Abstract
Background
In recent years, New Delhi metallo-beta-lactamases 1 (bla NDM-1) has been reported with increasing frequency and become prevalent. The present study was undertaken to investigate the epidemiological dissemination of the bla NDM-1 gene in Enterobacter cloacae isolates at a teaching hospital in Yunnan, China.
Methods
Antimicrobial susceptibility testing was performed using VITEK 2 system and E test gradient strips. The presence of integrons and insertion sequence common region 1 were examined by PCR and sequencing. Clonal relatedness was assessed by pulsed-field gel electrophoresis (PFGE) and multilocus sequence typing. Conjugation experiments and Southern blot hybridization were performed to determine the transferability of plasmids.
Results
Ten E. cloacae isolates and their Escherichia coli transconjugants were exhibited similar resistant patterns to carbapenems, cephalosporins and penicillins. 8 (80%) of E. cloacae isolates carried class 1 integron and 1 (12.5%) carried class 2 integron. Integron variable regions harbored the genes which encoded resistance to aminoglycosides (aadA1, aadA2, aadA5, aadB, aac(6′)-Ib-cr), sulfamethoxazole/trimethoprim (dfrA17, dfrA12, dfrA15) and Streptozotocin (sat2). Six E. cloacae isolates belonged to ST74 and exhibited highly similar PFGE patterns. Each isolate shared an identical plasmid with ~33.3 kb size that carried the bla NDM-1 gene, except T3 strain, of which the bla NDM-1 gene was located on a ~50 kb plasmid.
Conclusions
Our findings suggested that plasmid was able to contribute to the dissemination of bla NDM-1. Hence, more attention should be devoted to monitor the dissemination of the bla NDM-1 gene due to its horizontal transfer via plasmid. In addition, nosocomial surveillance system should actively monitor the potential endemic clone of ST74 to prevent their further spread.
Similar content being viewed by others
Background
Enterobacter cloacae is an important nosocomial pathogen, which can cause various infections including urinary tract, skin and soft tissue, respiratory tract, surgical site, biliary tract, sepsis, intravenous catheters, central nervous system and outbreaks at neonatal units [1, 2]. New Delhi metallo-beta-lactamases 1 (bla NDM-1) are Ambler class B Metallo-β-lactamases(MBLs)with carbapenemase activity that confers resistance to all β-lactams except aztreonam, was first identified in a carbapenem-resistant Klebsiella pneumoniae strain recovered from a Swedish patient who was hospitalized in India in 2008 [3], and mainly detected in carbapenem-resistant Acinetobacter spp. in mainland China. However, NDM-1-mediated carbapenem resistance in E. cloacae has been rarely reported in China.
The widespread dissemination of bla NDM-1 is mainly due to plasmids, integrons, insertion sequence common region (ISCR) and clonal outbreaks [4]. Plasmids are extrachromosomal DNA molecules capable of autonomous replication, and can confer resistance to the major antimicrobials [5]. Integrons are bacterial genetic elements able to capture and express genes contained within mobile gene cassettes. Typically, integrons are composed of two conserved regions, a 3′ conserved segment (3′CS) and a 5′ conserved segment (5′CS), as well as an internal variable region containing gene cassettes that encode antimicrobial resistance determinants [6]. ISCR elements can transpose adjacent DNA sequences by a process called rolling-circle replication, now it is recognized as powerful antibiotic resistance gene capture systems and playing a major role in spread of antibiotic resistance genes. However, whether these mobile elements mediate the dissemination of bla NDM-1 gene is still an unsolved mystery in the region. Therefore, the aim of this study is to explore the epidemiological dissemination of the bla NDM-1 gene in E. cloacae isolates at a teaching hospital in Yunnan, China.
Methods
Bacterial strains
In total, ten NDM-1-producing E. cloacae isolates were collected from hospitalized patients in the First Affiliated Hospital of Kunming Medical University between June 2012 and January 2016. All isolates were identified by VITEK2 automated identification system (bioMerieux, France). Carbapenemase activity was assessed by the modified Hodge test, MBL production was examined by imipenem-ethylenediaminetetraacetic acid (EDTA) disk method and the bla NDM-1 gene was determined by PCR in the early stage of the study. All patients were of Yunnan descent and none had a recent history of travelling epidemic area (Table 1).
Antimicrobial susceptibility testing
Antimicrobial susceptibilities for the NDM-1-producing isolates and transconjugants were initially tested using the VITEK2 system. MICs of imipenem, meropenem and ertapenem were re-evaluated using E test gradient strips (bioMerieux, France) on Mueller–Hinton agar plates and the results interpreted according to the CLSI guidelines [7]. Escherichia coli ATCC 25922 was used as quality control strain.
PCR amplification and sequencing
Isolates were grown overnight in M–H Agar plates at 37 °C and genomic DNA was extracted using boiling method. Class 1, 2, 3 integrons and ISCR1 were, respectively, amplified using the primers intI1/intI1, intI2/intI2, intI3/intI3, hep58/hep59, hep74/hep51, orf513F/orf513R and orf513F/sul1R (Table 2). The amplified PCR products were analyzed by electrophoresis in 2% agarose gels and finally visualized in gel documentation system. PCR amplification products were sequenced. The resulting DNA sequences were analyzed by the BLAST program (http://www.ncbi.nlm.nih.gov/BLAST/).
Pulsed-field gel electrophoresis (PFGE) and multilocus sequence typing (MLST)
Bacterial genomic DNA was prepared in agarose plugs and digested with the restriction enzymes XbaI (Promega, USA). The DNA fragments were separated by use of a CHEF Mappar XA PFGE system (Bio-Rad, USA), with running time of 22 h and pulse times ranging from 5 to 40 s. The running buffer was 0.5 × Tris-boric acid-EDTA (TBE). Salmonella ser. Braenderup H9812 was used as a standard for comparison. PFGE patterns were compared visually following previously described criteria [12]. Multilocus sequence typing (MLST) was performed on representative isolates. Internal fragments of the seven housekeeping genes were amplified using the primers given at the Institute Pasteur MLST Databases web site (http://pubmlst.org/ecloacae/). The PCR products were sequenced. Sequence types (STs) were assigned using online database tools.
Conjugation experiments and Plasmid analysis
The transfer of carbapenem resistance was tested using a conjugation test, E. coli 600 (rifampicin-resistant) was used as the recipient strain, NDM-1-producing E. cloacae clinical isolates were used as the donor strains. Donor and recipient cells from M–H broth cultures were mixed in a ratio of 2:1 and transconjugant clones were screened on M–H agar plates containing rifampicin (256 mg/L) and Imipenem (1 mg/L). Conjugation events occurred at 37 °C. The presence of the bla NDM-1 gene in transconjugants was determined by PCR and sequencing. Genomic DNA was digested with S1 nuclease (Promega, USA). The linearized plasmids and partially digested genomic DNA were separated through the CHEF-Mapper XA PFGE system with a switch time from 2.16 to 63.8 s for 18 h at 6 V/cm at 14 °C. Linear plasmids generated by S1-PFGE were transferred to nvlon membrane (Millipore, USA) and hybridized with a digoxigenin-labeled probe specific to bla NMD-1. Probe labeling and signal detection were carried out with DIG high primer DNA labeling and detection starter kit according to the manufacturer’s instructions (Roche Applied Sciences, Germany).
Results
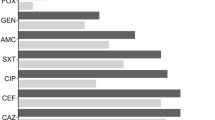
Antimicrobial susceptibility testing
The antibiotic susceptibility results showed that all the NDM-1-producing E. cloacae isolates exhibited resistance to carbapenems, cephalosporins and penicillins. Only one isolates remained susceptible to aztreonam, which was not hydrolysed by metallo-carbapenemases, thus suggesting the presence of additional β-lactamases in the remaining isolates. Ten isolates exhibited different level resistance to tetracycline, amikacin, ciprofloxacin and tigecycline, seven isolates were resistance to tetracycline, one to amikacin, nine to ciprofloxacin and one to tigecycline. These results are summarized in Table 3.
Detection of integrons and ISCR1
Class 1 integrase gene was detected in 80% (8/10), while the variable region of class 1 integron was detected in 70% (7/10) NDM-1-producing E. cloacae isolates. Among them, six different gene cassette arrays were found, which included: dfrA12+aadA2, dfrA15+dfrA17, aadA2+aadA5+dfrA17, dfrA15+aadB+aadA2, dfrA15 and dfrA15+aac (6′)-Ib-cr. Those genes encoded resistance to aminoglycosides and sulfamethoxazole/trimethoprim. 10% (1/10) strains possessed class 2 integron, and the variable region of class 2 integron harbored sat2+aadA1 genes, which mediated antibiotic resistance to streptothricin and streptomycin. None of the isolates harbored class 3 integron. 50% (5/10) isolates carried ISCR1 elements. However, in the five ISCR1 positive isolates, the cassette arrays could not be detected.
PFGE and MLST typing
According to Tenover’s criteria [12], Six E. cloacae isolates, of which four obtained from transplantation center, one from general practice and one from emergency intensive care unit, belonged to ST74 and shared the same PFGE fingerprint pattern (Fig. 1), suggesting they were clonally related, the remaining strains were characterized by unique genotypes. MLST of representative isolates assigned the E. cloacae to four sequence type (ST), ST74, ST182, ST754 and ST175, respectively.
Plasmid analysis
Conjugation experiments revealed that plasmids harboring bla NDM-1 were transformed into E. coli 600. All transconjugants conferred resistance to carbapenems, cephalosporins and penicillins while all of them remained susceptible to ciprofloxacin and amikacin (Table 1). Isolates harbored three to five plasmids according to S1-PFGE electrophoresis. Southern hybridization analysis with a bla NDM-1-specific probe revealed that bla NDM-1 was located on a ~33.3 kb plasmid in nine isolates and on a ~50 kb plasmid in one isolates (Fig. 2).
Results of S1 nuclease PFGE and Southern blot hybridization. Lane M PFGE marker, Salmonella ser. Braenderup H9812; lanes 1–7 Strains (T1–T7) digested with S1 nuclease; lanes 8–14 hybridized plasmids of strains (T7–T1) with the bla NDM-1 probe; lanes 15–17 strains (T8–T10) digested with S1 nuclease; lanes 18–20 hybridized plasmids of strains (T8–T10) with the bla NDM-1 probe
Discussion
The bla NDM-1 was first identified in a clinical isolate of K. pneumoniae in New Delhi, India, and suddenly got disseminated around the world. The bla NDM-1-carrying bacteria conferred resistance to all most β-lactam antibiotics. Thus, treatment of infections with NDM-producing bacteria was a major challenge, leaving few options for clinical treatment beside tigecycline or colistin. The bla NDM-1 gene have been identified in a variety of gram-negative bacilli, including Acinetobacter spp. [13], Enterobacteriaceae [14] and Pseudomonas aeruginosa [15]. Lack of uncontaminated potable water and abuse of over-the-counter antibiotic administration offered the ideal setting for the development of a latent endemic situation, and international “medical tourism” played an important role in the spread of bla NDM-1 gene [16]. Yunnan Kunming is a famous tourist city in the world, and large numbers of domestic and foreign tourists come here every year, thus “medical tourism” may play an important role in the spread of bla NDM-1 among carbapenem-resistant bacteria in this region.
In China, plasmid-carrying blaNDM-1 have been identified in Enterobacteriaceae isolates in several regions including Beijing, Shanghai, Hong Kong, Shandong Henan and Yunnan province, the size of plasmids harboring bla NDM-1 were vary from ~50 to 360 kb [17, 18]. Our research shows that bla NDM-1 gene was mainly located on a plasmid with ~33.3 kb size, were different from previously reported in China before. The bla NDM-1 gene was not detected in integrons and ISCR1 mobile elements. Integrons only carried these genes encoding resistance to aminoglycosides [aadA1, aadA2, aadA5, aadB, aac(6′)-Ib-cr], sulfamethoxazole/trimethoprim (dfrA17, dfrA12, dfrA15) and Streptozotocin (sat2). Those results suggested that plasmid was the most important mobile element that mediated the dissemination of bla NDM-1 and integrons were the basis for the formation of multiple drug-resistant bacteria in the region. In addition, it was worth noting that there had been some evidences which demonstrated that integrons and ISCR mobile elements were located on plasmids [4], thus, the resistance gene through the plasmids spreading was not a single element, but by 1 + 1 or 1 + 2 mode. This mode of dissemination should arouse high concern of the relevant departments.
Clonal spread was an important factor involved in the prevalence of NDM-1-producing Enterobacteriaceae. Outbreak of NDM-1-producing K. pneumoniae ST105 and ST147 have been reported in Yunnan [17] and Xi’an [19], and NDM-1-producing E. cloacae ST120 have been reported in Henan [18], China, respectively. Our study showed that 5 clusters for 10 strains, 1 cluster from 6 closely related isolates was found to exhibit similarities which is more than 90%. The result suggested that 6 NDM-1-producing E. cloacae isolates were clonally related. However, there was no significant epidemiological relatedness among them. Hence, we could not trace their origin. MLST analysis revealed four ST types including ST74, ST754, ST175 and ST182, among them, ST74 was the major type in NDM-1-producing E. cloacae isolates, which was different from previous types reported before such as ST66, ST78, ST108, ST114 and ST120 [18]. ST74 has been identified among non-susceptible to ertapenem of E. cloacae isolates in North-Eastern France, and was associated with OXA-48-producing E. cloacae isolates in Spain [20, 21]. The present study is the first to report on an outbreak of NDM-1-producing E. cloacae ST74.
Infection control measures were strengthened to prevent the further transmission of bla NDM-1. They included hand hygiene, contact isolation, active screening, environmental surface disinfection, standard aseptic manipulation techniques, among them, hand hygiene was the most effective and economical strategy for reducing cross infection [16].
To conclude, our study demonstrated that plasmids were the most important elements that mediate horizontal transfer of the bla NDM-1 gene. Furthermore, we identified a potential endemic clone of ST74. The emergence of NDM-1-producing E. cloacae ST74 isolates is worrying, nosocomial surveillance system should pay more attention to prevent their further spread.
Abbreviations
- NDM-1:
-
New Delhi metallo-beta-lactamase 1
- ISCR1:
-
insertion sequence common region 1
- PCR:
-
polymerase chain reaction
- PFGE:
-
pulse field gel electrophoresis
- MLST:
-
multilocus sequence typing
- MBLs:
-
metallo-β-lactamases
- 5CS & 3CS:
-
5′ & 3′-conserved segments
- CLSI:
-
Clinical and Laboratory Standards Institute
- M–H:
-
Mueller–Hinton
- MIC:
-
minimum inhibitory concentration
References
Miyoshi-Akiyama T, Hayakawa K, Ohmagari N, Shimojima M, Kirikae T. Multilocus sequence typing (MLST) for characterization of Enterobacter cloacae. PLoS ONE. 2013;8(6):e66358. doi:10.1371/journal.pone.0066358.
Yang FC, Yan JJ, Hung KH, Wu JJ. Characterization of ertapenem-resistant Enterobacter cloacae in a Taiwanese University Hospital. J Clin Microbiol. 2012;50(2):223–6. doi:10.1128/JCM.01263-11.
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR. Characterization of a new metallo-beta-lactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrobial Agents Chemother. 2009;53(12):5046–54.
Zhao WH, Hu ZQ. Acquired metallo-β-lactamases and their genetic association with class 1 integrons and ISCR elements in Gram-negative bacteria. Futur Microbiol. 2015;10(5):873–87. doi:10.2217/fmb.15.18.
Carattoli A. Resistance plasmid families in Enterobacteriaceae. Antimicrob Agents Chemother. 2009;53(6):2227–38. doi:10.1128/AAC.01707-08.
Lima AM, de Melo ME, Alves LC, Brayner FA, Lopes AC. Investigation of class 1 integrons in Klebsiella pneumoniae clinical and microbiota isolates belonging to different phylogenetic groups in Recife, State of Pernambuco. Rev Soc Bras Med Trop. 2014;47(2):165–9.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: twenty-fourth informational supplement update document M100-S24. Wayne: CLSI; 2014.
Shibata N, Doi Y, Yamane K, Yagi T, Kurokawa H, Shibayama K, Kato H, Kai K, Arakawa Y. PCR typing of genetic determinants for metallo-beta-lactamases and integrases carried by gram-negative bacteria isolated in Japan, with focus on the class 3 integron. J Clin Microbiol. 2003;41(12):5407–13.
White PA, McIver CJ, Deng Y, Rawlinson WD. Characterisation of two new gene cassettes, aadA5 and dfrA17. FEMS Microbiol Lett. 2000;182(2):265–9.
White PA, McIver CJ, Rawlinson WD. Integrons and gene cassettes in the Enterobacteriaceae. Antimicrob Agents Chemother. 2001;45(9):2658–61.
Quiroga MP, Andres P, Petroni A, Soler Bistué AJ, Guerriero L, Vargas LJ, Zorreguieta A, Tokumoto M, Quiroga C, Tolmasky ME, Galas M, Centrón D. Complex class 1 integrons with diverse variable regions, including aac(6′)-Ib-cr, and a novel allele, qnrB10, associated with ISCR1 in clinical enterobacterial isolates from Argentina. Antimicrob Agents Chemother. 2007;51(12):4466–70.
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995;33(9):2233–9.
Huang TW, Lauderdale TL, Liao TL, Hsu MC, Chang FY, Chang SC, Khong WX, Ng OT, Chen YT, Kuo SC, Chen TL, Mu JJ, Tsai SF. Effective transfer of a 47 kb NDM-1-positive plasmid among Acinetobacter species. J Antimicrob Chemother. 2015;70(10):2734–8. doi:10.1093/jac/dkv191.
Qu H, Wang X, Ni Y, Liu J, Tan R, Huang J, Li L, Sun J. NDM-1-producing Enterobacteriaceae in a teaching hospital in Shanghai, China: IncX3-type plasmids may contribute to the dissemination of blaNDM-1. Int J Infect Dis. 2015;34:8–13. doi:10.1016/j.ijid.2015.02.020.
Zafer MM, Amin M, El Mahallawy H, Ashour MS, Al Agamy M. First report of NDM-1-producing Pseudomonas aeruginosa in Egypt. Int J Infect Dis. 2014;29:80–1. doi:10.1016/j.ijid.2014.07.008.
Voulgari E, Gartzonika C, Vrioni G, Politi L, Priavali E, Levidiotou-Stefanou S, Tsakris A. The Balkan region: NDM-1-producing Klebsiella pneumoniae ST11 clonal strain causing outbreaks in Greece. J Antimicrob Chemother. 2014;69(8):2091–7. doi:10.1093/jac/dku105.
Zheng R, Zhang Q, Guo Y, Feng Y, Liu L, Zhang A, Zhao Y, Yang X, Xia X. Outbreak of plasmid-mediated NDM-1-producing Klebsiella pneumoniae ST105 among neonatal patients in Yunnan. China. Ann Clin Microbiol Antimicrob. 2016;15:10. doi:10.1186/s12941-016-0124-6.
Liu C, Qin S, Xu H, Xu L, Zhao D, Liu X, Lang S, Feng X, Liu HM. New Delhi metallo-β-lactamase 1(NDM-1), the dominant carbapenemase detected in carbapenem-resistant Enterobacter cloacae from Henan province, China. PLoS ONE. 2015;10(8):e0135044. doi:10.1371/journal.Pone.
Wang X, Xu X, Li Z, Chen H, Wang Q, Yang P, Zhao C, Ni M, Wang H. An outbreak of a nosocomial NDM-1-producing Klebsiella pneumoniae ST147 at a teaching hospital in mainland China. Microb Drug Resist. 2014;20(2):144–9. doi:10.1089/mdr.2013.0100.
Fernández J, Montero I, Martínez Ó, Fleites A, Poirel L, Nordmann P, Rodicio MR. Dissemination of multiresistant Enterobacter cloacae isolates producing OXA-48 and CTX-M-15 in a Spanish hospital. Int J Antimicrob Agents. 2015;46(4):469–74. doi:10.1016/j.ijantimicag.2015.07.003.
Guillard T, Cholley P, Limelette A, Hocquet D, Matton L, Guyeux C, Lebreil AL, Bajolet O, Brasme L, Madoux J, Vernet-Garnier V, Barbe C, Bertrand X, de Champs On Behalf of CarbaFrEst Group C. Fluoroquinolone Resistance Mechanisms and population structure of Enterobacter cloacae non-susceptible to Ertapenem in North-Eastern France. Front Microbiol. 2015; 6:1186. doi:10.3389/fmicb.2015.01186.
Authors’ contributions
YD designed the study; ND drafted the first version of this manuscript; SL and MN collected the isolates and clinical informations; ND performed the PFGE; ND and JM preformed the antimicrobial susceptibility test and conjugation experiment; RC, JY, MZ, SL, MN and ND carried out the molecular biology experiments. YD and YD participated in manuscript correction. All authors read and approved the final manuscript.
Acknowledgements
Escherchia coli 600 and Salmonella ser. Braenderup H9812 was a kind gift from Prof. Yunsong Yu, the First Affiliated Hospital of Zhejiang University. This study was supported by grants from the Health and Family Planning Commission of Yunnan Province (Grant No. 2016NS030).
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data and materials are available.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Du, N., Liu, S., Niu, M. et al. Transmission and characterization of bla NDM-1 in Enterobacter cloacae at a teaching hospital in Yunnan, China. Ann Clin Microbiol Antimicrob 16, 58 (2017). https://doi.org/10.1186/s12941-017-0232-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-017-0232-y