Abstract
Background
Lung infections caused by Streptococcus pneumonia are a global leading cause of death. The reactive oxygen species H2O2 is one of the virulence factors of Streptococcus pneumoniae. The Golgi apparatus is essential for the inflammatory response of a eukaryotic cell. Golgi fragmentation was previously shown to be induced by bacterial pathogens and in response to H2O2 treatment. This led us to investigate whether the Golgi apparatus is actively involved and targeted in host–pathogen interactions during pneumococcal infections.
Methods
Following in vitro infection of BEAS-2B bronchial epithelial cells with Streptococcus pneumoniae for 16 h, the structure of the Golgi apparatus was assessed by fluorescence staining of the Golgi-associated protein, Golgin-97. To investigate the effect of H2O2 production on Golgi structure, BEAS-2B cells were treated with H2O2 or the H2O2 degrading enzyme Catalase, prior to Golgi staining. Artificial disruption of the Golgi apparatus was induced by treatment of cells with the GBF1 inhibitor, Golgicide A. A proinflammatory cellular response was induced by treatment of cells with the bacterial cell wall component and TLR4 ligand lipoteichoic acid.
Results
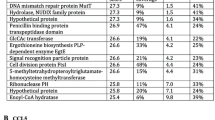
In vitro infection of bronchial epithelial cells with wild type Streptococcus pneumoniae led to a disruption of normal Golgi structure. Golgi fragmentation was not observed after deletion of the pneumococcal H2O2-producing gene, spxB, or neutralization of H2O2 by catalase treatment, but could be induced by H2O2 treatment. Streptococcus pneumoniae infection significantly reduced host cell protein glycosylation and artificial disruption of Golgi structure significantly reduced bacterial adherence, but increased bacterial counts in the supernatant. To understand if this effect depended on cell-contact or soluble factors, pneumococci were treated with cell-supernatant of cells treated with Golgicide A and/or lipoteichoic acid. This approach revealed that lipoteichoic acid conditioned medium inhibits bacterial replication in presence of host cells. In contrast, artificial Golgi fragmentation by Golgicide A treatment prior to lipoteichoic acid treatment rescued bacterial replication. This effect was associated with an increase of IL-6 and IL-8 in the supernatant of lipoteichoic acid treated cells. The increased cytokine release was abolished if cells were treated with Golgicide A prior to lipoteichoic acid treatment.
Conclusion
Streptococcus pneumoniae disrupts the Golgi apparatus in an H2O2-dependent manner, thereby inhibiting paracrine anti-infective mechanisms.
Video Abstract
Similar content being viewed by others
Background
Streptococcus pneumoniae (Spn) is a major agent of community acquired pneumonia, as well as other invasive infectious diseases like otitis media, meningitis and sepsis, thereby causing an estimated 829.000 annual deaths, globally [1]. Typically, pneumococcal disease starts with asymptomatic bacterial colonization of the upper respiratory tract. If the immune system is weakened, the bacteria may advance to the lower respiratory tract and start to replicate in the lung alveoli, causing pneumonia.
Spn employs an array of virulence factors in order to successfully adhere to host cells, evade the immune system and progress through the epithelial barrier. Amongst those are an array of often glycosylated surface proteins which mediate adherence to the host epithelium [2,3,4]. In addition to these surface structures, Spn virulence factors comprise soluble factors such as the pore-forming cytolysin pneumolysin and the oxidant H2O2.
H2O2 in Spn is produced predominantly by the pneumococcal pyruvate oxidase (spxB) as a by-product of acetyl-pyruvate production [5]. It then accumulates due to the absence of the H2O2-degrading enzyme catalase [6]. In host–pathogen interaction during pneumococcal infection, H2O2 was shown to induce DNA damage and apoptosis in alveolar epithelial cells [7]. It was, furthermore, shown to suppress the NLRP3 and NLRC4 dependent inflammasome and mediate pneumococcal protection against the innate immune response [8].
The lung epithelium constitutes the first line of defense against pneumococcal infection in the lower airways. Upon detection of pathogens, it orchestrates a strong proinflammatory response to recruit immune cells and clear the site of infection. The Golgi apparatus (Golgi) is a host cell organelle with multi-faceted functions. Intracellular trafficking and sorting mediated through the Golgi is vital for the proper execution of the proinflammatory response. Newly synthesized proteins enter the Golgi through the nucleus-facing cis-Golgi network. Golgi-membrane associated tethering proteins transport these new proteins towards the trans-Golgi cisterna and the trans-Golgi network [9]. Tethering proteins within the trans-Golgi network then sort the proteins by destination [10]. A second main function of the Golgi is the posttranslational glycosylation of proteins. Glycosyltransferases and are distributed through the Golgi in a defined sequence reaching from the cis- to the trans-Golgi-network, catalyzing the attachment of glycosylation motifs onto the protein [11]. It was recently shown that the Golgi apparatus exhibits structural damage upon H2O2 treatment [12].
In this study, we analysed whether Spn infection of BEAS-2B lung epithelial cells interferes with Golgi structure and function and found an H2O2-dependent fragmentation of the Golgi upon Spn infection. Artificial disruption of the Golgi resulted in attenuated cytokine secretion and increased bacterial replication, thereby promoting the infection process.
Material and methods
Cultivation and stimulation of BEAS-2B cells
The human bronchial epithelial cell line BEAS-2B was obtained from ATCC (CRL-9606) and cultivated in BEGM medium (Lonza, CC-3170) according to ATCC guidelines without fibronectin coating. Approximately 2*105 cells per well were seeded into 24 well-plates (surface area 1.1 cm2) and cultivated for 24 h prior to infection/stimulation. For stimulation experiments, medium was exchanged and cells were treated with H2O2 (Sigma-Aldrich, H1009), 40 or 80 µM for 24 h or with Golgicide A (Tocris, 3584), 4 µM for 4 or 24 h. To generate Golgicide A/lipoteichoic acid (LTA) conditioned supernatants, cells were first treated with Golgicide A, 4 µM for 4 h. Afterwards, medium was exchanged and cells were treated with LTA, 1 µg/ml for additional 2 h and medium collected.
Bacterial cultivation and infection of BEAS-2B cells
Spn strains D39, TIGR4, D39ΔspxB and D39Δply were kindly provided by Sven Hammerschmidt (University of Greifswald). Spn was incubated over night at 37 °C / 5% CO2 on Columbia Blood agar plates (Becton Dickinson, 254005). Single colonies were inoculated into THY media (30 g/l Todd-Hewitt-Bouillon, Roth, X936.1 and 5 g/l yeast extract, Roth, 2363.2) and incubated at 37 °C / 5% CO2 until early logarithmic phase (approx. OD600 = 0.33) was reached. For BEAS-2B infection, bacteria were centrifuged (3000xg, 10 min) and inoculated into fresh bronchial epithelial cell growth medium (BEGM) according to desired multiplicity of infection (MOI). Control cells were left untreated. For adherence and internalization assays, BEAS-2B were infected at MOI 20 for 2 h. Infected cells were washed with PBS to remove non-adherent bacteria. Cells were then detached using trypsin and lysed in distilled H2O. Dilutions of the cell lysate were plated on blood agar plates to determine CFU.
Cell viability measurement
MTT assays were performed on 96-well plates to assess cell viability. After stimulation or infection, medium was replaced with fresh medium, supplemented with 0.5 mg/ml MTT reagent (Merck, CT01-5). Cells were incubated for approx. 3 h, until visible dark crystals had formed. Medium was removed and crystals dissolved in 100 µl 1:1 DMSO:EtOH. Absorbance was measured in a plate reader at λ = 570 nm. Viability was assessed as absorbance of treated samples relative to control cells.
Immuno-fluorescence staining
BEAS-2B cells were seeded and cultivated on 12 mm glass slides. After stimulation or infection, cells were washed with PBS and fixed with 4% paraformaldehyde for 20 min at room temperature. After blocking with 4% milk powder in PBS, cells were incubated with the primary antibody (mouse α Golgin-97, ThermoFisher, 14–9767-82), diluted 1:50 in TBS + 0.35% TritonX-100 for 2 h. Cells were washed with PBS and incubated with the secondary antibody (Goat α mouse, Alexa Fluor 488, ThermoFisher, A-11001; dilution 1:500) and DAPI (1:1000, Sigma, D9542), in TBS + TritonX-100 for 30 min. Cells were washed three times with PBS and once with distilled water and embedded in Mowiol® 4–88 prior to microscopy. Fluorescence images were taken using an AXIO Verta1 microscope (Zeiss) with a TCS SP5 II camera with HCX PL (Leica) at 1000-fold magnification.
Quantification of the Golgi surface area
For quantification of the Golgi area, we adjusted a method published previously [13]. Fluorescence images were converted into binary images using Fiji ImageJ, V2.9.0: First, the signal intensity over the whole image was determined. A threshold for conversion into a binary image was set so that only signals with an intensity of at least 15% of the maximum signal intensity were included. The whole signal area was then measured as surface area and normalized against the cell count as determined by counting DAPI-stained nuclei.
Cytokine measurement
Supernatant containing secreted proteins was reduced to 100 µl volume by vacuum evaporation at 30 °C for 7 h. A panel of 13 different cytokines was detected in the concentrated supernatant using the LEGENDplex™ human inflammation panel 1 multiplex FACS kit (BioLegend, Cat: 740809, Lot No. B347171); of these, IL-6, IL-8 and IL-18 were reproducibly detected above quantification threshold. Experiments were performed according to manufacturer's protocol and measured on a BD FACSymphony A1 flow cytometer with BD FACS diva 9.0 software. Results were analyzed using LEGENDplex™ Data Analysis Software Suite.
Statistics
Data was plotted and analyzed using Prism software V9.5.0 (GraphPad, La Jolla, USA). Data are depicted as mean values + SEM for at least three biologically independent replicates. P-values ≤ 0.05 were considered statistically significant and marked with *. Unless indicated otherwise, tests were performed vs. corresponding control.
Results
Spn infection induces breakdown of Golgi structure
We first assessed the effect of Spn D39 infection on Golgi integrity in bronchial epithelial cells using immunofluorescence staining for Golgin-97. Upon pneumococcal infection, we found a disruption of Golgi integrity as defined by a scattered fluorescence signal (Fig. 1A). Quantification of the total signal distribution showed an approximately two-fold increase of total Golgi area upon Spn infection, compared to uninfected controls (Fig. 1B). The same effect was observed when infecting BEAS-2B cells with the predominantly extracellular but highly aggressive pneumococcal strain TIGR4 (Figure S1).
Spn infection disrupts the structural integrity of the Golgi apparatus. BEAS-2B cells were infected with Spn D39, MOI 1 for 16 h or left uninfected. Cells were fixed and fluorescence stained for Golgin-97 and the nucleus (DAPI). Binary images were generated and used to quantify the Golgi area. A Immunofluorescence images. Overlays were generated using the false-colored DAPI- and Golgin-97 images. B Quantification of the Golgi surface area, normalized to uninfected controls. (Statistics: paired two-tailed t-test; * = p < 0.05; Scale: 10 µm; at least 600 cells from 5 independent experiments were quantified)
Deletion of the pneumococcal peroxidase rescues Golgi integrity
As H2O2 is an important Spn virulence factor and was previously shown to induce Golgi scattering, we next aimed to determine if H2O2 is involved in Spn-mediated disruption of the Golgi apparatus. BEAS-2B cells were infected with a Spn D39 strain that is deficient of the H2O2-producing pneumococcal peroxidase (ΔspxB). Afterwards, cells were fluorescence stained and the Golgi surface area was quantified. The ΔspxB strain induced less Golgi scattering than wild type Spn D39 without affecting cell viability, supporting a H2O2-dependent mechanism of Golgi disruption (Fig. 2A, B, C). We further assessed, whether the pneumococcal pore-forming toxin pneumolysin is involved in Golgi fragmentation. However, deletion of pneumolysin did not significantly affect the ability of Spn to induce Golgi fragmentation, compared to the wild type strain (Figure S2).
Deletion of the pneumococcal peroxidase rescues Golgi integrity. BEAS-2B cells were infected with Spn D39 WT or Spn D39 ΔspxB or left untreated. Cells were fixed and fluorescence stained for Golgin-97 and the nucleus (DAPI). A Immunofluorescence images of infected and uninfected cells. B Quantification of the Golgi surface area, relative to uninfected controls. C 16 h post infection, mitochondrial activity was assessed by MTT assay. (Statistics: paired two-tailed t-test for ΔspxB vs. WT; * = p < 0.05; Scale: 10 µm; at least 500 cells from 4 independent experiments were quantified)
H 2 O 2 inactivation prevents Golgi disruption
To confirm the association of H2O2 production and Golgi scattering, we treated Spn D39 WT-infected BEAS-2B cells with the H2O2 degrading enzyme Catalase during infection (Fig. 3 A, B). Additionally, we treated cells directly with 40 or 80 µM H2O2 for 16 h prior to Golgi staining (Fig. 3 C, D). While Catalase treatment protected the Golgi structure upon Spn infection, H2O2 treatment induced Golgi disruption in a concentration-dependent manner. Taken together, these results support a H2O2 dependency of Spn induced Golgi scattering.
H2O2 production induces Golgi disruption. A BEAS-2B cells were infected with Spn D39 WT, MOI 1 for 16 h with or without addition of recombinant Catalase or left untreated. Cells were fixed and Golgin-97 and the nucleus stained. B Quantification of (A). C Cells were treated with H2O2 at indicated concentrations for 16 h. Cells were fixed and Golgin-97 and the nucleus stained. D Quantification of (C). (Statistics: paired two-tailed t-test; * = p < 0.05; Scale: 10 µm; at least 500 cells from 4 independent experiments were quantified)
Golgi disruption reduces bacterial adherence but increases replication
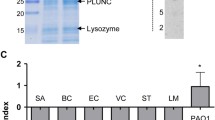
As the Golgi plays an important role in mediating protein glycosylation, we hypothesized that pneumococcal interference with the Golgi might affect bacterial adherence to the host cell at the beginning of the infection process. To test our hypothesis, BEAS-2B cells were treated with Golgicide A to artificially induce Golgi fragmentation, prior to infection with Spn. Successful Golgi disruption and unaffected cell viability was confirmed by immunofluorescence microscopy and MTT assay (Figure S3). We found that Golgi disruption resulted in a 0.6-fold reduced bacterial adherence (Fig. 4A). Next, we assessed the influence of Golgicide A treatment on the bacterial replication during the infection process. Following Golgicide A treatment, bacterial replication in the cell culture media was increased by factor 2.8 compared to untreated controls, suggesting that Golgi disruption causes impaired secretion of antibacterial factors (Fig. 4B). To test whether these factors exert antibacterial effects directly or via a host cell-dependent mechanism, we induced pro-inflammatory activation of control or Golgicide A-treated cells using the TLR2-ligand LTA, followed by collection of the conditioned media (experimental setup illustrated in Fig. 4C). In absence of host cells, conditioned media did not influence bacterial replication, ruling out a direct antibacterial effect (Fig. 4D). However, when naïve cells were treated with conditioned media prior to infection, supernatant of LTA-stimulated, but not Golgicide A-treated cells reduced bacterial replication (Fig. 4D). In contrast, bacterial replication was rescued when supernatants were generated from cells treated with Golgicide A prior to LTA treatment. We therefore measured the quantity of anti-bacterial cytokines IL-6, IL-8 and IL-18. LTA treatment increased the secretion of IL-6 and IL-8 in cells with intact Golgi apparatus, whereas cytokine induction was abolished in Golgicide A treated cells (Fig. 4E, F, G). In summary, disruption of the Golgi apparatus leads to altered host cell glycosylation patterns and impaired cytokine secretion, which is associated with increased bacterial growth.
Golgi disruption reduces bacterial adherence but improves replication. A BEAS-2B cells were stimulated with Golgicide A, 4 µM or DMSO for 24 h. Afterwards, cells were infected with Spn D39, MOI 20 for 2 h. Cells were detached, lysed in distilled water and serial dilutions plated to determine numbers of adherent and internalized bacteria. B BEAS-2B cells were stimulated with Golgicide A or DMSO for 4 h. Afterwards, cells were infected with Spn D39, MOI 1 for 9 h and bacterial replication determined. C-F Cells were treated with Golgicide A or DMSO of 4 h. Medium was exchanged and cells were stimulated with LTA or PBS for 2 h and the supernatant collected. For infection experiments, cells were infected with Spn, MOI 1 for 16 h in infection medium consisting of 1:1 fresh cell culture medium and supernatant from 1). C Experimental setup. D BEAS-2B were infected with Spn D39, MOI 1 for 9 h in a 1:1 mixture of fresh cell culture medium and conditioned medium as indicated. Additionally, bacteria were cultivated in a host cell free mixture of fresh/conditioned medium for 9 h. Resulting CFU were determined. E, F, G Concentrations of IL-6, IL-8 and IL-18 were determined in Golgicide A/LTA-conditioned cell culture supernatants. (N = 3–4; Statistics: paired two-tailed t-test (A, B, E, F, G), One-way ANOVA with Fisher’s LSD (D); * = p < 0.05; ns = not significant)
Discussion
In this study, we observed that Spn infection interferes with Golgi structure and function in lung epithelial cells, thereby disturbing paracrine immune mechanisms. Fluorescence staining of the Golgi-associated protein Golgin-97 revealed a pneumococcal-induced structural disruption of the Golgi. Golgi fragmentation depended on the pneumococcal virulence factor H2O2. Artificial disruption of the Golgi apparatus by Golgicide A treatment influenced the infection process by inhibiting cytokine secretion, reducing bacterial adherence, but promoting replication.
The Golgi was previously reported as an important factor in the inflammatory response of epithelial cells [14]. Consequently, a range of intracellular pathogens were reported to interact with the Golgi. SARS-CoV2 was recently shown to disrupt the Golgi apparatus via a currently undefined mechanism [15]. Hepatitis C virus was shown to activate the Golgi-localized immunity related GTPase M, which phosphorylates the guanine nucleotide exchange factor GBF1, leading to disruption of the Golgi [16]. Upon bacterial infection, host-cell invading Rickettsia rickettsii and Streptococcus pyogenes were previously shown to disrupt Golgi structure [17, 18]. In contrast, encapsulated strains of Spn typically replicate extracellularly and only show minor tendencies to invade the host cell [19]. Thus, the present study is the first to show Golgi disruption in response to infection with extracellular bacteria. In neuroblastoma cells, H2O2, a common oxidant and virulence factor of Spn, was previously reported to induce Golgi fragmentation [12]. H2O2 treatment was shown to induce protease activity, leading to the degradation of the Golgi structure protein Ark1 and therefore Golgi fragmentation, as assessed by diffuse distribution of the tethering protein Golgin-97 [12, 20]. Here we hypothesized that Golgi disruption during Spn infection of epithelial cells is induced by a H2O2 dependent mechanism. We confirmed our hypothesis by demonstrating an induction of Golgi fragmentation in bronchial epithelial cells by H2O2 treatment, starting at 40 µM H2O2. This is likely to be relevant for the infection process, as H2O2 concentrations in liquid cultures of Spn were determined to reach up to 400 µM [5]. Treatment of infected cells with the H2O2-degrading enzyme catalase prevented Golgi fragmentation, and infection with the H2O2-deficient Spn strain ΔspxB failed to induce Golgi fragmentation, further supporting the involvement of H2O2. As a deletion of the pore-forming toxin pneumolysin did not significantly affect Golgi structure, we conclude that H2O2 is the main factor involved in pneumococci-induced Golgi disruption. Interestingly, catalase expression is a common feature of lung epithelial cells but reduced following Influenza A virus infection [21]. Thereby, catalase production might constitute a host cell defense mechanism against Golgi fragmentation and constitute a further mechanism by which initial Influenza A infection benefits a superinfection with Spn.
Beside its role in intracellular trafficking and organization of the cytoskeleton, the Golgi plays an important role in protein glycosylation. Disruption of the Golgi was linked to impaired protein glycosylation [22]. Bacterial adherence to the host epithelium is an important part of the pneumococcal infection process [23]. Mediated by various pneumococcal surface proteins and teichoic acids, Spn adheres to protein structures on the surface of the epithelial cells. Since extracellular protein domains are frequently glycosylated [24], we investigated whether artificial Golgi disruption by Golgicide A treatment [25] affects the adherence process. Indeed, upon Golgi disruption, the amount of adherent and internalized bacteria was reduced compared to untreated controls.
As the Golgi is well-established to be involved in the cellular antibacterial response [17], we next investigated whether Golgi disruption affects bacterial growth during the infection process. Indeed, bacterial replication increased if the epithelial cell Golgi apparatus was disrupted prior to infection. This effect was likely mediated by interference with Golgi-dependent secretory processes: after anti-bacterial activation with the Toll-like receptor 2-ligand LTA, epithelial cells secreted inflammatory cytokines IL-6 and IL-8 into their supernatant. These supernatants could in turn activate naïve epithelial cells, resulting in reduced bacterial replication upon Spn infection. When we experimentally disrupted the Golgi-apparatus of the secreting cells, this abolished both, cytokine secretion and supernatant-induced bacterial growth inhibition. This stands in accordance to previous results identifying a link between Golgi mediated membrane trafficking and cytokine secretion [26,27,28] and might constitute a mechanism for the previously reported inhibition of the inflammatory response in pneumococcal infections [29].
Epithelial cells form a first line of defense against invading pathogens. Therefore, these results might have important implications for the progression of a wide range of disease, e.g., infections with S. oralis or intestinal infections [29]. H2O2 production by commensal bacteria was furthermore reported to be an important part of the progression of inflammatory bowel disease [30]. The here reported H2O2-dependent Golgi fragmentation might constitute an additional mechanism of disease progression and H2O2 neutralization might form a readily available treatment option to slow disease progression and prevent tissue damage. However, in this study, we exclusively focused on the interference of Spn-produced H2O2 with the Golgi function in immortalized bronchial epithelial cells. Further work is needed to confirm this effect in more complex models. For instance, it would be of interest whether disruption of cytokine secretion following Golgi fragmentation affects the ability to recruit immune cells to the side of infection. The response of the innate immune system towards bacterial infection relies on secretory processes [31]. In particular, neutrophils were shown to rely on proper Golgi function to initiate antibacterial secretory processes [32]. Should Spn-mediated Golgi fragmentation occur in immune cells in addition to epithelial cells, this might constitute a new mechanism of immune evasion utilized by Spn. Lastly, by utilizing catalase to degrade H2O2, we identified an option to protect the Golgi apparatus during Spn infection in vitro. This provides a useful tool to study the effect of H2O2 on the Golgi and raises the question whether H2O2 neutralization might constitute a supportive treatment option during pneumococcal infection.
While animal experiments were beyond the scope of this study, further work should be done to confirm our results in vivo and assess the role of catalase as a potential Golgi-protective mechanism during lung infection. Therefore, mice should be infected with Spn, WT or ΔspxB to assess Golgi structure and secretion processes during infection. Infection of mice will furthermore serve as a useful models to investigate the effect of antioxidants during pneumococcal infection, with particular regard to Golgi structure and function.
Conclusion
In summary, we report a novel interference of an extracellular bacterial pathogen with the Golgi apparatus, leading to an H2O2-dependent breakdown of Golgi structure and function. Our results further reveal a double-edged effect of Golgi fragmentation on the infection process. While initial infection might be hampered by a reduced bacterial ability to adhere to the host cell, in later stages Golgi disruption reduces the cellular defense against the pathogen. Thereby, our study provides evidence on a novel field of host–pathogen interaction during infections with the major human pathogen Streptococcus pneumoniae.
Availability of data and materials
All data generated and analysed during this study are included in this published article. Raw images are available from BS upon reasonable request.
References
Ikuta KS, Swetschinski LR, Robles Aguilar G, Sharara F, Mestrovic T, Gray AP, Davis Weaver N, Wool EE, Han C, Gershberg Hayoon A, Aali A, Abate SM, Abbasi-Kangevari M, Abbasi-Kangevari Z, Abd-Elsalam S, Abebe G, Abedi A, Abhari AP, Abidi H, Aboagye RG, Absalan A, Abubaker Ali H, Acuna JM, Adane TD, Addo IY, Adegboye OA, Adnan M, Adnani QES, Afzal MS, Afzal S, et al. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2022;400:2221–48.
Pérez-Dorado I, Galan-Bartual S, Hermoso JA. Pneumococcal surface proteins: when the whole is greater than the sum of its parts. Mol Oral Microbiol. 2012;27:221–45.
Radhakrishnan D, Yamaguchi M, Kawabata S, Ponnuraj K. Streptococcus pneumoniae surface adhesin PfbA and its interaction with erythrocytes and hemoglobin. Int J Biol Macromol. 2018;120:135–43.
Hammerschmidt S. Adherence molecules of pathogenic pneumococci. Curr Opin Microbiol. 2006;9:12–20.
Lisher JP. Tsui H-CT, Ramos-Montañez S, Hentchel KL, Martin JE, Trinidad JC, Winkler ME, Giedroc DP: Biological and Chemical Adaptation to Endogenous Hydrogen Peroxide Production in Streptococcus pneumoniae D39. mSphere. 2017;2(1):e00291-16.
McLeod JW, Gordon J. Production of Hydrogen Peroxide by Bacteria. Biochem J. 1922;16:499–506.
Rai P, Parrish M, Tay IJJ, Li N, Ackerman S, He F, Kwang J, Chow VT, Engelward BP. Streptococcus pneumoniae secretes hydrogen peroxide leading to DNA damage and apoptosis in lung cells. Proc Natl Acad Sci USA. 2015;112(26):E3421-30.
Erttmann SF, Gekara NO. Hydrogen peroxide release by bacteria suppresses inflammasome-dependent innate immunity. Nat Commun. 2019;10(1):3493.
Makaraci P, Kim K. trans-Golgi network-bound cargo traffic. Eur J Cell Biol. 2018;97:137–49.
Liu F, Stanton JJ, Wu Z, Piwnica-Worms H. The human Myt1 kinase preferentially phosphorylates Cdc2 on threonine 14 and localizes to the endoplasmic reticulum and Golgi complex. Mol Cell Biol. 1997;17(2):571–83. https://doi.org/10.1128/MCB.17.2.571.
Stanley P. Golgi glycosylation. Cold Spring Harb Perspect Biol. 2011;3(4):a005199.
Ireland SC, Huang H, Zhang J, Li J, Wang Y. Hydrogen peroxide induces Arl1 degradation and impairs Golgi-mediated trafficking. MBoC. 2020;31:1931–42.
Wortzel I, Koifman G, Rotter V, Seger R, Porat Z. High Throughput Analysis of Golgi Structure by Imaging Flow Cytometry. Sci Rep. 2017;7:788.
Tao Y, Yang Y, Zhou R, Gong T. Golgi Apparatus: An Emerging Platform for Innate Immunity. Trends Cell Biol. 2020;30:467–77.
Hackstadt T, Chiramel AI, Hoyt FH, Williamson BN, Dooley CA, Beare PA, de Wit E, Best SM, Fischer ER. Disruption of the Golgi Apparatus and Contribution of the Endoplasmic Reticulum to the SARS-CoV-2 Replication Complex. Viruses. 2021;13:1798.
Hansen MD, Johnsen IB, Stiberg KA, Sherstova T, Wakita T, Richard GM, Kandasamy RK, Meurs EF, Anthonsen MW. Hepatitis C virus triggers Golgi fragmentation and autophagy through the immunity-related GTPase M. Proc Natl Acad Sci USA. 2017;114(17):E3462–71.
Aistleitner K, Clark T, Dooley C, Hackstadt T. Selective fragmentation of the trans-Golgi apparatus by Rickettsia rickettsii. PLoS Pathog. 2020;16:e1008582.
Nozawa T, Iibushi J, Toh H, Minowa-Nozawa A, Murase K, Aikawa C, Nakagawa I. Intracellular Group A Streptococcus Induces Golgi Fragmentation To Impair Host Defenses through Streptolysin O and NAD-Glycohydrolase. mBio. 2021;12(1):e01974-20.
Hyams C, Trzcinski K, Camberlein E, Weinberger DM, Chimalapati S, Noursadeghi M, Lipsitch M, Brown JS. Streptococcus pneumoniae Capsular Serotype Invasiveness Correlates with the Degree of Factor H Binding and Opsonization with C3b/iC3b. Infect Immun. 2013;81:354–63.
Fligiel SE, Lee EC, McCoy JP, Johnson KJ, Varani J. Protein degradation following treatment with hydrogen peroxide. Am J Pathol. 1984;115:418–25.
Kumar P, Khanna M, Srivastava V, Tyagi YK, Raj HG, Ravi K. Effect of quercetin supplementation on lung antioxidants after experimental influenza virus infection. Exp Lung Res. 2005;31:449–59.
Davids M, Kane MS, He M, Wolfe LA, Li X, Raihan MA, Chao KR, Bone WP, Boerkoel CF, Gahl WA, Toro C. Disruption of Golgi morphology and altered protein glycosylation in PLA2G6-associated neurodegeneration. J Med Genet. 2016;53:180–9.
Novick S, Shagan M, Blau K, Lifshitz S, Givon-Lavi N, Grossman N, Bodner L, Dagan R, Nebenzahl YM. Adhesion and invasion of Streptococcus pneumoniae to primary and secondary respiratory epithelial cells. Mol Med Rep. 2017;15:65–74.
Reily C, Stewart TJ, Renfrow MB, Novak J. Glycosylation in health and disease. Nat Rev Nephrol. 2019;15:346–66.
Sáenz JB, Sun WJ, Chang JW, Li J, Bursulaya B, Gray NS, Haslam DB. Golgicide A reveals essential roles for GBF1 in Golgi assembly and function. Nat Chem Biol. 2009;5(3):157–65. https://doi.org/10.1038/nchembio.144.
Manderson AP, Kay JG, Hammond LA, Brown DL, Stow JL. Subcompartments of the macrophage recycling endosome direct the differential secretion of IL-6 and TNFalpha. J Cell Biol. 2007;178:57–69.
Chiaruttini G, Piperno GM, Jouve M, de Nardi F, Larghi P, Peden AA, Baj G, Müller S, Valitutti S, Galli T, Benvenuti F. The SNARE VAMP7 Regulates Exocytic Trafficking of Interleukin-12 in Dendritic Cells. Cell Rep. 2016;14:2624–36.
Revelo NH, Ter Beest M, van den Bogaart G. Membrane trafficking as an active regulator of constitutively secreted cytokines. J Cell Sci. 2019;133(5):jcs234781.
Matsushima H, Kumagai Y, Vandenbon A, Kataoka H, Kadena M, Fukamachi H, Arimoto T, Morisaki H, Fujiwara N, Okahashi N, Kuwata H. Microarray analysis of macrophage response to infection with Streptococcus oralis reveals the immunosuppressive effect of hydrogen peroxide. Biochem Biophys Res Commun. 2017;485:461–7.
Strus M, Gosiewski T, Fyderek K, Wedrychowicz A, Kowalska-Duplaga K, Kochan P, Adamski P, Heczko PB. A role of hydrogen peroxide producing commensal bacteria present in colon of adolescents with inflammatory bowel disease in perpetuation of the inflammatory process. J Physiol Pharmacol. 2009;60(Suppl 6):49–54.
Gandhi VD, Vliagoftis H. Airway epithelium interactions with aeroallergens: role of secreted cytokines and chemokines in innate immunity. Front Immunol. 2015;6:147.
Sheshachalam A, Srivastava N, Mitchell T, Lacy P, Eitzen G. Granule protein processing and regulated secretion in neutrophils. Front Immunol. 2014;5:448.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work has been funded in part by grants of the Bundesministerium für Bildung und Forschung (Federal Ministry of Education and Research: PermedCOPD – FKZ 01EK2203A; ERACoSysMed2 – SysMed-COPD – FKZ 031L0140; e:Med CAPSYS – FKZ 01ZX1604E), the Deutsche Forschungsgemeinschaft (SFB/TR-84 TP C01), and the von-Behring-Röntgen-Stiftung (66-LV07) as well as the Hessisches Ministerium für Wissenschaft und Kunst (LOEWE Diffusible Signals LOEWE-Schwerpunkt Diffusible Signals) to B.S.
Author information
Authors and Affiliations
Contributions
B.K., A.W., E.V., B.J.B., B.S. defined research goals and designed the study. B.K., A.W., S.R. and L.D.H. performed research. B.K. and W.B. analyzed data. B.K. wrote the manuscript. All authors reviewed the manuscript, provided feedback and agreed to its publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Spn TIGR4 infection disrupts the structural integrity of the Golgi apparatus. BEAS-2B cells were infected with Spn TIGR4, MOI 2 for 7 h or left uninfected. Cells were fixed and fluorescence stained for Golgin-97 and the nucleus (DAPI). Binary images were generated and used to quantify the Golgi area. A) Immunofluorescence images. Overlays were generated using the false-colored DAPI- and Golgin-97 images. B) Quantification of the Golgi surface area, normalized to uninfected controls. C) Mitochondrial activity after infection, assessed by MTT assay. (Scale: 10 µm; Statistics: paired two-tailed t-test; N=3-4; * = p<0.05; Scale: 10 µm; at least 300 cells from 3 independent experiments were quantified). Figure S2. Deletion of the pneumococcal pore-forming toxin pneumolysin does not affect Golgi integrity. BEAS-2B cells were infected with Spn D39 WT or Spn D39 Δply for 16 h or left untreated. Cells were fixed and fluorescence stained for Golgin-97 and the nucleus (DAPI). A) Immunofluorescence images of infected and uninfected cells. B) Quantification of the Golgi surface area, relative to uninfected controls. C) Mitochondrial activity, assessed by MTT assay. (Statistics: paired two-tailed t-test for Δply vs. WT; N = 4-5; * = p<0.05; Scale: 10 µm; at least 600 cells from 5 independent experiments were quantified). Figure S3. Golgicide A treatment efficiently disrupts the Golgi apparatus. A) BEAS-2B cells were stimulated with indicated amounts of Golgicide A for 4 h. Control cells were treated with DMSO. Afterwards, cells were fixated and stained for Golgin-97 and the nucleus. B) BEAS-2B cells were treated with Golgicide A, 4 µM for 4 h. Afterwards, medium was replaced with fresh medium containing 4 µM Golgicide and cells were incubated for additional 16 h. Control cells were treated with DMSO. After stimulation, mitochondrial activity was assessed by MTT assay. (Scale: 10 µM; N=3; Statistics: paired t-test (ns = not significant).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Klabunde, B., Wesener, A., Bertrams, W. et al. Streptococcus pneumoniae disrupts the structure of the golgi apparatus and subsequent epithelial cytokine response in an H2O2-dependent manner. Cell Commun Signal 21, 208 (2023). https://doi.org/10.1186/s12964-023-01233-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12964-023-01233-x