Abstract
Background
Plasmodium vivax is responsible for much of malaria outside Africa. Although most P. vivax infections in endemic areas are asymptomatic and have low parasite densities, they are considered a potentially important source of transmission. Several studies have demonstrated that asymptomatic P. vivax carriers can transmit the parasite to mosquitoes, but the efficiency has not been well quantified. The aim of this study is to determine the relationship between parasite density and mosquito infectivity, particularly at low parasitaemia.
Methods
Membrane feeding assays were performed using serial dilutions of P. vivax-infected blood to define the relationship between parasitaemia and mosquito infectivity.
Results
The infection rate (oocyst prevalence) and intensity (oocyst load) were positively correlated with the parasite density in the blood. There was a broad case-to-case variation in parasite infectivity. The geometric mean parasite density yielding a 10% mosquito infection rate was 33 (CI 95 9–120) parasites/µl or 4 (CI 95 1–17) gametocytes/µl. The geometric mean parasite density yielding a 50% mosquito infection rate was 146 (CI 95 36–586) parasites/µl or 13 (CI 95 3–49) gametocytes/µl.
Conclusion
This study quantified the ability of P. vivax to infect Anopheles dirus at over a broad range of parasite densities. It provides important information about parasite infectivity at low parasitaemia common among asymptomatic P. vivax carriers.
Similar content being viewed by others
Background
Malaria continues to be a global scourge of humans. According to the World Health Organization (WHO), the latest estimate of malaria burden was 229 million cases in 2019, of which 409,000 died [1]. A mosquito-borne disease, malaria is caused by the infection of protozoan parasites of the genus Plasmodium. The vast majority of clinical incidences of malaria are due to Plasmodium falciparum and Plasmodium vivax. In the last two decades, the global malaria reduction effort has led to a significant decrease in the case number, but the progress appeared to have slowed down in the last few years [1]. Because malaria is vector-borne, disease control and elimination strategies rely heavily on vector control measures, such as insecticide-treated nets and indoor residual spraying. Additional means to reduce transmissions such as prompt treatment and reporting, reactive surveillance, and use of the 8-aminoquinoline drug primaquine to inactivate gametocytes have also been adopted by various countries [1,2,3].
Most P. vivax infections in endemic areas are asymptomatic, even in low transmission settings approaching elimination [4,5,6,7,8,9]. Because asymptomatic carriers can transmit the disease [10,11,12,13,14,15,16], they represent a challenge for malaria elimination. At present, the extent to which P. vivax carriers contribute to transmission has not been quantified in most settings. Although asymptomatic carriers are much more prevalent than patients, they are less infectious to the mosquitoes due to the lower parasite density in blood. The relative contributions of asymptomatic carriers and patients in a population to malaria transmission depend on the relative prevalence, infectivity, and contact frequency with the mosquito vectors. Few studies have attempted to assess the relative infectivity of asymptomatic carriers and patients [12,13,14,15,16,17]. Recent studies from Ethiopia and Amazonia predicted that asymptomatic carriers contribute approximately 30–80% of transmission [14, 16]. In mainland Southeast Asia, it was recently found that human asymptomatic infections and mosquito infections arose closely in time after mass drug administration (MDA) of dihydroartemisinin-piperaquine with low dose primaquine, suggesting that asymptomatic carriers be the key drivers of transmission [18].
There remains a gap in understanding of how well P. vivax transmits from humans to mosquitoes. Although many mosquito feeding assays have been performed and together provided a valuable dataset of P. vivax infectivity [10,11,12,13,14,15, 19,20,21,22,23,24,25,26,27], the majority of data were obtained at the clinical level of parasite densities. Far fewer data have been acquired at low-density levels typical of asymptomatic carriers [28]. This study aims to fill this gap by determining the quantitative relationship between P. vivax parasite density and mosquito infectivity over a broad range of parasitaemia. Serial dilution of patient blood was used to generate parasite densities at different levels. The membrane feeding assay (MFA) was used with laboratory-reared Anopheles dirus, a major vector in Southeast Asia, to measure P. vivax transmission.
Methods
Blood collection from Plasmodium vivax patients
Plasmodium vivax-infected blood was collected from symptomatic patients who attended malaria clinics in Tak and Ubon Ratchathani provinces of Thailand. The study was approved by the Ethics Committee of Faculty of Tropical Medicine, Mahidol University (MUTM 201 L-040-05). Enrollment was limited to malaria patients who were ≥ 18 years old. From each patient, venous blood (20 ml) was collected in a heparinized tube. Blood was immediately placed in a warm box (37 ℃ ± 5 ℃) and transported to a field laboratory or the Mahidol Vivax Research Unit (MVRU) in Bangkok for MFA.
Blood preparation and membrane feeding assay
For every P. vivax-infected blood sample, P. vivax mono-species infection was confirmed by nested PCR as previously described [29, 30]. Blood was washed with pre-warmed serum-free RPMI 1640 medium and centrifuged at 800 × g for 10 min at 37 °C. Packed infected blood was resuspended with an equal volume of naïve human AB serum to 50% haematocrit (hct). The resuspended blood was subjected to 2-fold serial dilution with warmed 50% hct-O cells in human AB serum, generating 13 different levels of parasitaemia. The final volume for each dilution was 600 µl. The diluted blood was kept at 37 °C until MFA. A thick-film slide was prepared at each parasite concentration for microscopic examination by dotting 1 µL of blood at per spot, five spots per side. The remaining blood was used to feed 100 female An. dirus mosquitoes using MFA.
Light microscopic examination of blood smears
Thick blood smears were stained with 10% Giemsa solution for 10 min, rinsed with running tap water, and air dried. Total parasites per 1 µl spot were counted once under a light microscope (LM) for all original and serially diluted blood samples fed to the mosquitoes. Counts were made separately for asexual and sexual stages.
Nested PCR analysis
To confirm P. vivax mono-infection, nested PCR was performed as previously described [29, 30], using genus and species-specific primers against the 18 S ribosomal RNA genes. Briefly, DNA was extracted by QIAamp® DNA Mini Kit (Qiagen, Germany) according to the manufacturer’s instructions. The first round of PCR was performed using the purified DNA as the template with genus-specific primers. The PCR product was then used as the DNA template for a second PCR reaction which used the same forward primer with a species-specific reverse primer. The second PCR was performed in 5 separate reactions, each detecting P. falciparum, P. vivax, Plasmodium malariae, Plasmodium ovale, or Plasmodium knowlesi DNA. Water was used as the template for the negative controls. The PCR products were visualized on agarose gel after electrophoresis.
Mosquito rearing
A colony of An. dirus was maintained in the insectary of the MVRU. The colony was established in 2011 from the original colony obtained from the Armed Force Research Institute of Medical Sciences, Bangkok, Thailand, as previously described [25]. Briefly, the mosquitoes were reared at 26–27 °C (± 1 °C), 70–80% (± 10%) relative humidity, and with a 12 h day/night cycle. For MFA, female mosquito cartons were placed inside an insulated plastic cooler and ground transported from Bangkok to the field sites. For MFA, female mosquitoes (only 5 to 7 day-old mosquitoes) were used after 6 h sugar starvation. Approximately 100 starved mosquitoes were used for each diluted blood sample.
Membrane feeding assay (MFA)
To feed 100 female mosquitoes, 400 µL of each diluted blood was added to a water-jacketed glass membrane feeder covered with a Baudruche membrane and maintained at 37 °C with a circulating-water system to prevent the transition of gametocytes to gametes. Mosquitoes were allowed to feed for 30 min. The engorged mosquitoes were maintained with 10% sucrose solution. All engorged-mosquito midguts were dissected on day 7 post feeding, stained with 0.05% mercurochrome, and examined under an LM. Two parameters were determined for each feeding experiment: (i) mosquito infection rate (percent oocyst-positive mosquitoes in all mosquitoes dissected) and (ii) oocyst intensity (the mean oocyst count in all mosquito dissected).
Data analysis
When available, parasite and gametocyte densities used in the analysis were direct microscopic counts. At low densities, when no parasite was detected under the microscope, the densities were imputed based on the known fold-dilution of the original samples. All imputed values were less than 5 parasites (or gametocytes) per µl. To determine the parasite (or gametocyte) densities yielding 10% and 50% oocyst prevalence, the rising phase of each dose response (from 0% up to 85% infection rate) was fit to the Hill’s equation using Quest Graph IC50 Calculator [31] with two free parameters, the Hill coefficient and the half-maximal concentration; the minimum and maximum infection rates were set to 0% and 100%, respectively.
Results
General characteristics of P. vivax isolates
Eight P. vivax-infected blood samples were obtained from different malaria patients who visited a health facility in Thailand in 2016–2017. All infections were confirmed to be mono-species by nested PCR [30]. The infection characteristics are summarized in Table 1. The geometric mean parasite density was 1328 (CI95 593–2973) parasites/µL. The geometric mean gametocyte density was 153 (CI95 92–254) gametocytes/µL. The mean female/male ratio was 4.4 (CI95 1.6–7.2).
Relationship between parasite density and mosquito infection
Twelve parasite densities were obtained for each parasite isolate in addition to the original parasite density. The lowest data point represents a 4096-fold reduction of parasite density relative to the original. The parasite density of each diluted blood sample was re-evaluated by LM to ensure that no gross error was introduced by serial dilution. Figure 1 demonstrates the consistency between the LM counts and the calculated parasite densities based on known dilution factors. Actual counts were used in all analysis, except when no parasite was detected, in which case the imputed parasite density value was used.
Plasmodium vivax densities in serially diluted blood samples. Shown are the relationships between actual LM counts and calculated parasite densities based on the dilution factors for a total blood-stage parasites, b total gametocytes, c female gametocytes and d male gametocytes. For each plot, data from all 8 cases were combined. Only data with calculated densities above 3 per microliter were included. Trendlines represent the best linear fits with zero crossing on the log-log scale
In all cases, the MFA showed that both the mosquito infection rate and the oocyst intensity declined as the infected blood was diluted (Fig. 2). In 5/8 cases, a complete or nearly complete dose response was observed. In these cases, the infection rate was over 80% at the highest parasite density (no dilution) and decreased to 0% after the blood was sufficiently diluted. In the three other cases, the infection rate at the highest parasite density was 37–58% resulting in a partial dose response. The lowest infective parasite density (IPL), i.e. the parasite density causing infection in at least one mosquito, ranged from 2 to 129 parasites/µl. The lowest infective gametocyte density (IGL) ranged from 0.2 to 5 gametocytes/µl (Table 2).
The dose response of the mosquito infection rate was further analyzed by non-linear regression. For each parasite isolate, the characteristic parasitaemia resulting in 10% and 50% mosquito infection, referred to as IP10 and IP50, respectively, were determined by fitting the dose response to Hill’s equation and solving the best-fit equation for the 10% and 50% infection rates respectively. The infective gametocytaemias (IG10 and IG50) were similarly determined. Table 3 displays these parameters for each parasite isolates. The geometric means of IP10 and IG10 were 33 (CI95% 9–120) parasites/µl and 4 (CI95% 1–17) gametocytes/ µl, respectively. The geometric means of IP50 and IG50 were 146 (CI95% 36–586) parasites/µl and 13 (CI95% 3–49) gametocytes/µl, respectively. Thus, on average, 33 parasites/µl (or 4 gametocytes/µl) was required to achieve 10% infection in An. dirus. Similarly, 146 parasites/µl (or 13 gametocytes/µl) was required to infect 50% of the mosquitoes.
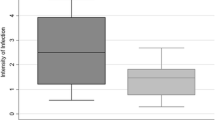
Relationship between the oocyst density and mosquito infection rate
The data from the feeding experiments of the 8 isolates demonstrated a well-defined and robust relationship between the mosquito infection rate and the oocyst intensity (Fig. 3). The trend (filled symbols) increased monotonically and plateaued near the 100% infection rate. This relationship is nearly identical to the previously published one (open symbol) [25] despite the two studies being conducted several years apart. Therefore, the relationship between the mosquito infection rate and the oocyst intensity is robust; one parameter can reasonably predict the other.
Relationship between oocyst density and mosquito infection rate. Black circles represent values from individual feeding experiments in this study. White circles represent values from individual feeding experiments with AB serum replacement from a previous study [25]. The solid red line is the best fit by Hill’s equation
Discussion
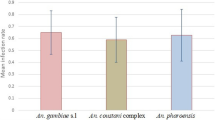
The relationship between P. vivax parasite density in blood and mosquito infectivity is important for estimating the potential of each infected individual to transmission. Several studies have examined this relationship [12, 14, 20, 21, 23,24,25], but the results are variable, presumably reflecting biological differences between different mosquito species and/or parasite isolates as well as methodological differences in the feeding assays [28]. For example, in a study from Ethiopia using Anopheles arabiensis and Anopheles pharoensis [23], the infection rate by MFA was found to increase with gametocyte density and plateaued at about 30–40%. In the same study, the gametocyte density of 50–100 gametocytes/µl was needed to attain the sizable infection rate of 20%. A separate study using An. arabiensis [24] also found that similarly high gametocyte densities were needed to achieve this level of infection. In contrast, in a study using An. dirus [25], only a few P. vivax gametocytes/µl were sufficient to result in a 20% infection rate. In this study, MFAs were performed using serially diluted patient blood with the specific aim of generating a dataset with a balanced parasite density distribution. It was found that the lowest parasite density that gave rise to mosquito infection ranged from 2 to 129 parasites/µl, or from undetectable to 5 gametocytes/µl. While these density values provide a glimpse of transmission potential at low parasite densities, they have limited utility. This is because the values of IPL and IGL depend on the absolute number of mosquitoes examined for infection. As more mosquitoes are examined, IPL and IGL will tend to be lower due to the increased oocyst detection sensitivity. Because of this, it is preferable to characterize the mosquito infectivity by characteristic concentrations like IP10 or IG10. In this study, the geometric mean of IP10 was 33 (CI95% 9–120) parasites/µl and the geometric mean of IG10 was 4 (CI95% 1–17) gametocytes/µl. The 95% confidence interval was broad, reflecting high variation across different feeding experiments. Of note, the value of IP10 is similar to the value predicted by the trendline in a previous study [25], which used 94 independent P. vivax isolates, each at a single parasite density. Thus, the serial dilution MFA provided comparable mosquito infection data with far fewer parasite isolates.
The value of IP10 of 33 parasites/µl suggests that many asymptomatic P. vivax carriers have non-negligible potential to transmit. According to the estimated density distribution of P. vivax in Southeast Asia [32], 22% of asymptomatic carriers are predicted to have parasite density higher than 33 parasites/µl. With the following set of simple assumptions: (a) An. dirus as the sole vector, (b) asymptomatic carriers representing 95% of all P. vivax infections at a given time, (c) 22% of carriers transmitting at the 10% infection rate (or higher), (d) carriers receiving twice more mosquito bites than patients based on the relative outdoor/indoor biting rates [33], and (e) all P. vivax patients transmitting at the average 80% infection rate [25], the contribution of asymptomatic carriers to onward transmission would be similar to that of patients, if not higher. Thus, in Southeast Asia, asymptomatic carriers are likely a critical infectious reservoir. Consistently, in a previous MDA study, it was found that P. vivax asymptomatic infections in humans and wild mosquitoes arose closely in time after the blood stage clearance by the MDA, suggesting a close relationship between the two [18].
This study also has a few limitations. Using serum replacement and serial dilution in MFA imposed two unnatural conditions that may impact the interpretation of the findings. Firstly, MFA may not fully reflect natural transmission through skin feeding. Although studies have suggested that MFA is an acceptable surrogate for natural feeding [19, 34, 35], these studies were conducted at high parasitaemia using patient blood. There is currently no evidence for, or against, the use of MFA for determining transmission at very low P. vivax density. It is plausible that gametocytes are sequestered in the skin to promote their uptake during blood feeding [36, 37], in which case the true potential of P. vivax transmission would have been underestimated by MFA. On the other hand, other unknown factors may also impede transmission from the skin in which case MFA would have overestimated the transmission. Secondly, serially diluting blood in naive AB serum with O red cells removed the immunological factors in the original blood which can influence transmission. Plasma components such as naturally acquired antibodies have been shown to modulate parasite transmission, either by inhibiting it [38, 39] or promoting it [40]. Other soluble mediators including cytokines could also interfere [35, 41,42,43]. With serum replacement, the experiments in this study did not capture these effects. However, in transmission settings where malaria has become low for several years, the effect of antibodies is likely to be small. This is because naturally acquired transmission-blocking immunity had a short duration, declining significantly within months without boosting [39, 44]. Consistent with this, the infectivity dose response in a previous study conducted in a low transmission setting of Thailand was not significantly affected by plasma replacement [25].
Conclusion
The present study quantified the sexual transmission of P. vivax at different parasite dilutions, encompassing the parasitaemia range found in asymptomatic blood-stage parasite carriers. The findings provide critical information for estimating the contribution of asymptomatic infections in malaria transmission. The data suggest that the asymptomatic reservoir is an important source of transmission.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LM:
-
Light microscopy
- MDA:
-
Mass drug administration
- MFA:
-
Membrane feeding assay
- IP:
-
Infective parasitaemia
- IG:
-
Infective gametocytaemia
References
World malaria report. 20 years of global progress and challenges. Geneva: World Health Organization; 2020.
Lertpiriyasuwat C, Sudathip P, Kitchakarn S, Areechokchai D, Naowarat S, Shah JA, et al. Implementation and success factors from Thailand’s 1–3-7 surveillance strategy for malaria elimination. Malar J. 2021. https://doi.org/10.1186/s12936-021-03740-z.
Cao J, Sturrock HJ, Cotter C, Zhou S, Zhou H, Liu Y, et al. Communicating and monitoring surveillance and response activities for malaria elimination: China’s “1-3-7” strategy. PLoS Med. 2014;11:e1001642.
Vasquez-Jimenez JM, Arevalo-Herrera M, Henao-Giraldo J, Molina-Gomez K, Arce-Plata M, Vallejo AF, et al. Consistent prevalence of asymptomatic infections in malaria endemic populations in Colombia over time. Malar J. 2016;15:70.
Waltmann A, Darcy AW, Harris I, Koepfli C, Lodo J, Vahi V, et al. High rates of asymptomatic, sub-microscopic Plasmodium vivax infection and disappearing Plasmodium falciparum malaria in an area of low transmission in Solomon Islands. PLoS Negl Trop Dis. 2015;9:e0003758.
Nguitragool W, Mueller I, Kumpitak C, Saeseu T, Bantuchai S, Yorsaeng R, et al. Very high carriage of gametocytes in asymptomatic low-density Plasmodium falciparum and P. vivax infections in western Thailand. Parasit Vectors. 2017;10:512.
Shimizu S, Chotirat S, Dokkulab N, Hongchad I, Khowsroy K, Kiattibutr K, et al. Malaria cross-sectional surveys identified asymptomatic infections of Plasmodium falciparum, Plasmodium vivax and Plasmodium knowlesi in Surat Thani, a southern province of Thailand. Int J Infect Dis. 2020;96:445–51.
Hailemeskel E, Tebeje SK, Behaksra SW, Shumie G, Shitaye G, Keffale M, et al. The epidemiology and detectability of asymptomatic Plasmodium vivax and Plasmodium falciparum infections in low, moderate and high transmission settings in Ethiopia. Malar J. 2021;20:59.
Sattabongkot J, Suansomjit C, Nguitragool W, Sirichaisinthop J, Warit S, Tiensuwan M, et al. Prevalence of asymptomatic Plasmodium infections with sub-microscopic parasite densities in the northwestern border of Thailand: a potential threat to malaria elimination. Malar J. 2018;17:329.
Coleman RE, Kumpitak C, Ponlawat A, Maneechai N, Phunkitchar V, Rachapaew N, et al. Infectivity of asymptomatic Plasmodium-infected human populations to Anopheles dirus mosquitoes in western Thailand. J Med Entomol. 2004;41:201–8.
Vantaux A, Samreth R, Piv E, Khim N, Kim S, Berne L, et al. Contribution to malaria transmission of symptomatic and asymptomatic parasite carriers in Cambodia. J Infect Dis. 2018;217:1561–8.
Martins-Campos KM, Kuehn A, Almeida A, Duarte APM, Sampaio VS, Rodriguez IC, et al. Infection of Anopheles aquasalis from symptomatic and asymptomatic Plasmodium vivax infections in Manaus, western brazilian Amazon. Parasit Vectors. 2018;11:288.
Vallejo AF, Garcia J, Amado-Garavito AB, Arevalo-Herrera M, Herrera S. Plasmodium vivax gametocyte infectivity in sub-microscopic infections. Malar J. 2016;15:48.
Tadesse FG, Slater HC, Chali W, Teelen K, Lanke K, Belachew M, et al. The relative contribution of symptomatic and asymptomatic Plasmodium vivax and Plasmodium falciparum infections to the infectious reservoir in a low-endemic setting in Ethiopia. Clin Infect Dis. 2018;66:1883–91.
Alves FP, Gil LH, Marrelli MT, Ribolla PE, Camargo EP, Da Silva LH. Asymptomatic carriers of Plasmodium spp. as infection source for malaria vector mosquitoes in the brazilian Amazon. J Med Entomol. 2005;42:777–9.
Ferreira M, Corder R, Johansen I, Kattenberg J, Moreno M, Rosas-Aguirre A, et al. Relative contribution of low-density and asymptomatic infections to Plasmodium vivax transmission in the Amazon: pooled analysis of individual participant data from population-based cross-sectional surveys. Lancet Reg Health Am. 2022;9:100169.
Almeida GG, Costa PAC, Araujo MDS, Gomes GR, Carvalho AF, Figueiredo MM, et al. Asymptomatic Plasmodium vivax malaria in the brazilian Amazon: submicroscopic parasitemic blood infects Nyssorhynchus darlingi. PLoS Negl Trop Dis. 2021;15:e0009077.
Chaumeau V, Kajeechiwa L, Fustec B, Landier J, Naw Nyo S, Nay Hsel S, et al. Contribution of asymptomatic Plasmodium infections to the transmission of malaria in Kayin State, Myanmar. J Infect Dis. 2019;219:1499–509.
Sattabongkot J, Maneechai N, Rosenberg R. Plasmodium vivax: gametocyte infectivity of naturally infected thai adults. Parasitology. 1991;102 Pt 1:27–31.
Bharti AR, Chuquiyauri R, Brouwer KC, Stancil J, Lin J, Llanos-Cuentas A, et al. Experimental infection of the neotropical malaria vector Anopheles darlingi by human patient-derived Plasmodium vivax in the peruvian Amazon. Am J Trop Med Hyg. 2006;75:610–6.
Zhu G, Xia H, Zhou H, Li J, Lu F, Liu Y, et al. Susceptibility of Anopheles sinensis to Plasmodium vivax in malarial outbreak areas of central China. Parasit Vectors. 2013;6:176.
Moreno M, Tong C, Guzman M, Chuquiyauri R, Llanos-Cuentas A, Rodriguez H, et al. Infection of laboratory-colonized Anopheles darlingi mosquitoes by Plasmodium vivax. Am J Trop Med Hyg. 2014;90:612–6.
Abduselam N, Zeynudin A, Berens-Riha N, Seyoum D, Pritsch M, Tibebu H, et al. Similar trends of susceptibility in Anopheles arabiensis and Anopheles pharoensis to Plasmodium vivax infection in Ethiopia. Parasit Vectors. 2016;9:552.
Chali W, Ashine T, Hailemeskel E, Gashaw A, Tafesse T, Lanke K, et al. Comparison of infectivity of Plasmodium vivax to wild-caught and laboratory-adapted (colonized) Anopheles arabiensis mosquitoes in Ethiopia. Parasit Vectors. 2020;13:120.
Kiattibutr K, Roobsoong W, Sriwichai P, Saeseu T, Rachaphaew N, Suansomjit C, et al. Infectivity of symptomatic and asymptomatic Plasmodium vivax infections to a southeast asian vector, Anopheles dirus. Int J Parasitol. 2017;47:163–70.
Timinao L, Vinit R, Katusele M, Koleala T, Nate E, Czeher C, et al. Infectivity of symptomatic malaria patients to Anopheles farauti colony mosquitoes in Papua New Guinea. Front Cell Infect Microbiol. 2021;11:771233.
Araujo MDS, Andrade AO, Dos Santos NAC, Castro RB, Pereira DB, Rodrigues MMS, et al. First observation of experimental Plasmodium vivax infection of three malaria vectors from the brazilian Amazon. Vector Borne Zoonotic Dis. 2020;20:517–23.
Bantuchai S, Imad H, Nguitragool W. Plasmodium vivax gametocytes and transmission. Parasitol Int. 2021;87:102497.
Ngernna S, Rachaphaew N, Thammapalo S, Prikchoo P, Kaewnah O, Manopwisedjaroen K, et al. Case series of human Plasmodium knowlesi infection on the southern border of Thailand. Am J Trop Med Hyg. 2019;101:1397–401.
Yorsaeng R, Saeseu T, Chotivanich K, Felger I, Wampfler R, Cui L, et al. Indigenous Plasmodium malariae infection in an endemic population at the Thai-Myanmar border. Am J Trop Med Hyg. 2019;100:1164–9.
Quest, Graph™. EC50 Calculator (v.1). https://www.aatbio.com/tools/ec50-calculator-v1%20.
Imwong M, Stepniewska K, Tripura R, Peto TJ, Lwin KM, Vihokhern B, et al. Numerical distributions of parasite densities during asymptomatic malaria. J Infect Dis. 2016;213:1322–9.
Tananchai C, Pattanakul M, Nararak J, Sinou V, Manguin S, Chareonviriyaphap T. Diversity and biting patterns of Anopheles species in a malaria endemic area, Umphang Valley, Tak Province, Western Thailand. Acta Trop. 2019;190:183–92.
Sattabongkot J, Maneechai N, Phunkitchar V, Eikarat N, Khuntirat B, Sirichaisinthop J, et al. Comparison of artificial membrane feeding with direct skin feeding to estimate the infectiousness of Plasmodium vivax gametocyte carriers to mosquitoes. Am J Trop Med Hyg. 2003;69:529–35.
Vallejo AF, Rubiano K, Amado A, Krystosik AR, Herrera S, Arevalo-Herrera M. Optimization of a membrane feeding assay for Plasmodium vivax infection in Anopheles albimanus. PLoS Negl Trop Dis. 2016;10:e0004807.
Gaillard FO, Boudin C, Chau NP, Robert V, Pichon G. Togetherness among Plasmodium falciparum gametocytes: interpretation through simulation and consequences for malaria transmission. Parasitology. 2003;127:427–35.
Lawniczak MK, Eckhoff PA. A computational lens for sexual-stage transmission, reproduction, fitness and kinetics in Plasmodium falciparum. Malar J. 2016;15:487.
Mendis KN, Munesinghe YD, de Silva YN, Keragalla I, Carter R. Malaria transmission-blocking immunity induced by natural infections of Plasmodium vivax in humans. Infect Immun. 1987;55:369–72.
Arevalo-Herrera M, Solarte Y, Rocha L, Alvarez D, Beier JC, Herrera S. Characterization of Plasmodium vivax transmission-blocking activity in low to moderate malaria transmission settings of the colombian Pacific coast. Am J Trop Med Hyg. 2011;84:71–7.
Peiris JS, Premawansa S, Ranawaka MB, Udagama PV, Munasinghe YD, Nanayakkara MV, et al. Monoclonal and polyclonal antibodies both block and enhance transmission of human Plasmodium vivax malaria. Am J Trop Med Hyg. 1988;39:26–32.
Abeles SR, Chuquiyauri R, Tong C, Vinetz JM. Human host-derived cytokines associated with Plasmodium vivax transmission from acute malaria patients to Anopheles darlingi mosquitoes in the peruvian Amazon. Am J Trop Med Hyg. 2013;88:1130–7.
Karunaweera ND, Carter R, Grau GE, Kwiatkowski D, Del Giudice G, Mendis KN. Tumour necrosis factor-dependent parasite-killing effects during paroxysms in non-immune Plasmodium vivax malaria patients. Clin Exp Immunol. 1992;88:499–505.
Naotunne TS, Karunaweera ND, Mendis KN, Carter R. Cytokine-mediated inactivation of malarial gametocytes is dependent on the presence of white blood cells and involves reactive nitrogen intermediates. Immunology. 1993;78:555–62.
Ranawaka MB, Munesinghe YD, de Silva DM, Carter R, Mendis KN. Boosting of transmission-blocking immunity during natural Plasmodium vivax infections in humans depends upon frequent reinfection. Infect Immun. 1988;56:1820–4.
Acknowledgements
The authors thank the field, insectary, molecular laboratory, and administrative staff of Mahidol Vivax Research Unit (MVRU), Faculty of Tropical Medicine, Mahidol University.
Funding
This research project is supported by Mahidol university (Basic Research Fund: Fiscal year 2022), Thailand Research Fund (TRG5880144), National Institute for Allergy and Infectious Diseases (R21 AI123934-01), and Korea Centers for Disease Control (NRIH-DMP2016-2017). TS was supported by a grant from the National Institute for Allergy and Infectious Diseases and the National Institute of Health (U19 AI089672).
Author information
Authors and Affiliations
Contributions
T.S. analysed data, performed experiments, wrote and edited the manuscript. P.S., C.K., C.S., and N.M. performed experiments. L.C. reviewed and edited the manuscript. J.S. supervised experiments and reviewed the manuscript. W.R. conceived the study, designed experiments, performed experiments, and edited the manuscript. W.N. conceived the study, analysed data, wrote and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Faculty of Tropical Medicine, Mahidol University (MUTM 2011-040-05). Informed consent was obtained from all participants before participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Surit, T., Sripoorote, P., Kumpitak, C. et al. Transmission efficiency of Plasmodium vivax at low parasitaemia. Malar J 22, 22 (2023). https://doi.org/10.1186/s12936-022-04435-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04435-9