Abstract
Background
Ultrasensitive rapid diagnostic test (usRDT) was recently developed to improve the detection of low-density Plasmodium falciparum infections. However, its diagnostic performance has not been evaluated in the Democratic Republic of Congo (DRC). This study aims to determine the performance of the usRDT in malaria diagnosis in asymptomatic individuals under field condition in Kisangani, Northeast of DRC.
Methods
A community-based cross-sectional study was carried out from June to August 2022 on 312 asymptomatic individuals residing in the city of Kisangani. Capillary blood samples were collected by finger prick for microscopic examination of thick and thin blood film, RDTs, and nested polymerase chain reaction (PCR). Alere™ Malaria Ag P.f usRDT and conventional RDT (cRDT/SD Bioline Malaria Ag P.f) kits were used for the detection of Plasmodium histidine rich protein 2 (HRP2) antigen as a proxy for the presence of P. falciparum. The diagnostic performance of the usRDT was compared with cRDT, microscopy and PCR.
Results
The prevalence of asymptomatic P. falciparum malaria was 40.4%, 42.0%, 47.1% and 54.2% by cRDT, microscopy, usRDT and PCR, respectively. By using PCR as a reference, usRDT had sensitivity and specificity of 87.0% (95% CI 81.4–91.7) and 100.0% (95% CI 97.5–100.0), respectively, whereas the cRDT had sensitivity and specificity of 74.6% (95% CI 67.3–80.9) and 100% (95% CI 97.1–100.0), respectively. By using microscopy as a reference, usRDT had sensitivity and specificity of 96.9% (95% CI 92.4–99.2) and 89.0% (95% CI 83.5–93.1), respectively, while the cRDT had sensitivity and specificity of 96.2% (95% CI 92.3–98.7) and 100% (95% CI 97.9–100.0), respectively.
Conclusion
The usRDT showed better diagnostic performance with higher sensitivity than the cRDT which is currently in use as point-of-care test. Further research is necessary to assess the access and cost-effectiveness of the usRDTs to use for malaria surveillance.
Similar content being viewed by others
Background
Malaria remains a global public health concern, affecting hundreds of millions of people each year. In 2021 alone, an estimated 247 million cases and 619,000 deaths due to malaria were reported globally. Most of the cases (95%) and deaths (96%) were in the African region [1]. The Democratic Republic of Congo (DRC) is one of the highest burden African countries, accounting for 12% of all malaria cases and 13% of malaria-related deaths globally [1]. It is estimated that about 97% of the population of the DRC live in zones with stable malaria transmission [2]. Plasmodium falciparum is the predominant cause of malaria in the country [3].
Vector control using long-lasting insecticidal nets (LLINs) and indoor residual spraying (IRS), and prompt detection and treatment of symptomatic malaria cases are the key strategies widely used for malaria prevention and control in Africa [4]. The scale-up of these control tools and strategies have significantly reduced malaria burden in the region in the past decades, averting an estimated 663 million malaria cases between 2000 and 2015 [4, 5]. Although this progress has stalled since 2015 due to different reasons [6, 7], the past gains have brought the notion of malaria elimination in Africa [8], and countries are intensifying the control interventions to keep up the momentum of fighting against malaria.
One of the major challenges to malaria control and elimination efforts in sub-Saharan Africa is asymptomatic malaria, which is highly prevalent in many African settings including DRC [9,10,11,12]. Asymptomatic individuals often do not seek treatment for their infection but represent a potential reservoir of malaria parasites, thereby sustaining the transmission [13,14,15]. The World Health Organization (WHO) recommends transforming malaria surveillance into a core intervention to address this challenge and hasten the progress towards elimination [8]. This involves using active case detection (ACD) methods such as mass or targeted screening of population following an index case identified at a health facility to treat asymptomatic malaria-positive cases and eventually interrupt the transmission [8, 16]. ACD is usually performed in the community and hence depends on prompt diagnosis by using rapid diagnostic tests (RDTs) and microscopy [8, 16, 17].
However, the effectiveness of ACD is limited due to the inability of the commonly used malaria diagnostic tools to detect low density asymptomatic infections [17,18,19,20]. Microscopic examination of thick and thin blood film is considered the gold standard method as it allows identification of parasite species and estimation of parasitaemia [21]. However, lack of competent microscopists and misdiagnosis due to low parasitaemia are the main challenges in many countries [21]. Conventional RDTs (cRDTs) have also played a significant role in malaria control efforts, with additional advantages in terms of speed, cost-effectiveness and convenience of use with minimum training. However, they have low sensitivity with detection limit of about 100–200 parasites/µL (p/µL) and hence they cannot detect low-density P. falciparum infections [20, 22,23,24]. Molecular techniques such as polymerase chain reaction (PCR) have greater sensitivity than both the cRDTs and microscopy, with a capacity of detecting infections with parasite density as low as 0.2 p/µL [25,26,27]. However, using PCR in the field on large scale is impractical as it requires expensive laboratory equipment, reagents and well-trained personnel [25, 28].
To overcome the limitation of the cRDTs, ultra-sensitive RDT (Abbott Alere™ Malaria Ag P. falciparum usRDT) has recently been developed for the detection of P. falciparum infections [24]. It is a histidine rich protein 2 (HRP2)-based test that has more than tenfold lower limit of detection (10–40 pg/ ml of HRP2) when compared to the conventional SD Bioline Malaria Ag P.f RDT (800–1000 pg/ml of HRP2), and was prequalified by the WHO in 2019 [29]. The usRDT has a capacity of detecting low-density infections with parasitaemia as low as 1.2 p/µL, with a potential of detecting new erythrocytic-stage P. falciparum infections in earlier days than the cRDT [24, 29, 30].
Previous studies conducted in different malaria transmission settings have shown wide variation in usRDT sensitivities compared to PCR [24, 29, 31,32,33]. Cross-sectional surveys conducted in Mozambique, Uganda, Myanmar and Ghana reported sensitivity estimates of usRDT ranging from 68.2% to 84% for detection of asymptomatic P. falciparum infections [24, 30, 34], and sensitivity of up to 99% for detection of infections among febrile patients [35, 36]. In systematic reviews, the pooled sensitivity of the usRDTs in asymptomatic individuals is estimated to reach up to 50% versus 27% for cRDTs when PCR was used as a reference [37, 38]. In some studies where malaria prevalence was determined by using both usRDT and cRDT, the prevalence was found to be 1.5–2 times higher using the usRDT compared to the cRDT [33, 39,40,41,42]. On the other hand, usRDT did not show better diagnostic performance over the cRDT in some studies [31, 32].
Although most studies from other countries reported better sensitivity of usRDTs compared to the cRDT, no study evaluating the diagnostic performance of usRDTs has been conducted in the DRC. Hence, this study aimed to evaluate the performance of the usRDT in diagnosing P. falciparum malaria under field condition among asymptomatic individuals in Kisangani, Northeast of DRC.
Methods
Study design and setting
A community-based cross-sectional study was carried out in selected communes of Kisangani from June to August, 2022. Kisangani is a capital city of the province of Tshopo in the Northeast of the DRC (Fig. 1). It is located at 1724 km northwest of Kinshasa, the capital of DRC. The city has an area of 1910 Km2 and the estimated population size is 1602,144 [43]. The climate of Kisangani is equatorial type in general. The temperature varies between 25° and 28°, and it rains all year round with periods of maximum and minimum rain. The city is made up of 6 communes, each of which constitutes a health zone and includes a general reference hospital as well as health centers. Malaria is endemic in the province of Tshopo in general and the city of Kisangani in particular. Anopheles mosquitoes are known to maintain an intense (up to 1000 infective bites per person per year) and perennial transmission of malaria in the area [2, 44].
Sample size and sampling techniques
The sample size was calculated using the method of Buderer et al. [45]. First, the proportion of true positive (TP) plus false negative (FN) for sensitivity (Se); and the true negative (TN) plus false positive (FP) for specificity (Sp) were determined using the following equations:
where \({Z}_{\alpha /2}\), the normal distribution value, was set to 1.96 as corresponding with the 95% confidence interval (CI), W, the maximum acceptable width of the 95% CI, is set to 7%, and the expected sensitivity of 68.2% and specificity of 99% are defined based on the estimates from previous studies done in Mozambique [34]. The next step was to calculate the sample size (N) required for sensitivity and specificity using the following equations:
where P is the anticipated prevalence of malaria. Taking the prevalence of asymptomatic malaria of 63% in 2016 in the northeast part of DRC [9], and considering an expected nonresponse rate of 15%, a minimum of 312 and 15 samples were required for sensitivity and specificity, respectively. Finally, the larger sample size (312) was used for this study.
The city of Kisangani is administratively subdivided into six communes. This study covered three communes selected randomly: Kabondo, Makiso and Kisangani. The sample size was proportionally allocated to each commune based on their population size. A systematic sampling technique was used to select 312 households, and one individual was randomly selected per household (Fig. 2). Households were visited during the weekends and evening hours when most individuals were at their home to make sure that each household member has equal chance of being selected as a study participant. When the randomly selected individuals were not found at home during the first household visits, return visits were scheduled to collect samples and relevant data from the selected individuals. Individuals who took anti-malarial treatment within four weeks of the blood sample collection were not included in this study.
Data collection
Information on socio-demographic factors, malaria history, and preventive methods was obtained from the participants using a pre-tested, structured questionnaire. The questionnaire included questions on sex, age, educational level, residence, occupation, marital status, history of fever in the preceding 72 h, previous anti-malarial treatment in the preceding month, and whether the participants slept under insecticide-treated nets (ITNs)/LLINs the previous night. Prior to commencement of the study, a pretest was conducted in a neighboring commune on five percent of the total sample size, and the questionnaire was further modified after the pretest. The axillary temperature was measured using an electronic thermometer before each blood sample collection and fever was defined as a temperature ≥ 37.5 °C. Finger-prick blood sample was collected from each study participant for RDTs, microscopic examination of thick and thin blood film, and PCR. For the PCR, 2–3 dry blood spots (DBS), each with 50µL of blood, was prepared on Whatman 3 MM filter paper for each study participant. Blood sample collection from all study participants was done by experienced laboratory technologists.
Laboratory work
Rapid diagnostic tests
Both cRDT (SD Bioline Malaria Ag P.f, Catalog Number: 05FK50-40, Abbott, USA) and usRDT (Alere™ Malaria Ag P.f Ultra-Sensitive, Catalog Number: 05FK140, Abbott, USA) were used to test for P. falciparum HRP2 according to the manufacturer’s instructions. For both RDT kits, 5 µL of capillary whole blood was applied to sample well, followed by addition of four drops of assay buffer. The test results were read after 15 min for the cRDT and after 20 min for the usRDT. A positive signal (red color) on both control and test lines was considered as a positive test result for P. falciparum, and a positive control line without signal on the test line was interpreted as a negative result. Any test result without a signal on the control line was considered an invalid test and the test was repeated in this case. All individuals found positive for malaria by RDTs were advised to visit the nearest health facility for treatment.
Microscopic examination
Thick and thin blood smears were made on the same slide, and the thin smears were fixed by absolute methanol. The slides were then transported to the Kisangani provincial laboratory and stained with 10% Giemsa following standard operating procedures [46]. All slides were examined microscopically by an experienced laboratory technologist. The slides were considered negative if no parasite was seen after examining 100 high power fields. Asexual parasite density was quantified against 200 leucocytes. This was converted to the number of parasites per microliter of blood assuming a white blood cell (WBC) count of 8,000/µL as recommended by the WHO [21]. Parasite density was classified as low parasitaemia (< 1000 p/µL), moderate (1000–4999 p/µL), high (5000–99,999 p/µL), and hyper parasitaemia (≥ 100,000 p/µL) [47]. Quality control slides (all positive blood smear slides and 10% of the negative slides) were re-examined by another blinded senior laboratory technologist.
Molecular diagnosis using polymerase chain reaction
The collected DBS were transported to the Institut National de Recherche Biomédicale (INRB) in Kinshasa to test for the presence of P. falciparum by PCR. DNA was extracted from the DBS using the QIAamp DNA Mini Kit (QIAGEN, UK), following the manufacturer’s instructions.
A nested PCR was used to amplify species-specific sequences of the small sub-unit ribosomal ribonucleic acid (18S SSU rRNA) genes of P. falciparum as previously described elsewhere [48, 49]. In the first amplification reaction, a pair of oligonucleotide primers (genus-specific rPLU1: 5′-TCAAAGATTAAGCCATGCAAGTGA-3′ and rPLU5: 5′-CCTGTTGTTGCCTTAAACTCC-3′) was used to amplify fragment of the genes [49]. The product of this first reaction was then used as DNA template for the second amplification reaction. Both the first and second PCR amplifications were carried out in a total volume of 25 µL consisting of 2 µL template; 0.25 μM of each primer; 1.5 mM magnesium chloride; 0.2 mM dNTPs; 1X PCR Buffer; and 1U Taq polymerase. Primers specific to P. falciparum (rFAL1: 5′-TTAAACTGGTTTGGGAAAACCAAATATATT-3′ and rFAL2: 5′-ACACAATGAACTCAATCATGACTACCCGTC-3′) were used [49]. The PCR assays were performed using a PTC-100 Thermal Cycler (MJ Research Inc.), with the following cycling condition: initial denaturation at 94 °C for 4 min, followed by 25 cycles of denaturation at 94 °C for 1 min, annealing at 65 °C for 2 min and extension at 72 °C for 2 min, and final extension at 72 °C for 4 min. The amplicons were electrophoresed using 2% agarose gel prepared in Tris–borate-EDTA and stained with ethidium bromide for visual detection by ultraviolet transilluminator. Purified 3D7 DNA parasite strain was used as a positive control whereas a negative control without a DNA template was run in all reactions for quality control. Plasmodium falciparum infections detected by PCR but not by microscopy were classified as sub-microscopic infections [50].
Data analysis
Data were checked for completeness and consistency, coded and entered into Epi-info version 7.0, and exported into the Statistical Package for Social Science version 25 (SPSS, Chicago, IL, USA) and JASP 0.16 (JASP TEAM, University of Amsterdam, The Netherlands) for further analysis. The basic characteristics of the study participants were summarized using descriptive statistics.
Sensitivity, specificity, positive predictive value, and negative predictive value of cRDT and usRDT were determined using microscopy and PCR as reference methods [51]. The 95% confidence interval was calculated for each performance indicator using MedCalc statistical software [52]. Kappa coefficient was calculated to assess the agreement among the different diagnostic methods. Depending on the value of the kappa, the level of the agreement between RDTs and the reference methods was considered non-existent if the kappa value was between 0 and 0.2; minimal if it was between 0.21 and 0.39; low between 0.40 and 0.59; moderate between 0.60 and 0.79; strong between 0.80 and 0.90 and almost perfect agreement with a kappa value greater than 0.90 [53].
Results
Characteristics of the study participants
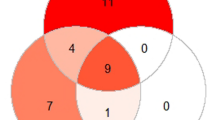
Most of the study participants (94.2%) were over the age of 15 years, with mean age of 25.4. The majority (54.5%) of the participants were females. Study participants from Makiso, Kabondo and Kisangani represent 34.4%, 34.3% and 31.3%, respectively. Most (94%) of the study participants reported that they had at least one LLIN in their house and 79% of them reported to have used LLINs the previous night. Only 4.2% of the study participants reported that IRS was applied to their houses in the past 6 months. Malaria prevalence by cRDT, microscopy, usRDT and PCR was 40.4%, 42.0%, 47.1% and 54.2%, respectively (Table 1). Of the 312 study participants tested, 125 (40.1%) were positive for the 4 diagnostic methods used in this study (Fig. 3).
RDTs performance against microscopy
Using microscopy as a reference, usRDT showed an overall sensitivity and specificity of 96.9% (95% CI 92.4–99.2) and 89.0% (95% CI 83.5–93.1), respectively. The cRDT had sensitivity and specificity values of 96.2% (95% CI 91.3–98.7) and 100% (95% CI 97.9–100.0), respectively. The level of agreement between microscopy and both RDT types was significant, with a strong agreement documented between usRDT and microscopy (Kappa = 0.84, p < 0.01), and almost perfect agreement between cRDT and microscopy (Kappa = 0.96, p < 0.01) (Table 2).
Performance of RDTs against PCR
The cRDT failed to detect a total of 43 of the 169 positive cases by PCR, representing a false negative rate of 25.4%. Of these 43 cases, 22 were correctly detected by usRDT. In comparison, the usRDT failed to detect P. falciparum in 22 of the 169 positive cases, giving a false negative rate of 13.0% (Fig. 3). Using PCR as a reference, the usRDT showed higher sensitivity (87.0%, 95% CI 81.4–91.7) when compared with cRDT (74.6%, 95% CI 67.3–80.9). Both cRDT and usRDT were highly specific (100%). Overall, the level of agreement between both cRDT and usRDT and PCR was significant (p < 0.05). The level of agreement between usRDT and PCR was stronger (Kappa = 0.86, p < 0.01) and higher than that of cRDT versus PCR (Kappa = 0.72, p < 0.01), which was a moderate agreement (Table 3).
Distribution of parasitaemia according to RDTs positive results
Most of the malaria positive study participants (97.0%) had low parasitaemia whereas 3.0% of them had moderate parasitaemia. The mean parasitaemia was 541.30 (± 300.32) p/µL for cRDT positive results with minimum and maximum values of 78 p/µl and 2678 p/µL, respectively. Regarding the usRDT positive results, the mean parasitaemia was 467.62 (± 334.62) p/µL with a minimum parasitaemia of 0 p/µL and a maximum parasitaemia of 2678 p/µL.
Performance of RDTs based on the parasite density
The performance of the two RDT kits in terms of sensitivity was higher in people with moderate parasitaemia compared to people with low parasitaemia. For the usRDT, the sensitivity was 100% and 86.6% (95% CI 80.4–91.4) for moderate and low parasitaemia cases, respectively, whereas for the cRDT, the sensitivity was 100% and 73.8% (95% CI 66.4–80.3) for moderate and low parasitaemia cases, respectively (Table 4).
Discussion
In this study, the usRDT showed better diagnostic performance in detecting asymptomatic P. falciparum infections with sensitivity of 87% as compared to the cRDT which had sensitivity of 74.6%, using PCR as a reference. This is consistent with the findings of previous studies conducted in Uganda and Myanmar [24], Ghana [30], Mozambique [34] and Haiti [54], which reported higher sensitivity for the usRDT than the cRDT. The level of agreement between the usRDT and PCR was stronger and higher than that of cRDT versus PCR. This is likely due to the fact that usRDT has a detection limit closer to PCR than the cRDT [24, 30, 49].
On the other hand, usRDT yielded false negative results in 13.0% of the PCR positive samples although this was two times lower when compared to the false negative rate of the cRDT (26.0%). The false negative results recorded by both usRDT and cRDT might be due to the presence of low parasite density below their respective limit of detection. The presence of parasites with P. falciparum HRP2/3 gene deletions could also result in false negative RDT results [55,56,57], although the magnitude of the HRP2/3 gene deletions was not determined in this study. Moreover, a prozone effect due to an excess of either antibodies or HRP2 antigens could contribute to the false negative RDT results [58].
Studies have shown that HRP2 antigen of P. falciparum can persist in the circulation for weeks after an infection is cleared by treatment, and this can give false positive RDT results even in the absence of active infection [59, 60]. In this study, however, both usRDT and cRDT showed 100% specificity with no false positive results by both RDT types, using PCR as a reference. The absence of false positive RDT result might be due to participants selection criteria implemented during this study as people who took anti-malarial drugs within four weeks of the commencement of sample collection were not included in the study. With microscopy as a reference, the usRDT had a similar sensitivity but lower specificity than the cRDT. The difference in specificity between usRDT and cRDT documented in this study was similar to the previous reports from Uganda and Myanmar [24]. The lower specificity of usRDT could be partly attributed to the enhanced sensitivity of the usRDT at detecting lower density parasitaemia and lower concentrations of HRP2 antigens compared to the cRDT [24, 29, 32, 61, 62] and partly due to the presence of sub-microscopic infections. In this study, 23% of the malaria positive cases were submicroscopic infections and half of these were detected by the usRDT, while cRDT missed all submicroscopic PCR positive cases (Fig. 3).
The relative sensitivity of the two RDT types varied based on parasite density. The usRDT exhibited significantly higher sensitivity than the cRDT in detecting low parasitaemia infections, whereas both usRDT and cRDT showed 100% sensitivity for moderate parasitaemia. Other studies have also documented similar findings [24, 29]. In Uganda and Myanmar for instance, the usRDT was shown to detect low parasitaemia infections with parasite density as low as 1.2 p/µL, while cRDT failed to detect P. falciparum in samples with parasitaemia of up to 183 p/uL [24], confirming that the usRDT has a better diagnostic performance in detecting low-density P. falciparum infections than the cRDT. This suggests that the usRDT could be a potential diagnostic tool for screening asymptomatic and submicroscopic Plasmodium infections for prompt case treatment especially in settings targeted for malaria elimination.
It is worth mentioning that the prevalence of asymptomatic P. falciparum infection was high, around 54.2% by PCR, in the study area despite high LLIN ownership. A multi-center study conducted in 2016 in DRC by Mvumbi et al. has also reported an overall malaria prevalence of 43% using PCR, and a prevalence rate of over 63% in Maniema region near Tshopo district, where the city of Kisangani is located [9]. Thus, the high asymptomatic malaria prevalence documented in this study could be due to the study setting since it is located in an area with intense malaria transmission where the number of infectious mosquito bites can reach as high as 1000 bites per person per year [44]. The high malaria parasite prevalence despite high LLIN coverage in the study area suggests that further studies should be carried out to assess LLIN utilization, as sub-optimal utilization could affect the effectiveness of the LLINs. On the other hand, people could be bitten by mosquito vectors in the early evening and morning hours before people sleep under the LLINs, suggesting the need to determine vector biting behaviour in the study area. Moreover, determining insecticide susceptibility level of malaria vectors and other contributing factors [63] is crucial in order to design appropriate control interventions. It is also important to note that the prevalence of sub-microscopic asymptomatic P. falciparum infections was 12.5% in the study area. This implies that malaria surveillance system should be strengthened in the area using sensitive diagnostic tools such as usRDT in order to accurately identify malaria hotspot areas to prioritize control intervention based on evidence.
The limitation of this study is that parasitaemia was quantified using microscopy and parasite density was not determined for PCR positive samples which were negative by microscopy.
Conclusion
In this study, usRDT showed higher sensitivity than cRDT in detecting P. falciparum infections among asymptomatic individuals in a high malaria transmission setting of Kisangani. This is the first study that evaluated the performance of usRDT in DRC and generated evidence to guide policy and the program on the implementation of this tool to diagnose asymptomatic individuals. This study also documented high prevalence of asymptomatic P. falciparum infections among communities residing in the city of Kisangani. Further research is necessary to assess the impact and cost-effectiveness of the usRDTs to be used in the health care system.
Availability of data and materials
Data supporting the conclusions of this article are included within the article. Raw data are available from the corresponding author upon reasonable request.
Abbreviations
- ACD:
-
Active case detection
- CI:
-
Confidence interval
- cRDT:
-
Conventional rapid diagnostic test
- DBS:
-
Dry blood spot
- DRC:
-
Democratic Republic of the Congo
- HRP2/3:
-
Histidine rich protein 2/3
- IRS:
-
Indoor residual spraying
- LLIN:
-
Long-lasting insecticidal net
- PCR:
-
Polymerase chain reaction
- RDT:
-
Rapid diagnostic test, Se: sensitivity
- Sp:
-
Specificity
- usRDT:
-
Ultrasensitive rapid diagnostic test
- WHO:
-
World Health Organization
References
WHO. World malaria report 2022. Geneva: World Health Organization; 2022.
PNLP, Swiss TPH, KSPH, INRB and INFORM. An epidemiological profile of malaria in the Democratic Republic of Congo. A report prepared for the Federal Ministry of Health, Democratic Republic of Congo, the Roll Back Malaria Partnership and the Department for International Development, UK. March, 2014.
Mitchell CL, Topazian HM, Brazeau NF, Deutsch-Feldman M, Muwonga J, Sompwe E, et al. Household Prevalence of Plasmodium falciparum, Plasmodium vivax, and Plasmodium ovale in the Democratic Republic of the Congo, 2013–2014. Clin Infect Dis. 2021;73:e3966–9.
Bhatt S, Weiss D, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–11.
WHO. World malaria report 2015. Geneva: World Health Organization; 2015.
Dhiman S. Are malaria elimination efforts on right track? An analysis of gains achieved and challenges ahead. Infect Dis Poverty. 2019;8:14.
Mayor A, Bassat Q. “Resistance” to diagnostics: a serious biological challenge for malaria control and elimination. EBioMedicine. 2019;50:9–10.
WHO. Global technical strategy for malaria 2016–2030. Geneva: World Health Organization; 2015.
Mvumbi DM, Bobanga TL, Melin P, De Mol P, Kayembe J-MN, Situakibanza HN-T, et al. High prevalence of Plasmodium falciparum infection in asymptomatic individuals from the Democratic Republic of the Congo. Malar Res Treat. 2016. https://doi.org/10.1155/2016/5405802.
Djoufounna J, Mayi MPA, Bamou R, Foyet JV, Tabue R, Lontsi-Demano M, et al. High prevalence of asymptomatic Plasmodium falciparum malaria in Makenene, a locality in the forest-savannah transition zone, Centre Region of Cameroon. Curr Res Parasitol Vector Borne Dis. 2022;2: 100104.
Lindblade KA, Steinhardt L, Samuels A, Kachur SP, Slutsker L. The silent threat: asymptomatic parasitemia and malaria transmission. Expert Rev Anti Infect The. 2013;11:623–39.
Yimam Y, Nateghpour M, Mohebali M, Abbaszadeh Afshar MJ. A systematic review and meta-analysis of asymptomatic malaria infection in pregnant women in sub-Saharan Africa: a challenge for malaria elimination efforts. PLoS ONE. 2021;16: e0248245.
Bousema JT, Gouagna LC, Drakeley CJ, Meutstege AM, Okech BA, Akim IN, et al. Plasmodium falciparum gametocyte carriage in asymptomatic children in western Kenya. Malar J. 2004;3:18.
Bousema T, Okell L, Felger I, Drakeley C. Asymptomatic malaria infections: detectability, transmissibility and public health relevance. Nat Rev Microbiol. 2014;12:833–40.
Degefa T, Zeynudin A, Zemene E, Emana D, Yewhalaw D. High prevalence of gametocyte carriage among individuals with asymptomatic malaria: implications for sustaining malaria control and elimination efforts in Ethiopia. Human Parasit Dis. 2016;8:17.
Wickremasinghe R, Fernando SD, Thillekaratne J, Wijeyaratne PM, Wickremasinghe AR. Importance of active case detection in a malaria elimination programme. Malar J. 2014;13:186.
Aidoo EK, Afrane YA, Machani MG, Chebore W, Lawson BW, Atieli H, et al. Reactive case detection of Plasmodium falciparum in western Kenya highlands: effective in identifying additional cases, yet limited effect on transmission. Malar J. 2018;17:111.
Laishram DD, Sutton PL, Nanda N, Sharma VL, Sobti RC, Carlton JM, et al. The complexities of malaria disease manifestations with a focus on asymptomatic malaria. Malar J. 2012;11:29.
Lo E, Zhou G, Oo W, Afrane Y, Githeko A, Yan G. Low parasitemia in submicroscopic infections significantly impacts malaria diagnostic sensitivity in the highlands of Western Kenya. PLoS ONE. 2015;10: e0121763.
Hemingway J, Shretta R, Wells TN, Bell D, Djimdé AA, Achee N, et al. Tools and strategies for malaria control and elimination: what do we need to achieve a grand convergence in malaria? PLoS Biol. 2016;14: e1002380.
WHO. Malaria microscopy quality assurance manual-version 2. Geneva: World Health Organization; 2016.
Slater HC, Ross A, Ouédraogo AL, White LJ, Nguon C, Walker PG, et al. Assessing the impact of next-generation rapid diagnostic tests on Plasmodium falciparum malaria elimination strategies. Nature. 2015;528:S94–101.
Laban NM, Kobayashi T, Hamapumbu H, Sullivan D, Mharakurwa S, Thuma PE, et al. Comparison of a Pf HRP2-based rapid diagnostic test and PCR for malaria in a low prevalence setting in rural southern Zambia: implications for elimination. Malar J. 2015;14:25.
Das S, Jang IK, Barney B, Peck R, Rek JC, Arinaitwe E, et al. Performance of a high-sensitivity rapid diagnostic test for Plasmodium falciparum malaria in asymptomatic individuals from Uganda and Myanmar and naive human challenge infections. Am J Trop Med Hyg. 2017;97:1540.
Mathison BA, Pritt BS. Update on malaria diagnostics and test utilization. J Clin Microbiol. 2017;55:2009–17.
Li P, Zhao Z, Wang Y, Xing H, Parker DM, Yang Z, et al. Nested PCR detection of malaria directly using blood filter paper samples from epidemiological surveys. Malar J. 2014;13:175.
Naeem MA, Ahmed S, Khan SA. Detection of asymptomatic carriers of malaria in Kohat district of Pakistan. Malar J. 2018;17:44.
Urdea M, Penny LA, Olmsted SS, Giovanni MY, Kaspar P, Shepherd A, et al. Requirements for high impact diagnostics in the developing world. Nature. 2006;444(Suppl 1):73–9.
Das S, Peck RB, Barney R, Jang IK, Kahn M, Zhu M, et al. Performance of an ultra-sensitive Plasmodium falciparum HRP2-based rapid diagnostic test with recombinant HRP2, culture parasites, and archived whole blood samples. Malar J. 2018;17:118.
Acquah FK, Donu D, Obboh EK, Bredu D, Mawuli B, Amponsah JA, et al. Diagnostic performance of an ultrasensitive HRP2-based malaria rapid diagnostic test kit used in surveys of afebrile people living in Southern Ghana. Malar J. 2021;20:125.
Yeung S, McGregor D, James N, Kheang ST, Kim S, Khim N, et al. Performance of ultrasensitive rapid diagnostic tests for detecting asymptomatic Plasmodium falciparum. Am J Trop Med Hyg. 2020;102:307–9.
Hofmann NE, Antunes Moniz C, Holzschuh A, Keitel K, Boillat-Blanco N, Kagoro F, et al. Diagnostic performance of conventional and ultrasensitive rapid diagnostic tests for malaria in febrile outpatients in Tanzania. J Infect Dis. 2019;219:1490–8.
Landier J, Haohankhunnatham W, Das S, Konghahong K, Christensen P, Raksuansak J, et al. Operational performance of a Plasmodium falciparum ultrasensitive rapid diagnostic test for detection of asymptomatic infections in Eastern Myanmar. J Clin Microbiol. 2018;56:e00565-e618.
Galatas B, Mayor A, Gupta H, Balanza N, Jang IK, Nhamussua L, et al. Field performance of ultrasensitive and conventional malaria rapid diagnostic tests in southern Mozambique. Malar J. 2020;19:451.
Kyabayinze D, Kajungu D, Nambuya PM, Okiira C, Ndawula B, Kawooya M, et al. Evaluating field performance of highly sensitive malaria RDT: detection of infection among febrile patients, asymptomatic pregnant women and household contacts in Mpigi. Research Square: Uganda; 2021.
Manjurano A, Omolo JJ, Lyimo E, Miyaye D, Kishamawe C, Matemba LE, et al. Performance evaluation of the highly sensitive histidine-rich protein 2 rapid test for Plasmodium falciparum malaria in North-West Tanzania. Malar J. 2021;20:58.
Danwang C, Kirakoya-Samadoulougou F, Samadoulougou S. Assessing field performance of ultrasensitive rapid diagnostic tests for malaria: a systematic review and meta-analysis. Malar J. 2021;20:245.
Yimam Y, Mohebali M, Abbaszadeh Afshar MJ. Comparison of diagnostic performance between conventional and ultrasensitive rapid diagnostic tests for diagnosis of malaria: a systematic review and meta-analysis. PLoS ONE. 2022;17: e0263770.
Slater HC, Ding XC, Knudson S, Bridges DJ, Moonga H, Saad NJ, et al. Performance and utility of more highly sensitive malaria rapid diagnostic tests. BMC Infect Dis. 2022;22:121.
Hofmann NE, Gruenberg M, Nate E, Ura A, Rodriguez-Rodriguez D, Salib M, et al. Assessment of ultra-sensitive malaria diagnosis versus standard molecular diagnostics for malaria elimination: an in-depth molecular community cross-sectional study. Lancet Infect Dis. 2018;18:1108–16.
Owalla TJ, Okurut E, Apungia G, Ojakol B, Lema J, Murphy SC, et al. Using the ultrasensitive Alere Plasmodium falciparum malaria Ag HRP-2™ rapid diagnostic test in the field and clinic in Northeastern Uganda. Am J Trop Med Hyg. 2020;103:778.
Girma S, Cheaveau J, Mohon AN, Marasinghe D, Legese R, Balasingam N, et al. Prevalence and epidemiological characteristics of asymptomatic malaria based on ultrasensitive diagnostics: a cross-sectional study. Clin Infect Dis. 2019;69:1003–10.
CAID. Cellule d’Analyses des Indicateurs de Développement (Development indicator analysis unit). 2023 https://caid.cd/. Accessed 08 Jul 2023
Bain LE, Dobermann D. Malaria, HIV and TB in the Democratic Republic of the Congo: epidemiology, disease control challenges and interventions. K4D Help Desk. 2022. https://doi.org/10.19088/K4D.2022.034.
Buderer NMF. Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med. 1996;3:895–900.
WHO. Basic malaria microscopy: tutor’s guide. Geneva: World Health Organization; 2010.
Sumbele IU, Ning TR, Bopda OS, Nkuo-Akenji T. Variation in malariometric and red cell indices in children in the Mount Cameroon area following enhanced malaria control measures: evidence from a repeated cross-sectional study. Malar J. 2014;13:334.
Snounou G, Singh B. Nested PCR analysis of Plasmodium parasites. Methods Mol Med. 2002. https://doi.org/10.1385/1-59259-271-6:189.
Singh B, Bobogare A, Cox-Singh J, Snounou G, Abdullah MS, Rahman HA. A genus-and species-specific nested polymerase chain reaction malaria detection assay for epidemiologic studies. Am J Trop Med Hyg. 1999;60:687–92.
Tran TM, Aghili A, Li S, Ongoiba A, Kayentao K, Doumbo S, et al. A nested real-time PCR assay for the quantification of Plasmodium falciparum DNA extracted from dried blood spots. Malar J. 2014;13:393.
Kosinski AS. A weighted generalized score statistic for comparison of predictive values of diagnostic tests. Stat Med. 2013;32:964–77.
MedCalc Software Ltd. Diagnostic test evaluation calculator. https://www.medcalc.org/calc/diagnostic_test.php Accessed 2 Nov 2023.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia Medica. 2012;22:276–82.
Rogier E, Hamre KE, Joseph V, Plucinski MM, Presume J, Romilus I, et al. Conventional and high-sensitivity malaria rapid diagnostic test performance in 2 transmission settings: Haiti 2017. J Infect Dis. 2020;221:786–95.
Agaba BB, Yeka A, Nsobya S, Arinaitwe E, Nankabirwa J, Opigo J, et al. Systematic review of the status of pfhrp2 and pfhrp3 gene deletion, approaches and methods used for its estimation and reporting in Plasmodium falciparum populations in Africa: review of published studies 2010–2019. Malar J. 2019;18:355.
Alemayehu GS, Blackburn K, Lopez K, Cambel Dieng C, Lo E, Janies D, et al. Detection of high prevalence of Plasmodium falciparum histidine-rich protein 2/3 gene deletions in Assosa zone, Ethiopia: implication for malaria diagnosis. Malar J. 2021;20:109.
Akinyi Okoth S, Abdallah JF, Ceron N, Adhin MR, Chandrabose J, Krishnalall K, et al. Variation in Plasmodium falciparum histidine-rich protein 2 (Pfhrp2) and Plasmodium falciparum histidine-rich protein 3 (Pfhrp3) gene deletions in Guyana and Suriname. PLoS ONE. 2015;10: e0126805.
Gillet P, Mori M, Van Esbroeck M, Ende JVD, Jacobs J. Assessment of the prozone effect in malaria rapid diagnostic tests. Malar J. 2009. https://doi.org/10.1186/1475-2875-8-271.
Adjei GO, Sulley AM, Goka BQ, Enweronu-Laryea C, Renner L, Alifrangis M, et al. Performance of a histidine rich protein-2 based (First Response) and a p-Lactate Dehydrogenase-based (Optimal) rapid diagnostic test for diagnosis of malaria in patients with pediatric sickle cell disease. Clin Infect Dis. 2022;75:435–41.
Kiemde F, Bonko MdA, Tahita MC, Lompo P, Rouamba T, Tinto H, et al. Accuracy of a Plasmodium falciparum specific histidine-rich protein 2 rapid diagnostic test in the context of the presence of non-malaria fevers, prior anti-malarial use and seasonal malaria transmission. Malar J. 2017. https://doi.org/10.1186/s12936-017-1941-6.
Okell LC, Ghani AC, Lyons E, Drakeley CJ. Submicroscopic infection in Plasmodium falciparum-endemic populations: a systematic review and meta-analysis. J Infect Dis. 2009;200:1509–17.
Mpina M, Stabler TC, Schindler T, Raso J, Deal A, Acuche Pupu L, et al. Diagnostic performance and comparison of ultrasensitive and conventional rapid diagnostic test, thick blood smear and quantitative PCR for detection of low-density Plasmodium falciparum infections during a controlled human malaria infection study in Equatorial Guinea. Malar J. 2022;21:99.
Morgan CE, Topazian HM, Brandt K, Mitchell C, Kashamuka MM, Muwonga J, et al. Association between domesticated animal ownership and Plasmodium falciparum parasite prevalence in the Democratic Republic of the Congo: a national cross-sectional study. Lancet Microbe. 2023;4:e516–23.
Acknowledgements
We would like to thank field assistants Kisubi Astride and Lumbu Tabytha for their support during data collection process and Wanga Paulin for her technical support during laboratory work. We are grateful to Ming-Chieh Lee for his support in mapping the study area. We would also like to thank the MOUNAF project for its financial support during the research work. We are grateful to the study participants for their willingness to participate in the study.
Funding
This work was supported by the Intra Africa mobility Program MOUNAF. The funder had no role in the study design, data collection, data analysis, data interpretation, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
ML, TD and DY conceived and designed the study. ML involved in data collection, laboratory work and data analysis. KE and AZ involved in study coordination. ML and TD wrote the manuscript. KE, AZ and DY reviewed the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by Jimma University Institutional Review Board (IRB). An ethical clearance letter together with the study protocol was submitted to the University of Kisangani IRB. Based on the recommendation of the local IRB, the ethical clearance letter was then submitted to higher officials of the City of Kisangani and a support letter was obtained. Written informed consent was sought from the study participants. Assent and written parental/guardian consent were obtained for children and individuals who were unable to provide informed consent. Confidentiality of the participants was maintained. Individuals found positive were treated with appropriate antimalarial drugs at the nearest health facility.
Consent for publication
Not applicable.
Competing interests
The authors have declared that there are no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lupaka, M., Degefa, T., Eba, K. et al. Diagnostic performance of ultrasensitive rapid diagnostic test for the detection of Plasmodium falciparum infections in asymptomatic individuals in Kisangani, Northeast Democratic Republic of Congo. Malar J 22, 354 (2023). https://doi.org/10.1186/s12936-023-04790-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-023-04790-1