Abstract
Background
Congenital heart disease (CHD) is the most prevalent birth defect in recent decades. The aim of this research was to examine the association between maternal housing renovation exposure during the periconceptional period and isolated congenital heart disease (CHD) in their offspring.
Methods
A multi-hospitals case-control study was conducted from six tertiary A hospitals in Xi’an, Shaanxi, Northwest China based on questionnaires and interviews to address this question. The cases included fetuses or newborns diagnosed with CHD. Controls consisted of healthy newborns without birth defects. In total, 587 cases and 1180 controls were enrolled in this study. The association between maternal periconceptional housing renovation exposure and isolated CHD for offspring was assessed by estimating odds ratios (OR) with multivariate logistic regression models.
Results
After adjusting for potential confounding variables, it was found that maternal exposure to home improvement projects was associated with a higher probability of isolated CHD in offspring (adjusted OR: 1.77, 95% CI: 1.34, 2.33). Additionally, the risk of the ventricular septal defect (VSD) and patent ductus arteriosus (PDA) for CHD types was significantly associated with maternal exposure to housing renovations (VSD: adjusted OR = 1.56, 95% CI: 1.01, 2.41; PDA: adjusted OR = 2.50, 95% CI: 1.41, 4.45).
Conclusions
Our study suggests that maternal exposure to housing renovation during the periconceptional period was associated with an increased risk of isolated CHD in offspring. Consequently, it would be beneficial to avoid living in a renovated home from 12 months before pregnancy through the first trimester to lower isolated CHD in infants.
Similar content being viewed by others
Introduction
Congenital heart disease (CHD) refers to the malformation caused by abnormal cardiovascular development in the developing fetus. CHD is the most prevalent birth defect, leading to miscarriage, stillbirth, and infant deaths [1]. Worldwide, the incidence of CHD is about 4–10 per 1,000 live births and is increasing [2]. According to China’s birth defect surveillance data, the occurrence of CHD reached 8–10% in live births, and 150,000 newborns are born each year with CHD [3]. However, because the epidemiology studies and data on CHD from low-and-middle-income countries are far more limited, the CHD prevalence is frequently underestimated in these countries [4]. Therefore, CHD has become a significant public health problem worldwide and in China. Although some studies suggested that CHD may be developed during the first trimester of pregnancy due to genetic factors, environmental factors, or gene-environment interaction [5, 6], the pathogenesis of CHD is still unknown [7].
More Chinese have relocated into modern homes after renovation in order to improve their living standards as a result of the social economy’s rapid development and urbanization. Unfortunately, with time, decorative materials emit volatile and organic pollutants that have an adverse effect on human health. Several studies have revealed that maternal exposure to organic solvents (toluene and xylene) potentially increased the risk of abnormal fetal development [8,9,10,11]. Additionally, there is evidence in experimental model systems that prenatal exposure to environmental pollutantspolycyclic (trichloroethylene or aromatic hydrocarbons) causes developmental abnormalities in the hearts of avian embryos and embryos in animals [9, 12,13,14]. However, there is a paucity of data to demonstrate the association between maternal housing renovation exposure during the periconceptional period and isolated CHD risk [15]. In order to investigate the relationship between maternal housing remodeling exposure during the periconceptional period and the risk of isolated CHD in their offspring, a hospital-based case-control research was carried out in Xi’an, China.
Methods
Study design and participants
We conducted a case-control study in six tertiary A hospitals from January 2014 to December 2016 in Xi’an, Shaanxi province, China. At the obstetrics departments, neonates and mothers were chosen as cases and controls after childbirth. Inclusion criteria and exclusion criteria for the cases were as follows: (1) Singleton pregnancy; (2) End of pregnancy was between January 2014 and December 2016; (3) Mothers whose fetuses or children were diagnosed with isolated CHDs from 28 weeks of pregnancy to 28 days after birth, and the pregnancy outcomes with live birth, stillbirth or termination after fetal anomaly were included in case group; (4) All children diagnosed with a patent ductus arteriosus (PDA) born at term; (5) The case group excluded any fetus or child with birth defects other than CHD.
Two controls were selected after one case was recruited. Inclusion criteria and exclusion criteria for the controls were as follows: (1) Controls came from the same year as the case; (2) Controls came from the same hospital as the case; (3) In the control group, live births with a singleton pregnancy were included; 4)The control group excluded mothers whose fetus or child with birth defects. In the case group, 603 participants were surveyed with a no-reply rate of 2.65% (16 cases). In the control group, 1216 participants were surveyed with a no reply rate of 2.96% (36 cases). Finally, the analysis included 587 cases and 1180 controls who had completed the questionnaires.
Data collection
A standardized questionnaire was designed by the Department of Epidemiology and Health Statistics, School of Public Health, Xi’an Jiaotong University. The questionnaire included sociodemographic characteristics, life behaviors, nutrient supplements, family history of birth defects, and environmental factors during the periconceptional period. Mostly through hospital medical records, additional details, such as pregnancy history, disease and medication usage throughout pregnancy, and delivery status, were acquired. Furthermore, all participants were interviewed by face-to-face during their stay in the delivery hospital. And the interviewers were uniformly trained staff from the Department of Epidemiology and Health Statistics, Xi’an Jiaotong University.
We established a team of experts on CHD diagnosis, and the expert team comprised several senior medical technicians from the congenital heart surgery, ultrasound, obstetrics, and gynecology departments of the Northwest Women’s and Children’s Hospital and the First Affiliated Hospital of Xi’an Jiaotong University. The diagnoses of CHD were based on the ICD-10 by the expert team.
The definitions of housing renovation
This study collected housing renovation exposure during the periconceptional period from self-reporting by the mothers in question. Housing renovation exposure was defined as the usage of laminated board, plywood, ceramic tile, marble, oil-based paint, latex or acrylic coating, wallpapers, or carpets during house or work renovations that occurred from one year before to pregnancy through the first trimester of pregnancy.
Covariates
Potential confounders correlated with CHD such as demographic characteristics, life behaviors and nutrient supplements were also collected for the participants. These variables included maternal age, maternal body mass index (BMI), education (primary school and below, junior middle school, high middle school, above high middle school), ethnicity (Han, other), residence (rural, urban), family wealth index (low, medium, high), parity (0, 1, ≥ 2), abortion history (yes, no), family history of birth defects (yes, no), active or passive smoke (yes, no), drinking (yes, no), folic acid supplement (yes, no), fever (yes, no), taking medicine (yes, no), gestational diabetes mellitus (GDM) (yes, no), TORCH infections (yes, no), industrial exposure (yes, no).
The early pregnancy period was defined as the first trimester of pregnancy (up to 12 weeks gestation). The 12 months before conception through the first trimester of pregnancy were referred to as the periconceptional period. Active smoke was defined as ≥ 1 cigarette per week for three consecutive months during the periconceptional period. Passive smoke was defined as ≥ 15 min of smoke inhalation per day for one month during early pregnancy. Drinking refers to drinking alcoholic products (beer, red wine, or white wine) at least one time during early pregnancy. The folic acid supplement was defined as the regular use of folic acid (≥ 400 µg folic acid per day) from 3 months before pregnancy through the first trimester of pregnancy for more than one consecutive month. Fever was defined as febrile episodes (> 38 °C) at least once during early pregnancy. Taking medicine was defined as taking any drugs such as antibiotics or hormones during early pregnancy. GDM was defined as fasting plasma glucose (FPG) ≥ 5.1 mmol/L, or one h plasma glucose ≥ 10.0 mmol/L or two h plasma glucose ≥ 8.5 mmol/L in a 75 g oral glucose tolerance test (OGTT) at 24–28 weeks of gestation. TORCH infections were defined as toxoplasmosis, rubella, cytomegalovirus, and herpes simplex infections. Living within a 10-kilometer radius of mines, paper mills, cement plants, power plants, pesticide factories, and fertilizer factories during the periconceptional period was considered to be industrial exposure.
Statistical analysis
The participants’ baseline characteristics are summarized using counts and proportions for categorical variables. The chi-squared test or Fisher’s exact test was performed to compare categorical variables. The family wealth index was created from a database of household income, assets, and facilities using the principle component analysis approach. This index was categorized into tertials (low, medium, high) that indicated the poorest, middle-class, and wealthiest households. The univariate and multivariate logistic regression models were used to assess the effect of housing renovation on isolated CHD and the main subtype of CHD (ventricular septal defect (VSD), atrial septal defect (ASD), PDA, atrioventricular septal defect (AVSD), and tetralogy of Fallot (TOF)). Model 2 adjusted baseline demographic characteristics (maternal age, BMI, education, ethnicity, residence, family wealth index). Model 3 adjusted all baseline covariates (maternal age, BMI, education, ethnicity, residence, family wealth index, parity, abortion history, family history of birth defects, active or passive smoke, drinking, folic acid supplement, fever, taking medicine, GDM, TORCH infections, and industries exposure).
A sensitivity analysis was conducted using two approaches to assess the robustness of our findings. To examine the potential heterogeneity of a housing renovation effect on isolated CHD, we estimated the effects of housing renovation in subgroups of different maternal characteristics. Additionally, propensity scores matching (1:1) was used for controlling confounding factors, and further assessing the effect of housing renovation on isolated CHD.
All statistical analysis in this study was completed through SAS9.4. A two-tailed P-value below 0.05 was considered statistically significant.
Results
Participant characteristics
A total of 587 mothers with isolated CHD offspring (case group) and 1180 mothers with normal offspring (control group) were analyzed in the study. The characteristics of participants were compared between the case group and control group (Table 1). Compared to the control group, the case group was more likely to have to live in rural areas, had higher BMI, parity, family history of birth defects, active or passive smoking, drinking, taking medicine, TORCH indections, and industries exposure during the periconceptional period. Finally, the case group was more likely to have a lower age, education level and family wealth index, less Han ethnicity, and folic acid supplementation.
Housing renovation and isolated CHD
As mentioned in Table 2, the case group had a greater probability of being exposed to housing renovations than the control group (25.72% vs. 19.07%). After adjusting for baseline demographic characteristics, exposure to housing renovation was associated with an increased risk for isolated CHD in offspring (adjusted OR = 1.60, 95% CI: 1.23, 2.07). After adjusting for all covariates, the risk of developing isolated CHD was 1.77 (95% CI: 1.34, 2.33).
The association between housing renovation and the substyle of isolated CHD was further analyzed (Table 2). After adjusting for all covariates, housing renovation exposure was associated with an increased risk for VSD and PDA in offspring (VSD: adjusted OR = 1.56, 95% CI: 1.01, 2.41; PDA: adjusted OR = 2.50, 95% CI: 1.41, 4.45). However, there was no significant influence on the other CHD types, such as ASD (adjusted OR = 1.28, 95% CI: 0.67, 2.44), AVSD (adjusted OR = 1.36, 95% CI: 0.65, 2.86), and TOF (adjusted OR = 1.45, 95% CI: 0.65, 3.21).
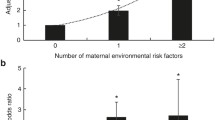
Sensitivity analyses
In addition, the relationship between isolated CHD and exposure to housing renovations was investigated in various demographic subgroups. Housing renovation exposure was associated with a higher risk of isolated CHD in all subgroups, and this association was statistically significant for women aged < 30 years and ≥ 30 years, above high middle school education level, rural or urban residence, medium or high family wealth index, first birth, abortion history or none abortion. Housing renovation exposure was not significantly interacted with any of the covariates for isolated CHD (Table 3).
Additionally, propensity scores for housing renovation exposure were calculated for each participant using multivariable logistic regression, which was used to match 423 (72.06% of 587) cases with 423 controls. After matching, the case group and the control group were similar with regards to all of the baseline covariates except education level (Supplementary Table 1). After propensity scores matching, exposure to housing renovation was associated with an increased risk for isolated CHD in offspring (OR = 1.65, 95% CI: 1.21, 2.26) (Supplementary Table 2).
Discussion
Based on a case-control study, we explored the association between periconceptional housing renovation exposure and isolated CHD risk in Xi’an, China. It was found that periconceptional maternal exposure to housing renovation was associated with a greater risk of isolated CHD in offspring. In addition, maternal housing renovation exposure was associated with increased risk for VSD and PDA in subtypes for isolated CHD.
Housing renovation operations are becoming more frequent and an increasing range of renovation materials are being created, thanks to China’s economy and urbanization. Housing decoration materials commonly contain laminated board, plywood, ceramic tile, marbles, oil-based paint, latex or acrylic coating, wallpapers, and carpets, which include various kinds of environmentally hazardous materials that have been reported. For example, formaldehyde and volatile organic compounds (VOCs) (benzene, toluene, xylene, and styrene) can be found in plywood, heavy metals, organic solvents, and VOCs are emitted from dyes, and paints [16, 17]. As a result, many environmentally hazardous materials may be released into the room air after housing renovations, for example, Coombs et al. reported that formaldehyde concentrations were significantly higher in post-renovated than in pre-renovated homes (0.03 vs. 0.01 ppm) [18]. Moreover, low-quality decoration materials may release higher environmentally hazardous materials into the room air [19].
Early pregnancy is a critical period in fetal heart development and the environment at conception, and early pregnancy can impact the developing embryo [20, 21]. Our study found that mothers exposed to housing renovation during the periconceptional period were associated with an increased risk of isolated CHD in offspring. Liu Z et al. conducted a small-size case-control study (346 cases and 408 controls) and found that maternal exposure to housing renovation may have an increased risk of CHD (OR = 1.89, 95%CI: 1.29, 2.77) [1]. Our study had a larger sample size, and the results are in agreement with those of the previous study. Nevertheless, Motoki N et al. discovered that maternal exposure to housing renovation during pregnancy was not substantially associated with an increased risk of CHD (OR = 1.08, 95%CI: 0.72, 1.61). Their research was based on the Japan Environment and Children’s Study, which included 67,503 singleton live births [22]. In an above cohort study, the period of housing renovation exposure was defined as full-term pregnancy, including the first, second, and third trimesters of pregnancy. In our study, the period of housing renovation exposure was defined as from 1 year before pregnancy through the first trimester of pregnancy. Because a crucial period in fetal heart development is the first trimester of pregnancy, the different periods of housing renovation may lead to different effects on CHD in offspring, which may cause different results.
The association between housing renovation exposure and CHD may be attributed to organic pollutants and other volatile contaminants being released from decoration materials. According to a prior study, women whose homes had been decorated in the previous three years had higher urinary benzophenone concentrations than women whose homes had not been decorated [23]. Several studies have revealed that maternal occupational exposure to organic solvents, such as acetone, toluene, xylene, and Stoddard solvent or Chlorinated solvents potentially increased the overall risk of CHD and other system anomalies [8,9,10,11]. Also, maternal exposure to organic dyes, lacquers, pigments, and paints during early pregnancy was related to higher cardiac anomalies in the fetus [24, 25]. Some studies showed that exposure to benzene, trichloroethylene, and formaldehyde might increase the prevalence of CHD in offspring [9, 26, 27].
Housing renovation may have different effects on different phenotypes of CHD. By investigating the relationship between housing renovation exposure and the major CHD types, it was found that exposure to housing renovation exposure was associated with an elevated risk for VSD and PDA, which was supported by additional studies. Based on a case-control study, which included all infants born in Finland during 1982–1983 with a VSD, J. Tikkanen and O. P. Heinonen found that maternal exposure to organic solvents during the first trimester may increase the risk of VSD in offspring (OR = 1.8, 95% CI: 1.0, 3.4) [28]. Additionally, a case-control study in the Netherlands found that paternal occupational exposure to phthalates was associated with peri-membranous VSD (adjusted OR = 2.84, 95% CI: 1.37, 5.92) in offspring [29]. While paternal alkylphenolic compound exposure and a higher concentration of maternal blood titanium level increased the risk for PDA in the offspring (OR = 1.95, 95% CI: 1.30, 2.93; OR 2.41, 95% CI: 1.34, 4.36) [30, 31]. Although the association between housing renovation and other phenotypes of CHD (ASD, AVSD, and TOF) was not significant in our study, other research has shown housing renovation exposure or occupational polycyclic aromatic hydrocarbons exposure in pregnancy may be associated with an increased risk for the conotruncal heart defect, specifically TOF [1, 32]. Differences in sample sizes, definitions of exposure and CHD phenotypes, and diagnostic capabilities may contribute to inconsistent outcomes.
This case-control study investigated the association between maternal housing renovation exposure and isolated CHD occurrence. Our study found that maternal exposure to interior housing renovation activity during the periconceptional period may be associated with an increased risk of isolated CHD in offspring. This study added to evidence of the association between housing renovation exposure and the risk of isolated CHD. However, some limitations should be acknowledged. First, although we have established selection criteria for including controls, the selection bias cannot be fully controlled in a hospital-based case-control study. Second, our study did not investigate the specific kinds of housing renovation exposures and the timing of exposures, then we could not perform some sensitivity analysis. Third, even though we account for potential confounders using multivariable regressions and propensity values matching, unmeasured or hidden confounders (such as maternal occupational exposure to solvents/formaldehyde and genetic factors) may still impact the results. Finally, we need to establish a large population cohort with specific ecological contaminants and chemical exposure assessment to confirm the relationship between maternal housing renovation and isolated CHD.
Conclusions
This study found that maternal exposure to housing renovation during the periconceptional period was associated with an increased risk of isolated CHD in offspring. In addition, living in a newly redecorated house may increase the fetus’ risk of VSD and PDA. Therefore, in order to prevent isolated CHD in infants, it may be beneficial to avoid living in a renovated house from 12 months before pregnancy through the first trimester of pregnancy.
Data Availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
References
Liu Z, Li X, Li N, Li S, Deng K, Lin Y, Chen X, You F, Li J, Mu D, et al. Association between maternal exposure to housing renovation and offspring with congenital heart disease: a multi-hospital case-control study. Environ Health. 2013;12:25.
van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, Roos-Hesselink JW. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58(21):2241–7.
Zhao QM, Liu F, Wu L, Ma XJ, Niu C, Huang GY. Prevalence of congenital heart disease at live birth in China. J Pediatr. 2019;204:53–8.
Zimmerman M, Sable C. Congenital heart disease in low-and-middle-income countries: focus on sub-saharan Africa. Am J Med Genet C Semin Med Genet. 2020;184(1):36–46.
Bouma BJ, Mulder BJ. Changing Landscape of congenital heart disease. Circ Res. 2017;120(6):908–22.
Tai CG, Graff RE, Liu J, Passarelli MN, Mefford JA, Shaw GM, Hoffmann TJ, Witte JS. Detecting gene-environment interactions in human birth defects: study designs and statistical methods. Birth Defects Res A Clin Mol Teratol. 2015;103(8):692–702.
Burroughs Pena MS, Rollins A. Environmental Exposures and Cardiovascular Disease: a challenge for Health and Development in Low- and Middle-Income Countries. Cardiol Clin. 2017;35(1):71–86.
Cordier S, Bergeret A, Goujard J, Ha MC, Ayme S, Bianchi F, Calzolari E, De Walle HE, Knill-Jones R, Candela S, et al. Congenital malformation and maternal occupational exposure to glycol ethers. Occupational exposure and congenital malformations Working Group. Epidemiology. 1997;8(4):355–63.
Drake VJ, Koprowski SL, Lough J, Hu N, Smith SM. Trichloroethylene exposure during cardiac valvuloseptal morphogenesis alters cushion formation and cardiac hemodynamics in the avian embryo. Environ Health Perspect. 2006;114(6):842–7.
Thulstrup AM, Bonde JP. Maternal occupational exposure and risk of specific birth defects. Occup Med (Lond). 2006;56(8):532–43.
Vaktskjold A, Talykova LV, Nieboer E. Congenital anomalies in newborns to women employed in jobs with frequent exposure to organic solvents–a register-based prospective study. BMC Pregnancy Childbirth. 2011;11:83.
Johnson PD, Goldberg SJ, Mays MZ, Dawson BV. Threshold of trichloroethylene contamination in maternal drinking waters affecting fetal heart development in the rat. Environ Health Perspect. 2003;111(3):289–92.
Incardona JP, Collier TK, Scholz NL. Defects in cardiac function precede morphological abnormalities in fish embryos exposed to polycyclic aromatic hydrocarbons. Toxicol Appl Pharmacol. 2004;196(2):191–205.
Farwell A, Nero V, Croft M, Bal P, Dixon DG. Modified japanese medaka embryo-larval bioassay for rapid determination of developmental abnormalities. Arch Environ Contam Toxicol. 2006;51(4):600–7.
Baldacci S, Gorini F, Santoro M, Pierini A, Minichilli F, Bianchi F. Environmental and individual exposure and the risk of congenital anomalies: a review of recent epidemiological evidence. Epidemiol Prev. 2018;42(3–4 Suppl 1):1–34.
Kauppinen T. Occupational exposure to chemical agents in the plywood industry. Ann Occup Hyg. 1986;30(1):19–29.
Wieslander G, Norback D, Bjornsson E, Janson C, Boman G. Asthma and the indoor environment: the significance of emission of formaldehyde and volatile organic compounds from newly painted indoor surfaces. Int Arch Occup Environ Health. 1997;69(2):115–24.
Coombs KC, Chew GL, Schaffer C, Ryan PH, Brokamp C, Grinshpun SA, Adamkiewicz G, Chillrud S, Hedman C, Colton M, et al. Indoor air quality in green-renovated vs. non-green low-income homes of children living in a temperate region of US (Ohio). Sci Total Environ. 2016;554–555:178–85.
Ewers L, Clark CS, Peng H, Roda SM, Menrath B, Lind C, Succop P. Lead levels in new residential enamel paints in Taipei, Taiwan and comparison with those in mainland China. Environ Res. 2011;111(6):757–60.
Dolk H, Loane M, Garne E. The prevalence of congenital anomalies in Europe. Adv Exp Med Biol. 2010;686:349–64.
Gilboa SM, Salemi JL, Nembhard WN, Fixler DE, Correa A. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation. 2010;122(22):2254–63.
Motoki N, Inaba Y, Shibazaki T, Misawa Y, Ohira S, Kanai M, Kurita H, Nakazawa Y, Tsukahara T, Nomiyama T, et al. Maternal exposure to housing renovation during pregnancy and risk of offspring with congenital malformation: the Japan Environment and Children’s study. Sci Rep. 2019;9(1):11564.
Li J, Liu W, Xia W, Zhao H, Zhou Y, Li Y, Wu C, Liu H, Zhang B, Zhu Y, et al. Variations, determinants, and coexposure patterns of Personal Care Product Chemicals among chinese pregnant women: a longitudinal study. Environ Sci Technol. 2019;53(11):6546–55.
Tikkanen J, Heinonen OP. Risk factors for conal malformations of the heart. Eur J Epidemiol. 1992;8(1):48–57.
Shaw GM, Nelson V, Iovannisci DM, Finnell RH, Lammer EJ. Maternal occupational chemical exposures and biotransformation genotypes as risk factors for selected congenital anomalies. Am J Epidemiol. 2003;157(6):475–84.
Yauck JS, Malloy ME, Blair K, Simpson PM, McCarver DG. Proximity of residence to trichloroethylene-emitting sites and increased risk of offspring congenital heart defects among older women. Birth Defects Res A Clin Mol Teratol. 2004;70(10):808–14.
Watson RE, Jacobson CF, Williams AL, Howard WB, DeSesso JM. Trichloroethylene-contaminated drinking water and congenital heart defects: a critical analysis of the literature. Reprod Toxicol. 2006;21(2):117–47.
Tikkanen J, Heinonen OP. Risk factors for ventricular septal defect in Finland. Public Health. 1991;105(2):99–112.
Snijder CA, Vlot IJ, Burdorf A, Obermann-Borst SA, Helbing WA, Wildhagen MF, Steegers EA, Steegers-Theunissen RP. Congenital heart defects and parental occupational exposure to chemicals. Hum Reprod. 2012;27(5):1510–7.
Sun J, Mao B, Wu Z, Jiao X, Wang Y, Lu Y, Ma X, Liu X, Xu X, Cui H, et al. Relationship between maternal exposure to heavy metal titanium and offspring congenital heart defects in Lanzhou, China: a nested case-control study. Front Public Health. 2022;10:946439.
Fazekas-Pongor V, Csaky-Szunyogh M, Fekete M, Meszaros A, Cseh K, Penzes M. Congenital heart diseases and parental occupational exposure in a hungarian case-control study in 1997 to 2002. Congenit Anom (Kyoto). 2021;61(2):55–62.
Patel J, Nembhard WN, Politis MD, Rocheleau CM, Langlois PH, Shaw GM, Romitti PA, Gilboa SM, Desrosiers TA, Insaf T, et al. Maternal occupational exposure to polycyclic aromatic hydrocarbons and the risk of isolated congenital heart defects among offspring. Environ Res. 2020;186:109550.
Acknowledgements
We thank all the participants and investigators in this study. We also thank the staff from Xi’an Jiaotong University for their assistance with the data collection.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82103924; No. 72174167; No. 81230016) and the Key Research and Development Program of Shaanxi Province (No. 2021ZDLSF02-14, No. 2022ZDLSF02-11).
Author information
Authors and Affiliations
Contributions
Pengfei Qu: Conceptualization, Methodology, Data curation, Investigation, Writing - original draft, Writing -review & editing. Doudou Zhao: Data curation, Methodology, Investigation. Mingxin Yan: Data curation, Investigation. Danmeng Liu: Methodology, Investigation. Ruo Zhang: Investigation. Shanshan Li: Investigation. Leilei Pei: Investigation. Hong Yan: Conceptualization, Supervision, Funding acquisition. Lingxia Zeng: Conceptualization, Supervision. Shaonong Dang: Conceptualization, Supervision, Writing - review & editing.All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study (No. 2012008) was approved by the Human Research Ethics Committee of Xi’an Jiaotong University Health Science Center. All pregnant women were informed about the study and provided written informed consent.
Consent for publication
All authors are responsible for reported research. They have approved the manuscript.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qu, P., Zhao, D., Yan, M. et al. Maternal exposure to housing renovation during the periconceptional period and the risk of offspring with isolated congenital heart disease: a case-control study. Environ Health 22, 37 (2023). https://doi.org/10.1186/s12940-023-00990-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-023-00990-z