Abstract
Purpose
The purpose of this study was to explore the risk factors for synchronous liver metastasis (LM) of colorectal cancer (CRC) and to construct a nomogram for predicting the occurrence of synchronous LM based on baseline and pathological information.
Methods
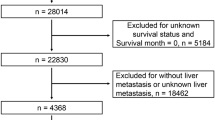
The baseline and pathological information of 3190 CRC patients were enrolled in the study from the Department of Colorectal Surgery, the Second Affiliated Hospital of Harbin Medical University between 2012 and 2020. All patients were divided into development and validation cohorts with the 1:1 ratio. The characters of LM and none-LM patients in newly diagnosed colorectal cancer were utilized to explore the risk factors for synchronous LM with the univariate and multivariate logistic regression analyses. A predictive nomogram was constructed by using an R tool. In addition, receiver operating characteristic (ROC) curves was calculated to describe the discriminability of the nomogram. A calibration curve was plotted to compare the predicted and observed results of the nomogram. Decision-making curve analysis (DCA) was used to evaluate the clinical effect of nomogram.
Results
The nomogram consisted of six features including tumor site, vascular invasion (VI), T stage, N stage, preoperative CEA, and CA-199 level. ROC curves for the LM nomogram indicated good discrimination in the development (AUC = 0.885, 95% CI 0.854–0.916) and validation cohort (AUC = 0.857, 95% CI 0.821–0.893). The calibration curve showed that the prediction results of the nomogram were in good agreement with the actual observation results. Moreover, the DCA curves determined the clinical application value of predictive nomogram.
Conclusions
The pathologic-based nomogram could help clinicians to predict the occurrence of synchronous LM in postoperative CRC patients and provide a reference to perform appropriate metastatic screening plans and rational therapeutic options for the special population.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common malignancy in the world, with high incidence and mortality globally. Metastases is one of the most common contributors for death in CRC, of which liver metastasis (LM) is the most fatal [1]. At present, research on LM in CRC patients is continuing [2,3,4]. It is important to note that LM are found in more than 25% of patients with CRC at the time of their first diagnosis and occur in up to 25% of patients following removal of the primary tumor [5, 6]. The 5-year survival rate for patients with CRC is approximately 56%, but can be significantly reduced when distant metastases are detected [7, 8].
LM of CRC can be divided into synchronous and metachronous LM [9]. Synchronous LM was defined as LM detected at the time of diagnosis of the primary tumor or within 6 months after diagnosis. Jennie et al found that up to 18.3% of patients developed LM after radical CRC surgery. Therefore, early detection of high-risk postoperative populations for synchronous LM can help physicians to improve survival by targeting screening and individualizing treatment. With the development of scientific research capacity, more and more risk factors affecting LM of CRC have been discovered such as T stage, N stage, tumor site, preoperative CEA level, and so on [10, 11]. However, most studies did not include vascular invasion (VI) as a pathological factor. Both the Association of Directors of Anatomic and Surgical Pathology [12] and the College of American Pathologists [13] emphasis is placed on documenting VI during routine pathological examination of cancer specimens. These institutions emphasized that VI was an independent predictor of poor prognosis and increased risk of LM because VI necessarily increased the risk of tumor cell entry into the bloodstream. Many studies have reached similar conclusions [14, 15]. In addition, VI is an indication for adjuvant chemotherapy in stage II patients. Therefore, there are sufficient and necessary reasons to consider VI as a risk predictor for synchronous LM. Nomogram is a kind of graphical prediction model with friendly interface, which has strong clinical application value. By assigning points, we can not only observe the influence of certain parameters but also predict the probability of a particular event from the total score. To our knowledge, this is the first nomogram including VI to predict synchronous LM of CRC.
Methods
Patients
Three thousand one hundred ninety CRC cases were collected from the department of colorectal surgery, the Second Affiliated Hospital of Harbin Medical University between 2012 and 2020.
Inclusion criteria included (1) patients diagnosed with CRC and underwent surgery; (2) aged ≥ 18 years old; (3) Patients with complete pathological information; (4) CRC was the only primary malignancy. Exclusion criteria included (1) patients received preoperative neoadjuvant chemoradiotherapy; (2) the baseline and pathological information of the patient was incomplete; (3) distant metastases other than LM, and (4) postoperative resection margin of tumor was positive.
The colorectal cancer patients included in this study were treated with surgery only before the diagnosis of liver metastasis.
Variables
According to our study, age was regrouped into < 60, 60–74, and ≥ 75 years old; sex was classified as male and female; BMI was recorded as < 25 and ≥ 25; tumor size was divided into two groups: ≤ 5 cm and > 5 cm. The tumor site was grouped into right-sided colon (cecum, ascending colon, hepatic flexure, and transverse colon) and left-sided colon (splenic flexure, descending colon and sigmoid colon). The histology variable was classified as “adenocarcinoma,” “mucinous adenocarcinoma,” or “others”; the grade variable was classified as I/II and III/IV (“well-differentiated/moderately differentiated,” and “poorly differentiated/undifferentiated”) stage and the tumor type variable was classified as “ulcer type,” “uplift type,” and “infiltrating type.” Similarly, T stages, N stages, and lymph nodes examined (LNE) are grouped. The most prominent variable that VI, nerve invasion, and lymphatic invasion were classified as “yes” or “no.” The preoperative CEA level variable was classified as “positive” (≥ 5 ng/ml) and “negative” (< 5 ng/ml). In the same way, CA199 level variable was classified as “positive” (≥ 37 U/ml) and “negative” (< 37 U/ml).
Statistical analysis
All statistical analyses were performed by R tool and SPSS 22.0. In this study, all patients were randomly (1:1 ratio) divided into development and validation cohorts and summarized by number and percentage. The characters of LM and none-LM patients in newly diagnosed colorectal cancer were utilized to explore the risk factors for synchronous LM with the univariate and multivariate logistic regression analyses. Nomogram was constructed based on the results of multivariate regression model and its performance was further evaluated by calibration and ROC. The DCA curve was used to evaluate the clinical decision ability of the model. In addition, all variables were assigned and the best cutoff value was calculated based on the total score by Youden’s index. The difference was considered statistically significant for a two-sided P < 0.05.
Results
Patients’ characteristics
A total of 3190 patients were divided evenly into the development and validation cohorts. There were 104(6.5%) LM patients in development cohort and 107(6.7%) LM patients in validation cohort. In all patients, the majority of patients were men, aged 60–74 and had a BMI of less than 25. Overall, the main proportions of the patients were associated with rectum, tumor size ≤ 5 cm, ulcer type, grade I/II, adenocarcinoma, preoperative CEA and CA-199 level negative, T4 stage, N0 stage, and LNE ≥ 12. In the encroachment around, VI accounted for 28.8% and 30.5% in the development and validation cohorts. The detailed data was summarized in Table 1.
Construction and validation of nomogram to predict LM probability
Univariate and multivariate logistic regression analyses were performed to determine the independent risk factors for LM. In univariate analysis, the candidate predictors for the model were age, BMI, sex, tumor size and site, tumor type, grade, histology, T stage, N stage, LNE, VI, nerve invasion, lymphatic invasion, preoperative CEA, and CA-199 level. All the predictors except for age, BMI, sex, tumor type, histology, and LNE were of statistical significance in the development cohort, which were then further analyzed by multivariate logistic regression model. And the results indicated that tumor site (OR = 2.228, 95%CI = 1.272–3.901 for right-sited colon, P = 0.005; OR = 1.635, 95%CI = 0.889–3.007 for left-sited colon, P = 0.114; using rectum as the reference), VI (OR = 1.965, 95%CI = 1.182–3.266 for yes, P = 0.009; using no as the reference), T stage (OR = 0.130, 95%CI = 0.017–1.014 for T1/T2, P = 0.052; OR = 0.417, 95%CI = 0.245–0.710 for T3, P = 0.001; using T4 as the reference), N stage (OR = 1.252, 95%CI = 0.665–2.359 for N1, P = 0.487; OR = 4.071, 95%CI = 2.117–7.830 for N2, P < 0.001; using N0 as the reference), CEA level (OR = 3.043, 95%CI = 1.836–5.043 for CEA positive, P < 0.001, using CEA negative as the reference), CA-199 level (OR = 6.006, 95%CI = 3.697–9.756 for CA-199 positive, P < 0.001, using CA-199 negative as the reference) were independent risk factors in predicting LM (Table 2).
Subsequently, we constructed a nomogram to predict LM for postoperative patients based on independent risk factors (tumor site, VI, T stage, N stage, CEA, and CA-199 level) (Fig. 1). The AUCs for development and validation cohort were 0.885 (95%CI = 0.854–0.916) and 0.857 (95%CI = 0.821–0.893), respectively (Fig. 2). The calibration curves (development cohort: p = 0.772; validation cohort: p = 0.198) showed the relatively satisfactory prediction accuracy of the nomogram (Fig. 3). In addition, the DCA curve also indicated good clinical practicability in both cohorts (Fig. 4).
Using the nomogram derived scores, all LM patients were classified into two subgroup low-risk (risk score ≤ 193) and high-risk groups (risk score > 193) (Fig. 5). And we found there were significant differences in the occurrence of LM between the high- and low-risk groups in development cohort (P < 0.001) and validation cohort (P < 0.001) (Fig. 6).
Discussion
CRC is one of the major causes of cancer morbidity and mortality both in the worldwide. Distant metastasis disease is the main cause of poor prognosis in patients with CRC and the liver is the most common organ for metastasis. Over the course of the disease, a total of 50% of patients with CRC are likely to develop LM [16]. And the death rate remains high [17]. This also explains the necessity of this study. Nowadays, many studies have identified many independent factors for LM in patients with CRC but few studies developed predictive nomogram and the factors included are incomplete, this also has led to questions about the accuracy of those nomograms [18, 19]. None of these studies had complete pathological information, such as VI, nerve invasion and lymphatic invasion, although nerve invasion and lymphatic invasion were not an independent risk factor in this study. Our study included not only the baseline information of the patients, but also the postoperative pathological information of the patients such as the VI. This greatly increases the sensitivity and specificity of this model. This nomogram can help identify high-risk groups for synchronous LM after surgery and help clinicians conduct targeted screening and individualized treatment.
According to previous studies, the prevalence of CRC LM is more common than other metastases, such as the brain or bone [20, 21] and the prevalence of LM was more than 20% [22, 23]. However, the prevalence in this study was less than 20% which was consistent with one study conducted by Manfredi and his colleagues in France [24]. In this study, the incidence of elderly patients was significantly lower than that of young patients, with an incidence of only 13.2%. Because in the past few years, as colonoscopy screening has become more widespread, more and more early signs of cancer have been detected, leading to higher rates of disease in younger people and reducing the prevalence of LM. Tumor size has been shown to be an important factor in the development of LM from CRC [11], while little effect of tumor size was found in this study which might be partly attributed to sample size. Therefore, factors contributing to the development of LM after CRC should be identified and a screening method developed to determine the risk of LM in patients with postoperative CRC.
This study showed that tumor site, T stage, N stage, VI, preoperative CEA level, and CA-199 level were significantly associated with LM development, which were seldom reported before. In our nomogram, colon cancer (CC) is found to be more likely to metastasize than rectal cancer. The most common mechanism is that the metastatic pattern is different. In CC, most mesenteric drainage enters the hepatic portal vein system and the rectal venous-collected blood flows into the systemic circulation [25]. And right-sited CC is found to be more likely to metastasize than left-sited CC, which is consistent with previous articles [11, 23, 24], it was reported that the discrepancy was caused by molecular biological differences [26, 27]. In addition, it is well known that high T stage, N stage, and tumor marker levels represent the malignancy of the tumor, indicating a high likelihood of LM. To some extent, it may explain the difference in prognosis, but this complex issue needs further research.
Since VI is closely related to progression and recurrence of the disease, both the Association of Directors of Anatomic and Surgical Pathology and the College of American Pathologists emphasis is placed on documenting VI during routine pathological examination of cancer specimens. It is reported that the pathologic detection rate of VI was 23% [28]. The proliferation of tumor cells requires energy and nutrition, tumor and other cells secrete VEGF, angiopoietin-like protein, and corresponding inflammatory cells to promote the formation of new blood vessels, thus providing an important channel for these functions [29]. Invasion of blood vessels by tumor cells is a key step in LM. Fujii T and Xie W et al. found that VI is closely related to the depth of tumor invasion and degree of differentiation [30, 31]. A previous study has shown that VI is significantly associated with metastasis and high recurrence rates [32]. Furthermore, VI has been shown to be associated with reduced overall survival (OS) and disease-free survival (DFS), serving as a strong prognostic indicator [33]. These studies indicate that VI is an essential factor in LM of CRC. The inclusion of this factor improves the accuracy and persuasiveness of our model.
In addition, our research has certain research significance and advantages. Our model mainly identified patients at high risk of developing LM after surgery. For example, a right-sited (40 points) CC patient with VI (32 points), T4 stage (100 points), N2 (62 points), CEA level is positive (58 points), and CA199 level is negative (0 points) has a total of 292 points (high-risk group), resulting the diagnostic possibility is 0.38. In high-risk groups, where there may be micrometastases that were not detected before surgery, the enhanced computed tomography and monitoring should be justified after surgery. In addition, for high-risk patients, positron emission tomography computed tomography (PET-CT) and invasive procedures such as needle biopsy are also recommended for definite diagnosis if there is an undefined low-density liver lesion, because they are expensive and are not justified for general screening. If a positive liver result is found in a targeted examination, we can change the treatment plan in time so as not to delay the disease such as radiofrequency ablation and surgery [34,35,36]. Of course, this study only provides a reference rather than a guide, and specific decisions should be made based on clinical practice.
The study has several limitations. First of all, since this study is a retrospective study, involving 3190 patients from 2012 to 2020, there may be a possibility of inaccuracy due to the small amount of data, and inevitably there is observer and confusion bias. The current results require further validation in prospective clinical studies. Second, although our model has internal validation, there is a lack of external validation to further determine the model’s accuracy. Third, some underlying factors such as gene status are unknown [37]. The inclusion of these important factors can further improve the effectiveness of the nomogram.
In conclusion, this study performed prediction of synchronous LM in patients undergoing CRC surgery. Therefore, if patients with preoperative diagnosis of colorectal cancer, no LM and underwent surgery are identified as a high-risk patient by nomogram, we should enhance post-operative imaging of the liver, such as enhanced computed tomography, MRI and positron emission tomography computed tomography (PET-CT). It can help clinicians timely detect the disease progression of patients and take effective interventions to improve the quality of life of patients. This is crucial.
Availability of data and materials
The study data of validation cohort used and/or analyzed during the current study are available from the Second Affiliated Hospital of Harbin Medical University, China.
References
Zheng W, Wu F, Fu K, et al. Emerging mechanisms and treatment progress on liver metastasis of colorectal cancer. Onco Targets Ther. 2021;14:3013–36.
Sun YD, Zhang H, Chen YQ, et al. HMGB1, the next predictor of transcatheter arterial chemoembolization for liver metastasis of colorectal cancer? Front Oncol. 2020;10:572418.
Liang JY, Lin HC, Liu J, et al. A novel prognostic nomogram for colorectal cancer liver metastasis patients with recurrence after hepatectomy. Cancer Med. 2021;10(5):1535–44.
Yang L, Yu S, Ma D, Yu Z. An unusual liver mass initially misdiagnosed as colorectal cancer liver metastasis. Dig Liver Dis. 2021. https://doi.org/10.1016/j.dld.2021.01.024.
Minagawa M, Yamamoto J, Miwa S, et al. Selection criteria for simultaneous resection in patients with synchronous liver metastasis. Arch Surg. 2006;141(10):1006–12 discussion 13.
Reissfelder C, Rahbari NN, Koch M, et al. Validation of prognostic scoring systems for patients undergoing resection of colorectal cancer liver metastases. Ann Surg Oncol. 2009;16(12):3279–88.
Davini F, Ricciardi S, Zirafa CC, et al. Lung metastasectomy after colorectal cancer: prognostic impact of resection margin on long term survival, a retrospective cohort study. Int J Colorectal Dis. 2020;35(1):9–18.
Panahi MH, Panahi H, Mahdavi Hezaveh A, Mansournia MA, Bidhendi YR. Survival rate of colon and rectum cancer in Iran: a systematic review and meta-analysis. Neoplasma. 2019;66(6):988–94.
Engstrand J, Stromberg C, Nilsson H, Freedman J, Jonas E. Synchronous and metachronous liver metastases in patients with colorectal cancer-towards a clinically relevant definition. World J Surg Oncol. 2019;17(1):228.
Lee WS, Kim MJ, Yun SH, et al. Risk factor stratification after simultaneous liver and colorectal resection for synchronous colorectal metastasis. Langenbecks Arch Surg. 2008;393(1):13–9.
Tang M, Wang H, Cao Y, Zeng Z, Shan X, Wang L. Nomogram for predicting occurrence and prognosis of liver metastasis in colorectal cancer: a population-based study. Int J Colorectal Dis. 2021;36(2):271–82.
Higgins JP, McKenney JK, Brooks JD, et al. Recommendations for the reporting of surgically resected specimens of renal cell carcinoma: the Association of Directors of Anatomic and Surgical Pathology. Hum Pathol. 2009;40(4):456–63.
Washington MK, Berlin J, Branton P, et al. Protocol for the examination of specimens from patients with primary carcinoma of the colon and rectum. Arch Pathol Lab Med. 2009;133(10):1539–51.
Sato T, Ueno H, Mochizuki H, et al. Objective criteria for the grading of venous invasion in colorectal cancer. Am J Surg Pathol. 2010;34(4):454–62.
Suzuki A, Togashi K, Nokubi M, et al. Evaluation of venous invasion by Elastica van Gieson stain and tumor budding predicts local and distant metastases in patients with T1 stage colorectal cancer. Am J Surg Pathol. 2009;33(11):1601–7.
Chan KM, Wu TH, Wang YC, et al. Clinical relevance of oncologic prognostic factors in the decision-making of pre-hepatectomy chemotherapy for colorectal cancer hepatic metastasis: the priority of hepatectomy. World J Surg Oncol. 2018;16(1):24.
Wang X, Mao M, Xu G, et al. The incidence, associated factors, and predictive nomogram for early death in stage IV colorectal cancer. Int J Colorectal Dis. 2019;34(7):1189–201.
Yao J, Chen Q, Deng Y, et al. Nomograms predicting primary lymph node metastases and prognosis for synchronous colorectal liver metastasis with simultaneous resection of colorectal cancer and liver metastases. Ann Palliat Med. 2021;10(4):4220–31.
Li M, Li X, Guo Y, et al. Development and assessment of an individualized nomogram to predict colorectal cancer liver metastases. Quant Imaging Med Surg. 2020;10(2):397–414.
Yang L, He W, Xie Q, et al. Brain metastases in newly diagnosed colorectal cancer: a population-based study. Cancer Manag Res. 2018;10:5649–58.
Lei S, Ge Y, Tian S, et al. Colorectal cancer metastases to brain or bone and the relationship to primary tumor location: a population-based study. J Gastrointest Surg. 2020;24(8):1833–42.
Hackl C, Neumann P, Gerken M, Loss M, Klinkhammer-Schalke M, Schlitt HJ. Treatment of colorectal liver metastases in Germany: a ten-year population-based analysis of 5772 cases of primary colorectal adenocarcinoma. BMC Cancer. 2014;14:810.
Engstrand J, Nilsson H, Stromberg C, Jonas E, Freedman J. Colorectal cancer liver metastases - a population-based study on incidence, management and survival. BMC Cancer. 2018;18(1):78.
Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, Bouvier AM. Epidemiology and management of liver metastases from colorectal cancer. Ann Surg. 2006;244(2):254–9.
Zhu YJ, Chen Y, Hu HY, Zhou YW, Zhu YT, Liu JY. Predictive risk factors and online nomograms for synchronous colon cancer with liver metastasis. Front Oncol. 2020;10:1681.
Elnatan J, Goh HS, Smith DR. C-KI-RAS activation and the biological behaviour of proximal and distal colonic adenocarcinomas. Eur J Cancer. 1996;32A(3):491–7.
Hutajulu SH, Paramita DK, Santoso J, et al. Correlation between vascular endothelial growth factor-A expression and tumor location and invasion in patients with colorectal cancer. J Gastrointest Oncol. 2018;9(6):1099–108.
Betge J, Pollheimer MJ, Lindtner RA, et al. Intramural and extramural vascular invasion in colorectal cancer: prognostic significance and quality of pathology reporting. Cancer. 2012;118(3):628–38.
Carbone C, Piro G, Merz V, et al. Angiopoietin-like proteins in angiogenesis, inflammation and cancer. Int J Mol Sci. 2018;19(2). https://doi.org/10.3390/ijms19020431.
Fujii T, Sutoh T, Morita H, et al. Vascular invasion, but not lymphatic invasion, of the primary tumor is a strong prognostic factor in patients with colorectal cancer. Anticancer Res. 2014;34(6):3147–51.
Xie W, Liu J, Huang X, et al. A nomogram to predict vascular invasion before resection of colorectal cancer. Oncol Lett. 2019;18(6):5785–92.
Siddiqui MRS, Simillis C, Hunter C, et al. A meta-analysis comparing the risk of metastases in patients with rectal cancer and MRI-detected extramural vascular invasion (mrEMVI) vs mrEMVI-negative cases. Br J Cancer. 2017;116(12):1513–9.
Bhangu A, Fitzgerald JE, Slesser A, Northover JM, Faiz O, Tekkis P. Prognostic significance of extramural vascular invasion in T4 rectal cancer. Colorectal Dis. 2013;15(11):e665–71.
Rackauskas R, Bausys A, Sokolovas V, Paskonis M, Strupas K. Short- and long-term outcomes of surgery for colorectal and non-colorectal liver metastasis: a report from a single center in the Baltic country. World J Surg Oncol. 2020;18(1):164.
Horii N, Sawda Y, Kumamoto T, et al. Impact of intramuscular adipose tissue content on short- and long-term outcomes of hepatectomy for colorectal liver metastasis: a retrospective analysis. World J Surg Oncol. 2020;18(1):68.
Wang LJ, Zhang ZY, Yan XL, Yang W, Yan K, Xing BC. Radiofrequency ablation versus resection for technically resectable colorectal liver metastasis: a propensity score analysis. World J Surg Oncol. 2018;16(1):207.
Cai R, Lu Q, Wang D. Construction and prognostic analysis of miRNA-mRNA regulatory network in liver metastasis from colorectal cancer. World J Surg Oncol. 2021;19(1):7.
Acknowledgements
The authors acknowledge the efforts of the Second Affiliated Hospital of Harbin Medical University.
Funding
None
Author information
Authors and Affiliations
Contributions
Study concept and design: YXL and YLMW. Acquisition of data: YXL, YLMW, MYZ, and CLW. Analysis and interpretation of data: YXL, YLMW, HZ, MYZ, YW and CLW. Drafting of the manuscript: YXL and YLMW. Critical revision of the manuscript for important intellectual content: YXL, YLMW, ZQH, HX, HQH, QCT, and GYW. Corresponding author: GYW. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Second Affiliated Hospital of Harbin Medical University and Zhejiang Cancer Hospital. The study used de-identified data and adhered to World Medical Association’s Declaration of Helsinki for Ethical Human Research. The informed consent was not required according to personal identifying information was not included.
Consent for publication
No applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Wang, Y., Zhang, H. et al. Nomogram for predicting occurrence of synchronous liver metastasis in colorectal cancer: a single-center retrospective study based on pathological factors. World J Surg Onc 20, 39 (2022). https://doi.org/10.1186/s12957-022-02516-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02516-2