Abstract
Background
There is an increasing global interest in the role of Japanese diet as a possible explanation for the nation’s healthy diet, which contributes to the world’s highest life-expectancy enjoyed in Japan. However, nationwide studies on current food intake status among general Japanese population have not been established yet. This study examined the association between food intake patterns and cardiovascular risk factors (CVRF) such as waist circumference (WC), body mass index (BMI), blood pressure (SBP, DBP), HbA1c and blood lipid profiles among general Japanese adults.
Methods
De-identified data on the Japan National Health and Nutrition Survey (NHNS) 2012 with a total of 11,365 subjects aged 20–84 years were applied. Food intake patterns were derived by principal component analysis (PCA) based on 98 food groups. Generalized linear regression analysis was used to assess the relation between the food intake patterns and CVRF.
Results
We identified three food intake patterns: traditional Japanese, Westernized, and meat and fat patterns. Traditional Japanese pattern was significantly related to high WC and BMI in men, and high DBP in women. Westernized pattern was associated with lower SBP, but high total cholesterol and LDL cholesterol in both men and women. Meat and fat pattern was associated with high WC, high BMI, high blood pressure and blood lipid profiles in both men and women (trend P < 0.001).
Conclusion
The significant association between cardiovascular disease risks and three food intake patterns derived from the NHNS, showed a similar tendency to other dietary survey methods.
Similar content being viewed by others
Background
Cardiovascular disease (CVD) is one of the major contributors to the global burden of disease, and is the leading cause of premature mortality [1]. The vast majority of cardiovascular disease is explained by conventional risk factors such as cigarette smoking, hypertension, obesity, diabetes, dyslipidemia, and unhealthy lifestyle behaviors including poor dietary habits, excessive caloric intake, physical inactivity, and psychosocial stressors [2, 3]. Along with lifestyle factors such as physical activity, diet is one of the most important modifiable risk factors [4,5,6,7], providing effective means to achieve healthy and nutritious diets are essential for cardiovascular disease prevention [8].
Japan is unique among developed countries because the prevalence of cardiovascular disease morbidity and mortality remain substantially lower despite having the same trend in cardiovascular risk factors (CVRF) (such as rise in serum cholesterol, etc.) as other developed countries [9, 10]. The world’s highest healthy life expectancy enjoyed in Japan may be partly explained by the Japanese diet. For example, a very recent cohort study found that the food intake patterns of Japanese adults who followed the government recommended food guide for the nation (the Japanese Spinning Top Food Guide 2005) at the baseline, had lower rates of mortality than those who didn’t [11]. And, another nationwide study in elderly Japanese has observed that improvement in dietary habits, such as yearly increase in vegetables and meat intake, may contribute to decreasing prevalence of anemia [12].
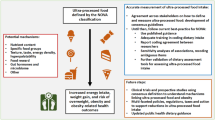
As dietary habits are influenced by lifestyle, socioeconomic and environmental factors such as family income, food prices, individual preferences, cultural beliefs, traditional single food- or nutrient-based approach may fail to take into consideration the complicated interaction and cumulative effects among nutrients. Therefore, overall assessment of food intake patterns, taking into account of the interactions, inter-correlations between nutrients and foods and their cumulative effects, has gained attention in the studies of the association between health and diseases [13].
Many epidemiologic cohort studies have been implemented to explain the correlation between food intake patterns and cardiovascular risk factors such as hypertension, obesity and blood lipid profiles [14, 15]. The scientific evidences have consistently shown that the food intake pattern rich in fruits, vegetables, fish and whole grains (known as healthy or prudent pattern) [16,17,18], DASH diet (Dietary Approaches to Stop Hypertension) [19] and Mediterranean diet [20,21,22,23] are favorable for reducing cardiovascular disease risks, whereas food intake patterns characterized by high fat and sugar or a meat-based diet have deleterious effects and have been associated with increased risks of obesity, type 2 diabetes, and cardiovascular disease [15, 24]. To date, only one cross-sectional study in Japanese reported that vegetable-rich diet pattern was significantly associated with favorable blood lipid profiles in women [25]. Most of the above mentioned cohort studies identified food intake pattern using intake data from semi-quantified food frequency questionnaires (FFQs), on limited populations. Because FFQs are developed to assess the habitual intakes of the specific population of research subjects, the food lists (5 to 350, median number 79) applied may not be able to reflect the intakes of the general population [26]. On the other hand, weighed dietary records are able to provide more details on actual intakes and provide more precise estimates of portion sizes than FFQs. The Japan National Health and Nutrition Survey (J-NHNS) is unique, as it is based on a single day dietary survey in which the survey participants are requested to weigh and record all foods consumed. Currently 2116 food items are available for use in the J-NHNS. Of these, 1789 food items are the same as those listed in the Standard Tables of Food Composition 2010 [27], and 50 food items are original for the survey. The foods are then grouped into 98 food groups, which has been consistently used since 2005 [28].
This study aimed to explore the food intake patterns and examine their association with cardiovascular risk factors such as waist circumference, body mass index (BMI), blood pressure, HbA1c level and blood lipid profiles among 11,365 Japanese aged 20–84 years, using the nationally representative data from J-NHNS conducted in year 2012, while controlling for a wide range of potential confounding factors.
Methods
Survey outlines of the 2012 J-NHNS
Out of the 2010 national census areas units, 475 areas stratified by prefecture were randomly extracted for the 2012 J-NHNS, consisting of 10 areas per prefecture (Tokyo: 15 areas). Approximately 50 households were included in each area. Participants were household members (aged 1 year and over) of all households residing in the selected area. Total number of households and family members aged 1 year and over in the 475 areas were approximately 23,750 and 61,000, respectively. Of the selected census areas, four alternative areas were re-selected to replace those unable to conduct this survey due to the influence of the Great East Japan Earthquake [28].
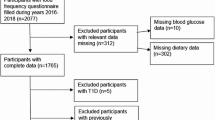
De-identified records on the 2012 J-NHNS with the permission of secondary use of data from Ministry of Health, Labor and Welfare were applied. A total of 11,365 subjects, 4686 men and 6679 women (pregnant and lactating mothers were excluded) aged 20–84 years who had a complete data on dietary intake, lifestyle factors, anthropological and blood pressure measurements, HbA1c measured in National Glyco-hemoglobin Standardization Program (NGSP) units (%), fasting blood lipid profiles [total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C)] were selected.
The dietary survey was conducted by semi-weighing of all foods consumed in the one-day dietary records of the household, with proportional distribution within the household members [29]. Information regarding the cooking status (boiled, roasted, etc.) of each food was recorded, and post-cooked nutrient values in the Standard Food Composition Tables 2010 were applied for estimating nutrient intakes. For foods categorized as “cereals” except bread, post-cooked weight of the food was applied as the intake food weight. Participants aged 20 years and above were asked to record the number of daily step counts measured with a pedometer as part of the physical examination. BMI was calculated by weight in kilograms divided by height in meters squared.
Definition of hypertension, diabetes, hypercholesterolemia and elevated LDL cholesterol
Hypertension was defined as either having a systolic blood pressure (SBP) of ≥140 mmHg or diastolic blood pressure (DBP) of ≥90 mmHg, currently under anti-hypertensive treatment, or previously diagnosed for hypertension. We defined diabetes based on HbA1c ≥6.5% or currently under anti-diabetic treatment, or previously diagnosed for diabetes. Subjects with hypercholesterolemia were defined as having serum total cholesterol level ≥ 240 mg/dL and subjects with elevated LDL cholesterol were defined as having serum LDL cholesterol level ≥ 140 mg/dL or subjects having lipid lowering medication for both. In the present study, anti-hyperlipidemia medication included both cholesterol-lowering medication and triglyceride-lowering medication.
Statistical analysis
The original 2116 food items used in the J-NHNS are categorized into 98 food groups [28]. Then food intake patterns were identified using principal component analysis (PCA) based on the 34 food groups reorganized from the original 98 food groups (Table 1). Analyses were done after excluding the subjects with total energy intake (kcal) under the 5th percentile (n = 1281, 1124 kcal) or above the 95th percentile (n = 1281, 2792 kcal). Eigen values > 1.5 were used to determine whether a factor should be considered as major food intake pattern. Varimax rotation was applied to review the correlations between variables and factors. Food groups with positive loadings in each pattern indicate the direct relationship and food groups with negative loadings shows the inverse relationship with that pattern. For each subject, the factor scores for each food intake pattern were calculated by summing the intakes of food items weighted by their factor loading [13]. Factor scores were then categorized into four groups based on the quartiles of factor scores. Spearman’s correlation coefficients were calculated between the factor scores of each pattern and energy-adjusted nutrient intakes so that the correlation between food intake patterns and specific nutrient intakes could be studied.
Generalized linear models was used to assess the association of adherence to three major food intake patterns with waist circumference, body mass index (BMI), systolic and diastolic blood pressure, HbA1c and blood lipid profiles (TC, LDL-C and HDL-C) after adjustment with other potential confounding variables; such as age in years, BMI, step counts/day (as continuous variables), smoking habit (1: current smoker, 2: past smoker, 3: non smoker), drinking habit (1: Yes, 2: No), and, medication status (hypertension, diabetes, and dyslipidemia, 1:Yes, 2: No). Trend association across quartile categories of each food intake pattern was assessed by using Cochrane-Armitage trend test for categorical variables and generalized linear regression analysis for continuous variables. Logistic regression analysis was used to determine the association of dietary patterns with the risk of hypertension, hypercholesterolemia and elevated LDL cholesterol. The odds ratios (OR) were estimated for each quartile compared with the lowest quartile of each food intake pattern as the reference. The association analyses were performed separately in men and women. Two-sided P values <0.05 were regarded as statistically significant. All statistical analyses were performed using Statistical Analysis System 9.3 (SAS Institute, Cary, NC, USA).
Results
Food intake pattern analysis
We identified three food intake patterns by principal component analysis: (a) “traditional Japanese” (greater intake of miso, soy sauce, fresh vegetables and fruits, beans and potatoes), (b) “Westernized” (greater intake of bread, dairy, butter and margarine, jam, low intake of rice and miso), (c) “Meat and fat” (high intake of meat, fat, sauce and mayonnaise, wheat and wheat products). These three food intake patterns accounted for 2.1%, 2.0% and 1.7%, respectively, explained 5.8% of the total variance in food intake (Table 1).
Spearman’s correlation coefficients showed positive correlations between nutrients and traditional Japanese pattern, while Westernized pattern showed positive correlation with total fat intake, micronutrients except vitamin D, vitamin B12, sodium and iron, and negative correlation with carbohydrate, ω-3 fatty acid. Meat and fat patterns showed positive correlation with total energy, protein and fat intake, ω-6 fatty acids, vitamin B1, sodium and iron, and negative correlation with other micronutrients (Table 2).
General characteristics of the subjects by food intake patterns
Table 3 shows the general characteristics of the study subjects according to quartile categories of each food intake pattern score. Subjects with a higher score for the traditional Japanese pattern were older, had higher BMI and waist circumference, higher SBP, lower LDL-C, higher proportion of having anti-hypertensive, anti-diabetic, anti-lipid medication and were likely to be past smoker in men and less likely to have smoking and drinking habits in women. Subjects with a higher score for the Westernized pattern were older, had lower BMI and waist circumference, higher LDL-C, were likely to have anti-hypertensive and anti-lipid medications, and were likely to have drinking habit than the group with lower Westernized pattern score. Participants with higher meat and fat pattern score were younger, had higher step counts, less likely to take anti-hypertensive, anti-diabetic and anti-lipid medications, but more likely to have smoking and drinking habits.
Energy and nutrients intake across the quartiles of food intake patterns
We explored the relationship between nutrients intake and the food intake pattern scores by generalized linear model analysis (Table 4). For all three food intake pattern scores, higher scores were associated with higher total energy intake in both men and women. A higher traditional Japanese pattern score was significantly associated with higher intakes of protein, ω-3, ω-6 fatty acids, dietary fiber, vitamin A, D, B1, B2, B6, B12, C, folate, sodium, potassium, calcium and iron in both men and women. Higher Westernized pattern score was associated with higher intake of protein, fat, ω-6 fatty acids, dietary fiber, vitamin A, B1, B2, B6, C, folate, sodium, potassium, calcium, and lower intake of ω-3 fatty acids, carbohydrates, vitamin D and vitamin B12. Higher meat and fat pattern score was associated with higher intakes of protein, fat, ω-6 fatty acids, dietary fiber, vitamin B1, B2, B6, sodium, iron and lower intakes of ω-3 fatty acids, vitamin B12, C, folate, potassium and calcium in both men and women.
Association of each food intake pattern with waist circumference, BMI, blood pressure and blood lipid profiles
Table 5 shows mean waist circumference, BMI, blood pressure, HbA1c and blood lipid profiles according to the quartiles for each food intake pattern. The multivariable adjusted geometric means for waist circumference (P for trend = 0.008) and BMI (P for trend = 0.001) in men, and mean DBP (P for trend = 0.019) in women were significantly increased according to the lowest to the highest quartile of traditional Japanese pattern. Men in the highest quartile of Westernized pattern had lower SBP (P for trend = 0.003), higher TC (P for trend = 0.047) and higher LDL-C (P for trend = 0.006), while women in the highest quartile of Westernized pattern had lower waist circumference (P for trend = 0.039), lower BMI (P for trend <0.001), lower SBP (P for trend = 0.001) and higher TC, HDL-C and LDL-C (P for trend <0.001 for all). Compared with the lowest quartile of the meat and fat pattern, those in the highest quartile had higher waist circumference (P for trend = 0.016), SBP (P for trend = 0.013), DBP (P for trend = 0.003), TC (P for trend <0.001) and LDL-C (P for trend <0.001) in men and higher waist circumference (P for trend <0.001), BMI (P for trend <0.001), TC (P for trend = 0.001) and LDL-C (P for trend = 0.013) in women. No association between HbA1c and food intake patterns was observed in both men and women.
Association of each food intake pattern with hypertension, diabetes, hypercholesterolemia and elevated LDL cholesterol
Table 6 showed the logistic regression analysis for the association of each food intake pattern with cardiovascular disease risk. Traditional Japanese pattern was related to a lower prevalence of hypertension in men and not in women. The multivariate-adjusted ORs (95% CI) for the lowest through highest quartiles of the traditional Japanese pattern were 1.00 (reference), 0.75 (0.59–0.95), 0.83 (0.65–1.04) and 0.67 (0.53–0.84), respectively (trend P = 0.003). Westernized pattern was associated with higher prevalence of hypercholesterolemia and elevated LDL cholesterol in women, but not in men. The multivariate-adjusted ORs (95% CI) comparing the highest quartile to the lowest were Q2: 1.13 (0.87–1.46), Q3: 1.33 (1.04–1.71) and Q4: 1.80 (1.41–2.29) for hypercholesterolemia (trend P < 0.001), and Q2: 1.19 (0.86–1.62), Q3: 1.43 (1.06–1.93) and Q4: 1.75 (1.30–2.35) for elevated LDL cholesterol (trend P < 0.001). Also, higher meat-fat pattern score was positively associated with hypertension, diabetes and hypercholesterolemia in men, but not in women (Table 6).
Discussion
In this cross-sectional analysis of the Japan NHNS 2012 data, we identified three food intake patterns derived by principal component analysis: the traditional Japanese pattern, Westernized pattern, meat and fat pattern. Food intake patterns showed differences in associations between CVRFs among men and women. The traditional Japanese pattern was significantly associated with increased BMI and waist circumference, but significantly lower prevalence of hypertension in men. This association may be partly explained by higher energy intake, but with higher vegetable as well as potatoes consumption, which are rich in potassium [30] and contributed to lower blood pressure [31]. However, the traditional Japanese pattern for women was found to have a positive association with diastolic blood pressure. High salt intake (such as from miso soup and Japanese pickles intake) in the highest quartile of traditional Japanese pattern in women may have contributed to raised diastolic blood pressure [32, 33].
Westernized pattern was inversely associated with SBP in men, waist circumference in both men and women, and BMI (in women). The Westernized pattern identified in our study is somewhat similar to previously reported ‘bread-dairy pattern’ or ‘Westernized breakfast pattern’, mainly comprising bread and danish, butter and margarine, milk, cheese and yogurt, fresh fruits but low intakes of rice, which was inversely related with abdominal obesity, BMI and blood pressure [34,35,36,37]. In our study population, subjects in the highest quartile of the Westernized pattern consumed greater amount of potassium intake than those in the lowest quartile. Because high potassium intake is a known protective factor for hypertension [31], the higher potassium intake from fresh fruits in the high Westernized pattern score group may have contributed to lower blood pressure. Additionally, foods or nutrients contributed to westernized breakfast pattern such as milk and yogurt, which are rich source of calcium, have also been shown to decrease blood pressure [38]. On the other hand, the Westernized pattern was positively associated with HDL-C (in women), TC and LDL-C in both men and women, and positively associated with hypercholesterolemia and elevated LDL cholesterol in women. This may be due to high fat intake among the highest quartile of Westernized pattern (Table 4) [39].
Interestingly, a simultaneous increase in both HDL and LDL cholesterol was observed with the higher Westernized pattern score in women, consistent with the finding reported by JY Shin et al., 2013 [35]. It has been reported that the average HDL-C levels are indeed high among Japanese people in general, due to genetic deficiency of cholesteryl ester transfer protein (CETP) [40]. In spite of high HDL-C levels, we speculate that these certain number of subjects with CETP deficiency had increased risk of dyslipidemia. Furthermore, this direct association of increased HDL cholesterol with the Westernized pattern might be mediated by lower carbohydrates [41] and higher saturated fat intake [42] and butter [43] among those in the highest quartile of the Westernized pattern.
As expected, meat and fat pattern identified in our study was positively associated with waist circumference, BMI, blood pressure, TC and LDL-C in both men and women, and higher prevalence of hypertension, diabetes and hypercholesterolemia in men after additional adjustment for waist circumference and BMI [44,45,46,47]. These positive associations may partly be attributable to the unhealthy cardiovascular risk constituents in meat and fat pattern (such as red meat and saturated fats and cholesterol) [48]. Our result is comparable to a cohort study in Japan that reported a pattern with high meat intakes was closely related to an increased risk of cardiovascular diseases [49].
However, the present study has some limitations. First, as the association was derived from the cross-sectional study, the causal relationship between food intake patterns and the cardiovascular risk factors could not be determined, and may have possibility of reverse causality. Awareness of previously diagnosed hypertension or dyslipidemia can alter their food intake patterns, such as an increase in the consumption of vegetables in hypertensive subjects [50]. However, the significant association persisted after adjusting for medication for hypertension, diabetes and hyperlipidemia. Second, as the Japan NHNS is usually conducted in November, the observed food intake patterns may not accurately reflect seasonal variations in food intake and availability. Third, although the food intake was estimated through a self-reported dietary record data and checking of the records were conducted by trained dieticians, under or over reporting of intake is inevitable. Last, because food intake patterns were derived from the one-day dietary record with a diverse variables of food items, explained variation in food groups of the principal component analysis was low compared to previous studies using FFQs. Because FFQs are developed to assess the habitual food intakes of the specific population of research subjects, the possible food intake patterns may have been pre-defined by their habitual intake which give rise to higher explained variance of each pattern compared to one-day dietary record. Previous study of dietary patterns by Hamer M et al. using weighed food record also showed a similar trend of low percentage of explained variance [51]. Moreover, a study of dietary patterns by McCann SE et al. using FFQs, also observed that the explained variance increased as the number of food groups decreased [52]. Despite these limitations, our study was based on a large-scale, nationally representative health and nutrition survey data, which was highly standardized in obtaining socio demographic and lifestyle characteristics as well as biological cardiovascular risk factors.
Conclusion
In summary, three major food intake patterns identified in this cross-sectional analysis, were found to have significant associations with cardiovascular risk factors. The traditional Japanese pattern showed protective effect against hypertension in men, Westernized pattern was positively associated with dyslipidemia in women, while meat-fat pattern was related to all cardiovascular risk factors in men. The association between cardiovascular disease risk factors and food intake patterns derived from one-day dietary records of the National Health and Nutrition Survey was similar to previous cohort studies examining habitual intake through FFQs.
Abbreviations
- BMI:
-
Body mass index
- CETP:
-
Cholesteryl ester transfer protein
- CVD:
-
Cardiovascular disease
- CVRF:
-
Cardiovascular risk factors
- DASH:
-
Dietary approaches to stop hypertension
- DBP:
-
Diastolic blood pressure
- FFQs:
-
Food frequency questionnaires
- HbA1c:
-
Hemoglobin A1c
- HDL-C:
-
High density lipoprotein cholesterol
- J-NHNS:
-
The Japan National Health and Nutrition Survey
- LDL-C:
-
low density lipoprotein cholesterol
- NGSP:
-
National Glyco-hemoglobin Standardization Program
- OR:
-
Odds ratio
- PCA:
-
Principal component analysis
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- WC:
-
Waist circumference
References
Roth GA, Nguyen G, Forouzanfar MH, Mokdad AH, Naghavi M, Murray CJ. Estimates of global and regional premature cardiovascular mortality in 2025. Circulation. 2015;132:1270–82.
Ezzati M, Riboli E. Behavioral and dietary risk factors for noncommunicable diseases. N Engl J Med. 2013;369:954–64.
Eilat-Adar S, Mete M, Fretts A, Fabsitz RR, Handeland V, Lee ET, Loria C, Xu J, Yeh J, Howard BV. Dietary patterns and their association with cardiovascular risk factors in a population undergoing lifestyle changes: the strong heart study. Nutr Metab Cardiovasc Dis. 2013;23:528–35.
Retelny VS, Neuendorf A, Roth JL. Nutrition protocols for the prevention of cardiovascular disease. Nutr Clin Pract. 2008;23:468–76.
Magnussen CG, Smith KJ, Juonala M. When to prevent cardiovascular disease? As early as possible: lessons from prospective cohorts beginning in childhood. Curr Opin Cardiol. 2013;28:561–8.
World Health Organization. Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation. In WHO technical report series 2003. (Geneva: World Health Organization; vol 916.)
Murtagh EM, Murphy MH, Boone-Heinonen J. Walking—the first steps in cardiovascular disease prevention. Curr Opin Cardiol. 2010;25:490–6.
Buttar HS, Li T, Ravi N. Prevention of cardiovascular diseases: role of exercise, dietary interventions, obesity and smoking cessation. Exp Clin Cardiol. 2005;10:229–49.
Iso H. Lifestyle and cardiovascular disease in Japan. J Atheroscler Thromb. 2011;18:83–8.
Sekikawa A, Miyamoto Y, Miura K, Nishimura K, Willcox BJ, Masaki KH, Rodriguez B, Tracy RP, Okamura T, Kuller LH. Continuous decline in mortality from coronary heart disease in Japan despite a continuous and marked rise in total cholesterol: Japanese experience after the seven countries study. Int J Epidemiol. 2015;44:1614–24.
Kurotani K, Akter S, Kashino I, Goto A, Mizoue T, Noda M, Sasazuki S, Sawada N. Tsugane S, and Japan public health center based prospective study group. Quality of diet and mortality among Japanese men and women: Japan Public Health Center based prospective study BMJ. 2016;352:i1209.
Imai E, Nakade M, Kasaoka T, Takimoto H. Improved prevalence of anemia and nutritional status among Japanese elderly participants in the National Health and nutritional survey Japan, 2003-2009. J Nutr Food Sci. 2016;6:495.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9.
Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008;118:230–7.
Wang D, He Y, Li Y, Luan D, Yang X, Zhai F, Ma G. Dietary patterns and hypertension among Chinese adults: a nationally representative cross-sectional study. BMC Public Health. 2011;11:925.
Hu FB. Plant-based foods and prevention of cardiovascular disease: an overview. Am J Clin Nutr. 2003;78:544S–51S.
Yokoyama Y, Nishimura K, Barnard ND, Takegami M, Watanabe M, Sekikawa A, Okamura T, Miyamoto Y. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med. 2014;174:577–87.
van Dam RM, Grievink L, Ocke MC, Feskens EJ. Patterns of food consumption and risk factors for cardiovascular disease in the general Dutch population. Am J Clin Nutr. 2003;77:1156–63.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–20.
Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92:1189–96.
Dontas AS, Zerefos NS, Panagiotakos DB, Vlachou C, Valis DA. Mediterranean diet and prevention of coronary heart disease in the elderly. Clin Interv Aging. 2007;2:109–15.
Estruch R, Ros E, Martinez-Gonzalez MA. Mediterranean diet for primary prevention of cardiovascular disease. N Engl J Med. 2013;369:676–7.
Rees K, Hartley L, Flowers N, Clarke A, Hooper L, Thorogood M, Stranges S. 'Mediterranean' dietary pattern for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;8:CD009825.
Na L, Han T, Zhang W, Wu X, Na G, Du S, Li Y, Sun C. A snack dietary pattern increases the risk of hypercholesterolemia in northern Chinese adults: a prospective cohort study. PLoS One. 2015;10:e0134294.
Sadakane A, Tsutsumi A, Gotoh T, Ishikawa S, Ojima T, Kario K, Nakamura Y, Kayaba K. Dietary patterns and levels of blood pressure and serum lipids in a Japanese population. J Epidemiol. 2008;18:58–67.
Cade J, Thompson R, Burley V, Warm D. Development, validation and utilisation of food-frequency questionnaires - a review. Public Health Nutr. 2002;5:567–87.
The Ministry of Education, Culture, Sports, Science and Technology. Standard Tables of Food Composition in Japan—2010—. Official Gazette Co-operation of Japan, Tokyo. 2010; pp.
Ministry of Health, Labour and Welfare. Annual Report of the National Nutrition Survey in 2012. Tokyo, Japan: Daiichi Publishing Co; 2016.
Ikeda N, Takimoto H, Imai S, Miyachi M, Nishi N. Data resource profile: the Japan National Health and nutrition survey (NHNS). Int J Epidemiol. 2016;44:1842–9.
Carla RM, Anne CK, Jean D. The role of potatoes and potato components in cardiometabolic health: a review. Ann Med. 2013;45:467–73.
Ekmekcioglu C, Elmadfa I, Meyer AL, Moeslinger T. The role of dietary potassium in hypertension and diabetes. J Physiol Biochem. 2016;72(1):93–106.
Takase H, Sugiura T, Kimura G, Ohte N, Dohi Y. Dietary sodium consumption predicts future blood pressure and incident hypertension in the Japanese normotensive general population. J Am Heart Assoc. 2015;4:e001959.
Wakasugi M, James Kazama J, Narita I. Associations between the intake of miso soup and Japanese pickles and the estimated 24-hour urinary sodium excretion: a population-based cross-sectional study. Intern Med. 2015;54:903–10.
Arisawa K, Uemura H, Yamaguchi M, Nakamoto M, Hiyoshi M, Sawachika F, Katsuura-Kamano S. Associations of dietary patterns with metabolic syndrome and insulin resistance: a cross-sectional study in a Japanese population. J Med Investig. 2014;61:333–44.
Shin JY, Kim JM, Kim Y. Associations between dietary patterns and hypertension among Korean adults: the Korean National Health and nutrition examination survey (2008-2010). Nutr Res Pract. 2013;7:224–32.
Akter S, Nanri A, Pham NM, Kurotani K, Mizoue T. Dietary patterns and metabolic syndrome in a Japanese working population. Nutr Metab (Lond). 2013;10:30.
Kris-Etherton PM, Grieger JA, Hilpert KF, West SG. Milk products, dietary patterns and blood pressure management. J Am Coll Nutr. 2009;28(Suppl 1):103S–19S.
Lee SA, Cai H, Yang G, Xu WH, Zheng W, Li H, Gao YT, Xiang YB, Shu XO. Dietary patterns and blood pressure among middle-aged and elderly Chinese men in shanghai. Br J Nutr. 2010;104:265–75.
Song S, Paik HY, Park M, Song Y. Dyslipidemia patterns are differentially associated with dietary factors. Clin Nutr. 2016;35(4):885–91.
Yokoyama S. Unique features of high-density lipoproteins in the Japanese: in population and in genetic factors. Nutrients. 2015;7:2359–81.
Santos FL, Esteves SS, da Costa PA, Yancy WS Jr, Nunes JP. Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev. 2012;13:1048–66.
Brinton EA, Eisenberg S, Breslow JL. A low-fat diet decreases high density lipoprotein (HDL) cholesterol levels by decreasing HDL apolipoprotein transport rates. J Clin Invest. 1990;85:144–51.
Engel S, Tholstrup T. Butter increased total and LDL cholesterol compared with olive oil but resulted in higher HDL cholesterol compared with a habitual diet. Am J Clin Nutr. 2015;102:309–15.
Nettleton JA, Polak JF, Tracy R, Burke GL, Jacobs DR Jr. Dietary patterns and incident cardiovascular disease in the multi-ethnic study of atherosclerosis. Am J Clin Nutr. 2009;90:647–54.
Togo P, Osler M, Sorensen TI, Heitmann BL. Food intake patterns and body mass index in observational studies. Int J Obes Relat Metab Disord. 2001;25:1741–51.
Berg CM, Lappas G, Strandhagen E, Wolk A, Toren K, Rosengren A, Aires N, Thelle DS, Lissner L. Food patterns and cardiovascular disease risk factors: the Swedish INTERGENE research program. Am J Clin Nutr. 2008;88:289–97.
Woo HD, Shin A, Kim J. Dietary patterns of Korean adults and the prevalence of metabolic syndrome: a cross-sectional study. PLoS One. 2014;9:e111593.
Vergnaud AC, Norat T, Romaguera D, Mouw T, May AM, Travier N, Luan J, Wareham N, Slimani N, Rinaldi S, et al. Meat consumption and prospective weight change in participants of the EPIC-PANACEA study. Am J Clin Nutr. 2010;92:398–407.
Shimazu T, Kuriyama S, Hozawa A, Ohmori K, Sato Y, Nakaya N, Nishino Y, Tsubono Y, Tsuji I. Dietary patterns and cardiovascular disease mortality in Japan: a prospective cohort study. Int J Epidemiol. 2007;36:600–9.
Tormo MJ, Navarro C, Chirlaque MD, Barber X, and EPIC Group of Spain, European Prospective Investigation on Cancer. Is there a different dietetic pattern depending on self-knowledge of high blood pressure? Eur J Epidemiol 2000; 16: 963–971.
Hamer M, McNaughton SA, Bates CJ, Mishra GD. Dietary patterns, assessed from a weighed food record, and survival among elderly participants from the United Kingdom. Eur J Clin Nutr. 2010;64(8):853–61.
McCann SE, Marshall JR, Brasure JR, Graham S, Freudenheim JL. Analysis of patterns of food intake in nutritional epidemiology: food classification in principal components analysis and the subsequent impact on estimates for endometrial cancer. Public Health Nutr. 2001;4(5):989–97.
Acknowledgements
We would like to thank Dr. Suminori Kono, the Principal Investigator, who designed and planned the research project and made this work possible.
Funding
This work was supported by Health and Labor Sciences Research Grants (Special Research Project H26-tokubetsu-shitei-033) from the Ministry of Health, Labor and Welfare of Japan.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
HT substantially contributed to the conception and design, and the acquisition of the data. HT and NCH contributed to the analysis and interpretation of the data and NCH drafted the manuscript. HS, SI and WS took part in the interpretation of the data and provided critical revisions of the manuscript for important intellectual content. HT made a final revision and approval of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained the consent of the secondary use of the 2012 NHNS data from Ministry of Health, Labor and Welfare. This study was approved by the institutional review board of the National Institute of Health and Nutrition.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Htun, N.C., Suga, H., Imai, S. et al. Food intake patterns and cardiovascular risk factors in Japanese adults: analyses from the 2012 National Health and nutrition survey, Japan. Nutr J 16, 61 (2017). https://doi.org/10.1186/s12937-017-0284-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-017-0284-z