Abstract
Background
Evidence on the association between visceral lipid accumulation and infertility remains limited and controversial. Therefore, the current investigation is the first investigation to unveil this correlation by utilizing novel indicators of visceral lipid accumulation.
Methods
The present study utilized the NHANES 2013–2020 dataset. Researchers utilized multiple logistic regression, smoothed curve fitting, and subgroup analysis to investigate the associations of waist circumference (WC), metabolic score for visceral fat (METS-VF), lipid accumulation product (LAP), visceral adiposity index (VAI) with infertility. Additionally, the eXtreme Gradient Boosting (XGBoost) algorithm model was utilized to evaluate the relative importance of the factors.
Results
After adjusting for potential factors that could influence the results, researchers discovered that all these four indicators of visceral lipid accumulation exhibited strong positive correlations with the probability of infertility. The subgroup analysis demonstrated that the correlations remained consistent in the majority of subgroups (P for interaction > 0.05). The results of XGBoost algorithm model indicate that METS-VF is the most meaningful factor in infertility. The ROC curve research revealed that while METS-VF had the greatest AUC values, there was no variation in the AUC value of different markers of visceral fat accumulation (P > 0.05).
Conclusions
The present investigation discovered that increased WC, METS-VF, LAP, and VAI were associated with a heightened prevalence of infertility.
Similar content being viewed by others
Introduction
Infertility is a medical condition that prevents pregnancy after 12 months of consistent, unprotected sexual intercourse [1]. Infertility, a prevalent issue in reproductive health on a global scale, impacts a substantial number of individuals, estimated at 186 million worldwide [2]. In the United States, a noteworthy proportion of women within the childbearing age bracket, roughly 12.7%, actively pursue infertility therapy annually [3]. Secondary infertility caused by reproductive system infections is the most common kind of female infertility [1]. Zhang et al. conducted a study that further validated pelvic inflammatory illness as the primary factor contributing to secondary infertility among women in local population [4]. A separate study including 71 American women has corroborated that genitourinary Chlamydia trachomatis is a significant factor contributing to female infertility [5]. Moreover, many medical disorders, including endometriosis and thyroid dysfunction, have been identified as potential factors contributing to infertility [6, 7]. There is evidence suggesting that lifestyle and environmental factors also exert an influence on the reproductive health of women via neuroendocrine pathways [8]. These identified risk factors potentially facilitate the production of an excessive amount of free radicals within the organism, hence initiating an oxidative state that poses a threat to the reproductive health of the organism [9]. Currently, making changes to one’s lifestyle is the most fundamental and economical approach to treating infertility. The Dietary Inflammatory Index (DII) measures the degree of dietary inflammation within the body. Vahid et al. surveyed 135 Iranian women and discovered that women with elevated DII scores have an increased likelihood of miscarriage in comparison with women adhering to an anti-inflammatory diet [10]. An empirical study with a sample of 577 women demonstrated that enhancing fertility can be achieved by diminishing the consumption of treats and drinks with a high-calorie content, alongside augmenting exercise [11]. Other primary methods used to treat infertility also include ovarian stimulation, in vitro fertilization, psychotherapy, and stem cell therapy [3, 12, 13]. However, given the intricate nature and exorbitant expenses associated with treatments of infertility, treating infertility remains to be a significant challenge in the realm of human reproductive health. Therefore, it is imperative to carry out additional research on the risk factors of infertility to offer novel insights and approaches for the prevention and management of infertility.
Obesity has evolved into an epidemic worldwide health disorder, impacting a huge number of individuals globally. According to dependable data, the prevailing prevalence of overweight or obesity is approximated to affect in excess of 1.1 billion individuals and approximately 10% of children worldwide [14]. Additionally, it should be noted that obesity approximately contributes to a range of 0.7–2.8% of a nation’s overall healthcare costs [15]. Numerous research has provided substantial evidence indicating a positive correlation between obesity and the heightened susceptibility to cardiovascular disorders, asthma, and type 2 diabetes [16,17,18]. During the past couple of decades, the influence of being overweight on female fertility has also received much scrutiny. A Danish investigation revealed that women with extreme obesity are far more likely to experience adverse pregnancy outcomes, such as gestational diabetes and pre-eclampsia. Furthermore, their infants exhibited significantly higher rates of obesity [19]. In addition, Fedorcsák et al. substantiated that women who are obese possess a reduced number of oocytes and are more susceptible to a miscarriage in a study including 383 women [20]. Consequently, more and more women acknowledge that maintaining a healthy weight can successfully promote women’s reproductive health. A prospective study conducted by Clark et al. demonstrated that overweight women with infertility who engaged in physical exercise to lose weight saw a restoration of ovulation and a decrease in miscarriage rates [21]. Another study conducted by Christinajoice et al. including 45 female participants demonstrated that bariatric surgery significantly improved the reproductive health of subjects [22]. Obesity raises the likelihood of infertility in women and has negative effects on assisted reproductive technologies [23, 24]. Nevertheless, most previous research on the correlation between obesity and infertility has predominantly relied on body mass index (BMI) as the primary indicator of obesity. It’s controversial because research has demonstrated that individuals with a high amount of visceral fat are at a greater risk of experiencing heart-related problems, regardless of whether their BMI is considered normal or excessive [25]. Therefore, relying solely on BMI for evaluating obesity is not reasonable, and taking into account central obesity offers a broader comprehension of the health concerns associated with obesity. While waist circumference (WC) is widely employed to measure central adiposity, it is important to consider that the accuracy of WC may be influenced by the subject’s height and BMI [26, 27]. Therefore, to address the limitations of WC, the researchers suggest developing novel indicators to accurately measure visceral lipid accumulation. The metabolic score for visceral fat (METS-VF), lipid accumulation product (LAP), and visceral adipose index (VAI) are reliable indicators used to measure the accumulation of visceral lipids. Numerous prior research has established a robust correlation between these indicators and various disorders [28,29,30]. Considering the easy accessibility of data for calculating these indicators, it is anticipated that they will assume a significant role in the assessment of a greater number of diseases in the future. No research has investigated the significance of indicators of visceral lipid accumulation in relation to female infertility. This study is the inaugural investigation to reveal the associations between these indicators and infertility. By doing so, it could offer a more effective approach for the future management and therapy for infertility in both affected individuals and those who may be susceptible. Additionally, it will provide novel perspectives on the impact of lipids on infertility. The researchers hypothesized that all four indicators of visceral lipid accumulation examined in this study would exhibit substantial correlations with infertility.
Methods
Data sources for the study
The National Health and Nutrition Examination Survey (NHANES) 2013–2020 is the resource of the data for the current analysis. The National Center for Health Statistics (NCHS) Ethics Review Board granted authorization for the human subjects in NHANES, and every single participant provided their informed permission. Demographic data, laboratory data, examination data, and questionnaire data were all gathered as part of this survey. These data were then further analyzed and used to research risk factors of various disorders. This study employed a sophisticated multi-stage probabilistic methodology, which ensured that the sample used was representativity and accurate.
Study population
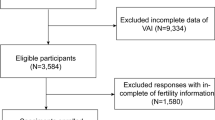
35,706 participants from the NHANES 2013–2020 were initially added. To choose the ones who best matched the current study, researchers further evaluated these people. First of all, subjects who were 45 years of age or older (n = 6,076) was ineligible as well as male subjects (n = 17,616). Participants who lacked indicators of visceral lipid accumulation data (n = 2,550), infertility data (n = 7,609), and covariate data (n = 554) were also eliminated. In the end, 1,301 qualified female individuals took part in the study (Fig. 1).
Definition of exposure variables
Researchers considered METS-VF, WC, VAI, and LAP as exposure variables. Their calculation is determined by the following formula [31]. At the Mobile Examination Center (MEC), professional health technicians measure individuals’ BMI, WC, and height carefully. High-density lipoprotein cholesterol (HDL-C) and triglycerides (TG) data were obtained using the Cobas 6000 Chemistry Analyzer. The Roche/Hitachi Cobas C Chemistry Analyzer - C311 yielded data on fasting blood glucose (FBG).
Gender was presumed to be 0 because there were no male participants in this study.
Definition of infertility
The ending variable was infertility. Through a query in the Computer Assisted Personal Interview (CAPI) system at the Mobile Examination Center (MEC), information about infertility was collected. When asked, “Have you been trying to get pregnant for one year? (RHQ074)”, individuals were categorized as having infertility if they responded positively; otherwise, they were categorized as not having infertility.
Covariates
Researchers evaluated these variables as covariates and accounted for them during data analysis since they could potentially affect how indicators of visceral lipid accumulation and infertility are related. Covariates of the investigation included race, educational attainment, matrimonial status, family income to poverty ratio, total cholesterol, smoking, alcohol usage, physical activity, menstruation status, pelvic inflammatory disease therapy, and use of hormonal medicines. Smokers are defined as having smoked at least 100 cigarettes. Drinkers are defined as having had 4 to 5 drinks or more per day in the past 12 months. Subjects were defined as having physical exercise if they had exercised at a moderate or vigorous intensity during a typical week. You are able to locate comprehensive measurement methods for each of these variables at the NHANES Official Website.
Methods and tools used for statistical analysis of data
Researchers used R version 3.4.3 and Empower software to assist with the present statistical investigation. Given the non-normal distribution of the continuous variables in the study, they were reported as the median (quartile 1-quartile 3). Categorical variables were represented using percentages. Additionally, the chi-square test was employed for categorical variables, while the Mann-Whitney U-test was utilized for continuous data. Three distinct models were established in the multiple logistic regression analysis to assess the correlation between the independent variables and the dependent variable. The first model did not adjust for any variable. The second model adjusted for age and race. And the third model adjusted for all covariates considered in the study, including age, race, education, marital status, family income to poverty ratio, total cholesterol, smoking, alcohol use, physical activity, menstrual status, treatment of pelvic inflammatory disease, and use of hormonal medications. Furthermore, smoothed curve fitting and threshold effect analysis were employed to explore potential non-linear relationships of exposure variables with outcome variables. In addition, researchers analyzed subgroups according to marital status, alcohol use, smoking, physical exercise, and regularity of menstruation. The researchers employed a novel approach by utilizing Python software to implement the eXtreme Gradient Boosting (XGBoost) algorithm, known for its effectiveness in machine learning models. This method was utilized to ascertain the relative significance of the chosen variables. Grid search and cross-validation techniques were utilized to optimize the XGBoost algorithm model and enhance its performance. In the XGBoost model, the adjusted hyperparameters included n_estimators, max_depth, and learning_rate. Specifically, the values for these hyperparameters were: n_estimators: 100, max_depth: 3, and learning_rate: 0.1. Researchers compared the association of different indicators of visceral lipid accumulation with visceral obesity and infertility by means of subject work characteristics (ROC) curve applying logistic regression and calculating the area under the curve (AUC). The Delong test, implemented in Medcalc statistical software, was used to compare the differences in AUC values. In the investigation, a significance level of P < 0.05 was used to determine statistically significant differences.
Results
Details of essential characteristics of participants
Table 1 provides a concise summary of the essential characteristics of the individuals involved in the study. The current study was conducted with 1,301 eligible female participants, whose median age was 33 years. Among the participants, 1,137 individuals were categorized as not having infertility, while 164 individuals met the criteria for infertility. Infertile patients exhibited distinct characteristics compared to those without infertility. They had higher median age, a greater proportion of individuals who used alcohol, and higher median values for BMI, WC, LAP, VAI, and METS-VF.
Correlations between indicators of visceral lipid accumulation and infertility
In the findings devoid of confounding adjustments, a positive correlation was discerned between WC, METS-VF, LAP, VAI, and the prevalence of infertility (Table 2). After adjusting for all other confounders, the prevalence of infertility demonstrated an escalation of 2% aligned with each unit rise in WC (Odds Ratio [OR] = 1.02, 95% Confidence Interval [CI]: 1.01–1.03). Drawing a parallel, the prevalence of infertility augmented by 82% (OR = 1.82, 95% CI: 1.39–2.40) concomitant with each unit climb in METS-VF, by 1% (OR = 1.01, 95% CI: 1.00-1.01) recurrent with each unit ascension in LAP, and by 12% (OR = 1.12, 95% CI: 1.03–1.23) with each unit increase in VAI. Furthermore, the calculating formula involved converting the centimeter (CM) units to decimeters (DM) in order to amplify the effect size values of WC and LAP with infertility. Once again, multiple logistic regression analysis was employed to examine the relationship of WC and LAP with infertility. The prevalence of infertility increased by 18% for each whole-number rise in WC (OR = 1.18, 95% CI: 1.09–1.29) and by 6% for each whole-number increase in LAP (OR = 1.06, 95% CI: 1.03–1.10) (Supplementary 1). The association between these visceral obesity proxies and infertility was further explored after converting WC, METS-VF, LAP, and VAI from continuous to categorical variables (tertiles). Within the model that has been fully adjusted, the prevalence of experiencing infertility was 202% higher in those with the highest tertiles of WC in comparison to subjects with the lowest tertiles of WC (OR = 2.02, 95% CI:1.28–3.18). The prevalence of infertility in the highest tertiles of METS-VF was 248% of that in the lowest tertiles of METS-VF (OR = 2.34, 95% CI:1.46–3.77). The prevalence of infertility in the highest tertiles of LAP was 234% of the risk in the lowest tertiles of LAP (OR = 1.82, 95% CI:1.39–2.40). The prevalence of infertility in the highest tertiles of VAI was 210% of the lowest tertiles of VAI (OR = 2.10, 95% CI:1.31–3.37). All P-trends were statistically significant.
Figure 2 offers a visual representation of the results derived from applying a procedure to fit a smoothed curve, while the outcomes of the threshold effect analysis are displayed in Table 3. After adjusting for all covariates, researchers noticed linear correlations of WC and METS-VF with infertility. However, the correlations of LAP and VAI with infertility were not linear. The additional computations revealed that the breakpoints of the correlation between LAP and infertility and the correlation between VAI and infertility were determined to be 28.8 and 1.25, respectively. Statistically significant associations of LAP and VAI with infertility were observed on the left side of the breakpoints. Whereas, on the right side of the breakpoint, researchers observed no statistically significant correlations.
Association between different evaluation indicators of central obesity and infertility. (A) Association between METS-VF and infertility; (B) Association between WC and infertility; (C) Association between LAP and infertility; (D) Association between VAI and infertility. The solid red line represents the smooth curve fit between variables. Blue bands represent the 95% of confidence interval from the fit. WC, waist circumference; METS-VF, metabolism score for visceral fat; LAP, lipid accumulation product; VAI, visceral adiposity index
Details of subgroup analysis
With the aim of determining the stability of the correlations of WC, METS-VF, LAP, and VAI with infertility in the population, additional subgroup analyses were conducted. Subgroup analyses were stratified by marital status, smoking habits, level of physical activity, and regular menstruation. The outcomes of these subgroup analyses, adjusting for all confounders, are displayed in Table 4. The results of the current investigation suggested that the correlations of WC, METS-VF, LAP, and VAI with infertility remained consistent throughout various populations (P for interaction > 0.05).
Assessing the relative importance of variables in the study through XGBoost algorithm modeling
In order to determine the relative significance of particular variables for infertility, researchers modeled the XGBoost algorithm using machine learning in the present study (Fig. 3). The current findings of machine learning indicated that marital status, alcohol use, education level, METS-VF, and age were the five most important factors. Furthermore, METS-VF was the most significant indicator of visceral lipid accumulation. The relative significance of METS-VF and WC is greater in comparison to the conventional BMI indicator. While the significance of LAP and VAI is lower compared to BMI.
Correlation of different indicators of visceral lipid accumulation with central obesity and infertility
Table 5; Fig. 4 display the outcomes of the ROC curve analysis. In terms of the association with infertility, the AUC values of METS-VF, WC, LAP, and VAI were 0.6090 (95% CI: 0.5651,0.6530), 0.6013 (95% CI: 0.5550,0.6476), 0.5904 (95% CI: 0.5462,0.6346), and 0.5744 (95% CI: 0.5310,0.6179), respectively. The AUC of METS-VF had the highest value, but there was no statistically significant difference in the AUC values of the four indicators of visceral lipid accumulation (P > 0.05). Furthermore, there was no statistically significant disparity between the AUC values of the four indicators of visceral lipid accumulation and the AUC values of BMI (P > 0.05). Visceral obesity in women was classified as having a WC equal to or greater than 88 cm [32]. Regarding visceral obesity, the AUC values of METS-VF, LAP, and VAI were 0.9808 (95% CI: 0.9755,0.9861), 0.9097 (95% CI: 0.9097,0.9384), and 0.7690 (95% CI: 0.7428,0.7951), respectively. These values indicate that METS-VF is associated with central obesity to a greater extent than VAI and LAP (P < 0.0001).
Sensitivity analysis
The original data had 554 participants excluded from the study due to missing corresponding covariates, which may reduced statistical test efficacy and bias associated with missing values. Therefore, the researchers employed multiple interpolations (MI), which were based on the R MI program, to estimate the impact of missing values. The R MI program was performed based on 5 repetitions and chained equations. The researchers performed multiple logistic regression analysis using the five sets of data obtained from MI. Next, the ORs, 95% CIs, and P-values of the multivariate logistic regression analyses were combined according to Rubin’s rule. To avoid the issue of excessively tiny impact value, the researchers opted to convert the units of WC utilized in the WC and LAP measurements to DM. As observed in Supplementary 2, the effect sizes of the interpolated data do not differ significantly from the original data, suggesting that missing data do not significantly affect the results.
Discussion
This study examined the correlation between four indicators of visceral lipid accumulation and infertility in a sample of 1,301 participants. The results of the current investigation demonstrate a strong and positive correlation between all four indicators of lipid accumulation with infertility. Furthermore, these positive connections were consistent throughout different population settings. The four indicators showed comparable association with infertility, whereas METS-VF is associated with central obesity to a greater extent than VAI and LAP.
This study is the first to examine the correlations between indicators of visceral lipid accumulation and infertility using the NHANES database. Although there is an increasing number of researchers investigating the potential connection between visceral obesity and infertility, the research in this field is still restricted, and the existing findings are subject to controversy. There is compelling data indicating that an increase in WC is linked to the occurrence of negative outcomes during pregnancy, such as gestational diabetes, preeclampsia, and macrosomia [33]. A study conducted by Gao et al. examined 976 Chinese mother-child couples in a birth cohort study. The study revealed that having central obesity before conception can result in various negative pregnancy outcomes associated with obesity [34]. An independent study including 261 Turkish women revealed that having an abnormally wide WC both prior to and throughout pregnancy is a significant warning sign for the development of gestational diabetes [35]. A study based on 1,679 black women found that patients with higher WC and waist-to-hip ratio (WHR) had lower fertility [36]. Furthermore, the relationship of visceral adiposity with polycystic ovarian syndrome (PCOS), a prevalent factor contributing to female infertility, caught the attention of researchers. A case-control study conducted in Indonesia demonstrated that increased WC, hip circumference, and WHR considerably elevate the likelihood of developing PCOS in women [37]. Interestingly, Loy et al. obtained contrasting outcomes from a multiracial prospective cohort. No significant relationship between fertility and alternative indicators of central adiposity, including WHR, WHtR, and a body shape index (ABSI), was found [38]. The current investigation’s findings add new evidence to the correlation between indicators of central lipid accumulation and infertility. Specifically, after adjusting for all covariates, the prevalence of infertility in the highest tertiles of WC, METS-VF, LAP, and VAI was 202%, 248%, 234%, and 210% of that in the lowest tertiles, relatively. And the findings of the current investigation support the idea that central obesity is a dangerous element for infertility in women of reproductive age, although the underlying mechanisms remain unclear.
The global prevalence of obesity has reached alarming levels, affecting about 20% of women in America within the reproductive age group [39]. Multiple research investigations have demonstrated a correlation between obesity and disruptions in the hypothalamic-pituitary-gonadal (HPG) axis, resulting in impaired ovulation and anomalies in the menstrual cycle among females [23, 40]. This can be related to the correlation between visceral obesity and the development of leptin resistance. By influencing the activity of kisspeptin neurons, leptin governs the organism’s ability to reproduce by indirectly affecting the activity of the gonadotropin-releasing hormone (GnRH) [41]. Obesity clearly interferes with the ability of leptin to fulfill its usual physiological role. Additionally, women who are obese exhibit elevated levels of circulating free fatty acids. These fatty acids have the potential to accumulate outside of adipocytes, increasing reactive oxygen species (ROS). The presence of ROS can induce stress in both mitochondria and endoplasmic reticulum, ultimately leading to apoptosis. This lipotoxic mechanism is responsible for the destruction of non-adipocytes and may have detrimental effects on the processes of meiosis and cytoplasmic maturation of oocytes. These effects can subsequently hinder the fertilization process and compromise the developmental competence of pre-implantation embryos [42]. Furthermore, an abundance of free fatty acids can cause low-grade inflammation to persist in a variety of bodily tissues, including reproductive tissues. The abundance of mRNAs specific to oocytes is regulated by obesity-dependent changes in proinflammatory signaling, which leads to the disruption of normal embryonic development [42, 43]. Complex mechanisms mediate the relationship between visceral obesity and infertility, although such mechanisms remain incompletely elucidated, thus necessitating further research on the role of visceral obesity in women’s reproductive health to provide guidance for the prevention of female reproductive disorders.
It is worth mentioning that many previous research studies investigating the connection of overweight with infertility have mostly employed BMI as a tool to evaluate overweight. However, obesity can be categorized into two main types: generalized obesity and central obesity [44]. Furthermore, it is important to recognize that whereas BMI primarily assesses the overall degree of obesity in individuals [45], it might not sufficiently evaluate differences in body fat and muscle composition [46]. The research carried out by Li et al. provided confirmation that WC had a negative influence on the likelihood of a successful live delivery using assisted reproductive technologies, regardless of BMI [47]. Tang et al. examined 3,542 women in a metabolically healthy population and found no correlation between BMI and infertility [48]. Additionally, previous investigations have demonstrated that an elevated BMI is correlated with a better prognosis in advanced heart failure, and it is uncertain whether there is an obesity paradox in infertility, given the correlation between infertility in women and a higher likelihood of getting severe cardiovascular disease. Moreover, a few scholars have suggested that the existence of the obesity paradox can be attributed to the limitations of BMI [49,50,51]. Therefore, it is theoretically reasonable to assert that employing indications of visceral obesity is a more effective, precise, and cautious approach to evaluating female reproductive well-being. Magnetic resonance imaging (MRI) and computed tomography (CT) are universally acknowledged as the most reliable methods for evaluating visceral fat. However, their utilization as preferred metrics for assessing visceral fat is limited due to their high cost and the specialized nature of the procedures involved [52]. Therefore, employing novel indicators of lipid accumulation to evaluate infertility would be a more ideal approach. The indicators that are included are METS-VF, LAP, and VAI. It was discovered that there was a robust positive correlation between all four metrics and infertility. The ROC analysis confirmed that all four metrics could be utilized to identify infertility. However, the XGBoost modeling revealed that, in comparison to the conventional obesity metric BMI, only the METS-VF and WC exhibited a more pronounced ability to identify infertility. This can be related to the fact that VAI and LAP were not initially intended to evaluate visceral fat [53], which may explain why VAI and LAP are not as effective as BMI in identifying certain disorders associated with obesity. Moreover, the current investigation discovered that METS-VF exhibited a greater significance in relation to female infertility and proved to be a more effective measure for evaluating visceral obesity. This superiority extends to risk factors for infertility. A study conducted in China showed that METS-VF can be a dependable identifying indicator of type 2 diabetes in the Chinese population, due to other indicators of obesity, and is not affected by gender, age, or BMI [54]. An independent cohort study carried out in China revealed a direct association of METS-VF with the prevalence of hypertension. Furthermore, out of the six indicators analyzed, METS-VF demonstrated the highest AUC value, indicating that it could be a reliable and effective predictor of the risk of hypertension [55]. Furthermore, METS-VF was found to be strongly associated with the population’s risk of hyperuricemia by Liu XZ et al. [56]. The reason why the METS-VF has a superior predictive capacity is not well understood. Researchers propose that the METS-VF includes the age of the individual, which is a significant risk factor for numerous diseases that are not considered by other evaluation indicators. Furthermore, METS-VF includes lipid biomarkers that not only indicate the extent of fat buildup but also provide insights into the functionality of lipid cells. Moreover, insulin resistance, a constituent of the METS-VF, is commonly seen in conjunction with obesity and abnormal tolerance for glucose, both of which are risk factors together known as metabolic syndrome [57, 58]. Metabolic syndrome is not only linked to female fertility but also to the onset of various other diseases [59]. While the other indicators, such as BMI, WC, and VAI only provide a rough estimate of visceral adipose tissue content based on the distribution of body fat and do not precise depictions of the impact of fat on metabolism, the METS-VF effectively captures the influence of visceral adipose tissue on metabolism [60]. In summary, the current work has demonstrated that METS-VF is a reliable indicator of both female infertility and visceral obesity. Therefore, it is imperative to determine the METS-VF values of women experiencing infertility in order to enhance the efficacy of their treatment and the overall management of their condition.
Study strengths and limitations
When compared to earlier research, this one has a number of remarkable strengths. Initially, researchers used a nationally representative sample of NHANES participants as the study population, adjusting the confounding factors and demonstrating for the first time the correlation between novel indicators of visceral lipid accumulation and infertility. Second, it was novel to employ machine learning with XGBoost algorithmic modeling to ascertain the relative significance of particular variables. The current research presents fresh proof of the correlation between visceral fat and infertility as well as novel suggestions for the management and treatment of infertility going forward. Although this study has yielded significant findings, it is imperative to recognize the inherent constraints that are linked to it. The current investigation was limited by its cross-sectional methodology, which prevented the development of a causal association between indicators of visceral lipid accumulation and infertility. Consequently, it is imperative to conduct a more extensive prospective investigation in order to corroborate the findings and confirm the results of the current investigation. Furthermore, an examination of infertility was conducted utilizing a questionnaire, potentially introducing inaccuracies in the findings if participants had imperfect recollection of the material. Moreover, because of the limited data on women’s reproductive health provided by NHANES, we were unable to distinguish whether infertility was primary or secondary. Nor can we rule out the role of male factors in female infertility. What’s more, it cannot be ignored that this investigation was conducted exclusively on the U.S. population, whether its conclusion can be applied to populations in other regions remains to be further investigated.
Conclusion
Elevated levels of WC, METS-VF, LAP, and VAI are connected with a greater possibility of female infertility. Given the ease and cost-efficiency of calculating these four indicators, it is advisable for physicians in clinical practice to conduct lipid testing and measure relevant physical indicators for women who may be experiencing infertility or have risk factors for infertility. This will allow for the calculation of the four indicators of visceral lipid accumulation and provide a comprehensive evaluation of the patient’s reproductive health. These findings present a valuable tool for early identification of infertility, particularly in the field of care of gynecology and obstetrics. Healthcare professionals can develop tailored dietary plans, exercise routines, and personalized treatment strategies for women experiencing infertility based on assessments of these four indicators of visceral lipid accumulation. The objective is to provide timely interventions for infertility, thereby improving the efficacy of infertility treatment and care. However, it’s worth noting that this study was conducted on a population of women in the United States. Therefore, further research is necessary to ascertain the generalizability of the findings to female populations in other regions.
Data availability
The original data were retrieved from https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. The data used in the article has been submitted as an additional file.
References
Vander Borght M, Wyns C. Fertility and infertility: definition and epidemiology. Clin Biochem. 2018;62:2–10.
Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21:411–26.
Carson SA, Kallen AN. Diagnosis and management of infertility: a review. JAMA. 2021;326:65–76.
Zhang F, Feng Q, Yang L, Liu X, Su L, Wang C, Yao H, Sun D, Feng Y. Analysis of the etiologies of female infertility in Yunnan minority areas. BMC Womens Health. 2021;21:88.
Wilkowska-Trojniel M, Zdrodowska-Stefanow B, Ostaszewska-Puchalska I, Zbucka M, Wołczyński S, Grygoruk C, Kuczyński W, Zdrodowski M. Chlamydia trachomatis urogenital infection in women with infertility. Adv Med Sci. 2009;54:82–5.
Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J Assist Reprod Genet. 2010;27:441–7.
Mazzilli R, Medenica S, Di Tommaso AM, Fabozzi G, Zamponi V, Cimadomo D, Rienzi L, Ubaldi FM, Watanabe M, Faggiano A, et al. The role of thyroid function in female and male infertility: a narrative review. J Endocrinol Invest. 2023;46:15–26.
Bala R, Singh V, Rajender S, Singh K. Environment, Lifestyle, and female infertility. Reprod Sci. 2021;28:617–38.
Agarwal A, Aponte-Mellado A, Premkumar BJ, Shaman A, Gupta S. The effects of oxidative stress on female reproduction: a review. Reprod Biol Endocrinol. 2012;10:49.
Vahid F, Shivappa N, Hekmatdoost A, Hebert JR, Davoodi SH, Sadeghi M. Association between maternal Dietary Inflammatory Index (DII) and abortion in Iranian women and validation of DII with serum concentration of inflammatory factors: case-control study. Appl Physiol Nutr Metab. 2017;42:511–6.
van Elten TM, Karsten MDA, Geelen A, van Oers AM, van Poppel MNM, Groen H, Gemke R, Mol BW, Mutsaerts MAQ, Roseboom TJ, Hoek A. Effects of a preconception lifestyle intervention in obese infertile women on diet and physical activity; a secondary analysis of a randomized controlled trial. PLoS ONE. 2018;13:e0206888.
Malina A, Błaszkiewicz A, Owczarz U. Psychosocial aspects of infertility and its treatment. Ginekol Pol. 2016;87:527–31.
Saha S, Roy P, Corbitt C, Kakar SS. Application of Stem Cell Therapy for Infertility. Cells. 2021; 10.
Haslam DW, James WP, Obesity. Lancet. 2005;366:1197–209.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–41.
Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141:1169–79.
Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Nohr EA, Timpson NJ, Andersen CS, Davey Smith G, Olsen J, Sørensen TI. Severe obesity in young women and reproductive health: the Danish National Birth Cohort. PLoS ONE. 2009;4:e8444.
Fedorcsák P, Storeng R, Dale PO, Tanbo T, Abyholm T. Obesity is a risk factor for early pregnancy loss after IVF or ICSI. Acta Obstet Gynecol Scand. 2000;79:43–8.
Clark AM, Thornley B, Tomlinson L, Galletley C, Norman RJ. Weight loss in obese infertile women results in improvement in reproductive outcome for all forms of fertility treatment. Hum Reprod. 1998;13:1502–5.
Christinajoice S, Misra S, Bhattacharya S, Kumar SS, Nandhini BD, Palanivelu C, Raj PP. Impact of Bariatric Surgery on Female Reproductive Health and maternal outcomes. Obes Surg. 2020;30:383–90.
Glenn T, Harris AL, Lindheim SR. Impact of obesity on male and female reproductive outcomes. Curr Opin Obstet Gynecol. 2019;31:201–6.
Rich-Edwards JW, Spiegelman D, Garland M, Hertzmark E, Hunter DJ, Colditz GA, Willett WC, Wand H, Manson JE. Physical activity, body mass index, and ovulatory disorder infertility. Epidemiology. 2002;13:184–90.
Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and Cardiovascular diseases. Circ Res. 2020;126:1477–500.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–69.
Freedman DS, Kit BK, Ford ES. Are the recent secular increases in Waist circumference among children and adolescents independent of changes in BMI? PLoS ONE. 2015;10:e0141056.
Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, Thorand B, Meisinger C. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep. 2019;9:9693.
Bello-Chavolla OY, Antonio-Villa NE, Vargas-Vázquez A, Viveros-Ruiz TL, Almeda-Valdes P, Gomez-Velasco D, Mehta R, Elias-López D, Cruz-Bautista I, Roldán-Valadez E, et al. Metabolic score for visceral Fat (METS-VF), a novel estimator of intra-abdominal fat content and cardio-metabolic health. Clin Nutr. 2020;39:1613–21.
Deng CY, Ke XP, Guo XG. Dietary calcium, phosphorus, and potassium intake associated with erectile dysfunction in the National Health and Nutrition Examination Survey (NHANES) 2001 to 2004. PLoS ONE. 2024;19:e0297129.
Deng CY, Ke XP, Guo XG. Investigating a novel surrogate indicator of adipose accumulation in relation to erectile dysfunction. Lipids Health Dis. 2024;23:139.
Kim D, Hou W, Wang F, Arcan C. Factors affecting obesity and Waist Circumference among US adults. Prev Chronic Dis. 2019;16:E02.
Wendland EM, Duncan BB, Mengue SS, Nucci LB, Schmidt MI. Waist circumference in the prediction of obesity-related adverse pregnancy outcomes. Cad Saude Publica. 2007;23:391–8.
Gao X, Yan Y, Xiang S, Zeng G, Liu S, Sha T, He Q, Li H, Tan S, Chen C, et al. The mutual effect of pre-pregnancy body mass index, waist circumference and gestational weight gain on obesity-related adverse pregnancy outcomes: a birth cohort study. PLoS ONE. 2017;12:e0177418.
Takmaz T, Yalvaç ES, Özcan P, Çoban U, Gökmen Karasu AF, Ünsal M. The predictive value of weight gain and waist circumference for gestational diabetes mellitus. Turk J Obstet Gynecol. 2019;16:199–204.
Wise LA, Palmer JR, Rosenberg L. Body size and time-to-pregnancy in black women. Hum Reprod. 2013;28:2856–64.
Mawaddatina T, Budihastuti UR, Rahayu D. Waist circumference, hip circumference, arm span, and waist-to-hip ratio high risk of polycystic ovarian syndrome. Scott Med J. 2021;66:186–90.
Loy SL, Cheung YB, Soh SE, Ng S, Tint MT, Aris IM, Bernard JY, Chong YS, Godfrey KM, Shek LP, et al. Female adiposity and time-to-pregnancy: a multiethnic prospective cohort. Hum Reprod. 2018;33:2141–9.
Broughton DE, Moley KH. Obesity and female infertility: potential mediators of obesity’s impact. Fertil Steril. 2017;107:840–7.
Imterat M, Agarwal A, Esteves SC, Meyer J, Harlev A. Impact of body Mass Index on female fertility and ART outcomes. Panminerva Med. 2019;61:58–67.
Barber TM, Kyrou I, Kaltsas G, Grossman AB, Randeva HS, Weickert MO. Mechanisms of Central Hypogonadism. Int J Mol Sci. 2021; 22.
Snider AP, Wood JR. Obesity induces ovarian inflammation and reduces oocyte quality. Reproduction. 2019;158:R79–90.
Davis JS. Connecting female infertility to obesity, inflammation, and Maternal Gut Dysbiosis. Endocrinology. 2016;157:1725–7.
Carmienke S, Freitag MH, Pischon T, Schlattmann P, Fankhaenel T, Goebel H, Gensichen J. General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis. Eur J Clin Nutr. 2013;67:573–85.
Moltrer M, Pala L, Cosentino C, Mannucci E, Rotella CM, Cresci B. Body mass index (BMI), waist circumference (WC), waist-to-height ratio (WHtR) e waist body mass index (wBMI): which is better? Endocrine. 2022;76:578–83.
Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes (Lond). 2008;32(Suppl 3):S56–59.
Li MC, Mínguez-Alarcón L, Arvizu M, Chiu YH, Ford JB, Williams PL, Attaman J, Hauser R, Chavarro JE. Waist circumference in relation to outcomes of infertility treatment with assisted reproductive technologies. Am J Obstet Gynecol. 2019; 220:578.e571-578.e513.
Tang J, Xu Y, Wang Z, Ji X, Qiu Q, Mai Z, Huang J, Ouyang N, Chen H. Association between metabolic healthy obesity and female infertility: the national health and nutrition examination survey, 2013–2020. BMC Public Health. 2023;23:1524.
Bosdou JK, Anagnostis P, Lainas GT, Kolibianakis EM. Female infertility and Cardiovascular Risk - A hype or an underestimated reality? Curr Pharm Des. 2020;26:5551–5.
Kim JE, Choi J, Kim M, Won CW. Assessment of existing anthropometric indices for screening sarcopenic obesity in older adults. Br J Nutr. 2023;129:875–87.
Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity Paradox in Heart failure. Prog Cardiovasc Dis. 2018;61:151–6.
Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, Lopez-Jimenez F, Rao G, St-Onge MP, Towfighi A, Poirier P. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124:1996–2019.
Wander PL, Hayashi T, Sato KK, Uehara S, Hikita Y, Leonetti DL, Kahn SE, Fujimoto WY, Boyko EJ. Design and validation of a novel estimator of visceral adipose tissue area and comparison to existing adiposity surrogates. J Diabetes Complications. 2018;32:1062–7.
Feng Y, Yang X, Li Y, Wu Y, Han M, Qie R, Huang S, Wu X, Zhang Y, Zhang J, et al. Metabolic score for visceral Fat: a novel predictor for the risk of type 2 diabetes mellitus. Br J Nutr. 2022;128:1029–36.
Feng Y, Yang X, Li Y, Wu Y, Han M, Qie R, Huang S, Wu X, Zhang Y, Liu D, et al. Metabolic score for visceral Fat: a reliable indicator of visceral obesity for predicting risk for hypertension. Nutrition. 2022;93:111443.
Liu XZ, Chen DS, Xu X, Li HH, Liu LY, Zhou L, Fan J. Longitudinal associations between metabolic score for visceral fat and hyperuricemia in non-obese adults. Nutr Metab Cardiovasc Dis. 2020;30:1751–7.
Ahmed B, Sultana R, Greene MW. Adipose tissue and insulin resistance in obese. Biomed Pharmacother. 2021;137:111315.
Xia W, Cai Y, Zhang S, Wu S. Association between different insulin resistance surrogates and infertility in reproductive-aged females. BMC Public Health. 2023;23:1985.
Cardozo E, Pavone ME, Hirshfeld-Cytron JE. Metabolic syndrome and oocyte quality. Trends Endocrinol Metab. 2011;22:103–9.
Kuang M, Qiu J, Li D, Hu C, Zhang S, Sheng G, Zou Y. The newly proposed Metabolic Score for Visceral Fat is a reliable tool for identifying non-alcoholic fatty liver disease, requiring attention to age-specific effects in both sexes. Front Endocrinol (Lausanne). 2023;14:1281524.
Acknowledgements
We would like to thank the support of Student Innovation Ability Project plan of Guangzhou Medical University. We thank Jianwen Chen (Sun Yat-sen University, Guangzhou, China) for providing statistical methodology consultation.
Funding
This work was supported by grants from Guangzhou Science and technology planning project (2023A03J0377 to YF and 2023A03J0043 to CL).
Author information
Authors and Affiliations
Contributions
Chenyuan Deng consulted and organized materials analysis data and wrote the manuscripts. Xinpeng Ke and Liangcai Lin proofread citations. Chaohui Li and Yong Fan conceptualized this project and supervised the overall work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The NHANES program was approved by the National Center for Health Statistics (NCHS) Ethics Review Board and all participants signed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Deng, C., Ke, X., Lin, L. et al. Association between indicators of visceral lipid accumulation and infertility: a cross-sectional study based on U.S. women. Lipids Health Dis 23, 186 (2024). https://doi.org/10.1186/s12944-024-02178-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02178-x