo, CAFs have been positive or negative for tumor growth, depending on the study. The role of CAFs in grafting-initiated prostate epithelium has been shown [104, 105]. The role of CAFs is to stimulate the cancer cells. They contribute to a permissive microenvironment that favors angiogenesis, cell migration, matrix stiffening, and in turn invasive phenotypes [95, 96]. CAF-enriched microenvironment directly affects EMC integrity, promoting fibrosis, interstitial pressure, hypoxia and impairing the delivery of antitumor drugs.
On the other hand, proteases from CAFs degrade ECM components and free growth factors and cytokines that contribute to proliferation of cancer cells. Lastly, CAFs, through this microenvironment modulation, could be relevant in the immune population and reactivity surrounding the tumor cells, however their role in immunosuppression in prostate cancer is not yet clarified.
The second component in the prostate cancer microenvironment is tumor vasculature. Like many other solid tumors, the prostate has aberrant vasculature showing a lack of pericyte coverage, vascular leakiness, and aberrant morphology of vessels [106]. In normal prostate, vascular endothelial growth factor (VEGF) expression is restricted to stromal cells. However, in carcinoma, VEGF expression increases in tumor cells. Prostate cancer favors angiogenesis, and tumor-associated vasculature secretes an array of paracrine effectors that can contribute to the growth of several types of solid tumors [107]. Experimentally, it was demonstrated that human umbilical vein endothelial cells enhance the invasion of prostate cancer cells in vitro [108]. The integration of vascular niche in the prostate is affected by androgen deprivation therapy. Androgens withdrawal promotes the loss of vascular integrity, pointing to the possibility that the vascular component of the prostate microenvironment can be an important component of treatment-induced therapy resistance since some experiments have shown a transient loss of vascular integrity that is recovered after a time of androgen deprivation [109]
The changes in vascularization make the environment hypoxic and acidic [110]. In general, it was considered that tumor cells adapt their metabolism favoring glycolysis to have a selective advantage in a non-physiological atmosphere, being glucose considered as oncometabolite. However, glucose is not frequently viewed as oncometabolite in PC, except for metastases [111]. In fact, glucose deprivation promotes androgen signaling and increases resistance to radiation treatment [112, 113]. Lactate and fatty acids predominate over glucose as energetic fuel in PC cells.
Both CAFs and the vascular component of the TME live together with the immune cells of the prostate stroma. Inflammation is a cancer-promoting process in the prostate. Chronic infection and inflammation cause cancer in the prostate [114]. Also, the progression of prostate tumors is followed by the increment of immune cells in the stroma, mostly dendritic cells and macrophages. Macrophages have a complex role in cancer, but in the prostate, tumor-associated macrophages (TAM) are frequently correlated with poorer outcomes [115]. Macrophages interact with fibroblasts in normal tissues when tissue repair is necessary. TFG-β and other cytokines mediate this interaction. CAFs produce high levels of TFG-β that correlate with lower survival in prostate cancer patients. TFG-β also promotes the accumulation of regulatory T cells in the tumor prostate. Thus, the reciprocal relation between stromal components contributes to progression and creates an immunosuppressive microenvironment [89]. Histology evidence reflects that more than 80% of prostate human samples studied have immune infiltration, and this chronic inflammation contributes to prostate cancer development [116]. The composition of immune infiltrate varies with disease stage and patient age, but mostly, CD3+ T cells, CD4+ T cells, CD20+ B cells, and macrophages are found [117]. Other frequent cells that appear in the TME of the prostate are natural killers (NK), mast cells and neutrophils that, in addition to macrophages, constitute the most relevant immune components of the stroma of the prostate tumor. Immune cell function is finely regulated by nutrient availability, and targeting metabolic activity is a recurrent strategy for malignant cells to proliferate.
One of the major immunosuppressive components in the prostatic TME is the dedifferentiated myeloid-derived suppressor cells (MDSCs). These cells, coming from myeloid cells in the bone marrow, are highly heterogeneous and can also differentiate into endothelial cells, fibroblasts, tumor-associated macrophages (TAMs) [118], or osteoclasts [119]. Consequently, MDSCs play a critical role in forming the pre-metastatic niche. According to their morphology, MDSCs are subdivided into two major subsets: Monocytic (M-MDSCs) and granulocytic (G-MDSCs). Despite their heterogeneity, MDSCs metabolically share a Warburg effect exhibition, which limits glucose availability for immune cells and the production of inhibitory cytokines by increasing fatty acid oxidation (FAO). In addition, the promotion of the catabolism of some amino acids, such as arginine, tryptophan, and cysteine, by MDSCs impedes activation of T cells [120]. In PC, several studies have already described the presence of MDSCs to support tumor growth [121]. Interestingly, enzalutamide, an AR antagonist used in metastatic PC, promotes the immunosuppressive activity of MDSCs by reducing mitochondrial metabolism and increasing glycolysis, VEGF and Arg1 expression in a CRPC model [122]. Therefore, the resistance to AR antagonism can be explained by MDSC metabolic function.
The biophysical properties of the stroma, like the cell communication between all the components of the stroma of the tumor prostate, play a critical role not only in the progression of the disease but also in the resistance of the tumor to radiation or cytotoxic therapy. This mechanism relies on the role of ECM synthesized by cellular components and the communication between these components and cancer cells. There is a growing interest in the communication mechanism between cancer cells and stromal cells. The role of extracellular vesicles (EVs), membrane-enclosed particles secreted by several cells, including cancer epithelial, immune, or non-immune cells, is interesting. EVs can carry cytoplasmic proteins, lipids, nucleic acids, or metabolites that affect cells in the same vicinity or far distance. They also have a role in modulating tumor immune response and have many functions, including oncogenic signals, angiogenesis, or tumor-evading signals. They are critical mediators by which tumors regulate their microenvironment and, in return, by which stromal cells modulate tumors [123, 124]. For example, exosomes from MDSCs ease CRPC progression [125]. On the other hand, Xu and colleagues recently described how exosomes from PC cells containing interleukin-8 (IL-8) alter the metabolism of stromal CD8+ T cells, switching from OXPHOS to thermogenesis [126].
Role of oncometabolites in shaping the tumor microenvironment and cancer metastasis
From the classical point of view of the Warburg Effect, lactate has been considered a waste product from glycolytic tumor cells which acidifies the TME. Lactic acidosis in the TME promotes metastasis, angiogenesis, and immunosuppression [127]. However, lactate can also be catabolized to pyruvate, fueling the TCA cycle and stimulating different anabolic signals [128]. In 2008, Sonveaux et al. showed that lactate uptake is preferred in OXPHOS-dependent cancer cells and is involved in cellular processes such as redox homeostasis [129]. In 2017, Hui et al. proposed lactate as the primary carbon source in the TCA cycle [130].
The lactate uptake, known as Reverse Warburg Effect, is particularly relevant in the prostatic TME and different from other tumors [131]. PC cells modify the metabolism of CAFs by Interleukin-6 (IL-6) secretion [132]. Epithelial tumor cells downregulate the tumor suppressor p62 in fibroblasts. Consequently, there is a reduction in the mTORC1 activity and c-Myc expression that causes a release of ROS and IL-6 and the activation of fibroblasts [133]. CAFs enhance glucose transporter GLUT1 and lactate exporter MCT4 levels, becoming glycolytic and secreting lactate [134, 135]. CAFs also activate Pyruvate kinase M2 (PKM2) in PC cells. This protein is translocated into the nucleus, losing its metabolic function and switching the metabolism to OXPHOS [134, 136]. Simultaneously, PC cells reduce GLUT1 levels and increase the levels of the lactate importer MCT1, consuming the lactate secreted by CAFs (Fig. 2) [134]. In 2019, Ippolito et al. studied the role of lactate coming from CAFs into tumor cells more in-depth. Lactate impacts the NAD+/NADH ratio, activating the mitochondrial regulator PGC-1α via SIRT1. Consequently, there is an increase in mitochondrial biomass and activity, an accumulation of oncometabolites from the TCA cycle, and more superoxide generation. Interestingly, along with lactate uptake, tumor cells established cellular bridges with CAFs to hijack functional mitochondria [48]. Although still not completely defined, this metabolic phenotype seems characteristic of primary tumors. The metastatic and CRPC forms secrete lactate via MCT4 and present reduced levels of MCT1 [137, 138].
The lactic acidification in the TME also impacts immunomodulation, particularly associated with TAMs. Acidosis alters interleukin-4-related macrophage activation (M2-immunosuppressive phenotype), promoting tumor growth. In addition, there is a negative correlation between macrophage infiltration and MCT4 levels (Fig. 2) [139]. Recently, Chaudagar et al. found an inverse correlation between glycolytic activity and antitumor TAM phagocytosis in metastastic CRPC (mCRPC) patients [140].
Besides lactate production, CAFs feed cancer cells through ketone bodies, molecules necessary to ensure lipid synthesis under glucose deprivation [141, 142]. Lipids are metabolites highly present in the tumor stroma, particularly in bone metastases [143]. While CAFs are the most abundant cells of the TME of primary tumors, adipose tissue is the majority in the bone marrow, where PC metastasis is more frequent. The high metabolic activity of the adipocytes promotes the proliferation and aggressiveness of cancer cells in bone metastasis, being proposed as responsible for the metabolic disbalance from OXPHOS to glycolysis [144]. In vitro, PC cells in the presence of adipocytes are more glycolytic by increasing HIF1α levels. However, physical interaction is not necessary, but the specific factors involved in PC progression are not elucidated yet [145]. Cutruzzolà et al. suggest adipocyte-secreted glycerol can feed cancer cells by entering the glycolytic pathway [144]. On the other hand, Whitburn and colleagues described that bone stromal cells upregulate glucose-6-phosphate dehydrogenase activity and, consequently, the pentose phosphate pathway (PPP) by IL-6 secretion (Fig. 2) [146].
Another oncometabolite related to lipid metabolism is choline, which is part of the phospholipid phosphatidylcholine. Choline is highly abundant in PC cells [147], and the TME influences choline metabolism [148]. However, it has not been elucidated which component regulates choline levels. Furthermore, PC cells secrete extracellular lipid vesicles enriched in Caveolin-1, phosphatidylcholine, sphingolipids, and cardiolipins [149]. Therefore, the tumor stroma regulates choline metabolism in PC cells, but choline secretion can also impact the TME. On the other hand, cholesterol is also highly concentrated in PC cells [150], and CAFs upregulate its synthesis and the steroid biosynthesis pathway [151], possibly by proinflammatory cytokines and chemokines, not via oncometabolite signaling.
Some amino acids are essential in shaping the TME in several cancers. Glutamine, the most abundant amino acid, plays a significant role in tumor cells but also the TME. Epigenetic regulation of Ras activity in prostatic CAFs metabolically links the stroma and the tumoral epithelia. The fibroblastic Ras-driven macropinocytosis triggers an increase in glutamine production. The glutamine excess is employed by tumor cells to promote tumor progression, neuroendocrine differentiation, and resistance to androgen deprivation therapy (ADT) (Fig. 2) [152]. Moreover, arginine, a semi-essential amino acid, is particularly relevant in immune cells [153]. Arginine metabolism is the metabolic bridge between malignant PC cells and TAM, increasing tumor aggressiveness [154]. Arginase (ARG) 1 and ARG2, enzymes responsible for catabolizing arginine into ornithine, activate immunosuppressive pathways in the hormone-refractory PC [155]. In addition, arginine is also in control of maintaining the unresponsiveness of tumor-infiltrating cytotoxic lymphocytes. In tumor cells, inhibition of ARG and nitric oxide synthase (converts arginine into nitric oxide) promotes lymphocyte responsiveness by reducing tyrosine nitration [156]. In mice, extracellular arginine is taken by MDSCs via upregulation of cationic amino acid transporter 2 (Cat2/Slc7a2), reducing its availability for immune cells [157]. In patients, it was also confirmed that high levels of Arg1 in a G-MDSC population inhibit the proliferation and cytotoxic activity of CD8 + T cells [158].
The function of famous oncometabolites like 2-hydroxyglutarate, fumarate, or succinate has not been extensively described for the PC microenvironment. Succinate from stromal cells can have a remarkable goal in oncogenic potential since PC cells consume it in an acidic environment, having an anaplerotic effect and enhancing the aggressive potential [159, 160]. Succinate can be secreted from CAFs through exosomes. CAFs-derived exosomes include lactate, acetate, amino acids, TCA cycle metabolites like succinate, and lipids. Furthermore, exosome secretion is pH dependent, being favored under an acidic environment. Unlike the lactate effect alone, CAFs-derived exosomes inhibit the electron transport chain, increasing glutamine carboxylation for biosynthesis in PC cells [161].
Influence of oncometabolites in CSC phenotype
Even if the impact of oncometabolites in the crosstalk between stromal cells and PC cells has been reasonably assessed, less clear is which are the oncometabolites responsible for maintaining the metabolic properties of CSCs. CSCs are generally characterized by a high glycolytic rate and low OXPHOS [162], but their metabolism is also tissue-dependent [163]. Thus, unlike PC cells, glucose can be a critical metabolite for stemness. The CSC cell line 3-AB OS, derived from the human osteosarcoma cell line MG63, is sensitive to glucose deprivation [164]. However, MG63 cells are more susceptible to glutamine deprivation [165]. Recently, it was described in the prostatic PC-3 cell line that cell density shifts metabolism from glycolysis towards OXPHOS and induces a CSC-like phenotype. However, it seems that glycolysis and not OXPHOS is critical for CSC phenotype since dichloroacetate, a pyruvate dehydrogenase inhibitor, blocks the acquisition of CSC properties [166]. Nevertheless, this study was performed in vitro with only one cell line, requiring more studies to extract consistent conclusions.
Among the candidates to regulate CSCs in PC, kynurenine, a metabolite from tryptophan metabolism, is more abundant than lactate in the PC microenvironment and can have immunosuppressive properties, promoting malignancy [167, 168]. Kynurenine has been involved in self-renewal, maintenance, and differentiation in embryonic stem cells (ESC) and induced pluripotent stem cells (iPSCs) [168, 169]. Therefore, this metabolite can be a major candidate for regulating CSCs in the prostate.
Therapeutic implications and future perspectives
Current Strategies targeting metabolic dysregulation, oncometabolites, and epigenetic modulation in prostate cancer
Biomarkers
Recent technical breakthroughs in analytical chemistry allow us to identify low-abundance metabolites in different biological matrixes and metabolic alterations along key pathways [170]. Since oncometabolites are characteristic of tumor development and progression, identifying their differential levels in diverse biological samples compared to healthy individuals could be an interesting approach as novel prostate cancer biomarkers. Here we sum up the oncometabolites differently identified in preclinical models and in urine, seminal fluid, and biopsies of PC patients.
Urine, as part of the urogenital system and an easy-to-get sample, could be a feasible matrix to look for patient biomarkers. Succinate is detected and less abundant in PC patients' urine (n = 32) compared to healthy controls (n = 32). The study's authors explained this as an indication of the disruption of the TCA cycle in tumor cells [171]. Interestingly, they also found hydroxyglutarate downregulated in the urine of PC patients. Kyneurine, another oncometabolite [172, 173], was found to have significantly higher median values in the urine of PC patients (n = 101) than in controls (n = 52) [54].
Due to the significant contribution of the prostate to the seminal fluid composition, it is reasonable to search for potential biomarkers within it. Citrate emerges as a widely differentially produced metabolite in seminal fluid. Although citrate is not an oncometabolite, it is a critical factor in prostate metabolism. In normal prostate, it is accumulated in epithelial cells due to zinc-induced TCA cycle blockade at the m-aconitase level. Citrate, along with zinc, is secreted to seminal fluid. However, metabolic reprogramming during PC initiation drops zinc and citrate levels, unblocking the TCA cycle [174]. Thus, citrate has lower levels in PC patients' seminal fluid than in control groups across different studies (PC n = 4, control n = 22 [175]; PC n = 28, control n = 33 [176]; PC n = 52, control n = 26 [177]; and PC n = 3, control n = 4 [178]).
Molecular and metabolic profiling of cancer biopsies is a novel opportunity to identify new features of solid tumors. Fumarate increased in patient cancer samples compared to adjacent benign tissue (n = 13) [49]. Furthermore, this oncometabolite positively correlated with gene expression of oncogenic HIF1ɑ and NF-kB pathways [49]. Tessem et al., 2016, tried to shed light on the metabolic profiling of solid tumors and find biomarkers despite different and complex mixtures of tissues within the sample. By selecting samples with a similar proportion of tumor and stroma across biopsies and groups, they could identify differentially elevated levels of succinate and reduced levels of citrate between PC patients (n = 95) and healthy individuals (n = 34) [179]. Finally, another oncometabolite linked to in situ tumor progression is lactate. Despite its low concentration, using transrectal ultrasound-guided biopsies, lactate was identified, and PC samples contained differentially higher levels than benign tissue (n = 82). Interestingly, they could reach an ability to detect this increase in lactate with as little as 5% of tumor content in the biopsy, making it a promising tool for PC detection [180].
Together with the advances in detection methods of metabolites, the field of EVs is also growing thanks to better and refined methods of isolation, characterization, and their new roles discovered in many hallmarks of cancer. Thus, PC patient-derived EVs isolation and characterization is being used as a biomarker search, as reviewed in [181]. Indeed, Clos-Garcia et al., 2018, isolated EVs from the urine of PC patients and then performed a metabolomic analysis of their cargo. Succinate could be detected in all samples (PC n = 31 and BPH n = 14), but with a fold-change of 1.211, the p-value of the comparison PC vs BPH was 0.11. Citrate and isocitrate were also identified, and interestingly they were significantly downregulated in EVs from PC [182]. Other oncometabolites detected in EVs are lactate and fumarate, identified in high concentrations in patient-derived CAFs, which are incorporated by PC cells in vitro to fuel their metabolic demands [161]. Furthermore, succinate has been identified in EVs derived from PC cells in vitro, with significantly higher levels than non-tumoral counterparts [183]. These findings make the characterization and search of specific (onco)metabolites in EVs of PC patients a stimulating research field.
Therapeutic agents
Once identified as potential biomarkers, the mechanical effects of oncometabolites on tumor initiation and progression also make them attractive therapeutic targets. Not only the classic oncometabolites and their downstream effects but also the different pathways related to the wide metabolic dysregulation that occurs along PC can offer an opportunity to understand more of the weaknesses of this tumor, trying to find new efficient candidate treatments.
Metabolic rewiring of glucose, lipids, and amino acids, among others, is a hallmark of PC. Early stages of PC, contrary to most tumors, are characterized by oxidative phosphorylation-based metabolism rather than aerobic glycolysis, while advanced CRPC stages rely on glycolysis [174, 184]. De novo lipogenesis and fatty acid oxidation (FAO) are early PC events, also correlating with disease progression [185, 186]. Glutamine, the most abundant amino acid in plasma, plays a crucial role in PC metabolism since it can be used as a substitute for glucose in TCA cycle, and as a building block for nucleotide synthesis and fatty acid production [186, 187]. Thus, targeting this metabolic dysregulation at different levels could become a practical therapeutic approach.
Focusing on using TCA cycle derivatives and oxidative phosphorylation, the mitochondrial electron transport chain could be an effective target in PC cells. There are several compounds showing effectiveness in preclinical studies. MSDC-0160 is an inhibitor of the mitochondrial pyruvate carrier (MPC), which breaks the link between cytosolic and mitochondrial metabolism. This drug reduces proliferation by preventing cell cycle progression and disrupts the TCA cycle in AR-driven PC models (cell lines and xenografts) [188]. Electron transport chain (ETC) complex-I inhibitors rotenone, its derivative deguelin, and IACS-010759 inhibit proliferation and induce apoptosis in PTEN-null models of PC [189, 190]. Metformin, which inhibits ETC complex-I and is the most common anti-diabetic drug, is being studied in 33 clinical trials as an anti-PC agent, and 8 of them have available results so far. Some remarkable results are the decline of PSA after combination of metformin with bicalutamide after 8 weeks (42.1% bicalutamide + metformin vs 11.1% only bicalutamide) in PC patients with overweight (ClinicalTrial.gov ID NCT02614859), and with castration after 7 months (placebo PSA 58.2 ng/mL vs metformin PSA 8.36 ng/mL, ClinicalTrial.gov ID NCT01620593, [191]), and its detection in the prostatic tissue after consumption for 12 weeks, but without changes in tumor progression markers (ClinicalTrials.gov ID NCT01433913, [192]). However, other studies finished without concluding beneficial results, making it necessary to study refinement mechanisms further to explode the potentiality of metformin or identify potential patient candidates that could be benefited from metformin treatment. In vitro, some of the mechanisms of action described is to effectively induce p53-dependent apoptosis in PC cells when combined with 2-deoxyglucose, inhibiting glycolysis and mitochondrial respiration together [193, 194].
As an energy sensor, 5’AMP-activated kinase (AMPK) exerts many actions widely regarded as tumorigenic suppressors. Selective AMPK-activator MT 63–78 inhibits proliferation and induces apoptosis in PC cells by disrupting lipogenesis [195]. Moreover, due to the dependence on liponeogenesis of PC cells, fatty acid synthase (FASN) inhibitors are showing promising results. C75-dependent FASN blockade reduces the proliferation of LNCaP cells and tumor growth in vivo [196]. Another orally available, reversible, selective FASN inhibitor, TVB-3166, inhibits anchorage-dependent cell growth and induces apoptosis in PC cell lines and patient-derived xenografts through different downstream mechanisms [197]. Finally, FASN inhibitor TV-2640 is currently in phase I clinical trial (ClinicalTrial.gov ID NCT05743621). The study aims to determine the effects of this drug together with AR-inhibitor enzalutamide in mCRPC. Fatty acid oxidation is another attractive target. The commercially available drug ranolazine is employed for heart angina, but decreased tumor growth in a xenograft PC model [198] and sensitized to antiandrogen treatment in vitro and in a xenograft [199] when administered orally. This drug inhibits carnitine palmitoyltransferase (CPT1) and, thus, lipid oxidation.
Moreover, Telaglenastat (CB-839) is a promising orally available small molecule that inhibits glutaminase 1 (GLS1). It induces autophagy and has anti-tumor activity in multiple preclinical tumor models, including PC, alone or in combination with other treatments [200]. Telaglenastat is currently in a Phase II clinical trial, testing the effectiveness of its combination with talazoparib, a poly-ADP ribose polymerase (PARP) inhibitor, in mCRPC patients (ClinicalTrial.gov ID NCT04824937).
Regarding classic oncometabolites and metabolic rewiring, succinate is accumulated due to antiandrogen treatments, representing another therapeutic approach. Saxena et al., 2021, showed that AR transcriptionally regulates SDH subunits SDHA and SDHB. Antiandrogen therapy suppresses SDH, causing succinate accumulation. Succinate triggers a response of survival and adaption to treatments through a complex cascade that activates AR co-chaperone p-Hsp27. This way, combining antiandrogens with the p-Hsp27 inhibitor Ivermectin could be a potential improvement against antiandrogen resistance, as shown in preclinical models of LNCaP xenografts [46].
The interplay between TME, epigenetics, and cancer cells is also essential. Androgen-deprivation therapy can produce epigenetic changes in CAFs. Hypermethylation of RASAL3 promoter, a tumor suppressor that inhibits Ras function, induces glutamine secretion by CAFs. This glutamine is incorporated via facilitated transport by cancer cells, which is then derived to TCA cycle. Selectively targeting glutamine uptake by L-γ-Glutamyl-p-nitroanilide (GPNA), an inhibitor of glutamine transporter SLC1A5, showed a reduction of tumor proliferation in a preclinical 3D model and tumor growth suppression in a xenograft when combined with castration of mice [152]. Another study by Chaudagar et al., 2023, explores the potential advance inhibiting PI3K-dependent lactate production in cancer cells. As previously described, lactate secreted by PC cells is incorporated by TAMs in the TME, inducing the epigenetic change of histone lactylation and further reducing TAMs phagocytic and immunosuppressive effect on the tumor cells. Targeting PI3K pathway with Copanlisib along with ADT reduces lactate secretion and, thus, tumor growth repression helped by immunosuppression of activated TAMs in a PTEN/p53-deficient murine PC model [140].
Cells with low or absent AR expression and IDH1 R132H mutation are more likely to accumulate R-2HG than those with intact AR signaling [45]. The oncometabolite R-2HG induces PC AR− cells invasion through TGFβ1/p-Smad2/3 signaling in vitro. In fact, AR− cells carrying IDH1 R132H mutation metastasized more than their wild-type counterparts in a xenograft model. Since R-2HG is responsible for this phenomenon, the authors of this work propose the study of Tibsovo (ivosidenib). FDA has already approved this IDH1 inhibitor for patients with refractory acute myeloid leukemia (AML) who have IDH1 mutation(s) as a candidate drug to be tested in combination with bipolar antiandrogen therapy [45]. Targeting IDH1 mutations in PC can also have a beneficial impact on epigenetic imbalance. An epigenomic study of mCRPC patients identified a subset of CpG Methylator Phenotype (CMP), this is, with a high methylation profile, which harbored exclusive mutations in IDH1 among others (TET2 or BRAF) [201]. Altogether, IDH1 could be a therapeutic target in the small subset of IDH-mutant PCa patients by potentially improving the response to ADT reducing R-2HG and epigenetic imbalance.
Future directions: exploiting the Interplay of oncometabolites, epigenetic changes and CSCs for therapeutic purposes
Understanding the complex interplay of oncometabolites, epigenetic changes, and CSCs has provided groundbreaking insights into the mechanistic pathways and gene regulatory networks underlying the development and progression of prostate cancer.
The recognition that oncometabolites play a central role in reprogramming the cancer epigenome has spurred the concept of 'metabostemness'. This phenomenon underscores the reciprocal interaction between cancer metabolism and stemness, where aberrant metabolites can reshape the epigenetic landscape to bolster stemness traits and promote a more malignant phenotype [80].
Oncometabolites like succinate, fumarate, and 2-hydroxyglutarate, arising due to mutations in metabolic enzymes like SDH, FH, and IDH, have been linked to changes in DNA and histone modifications, further leading to the activation of EMT and enhancement of cancer stemness properties [28]. One of the potential therapeutic strategies could be to develop small molecule inhibitors or therapeutic agents targeting these mutated enzymes, thereby curbing the production of oncometabolites and subsequently counteracting cancer progression.
Such a strategy has been demonstrated in the case of cholangiocarcinoma, where IDH1 mutations resulted in the production of the oncometabolite 2-hydroxyglutarate, leading to epigenetic alterations and changes in the expression of key genes involved in cell differentiation and survival [202]. Based on these findings, small-molecule inhibitors of the IDH1 mutated enzyme are currently under investigation in preclinical and clinical phases as promising treatments for IDH1-mutated intrahepatic cholangiocarcinomas [203, 204]. Interestingly, this approach is mirrored in a recent phase 3 trial for IDH-mutant grade 2 gliomas, where the inhibitor vorasidenib demonstrated significant improvements in progression-free survival and delay in the need for further anticancer intervention [205]. A similar approach could be contemplated for prostate cancer, with the development of specific inhibitors targeting the metabolic enzymes associated with the production of detrimental oncometabolites.
Moreover, the identification of specific markers associated with CSCs and EMT could provide potential therapeutic targets [206]. Notably, therapies could be designed to target these markers, thus providing a means of eliminating the CSC population, attenuating EMT, and curbing metastasis [207]. Such therapies could also potentially reverse therapy resistance, considering the role of CSCs in this phenomenon.
The recent revelations about the association between some mutations in therapy-resistant prostate cancer patients, higher levels of gene expression involved in stemness, EMT, and invasiveness [83, 208], also provide an opportunity to discover new targets for therapy. There is a need for the development of a precision medicine approach to tackle prostate cancer, wherein these potential therapeutic targets can be exploited to devise patient-specific treatments.
Furthermore, as CSCs have shown remarkable adaptability to various microenvironmental signals, it is equally important to study the TME and its influence on the CSC phenotype and epigenetic landscape. These studies could provide clues on how to make the tumor environment less conducive for the growth and proliferation of CSCs.
In conclusion, future research needs to intensify efforts on studying the complex interplay between oncometabolites, epigenetic changes, and CSCs. The key lies in exploiting these intricate relationships to identify potential therapeutic targets and develop effective treatment strategies for not only prostate cancer, but also other types of cancer where similar mechanisms are involved. The dawn of precision medicine offers a new hope in the fight against cancer, and the focus should be on exploring innovative and targeted approaches to capitalize on the wealth of knowledge we have gained so far.
Conclusions
Our comprehensive review discusses the interplay between oncometabolites, epigenetic changes, and CSCs in prostate cancer and offers several key insights with significant implications for understanding and managing this prevalent disease. Firstly, we have elucidate the concept of 'metabostemness', a novel paradigm that underscores how metabolic dysregulation in cancer can perpetuate stem cell-like traits, leading to more aggressive and therapy-resistant tumor phenotypes.. The discovery that oncometabolites, such as succinate, fumarate, and 2-hydroxyglutarate, can induce significant epigenetic modifications offers a novel view on cancer pathogenesis. These insights highlight the potential of targeting metabolic pathways as a novel therapeutic strategy, as occur in cholangiocarcinoma [209, 210] and may be translated to prostate cancer treatment. Additionally, we discuss the critical role of specific genetic and epigenetic determinants in prostate cancer progression. We provide evidence that therapy-resistant prostate cancer patients often harbor certain mutations, and exhibit higher levels of genes associated with stemness, EMT, and invasiveness. This finding not only advances our molecular understanding of the disease but could be leveraged to discover new targets for therapy, paving the way for a more precise approach to prostate cancer treatment.
Another crucial aspect of our review is the emphasis on the TME and its influence on CSCs. Our findings suggest that modulating the TME could be key to inhibiting CSC growth and proliferation, thereby impeding cancer progression and metastasis.
In essence, this review contributes to the existing literature by integrating various molecular aspects of prostate cancer into a coherent framework. It underscores the importance of a multi-faceted approach encompassing genetic, metabolic, and epigenetic factors in developing more effective therapeutic strategies. As we move towards an era of precision medicine, the insights gained from this review not only enhance our understanding of prostate cancer but also highlight critical research areas that warrant further exploration. This work establishes a cornerstone for subsequent investigations, bolstering optimism for the enhanced treatment and care of prostate cancer patients globally.
Abbreviations
- 2-HG:
-
2-Hydroxyglutarate
- α-KG:
-
α-Ketoglutarate
- α-SMH:
-
α-Smooth muscle actin
- ACLY:
-
ATP citrate lyase
- ADT:
-
Androgen deprivation therapy
- ALDH:
-
Aldehyde dehydrogenase
- AMPK:
-
5’-AMP-activated kinase
- AML:
-
Acute myeloid leukemia
- AR:
-
Androgen Receptor
- ARG:
-
Arginase
- BPH:
-
Bening prostatic hyperplasia
- CAF:
-
Cancer-asssociated fibroblast
- CAIX:
-
Carbonic anhydrase IX
- Cat2:
-
Cationic amino acid transporter 2
- CMP:
-
CpG Methylator Phenotype
- CPT1:
-
Carnitine palmitoyltransferase
- CSC:
-
Cancer stem cell
- circRNA:
-
Circular RNA
- CRPC:
-
Castration-resistant prostate cancer
- ECM:
-
Extracellular matrix
- EMT:
-
Epithelial-to-mesenchymal transition
- ERG:
-
ETS-related gene
- ESC:
-
Embryonic stem cell
- ETC:
-
Electron transport chain
- EV:
-
Extracellular vesicle
- FAD:
-
Flavin adenine dinucleotide
- FAO:
-
Fatty acid oxidation
- FASN:
-
Fatty acid synthase
- FH:
-
Fumarate hydratase
- GABA:
-
γ-Aminobutyric acid
- GAD:
-
Glutamic acid decarboxylase
- GLS-1:
-
Glutaminase 1
- G-MDSC:
-
Granulocytic MDSC
- GPNA:
-
L-γ-Glutamyl-p-nitroanilide
- HIF:
-
Hypoxia inducible factor
- IDH:
-
Isocitrate dehydrogenase
- IL-6:
-
Interleukin-6
- IL-8:
-
Interleukin-8
- iPSC:
-
Induced pluripotent stem cell
- KDM:
-
Histone lysine demethylase
- LDH:
-
Lactate dehydrogenase
- LSH:
-
Lymphoid-specific helicase
- mCRPC:
-
Metastatic castration-resistant prostate cancer
- MCT:
-
Monocarboxylate transporter
- MDH:
-
Malate dehydrogenase
- MDSC:
-
Myeloid-Derived Suppressor Cell
- MET:
-
Mesenchymal-to-epithelial transition
- M-MDSC:
-
Monocytic MDSC
- MPC:
-
Mitochondrial pyruvate carrier
- MutIDH1/2:
-
Mutated form of the enzyme isocitrate dehydrogenase
- NF-kB:
-
Nuclear factor kB
- NK:
-
Natural killer
- NPC:
-
Nasopharyngeal carcinoma
- OXPHOS:
-
Oxidative phosphorylation
- PARP:
-
Poly-ADP ribose polymerase
- PC:
-
Prostate cancer
- PCSC:
-
Prostate cancer stem cell
- PGC1α:
-
Peroxisome proliferator-activated receptor γ co-activator 1 α
- PHGDH:
-
Phosphoglycerate dehydrogenase
- PI3K:
-
Phosphoinositide 3-kinase
- PIN:
-
Prostatic intraepithelial neoplasia
- PKM2:
-
Pyruvate kinase M2
- PPP:
-
Pentose phosphate pathway
- PSA:
-
Prostate specific antigen
- ROS:
-
Reactive oxygen species
- SIRT:
-
Sirtuin
- SOD:
-
Superoxide dismutase
- SDH:
-
Succinate dehydrogenase
- TAM:
-
Tumor-associated macrophages
- TCA:
-
Tricarboxylic acid cycle
- TERT:
-
Telomerase reverse transcriptase
- TET:
-
Ten eleven translocaion-enzyme
- TGF:
-
Transforming growth factor
- TME:
-
Tumor microenvironment
- VEGF:
-
Vascular endothelial growth factor
- Wnt3:
-
Wnt family member 3
References
Ittmann M. Anatomy and histology of the human and murine prostate. Cold Spring Harb Perspect Med. 2018;8:a030346.
Sandhu S, Moore CM, Chiong E, Beltran H, Bristow RG, Williams SG. Prostate cancer. Lancet. 2021;398:1075–90.
Espiritu SMG, Liu LY, Rubanova Y, Bhandari V, Holgersen EM, Szyca LM, et al. The evolutionary landscape of localized prostate cancers drives clinical aggression. Cell. 2018;173:1003-1013.e15.
Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019;10:63–89.
Hakozaki Y, Yamada Y, Kawai T, Nakamura M, Takeshima Y, Iwaki T, et al. Time to castration resistance is a novel prognostic factor of cancer-specific survival in patients with nonmetastatic castration-resistant prostate cancer. Sci Rep. 2022;12:16202.
Saad F, Bögemann M, Suzuki K, Shore N. Treatment of nonmetastatic castration-resistant prostate cancer: focus on second-generation androgen receptor inhibitors. Prostate Cancer Prostatic Dis. 2021;24:323–34.
Chandrasekar T, Yang JC, Gao AC, Evans CP. Mechanisms of resistance in castration-resistant prostate cancer (CRPC). Transl Androl Urol. 2015;4:365–80.
Oh M, Alkhushaym N, Fallatah S, Althagafi A, Aljadeed R, Alsowaida Y, et al. The association of BRCA1 and BRCA2 mutations with prostate cancer risk, frequency, and mortality: a meta-analysis. Prostate. 2019;79:880–95.
Khosh Kish E, Choudhry M, Gamallat Y, Buharideen SM, D D, Bismar TA. The Expression of Proto-Oncogene ETS-Related Gene (ERG) plays a central role in the oncogenic mechanism involved in the development and progression of prostate cancer. Int J Mol Sci. 2022;23:4772.
Croonquist PA, Van Ness B. The polycomb group protein enhancer of zeste homolog 2 (EZH 2) is an oncogene that influences myeloma cell growth and the mutant ras phenotype. Oncogene. 2005;24:6269–80.
Zoma M, Curti L, Shinde D, Albino D, Mitra A, Sgrignani J, et al. EZH2-induced lysine K362 methylation enhances TMPRSS2-ERG oncogenic activity in prostate cancer. Nat Commun. 2021;12:4147.
Xu K, Wu ZJ, Groner AC, He HH, Cai C, Lis RT, et al. EZH2 oncogenic activity in castration-resistant prostate cancer cells is Polycomb-independent. Science. 2012;338:1465–9.
Demichelis F, Rubin MA. TMPRSS2-ETS fusion prostate cancer: biological and clinical implications. J Clin Pathol. 2007;60:1185–6.
Yu J, Yu J, Mani R-S, Cao Q, Brenner CJ, Cao X, et al. An integrated network of androgen receptor, polycomb, and TMPRSS2-ERG gene fusions in prostate cancer progression. Cancer Cell. 2010;17:443–54.
Kachuri L, Hoffmann TJ, Jiang Y, Berndt SI, Shelley JP, Schaffer KR, et al. Genetically adjusted PSA levels for prostate cancer screening. Nat Med. 2023;29:1412–23.
Cirne F, Kappel C, Zhou S, Mukherjee SD, Dehghan M, Petropoulos J-A, et al. Modifiable risk factors for prostate cancer in low- and lower-middle-income countries: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2022;25:453–62.
Torrano V, Valcarcel-Jimenez L, Cortazar AR, Liu X, Urosevic J, Castillo-Martin M, et al. The metabolic co-regulator PGC1α suppresses prostate cancer metastasis. Nat Cell Biol. 2016;18:645–56.
Li Z, Low V, Luga V, Sun J, Earlie E, Parang B, et al. Tumor-produced and aging-associated oncometabolite methylmalonic acid promotes cancer-associated fibroblast activation to drive metastatic progression. Nat Commun. 2022;13:6239.
Lautert-Dutra W, Dos Reis RB, Squire JA. Precision medicine for prostate cancer-improved outcome prediction for low-intermediate risk disease using a six-gene copy number alteration classifier. Br J Cancer. 2023;128:2163–4.
Saad F. Continuing to improve outcomes of men with metastatic prostate cancer. Nat Rev Clin Oncol. 2019;16:597–8.
Hanahan D. Hallmarks of cancer: new dimensions. Cancer Discov. 2022;12:31–46.
Pavlova NN, Zhu J, Thompson CB. The hallmarks of cancer metabolism: still emerging. Cell Metab. 2022;34:355–77.
Khatami F, Aghamir SMK, Tavangar SM. Oncometabolites: a new insight for oncology. Mol Genet Genomic Med. 2019;7:e873.
Sajnani K, Islam F, Smith RA, Gopalan V, Lam AK-Y. Genetic alterations in Krebs cycle and its impact on cancer pathogenesis. Biochimie. 2017;135:164–72.
Du X, Hu H. The roles of 2-hydroxyglutarate. Front Cell Dev Biol. 2021;9:651317.
Fan J, Teng X, Liu L, Mattaini KR, Looper RE, Vander Heiden MG, et al. Human phosphoglycerate dehydrogenase produces the oncometabolite D-2-hydroxyglutarate. ACS Chem Biol. 2015;10:510–6.
Galluzzi L, Kroemer G. Potent immunosuppressive effects of the oncometabolite R-2-hydroxyglutarate. OncoImmunology. 2018;7:e1528815.
Dando I, Pozza ED, Ambrosini G, Torrens-Mas M, Butera G, Mullappilly N, et al. Oncometabolites in cancer aggressiveness and tumour repopulation. Biol Rev Camb Philos Soc. 2019;94:1530–46.
Ippolito L, Comito G, Parri M, Iozzo M, Duatti A, Virgilio F, et al. Lactate rewires lipid metabolism and sustains a metabolic-epigenetic axis in prostate cancer. Can Res. 2022;82:1267–82.
Faubert B, Li KY, Cai L, Hensley CT, Kim J, Zacharias LG, et al. Lactate metabolism in human lung tumors. Cell. 2017;171:358-371.e9.
Heid I, Münch C, Karakaya S, Lueong SS, Winkelkotte AM, Liffers ST, et al. Functional noninvasive detection of glycolytic pancreatic ductal adenocarcinoma. Cancer Metabol. 2022;10:24.
Longhitano L, Giallongo S, Orlando L, Broggi G, Longo A, Russo A, et al. Lactate rewrites the metabolic reprogramming of uveal melanoma cells and induces quiescence phenotype. Int J Mol Sci. 2023;24:24.
Zhang D, Tang Z, Huang H, Zhou G, Cui C, Weng Y, et al. Metabolic regulation of gene expression by histone lactylation. Nature. 2019;574:575–80.
Chen A-N, Luo Y, Yang Y-H, Fu J-T, Geng X-M, Shi J-P, et al. Lactylation, a novel metabolic reprogramming code: current status and prospects. Front Immunol. 2021;12:688910.
Yang Z, Yan C, Ma J, Peng P, Ren X, Cai S, et al. Lactylome analysis suggests lactylation-dependent mechanisms of metabolic adaptation in hepatocellular carcinoma. Nat Metab. 2023;5:61–79.
Wang J, Mao L, Wang J, Zhang X, Wu M, Wen Q, et al. Beyond metabolic waste: lysine lactylation and its potential roles in cancer progression and cell fate determination. Cell Oncol. 2023;46:465–80.
Zabala-Letona A, Arruabarrena-Aristorena A, Martín-Martín N, Fernandez-Ruiz S, Sutherland JD, Clasquin M, et al. mTORC1-dependent AMD1 regulation sustains polyamine metabolism in prostate cancer. Nature. 2017;547:109–13.
Chowdhury R, Yeoh KK, Tian Y-M, Hillringhaus L, Bagg EA, Rose NR, et al. The oncometabolite 2-hydroxyglutarate inhibits histone lysine demethylases. EMBO Rep. 2011;12:463–9.
Xu W, Yang H, Liu Y, Yang Y, Wang P, Kim S-H, et al. Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of α-ketoglutarate-dependent dioxygenases. Cancer Cell. 2011;19:17–30.
Li S-T, Huang D, Shen S, Cai Y, Xing S, Wu G, et al. Myc-mediated SDHA acetylation triggers epigenetic regulation of gene expression and tumorigenesis. Nat Metab. 2020;2:256–69.
Chen H, Zhu W, Li X, Xue L, Wang Z, Wu H. Genetic and epigenetic patterns in patients with the head-and-neck paragangliomas associate with differential clinical characteristics. J Cancer Res Clin Oncol. 2017;143:953–60.
He X, Yan B, Liu S, Jia J, Lai W, Xin X, et al. Chromatin remodeling factor LSH drives cancer progression by suppressing the activity of fumarate hydratase. Can Res. 2016;76:5743–55.
Kang MR, Kim MS, Oh JE, Kim YR, Song SY, Seo SI, et al. Mutational analysis of IDH1 codon 132 in glioblastomas and other common cancers. Int J Cancer. 2009;125:353–5.
Yang H, Liu Y, Bai F, Zhang J-Y, Ma S-H, Liu J, et al. Tumor development is associated with decrease of TET gene expression and 5-methylcytosine hydroxylation. Oncogene. 2013;32:663–9.
Xu H, Sun Y, You B, Huang CP, Ye D, Chang C. Androgen receptor reverses the oncometabolite R-2-hydroxyglutarate-induced prostate cancer cell invasion via suppressing the circRNA-51217/miRNA-646/TGFβ1/p-Smad2/3 signaling. Cancer Lett. 2020;472:151–64.
Saxena N, Beraldi E, Fazli L, Somasekharan SP, Adomat H, Zhang F, et al. Androgen receptor (AR) antagonism triggers acute succinate-mediated adaptive responses to reactivate AR signaling. EMBO Molec Med. 2021;13(5):e13427.
Quiros-Gonzalez I, Gonzalez-Menendez P, Mayo JC, Hevia D, Artime-Naveda F, Fernandez-Vega S, et al. Androgen-dependent prostate cancer cells reprogram their metabolic signature upon GLUT1 upregulation by manganese superoxide dismutase. Antioxidants (Basel). 2022;11:313.
Ippolito L, Morandi A, Taddei ML, Parri M, Comito G, Iscaro A, et al. Cancer-associated fibroblasts promote prostate cancer malignancy via metabolic rewiring and mitochondrial transfer. Oncogene. 2019;38:5339–55.
Franko A, Shao Y, Heni M, Hennenlotter J, Hoene M, Hu C, et al. Human prostate cancer is characterized by an increase in urea cycle metabolites. Cancers. 2020;12:1814.
Gao Y, Chen L, Du Z, Gao W, Wu Z, Liu X, et al. Glutamate decarboxylase 65 signals through the androgen receptor to promote castration resistance in prostate cancer. Can Res. 2019;79:4638–49.
Rodrigo MAM, Strmiska V, Horackova E, Buchtelova H, Michalek P, Stiborova M, et al. Sarcosine influences apoptosis and growth of prostate cells via cell-type specific regulation of distinct sets of genes. Prostate. 2018;78:104–12.
Strmiska V, Michalek P, Lackova Z, Guran R, Krizkova S, Vanickova L, et al. Sarcosine is a prostate epigenetic modifier that elicits aberrant methylation patterns through the SAMe-Dnmts axis. Mol Oncol. 2019;13:1002–17.
Heger Z, Gumulec J, Cernei N, Polanska H, Raudenska M, Masarik M, et al. Relation of exposure to amino acids involved in sarcosine metabolic pathway on behavior of non-tumor and malignant prostatic cell lines. Prostate. 2016;76:679–90.
Delkov D, Yoanidu L, Tomov D, Stoyanova R, Dechev I, Uzunova Y. Oncometabolites in urine – a new opportunity for detection and prognosis of the clinical progress of verified prostate cancer-a pilot study. Turk J Med Sci. 2022;52(3):699–706.
Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ. Prospective identification of tumorigenic prostate cancer stem cells. Can Res. 2005;65:10946–51.
Wang X, Xu H, Cheng C, Ji Z, Zhao H, Sheng Y, et al. Identification of a Zeb1 expressing basal stem cell subpopulation in the prostate. Nat Commun. 2020;11:706.
Skvortsov S, Skvortsova I-I, Tang DG, Dubrovska A. Concise review: prostate cancer stem cells: current understanding. Stem Cells. 2018;36:1457–74.
Li JJ, Shen MM. Prostate stem cells and cancer stem cells. Cold Spring Harb Perspect Med. 2019;9:a030395.
Shibue T, Weinberg RA. EMT, CSCs, and drug resistance: the mechanistic link and clinical implications. Nat Rev Clin Oncol. 2017;14:611–29.
Stylianou N, Lehman ML, Wang C, Fard AT, Rockstroh A, Fazli L, et al. A molecular portrait of epithelial–mesenchymal plasticity in prostate cancer associated with clinical outcome. Oncogene. 2019;38:913–34.
Chaves LP, Melo CM, Saggioro FP, Reis RBD, Squire JA. Epithelial-mesenchymal transition signaling and prostate cancer stem cells: emerging biomarkers and opportunities for precision therapeutics. Genes (Basel). 2021;12:1900.
Grant CM, Kyprianou N. Epithelial mesenchymal transition (EMT) in prostate growth and tumor progression. Transl Androl Urol. 2013;2:20211–20211.
Sandsmark E, Hansen AF, Selnæs KM, Bertilsson H, Bofin AM, Wright AJ, et al. A novel non-canonical Wnt signature for prostate cancer aggressiveness. Oncotarget. 2016;8:9572–86.
Bisson I, Prowse DM. WNT signaling regulates self-renewal and differentiation of prostate cancer cells with stem cell characteristics. Cell Res. 2009;19:683–97.
Nath D, Li X, Mondragon C, Post D, Chen M, White JR, et al. Abi1 loss drives prostate tumorigenesis through activation of EMT and non-canonical WNT signaling. Cell Commun Signal. 2019;17:120.
Karhadkar SS, Steven Bova G, Abdallah N, Dhara S, Gardner D, Maitra A, et al. Hedgehog signalling in prostate regeneration, neoplasia and metastasis. Nature. 2004;431:707–12.
Chang H-H, Chen B-Y, Wu C-Y, Tsao Z-J, Chen Y-Y, Chang C-P, et al. Hedgehog overexpression leads to the formation of prostate cancer stem cells with metastatic property irrespective of androgen receptor expression in the mouse model. J Biomed Sci. 2011;18:6.
Domingo-Domenech J, Vidal SJ, Rodriguez-Bravo V, Castillo-Martin M, Quinn SA, Rodriguez-Barrueco R, et al. Suppression of acquired docetaxel resistance in prostate cancer through depletion of notch- and hedgehog-dependent tumor-initiating cells. Cancer Cell. 2012;22:373–88.
Stoyanova T, Riedinger M, Lin S, Faltermeier CM, Smith BA, Zhang KX, et al. Activation of Notch1 synergizes with multiple pathways in promoting castration-resistant prostate cancer. Proc Natl Acad Sci U S A. 2016;113:E6457–66.
Kwon O-J, Zhang L, Wang J, Su Q, Feng Q, Zhang XHF, et al. Notch promotes tumor metastasis in a prostate-specific Pten-null mouse model. J Clin Invest. 2016;126:2626–41.
Stopsack KH, Nandakumar S, Wibmer AG, Haywood S, Weg ES, Barnett ES, et al. Oncogenic genomic alterations, clinical phenotypes, and outcomes in metastatic castration-sensitive prostate cancer. Clin Cancer Res. 2020;26:3230–8.
Chen B, Zhang Y, Li C, Xu P, Gao Y, Xu Y. CNTN-1 promotes docetaxel resistance and epithelial-to-mesenchymal transition via the PI3K/Akt signaling pathway in prostate cancer. Arch Med Sci. 2021;17:152–65.
Peng Y, Zheng J, Zhou Y, Li J. Characterization of a novel curcumin analog P1 as potent inhibitor of the NF-κB signaling pathway with distinct mechanisms. Acta Pharmacol Sin. 2013;34:939–50.
Jin R, Yi Y, Yull FE, Blackwell TS, Clark PE, Koyama T, et al. NF-κB gene signature predicts prostate cancer progression. Cancer Res. 2014;74:2763–72.
Gogola S, Rejzer M, Bahmad HF, Abou-Kheir W, Omarzai Y, Poppiti R. Epithelial-to-mesenchymal transition-related markers in prostate cancer: from bench to bedside. Cancers. 2023;15:2309.
Ruscetti M, Quach B, Dadashian EL, Mulholland DJ, Wu H. Tracking and functional characterization of epithelial-mesenchymal transition and mesenchymal tumor cells during prostate cancer metastasis. Can Res. 2015;75:2749–59.
Feinberg AP. Phenotypic plasticity and the epigenetics of human disease. Nature. 2007;447:433–40.
Shi Y. Histone lysine demethylases: emerging roles in development, physiology and disease. Nat Rev Genet. 2007;8:829–33.
Shi R, Liao C, Zhang Q. Hypoxia-driven effects in cancer: characterization, mechanisms, and therapeutic implications. Cells. 2021;10:678.
Naik PP, Panigrahi S, Parida R, Praharaj PP, Bhol CS, Patil S, et al. Metabostemness in cancer: linking metaboloepigenetics and mitophagy in remodeling cancer stem cells. Stem Cell Rev and Rep. 2022;18:198–213.
Baryła M, Semeniuk-Wojtaś A, Róg L, Kraj L, Małyszko M, Stec R. Oncometabolites—A link between cancer cells and tumor microenvironment. Biology. 2022;11:270.
Sciacovelli M, Gonçalves E, Johnson TI, Zecchini VR, da Costa ASH, Gaude E, et al. Fumarate is an epigenetic modifier that elicits epithelial-to-mesenchymal transition. Nature. 2016;537:544–7.
Lu J, Fei F, Wu C, Mei J, Xu J, Lu P. ZEB1: catalyst of immune escape during tumor metastasis. Biomed Pharmacother. 2022;153:113490.
Yu L, Liu S, Zhang C, Zhang B, Simoes BM, Eyre R, et al. Enrichment of human osteosarcoma stem cells based on hTERT transcriptional activity. Oncotarget. 2013;4:2326–38.
Zhang Y, Liu Y, Lang F, Yang C. IDH mutation and cancer stem cell. Essays Biochem. 2022;66:413–22.
Giafaglione JM, Crowell PD, Delcourt AML, Hashimoto T, Ha SM, Atmakuri A, et al. Prostate lineage-specific metabolism governs luminal differentiation and response to antiandrogen treatment. Nat Cell Biol. 2023;25:1821–32.
Ittmann M, Huang J, Radaelli E, Martin P, Signoretti S, Sullivan R, et al. Animal models of human prostate cancer: the consensus report of the New York meeting of the mouse models of human cancers consortium prostate pathology committee. Cancer Res. 2013;73:2718–36.
Slater M, Barden JA, Murphy CR. Changes in growth factor expression in the ageing prostate may disrupt epithelial-stromal homeostasis. Histochem J. 2000;32:357–64.
Shiao SL, Chu GC-Y, Chung LWK. Regulation of prostate cancer progression by the tumor microenvironment. Cancer Lett. 2016;380:340–8.
Chiarugi P, Paoli P, Cirri P. Tumor microenvironment and metabolism in prostate cancer. Semin Oncol. 2014;41:267–80.
Costello LC, Franklin RB. The clinical relevance of the metabolism of prostate cancer; zinc and tumor suppression: connecting the dots. Mol Cancer. 2006;5:17.
Beier A-MK, Puhr M, Stope MB, Thomas C, Erb HHH. Metabolic changes during prostate cancer development and progression. J Cancer Res Clin Oncol. 2023;149:2259–70.
Darby S, Sahadevan K, Khan MM, Robson CN, Leung HY, Gnanapragasam VJ. Loss of Sef (similar expression to FGF) expression is associated with high grade and metastatic prostate cancer. Oncogene. 2006;25:4122–7.
Bedeschi M, Marino N, Cavassi E, Piccinini F, Tesei A. Cancer-associated fibroblast: role in prostate cancer progression to metastatic disease and therapeutic resistance. Cells. 2023;12:802.
Tuxhorn JA, Ayala GE, Rowley DR. Reactive stroma in prostate cancer progression. J Urol. 2001;166:2472–83.
Tuxhorn JA, Ayala GE, Smith MJ, Smith VC, Dang TD, Rowley DR. Reactive stroma in human prostate cancer: induction of myofibroblast phenotype and extracellular matrix remodeling. Clin Cancer Res. 2002;8:2912–23.
Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat Rev Mol Cell Biol. 2002;3:349–63.
Mueller L, Goumas FA, Affeldt M, Sandtner S, Gehling UM, Brilloff S, et al. Stromal fibroblasts in colorectal liver metastases originate from resident fibroblasts and generate an inflammatory microenvironment. Am J Pathol. 2007;171:1608–18.
Kojima Y, Acar A, Eaton EN, Mellody KT, Scheel C, Ben-Porath I, et al. Autocrine TGF-beta and stromal cell-derived factor-1 (SDF-1) signaling drives the evolution of tumor-promoting mammary stromal myofibroblasts. Proc Natl Acad Sci U S A. 2010;107:20009–14.
Direkze NC, Hodivala-Dilke K, Jeffery R, Hunt T, Poulsom R, Oukrif D, et al. Bone marrow contribution to tumor-associated myofibroblasts and fibroblasts. Cancer Res. 2004;64:8492–5.
Potenta S, Zeisberg E, Kalluri R. The role of endothelial-to-mesenchymal transition in cancer progression. Br J Cancer. 2008;99:1375–9.
Zeisberg EM, Tarnavski O, Zeisberg M, Dorfman AL, McMullen JR, Gustafsson E, et al. Endothelial-to-mesenchymal transition contributes to cardiac fibrosis. Nat Med. 2007;13:952–61.
Radisky ES, Radisky DC. Stromal induction of breast cancer: inflammation and invasion. Rev Endocr Metab Disord. 2007;8:279–87.
Franco OE, Jiang M, Strand DW, Peacock J, Fernandez S, Jackson RS, et al. Altered TGF-β signaling in a subpopulation of human stromal cells promotes prostatic carcinogenesis. Cancer Res. 2011;71:1272–81.
Taylor RA, Toivanen R, Frydenberg M, Pedersen J, Harewood L, Australian Prostate Cancer Bioresource, et al. Human epithelial basal cells are cells of origin of prostate cancer, independent of CD133 status. Stem Cells. 2012;30:1087–96.
Russo G, Mischi M, Scheepens W, De la Rosette JJ, Wijkstra H. Angiogenesis in prostate cancer: onset, progression and imaging. BJU Int. 2012;110:E794-808.
Butler JM, Kobayashi H, Rafii S. Instructive role of the vascular niche in promoting tumour growth and tissue repair by angiocrine factors. Nat Rev Cancer. 2010;10:138–46.
Wang X, Lee SO, Xia S, Jiang Q, Luo J, Li L, et al. Endothelial cells enhance prostate cancer metastasis via IL-6→androgen receptor→TGF-β→MMP-9 signals. Mol Cancer Ther. 2013;12:1026–37.
Godoy A, Montecinos VP, Gray DR, Sotomayor P, Yau JM, Vethanayagam RR, et al. Androgen deprivation induces rapid involution and recovery of human prostate vasculature. Am J Physiol Endocrinol Metab. 2011;300:E263-275.
Fidelito G, Watt MJ, Taylor RA. Personalized medicine for prostate cancer: is targeting metabolism a reality? Front Oncol. 2021;11:778761.
Gonzalez-Menendez P, Hevia D, Mayo JC, Sainz RM. The dark side of glucose transporters in prostate cancer: are they a new feature to characterize carcinomas? Int J Cancer. 2018;142:2414–24.
Gonzalez-Menendez P, Hevia D, Alonso-Arias R, Alvarez-Artime A, Rodriguez-Garcia A, Kinet S, et al. GLUT1 protects prostate cancer cells from glucose deprivation-induced oxidative stress. Redox Biol. 2018;17:112–27.
Li J, Ayene R, Ward KM, Dayanandam E, Ayene IS. Glucose deprivation increases nuclear DNA repair protein Ku and resistance to radiation induced oxidative stress in human cancer cells. Cell Biochem Funct. 2009;27:93–101.
De Marzo AM, Platz EA, Sutcliffe S, Xu J, Grönberg H, Drake CG, et al. Inflammation in prostate carcinogenesis. Nat Rev Cancer. 2007;7:256–69.
Martori C, Sanchez-Moral L, Paul T, Pardo JC, Font A, de RuizPorras V, et al. Macrophages as a therapeutic target in metastatic prostate cancer: a way to overcome immunotherapy resistance? Cancers (Basel). 2022;14:440.
de Bono JS, Guo C, Gurel B, De Marzo AM, Sfanos KS, Mani RS, et al. Prostate carcinogenesis: inflammatory storms. Nat Rev Cancer. 2020;20:455–69.
De Nunzio C, Kramer G, Marberger M, Montironi R, Nelson W, Schröder F, et al. The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur Urol. 2011;60:106–17.
Corzo CA, Condamine T, Lu L, Cotter MJ, Youn J-I, Cheng P, et al. HIF-1α regulates function and differentiation of myeloid-derived suppressor cells in the tumor microenvironment. J Exp Med. 2010;207:2439–53.
Zhuang J, Zhang J, Lwin ST, Edwards JR, Edwards CM, Mundy GR, et al. Osteoclasts in multiple myeloma are derived from Gr-1+CD11b+myeloid-derived suppressor cells. PLoS ONE. 2012;7:e48871.
Hu C, Pang B, Lin G, Zhen Y, Yi H. Energy metabolism manipulates the fate and function of tumour myeloid-derived suppressor cells. Br J Cancer. 2020;122:23–9.
Koinis F, Xagara A, Chantzara E, Leontopoulou V, Aidarinis C, Kotsakis A. Myeloid-derived suppressor cells in prostate cancer: present knowledge and future perspectives. Cells. 2022;11:20.
Consiglio CR, Udartseva O, Ramsey KD, Bush C, Gollnick SO. Enzalutamide, an androgen receptor antagonist, enhances myeloid cell-mediated immune suppression and tumor progression. Cancer Immunol Res. 2020;8:1215–27.
Ludwig M, Rajvansh R, Drake JM. Emerging role of extracellular vesicles in prostate cancer. Endocrinology. 2021;162:bqab139.
Gaglani S, Gonzalez-Kozlova E, Lundon DJ, Tewari AK, Dogra N, Kyprianou N. Exosomes as a next-generation diagnostic and therapeutic tool in prostate cancer. Int J Mol Sci. 2021;22:10131.
Gao F, Xu Q, Tang Z, Zhang N, Huang Y, Li Z, et al. Exosomes derived from myeloid-derived suppressor cells facilitate castration-resistant prostate cancer progression via S100A9/circMID1/miR-506-3p/MID1. J Transl Med. 2022;20:346.
Xu F, Wang X, Huang Y, Zhang X, Sun W, Du Y, et al. Prostate cancer cell-derived exosomal IL-8 fosters immune evasion by disturbing glucolipid metabolism of CD8+ T cell. Cell Rep. 2023;42:113424.
Wang Z-H, Peng W-B, Zhang P, Yang X-P, Zhou Q. Lactate in the tumour microenvironment: from immune modulation to therapy. EBioMedicine. 2021;73:103627.
Li X, Yang Y, Zhang B, Lin X, Fu X, An Y, et al. Lactate metabolism in human health and disease. Sig Transduct Target Ther. 2022;7:1–22.
Sonveaux P, Végran F, Schroeder T, Wergin MC, Verrax J, Rabbani ZN, et al. Targeting lactate-fueled respiration selectively kills hypoxic tumor cells in mice. J Clin Invest. 2008;118:3930–42.
Hui S, Ghergurovich JM, Morscher RJ, Jang C, Teng X, Lu W, et al. Glucose feeds the TCA cycle via circulating lactate. Nature. 2017;551:115–8.
Li F, Simon MC. Cancer cells don’t live alone: metabolic communication within tumor microenvironments. Dev Cell. 2020;54:183–95.
Doldi V, Callari M, Giannoni E, D’Aiuto F, Maffezzini M, Valdagni R, et al. Integrated gene and miRNA expression analysis of prostate cancer associated fibroblasts supports a prominent role for interleukin-6 in fibroblast activation. Oncotarget. 2015;6:31441–60.
Valencia T, Kim JY, Abu-Baker S, Moscat-Pardos J, Ahn CS, Reina-Campos M, et al. Metabolic reprogramming of stromal fibroblasts through p62-mTORC1 signaling promotes inflammation and tumorigenesis. Cancer Cell. 2014;26:121–35.
Fiaschi T, Marini A, Giannoni E, Taddei ML, Gandellini P, De Donatis A, et al. Reciprocal metabolic reprogramming through lactate shuttle coordinately influences tumor-stroma interplay. Cancer Res. 2012;72:5130–40.
Pértega-Gomes N, Vizcaíno JR, Attig J, Jurmeister S, Lopes C, Baltazar F. A lactate shuttle system between tumour and stromal cells is associated with poor prognosis in prostate cancer. BMC Cancer. 2014;14:352.
Giannoni E, Taddei ML, Morandi A, Comito G, Calvani M, Bianchini F, et al. Targeting stromal-induced pyruvate kinase M2 nuclear translocation impairs oxphos and prostate cancer metastatic spread. Oncotarget. 2015;6:24061–74.
Choi SYC, Xue H, Wu R, Fazli L, Lin D, Collins CC, et al. The MCT4 gene: a novel, potential target for therapy of advanced prostate cancer. Clin Cancer Res. 2016;22:2721–33.
Pereira-Nunes A, Simões-Sousa S, Pinheiro C, Miranda-Gonçalves V, Granja S, Baltazar F. Targeting lactate production and efflux in prostate cancer. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165894.
El-Kenawi A, Gatenbee C, Robertson-Tessi M, Bravo R, Dhillon J, Balagurunathan Y, et al. Acidity promotes tumour progression by altering macrophage phenotype in prostate cancer. Br J Cancer. 2019;121:556–66.
Chaudagar K, Hieromnimon HM, Khurana R, Labadie B, Hirz T, Mei S, et al. Reversal of lactate and PD-1-mediated macrophage immunosuppression controls growth of PTEN/p53-deficient prostate cancer. Clin Cancer Res. 2023;29:1952–68.
Bonuccelli G, Tsirigos A, Whitaker-Menezes D, Pavlides S, Pestell RG, Chiavarina B, et al. Ketones and lactate “fuel” tumor growth and metastasis: evidence that epithelial cancer cells use oxidative mitochondrial metabolism. Cell Cycle. 2010;9:3506–14.
Martinez-Outschoorn UE, Pavlides S, Howell A, Pestell RG, Tanowitz HB, Sotgia F, et al. Stromal-epithelial metabolic coupling in cancer: integrating autophagy and metabolism in the tumor microenvironment. Int J Biochem Cell Biol. 2011;43:1045–51.
Luo G, He Y, Yu X. Bone marrow adipocyte: an intimate partner with tumor cells in bone metastasis. Front Endocrinol (Lausanne). 2018;9:339.
Cutruzzolà F, Giardina G, Marani M, Macone A, Paiardini A, Rinaldo S, et al. Glucose metabolism in the progression of prostate cancer. Front Physiol. 2017;8:97.
Diedrich JD, Rajagurubandara E, Herroon MK, Mahapatra G, Hüttemann M, Podgorski I. Bone marrow adipocytes promote the Warburg phenotype in metastatic prostate tumors via HIF-1α activation. Oncotarget. 2016;7:64854–77.
Whitburn J, Rao SR, Morris EV, Tabata S, Hirayama A, Soga T, et al. Metabolic profiling of prostate cancer in skeletal microenvironments identifies G6PD as a key mediator of growth and survival. Sci Adv. 2022;8:eabf9096.
Richman EL, Kenfield SA, Stampfer MJ, Giovannucci EL, Zeisel SH, Willett WC, et al. Choline intake and risk of lethal prostate cancer: incidence and survival123. Am J Clin Nutr. 2012;96:855–63.
Mori N, Wildes F, Takagi T, Glunde K, Bhujwalla ZM. The tumor microenvironment modulates choline and lipid metabolism. Front Oncol. 2016;6:262.
Vykoukal J, Fahrmann JF, Gregg JR, Tang Z, Basourakos S, Irajizad E, et al. Caveolin-1-mediated sphingolipid oncometabolism underlies a metabolic vulnerability of prostate cancer. Nat Commun. 2020;11:4279.
Siltari A, Syvälä H, Lou Y-R, Gao Y, Murtola TJ. Role of lipids and lipid metabolism in prostate cancer progression and the tumor’s immune environment. Cancers (Basel). 2022;14:4293.
Neuwirt H, Bouchal J, Kharaishvili G, Ploner C, Jöhrer K, Pitterl F, et al. Cancer-associated fibroblasts promote prostate tumor growth and progression through upregulation of cholesterol and steroid biosynthesis. Cell Commun Signal. 2020;18:11.
Mishra R, Haldar S, Placencio V, Madhav A, Rohena-Rivera K, Agarwal P, et al. Stromal epigenetic alterations drive metabolic and neuroendocrine prostate cancer reprogramming. J Clin Invest. 2018;128:4472–84.
Matos A, Carvalho M, Bicho M, Ribeiro R. Arginine and arginases modulate metabolism, tumor microenvironment and prostate cancer progression. Nutrients. 2021;13:4503.
Tsai C-S, Chen F-H, Wang C-C, Huang H-L, Jung S-M, Wu C-J, et al. Macrophages from irradiated tumors express higher levels of iNOS, arginase-I and COX-2, and promote tumor growth. Int J Radiat Oncol Biol Phys. 2007;68:499–507.
Gannon PO, Godin-Ethier J, Hassler M, Delvoye N, Aversa M, Poisson AO, et al. Androgen-regulated expression of arginase 1, arginase 2 and interleukin-8 in human prostate cancer. PLoS ONE. 2010;5:e12107.
Bronte V, Kasic T, Gri G, Gallana K, Borsellino G, Marigo I, et al. Boosting antitumor responses of T lymphocytes infiltrating human prostate cancers. J Exp Med. 2005;201:1257–68.
Cimen Bozkus C, Elzey BD, Crist SA, Ellies LG, Ratliff TL. Expression of cationic amino acid transporter 2 is required for myeloid-derived suppressor cell-mediated control of T cell immunity. J Immunol. 2015;195:5237–50.
Hossain DMS, Pal SK, Moreira D, Duttagupta P, Zhang Q, Won H, et al. TLR9-targeted STAT3 silencing abrogates immunosuppressive activity of myeloid-derived suppressor cells from prostate cancer patients. Clin Cancer Res. 2015;21:3771–82.
Zhunussova A, Sen B, Friedman L, Tuleukhanov S, Brooks AD, Sensenig R, et al. Tumor microenvironment promotes dicarboxylic acid carrier-mediated transport of succinate to fuel prostate cancer mitochondria. Am J Cancer Res. 2015;5:1665–79.
Sant’Anna-Silva ACB, Perez-Valencia JA, Sciacovelli M, Lalou C, Sarlak S, Tronci L, et al. Succinate anaplerosis has an onco-driving potential in prostate cancer cells. Cancers (Basel). 2021;13:1727.
Zhao H, Yang L, Baddour J, Achreja A, Bernard V, Moss T, et al. Tumor microenvironment derived exosomes pleiotropically modulate cancer cell metabolism. Elife. 2016;5:e10250.
Deshmukh A, Deshpande K, Arfuso F, Newsholme P, Dharmarajan A. Cancer stem cell metabolism: a potential target for cancer therapy. Mol Cancer. 2016;15:69.
Sancho P, Barneda D, Heeschen C. Hallmarks of cancer stem cell metabolism. Br J Cancer. 2016;114:1305–12.
Della Sala G, Pacelli C, Agriesti F, Laurenzana I, Tucci F, Tamma M, et al. Unveiling metabolic vulnerability and plasticity of human osteosarcoma stem and differentiated cells to improve cancer therapy. Biomedicines. 2021;10:28.
Ren L, Ruiz-Rodado V, Dowdy T, Huang S, Issaq SH, Beck J, et al. Glutaminase-1 (GLS1) inhibition limits metastatic progression in osteosarcoma. Cancer Metab. 2020;8:4.
Lai HW, Kasai M, Yamamoto S, Fukuhara H, Karashima T, Kurabayashi A, et al. Metabolic shift towards oxidative phosphorylation reduces cell-density-induced cancer-stem-cell-like characteristics in prostate cancer in vitro. Biol Open. 2023;12:bio059615.
Reznik E, Luna A, Aksoy BA, Liu EM, La K, Ostrovnaya I, et al. A landscape of metabolic variation across tumor types. Cell Syst. 2018;6:301-313.e3.
Rodrigues AS, Pereira SL, Ramalho-Santos J. Stem metabolism: insights from oncometabolism and vice versa. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165760.
Yamamoto T, Hatabayashi K, Arita M, Yajima N, Takenaka C, Suzuki T, et al. Kynurenine signaling through the aryl hydrocarbon receptor maintains the undifferentiated state of human embryonic stem cells. Sci Signal. 2019;12:eaaw3306.
Qiu S, Cai Y, Yao H, Lin C, Xie Y, Tang S, et al. Small molecule metabolites: discovery of biomarkers and therapeutic targets. Signal Transduct Target Ther. 2023;8(1):132.
Struck-Lewicka W, Kordalewska M, Bujak R, Yumba Mpanga A, Markuszewski M, Jacyna J, et al. Urine metabolic fingerprinting using LC-MS and GC-MS reveals metabolite changes in prostate cancer: a pilot study. J Pharm Biomed Anal. 2015;11(1):351–61.
Beyoğlu D, Idle JR. Metabolic rewiring and the characterization of oncometabolites. Cancers. 2021;13(12):2900.
Gouasmi R, Ferraro-Peyret C, Nancey S, Coste I, Renno T, Chaveroux C, et al. The kynurenine pathway and cancer: why keep it simple when you can make it complicated. Cancers. 2022;14(11):2793.
Ahmad F, Cherukuri MK, Choyke PL. Metabolic reprogramming in prostate cancer. Br J Cancer. 2021;125:1185–96.
Lynch MJ, Nicholson JK. Proton MRS of human prostatic fluid: correlations between citrate, spermine, and myo-inositol levels and changes with disease. Prostate. 1997;30(4):248–55.
Kline EE, Treat EG, Averna TA, Davis MS, Smith AY, Sillerud LO. Citrate concentrations in human seminal fluid and expressed prostatic fluid determined via 1H nuclear magnetic resonance spectroscopy outperform prostate specific antigen in prostate cancer detection. J Urol. 2006;176(5):2274–9.
Serkova NJ, Gamito EJ, Jones RH, O’Donnell C, Brown JL, Green S, et al. The metabolites citrate, myo-inositol, and spermine are potential age-independent markers of prostate cancer in human expressed prostatic secretions. Prostate. 2008;68(6):620–8.
Averna TA, Kline EE, Smith AY, Sillerud LO. A decrease in 1H nuclear magnetic resonance spectroscopically determined citrate in human seminal fluid accompanies the development of prostate adenocarcinoma. JUrol. 2005;173(2):433–8.
Tessem MB, Bertilsson H, Angelsen A, Bathen TF, Drabløs F, Rye MB. A balanced tissue composition reveals new metabolic and gene expression markers in prostate cancer. PLoS ONE. 2016;11(4):e0153727.
Tessem MB, Swanson MG, Keshari KR, Albers MJ, Joun D, Tabatabai ZL, et al. Evaluation of lactate and alanine as metabolic biomarkers of prostate cancer using 1H HR-MAS spectroscopy of biopsy tissues. Magn Reson Med. 2008;60(3):510–6.
Ramirez-Garrastacho M, Bajo-Santos C, Line A, Martens-Uzunova ES, de la Fuente JM, Moros M, et al. Extracellular vesicles as a source of prostate cancer biomarkers in liquid biopsies: a decade of research. Br J Cancer. 2021.
Clos-Garcia M, Loizaga-Iriarte A, Zuñiga-Garcia P, Sánchez-Mosquera P, Rosa Cortazar A, González E, et al. Metabolic alterations in urine extracellular vesicles are associated to prostate cancer pathogenesis and progression. J Extracell Vesicles. 2018;7(1):1470442.
Palviainen M, Laukkanen K, Tavukcuoglu Z, Velagapudi V, Kärkkäinen O, Hanhineva K, et al. Cancer alters the metabolic fingerprint of extracellular vesicles. Cancers. 2020;12(11):3292.
Flavin R, Zadra G, Loda M. Metabolic alterations and targeted therapies in prostate cancer. J Pathol. 2011;223:284–95.
Czernin J, Benz MR, Allen-Auerbach MS. PET imaging of prostate cancer using 11 C-Acetate. Positron Emission Tomography. 2009;4:163–72.
Zadra G, Loda M. Metabolic vulnerabilities of prostate cancer: diagnostic and therapeutic opportunities. Cold Spring Harb Perspect Med. 2018;8:a030569.
Mullen AR, Wheaton WW, Jin ES, Chen PH, Sullivan LB, Cheng T, et al. Reductive carboxylation supports growth in tumour cells with defective mitochondria. Nature. 2011;481:385–8.
Bader DA, Hartig SM, Putluri V, Foley C, Hamilton MP, Smith EA, et al. Mitochondrial pyruvate import is a metabolic vulnerability in androgen receptor-driven prostate cancer. Nat Metabol. 2018;2018(1):70–85.
Molina JR, Sun Y, Protopopova M, Gera S, Bandi M, Bristow C, et al. An inhibitor of oxidative phosphorylation exploits cancer vulnerability. Nat Med. 2018;24:1036–46.
Naguib A, Mathew G, Reczek CR, Watrud K, Ambrico A, Herzka T, et al. Mitochondrial complex I inhibitors expose a vulnerability for selective killing of Pten-null cells. Cell Rep. 2018;23(1):58–67.
Roy S, Malone S, Grimes S, Morgan SC. Impact of concomitant medications on biochemical outcome in localised prostate cancer treated with radiotherapy and androgen deprivation therapy. Clin Oncol. 2021;33(3):181–90.
Nguyen MM, Martinez JA, Hsu CH, Sokoloff M, Krouse RS, Gibson BA, et al. Bioactivity and prostate tissue distribution of metformin in a preprostatectomy prostate cancer cohort. Eur J Cancer Prev. 2018;27(6):557–62.
Zaidi S, Gandhi J, Joshi G, Smith NL, Khan SA. The anticancer potential of metformin on prostate cancer. Prostate Cancer Prostatic Dis. 2019;22(3):351–61.
Sahra IB, Laurent K, Giuliano S, Larbret F, Ponzio G, Gounon P, et al. Targeting cancer cell metabolism: The combination of metformin and 2-deoxyglucose induces p53-dependent apoptosis in prostate cancer cells. Cancer Res. 2010;70(6):2465–75.
Zadra G, Photopoulos C, Tyekucheva S, Heidari P, Weng QP, Fedele G, et al. A novel direct activator of AMPK inhibits prostate cancer growth by blocking lipogenesis. EMBO Mol Med. 2014;6(4):519–38.
Chen HW, Chang YF, Chuang HY, Tai WT, Hwang JJ. Targeted therapy with fatty acid synthase inhibitors in a human prostate carcinoma LNCaP/tk-luc-bearing animal model. Prostate Cancer Prostatic Dis. 2012;15(3):260–4.
Ventura R, Mordec K, Waszczuk J, Wang Z, Lai J, Fridlib M, et al. Inhibition of de novo palmitate synthesis by fatty acid synthase induces apoptosis in tumor cells by remodeling cell membranes, inhibiting signaling pathways, and reprogramming gene expression. EBioMedicine. 2015;2(8):808–24.
Guth A, Monk E, Agarwal R, Bergman BC, Zemski-Berry KA, Minic A, et al. Targeting fat oxidation in mouse prostate cancer decreases tumor growth and stimulates anti-cancer immunity. Int J Mol Sci. 2020;21:9660.
Flaig TW, Salzmann-Sullivan M, Su LJ, Zhang Z, Joshi M, Gijón MA, et al. Lipid catabolism inhibition sensitizes prostate cancer cells to antiandrogen blockade. Oncotarget. 2017;8(34):56051–65.
Myint ZW, Sun RC, Hensley PJ, James AC, Wang P, Strup SE, et al. Evaluation of glutaminase expression in prostate adenocarcinoma and correlation with clinicopathologic parameters. Cancers. 2021;13(9):2157.
Zhao SG, Chen WS, Li H, Foye A, Zhang M, Sjöström M, et al. The DNA methylation landscape of advanced prostate cancer. Nat Genet. 2020;52(8):778–89.
Crispo F, Pietrafesa M, Condelli V, Maddalena F, Bruno G, Piscazzi A, et al. IDH1 targeting as a new potential option for intrahepatic cholangiocarcinoma treatment-current state and future perspectives. Molecules. 2020;25:3754.
Sumbly V, Landry I, Rizzo V. Ivosidenib for IDH1 mutant cholangiocarcinoma: a narrative review. Cureus. 2022;14:e21018.
Adeva J. Current development and future perspective of IDH1 inhibitors in cholangiocarcinoma. Liver Cancer Int. 2022;3:17–31.
Mellinghoff IK, van den Bent MJ, Blumenthal DT, Touat M, Peters KB, Clarke J, et al. Vorasidenib in IDH1- or IDH2-mutant low-grade glioma. N Engl J Med. 2023;389:589–601.
Tanabe S, Quader S, Cabral H, Ono R. Interplay of EMT and CSC in cancer and the potential therapeutic strategies. Front Pharmacol. 2020;11:904.
Jayachandran A, Dhungel B, Steel JC. Epithelial-to-mesenchymal plasticity of cancer stem cells: therapeutic targets in hepatocellular carcinoma. J Hematol Oncol. 2016;9:74.
Chaves LP, Melo CM, Saggioro FP, dos Reis RB, Squire JA. Epithelial-mesenchymal transition signaling and prostate cancer stem cells: emerging biomarkers and opportunities for precision therapeutics. Genes. 2021;12:1900.
Tomacha J, Dokduang H, Padthaisong S, Namwat N, Klanrit P, Phetcharaburanin J, et al. Targeting fatty acid synthase modulates metabolic pathways and inhibits cholangiocarcinoma cell progression. Front Pharmacol. 2021;12:696961.
Kitagawa A, Osawa T, Noda M, Kobayashi Y, Aki S, Nakano Y, et al. Convergent genomic diversity and novel BCAA metabolism in intrahepatic cholangiocarcinoma. Br J Cancer. 2023;128:2206–17.
Acknowledgements
Not applicable.
Funding
I.D. was supported by the Ministero dell’Istruzione, dell’Università e della Ricerca (MIUR), and R.M.-S. by the Spanish Ministry of Science and Innovation (MINECO-PID2019-111418RB-100). G.A. is funded thanks to a fellowship supported by the Fondazione Umberto Veronesi. S.A.-R. is funded by “Severo Ochoa” program (FICYT, Principado de Asturias). P. G.-M. and M.C. are supported by the “Ramon y Cajal” program (RYC-2021–033856-I and RYC2021-031003-I) from the Spanish Ministry of Science and Innovation, Agencia Estatal de Investigación (MCIN/AEI/https://doi.org/10.13039/501100011033), and European UnionNextGeneration (EU/PRTR). G.V. was supported by the Instituto de Salud Carlos III (ISCIII) and confounded by the European Regional Development Fund (ERDF), “A way to make Europe”, grant number PI18/00442 integrated into the State Plan for R & D + I 2017–2020 and grant number PI21/00343 integrated into the State Plan for R &; D + I 2021–2023, by the European Commission through the Horizon 2020 European Training Networks program, grant number H2020-MSCA-ITN-308 2016 721532 and by the Madrid Region Government Network Program in Biosciences, grant number S2022/BMD-7434 (ASAP-CM).
Author information
Authors and Affiliations
Contributions
G.A.: Writing-original draft, Writing-review editing, Figure preparation.M.C.: Conceptualization, Writing-review editing, Supervision.A.Z. and G.V.: Writing-review editing, Figure Preparation, Supervision.S.A-R. and R.M.-S.: Writing-original draft, Figure Preparation, Writing-review editing.P. G.-M. and I.D.: Conceptualization, Writing-original draft, Writing-review editing, Figure preparation, Supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ambrosini, G., Cordani, M., Zarrabi, A. et al. Transcending frontiers in prostate cancer: the role of oncometabolites on epigenetic regulation, CSCs, and tumor microenvironment to identify new therapeutic strategies. Cell Commun Signal 22, 36 (2024). https://doi.org/10.1186/s12964-023-01462-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12964-023-01462-0