Abstract
Background
Trajectories of health-related quality of life (HRQoL) after driving cessation (DC) are thought to decline steeply, but for some, HRQoL may improve after DC. Our objective is to examine trajectories of HRQoL for individuals before and after DC. We hypothesize that for urban drivers, volunteers and those who access alternative transportation participants’ health may remain unchanged or improve.
Methods
This study uses data from the AAA Longitudinal Research on Aging Drivers (LongROAD) study, a prospective cohort of 2,990 older drivers (ages 65–79 at enrollment). The LongROAD study is a five-year multisite study and data collection ended October 31, 2022. Participants were recruited using a convenience sample from the health centers roster. The number of participants approached were 40,806 with 7.3% enrolling in the study. Sixty-one participants stopped driving permanently by year five and had data before and after DC. The PROMIS®-29 Adult Profile was utilized and includes: 1) Depression, 2) Anxiety, 3) Ability to Participate in Social Roles and Activities, 4) Physical Function, 5) Fatigue, 6) Pain Interference, 7) Sleep Disturbance, and 8) Numeric Pain Rating Scale.
Adjusted (age, education and gender) individual growth models with 2989 participants with up to six observations from baseline to year 5 in the models (ranging from n = 15,041 to 15,300) were utilized.
Results
Ability to participate in social roles and activities after DC improved overall. For those who volunteered, social roles and activities declined not supporting our hypothesis. For those who accessed alternative transportation, fatigue had an initial large increase immediately following DC thus not supporting our hypothesis. Urban residents had worse function and more symptoms after DC compared to rural residents (not supporting our hypothesis) except for social roles and activities that declined steeply (supporting our hypothesis).
Conclusions
Educating older adults that utilizing alternative transportation may cause initial fatigue after DC is recommended. Accessing alternative transportation to maintain social roles and activities is paramount for rural older adults after DC especially for older adults who like to volunteer.
Similar content being viewed by others
Introduction
Driving cessation (DC) has historically been associated with a decrease in social, physical and mental health outcomes in older adults, but these declines are mitigated over time [1, 2]. Research is emerging that health-related quality of life (HRQoL) may actually improve after DC due to increased time with family members or increased physical activity from using alternative transportation [3,4,5,6,7]. Individual HRQoL changes after DC may be obscured in aggregated data; individual-level modeling methods are therefore preferred [2, 7,8,9].
The goal is to examine the trajectories of eight domains of HRQoL for individuals before and after DC. Based on current research, we hypothesize that for different subgroups (i.e., urban drivers, volunteers and those that access to alternative transportation) participants’ social and physical health will improve [3,4,5,6,7].
Methods
Participants, design and procedures
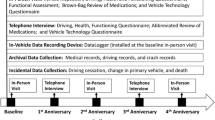
The AAA Longitudinal Research on Aging Drivers (LongROAD) cohort is a multisite prospective cohort of 2,990 older drivers [10]. Participants aged 65–79 years were recruited between July 2015 and March 2017 from: Ann Arbor, MI; Baltimore, MD; Cooperstown, NY; Denver, CO; and San Diego, CA. Key inclusion criteria for the study, include: 1) having a valid driver’s license, 2) staying in their current location for another five years, and 3) driving on average at least one time a week [10]. The LongROAD study is a five year study and data collection was completed October 31, 2022. The baseline visit and Year 2 were conducted in-person and Years 1 and 3 by telephone. Due to the COVID-19 pandemic, 33% of follow-up visits in Year 4 and 35% in Year 5 were conducted in-person with the rest conducted by a telephone interview.
Measures
Personal characteristics
Of the 2990 participants, 42% were in the 65–69 age category at baseline, 86% were non-Hispanic white, 53% were female, 63% were married, 41% had an advanced degree, 13% lived in rural areas (rural–urban commuting area codes: 4 and higher micropolitan/small town/rural), 54% volunteered and 11% accessed transportation options other than driving themselves, including public, on-demand, micro-mobility and friends/family [10].
Exposure
DC was operationalized as those who voluntarily or involuntarily stopped driving permanently, as determined by: 1) questions about driving status at each annual follow-up visit, 2) participants notifying the study team that they stopped driving, and 3) participants’ driving activity stopped based on objective driving data recorded from their vehicle [11]. If there was no activity for at least 30 days, then the study team reached out to the participants to identify their current driving status. Seventy-three participants stopped driving during the follow-up period. One person started driving again and thus was excluded from the analysis for a total of 2989 in the models. Sixty-nine participants who stopped driving were determined by questions about driving status at each annual follow-up visit. Three participants were determined by the other two methods. The year since DC is defined as the interview year minus the year of DC.
Primary outcomes
The outcomes were assessed before and after DC at their annual visits. Patient-Reported Outcomes Measurement Information System® or PROMIS®-29 Adult Profile (found to have construct validity and be reliable across three standard deviations) includes: 1) v1.0 (version 1.0)- Depression-4a (four items), 2) v1.0—Anxiety-4a, 3) v2.0 – Ability to Participate in Social Roles and Activities-4a, 4) Physical Function-4a, 5) v1.0-Fatigue-4a, 6) v1.0-Pain Intererence-4a, 7) v1.0-Sleep Disturbance-4a, and 8) Numeric Rating Scale v1.0 -Pain Intensity 1a [12].
Statistical analyses
A trajectory of each outcome measure was examined with an individual growth model, a type of linear mixed model with repeated measures of 2989 with the observations in the models ranging from 15,041 to 15300 [13]. The main independent variables were (1) year since the baseline (0, 1, …,5), (2) a binary indicator of DC (0, 1), and (3) years since DC (i.e., a segmented regression model) [14]. The DC variable was used to measure change in outcome (i.e., level) immediately after DC. The years since DC variable was used to measure change in outcome trend (i.e., slope) after DC. We estimated adjusted (age, gender and education) trajectories of each outcome based on the individual growth model.
To estimate and compare trajectories by subgroups (accessed transportation, volunteer, and rural–urban areas), we included the subgroup indicator, as well as interaction terms of subgroup indictor with the DC variable and year since DC variable in the model. We also included age, gender and education in the model as covariates to control for bias between different subgroups.
Results
Response and participation rates
The follow-up for years one through five are respectively: 96.5%, 90.8%, 85.2%, 74.4% and 68%. Sixty-one participants, out of the 72 who reported permanent DC, stopped driving after baseline and before year 5 follow-up. There was no record of the outcome if the participant died or withdrew from the study.
Characteristics of participants with driving cessation
Of the 61 participants who stopped driving, 30% were in the 65–69 age category, 80% were non-Hispanic white, 48% were female, 61% were married, 31% had an advanced degree, 15% lived in rural areas, 59% volunteered and 13% had access to transportation. Sixty-seven percent voluntarily stopped driving. The main reasons for stopping driving included: 1) specific medical condition – 32.76%, 2) 2) other reasons (e.g., license was suspended, car not working, suggested to stop driving by eye doctor etc.)– 20.69%, 3) problems with vision -13.79% 4) problems with mobility – 8.62%, 5) financial reasons – 8.62%, 6) loss of confidence in driving – 5.17%, 7) medications that may affect driving – 3.45%, 8) problems with memory – 3.45%, 9) got in a crash – 1.72% and 10) just don’t want to drive anymore – 1.72%.
Trajectories
Depression (β 3.07), anxiety (β 1.26), physical function (β -4.04), fatigue (β 2.27), pain interference (β 2.19) and pain intensity (β 0.54) all worsened immediately after DC, but the slope of decline was no different than during the pre-DC period (Fig. 1 and Table 1). In contrast, the Ability to Participate in Social Roles and Activities declined immediately after DC (β -3.58) but then increased with a steep slope (β 1.41). Sleep disturbance did not change before or after DC and continued to increase at the same rate.
Figure 2 visualizes the trajectories stratified by accessing transportation, volunteer status and rural–urban area after controlling for age, gender, and education. For accessing transportation, the slope declines at the same trend for depression, pain symptoms, sleep disturbance and anxiety; and improves for social roles and activities, particularly for participants with post-DC utilization of transportation. Those accessing transportation had a large immediate increase in fatigue after DC but the slope then continues with the same trend. Those participants who volunteer have fewer symptoms and better function before and after DC except participation in social roles and activities, which improved less for volunteers than for non-volunteers after DC. Similarly, participants with rural residence had better function and fewer symptoms before and after DC except for social roles and activities, which declined steeply compared to their more urban counterparts.
Discussion
The ability to participate in social roles and activities appeared to increase after DC, overall and in those accessing alternative transportation and non-volunteers, which may be due to increased interaction with family and friends [2,3,4,5,6]. Non-volunteers improving relative to volunteers was counterintuitive. This may be due to volunteers not accessing transportation to their volunteer activities which can be an integral part of their social roles and activities. Future studies should look at whether participants maintained their volunteering over time. In contrast, ability to participate dropped steeply for those in rural areas, where DC was considered at a priori to have greater potential impact [15]. Interestingly, social roles and activities declined the most for rural residence which may be due to either the lack of accessing transportation or the lack friends and family living nearby.
Edwards et al. (2009) reported significant declines in health among former drivers, including social and physical health, physical performance and the greatest decline in general health [1]. However, Edwards et al.’s analysis included former drivers at baseline; thus, not all of the participants were followed prospectively through their transition to DC. In this LongROAD study, we were able to address these limitations as well as assess the health outcomes at time since driving cessation to see if the trajectories differ at a further time period since DC [1, 2]. Our measure of DC is precise and current. Heterogeneity in the effects on DC were addressed in only one previous study that used a cluster analysis, but they were unable to address DC that accounted for time [2]. We did not adjust for vision or cognition because the goal of this study was to evaluate the change in HRQoL; adjusting for any health-related variables would have attenuated any change in HRQoL.
Conclusion
Participation in social roles and activities can increase after DC with utilization of alternative forms of transportation. Decreasing social roles and activities after DC are especially steep in rural areas. Efforts should be made to increase utilization of alternative forms of transportation in rural areas including public, on-demand, micro-mobility and friends/family.
Availability of data and materials
Data sharing is restricted due to limitations within the consent forms.
Abbreviations
- DC:
-
Driving cessation
- HRQoL:
-
Health-related quality of life
- LongROAD:
-
Longitudinal Research on Aging Drivers
- MI:
-
Michigan
- MD:
-
Maryland
- NY:
-
New York
- CO:
-
Colorado
- CA:
-
California
- PROMIS®:
-
Patient-Reported Outcomes Measurement Information System®
References
Edwards JD, Lunsman M, Perkins M, Rebok GW, Roth DL. Driving cessation and health trajectories in older adults. J Gerontol A Biol Sci Med Sci. 2009;64(12):1290–5. https://doi.org/10.1093/gerona/glp114. Epub 2009 Aug 12. PMID: 19675177; PMCID: PMC2773808.
Bennetts R, Taylor JE. Health and quality of life outcomes of driving cessation for older people are more complex than we thought. Clin Gerontol. 2022;45(4):821–32. https://doi.org/10.1080/07317115.2021.1978122. Epub 2021 Oct 19. PMID: 34665997.
Siren A, Haustein D. What are the impacts of giving up the driving licence? Ageing Soc. 2015;35(9):1821–38. https://doi.org/10.1017/S0144686X14000610.
Liddle J, Turpin M, Carlson G, McKenna K. The needs and experiences related to driving cessation for older people. Br J Occup Ther. 2008;71(9):379–88. https://doi.org/10.1177/030802260807100905.
Mullen NW, Parker B, Wiersma E, Stinchcombe A, Bédard M. Looking forward and looking back: older adults’ views of the impacts of stopping driving. Occup Ther Health Care. 2017;31(3):188–204. https://doi.org/10.1080/07380577.2017.1337282. (Epub 2017 Jul 20 PMID: 28726531).
Pellerito JM Jr. The effects of driving retirement on elderly men and women living in metropolitan Detroit. Topics Geriatric Rehabil. 2009;25:135–53. https://doi.org/10.1097/TGR.0b013e3181a1038d.
Ferrucci L, Kuchel GA. Heterogeneity of aging: individual risk factors, mechanisms, patient priorities, and outcomes. J Am Geriatr Soc. 2021;69(3):610–2. https://doi.org/10.1111/jgs.17011. Epub 2021 Jan 18. PMID: 33462804; PMCID: PMC9221786.
O’Connor ML, Edwards JD, Waters MP, Hudak EM, Valdés EG. Mediators of the association between driving cessation and mortality among older adults. J Aging Health. 2013;25(8 Suppl):249S-S269. https://doi.org/10.1177/0898264313497796. PMID:24385637;PMCID:PMC3882338.
Pollet TV, Stulp G, Henzi SP, Barrett L. Taking the aggravation out of data aggregation: a conceptual guide to dealing with statistical issues related to the pooling of individual-level observational data. Am J Primatol. 2015;77(7):727–40. https://doi.org/10.1002/ajp.22405. (Epub 2015 Mar 24 PMID: 25810242).
Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health. 2006;83(2):162–75. https://doi.org/10.1007/s11524-005-9016-3. PMID: 16736366; PMCID: PMC2527174.
Li G, Eby DW, Santos R, Mielenz TJ, Molnar LJ, Strogatz D, Betz ME, DiGuiseppi C, Ryan LH, Jones V, Pitts SI, Hill LL, DiMaggio CJ, LeBlanc D, Andrews HF. LongROAD Research Team. Longitudinal Research on Aging Drivers (LongROAD): study design and methods. Inj Epidemiol. 2017;4(1):22. https://doi.org/10.1186/s40621-017-0121-z. Epub 2017 Aug 1. PMID: 28736796; PMCID: PMC5537138.
Craig BM, Reeve BB, Brown PM, Cella D, Hays RD, Lipscomb J, Simon Pickard A, Revicki DA. US validation of health outcomes measured using the PROMIS-29. Value Health. 2014;17(8):846–53. https://doi.org/10.1016/j.jval.2014.09.005.
Chen H, Cohen P. Using individual growth model to analyze the change in quality of life from adolescence to adulthood. Health Qual Life Outcomes. 2006;21(4):10. https://doi.org/10.1186/1477-7525-4-10. PMID:16504035;PMCID:PMC1397823.
Gillings D, Makuc D, Siegel E. Analysis of interrupted time series mortality trends: an example to evaluate regionalized perinatal care. Am J Public Health. 1981;71(1):38–46. https://doi.org/10.2105/ajph.71.1.38. PMID:7258429;PMCID:PMC1619708.
Strogatz D, Mielenz TJ, Johnson AK, Baker IR, Robinson M, Mebust SP, Andrews HF, Betz ME, Eby DW, Johnson RM, Jones VC, Leu CS, Molnar LJ, Rebok GW, Li G. Importance of driving and potential impact of driving cessation for rural and urban older adults. J Rural Health. 2020;36(1):88–93. https://doi.org/10.1111/jrh.12369. (Epub 2019 Apr 25 PMID: 31022317).
Acknowledgements
Additional LongROAD Research Team members also includes Marian E. Betz, Lindsay Ryan, and Robert Santos. We greatly appreciate the contributions of Barbara Lang to overall study coordination and the study coordinators, research assistants, and participants.
Funding
This work is supported by the AAA Foundation for Traffic Safety. This research was supported in part by a Grant 1 R49 CE002096-01 from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, to the Center for Injury Epidemiology and Prevention at Columbia University. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
TJM and HJ conceptualized the study and study design. TJM, CD, DS, HA, VJ, LM, DE, LH and GL contributed to data acquisition. TJM and HJ conducted data interpretation and analysis. TJM and HJ prepared the manuscript. All authors participated in critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures in studies involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mielenz, T.J., Jia, H., DiGuiseppi, C. et al. Impact of driving cessation on health-related quality of life trajectories. Health Qual Life Outcomes 22, 13 (2024). https://doi.org/10.1186/s12955-024-02231-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-024-02231-4