Abstract
Background
Anopheles maculatus, Anopheles minimus and Anopheles dirus are the major vectors of malaria transmission in the Greater Mekong Subregion (GMS). The malaria burden in this region has decreased significantly in recent years as all GMS countries progress towards malaria elimination. It is necessary to investigate the Anopheles diversity and abundance status and assess the Plasmodium infection rates to understand the malaria transmission potential of these vector species in GMS countries to guide the development of up-to-date vector control strategies and interventions.
Methods
A survey of mosquitoes was conducted in Stung Treng, Sainyabuli and Phongsaly Provinces on the Cambodia-Laos, Thailand-Laos and China-Laos borders, respectively. Mosquito collection was done by overnight trapping at sentinel sites in each province. After morphological identification, the 18S rRNA-based nested-PCR was performed to detect malaria parasites in the captured Anopheles mosquitoes.
Results
A total of 18 965 mosquitoes comprising of 35 species of 2 subgenera (Subgenus Anopheles and Subgenus Cellia) and 4 tribes (Tribes Culicini, Aedini, Armigerini and Mansoniini) were captured. Tribe Culicini accounted for 85.66% of captures, followed by Subgenus Anopheles (8.15%). Anopheles sinensis dominated the Subgenus Anopheles by 99.81%. Plasmodium-infection was found in 25 out of the 1 683 individual or pooled samples of Anopheles. Among the 25 positive samples, 19, 5 and 1 were collected from Loum, Pangkhom and Siem Pang village, respectively. Eight Anopheles species were found infected with Plasmodium, i.e., An. sinensis, Anopheles kochi, Anopheles vagus, An. minimus, Anopheles annularis, Anopheles philippinensis, Anopheles tessellatus and An. dirus. The infection rates of Plasmodium falciparum, Plasmodium vivax and mixture of Plasmodium parasite species were 0.12% (2/1 683), 1.31% (22/1 683) and 0.06% (1/1 683), respectively.
Conclusions
Overall, this survey re-confirmed that multiple Anopheles species carry malaria parasites in the international border areas of the GMS countries. Anopheles sinensis dominated the Anopheles collections and as carriers of malaria parasites, therefore may play a significant role in malaria transmission. More extensive investigations of malaria vectors are required to reveal the detailed vector biology, ecology, behaviour, and genetics in GMS regions in order to assist with the planning and implementation of improved malaria control strategies.
Graphical Abstract

Similar content being viewed by others
Background
Currently, malaria remains one of the most life-threatening parasitic diseases in tropical and subtropical areas. According to the World Health Organization (WHO) World Malaria Report in 2021, there were approximate 241 million cases reported in 2020 in 85 malaria endemic countries. Twenty-nine of the 85 countries accounted for 96% of malaria cases globally, and Nigeria, the Democratic Republic of the Congo, Uganda, Mozambique, Angola and Burkina Faso alone accounted for about 55% of all cases globally [1]. In the WHO African Region, the number of estimated malaria cases in 2020 (228 million, accounted for about 95% of all cases) was higher than that in 2019 (215 million, accounted for about 94% of all cases), mainly because of disruptions to services during the COVID-19 pandemic [1].
The Greater Mekong Subregion (GMS) covers Cambodia, China's Yunnan Province, Lao People’s Democratic Republic (Lao PDR), Myanmar, Thailand and Vietnam [2, 3]: The region is still facing challenges in malaria elimination. The malaria situation in the GMS countries has greatly improved, which was evidenced by the continuous decline of annual malaria incidences [1, 4, 5]. The WHO South-East Asia Region accounted for about 2% of malaria cases globally in 2020, although malaria cases decreased by 78% from 23 million in 2000 to about 5 million in 2020 and malaria deaths by 75% from 35,000 in 2000 to 9,000 in 2020 [1]. Lao PDR has reduced malaria incidence significantly by over 75% between 2000 and 2015 [2]. The malaria positive rate was found as high as around 6.51% in 2007 in Cambodia [6], then the annual parasite incidence (API) in the country has declined steadily from 8 per 1,000 population in 2006 to 1 per 1,000 population in 2016 [7, 8]. In Thailand, the malaria incidence rate exhibited the most rapid reduction between 1965 and 2002, from 11.86% to 0.34% in the case of Plasmodium falciparum and 2.89% to 0.40% for Plasmodium vivax, respectively [9]. Similarly the annual parasite incidence decreased by 89% from 2.61 per 1, 00 to 0.28 per 1,000 between 2000 and 2016 [10]. In Myanmar, malaria deaths have decreased from 1,707 in 2005 to just 19 in 2018, and the incidence of reported malaria has fallen by 85% from 9.94 per 1,000 population in 2012 to 1.46 per 1,000 population in 2018 [11]. In Vietnam, malaria cases have sharply declined from 17,229 in 2010 to 4,813 in 2018 and malaria deaths fell from 21 in 2010 to 1 in 2018, with an almost 50% decrease in indigenous cases between 2015 and 2018 [12]. China was certified malaria-free by the World Health Organization on 30 June 2021. The indigenous cases declined from 1,308 in 2011 to 36 in 2015, and the last one P. vivax patient was reported from Yunnan Province in 2016. Since then, no indigenous malaria cases have been reported except the imported cases until now [13].
Vector control is one of the most important strategies in malaria control and elimination. It needs to be built on a thorough understanding of vector biology, ecology, behaviour, and genetics [14]. Successful integrated malaria control strategies rely on the better understanding of vector dynamics and distribution, the Plasmodium infection status of vector mosquitoes, insecticide resistance status, and the underlying causes of malaria transmission as well. In the GMS countries, malaria vectors are highly diverse in species composition and population dynamics [15,16,17]. Anopheles maculatus, Anopheles minimus and Anopheles dirus are the major vectors for malaria transmission. Anopheles dirus, An. minimus, Anopheles sundaicus and An. maculatus are dominant malaria vectors in Cambodia [3, 18], and An. dirus, An. maculatus and An. minimus in Laos [19,20,21,22,23]. Other potential vectors (including Anopheles nivipes, Anopheles philippinensis, Anopheles barbirostris, Anopheles lesteri, Anopheles annularis) for transmitting malaria in GMS regions had been long suspected [19, 20, 24]. Whereas Anopheles kochi plays a significant role in malaria transmission on the Bangladesh-Indian border, also acts as a potential vector of malaria transmission in Thailand [25,26,27]. In summary, the importance of each vector species in malaria transmission varies among these countries of GMS, because the influence of own different preferred ecological environments as well as geographical location. However, few studies have been performed to investigate the vectorial capability and ability of Anopheles mosquitoes in transmitting the malaria parasites in recent years. Hence, it is necessary to conduct surveys of Plasmodium infection among the vector species to provide valuable information for control and elimination of malaria in these regions.
Methods
Study sites
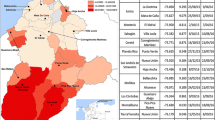
The study was conducted in July 2018 and from June to July 2019 at Siem Pang village in the Cambodian Siem Pang District of Stung Treng Province (14°20’N, 106°38’E) along the Cambodia-Laos border, and also Loum village in Thai Pak Lay Town of Sainyabuli Province (19°39’N, 101°82’E) along the Thailand-Laos border, and Pangkhom village in Lao Yot Ou District of Phongsaly Province (22°12’N, 101°79’E) along China-Laos border, respectively (Fig. 1). The sentinel sites for mosquito collection are 63.5, 689.7 and 398.6 m above sea level respectively, close to forested hillsides and adjacent to rice farming wetlands. Ten ethnic minorities with a total population of 25 348 in 2018 reside at Siem Pang village in the Siem Pang District. There are 666 local residents (Dai Ethnic Group, Flatland region) in 325 households in Loum village of Yot Ou District, and 1 210 local residents (Laotian Ethnic Group, Semi-mountainous area) in 127 households in Pangkhom village of Pak Lay Town, respectively, in 2019.
Mosquito collection and identification
Mosquitoes were collected by overnight trapping with battery-operated CDC light traps (Model 1012; John W. Hock Inc. USA). One light trap was installed each night at each monitoring site. The traps were set 1.5 m above the ground outdoor near cattle or pig sheds (C/PS), as well as indoor in human residences (rooms) (HR) with the house-owner’s permission, from 20:00 to 08:00 each day. A total of 70 light traps were established in the three villages. Out of the 70 light traps, 16 (4 nights for HR and C/PS), 36 (9 nights for HR and C/PS) and 18 (4 nights for HR and 5 nights for C/PS) were installed in Pangkhom, Loum and Siem Pang villages, respectively. In addition, human-baited double bed net traps (HDBNT) were set near the house, with one person resting on a bamboo bed covered by a untreated bed net. Mosquito collectors captured the adult mosquitoes between the nets at every 15 min internals from 19:00 to 6:00, using a battery-powered aspirator. All live adult mosquitoes were killed by freezing in a refrigerator, and subsequently classified based on sex, species and subgroup, following the standard procedures [28,29,30]. Each mosquito of the Anopheles spp. was placed individually in 2 ml cryovials containing 75% ethanol and taken to the Core Laboratory of Yunnan Institute of Parasitic Diseases for laboratory analyses as described below.
Genomic DNA extraction and PCR amplification
After morphological identification, the 18S rRNA-based nested-PCR was performed in Laboratory of Yunnan Institute of Parasitic Diseases, to detect malaria parasites in the captured Anopheles mosquitoes.
Genomic DNA was extracted from mosquitoes following the manufacturer’s instructions (QIAamp® DNA Mini Kit, Germany). For the mosquitoes which were collected at the same time in Yot Ou District of Phongsaly Province, either the whole body of individual mosquitoes or pools of ten mosquitoes of Anopheles sinensis and Anopheles vagus, were placed in 1.5 ml Eppendorf tubes and ground with pestles in 180 µl of buffer ATL. Then the genomic DNA was extracted following the tissue extraction protocol of manufacturer’s manual and preserved at -80℃ for subsequent PCR. However, for the fewer mosquitoes of Anopheles spp. were collected from the Siem Pang District of Stung Treng Province and Pak Lay Town of Sainyabuli Province, the whole body of individual mosquitoes were used for the Genomic DNA extraction.
The specific primers for molecular identification of Plasmodium spp. were designed as described previously [31, 32], based on 18S rRNA gene (Table 1). The rPLU5 and rPLU6 were genus-specific primers for 1st round PCR, while rPF1/2 and rPV1/2 were species-specific primers for detecting P. falciparum and P. vivax on 2nd round PCR, respectively. The reaction mixture (20 µl) contained 2.5 µl of 10 × buffer (500 mM KCl, 100 mM Tris–HCl (PH = 8.3) and 15 mM of MgCl2), 0.2 mM of dNTPs, 0.3 µM of each primer, 0.05 unit of Takara Taq (Dalian, China) and 2 µl of DNA for 1st round nested PCR or 1 µl of 1st round PCR product for 2nd round nested PCR. The amplification cycle was at 94 °C for 3 min, 34 cycles at 94 °C for 3 s, 58 °C for 30 s, 72 °C for 1 min, and 5 min at 72 °C for the final extension step [2]. One negative control (the sterile double-distilled water) and two positive controls (P. falciparum and P. vivax) were set in each experiment. The PCR products were detected by 2% agarose gel electrophoresis containing GoldView (Solarbio, China) and visualized under UV transillumination.
Statistical analysis
The mosquito population densities were obtained by calculating the mean number of mosquitoes collected by C/PS or HR per light per night. The formula for the calculation is: mosquito density (number/light·night) = No. of captured mosquitoes/(No. of CDC light traps*No. of captured nights).
The human-biting rates of Anopheles were obtained by calculating the mean number of captured Anopheles landing by HDBNT per person per hour. The formula for the calculation is: human-biting rates = No. of captured Anopheles landing/(No. of persons*No. of hours).
All statistical analyses were conducted with the software Statistical Package for Social Sciences (SPSS) version 23.0. The Kruskal–Wallis test was used to assess the different of the genus composition of captured mosquito vectors by each method in the sentinel sites, the different of the genus composition of captured mosquito vectors in each sentinel site between HR and C/PS methods, as well as the prevalence of the Plasmodium-positive mosquitoes between the sentinel sites. The Spearman's rank correlation coefficient test was calculated to assess the relationships in each sentinel site between the number of mosquitoes tested and Plasmodium-positive mosquitoes, respectively. The difference was considered statistically significant when P value was less than 0.05.
Results
Collection of mosquitoes
In total, 18 965 mosquitoes comprising of 35 species, two being in the genus Anopheles of 2 subgenera [Subgenus Anopheles (3 species), Subgenus Cellia (14 species)], 4 Tribes of Subfamily Culicinae [Tribe Culicini (8 species), Tribe Aedini (7 species), Tribe Armigerini (2 species) and Tribe Mansoniini (1 species)] were captured. The Tribe Culicini accounted for 85.66% (16 246/18 965) of mosquitoes captured, followed by Subgenus Anopheles 8.15% (1 545/18 965). Anopheles sinensis dominated the Subgenus Anopheles at 99.81% (1 542/1 545) of Anopheles captures (Additional file 1: Table S1).
A total of 18 520 adult mosquitoes were collected in Siem Pang, Loum and Pangkhom villages through overnight trapping with battery-operated CDC light traps and morphologically identified in the field. There were a statistical difference in genus composition of mosquito vectors for Siem Pang (X2 = 114.617; P = 0.000) and Loum (X2 = 32.364; P = 0.000) between the C/PS and HR methods, but no significant difference for Pangkhom (X2 = 3.333; P = 0.068) was found. The C/PS caught significantly more mosquitoes per light per night than HR in Siem Pang and Loum. The higher densities of captured mosquitoes of C/PS and HR were 772.83 and 157.78 mosquitoes per light per night in Loum village, followed by Siem Pang village (113.9 and 37.63) and Pangkhom village (28.38 and 12.88). These mosquitoes were classified into 2 Subfamilies (Anophelinae and Culicinae), 2 subgenera (Subgenus Anopheles, Subgenus Cellia), 4 Tribes (Tribe Aedini, Tribe Armigerini, Tribe Culicini and Tribe Mansoniini) and 34 species. The predominant genera were in the Tribe Culicini (8 species) and Subgenus Anopheles (2 species), which accounted for 85.59% (15 851/18 520) and 8.26% (1 530/18 520), respectively (Table 2). The genus composition of mosquito vectors differed significantly between the three sentinel sites, for HR (X2 = 22.733; P = 0.000) and C/PS (X2 = 1420.435; P = 0.000) respectively (Fig. 2). Culex tritaeniorhynchus of Tribe Culicini was the major species in Siem Pang, Loum and Pangkhom villages, accounting for 33.75% (486/1 440), 81.90% (13 719/16 751) and 41.95% (138/329), respectively. It is worth noting that Siem Pang village manifested a high prevalence of An. philippinensis (23.06%, 332/1 440), Culex fuscicephala (11.32%, 163/1 440) and Culex gelidus (10.63%, 153/1 440), whereas Loum and Pangkhom villages showed high prevalence of An. sinensis (9.08%, 1 521/16 751) and Cx. fuscicephala (6.41%, 1 073/16 751), as well as Armigeres subalbatus (26.44%, 87/329) and Aedes mediolineatus (6.69%, 22/329), respectively (Table 2).
Second, a total of 445 adult mosquitoes were collected by human-baited double bed net traps (HDBNT) for one night in Siem Pang and Loum villages. Overall 91.69% (408/445) of these mosquitoes were collected in Siem Pang and the fewer of 8.31% (37/445) in Loum, respectively. The human-biting rates of Anopheles were 1.82 and 1.55 mosquitoes per person per hour at Siem Pang and Loum village, respectively. The majority of Anopheles in Siem Pang and Loum were captured between 1:00 to 2:00 and 20:00–21:00, respectively. These mosquitoes were classified into 13 species and 2 subgenera (Subgenus Anopheles and Subgenus Cellia) and 3 Tribes (Tribe Aedini, Tribe Armigerini and Tribe Culicini) (Fig. 3). Similarly, high proportions of Tribe Culicini (88.76%, 395/445), Subgenus Cellia (4.94%, 22/445) and Subgenus Anopheles (3.37%, 15/445) (Additional file 1: Table S1) were observed. In Siem Pang village, the dominant mosquito species identified was Cx. tritaeniorhynchus (90.20%, 368/408), followed by An. dirus (3.68%, 15/408). In contrast, neither Cx. tritaeniorhynchus nor An. dirus mosquitoes were found in Loum village. The dominant mosquito species in Loum village were Cx. quinquefasciatus and An. sinensis, accounting for (45.95%, 17/37) and (37.84%, 14/37), respectively. The genus composition of mosquito vectors manifested significant difference between the two sentinel sites (X2 = 205.764; P = 0.000) (Fig. 3).
Observation on malaria parasite by nested PCR
The nested PCR was performed in collected Anopheles vectors to identify the sporozoite stages of malaria parasites. Out of 2 269 captured Anopheles mosquitoes, a total of 1 683 (1 344 An. sinensis, 161 An. vagus, 64 An. philippinensis, 42 An. tessellatus, 28 An. kochi, 23 An. dirus, 16 An. Maculatus, 4 An. minimus and 1 An. annularis) was tested. It was found that P. vivax predominated, 22 of these mosquitoes were positive for P. vivax, 2 for P. falciparum and 1 for co-infection (Table 3). The Loum village contributed the largest number of tested Anopheles mosquitoes (91.21%, 1 535/1 683), followed by Siem Pang village (8.08%, 136/1 683) and Pangkhom village (0.71%, 12/1 683). The higher malaria parasite rates (41.67%, 5/12) were found in Pangkhom village, the lower in Loum village (1.24%, 19/1 535) and Siem Pang village (0.74%, 1/136). Of the 25 samples of malaria positive mosquitoes, 19, 5 and 1 were collected from Loum, Pangkhom and Siem Pang village, respectively. The number of Anopheles species tested positive in Loum village was 4 [An. sinensis (0.52%, 7/1 340), An. minimus (75%, 3/4), An. kochi (60%, 3/5) and An. tessellatus (16.67%, 6/36)] and in Pangkhom village was 5 [An. sinensis (25%, 1/4), An. annularis (100%, 1/1), An. kochi (50%, 1/2), An. philippinensis (100%, 1/1) and An. vagus (33.33%, 1/3)]. One co-infection of P. falciparum and P. vivax was found in An. tessellatus collected from the Loum Village (Table 3). Only one An. dirus sample, collected from Siem Pang village of Stung Treng Province, was P. falciparum positive. The Anopheles species positive for Plasmodium in this study were An. sinensis accounting for 0.60% (8/1 344), An. vagus 0.62% (1/161), An. philippinensis 1.56% (1/64), An. dirus 4.35% (1/23, only in Siem Pang), An. kochi 14.29% (4/28) and An. minimus 75% (3/4, only in Loum), An. annularis 100% (1/1, only in Pangkhom) and An. tessellatus 14.29% (6/42, only in Pangkhom) (Table 3). Overall, the sporozoite rates of P. falciparum, P. vivax and co-infection in this study were 0.12% (2/1 683), 1.31% (22/1 683) and 0.06% (1/1 683), respectively. There was no significant difference in prevalence of the Plasmodium-positive mosquitoes between the sentinel sites (X2 = 0.210; P = 0.900). Additionally, no positive correlation between the number of mosquitoes tested and Plasmodium-positive mosquitoes for Siem Pang (Spearman’s rank coefcient = 0.393; P = 0.441), Loum (Spearman’s rank coefcient = 0.359; P = 0.553) and Pangkhom (Spearman’s rank coefcient = 0.417; P = 0.410), as well as between the total number of mosquitoes tested and Plasmodium-positive mosquitoes (Spearman’s rank coefcient = 0.418; P = 0.263), respectively.
Discussion
Despite the malaria situation in GMS countries having greatly improved in recent years through the implementation of the Mekong Malaria Elimination Programme, malaria remains a serious public health problem in forested and forest-fringe areas of these countries, especially along the international borders between the countries [33, 35, 37]. Malaria control in these areas is also beset with several technological and programmatic challenges (e.g. malaria vector surveillance, insecticide control of vector mosquitoes, ‘border malaria’ or malaria monitoring and control across international boundaries, multidrug resistance and artemisinin resistance monitoring) [3, 33,34,35,36,37,38].
The investigation of mosquito vectors in Stung Treng, Sainyabuli and Phongsaly Provinces of Cambodia-Laos, Thailand-Laos and China-Laos borders, respectively, revealed that more mosquitoes were collected by C/PS than HR method, and that Cx. tritaeniorhynchus of Tribe Culicini was found to be the dominant local species, which were the same as the results obtained in the southernmost counties/municipalities of Yunnan Province in China (Menglian and Jiangcheng counties in Simao Prefecture; Mengla and Menghai counties and Jinghong municipality in Xishuangbanna Prefecture) [39, 40], and Oudomxay, Louangphrabang, Phongsaly, Louang Namtha, Pocho and Champasak Provinces in Laos [15, 39, 41, 42]. The predominant malaria vector species were An. maculatus and An. philippinensis in Stung Treng Province, An. sinensis and An. vagus in Phongsaly Province, and An. sinensis and An. tessellatus in Sainyabuli Province, respectively. The other surveys found An. vagus in Champasak Province, Anopheles argyropus in 5 northernmost provinces in Laos, and An. sinensis in southernmost counties/municipalities of Yunnan Province of China. The reasons for these differences in species composition among regions could be the elevations, vegetation, different requirements for larval habitat and the pyrethroid insecticide used for vector control in local areas.
Anopheles maculatus, An. minimus and An. dirus are the major vectors of malaria transmission in the GMS regions [2, 3, 17, 43,44,45,46,47,48]. Anopheles kochi plays a significant role in malaria transmission on the Bangladesh-Indian border, as confirmed by the Plasmodium-positive specimens listed in previous studies [25,26,27], and An. kochi also acts as a potential vector of malaria transmission in Thailand [49,50,51], as the sporozoites of P. falciparum or P. vivax were identified in Thailand using the indirect fluorescent antibody (IFA) tests or enzyme-linked immunosorbent assays (ELISA) [50]. Plasmodium infection was found in a high number of Anopheles species (e.g. An. vagus, An. sinensis, An. kochi, An. minimus, An. annularis, An. philippinensis, An. tessellatus and An. dirus) in this investigation, which corroborates the similar results in previous studies [22, 42, 43, 45]. To explore the potential vector status of Anopheles mosquitoes in these regions, we listed the percentage of each Plasmodium-positive mosquito species in Asian countries (Additional file 2: Table S2). In the current study, 25 specimens of the above-mentioned Anopheles were Plasmodium-positive (2, 22 and 1 specimens infected with the P. falciparum, P. vivax and co-infection respectively) by nested-PCR, the co-infected sample was An. tessellatus mosquito collected from Phongsaly Province. The malaria parasite rate of An. sinensis, An. vagus, An. dirus, An. kochi and An. minimus were 0.60% (8/1 344), 0.62% (1/161), 4.35% (1/23, only for Stung Treng Province of Cambodia), 14.29% (4/28) and 75% (3/4, only for Phongsaly Province of Laos) respectively (Table 3), which were higher than the positive rates of An. minimus, An. vagus and An. kochi in Bangladesh [26], An. vagus and An. kochi in Indonesia [52], An. minimus, An. sinensis, An. vagus, An. dirus and An. kochi in Cambodia [53], An. minimus and An. dirus in Cambodia [54], An. dirus [22], An. kochi [42] and An. minimus [55] in Laos, An. minimus in Myanmar [56], An. minimus in 2011–2013 and 2013 [57, 58] as well as An. minimus and An. dirus in 2013–2015 [59] in Thailand and An. sinensis in Korea [60, 61], but lower than the An. sinensis in Laos [42]. Previous researches in Vietnam [54, 62], Cambodia [62], Laos [22] and Myanmar [46, 56] demonstrated that An. minimus and An. dirus are known vectors of Plasmodium sporozoites, whereas neither An. kochi nor An. sinensis was reported carrying sporozoites. Although cross-reacting antigen for Plasmodium has thus far not been shown using ELISA, it could potentially overestimate the entomological inoculation rate, particularly for P. falciparum transmission and when dealing with zoophilic species [27]. Durnez L [54] also confirmed a higher percentage of Plasmodium-positive in ELISA than that detected by PCR. According to the data of Additional file 2: Table S2, the Plasmodium-positive rates of An. minimus and An. dirus in Cambodia, and An. minimus in Vietnam have been decreased significantly with the passage of time, especially in Cambodia.
It is well-known that some of asymptomatic Plasmodium infections with lower parasite densities are undetectable by microscopy or RDTs [63]. If asymptomatic parasite carriers can be detected (through active case detection or passive case detection) and treated early, it would be especially beneficial to reduce or even interrupt malaria transmission. At the beginning of the twenty-first century, a high prevalence of asymptomatic malaria was present in GMS countries: In Laos, the parasite carriage rates were 20.4% and 31.1% by microscopy in the wet season and dry season respectively in Attapeu province during 2002–2004 [22], then decreased to 19.7% by ultra-sensitive quantitative (uPCR) in Savannakhet province of 2015 [63], 6.5% by PCR in Attapeu province of 2015 [64], as well as 7.63% and 7.91% by microscopy and nested PCR respectively in Phongsaly Province of 2016 [2]. A recent study revealed that extremely low prevalence of asymptomatic malaria infection (0.77% (39/5084)) occurred in the northern provinces (Phongsaly, Bokeo, Luang Prabang and Huaphanh Province) in 2016 [65]. In Cambodia, the parasite carriage rate was 11% by uPCR during 2013–2017 [66], but detected at a lower rate of 8.4% by nested real-time PCR in Ratanakiri province in 2016 [67] and 8.3% by PCR in Mondulkiri province from 2017 to 2018 [35]. In Thailand, the parasite carriage rate was 7.7% by PCR in Kanchanaburi Province in 2000 to 2002 [68], decreasing to 4.18% by PCR in Kanchanaburi and Ratchaburi provinces in 2012 [69], 2.45% (33/1 347) by quantitative PCR (qPCR) in Tak Province in 2012 to 2014 [70] as well as 0.52% (82/15 705) by PCR in Surat Thani in 2019 [36]. The parasite carriage rates have decreased significantly with the passage of time in South-East Asian countries. The above-mentioned parasite carriage rates were mainly for P. vivax-positive, except for the two studies in Attapeu province of Laos during 2002 to 2004 and Surat Thani province of Thailand in 2019 that indicated P. falciparum-positives. In our study reported here, 22 (88%, 22/25) of the positives in mosquitoes were P. vivax. Overall, P. vivax is now the major parasite contributing to malaria burden in the GMS countries and is possibly easier for people infected with it to become asymptomatic parasite carriers. At present, eliminating P. falciparum malaria is a top priority for the GMS countries. P. falciparum malaria is targeted to be eliminated by 2025, followed by elimination of all species by 2030 [71]. Therefore, sustained investigations are required to provide detailed understanding of asymptomatic parasite carriers in GMS regions in order to assist with the planning and implementation of improved malaria elimination strategies.
In conclusion, within the countries included in this study, the sentinel sites for mosquito collection were located near forested hillsides and adjacent to rice farming wetland. Malaria incidence in Lao PDR has significantly decreased by over 75% from 2000 to 2015 [2], while the annual parasite incidence (API) of Cambodia has steadily declined from 8 cases per 1000 population in 2006 to 1 case in 2016 [7, 8], and the API of Thailand decreased by 89% between 2000 and 2016 [10]. The number of P. falciparum cases decreased over time and P. vivax has become the dominant species [2, 22, 35, 63, 65,66,67,68,69,70]. In South-East Asia countries, the parasite carriage rates have decreased significantly with the passage of time. Multiple Anopheles mosquitoes have been reported carrying sporozoites in these regions [22, 25,26,27, 42, 46, 52,53,54,55,56,57,58,59,60,61,62], but the Plasmodium-positive rates of An. minimus and An. dirus in Cambodia and Vietnam decreased significantly over time. Furthermore, the importance of each vector species to malaria transmission varies greatly in these regions, due to different ecological settings as well as latitude and longitude of each region, as well as social settings. To accelerate towards elimination, GMS countries also need to focus on the proper management of the malaria cases or malaria treatment, especially cross-border malaria in the borderline areas without barriers, as well as vector control measures (about the vector biology, ecology and behaviour) to prevent the transmission of and relapses due to P. vivax in these regions.
Conclusion
Overall, this study re-confirmed that multiple Anopheles species carry malaria parasites in the international border areas of the GMS countries. Anopheles sinensis dominated the Anopheles and carried malaria parasites. However, more extensive investigations of malaria vectors are required to reveal the detailed vector biology, ecology, behaviour, and genetics in GMS regions in order to assist with the planning and implementation of improved malaria control strategies.
Availability of data and materials
Data supporting the conclusions of this article are included within the article. The raw datasets used and/or analyzed during this study are available from the corresponding author upon reasonable request.
Abbreviations
- GMS:
-
Greater mekong subregion
- Lao PDR:
-
Lao People’s Democratic Republic
- C/PS:
-
Cattle or pig sheds
- HDBNT:
-
Human-baited double bed net traps
- HR:
-
Human residences (rooms)
- ELISA:
-
Enzyme-linked immunosorbent assays
- IFA:
-
Indirect fluorescent antibody
- uPCR:
-
Ultra-sensitive quantitative PCR
- qPCR:
-
Quantitative PCR
- e.g.:
-
For example
References
WHO. World malaria report 2021. Geneva: World Health Organization; 2021. https://www.who.int/publications/i/item/9789240040496
Zhang C, Sorchampa S, Zhou H, Jiang J, Zhang Y. Survey of asymptomatic malaria and mosquito vectors in Muang Khua District of Phongsaly Province China-Laos Border. Int J Infect Dis. 2020;96:141–7.
Cui L, Yan G, Sattabongkot J, Cao Y, Chen B, Chen X, et al. Malaria in the greater mekong subregion: heterogeneity and complexity. Acta Trop. 2012;121:227–39.
WHO. World malaria report 2014. Geneva: World Health Organization; 2014. https://www.who.int/publications/i/item/9789241564830
WHO. World malaria report 2017. Geneva: World Health Organization; 2017. https://www.who.int/publications/i/item/9789241565523
Lek D, Menard D, Popovici J, Meek S, Socheat D, Rogers WO, et al. National malaria prevalence in Cambodia: microscopy versus polymerase chain reaction estimates. Am J Trop Med Hyg. 2016;95:588–94.
Kheang ST, Sovannaroth S, Barat LM, Dysoley L, Kapella BK, Po L, et al. Malaria elimination using the 1-3-7 approach: lessons from Sampov Loun Cambodia. BMC Public Health. 2020;20:544.
Por I, Sovannaroth S, Moran A, Dysoley L, Nguon S, Bunthy O, et al. Cost-effectiveness of malaria elimination in sampov loun operational District Cambodia. Malariaworld J. 2020;11:2.
Zhou G, Sirichaisinthop J, Sattabongkot J, Jones J, Cui L. Spatio-temporal distribution of Plasmodium falciparum and P. vivax malaria in Thailand. Am J Trop Med Hyg. 2005;72:256–62.
Sudathip P, Kongkasuriyachai D, Stelmach R, Bisanzio D, Sine J, Sawang S, et al. The investment case for malaria elimination in Thailand: a cost–benefit analysis. Am J Trop Med Hyg. 2019;100:1445–53.
Brown M, Bouanchaud P, Tesfazghi K, Phanalasy S, Thet MM, Nguyen H, et al. Motivation to test, treat, and report malaria cases: a quantitative assessment among private sector providers in the Greater Mekong Subregion. Malar J. 2022;21:82.
WHO. World malaria report 2019. Geneva: World Health Organization; 2019. https://www.who.int/publications/i/item/9789241565721
Huang F, Feng X-Y, Zhou S-S, Tang L-H, Xia Z-G. Establishing and applying an adaptive strategy and approach to eliminating malaria: practice and lessons learnt from China from 2011 to 2020. Emerg Microbes Infect. 2022;11:314–25.
Alout H, Yameogo B, Djogbenou LS, Chandre F, Dabire RK, Corbel V, et al. Interplay between Plasmodium infection and resistance to insecticides in vector mosquitoes. J Infect Dis. 2014;210:1464–70.
Wang J, Dong X, Guo X, Li C, Jiang J, Yang Z, et al. [Investigations on mosquito fauna and habitats in the north of Laos] (in Chinese). Chin J Vector Biol Control. 2016;27:549–54.
Socheath S, Seng C, RathTs DV, Deesin T, Apiwathanasorn C. Study on bionomics of principal malaria vectors in Kratie province, Cambodia. Southeast Asian J Trop Med Public Health. 2000;31(1):106–10.
Zhang C, Guo X, Yang R, Yang Y, Yang Z, Zheng Y, et al. [Evaluation on malaria hotspots in Yingjiang county of the China-Myanmar border area in 2015] (in Chinese). Chin J Parasitol Paras Dis. 2016;34:430–4.
Vantaux A, Samreth R, Piv E, Khim N, Kim S, Berne L, et al. Contribution to malaria transmission of symptomatic and asymptomatic parasite carriers in Cambodia. J Infect Dis. 2018;217:1561–8.
Meek SR. Vector control in some countries of Southeast Asia: comparing the vectors and the strategies. Ann Trop Med Parasitol. 1995;89:135–47.
Hii J, Rueda LM. Malaria vectors in the Greater Mekong Subregion: overview of malaria vectors and remaining challenges. Southeast Asian J Trop Med Public Health. 2013;44(1):73–165.
Toma T, Miyagi I, Okazawa T, Kobayashi J, Takakura M. Entomological surveys of malaria in Khammouane Province, Lao PDR, in 1999 and 2000. Southeast Asian J Trop Med Public Health. 2002;33:532–46.
Vythilingam I, Sidavong B, Chan ST, Phonemixay T, Vanisaveth V, Sisoulad P, et al. Epidemiology of malaria in Attapeu Province, Lao PDR in relation to entomological parameters. Trans R Soc Trop Med Hyg. 2005;99:833–9.
Suwonkerd W, Ritthison W, Ngo CT, Tainchum K, Chareonviriyaphap T. Vector biology and malaria transmission in Southeast Asia. In: Manguin S, editor. Anopheles mosquitoes—new insights into malaria vectors. London: IntechOpen; 2013. p. 2013.
Sinka ME, Bangs MJ, Manguin S, Chareonviriyaphap T, Patil AP, Temperley WH, et al. The dominant Anopheles vectors of human malaria in the Asia-Pacific region: occurrence data, distribution maps and bionomic précis. Parasit Vectors. 2011;4:89.
Al-Amin HM, Elahi R, Mohon AN, Kafi MA, Chakma S, Lord JS, et al. Role of underappreciated vectors in malaria transmission in an endemic region of Bangladesh-India border. Parasit Vectors. 2015;8:195.
Alam MS, Chakma S, Khan WA, Glass GE, Mohon AN, Elahi R, et al. Diversity of anopheline species and their Plasmodium infection status in rural Bandarban. Bangladesh Parasit Vectors. 2012;5:150.
Bashar K, Tuno N, Ahmed TU, Howlader AJ. False positivity of circumsporozoite protein (CSP)-ELISA in zoophilic anophelines in Bangladesh. Acta Trop. 2013;125:220–5.
Dong X, Zhou H, Gong Z. The mosquito fauna of Yunnan. London: Yunnan Science and Technology Press; 2010.
Baolin Lu. Fauna of China, Class Insecta, Diptera, Family Mosquito, vol. 1. Beijing: Beijing Science Press; 1997. (in Chinese).
Baolin Lu. Fauna of China, Class Insecta, Diptera, Family Mosquito, vol. 2. Beijing: Beijing Science Press; 1997. (in Chinese).
Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. 1993;61:315–20.
Perandin F, Manca N, Calderaro A, Piccolo G, Galati L, Ricci L, et al. Development of a real-time PCR assay for detection of Plasmodium falciparum, Plasmodium vivax, and Plasmodium ovale for routine clinical diagnosis. J Clin Microbiol. 2004;42:1214–9.
Delacollette C, D’Souza C, Christophel E, Thimasarn K, Abdur R, Bell D, et al. Malaria trends and challenges in the greater mekong subregion. Southeast Asian J Trop Med Public Health. 2009;40:674–91.
Socheat D, Denis MB, Fandeur T, Zhang Z, Yang H, Xu J, et al. Mekong malaria. II. Update of malaria, multi-drug resistance and economic development in the Mekong region of Southeast Asia. Southeast Asian J Trop Med Public Health. 2003;34(4):1–102.
Sandfort M, Vantaux A, Kim S, Obadia T, Pepey A, Gardais S, et al. Forest malaria in Cambodia: the occupational and spatial clustering of Plasmodium vivax and Plasmodium falciparum infection risk in a cross-sectional survey in Mondulkiri province. Cambodia Malar J. 2020;19:413.
Shimizu S, Chotirat S, Dokkulab N, Hongchad I, Khowsroy K, Kiattibutr K, et al. Malaria cross-sectional surveys identified asymptomatic infections of Plasmodium falciparum, Plasmodium vivax and Plasmodium knowlesi in Surat Thani, a southern province of Thailand. Int J Infect Dis. 2020;6:445–51.
Tsuboi T, Edwards HM, Canavati SE, Rang C, Ly P, Sovannaroth S, et al. Novel cross-border approaches to optimise identification of asymptomatic and artemisinin-resistant Plasmodium infection in mobile populations crossing Cambodian borders. PLoS ONE. 2015;10: e0124300.
Thomson R, Sochea P, Sarath M, MacDonald A, Pratt A, Poyer S, et al. Rubber plantations and drug resistant malaria: a cross-sectional survey in Cambodia. Malar J. 2019;18:379.
Wang J, Jiang J, Guo X, Zeng X, Sun X, Yang Z, et al. Analysis of community composition and geographical niche of mosquitoes in China-Laos border (in Chinese). Chin J Vect Biol Control. 2017;28:209–15.
Xie L, Lin A, Wang J, Chao Wu, Luo Y, Aishui Yu, et al. An investigation of mosquitoes and mosquito-borne pathogens in the southwest border regions of Yunnan province, China (in Chinese). Chin J Vect Biol Control. 2019;30:264–7.
Sorchampa S, Guo X, Wang J, Zhou H. Investigation of mosquito species in Muangsing county of Luangnamtha ptovince, Lao PDR] (in Chinese). Chin J Vector Biol Control. 2017;28:66–8.
Wang W, Yang R, Luo C, Guo X, Jiang J, Zhou H, et al. Investigation on species and sporozoite rate of Anopheles spp in Champasak Province of Laos (in Chinese). Chin J Parasitol Paras Dis. 2018;36:56–60.
Sriwichai P, Samung Y, Sumruayphol S, Kiattibutr K, Kumpitak C, Payakkapol A, et al. Natural human Plasmodium infections in major Anopheles mosquitoes in western Thailand. Parasit Vect. 2016;9:17.
Manh CD, Beebe NW, Van V, Tao LQ, Cooper RD. Vectors and malaria transmission in deforested, rural communities in north-central Vietnam. Malar J. 2010;9:259.
Vythilingam I, Phetsouvanh R, Keokenchanh K, Yengmala V, Hakim SL. The prevalence of Anopheles (Diptera: Culicidae) mosquitoes in Sekong Province, Lao PDR in relation to malaria transmission. Trop Med Int Health. 2010;8:525–35.
Zhou X, Shi W, Zhang Y, Zhou X, Hu L, Wang X, Wang J. [Distribution of Anopheles minimus and its role in malaria transmission in the Kachin Region of Myanmar] (in Chinese). J Pathog Biol. 2010;5:578–84.
Tananchai C, Pattanakul M, Nararak J, Sinou V, Manguin S, Chareonviriyaphap T. Diversity and biting patterns of Anopheles species in a malaria endemic area, Umphang Valley, Tak Province, western Thailand—ScienceDirect. Acta Trop. 2019;190:183–92.
Chareonviriyaphap T, Prabaripai A, Bangs MJ, Aum-Aung B. Seasonal abundance and blood feeding activity of Anopheles minimus Theobald (Diptera: Culicidae) in Thailand. J Med Entomol. 2003;40:876–81.
Sithiprasasna R, Jaichapor B, Chanaimongkol S, Khongtak P, Lealsirivattanakul T, Tiang-Trong S, et al. Evaluation of candidate traps as tools for conducting surveillance for Anopheles mosquitoes in a malaria-endemic area in western Thailand. J Med Entomol. 2004;41:151–7.
Rosenberg R, Andre RG, Somchit L. Highly efficient dry season transmission of malaria in Thailand. Trans R Soc Trop Med Hyg. 1990;84:22–8.
Somboon P, Suwonkerd W, Lines JD. Susceptibility of Thai zoophilic Anophelines and suspected malaria vectors to local strains of human malaria parasites Southeast Asian. J Trop Med Public Health. 1994;25:766–70.
St Laurent B, Burton TA, Zubaidah S, Miller HC, Asih PB, Baharuddin A, et al. Host attraction and biting behaviour of Anopheles mosquitoes in South Halmahera. Indonesia Malar J. 2017;16:310.
Vantaux A, Riehle MM, Piv E, Farley EJ, Chy S, Kim S, et al. Anopheles ecology, genetics and malaria transmission in northern Cambodia. Sci Rep. 2021;11:6458.
Durnez L, Van Bortel W, Denis L, Roelants P, Veracx A, Trung HD, et al. False positive circumsporozoite protein ELISA: a challenge for the estimation of the entomological inoculation rate of malaria and for vector incrimination. Malar J. 2011;10:195.
Marcombe S, Maithaviphet S, Bobichon J, Phommavan N, Nambanya S, Corbel V, et al. New insights into malaria vector bionomics in Lao PDR: a nationwide entomology survey. Malar J. 2020;19:396.
Shi W, Zhou X, Zhang Y, Zhou X, Hu L, Wang X, et al. [Investigation on malaria vectors in western part of China-Myanmar border] (in Chinese). Chin J Parasitol Paras Dis. 2011;29:134–7.
Tainchum K, Ritthison W, Chuaycharoensuk T, Bangs MJ, Manguin S, Chareonviriyaphap T. Diversity of Anopheles species and trophic behavior of putative malaria vectors in two malaria endemic areas of northwestern Thailand. J Vector Ecol. 2015;39:424–36.
Kwansomboon N, Chaumeau V, Kittiphanakun P, Cerqueira D, Corbel V, Chareonviriyaphap T. Vector bionomics and malaria transmission along the Thailand-Myanmar border: a baseline entomologic. J Vector Ecol. 2017;42:84–93.
Chaumeau V, Fustec B, Nay Hsel S, Montazeau C, Naw Nyo S, Metaane S, et al. Entomological determinants of malaria transmission in Kayin state, Eastern Myanmar: A 24-month longitudinal study in four villages. Wellcome Open Res. 2019;3:109.
Lee HW, Shin EH, Cho SH, Lee HI, Kim CL, Lee WG, et al. Detection of vivax malaria sporozoites naturally infected in Anopheline mosquitoes from endemic areas of northern parts of Gyeonggi-do (Province) in Korea. Korean J Parasitol. 2002;40:75–81.
Oh SS, Hur MJ, Joo GS, Kim ST, Go JM, Kim YH, et al. Malaria vector surveillance in Ganghwa-do, a malaria-endemic area in the Republic of Korea. Korean J Parasitol. 2010;48:35–41.
Trung HD, Van Bortel W, Sochantha T, Keokenchanh K, Quang NT, Cong LD, et al. Malaria transmission and major malaria vectors in different geographical areas of Southeast Asia. Trop Med Int Health. 2004;9:230–7.
Phommasone K, Adhikari B, Henriques G, Pongvongsa T, Phongmany P, von Seidlein L, et al. Asymptomatic Plasmodium infections in 18 villages of southern Savannakhet Province, Lao PDR (Laos). Malar J. 2016;15:296.
Iwagami M, Keomalaphet S, Khattignavong P, Soundala P, Lorphachan L, Matsumoto-Takahashi E, et al. The detection of cryptic Plasmodium infection among villagers in Attapeu province Lao PDR. PLoS Negl Trop Dis. 2017;11: e0006148.
Lover AA, Dantzer E, Hongvanthong B, Chindavongsa K, Welty S, Reza T, et al. Prevalence and risk factors for asymptomatic malaria and genotyping of glucose 6-phosphate (G6PD) deficiencies in a vivax-predominant setting, Lao PDR: implications for sub-national elimination goals. Malar J. 2018;17:218.
von Seidlein L, Peerawaranun P, Mukaka M, Nosten FH, Nguyen T-N, Hien TT, et al. The probability of a sequential Plasmodium vivax infection following asymptomatic Plasmodium falciparum and P. vivax infections in myanmar, vietnam, cambodia, and laos. Malar J. 2019;18:449.
Durnez L, Pareyn M, Mean V, Kim S, Khim N, Menard D, et al. Identification and characterization of areas of high and low risk for asymptomatic malaria infections at sub-village level in Ratanakiri. Cambodia Malar J. 2018;17:27.
Coleman RE, Sattabongkot J, Promstaporm S, Maneechai N, Tippayachai B, Kengluecha A, et al. Comparison of PCR and microscopy for the detection of asymptomatic malaria in a Plasmodium falciparum/vivax endemic area in Thailand. Malar J. 2006;5:121.
Nguitragool W, Mueller I, Kumpitak C, Saeseu T, Bantuchai S, Yorsaeng R, et al. Very high carriage of gametocytes in asymptomatic low-density Plasmodium falciparum and P. vivax infections in western Thailand. Parasit Vectors. 2017;10:512.
Baum E, Sattabongkot J, Sirichaisinthop J, Kiattibutr K, Jain A, Taghavian O, et al. Common asymptomatic and submicroscopic malaria infections in Western Thailand revealed in longitudinal molecular and serological studies: a challenge to malaria elimination. Malar J. 2016;15:333.
WHO. Strategy for Malaria Elimination in the Greater Mekong Subregion (2015–2030). Geneva: World Health Organization, 2015. https://www.who.int/publications/i/item/9789290617181
Acknowledgements
We greatly thank all the participating staff of Yunnan Institute of Parasitic Diseases in China, the Centre for Malaria Parasitology and Entomology (CMPE), Phonsaly and Sainyabuli health department as well as Department of Communicable Disease Control of the Ministry of Health in Laos, SREA SAMBO and SIEM PANG Hospital in Siem Pang District of Stung Treng Province, Provincial Health Department of Stung Treng as well as National Center for Parasitology, Entomology & Malaria Control in Cambodia who participated in sampling and data collection. We are also grateful to Dr. Phoutnalong Vilay, Dr. Rin Ravuth and Chunfu Li for participating in fieldwork.
Funding
This study was supported by the National Natural Science Foundation of China (Grant number 31601002, 81160357, 30960327, 30660160, U1902211), Yunnan Provincial Collaborative Innovation Center for Public Health and Disease Prevention and Control (Grant number 2014YNPHXT03) and the China-ASEAN Public Health Cooperation Fund and Joint Control of Malaria and Dengue in Lancang-Mekong River Area.
Author information
Authors and Affiliations
Contributions
Mosquito collection and identification: CLZ, RY, LBW and CHL. Data collection: CLZ, RY, LBW, CHL, YMY, YD, JW, YL and HNZ. Data and statistical analysis and manuscript preparation: CLZ, RY and YMY. Experimental work: CLZ, YD, JW and YL. Procurement of funding: YMY and HNZ. Study conception/design and critical review of the manuscript: CLZ, YMY and HNZ. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Genus/Species compositions of Anopheles mosquitoes trapped by the different methods in Siem Pang, Loum and Pangkhom villages.
Additional file 2: Table S2.
The percentage of mosquitoes with Plasmodium-positive by the different methods in Asian countries.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, C., Yang, R., Wu, L. et al. Survey of malaria vectors on the Cambodia, Thailand and China-Laos Borders. Malar J 21, 399 (2022). https://doi.org/10.1186/s12936-022-04418-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04418-w