Abstract
Background
Bradykinin, a vasoactive peptide, has many biological functions. For example, it accelerates angiogenesis. Thus, we studied the effects of bradykinin on the survival of perforator flaps.
Methods
Averagely, 50 male Sprague–Dawley rats were divided into control and bradykinin groups and underwent procedures to the multiterritory perforator flap. Areas of flap survival were tested 7 days later. Flap perfusion was evaluated by laser Doppler imaging. We assessed the extent of autophagy by determining LC3-II/I, Beclin 1, and p62. Flap angiogenesis was assessed by immunohistochemistry and H&E staining. We measured the level of vascular endothelial growth factor (VEGF) protein using western blot. We assessed oxidative stress by measuring the activity of superoxide dismutase (SOD) and malondialdehyde (MDA) levels. The apoptotic index was also evaluated by western blot, and we determined nitric oxide (NO) production using an NO assay kit.
Results
The bradykinin group exhibited significantly larger areas of flap survival, higher blood supply, and more neovascularization. The bradykinin group also had higher SOD activity, higher VEGF expression and NO content, and reduced MDA compared to the control group. Rats treated with bradykinin also had lower levels of apoptosis and autophagy relative to the control group.
Conclusion
Our results suggest that bradykinin promotes the survival of multiterritory perforator flaps by increasing angiogenesis, promoting the release of NO, suppressing apoptosis, reducing oxidative stress, and inhibiting autophagy.
Similar content being viewed by others
Background
The skin, a protective barrier, is highly vulnerable to trauma which can cause serious skin defects. A multiterritory perforator flap can be used to cover these skin defects. It is a skin flap that involves a perforator artery of 0.5 mm or greater, and is widely used because of their advantages [1, 2]. For example, when the skin is injured or defected by severe trauma and burn etc., the multiterritory perforator flaps can cover the huge skin defects. However, avoiding necrosis of such flaps remains a challenge. Many studies have proven that necrosis of the perforator flap always occurs at the dynamic and potential territories [3,4,5]. Previous studies have also demonstrated that inadequate blood supply [6], oxidative stress [7], and cells apoptosis [8] are important factors that lead to flap necrosis. Thus, there is a need to find an effective way to improve the survival of the multiterritory perforator flaps.
Bradykinin, a vasoactive peptide released from precursor kininogens by a protease known as kallikrein [9], is an important component of both acute and chronic inflammatory processes [10, 11]. However, bradykinin performs several other biological functions as well. For example, it increases expression of VEGF via the bradykinin B2 receptor [12]. The levels of VEGF are particularly affected; vascular endothelial cells are stimulated to regenerate and proliferate, thus accelerating angiogenesis [13]. Yoshida et al. [14] recently reported that kallikrein gene delivery weakened apoptosis in ischemia–reperfusion (I/R) injury and myocardial infarction via bradykinin. Bradykinin had anti-apoptotic effects in a model of coronary artery disease [15]. Bradykinin also played an antioxidative role in a rat model of acute hyperglycemia [16], in which it reduced oxidative stress under conditions of hyperglycemia. Moreover, many studies suggest that bradykinin negatively regulates both apoptotic and autophagic responses via the PI3K/Akt signaling pathway [17,18,19]. Excessive autophagy is detrimental although the process of autophagy is advantageous to cell survival [20, 21]. Inhibition of autophagy could inhibit oxidative stress, suppress apoptosis, and enhance perforator flap survival [8].
Several recent publications have demonstrated that bradykinin stimulates nitric oxide (NO) production [22,23,24]. NO, the product of nitric oxide synthase (NOS), promotes cell proliferation and angiogenesis [25]. NO also inhibits apoptosis and autophagy by stimulating the PI3K/Akt signaling pathway [19], which is beneficial for flap survival. Therefore, we hypothesized that bradykinin inhibits apoptosis and autophagy by promoting the release of NO, which may also improve flap survival.
The anti-apoptotic functions of bradykinin, with its ability to inhibit autophagy, inhibit oxidative stress, accelerate vascularization, and promote the release of NO, should be beneficial to improve multiterritory perforator flap survival. In this study, we hypothesized that bradykinin enhances the survival of multiterritory perforator flaps and analyzed its role in doing so in rats. We used histological and protein analyses to investigate whether bradykinin had these effects in a multiterritory perforator flap. We hope our study leads to novel strategies to improve flap survival.
Methods
Animals
Sprague–Dawley (SD) rats, with a closed group of genetic characteristics [26], were used in this study. Fifty healthy male specific-pathogen-free (SPF) rats weighing 250 to 300 g were purchased from the Wenzhou Medical University (license no. SCXK [ZJ] 2015–0001). All used procedures and animal care conformed to the Health Guidelines National Institutes for the Care and Use of Laboratory Animals. The Wenzhou Medical University Animal Research Committee approved the study (wydw 2014–0015). Rats were housed in separate cages with free access to food and water under standard environmental conditions such as temperature 22–25 °C, humidity 60–70%, and 12-h light:12-h dark cycle. Rats were divided into two groups randomly: the bradykinin group and the saline (control) group. Each group contained 25 rats.
Flap animal model
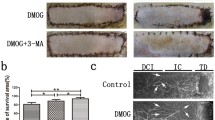
Rats were anesthetized with intraperitoneal pentobarbital (60 mg/kg) [8]. Before surgery, we removed dorsal fur with a depilatory cream and electric shaver. A deep circumflex iliac artery (DCIA) flap was made on the right side of each rat dorsum [27]. In the particular flap, there are three vascular territories: the anatomic territory, the dynamic territory, and the potential territory. In this flap model, the anatomic territory has a deep circumflex iliac (DCI), the dynamic territory has an intercostal artery (IC), and the potential territory has a thoracodorsal artery (TD) [8]. The flap position was approximately 2.5 × 11 cm in size, and it was standardized by bony landmarks. Transillumination identified the choke vessel zone (CVZ) between the IC and TD. Next, the flap was sutured into the original position after the TD and IC were ligated.
Drug administration
Rats in the bradykinin group were injected intraperitoneal bradykinin (150 μg/kg; purity = 98.97%; Medchem Express, Princeton, NJ, USA) [28] 30 min before the procedure. Rats in the control group were injected normal saline at an equal volume for the same days. All rats were housed individually. All rats were sacrificed after 7 days.
Flap assessment
On postoperative day 7 (POD 7), we took high-resolution photographs of the flap with a digital camera. We measured surviving flap areas by superimposing the photographs onto graph paper. The percentages of the viable area were quantified as follows: (range of survival/total flap size) × 100%.
Experimental design
Five rats in each group were used for each test method. In details, five rats in each group were used for flap survival observation and Laser Doppler perfusion imaging; five rats in each group were used for hematoxylin and eosin (H&E) and immunohistochemistry (IHC) staining; five rats in each group were used for superoxide dismutase (SOD) activity and malondialdehyde (MDA) content tests; five rats in each group were used for NO content test; and another five rats in each group were used for western blot.
Hematoxylin and eosin staining
A sample (1 × 1 cm) from each flap CVZ [27] was collected after the sacrifice of rats on POD 7, and routine procedures of H&E staining kit (Solarbio Science & Technology, Beijing, China) were performed. The thickness of the flap tissue was measured under a light microscope, and the number of microvessels in each area (/mm2) was calculated to understand the condition of microvascular density (MVD).
Western blot analysis
On POD 7, flaps from the CVZ were stored at − 80 °C. We determined protein concentrations by using the BCA assay (Thermo Fisher Scientific, Rockford, IL, USA). We performed routine procedures. The membranes were incubated with the following primary antibodies: VEGF (1:1000; Abcam, Cambridge, UK), p62 (1:1000; Abcam, Cambridge, UK), Beclin 1 (1:1000; Cell Signaling Technology (CST), Danvers, MA, USA), LC3 (1:1000; Sigma-Aldrich, St. Louis, MO, USA), cleaved caspase-3 (1:1000; CST), Bax (1:1000; CST), BCL-2 (1:1000; CST) and GAPDH (1:2000; Bioworld Technology, St. Louis Park, MN, USA). Next, membranes were incubated with goat anti-rabbit secondary antibody for 2 h. We quantified band intensity using Image Lab (ver. 5.2, Bio-Rad Laboratories, Hercules, CA, USA).
Immunohistochemistry
On POD 7, samples from the CVZ which were fixed in paraformaldehyde were sectioned into 5 μm slices. Sections were rehydrated in a graded series of ethanol after they were deparaffinized through xylene. Then, sections were immersed in 3% H2O2 and incubated to saturate nonspecific sites. Last sections were incubated with CD34 (1:50; Abcam, Cambridge, UK) at 4 °C overnight. Sections were imaged at × 100 magnification on an image acquisition system (Olympus, Tokyo, Japan). The number of CD34-positive microvessels was calculated in five dense fields.
Laser Doppler perfusion imaging
On POD 7, blood perfusion images were obtained by a Laser Doppler instrument (Moor Instruments, Axminster, UK).
Superoxide dismutase activity and malondialdehyde content
SOD and MDA test kits (Nanjing Jiancheng Biology Institution, Nanjing, China) were used to measure the oxidative stress on the flaps. The flap specimens were obtained from the choke vessel zone on POD 7, weighed, homogenized, and diluted to 10% (volume/volume) on an ice bath. Then, SOD activity and MDA content were detected with the method as reported previously [27].
NO content assay
NO was assayed spectrophotometrically by measuring the products of NO metabolism using NO content assay kits [27] (Nanjing Jiancheng Biology Institution, Nanjing, China).
Statistical analyses
We performed statistical analyses using SPSS version 19.0 (SPSS, Chicago, IL, USA). All data are presented as means ± standard errors of the mean (SEMs). We compared data between groups using Student’s independent t test and one-way repeated measures analysis of variance. In all analyses, P < 0.05 was considered to indicate statistical significance.
Results
Surviving area and blood perfusion
The boundary between the surviving and necrotic regions was evident on POD 7 (Fig. 1a). The control group survival rate was 71.83 ± 2.52%, which differed significantly from that of the bradykinin group (85.83 ± 0.98%). Compared to the control group, flap survival was better in the bradykinin group, with less necrosis (P < 0.01; Fig. 1b). Laser Doppler images revealed the flap perfusion differences (perfusion units (PU)) were evident on POD 7 (Fig. 1c). Bradykinin improved blood supply at the CVZ compared to the control group (control group, 428.38 ± 23.39; bradykinin group, 505.85 ± 25.52; P < 0.05; Fig. 1d).
a Photographs of the postoperative flaps from the bradykinin and control groups on day 7. b The flap survival rate (%) in the bradykinin group (85.83 ± 0.98%) and control group (71.83 ± 2.52%). c The perfusion images of a flap on POD 7. Red denotes high perfusion, and blue denotes low perfusion with the scale bar. d The perfusion value on POD 7 (control group, 428.38 ± 23.39; bradykinin group, 505.85 ± 25.52). n = 5 per group. *P < 0.05, **P < 0.01
Histology
The flaps from rats treated with bradykinin showed more neovascularization and less necrosis than those from the control group (H&E staining; Fig. 2a). The mean MVD in the CVZ was higher in flaps from the bradykinin group than the control group (39.47 ± 1.35 vs. 30.38 ± 2.10, respectively; P < 0.05; Fig. 2b). Endothelial cells can be labeled by CD34. The number of CD34-positive vessels/mm2 can indicate the mean MVD. Immunohistochemistry staining revealed that the number of CD34-positive vessels was higher in the bradykinin group than the control group (42.13 ± 2.59/mm2 vs. 31.92 ± 1.40/mm2, respectively; P < 0.05; Fig. 3a, b).
Western blot assay for VEGF
The expression of VEGF in the CVZ of all perforator flaps was revealed by western blotting (Fig. 4a). VEGF expression was higher in the bradykinin group (P < 0.05; Fig. 4b).
Western blot analyses of the apoptotic index
The expression of apoptotic proteins, including cleaved caspase-3, Bax, and Bcl-2, was investigated. Cleaved caspase-3 and Bax are two types of apoptotic proteins that participate in apoptosis, whereas Bcl-2 can resist apoptosis [20, 21]. The levels of cleaved caspase-3 and Bax were decreased, whereas that of BCL-2 was increased on POD 7 in the bradykinin group (P < 0.05; Fig. 5a, b).
a Expression of apoptotic proteins (cleaved caspase-3, Bax, and BCL-2). b The relative protein levels of apoptotic proteins. Expression of apoptotic proteins were evaluated by optical density analyses, calculated as the fold relative to the control, and normalized to GAPDH. n = 5 per group. *P < 0.05
SOD and MDA content
Compared to the control group, mean SOD activity was much higher in the bradykinin group (45.46 ± 1.43 U mg protein−1 vs. 30.61 ± 1.47 U mg protein−1, respectively; P < 0.05; Fig. 6a). The bradykinin group also had a much lower mean level of MDA (41.39 ± 1.67 nmol mg protein−1) (60.05 ± 2.25 nmol mg protein−1; P < 0.05; Fig. 6b).
Western blot analyses of autophagy markers
Western blot was used to assess Beclin 1 and LC3II/LC3I expression in the CVZ of all perforator flaps. The ratio of LC3 II to LC3 I was downregulated as well as Beclin 1 in the bradykinin group. The control group had a higher LC3II/LC3I ratio and Beclin 1 expression than the bradykinin group (P < 0.05; Fig. 7a). p62 is a marker of autophagic flux. Expression of p62 was much higher in the bradykinin group than the control group (P < 0.05; Fig. 7b).
NO content
Compared to the control group, NO production was higher in the bradykinin group (1.18 ± 0.22 vs. 0.82 ± 0.15, respectively; P < 0.05; Fig. 8).
Discussion
Bradykinin, a vasoactive peptide, is produced by the protease degradation of high molecular weight or low molecular weight kininogens [29]. Bradykinin plays important roles in both acute and chronic inflammatory processes. However, it also has anti-apoptotic [30] and antioxidative [31] properties and promotes vascularization [32]. Thus, we hypothesized that bradykinin would improve the viability of multiterritory perforator flaps by promoting vascularization, suppressing apoptosis, inhibiting autophagy, promoting the release of NO, and reducing oxidative stress.
Several authors have reported that treatment with bradykinin increases VEGF expression in tumors [33]. VEGF can promote angiogenesis [13]. In a kininogen-deficient rat tumor model (which cannot intrinsically generate bradykinin), expression of VEGF and the extent of angiogenesis were significantly less than in normal rats [34]. In skin flaps, VEGF which is particularly active in dermal vascular structures is secreted by fibroblasts and keratinocytes in the cutis [35]. VEGF can also promote vascularization in multiterritory perforator flaps [27]. In our study, the VEGF protein levels were upregulated after treatment with bradykinin. Western blot analyses also showed lower VEGF levels in the control group than the bradykinin group. In addition, MVD showed more neovascularization in the bradykinin group relative to the control group. So, we know that bradykinin promotes vascularization in multiterritory perforator flaps by improving VEGF expression.
A postoperative flap that suffers from I/R injury exhibits increased production of ROS, apoptosis, inflammation, and so forth [36, 37]. Several publications have described effective therapeutic strategies for inhibiting I/R injury [36,37,38]. Among them, the use of hyperbaric oxygen to inhibit I/R injury is accepted both clinically and experimentally [39, 40]. Flap survival is further improved by combining treatment with hyperbaric oxygen and vascular growth factor [41, 42]. As mentioned previously, the pathophysiological action of I/R injury determined the final outcome of the flap.
Apoptosis plays a vital role in flap survival. The I/R process can induce apoptosis which can lead to cell death [43]. Burns et al. reported that cellular apoptosis can lead to I/R injury [43]. With less apoptosis, flaps exhibit a better blood supply and larger survival area [44]. When apoptosis is exacerbated, attenuation of apoptosis ameliorates healing. Bradykinin had an anti-apoptotic effect under conditions of diabetes [45]. Our results also show that bradykinin inhibits apoptosis, as reflected by increased BCL-2 levels and decreased Bax levels [46, 47]. We also found that cleaved caspase-3 activity was reduced in the bradykinin group [48]. So, we reach the conclusion that bradykinin can suppress apoptosis in a multiterritory perforator flap.
I/R injury can produce ROS, a significant component of the complex oxidation process. ROS include free radicals, oxygen ions, and peroxides that initiate I/R damage [49,50,51]. ROS formed during I/R injury cause a lot of changes that damage microcirculation (e.g., swelling of endothelial cells, vasoconstriction) [37]. When skin flaps experience ischemia, the oxidase system will be upregulated significantly [52, 53]. This system is an important source of ROS production during ischemia [54, 55]. Inhibition of the xanthine oxidase system reduces the formation of ROS and increases the survival rate of flaps [53, 56]. MDA content and SOD activity are biomarkers of oxidative stress. In our research, we used MDA content and SOD activity to assess oxidative stress. Bradykinin has a cardioprotective effect in acute cardiac I/R injury [57]. In this research, the MDA content was much lower in the bradykinin group relative to the control group, whereas SOD activity was higher. Thus, bradykinin suppresses oxidative stress in multiterritory perforator flaps.
ROS can induce angiogenesis but an excessive amount of ROS inhibits angiogenesis [58,59,60]. It remains to be determined about the effects of ROS on angiogenesis. These effects are likely dependent on different characteristics of a disease. In the present study, bradykinin improved the survival of multiterritory perforator flaps by suppressing oxidative stress and accelerating vascularization. However, the relationship between oxidative stress and vascularization in multiterritory perforator flaps after treatment with bradykinin remains to be confirmed.
Scherz–Shouval and Elazar previously reported that ROS induces autophagy [61]. By contrast, Vande et al. reported that excessive autophagy increased the level of ROS production [62]. Excessive autophagic activity has a detrimental effect. It can consume functional components under conditions of excessive autophagy and promote cell death [20, 63]. For instance, many experts have reported that excessive autophagy enhances apoptosis, ROS production, and tissue injury [62,63,64]. The effects of autophagy vary by disease or different periods of a disease [65]. Wang et al. reported that inhibiting autophagy enhanced perforator flap survival [8]. In the current study, bradykinin also regulated autophagy levels. Western blot analyses revealed that expression of LC3II/LC3I and Beclin 1 decreased, which indicates that autophagy was inhibited in the bradykinin group. p62 is an autophagic flux marker. p62 was increased in the group treated with bradykinin, which indicates that autophagy was inhibited. Thus, bradykinin likely downregulates the level of autophagy in multiterritory perforator flaps.
Several authors have reported that bradykinin can activate the PI3K/Akt signaling pathway [18, 24, 66]. This signaling pathway promotes the release of NO [22, 23]. Low levels of NO inhibit PTEN activity, thereby stimulating the Akt signaling pathway, which suppresses neuronal apoptosis [67]. Inactivation of PTEN results in increased mTORC1 activity, leading to the inhibition of autophagy [19]. NO, the product of NOS, promotes cell proliferation and angiogenesis [25], which is also beneficial for flap survival. In our study, NO levels decreased in the control group compared to the bradykinin group. Thus, NO inhibits apoptosis, autophagy, and tissue injuries. From the results, we conclude that bradykinin suppresses apoptosis and autophagy by promoting the release of NO in perforator flaps. The function of NO in angiogenesis is also important for flap survival.
Conclusion
Bradykinin increased angiogenesis, suppressed apoptosis, inhibited autophagy, and suppressed oxidative stress, leading to higher perforator flap survival rate. In addition, NO production was promoted in perforator flaps treated with bradykinin, which may suppress apoptosis and inhibit autophagy.
Abbreviations
- BK:
-
Bradykinin
- CON:
-
Control
- CST:
-
Cell Signaling Technology
- CVZ:
-
Choke vessel zone
- DCI:
-
Deep circumflex iliac
- DCIA:
-
Deep circumflex iliac artery
- H&E:
-
Hematoxylin and eosin
- I/R:
-
Ischemia–reperfusion
- IC:
-
Intercostal artery
- IHC:
-
Immunohistochemistry
- MDA:
-
Malondialdehyde
- MVD:
-
Microvascular density
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- POD:
-
Postoperative day
- PU:
-
Perfusion units
- SEMs:
-
Standard errors of the mean
- SOD:
-
Superoxide dismutase
- TD:
-
Thoracodorsal artery
- VEGF:
-
Vascular endothelial growth factor
References
Taylor GI, Corlett RJ, Dhar SC, Ashton MW. The anatomical (angiosome) and clinical territories of cutaneous perforating arteries: development of the concept and designing safe flaps. Plast Reconstr Surg. 2011;127(4):1447–59.
Morris SF, Tang M, Almutari K, Geddes C, Yang D. The anatomic basis of perforator flaps. Clin Plast Surg. 2010;37(4):553–70 xi.
Taylor GI, Corlett RJ, Caddy CM, Zelt RG. An anatomic review of the delay phenomenon: II. Clin Appl Plast Reconstr Surg. 1992;89(3):408–16 discussion 417-408.
Miyamoto S, Minabe T, Harii K. Effect of recipient arterial blood inflow on free flap survival area. Plast Reconstr Surg. 2008;121(2):505–13.
Fichter AM, Ritschl LM, Robitzky LK, et al. Impact of different antithrombotics on the microcirculation and viability of perforator-based ischaemic skin flaps in a small animal model. Sci Rep. 2016;6:35833.
Yang M, Sheng L, Li H, Weng R, Li QF. Improvement of the skin flap survival with the bone marrow-derived mononuclear cells transplantation in a rat model. Microsurgery. 2010;30(4):275–81.
Lima LP, de Oliveira AA, de Lima Silva JJ, et al. Electroacupuncture attenuates oxidative stress in random skin flaps in rats. Aesthet Plast Surg. 2012;36(5):1230–5.
Wang L, Jin Z, Wang J, et al. Detrimental effect of hypoxia-inducible factor-1alpha-induced autophagy on multiterritory perforator flap survival in rats. Sci Rep. 2017;7(1):11791.
Dewhirst MW, Vinuya RZ, Ong ET, et al. Effects of bradykinin on the hemodynamics of tumor and granulating normal tissue microvasculature. Radiat Res. 1992;130(3):345–54.
Steranka LR, Farmer SG, Burch RM. Antagonists of B2 bradykinin receptors. FASEB J. 1989;3(9):2019–25.
Kaplan AP, Silverberg M, Ghebrehiwet B, Atkins P, Zweiman B. The kallikrein-kinin system in inflammation. Adv Exp Med Biol. 1989;247A:125–36.
Miura S, Matsuo Y, Saku K. Transactivation of KDR/Flk-1 by the B2 receptor induces tube formation in human coronary endothelial cells. Hypertension. 2003;41(5):1118–23.
Kalka C, Tehrani H, Laudenberg B, et al. VEGF gene transfer mobilizes endothelial progenitor cells in patients with inoperable coronary disease. Ann Thorac Surg. 2000;70(3):829–34.
Yoshida H, Zhang JJ, Chao L, Chao J. Kallikrein gene delivery attenuates myocardial infarction and apoptosis after myocardial ischemia and reperfusion. Hypertension. 2000;35(1 Pt 1):25–31.
Cangiano E, Marchesini J, Campo G, et al. ACE inhibition modulates endothelial apoptosis and renewal via endothelial progenitor cells in patients with acute coronary syndromes. Am J Cardiovasc Drugs. 2011;11(3):189–98.
Mikrut K, Paluszak J, Kozlik J, et al. The effect of bradykinin on the oxidative state of rats with acute hyperglycaemia. Diabetes Res Clin Pract. 2001;51(2):79–85.
Xu X, Tu L, Jiang W, et al. Bradykinin prevents the apoptosis of NIT-1 cells induced by TNF-alpha via the PI3K/Akt and MAPK signaling pathways. Int J Mol Med. 2012;29(5):891–8.
Hammerschmidt S, Kuhn H, Gessner C, Seyfarth HJ, Wirtz H. Stretch-induced alveolar type II cell apoptosis: role of endogenous bradykinin and PI3K-Akt signaling. Am J Respir Cell Mol Biol. 2007;37(6):699–705.
Kaminskyy VO, Zhivotovsky B. Free radicals in cross talk between autophagy and apoptosis. Antioxid Redox Signal. 2014;21(1):86–102.
Smith CM, Chen Y, Sullivan ML, Kochanek PM, Clark RS. Autophagy in acute brain injury: feast, famine, or folly? Neurobiol Dis. 2011;43(1):52–9.
Nishida K, Yamaguchi O, Otsu K. Crosstalk between autophagy and apoptosis in heart disease. Circ Res. 2008;103(4):343–51.
Sheng ZL, Yao YY, Li YF, Fu C, Ma GS. Transplantation of bradykinin-preconditioned human endothelial progenitor cells improves cardiac function via enhanced Akt/eNOS phosphorylation and angiogenesis. Am J Transl Res. 2015;7(7):1214–26.
Yang XM, Krieg T, Cui L, Downey JM, Cohen MV. NECA and bradykinin at reperfusion reduce infarction in rabbit hearts by signaling through PI3K, ERK, and NO. J Mol Cell Cardiol. 2004;36(3):411–21.
Bell RM, Yellon DM. Bradykinin limits infarction when administered as an adjunct to reperfusion in mouse heart: the role of PI3K, Akt and eNOS. J Mol Cell Cardiol. 2003;35(2):185–93.
Moraes MS, Costa PE, Batista WL, et al. Endothelium-derived nitric oxide (NO) activates the NO-epidermal growth factor receptor-mediated signaling pathway in bradykinin-stimulated angiogenesis. Arch Biochem Biophys. 2014;558:14–27.
Malkesman O, Braw Y, Maayan R, et al. Two different putative genetic animal models of childhood depression. Biol Psychiatry. 2006;59(1):17–23.
Tao XY, Wang L, Gao WY, et al. The effect of inducible nitric oxide synthase on multiterritory perforator flap survival in rats. J Reconstr Microsurg. 2016;32(9):643–9.
Nemethova M, Talian I, Danielisova V, et al. Delayed bradykinin postconditioning modulates intrinsic neuroprotective enzyme expression in the rat CA1 region after cerebral ischemia: a proteomic study. Metab Brain Dis. 2016;31(6):1391–403.
Deacon K, Knox AJ. Human airway smooth muscle cells secrete amphiregulin via bradykinin/COX-2/PGE2, inducing COX-2, CXCL8, and VEGF expression in airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2015;309(3):L237–49.
Kono Y, Sawada S, Kawahara T, et al. Bradykinin inhibits serum-depletion-induced apoptosis of human vascular endothelial cells by inducing nitric oxide via calcium ion kinetics. J Cardiovasc Pharmacol. 2002;39(2):251–61.
Kayashima Y, Smithies O, Kakoki M. The kallikrein-kinin system and oxidative stress. Curr Opin Nephrol Hypertens. 2012;21(1):92–6.
Parenti A, Morbidelli L, Ledda F, Granger HJ, Ziche M. The bradykinin/B1 receptor promotes angiogenesis by up-regulation of endogenous FGF-2 in endothelium via the nitric oxide synthase pathway. FASEB J. 2001;15(8):1487–9.
Ishihara K, Kamata M, Hayashi I, Yamashina S, Majima M. Roles of bradykinin in vascular permeability and angiogenesis in solid tumor. Int Immunopharmacol. 2002;2(4):499–509.
Ikeda Y, Hayashi I, Kamoshita E, et al. Host stromal bradykinin B2 receptor signaling facilitates tumor-associated angiogenesis and tumor growth. Cancer Res. 2004;64(15):5178–85.
Detmar M, Yeo KT, Nagy JA, et al. Keratinocyte-derived vascular permeability factor (vascular endothelial growth factor) is a potent mitogen for dermal microvascular endothelial cells. J Invest Dermatol. 1995;105(1):44–50.
Wang WZ, Baynosa RC, Zamboni WA. Update on ischemia-reperfusion injury for the plastic surgeon: 2011. Plast Reconstr Surg. 2011;128(6):685e–92e.
van den Heuvel MG, Buurman WA, Bast A, van der Hulst RR. Review: ischaemia-reperfusion injury in flap surgery. J Plast Reconstr Aesthet Surg. 2009;62(6):721–6.
Leite MT, Gomes HC, Percario S, Russo CR, Ferreira LM. Dimethyl sulfoxide as a block to the deleterious effect of nicotine in a random skin flap in the rat. Plast Reconstr Surg. 2007;120(7):1819–22.
Xiao YD, Liu YQ, Li JL, et al. Hyperbaric oxygen preconditioning inhibits skin flap apoptosis in a rat ischemia-reperfusion model. J Surg Res. 2015;199(2):732–9.
Perrins DJ. Influence of hyperbaric oxygen on the survival of split skin grafts. Lancet. 1967;1(7495):868–71.
Bayati S, Russell RC, Roth AC. Stimulation of angiogenesis to improve the viability of prefabricated flaps. Plast Reconstr Surg. 1998;101(5):1290–5.
Xie XG, Zhang M, Dai YK, Ding MS, Meng SD. Combination of vascular endothelial growth factor-loaded microspheres and hyperbaric oxygen on random skin flap survival in rats. Exp Ther Med. 2015;10(3):954–8.
Burns AT, Davies DR, McLaren AJ, et al. Apoptosis in ischemia/reperfusion injury of human renal allografts. Transplantation. 1998;66(7):872–6.
Song K, Zhang M, Hu J, et al. Methane-rich saline attenuates ischemia/reperfusion injury of abdominal skin flaps in rats via regulating apoptosis level. BMC Surg. 2015;15:92.
Kwak SJ, Paeng J, Kim DH, et al. Local kallikrein-kinin system is involved in podocyte apoptosis under diabetic conditions. Apoptosis. 2011;16(5):478–90.
Xia CF, Yin H, Yao YY, et al. Kallikrein protects against ischemic stroke by inhibiting apoptosis and inflammation and promoting angiogenesis and neurogenesis. Hum Gene Ther. 2006;17(2):206–19.
Xia CF, Yin H, Borlongan CV, Chao L, Chao J. Kallikrein gene transfer protects against ischemic stroke by promoting glial cell migration and inhibiting apoptosis. Hypertension. 2004;43(2):452–9.
Tang M, Cui M, Dong Q, et al. The bradykinin B2 receptor mediates hypoxia/reoxygenation induced neuronal cell apoptosis through the ERK1/2 pathway. Neurosci Lett. 2009;450(1):40–4.
Kerrigan CL, Stotland MA. Ischemia reperfusion injury: a review. Microsurgery. 1993;14(3):165–75.
Aydogan H, Gurlek A, Parlakpinar H, et al. Beneficial effects of caffeic acid phenethyl ester (CAPE) on the ischaemia-reperfusion injury in rat skin flaps. J Plast Reconstr Aesthet Surg. 2007;60(5):563–8.
Feng GM, Yang WG, Huan-Tang Chen S, et al. Periodic alterations of jejunal mucosa morphology following free microvascular transfer for pharyngoesophageal reconstruction. J Plast Reconstr Aesthet Surg. 2006;59(12):1312–7.
Im MJ, Hoopes JE, Yoshimura Y, Manson PN, Bulkley GB. Xanthine: acceptor oxidoreductase activities in ischemic rat skin flaps. J Surg Res. 1989;46(3):230–4.
Angel MF, Im MJ, Chung HK, Vander Kolk CA, Manson PN. Effects of combined cold and hyperbaric oxygen storage on free flap survival. Microsurgery. 1994;15(9):648–51.
Shah AM, Channon KM. Free radicals and redox signalling in cardiovascular disease. Heart. 2004;90(5):486–7.
Kakita T, Suzuki M, Takeuchi H, Unno M, Matsuno S. Significance of xanthine oxidase in the production of intracellular oxygen radicals in an in-vitro hypoxia-reoxygenation model. J Hepato-Biliary-Pancreat Surg. 2002;9(2):249–55.
Im MJ, Manson PN, Bulkley GB, Hoopes JE. Effects of superoxide dismutase and allopurinol on the survival of acute island skin flaps. Ann Surg. 1985;201(3):357–9.
Egom EE, Ke Y, Solaro RJ, Lei M. Cardioprotection in ischemia/reperfusion injury: spotlight on sphingosine-1-phosphate and bradykinin signalling. Prog Biophys Mol Biol. 2010;103(1):142–7.
Ushio-Fukai M, Tang Y, Fukai T, et al. Novel role of gp91(phox)-containing NAD(P)H oxidase in vascular endothelial growth factor-induced signaling and angiogenesis. Circ Res. 2002;91(12):1160–7.
West XZ, Malinin NL, Merkulova AA, et al. Oxidative stress induces angiogenesis by activating TLR2 with novel endogenous ligands. Nature. 2010;467(7318):972–6.
Okuno Y, Nakamura-Ishizu A, Otsu K, Suda T, Kubota Y. Pathological neoangiogenesis depends on oxidative stress regulation by ATM. Nat Med. 2012;18(8):1208–16.
Scherz-Shouval R, Elazar Z. Regulation of autophagy by ROS: physiology and pathology. Trends Biochem Sci. 2011;36(1):30–8.
Vande Velde C, Cizeau J, Dubik D, et al. BNIP3 and genetic control of necrosis-like cell death through the mitochondrial permeability transition pore. Mol Cell Biol. 2000;20(15):5454–68.
Matsui Y, Takagi H, Qu X, et al. Distinct roles of autophagy in the heart during ischemia and reperfusion: roles of AMP-activated protein kinase and Beclin 1 in mediating autophagy. Circ Res. 2007;100(6):914–22.
Zheng B, Mao JH, Qian L, et al. Pre-clinical evaluation of AZD-2014, a novel mTORC1/2 dual inhibitor, against renal cell carcinoma. Cancer Lett. 2015;357(2):468–75.
Zhou KL, Zhang YH, Lin DS, Tao XY, Xu HZ. Effects of calcitriol on random skin flap survival in rats. Sci Rep. 2016;6:18945.
Dong R, Chen W, Feng W, et al. Exogenous bradykinin inhibits tissue factor induction and deep vein thrombosis via activating the eNOS/phosphoinositide 3-kinase/Akt signaling pathway. Cell Physiol Biochem. 2015;37(4):1592–606.
Numajiri N, Takasawa K, Nishiya T, et al. On-off system for PI3-kinase-Akt signaling through S-nitrosylation of phosphatase with sequence homology to tensin (PTEN). Proc Natl Acad Sci U S A. 2011;108(25):10349–54.
Acknowledgements
Not applicable
Funding
This research was sustained by Zhejiang Province Medical Science and Technology Project of China (2014ZDA015) and Zhejiang Province Natural Science Foundation of China (LY15H060010).
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Author information
Authors and Affiliations
Contributions
JW designed the study. CL, LW, LD, and JW collected the data. JW performed the statistical analysis. JW and EJ drafted the manuscript. JW and WG revised and proofread the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Eighty healthy male Sprague-Dawley rats weighing 250 to 300 g were purchased from Wenzhou Medical University (License No. SCXK [ZJ] 2015–0001). All use procedures and animal care conformed to the Health Guidelines National Institutes for the Care and Use of Laboratory Animals. The Wenzhou Medical University Animal Research Committee approved the study (wydw 2014–0015).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wang, J., Ji, E., Lin, C. et al. Effects of bradykinin on the survival of multiterritory perforator flaps in rats. World J Surg Onc 17, 44 (2019). https://doi.org/10.1186/s12957-019-1570-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-019-1570-3