Abstract
Background
Duchenne muscular dystrophy (DMD) is a genetic disease resulting in progressive muscle weakness, loss of ambulation, and cardiorespiratory complications. Direct estimation of health-related quality of life for patients with DMD is challenging, highlighting the need for proxy measures. This study aims to catalog and compare existing published health state utility estimates for DMD and related conditions.
Methods
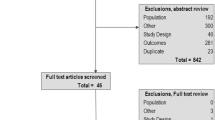
Using two search strategies, relevant utilities were extracted from the Tufts Cost-Effectiveness Analysis Registry, including health states, utility estimates, and study and patient characteristics. Analysis One identified health states with comparable utility estimates to a set of published US patient population utility estimates for DMD. A minimal clinically important difference of ± 0.03 was applied to each DMD utility estimate to establish a range, and the registry was searched to identify other health states with associated utilities that fell within each range. Analysis Two used pre-defined search terms to identify health states clinically similar to DMD. Mapping was based on the degree of clinical similarity.
Results
Analysis One identified 4,308 unique utilities across 2,322 cost-effectiveness publications. The health states captured a wide range of acute and chronic conditions; 34% of utility records were extrapolated for US populations (n = 1,451); 1% were related to pediatric populations (n = 61). Analysis Two identified 153 utilities with health states clinically similar to DMD. The median utility estimates varied among identified health states. Health states similar to the early non-ambulatory DMD phase exhibited the greatest difference between the median estimate of the sample (0.39) and the existing estimate from published literature (0.21).
Conclusions
When available estimates are limited, using novel search strategies to identify utilities of clinically similar conditions could be an approach for overcoming the information gap. However, it requires careful evaluation of the utility instruments, tariffs, and raters (proxy or self).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Duchenne muscular dystrophy (DMD) is a rare, X-linked neuromuscular disease characterized by progressive muscle weakness [1, 2], affecting approximately 1 in 3,500-5,050 live male births [3, 4, 5]. DMD is typically diagnosed in early childhood and presents with a progressive, irreversible course, including loss of ambulation followed by loss of upper limb, respiratory, and cardiac function [6,7,8]. Patients with DMD generally pass away prematurely in the third decade of life [4, 9]. Although there is no cure for DMD, management includes corticosteroids, physical therapy, assisted ventilation, and spinal surgery [8]. Exon-skipping therapies and gene therapy are available to a subset of patients [10,11,12,13,14].
Measuring health-related quality of life (HRQoL) is critical for providing insight into the overall burden of chronic health conditions, such as DMD [15]. Due to its clinical severity, the HRQoL among patients with DMD is substantially lower than that of the general population, decreasing as the disease progresses [16].
HRQoL can be quantified using health state utilities (i.e., preference for a particular health status). Utility estimates, which are presented on a cardinal scale of 0 to 1 with 0 representing death and 1 representing perfect health, are derived through a variety of methods broadly categorized as either direct or indirect measures [17]. The Health Utilities Index (HUI) Questionnaire is one of the most commonly used approaches for estimating utilities in DMD [18].
Health state utilities are used to calculate quality-adjusted life years (QALYs), the most common health metric used in health economic evaluations. Cost-effectiveness analyses (CEAs) aim to maximize health benefits given available resources and could be used to aid in reimbursement or resource allocation decisions [17, 19]. Over the last 40 years, the number of published CEAs has increased substantially [20, 21]. Within the United States (US), CEAs are also used to inform the value of drugs and emerging health technologies, and are cited in practice guidelines or insurance policies [19].
Despite its importance in understanding patients’ burden and influencing decision-making, measuring the HRQoL in DMD remains a challenge. Available research is limited due to small patient populations and limited standardized utility estimation methods for pediatric populations [22, 23], and systematic reviews have noted the relative lack of published studies evaluating DMD-specific utility values [4, 24]. In these studies, health states generally focus on ambulatory ability (i.e., early ambulatory [EA], late ambulatory [LA], early non-ambulatory [ENA], and late non-ambulatory [LNA]). Thus, it is important to contextualize available utility estimates for DMD health states relative to other diseases. Using utilities of clinically similar conditions could be a strategy for overcoming limited available estimates. This study aims to catalog and compare existing published utilities for DMD with those reported for comparable conditions.
Methods
Resources and utility selection
Published utility estimates were identified using the Tufts CEA Registry [21], a comprehensive database of CEAs published from 1976 to the present. The CEA Registry focuses on a subset of cost-utility analyses that quantify health benefits in QALYs, which account for changes in both longevity and utility. At the time of this analysis, there were over 33,000 utility weights across more than 10,000 CEAs published from 1976 to 2021 within the registry [21]. Eligible utility weight records included those derived from various countries, diseases, utility instruments, preference weights, and respondent types (i.e., proxy or self).
Analysis One: identify and catalog comparable utility estimates to DMD
The first analysis consisted of identifying health states that have comparable HRQoL utility estimates with published US DMD utility estimates. First, utility estimates for four major DMD health states were obtained through the only available US study published at the time of the analysis: EA (utility, 0.73), LA (0.64), ENA (0.21), and LNA (0.18) [25]. These values were derived using the HUI Questionnaire Mark 3.0 online. Next, a minimal clinically important difference (MCID) of ± 0.03 was applied to each estimate to establish a utility range (Table 1). This range was deemed reasonable for generic multi-attribute preference-based measures because health states that differ by < ± 0.03 units cannot be reliably differentiated; utility estimates with changes > 0.03 are generally regarded as a significant change [17, 26, 27]. The registry was next searched to identify other health states with associated utilities that fell within each range. All utility instruments in addition to the HUI were included in the analysis although utility instruments were not universally captured in the registry if unspecified in the original study. Utility records were excluded if the health state was unspecified (i.e., intervention-specific utilities with no designated clinical condition), a disutility, or a duplicate record (i.e., records with identical health states and utility estimates).
Analysis Two: identify and catalog comparable health states to DMD
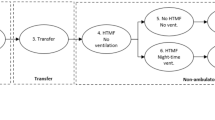
The second analysis consisted of identifying HRQoL utility estimates for health states that are similar to the clinical conditions of DMD. The registry was searched using pre-defined search terms, such as difficulty walking, joint and muscle weakness, loss of ambulation, and the use of a wheelchair (Table S1). These search terms were derived by the co-authors based on their understanding of DMD.
A clinical expert in DMD presentation (coauthor RS) next mapped each identified health state to five possible categories based on the degree of clinical similarity: EA, LA, ENA, LNA, and undetermined. Health states were first classified as ambulant or non-ambulant. If the health state was ambulant, then they were classified as either EA or LA depending on the severity of the health state. More severe ambulant health states in which individuals were able to walk independently but may have been falling or requiring assistance for stairs were classified as LA. Health states that required assistance to walk or stand or that used a wheelchair were classified as non-ambulant. The non-ambulant health states were further classified into ENA or LNA based on severity of symptoms. If respiratory support was required (such as in spinal muscular atrophy type 1), then they were classified similar to LNA. Health states, such as “secondary progressive multiple sclerosis expanded disability status scale 6<: walking aid or wheelchair required and restricted to bed,” were too broad, covering LA, ENA, and LNA health states; therefore, they were classified as LA, ENA, and LNA and given a low relevancy score. Others that were too general (e.g., “severe musculoskeletal pain”) did not provide enough information to be classified into a health state.
Once the health state was mapped, the clinical expert gave a “relevancy score” on a scale of 0 to 10 based on how clinically similar the health state was to the DMD health state: score of 10, absolute relevance; score of < 10 to ≥ 8, substantial relevance; score of < 8 to ≥ 6, moderate relevance; <6 to ≥ 4, fair relevance; and < 4, slight-to-poor relevance. Health states were not specifically restricted to those plausible for a DMD model but had to reflect the signs and/or symptoms that would be relevant to DMD. For example, the multiple sclerosis health state, “relapsing-remitting multiple sclerosis, expanded disability status scale: confined to bed and can still communicate and eat,” had a score of 10 and was mapped to the DMD LNA state. In addition, patients may experience the same condition in multiple DMD health states; therefore, some health states were mapped to ≥ 2 DMD health states. For example, a “gait disturbance” health state from a CEA studying surgical treatments for essential tremor [28] received a relevancy score of 5 for both the EA and LA states. This indicated some ambiguity of the health state being mapped, but general relevance with a DMD health state.
These relevancy scores were assigned using subjective, albeit expert, judgment. As a result, the set of health states with relevancy scores of 10 were used in the base case analysis while those with relevancy scores ≥ 8 were used in sensitivity analysis.
Data extraction and statistical analyses
The following data were extracted from each utility record for both analyses: study reference information (e.g., primary author, journal, year of publication), health state, and utility estimate. When available, baseline clinical and demographic characteristics, sample size, utility instrument, and respondent type (i.e., patient, parent/caregiver; and proxy or direct) were also extracted. Data from eligible studies were extracted using Stata® (Version 15.1) [29] and recorded in Microsoft Excel® (2013) [30]. Table S2 provides a detailed list of all data extracted for each identified utility record. After all data were extracted, descriptive statistics were calculated, including mean, median, standard deviation, and interquartile range. Summary statistics were stratified by the four DMD health states.
Results
Analysis One: Health states with utility estimates comparable to DMD health states
Analysis One identified 7,914 potentially relevant utility records; 3,606 (45.6%) were deemed ineligible and excluded from the study (i.e., non-specified health states, disutilities, or duplicate records). The remaining 4,308 (54.4%) unique utility records were included and mapped to the relevant DMD health state based on the utility estimate for each identified health state: EA (0.70–0.76), LA (0.61–0.67), ENA (0.18–0.24), and LNA (0.15–0.21). These utility records were extracted from 2,322 unique CEA studies. Significantly more utility records were identified for the ambulatory phases (EA, n = 2,174; LA, n = 1,841) than for the non-ambulatory phases (ENA, n = 223; LNA, n = 217). Given an overlap between the MCID utility range for the ENA and LNA phases, health states with utility estimates that ranged 0.18 to 0.21 (n = 147) were included in both ENA and LNA datasets.
The identified utilities included a variety of health states representing a wide range of acute and chronic diseases (Table 1). Whereas myocardial infarction, coronary heart disease, chronic obstructive pulmonary disease, locoregional breast cancer, and type 2 diabetes were the most common health states that fell within EA ranges, non-small cell lung cancer, end-stage renal disease, stroke, and hip fracture were the most common that fell within LA ranges. Due to the substantially lower utility range thresholds, health states for the non-ambulatory phases represented more severe, terminal, or chronic conditions, including severe stroke, chronic liver disease, terminal breast cancer, and Alzheimer’s disease. Table 2 provides summary statistics of the identified utility records. Table S3 provides health states, utility values, and study characteristics that specifically utilized the HUI instrument, which was also utilized in the study from which the DMD health state utilities were obtained.
A third of the utilities were derived from US-based CEAs (Table 2). For the non-ambulatory phases, 62 (4.3%) of the identified utilities from US-based CEAs had estimates ranging from 0.18 to 0.21 and were included in both ENA and LNA datasets. The majority of identified utility records from US-based CEAs originated from secondary sources (i.e., extrapolated from other studies and then included in the CEA model); however, it was unclear whether the utility was originally estimated from US populations. Of those utilities from US-based CEAs, 34 (2.3%) were estimated using the HUI instrument (EA, n = 16/706 [2.3%]; LA, 12/642 [1.9%]; ENA, n = 6/103 [5.8%]).
Of the 4,015 identified ambulatory DMD health state utilities, less than a fifth mentioned the age of the population (EA, n = 471/2,174 [21.7%]; LA, n = 218/1,841 [11.8%]). Among those utilities that reported an age, populations ranged from newborns/infants to > 95 years of age, although most utilities represented adult populations ≥ 18 years or older (EA, n = 442 [93.8%]; LA, n = 208 [95.4%]). Only 51 utilities represented pediatric populations (i.e., ≤ 17 years) (EA, n = 37 [7.9%]; LA, n = 14 [6.4%]). A handful included both pediatric and adult populations (EA, n = 8 [1.7%]; LA, n = 4 [1.8%]). For non-ambulatory phase utilities, less than a third mentioned the population age (ENA, n = 37/223 [16.6%]; LNA, n = 34/217 [15.7%]), with 26 of those utilities included in both datasets. Table 2 shows summary statistics of utility records for pediatric populations. Most included ambulatory utilities versus non-ambulatory utilities.
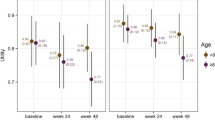
Analysis Two: Health states with clinical similarities to DMD health states
Using the pre-defined search terms listed in Table S1, 236 eligible utility records with health state descriptions that included one of those terms were identified. After the clinical expert mapped each to a DMD health state based on clinical similarity, 48.3% (n = 114) of the health states received a relevancy score of 10 (i.e., absolutely relevant to the clinical conditions of the mapped DMD health state) with median utility estimates of 0.71 (n = 35) for those mapped to EA, 0.54 (n = 31) for LA, 0.39 (n = 39) for ENA, and 0.30 (n = 9) for LNA (Table 3). The median utility estimates deviated from published utility estimates for DMD by varying degrees. Given the highly skewed distributions of utility values within each sample as seen by the interquartile ranges, the median value was considered rather than the mean. Health states clinically similar to the ENA phase exhibited the greatest deviation where the median utility estimate (0.39) was 85.7% higher compared to the published DMD estimate (0.21) (Fig. 1A). Health states clinically similar to the LNA health state (0.30) were 66.7% higher than the published DMD estimate (0.18). Health states clinically similar to the EA phase exhibited the smallest difference (0.73 vs. 0.71, 2.7% decrease) (Table 4; Fig. 1B).
Differences in utility estimates for health states clinically similar to DMD and existing DMD utility estimates. (A) Changes in utility estimates compared to existing utility estimates for each DMD health state for the total sample of utilities with a relevancy score of 10 (n = 114). (B) Changes in utility estimates compared to existing utility estimates for each DMD health state for the sample of utilities from a US-based CEA study with a relevancy score of 10 (n = 31). CEA, cost-effectiveness analysis; DMD, Duchenne muscular dystrophy; HRQoL, Health-related quality of life; ∆, change in utility estimate; Mdn, median; US, United States
From the 236 health states identified in Analysis Two, 26.3% (n = 62) were from US-based CEAs. However, 79.0% (n = 49) of those utilities originated from a secondary source, which may or may not have been a US-based utility study. The difference in utility value was more pronounced when comparing utilities extracted from US-based CEAs compared with those in the overall analysis. The US-based median utility estimates with a relevancy score of 10 (n = 31) deviated substantially from published DMD health states with the LNA and ENA health states exhibiting the greatest difference (127.8% and 114.3% increase, respectively) (Table 4; Fig. 1B).
When expanding the criteria to include relevancy scores ≥ 8, 64.8% (n = 153) of the health states were considered substantially or absolutely relevant to their mapped DMD health state. This more relaxed criterion mapped 39 additional health states. With the exception of the LNA health state, the median utility estimates did not differ from those obtained from the more stringent criterion (i.e., relevancy score of 10) (Table 3, Figure S1). For the LNA health state, the gap closed considerably between the median estimates of the sensitivity analysis (0.20) and the published DMD estimate (0.18). The number of mapped health states nearly doubled for this DMD phase, resulting in a highly skewed distribution of utility estimates (interquartile range, 0.05–0.41). When the relevancy score criterion was relaxed to ≥ 8 for the US-based CEA utility estimates, there were still considerable differences compared to the DMD estimates for the ENA and LNA phases (0.45 vs. 0.21 and 0.40 vs. 0.18, respectively) (Table 4, Figure S2).
There was uncertainty surrounding the clinical similarity of the 136 health states that received a relevancy score of < 8. Figure S3 provides a distribution of relevancy scores, stratified by level of relevance and each mapping category. Due to highly ambiguous descriptions, the clinical similarity of 12.7% (n = 30) of the health states could not be determined. For example, “musculoskeletal pain” is a common problem experienced by patients with DMD to varying degrees across all ambulatory phases although not routinely assessed [31]. Thus, the health state could not be mapped with any level of certainty to a specific DMD health state. Figures S4 and S5 and Table S4 show the statistics of health states with relevancy scores ≥ 6 or ≥ 4.
Only 6.4% (n = 15) of the health states identified in Analysis Two mentioned the age of the populations, ranging from newborns/infants to adults ≥ 60 years. Most represented adult populations of an unspecified age range (80.0%, n = 12). Two health states represented adults ≥ 50 years, while only one health state represented newborns/infants.
Discussion
This study implemented novel search strategies to catalog and compare a variety of health state utilities to those existing for DMD. This methodology as applied to the Tufts CEA Registry database is the first study of its kind to the authors’ awareness, and provides a blueprint for future studies, particularly studies to provide context for utilities for rare diseases where estimates are limited or based on small sample sizes. In Analysis One, which identified health states with comparable utility values to the four DMD health states, there were substantially more utility values found within the range for EA and LA utility estimates compared to the range for ENA and LNA utility estimates. These data highlight that more diseases have utility estimates closer to 1 than to 0. A sample of health states with similar utility values to the four DMD health states demonstrates a wide range of health conditions and provides context for the DMD utility estimates. In Analysis Two, which identified health states that were clinically similar to DMD health states albeit to varying degrees, nearly half were deemed absolutely relevant to a single DMD state. However, the utility values deviated from published DMD utility values. In health states clinically similar to the ENA and LNA health states, utility estimates were higher compared to the published DMD estimate; those clinically similar to the EA phase were similar.
Cataloging health states with similar utility estimates to DMD revealed contextual factors, such as clinical similarity, that are worth examining. Although health states identified in Analysis One share similar utility estimates to the US DMD population, there is a contrast when considering patient experiences, including the impact of the disease on various aspects of health which resulted in the corresponding utility estimate. While disease characteristics are unique, it is interesting to observe the various diseases with utilities close to the published DMD utilities. Of note, the published utility estimates for non-ambulatory patients with DMD were close to estimates for fatal conditions and events (e.g., terminal cancers or severe strokes). Among health states whose utilities were derived from the HUI instrument, the utility for moderate-to-advanced Alzheimer’s disease corresponded to those for non-ambulatory patients with DMD. However, for health states with utility estimates similar to the EA phase, diseases and severity varied and included cerebral palsy, single amputations, hearing loss, and myocardial infarctions.
In Analysis Two, there was immense variability between cataloged and existing utility estimates for the DMD US population, demonstrating the heterogeneity of available utility estimates. Median estimates from clinically similar health states (score of 10) to the LA, ENA, and LNA phases exhibited utility value differences greater than 0.03 (i.e., a MCID) compared with the published DMD estimates. In fact, health states mapped to the ENA phase had a median utility estimate that was nearly twice that of the published DMD estimate. While wide variability was observed between non-DMD and published DMD utility estimates, that variability is not solely due to the disease or condition itself. Utility values for a given health state are not absolute as they are dependent on the methodology and the type of respondent [17, 32]. Utility values can be estimated using a variety of methods, either direct or indirect [17]. This is particularly noteworthy in diseases that include a loss of mobility, where the impact of this loss on utility estimates can vary widely depending on the utility instrument [33]. Additionally, parents or caregivers are often the proxy respondents for young patients or those suffering from impairments too severe to express their own preferences [17, 22, 34]. Using public or proxy preferences for chronic conditions may not provide an accurate reflection of the patients’ experiences because patients learn to adapt to their disease over time [35, 36]. Thus, there can be substantial utility value variability for the exact same health state. The standard gamble method in direct utility elicitation exercises consistently provides higher utility estimates compared to a time-trade off approach [37]. Prior studies have also documented variation in HRQoL estimates for similar health states among a wide range of diseases and conditions [32]. For example, a “severe angina” health state utility estimate can range from 0.354 to 0.707 depending on severity, treatment type, patient group, and/or methodological characteristics (e.g., utility instrument, proxy measures, country) [32].
Since HRQoL estimates are an essential component of value assessments, variability in utility values can impact the informative power and comparability of economic evaluations [32]. For example, CEA results that use QALYs could differ dramatically depending on the utility values used. Furthermore, there may be difficulties in measuring utility estimates for rare diseases or pediatric populations [4, 22,23,24]. Researchers conducting CEAs may not have the resources to gather and estimate original HRQoL estimates in these challenging situations and may opt to leverage existing utility values from other sources for the CEA models [17, 32]. In fact, the overwhelming majority of health states cataloged in this study were extrapolated from secondary sources. However, definitions of DMD health states can vary because patients may experience similar symptoms in multiple health states, and there may be inconsistent definitions for the high-level health states [38, 39]. This can result in ambiguity in utility estimates, highlighted by the utility range overlap between for the ENA and LNA health states. This has implications for developing informative, comparable economic evaluations, which are becoming key to health care decision making [20, 40].
Utility estimates are also used for calculations of disease severity based on absolute or proportional QALY shortfalls [17, 41]. Some health technology assessment bodies consider QALY shortfalls in their value assessments to adjust the willingness-to-pay threshold, including the National Institute for Health and Care Excellence (NICE) in the United Kingdom [42], the National Health Care Institute in the Netherlands [43], and the Norwegian Institute of Public Health [44]. A new methodology, the Generalized Risk-Adjusted Cost-Effectiveness (GRACE), adjusts the willingness-to-pay threshold in a CEA based on numerous factors, including the severity of disease as reflected in the expected utility [45]. These changes to traditional CEA based on the QALY or expected utility highlight the importance of accurate utility measures.
Understanding patient preferences is critical to developing robust value assessments, especially given that patients’ feelings about their condition (e.g., losing the ability to walk) may not align with those of the general public [46,47,48,49]. This includes an analysis of DMD patients that observed noticeably higher visual analog scale (VAS) scores compared to HUI and EQ-5D scores, especially for non-ambulatory patients [49]. The results of this study could provide contextual considerations for existing utility estimates and corresponding value assessments. Extracting health states with similar utility estimates or clinically similar health states could be a good starting point. Although the focus of this study is on DMD, the methodology could be generalizable to other diseases with large variability or paucity of utility data (e.g., rare diseases, severe diseases, or diseases with heterogeneity in rate of progression). Specifically, decisionmakers may choose to assess treatments using utility values from clinically similar health states; however, further research is needed to assess decisionmakers’ willingness to apply this novel approach in practice. Furthermore, researchers could build models with alternative outcomes to examine the potential impact to reimbursement or resource allocation decisions. This is especially relevant to DMD where promising, novel treatments, such as gene therapy, are emerging [14, 50].
This study had some limitations. First, data for utility records sometimes lacked the specificity needed to extract information on population characteristics (e.g., age, sex, country) if the authors of the original CEA study failed to include detailed information on the health states and elicitation methods. Second, mapping the health states in Analysis Two to a DMD health state was based on subjective (albeit expert) assessments. As a result, the scaled score from 0 to 10 allowed some room for uncertainty, and sensitivity analyses were conducted on health states with relevancy scores ≥ 8. Furthermore, differences in the utility values found in Analysis Two could be due to several different factors given that utility estimates can vary depending on the population and methodology employed. Further studies are necessary to examine utility values by respondent and utility instrument utilized. Finally, the pre-defined search terms used in Analysis Two may not have been comprehensive.
Conclusion
This study identified heterogeneity in health state utility estimates for conditions with similar utility estimates to existing DMD utilities as well as significant variability in utility estimates for health states clinically similar to DMD. This methodology could yield contextual factors, such as clinical comparisons, that could inform economic evaluations but requires careful evaluation of the types of utility instruments, tariffs, and respondent type (proxy or self).
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CEA:
-
Cost-effectiveness analyses
- DMD:
-
Duchenne muscular dystrophy
- GRACE:
-
Generalized Risk-Adjusted Cost-Effectiveness
- HRQoL:
-
Health-related quality of life
- HUI:
-
Health Utilities Index
- MCID:
-
Minimal clinically important difference
- NICE:
-
National Institute for Health and Care Excellence
- QALYs:
-
Quality-adjusted life years
References
Bushby K, Finkel R, Birnkrant DJ, Case LE, Clemens PR, Cripe L, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and pharmacological and psychosocial management. Lancet Neurol. 2010;9:77–93.
Bushby K, Finkel R, Birnkrant DJ, Case LE, Clemens PR, Cripe L, Kaul A, Kinnett K, McDonald C, Pandya S, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: implementation of multidisciplinary care. Lancet Neurol. 2010;9:177–89.
Mendell JR, Shilling C, Leslie ND, Flanigan KM, al-Dahhak R, Gastier-Foster J, Kneile K, Dunn DM, Duval B, Aoyagi A, et al. Evidence-based path to newborn screening for Duchenne muscular dystrophy. Ann Neurol. 2012;71:304–13.
Szabo SM, Audhya IF, Malone DC, Feeny D, Gooch KL. Characterizing health state utilities associated with Duchenne muscular dystrophy: a systematic review. Qual Life Res. 2020;29:593–605.
Crisafulli S, Sultana J, Fontana A, Salvo F, Messina S, Trifirò G. Global epidemiology of Duchenne muscular dystrophy: an updated systematic review and meta-analysis. Orphanet J Rare Dis. 2020;15:141.
Hoffman EP, Brown RH Jr., Kunkel LM. Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell. 1987;51:919–28.
Humbertclaude V, Hamroun D, Bezzou K, Berard C, Boespflug-Tanguy O, Bommelaer C, Campana-Salort E, Cances C, Chabrol B, Commare MC, et al. Motor and respiratory heterogeneity in Duchenne patients: implication for clinical trials. Eur J Paediatr Neurol. 2012;16:149–60.
Salmaninejad A, Jafari Abarghan Y, Bozorg Qomi S, Bayat H, Yousefi M, Azhdari S, Talebi S, Mojarrad M. Common therapeutic advances for Duchenne muscular dystrophy (DMD). Int J Neurosci. 2021;131:370–89.
Broomfield J, Hill M, Guglieri M, Crowther M, Abrams K. Life Expectancy in Duchenne muscular dystrophy: reproduced individual Patient Data Meta-analysis. Neurology. 2021;97:e2304–14.
US Food and Drug Administration. VYONDYS 53 (golodirsen) injection, for intravenous use. Prescribing Information ed.; 2019.
US Food and Drug Administration. EXONDYS 51 (eteplirsen) injection, for intravenous use. Prescribing Information ed.; 2019.
US Food and Drug Administration. VILTEPSO (viltolarsen) injection, for intravenous use. Prescribing Information ed.; 2019.
US Food and Drug Administration. AMONDYS 45 (casimersen) injection, for intravenous use. Prescribing Information ed.; 2021.
US Food and Drug Administration. ELEVIDYS (delandistrogene moxeparvovec-rokl) suspension, for intravenous use. Prescribing Information ed.; 2024.
The World Health Organization Quality of Life assessment (WHOQOL). Position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9.
Landfeldt E, Lindgren P, Bell CF, Guglieri M, Straub V, Lochmuller H, Bushby K. Health-related quality of life in patients with Duchenne muscular dystrophy: a multinational, cross-sectional study. Dev Med Child Neurol. 2016;58:508–15.
Neumann PJGT, Russell LB, Sanders GD, Siegel JE. Second panel on cost-effectiveness in Health and Medicine. Oxford University Press; 2016.
Horsman J, Furlong W, Feeny D, Torrance G. The Health utilities Index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54.
Neumann PJ, Sanders GD. Cost-effectiveness analysis 2.0. N Engl J Med. 2017;376:203–5.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, Kuntz KM, Meltzer DO, Owens DK, Prosser LA, et al. Recommendations for Conduct, Methodological Practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in Health and Medicine. JAMA. 2016;316:1093–103.
Cost-Effectivness. Analysis Registry [www.cearegistry.org ].
Prosser LA. Current challenges and future research in measuring preferences for pediatric health outcomes. J Pediatr. 2009;155:7–9.
Thorrington D, Eames K. Measuring Health Utilities in Children and adolescents: a systematic review of the literature. PLoS ONE. 2015;10:e0135672.
Ryder S, Leadley RM, Armstrong N, Westwood M, de Kock S, Butt T, Jain M, Kleijnen J. The burden, epidemiology, costs and treatment for Duchenne muscular dystrophy: an evidence review. Orphanet J Rare Dis. 2017;12:79.
Landfeldt E, Lindgren P, Bell CF, Schmitt C, Guglieri M, Straub V, Lochmuller H, Bushby K. The burden of Duchenne muscular dystrophy: an international, cross-sectional study. Neurology. 2014;83:529–36.
Drummond M. Introducing economic and quality of life measurements into clinical studies. Ann Med. 2001;33:344–9.
Kaplan RM. The minimally clinically important difference in generic utility-based measures. COPD. 2005;2:91–7.
Li C, Gajic-Veljanoski O, Schaink AK, Higgins C, Fasano A, Sikich N, Dhalla I, Ng V. Cost-effectiveness of magnetic resonance-guided focused Ultrasound for essential tremor. Mov Disord. 2019;34:735–43.
StataCorp. Stata Statistical Software: release 15. College Station. TX: StataCorp LLC; 2017.
Microsoft Corporation. Microsoft Excel. Retrieved from https://office.microsoft.com/excel. 2013.
Kim A, Park M, Shin HI. Pain characteristics among individuals with Duchenne muscular dystrophy according to their clinical stage. BMC Musculoskelet Disord. 2022;23:536.
Tengs TO, Wallace A. One thousand health-related quality-of-life estimates. Med Care. 2000;38:583–637.
Freath LL, Curry AS, Cork DMW, Audhya IF, Gooch KL. QALYs and ambulatory status: societal preferences for healthcare decision making. J Med Econ. 2022;25:888–93.
Landfeldt E, Lindgren P, Bell CF, Guglieri M, Straub V, Lochmuller H, Bushby K. Quantifying the burden of caregiving in Duchenne muscular dystrophy. J Neurol. 2016;263:906–15.
Schwartz CE, Andresen EM, Nosek MA, Krahn GL, Measurement REPHS. Response shift theory: important implications for measuring quality of life in people with disability. Arch Phys Med Rehabil. 2007;88:529–36.
Vanier A, Oort FJ, McClimans L, Ow N, Gulek BG, Bohnke JR, Sprangers M, Sebille V, Mayo N. Response shift - in Sync Working G: response shift in patient-reported outcomes: definition, theory, and a revised model. Qual Life Res. 2021;30:3309–22.
Lipman SA, Brouwer WBF, Attema AE. What is it going to be, TTO or SG? A direct test of the validity of health state valuation. Health Econ. 2020;29:1475–81.
Kim J, Jung IY, Kim SJ, Lee JY, Park SK, Shin HI, Bang MS. A New Functional Scale and Ambulatory Functional classification of Duchenne muscular dystrophy: Scale Development and preliminary analyses of reliability and validity. Ann Rehabil Med. 2018;42:690–701.
Mercuri E, Signorovitch JE, Swallow E, Song J, Ward SJ, Group DMDI, Trajectory Analysis P. Categorizing natural history trajectories of ambulatory function measured by the 6-minute walk distance in patients with Duchenne muscular dystrophy. Neuromuscul Disord. 2016;26:576–83.
Rutten F. Economic evaluation and health care decision-making. Health Policy. 1996;36:215–29.
Brazier J. Valuing health states for use in cost-effectiveness analysis. PharmacoEconomics. 2008;26:769–79.
McDougall JA, Furnback WE, Wang BCM, Mahlich J. Understanding the global measurement of willingness to pay in health. J Mark Access Health Policy. 2020;8:1717030.
Reckers-Droog VT, van Exel NJA, Brouwer WBF. Looking back and moving forward: on the application of proportional shortfall in healthcare priority setting in the Netherlands. Health Policy. 2018;122:621–9.
Ottersen T, Forde R, Kakad M, Kjellevold A, Melberg HO, Moen A, Ringard A, Norheim OF. A new proposal for priority setting in Norway: open and fair. Health Policy. 2016;120:246–51.
Lakdawalla DN, Phelps CE. Health Technology Assessment with diminishing returns to Health: the generalized risk-adjusted cost-effectiveness (GRACE) Approach. Value Health. 2021;24:244–9.
Insinga RP, Fryback DG. Understanding differences between self-ratings and population ratings for health in the EuroQOL. Qual Life Res. 2003;12:611–9.
Polsky D, Willke RJ, Scott K, Schulman KA, Glick HA. A comparison of scoring weights for the EuroQol derived from patients and the general public. Health Econ. 2001;10:27–37.
Wilson R, Hansen P, Langley J, Derrett S. A comparison of injured patient and general population valuations of EQ-5D health states for New Zealand. Health Qual Life Outcomes. 2014;12:21.
Audhya IF, Szabo SM, Bever A, O’Sullivan F, Malone DC, Feeny D, Neumann P, Iannaccone ST, Jayasinghe P, Gooch KL. Estimating health state utilities in Duchenne muscular dystrophy using the health utilities index and EQ-5D-5L. J Patient Rep Outcomes. 2023;7:132.
Bez Batti Angulski A, Hosny N, Cohen H, Martin AA, Hahn D, Bauer J, Metzger JM. Duchenne muscular dystrophy: disease mechanism and therapeutic strategies. Front Physiol. 2023;14:1183101.
Acknowledgements
Dominic Voehler and Isabel Present assisted with data extraction.
Funding
This study was supported by Sarepta Therapeutics, Inc.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Lauren Do and David Kim. The first draft of the manuscript was written by Lauren Do and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
NA.
Consent for publication
NA.
Competing interests
At the time of the study, Lauren Do and David Kim were affiliated with the Cost-Effectiveness Analysis Registry that receives unrestricted sponsorships from a number of government, private foundation and pharmaceutical industry sponsors (full list is available at https://cevr.tuftsmedicalcenter.org/sponsorship). Lauren Sedita, Alexa Klimchak, and Rachel Salazar are employees of Sarepta Therapeutics, Inc and may hold stock/options.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Do, L.A., Sedita, L.E., Klimchak, A.C. et al. Cataloging health state utility estimates for Duchenne muscular dystrophy and related conditions. Health Qual Life Outcomes 22, 72 (2024). https://doi.org/10.1186/s12955-024-02287-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-024-02287-2