Abstract
As parasites, Plasmodium species depend upon their host for survival. During the blood stage of their life-cycle parasites invade and reside within erythrocytes, commandeering host proteins and resources towards their own ends, and dramatically transforming the host cell. Parasites aptly avoid immune detection by minimizing the exposure of parasite proteins and removing themselves from circulation through cytoadherence. Erythrocytic disorders brought on by host genetic mutations can interfere with one or more of these processes, thereby providing a measure of protection against malaria to the host. This review summarizes recent findings regarding the mechanistic aspects of this protection, as mediated through the parasites interaction with abnormal erythrocytes. These novel findings include the reliance of the parasite on the host enzyme ferrochelatase, and the discovery of basigin and CD55 as obligate erythrocyte receptors for parasite invasion. The elucidation of these naturally occurring malaria resistance mechanisms is increasing the understanding of the host-parasite interaction, and as discussed below, is providing new insights into the development of therapies to prevent this disease.
Similar content being viewed by others
Background
The clinical symptoms of malaria occur during the blood stage of Plasmodium’s life cycle. Safely ensconced within the host erythrocyte, parasites develop and replicate whilst concealing their presence from the immune system. After consuming the contents of the host cell, and growing and multiplying to fill the available space, the progeny egress as merozoites, and, after briefly existing extracellularly, invade fresh erythrocytes, continuing the cycle of growth and proliferation. This cycle depends on an elaborate interplay between host and parasite proteins, which has been meticulously established over thousands of years of co-evolution. As such, any perturbations to the composition or arrangement of proteins in the host erythrocyte can potentially impede the parasite’s growth and survival, and thereby increase the resistance of the host to infection. Indeed, abnormalities of the erythrocyte are relatively common, especially in populations residing in malaria-endemic regions, consistent with the positive selection for these conditions. The mechanistic basis for protection against malaria is partly understood in some abnormalities; parasite invasion and intraerythrocytic development are often affected. However, recent studies have revealed a more complex picture, with many conditions sharing multiple and over-lapping pathways that advantage the host. The understanding of the parasite-erythrocyte interaction is also being challenged as novel and highly intimate relationships between the parasite and its host cell are discovered. This review will summarize the current knowledge regarding Plasmodium’s interaction with abnormal host erythrocytes, the mechanisms by which these abnormalities can inhibit the blood stage of Plasmodium’s life cycle, and the implications of these findings for malaria treatment.
Genetic erythrocyte abnormalities and malaria susceptibility
Erythrocytes have a limited lifespan (120 days in humans) and, therefore, must be continually replenished in a process known as erythropoiesis. In this process haematopoietic stem cells replicate and differentiate into erythroblasts, and following expulsion of their nucleus and most organelles, develop into reticulocytes. Reticulocytes are released from the bone marrow into the bloodstream and following further depletion of organelles and intracellular RNA, become mature erythrocytes. There are a number of erythrocyte disorders that result from mutations in the genes expressed during erythropoiesis; many are highly prevalent, particularly in populations with a long history of malaria exposure. It was first observed nearly 70 years ago that people with ‘sickled’ erythrocytes were less likely to suffer from malaria [1]. This condition is common in various West and Central African ethnicities. Now known as sickle cell trait, this and many other erythrocytic disorders, have been strongly associated with reduced malaria susceptibility. In fact, mutations causing erythrocyte abnormalities are the most commonly observed genetic traits in humans [2]. Genetic mutations associated with malaria resistance have been extensively reviewed previously [3–5]; a summary of known erythrocytic genetic disorders and their association with malaria susceptibility is given in Table 1.
Mechanisms by which erythrocyte abnormalities protect against malaria
Early studies towards identifying malaria protective mechanisms imparted by erythrocyte abnormalities largely focussed on the ability of the parasite to invade and grow within erythrocytes. These studies were facilitated by an in vitro culturing system for Plasmodium falciparum, which allowed researchers to easily compare between erythrocytes obtained from subjects with various genetic conditions. As the understanding of malaria pathogenesis was expanded, the importance of factors such as cytoadherence and the ability of the immune system to detect parasitized erythrocytes was also recognized. Studies then addressed how erythrocyte abnormalities could affect not only parasite invasion and growth under in vitro conditions, but also their effects in vivo, and how this may influence host resistance to malaria infection. This review considers how specific erythrocyte abnormalities affect four distinct features of the parasite-host interaction. Namely, merozoite invasion, parasite growth, cytoadherence, and erythrocyte senescence.
Merozoite invasion of the erythrocyte
The brief interval between parasite egress and reinvasion of a new erythrocyte has long been considered a potential weak point in its blood stage lifecycle. In vitro studies have shown that P. falciparum merozoites are exposed for approximately 2 min from egress to reinvasion, while the actual invasion event is completed in less than 30 s [6]. During this period the parasite is particularly susceptible to host recognition and attack mechanisms, due to the potential for direct contact with opsonins and immune cells; the parasite also becomes nonviable if it fails to invade a new cell [7]. Consequently, any disruption to the invasion pathway is beneficial to the host, and several abnormalities are known to directly affect this process.
There are several well-characterized genetic mutations in erythrocyte membrane proteins that are associated with impaired merozoite invasion. For example, African populations carry a highly prevalent single nucleotide polymorphism (SNP) in the promoter region controlling expression of the Duffy antigen receptor for chemokines gene (DARC or Duffy; rs2814778). The SNP prevents erythrocytic expression and results in the Duffy-negative blood phenotype [8]. Duffy is a ligand for a P. vivax merozoite protein called the Duffy-binding protein (PvDBP) and the Duffy-PvDBP interaction is essential for merozoite invasion of the erythrocyte [9, 10]. Therefore, Duffy-negative individuals are protected against Plasmodium vivax infection and in areas of Africa with a high incidence of this SNP, P. vivax infection is virtually non-existent [11, 12]. In contrast P. vivax is common in other malaria endemic areas where populations do not carry this polymorphism (Asia and South America) [12, 13]. However, complete protection due to this polymorphism has been questioned recently by observations of P. vivax infection in Duffy negative individuals in several studies [14–16]. In contrast to P. vivax, P. falciparum merozoites utilize several redundant invasion pathways and different host ligands. In 1977, Miller et al. [17] reported that erythrocytes from individuals with the rare En (a−) mutation were resistant to P. falciparum merozoite invasion. En (a−) erythrocytes lack Glycophorin A (GYPA), highlighting a possible role for this protein as a parasite ligand. Indeed, GYPA is now known to be a binding partner of P. falciparum erythrocyte binding antigen 175 (PfEBA-175) [18, 19], and more recently, was found to bind to merozoite surface protein 1 (PfMSP1) [20]. In the later study, the erythrocyte surface band 3-GYPA complex was shown to be essential for invasion by both P. falciparum and the rodent malaria parasite, Plasmodium yoelii. Mutations in other erythrocyte glycophorins (GYPB and GYPC) are common in endemic malaria populations, and recent studies have demonstrated comparable importance for these proteins in parasite invasion. The P. falciparum protein erythrocyte-binding ligand-1 (PfEBL-1) binds to GYPB [21, 22], while GYPC is a receptor for erythrocyte binding antigen 140 (PfEBA-140) [23]. Antibodies against the binding domains of both PfEBL-1 and PfEBA-140 inhibit merozoite invasion, while erythrocytes deficient in either GYPB (blood group S-s-U-), or GYPC (Gerbich negativity) are resistant to invasion [21–24]. Erythrocyte expressed complement receptor 1 (CR1) is also a demonstrated receptor for the P. falciparum merozoite protein PfRh4, with antibodies against CR1, as well as soluble CR1 protein, preventing invasion [25, 26]. This may partially explain the enhanced malaria resistance exhibited by individuals with inherited mutations resulting in CR1 deficiency [27]. Recently, two high throughput screening approaches were developed to identify novel host binding partners of merozoite proteins involved in invasion. The first utilized the Avidity-based extracellular interaction screen (AVEXIS) to identify binding interactions between erythrocyte and merozoite proteins [28]. This led to the discovery of a single definitive interaction between the host protein basigin and P. falciparum reticulocyte-binding protein homologue 5 (PfRH5). Antibody blocking studies demonstrated that this interaction is essential for invasion by all P. falciparum strains tested to date [28, 29], and erythrocytes expressing naturally occurring mutations in basigin (known as the Ok blood group antigen) also prevented parasite invasion [28]. This host-parasite receptor ligand interaction also appears to be important in clinical disease based on the findings that naturally acquired antibodies to PfRH5 are associated with improved outcomes to infection [30]. Another screening approach has utilized in vitro differentiated human erythroid cells in conjunction with short hairpin RNA (shRNA) libraries to target and screen for erythroid-expressed proteins necessary for P. falciparum merozoite invasion. As well as corroborating a requirement for basigin and CR1 in invasion, a novel interaction involving erythrocyte CD55, also known as Decay accelerating factor (DAF), was found to be essential for the invasion process. The requirement for this interaction was confirmed utilizing naturally-occurring CD55 null erythrocytes, which were refractory to invasion by several P. falciparum strains, including clinical isolates [31]. Interestingly, polymorphisms in CD55 are enriched in populations with historical exposure to malaria [32, 33], indicating a possible selection pressure on this gene. Importantly, the identification of host cell receptor-parasite ligand interactions has produced several possible targets for vaccine or therapeutic development.
The erythrocyte membrane is supported by an underlying network of proteins called the cytoskeleton, which provides the cell with structure and deformability, and serves as an anchoring point for membrane proteins. Hereditary elliptocytosis and hereditary spherocytosis are conditions caused by mutations in genes encoding cytoskeletal proteins, including alpha spectrin, beta spectrin, ankyrin, band 3 and protein 4.1, which affect molecule conformation or abundance. Mutations in genes encoding some of these proteins have been associated with increased protection against infection or severe forms of malaria. A well-known example is Southeast Asian ovalocytosis (SAO), which is caused by mutations in the gene encoding band 3. Band 3 is a transmembrane protein that normally exists as a dimer or tetramer and interacts with both the cytoskeleton and cell membrane; it also functions as an anion transporter. In SAO, mutations disrupt the anion transporter activity and result in the formation of large-sized aggregates [34–36], resulting in increased cell membrane rigidity [37–39], oval shaped cell morphology, reduced band 3 mobility in the membrane [40–42], and decreased expression of surface antigens [43, 44]. Homozygous inheritance of SAO-causing band 3 mutations results in embryonic lethality, however heterozygosity is associated with a marked protection against severe P. falciparum malaria, particularly cerebral malaria [45, 46]. Despite the fitness cost, frequencies of these mutations are remarkably high some populations, particularly those residing in Papua New Guinea [47]. There is strong evidence that P. falciparum merozoite invasion of SAO erythrocytes is impaired, which could plausibly explain the reduced malaria susceptibility conveyed by this condition [37, 39, 48, 49]. Mechanistic explanations variously include increased membrane rigidity, direct interference with parasite/band 3 binding [37–39, 50, 51], a loss or reduction of merozoite ligands, such as GYPA (which forms a complex with band 3) [20, 43, 44], and reduced band 3 mobility [52, 53]. Interestingly, cells with artificially inhibited band 3 mobility also exhibit reduced rates of merozoite invasion [53]. Erythrocytes from patients with other forms of hereditary elliptocytosis and spherocytosis have shown more variable, and sometimes inconsistent effects on parasite invasion. Erythrocytes deficient in protein 4.1 are reported to be less vulnerable to parasite invasion [54], which could possibly be explained by a secondary deficiency of GYPC (90% less in protein 4.1 deficient cells), although the role of GYPC as a parasite ligand was not investigated in this study. Utilizing a recently developed method for measuring merozoite invasion in vivo [55, 56], a study in mice carrying a mutation in ankyrin-1 (Ank1) reported reduced rates of erythrocyte invasion by Plasmodium chabaudi merozoites; this coincides with increased resistance and reduced parasitaemia reported in these mice [57]. Investigations of hereditary spherocytosis caused by mutations in alpha spectrin have also reported reduced merozoite invasion [58], however these studies are contradictory and the exact effects of these conditions remain inconclusive [59].
Overall, the disruption of parasite invasion is an obvious and testable mechanism by which erythrocyte disorders can protect the host against malaria infection. This is most evident for mutations that disrupt a specific parasite-erythrocyte binding interaction. Erythrocytes with structural abnormalities, such as spherocytosis and ovalocytosis, may also present the merozoite with a less than ideal substrate for invasion, however the mechanisms are difficult to establish, and findings are less consistent.
Intraerythrocytic growth
After gaining entry into an erythrocyte the Plasmodium parasite must dramatically remodel the host cell cytoplasm and membrane in order to grow, replicate, and eventually egress. The success of the parasite at this stage depends on several factors; the ability to digest haemoglobin, establishment of pathways to import nutrients, export waste products and traffic synthesized proteins around the cell, scavenging of host proteins, and, finally, effective dissolution of the cell membrane during egress.
There are five types of haemoglobinopathies found at high frequencies in both extant and historically malaria afflicted populations, and each has been implicated to varying degrees in perturbing the intraerythrocytic development and growth of Plasmodium. Three of these involve single amino acid substitutions in the beta globin chain of haemoglobin; sickle cell (HbS, β6Glu to Val, rs334), haemoglobin C (HbC, β6Glu to Lys, rs33930165), and haemoglobin E (HbE, β26Glu to Lys, rs33950507). The remaining two types of haemoglobinopathies, alpha and beta thalassaemia, arise due to reduced expression of the alpha and beta globin chains of haemoglobin, respectively, caused by various polymorphisms in the genes encoding these proteins. Impaired parasite growth in these cells (here defined specifically as the ability of an individual parasite to grow, replicate and produce new viable merozoites) has been frequently reported, although studies are often contradictory (for review see Taylor et al. [60]). An impairment in parasite growth has been consistently observed in homozygous haemoglobin C (HbCC) erythrocytes [61–63], which is proposed to be caused by spontaneous degradation of parasites in a subset of damaged mutant cells with an increased haemoglobin concentration [63]. Parasite growth is also impaired in homozygous haemoglobin E (HbEE) erythrocytes [64]. Two early studies by Friedman et al. [61, 65] indicated a role for oxygen tension in parasite growth in heterozygous HbS (HbAS or sickle cell trait), homozygous HbS (HbSS or sickle cell disease), alpha thalassaemia trait, and beta thalassaemia minor. Under low oxygen tension parasitized HbAS and HbSS cells underwent sickling and growth was attenuated. Conversely, in thalassaemic cells growth impairment occurred only under high oxygen tension. In the more severe form of alpha thalassaemia, known as haemoglobin H (HbH), a growth impairment has been consistently observed, however the mechanism remains unknown [66, 67]. More recent studies have suggested two novel mechanisms of parasite growth impairment in haemoglobinopathies. A study by Cyrklaff et al. [68] describes a process whereby host actin filaments are utilized by the parasite in developing Maurer’s clefts. In HbAS and heterozygous haemoglobin C (HbAC) cells, host actin filaments are dispersed further into the erythrocyte cytosol and are significantly longer than in normal cells, consequently, during remodelling by the parasite they fail to support the formation of normal Maurer’s clefts. The authors suggest this may be due to interference from oxidized forms of haemoglobin present in these cells, known as haemichromes. More recently, studies using a conditional protein export system indicated that the trafficking of parasite proteins across the parasitophorous vacuole is delayed and occurs at a slower rate in HbAS, HbAC, and HbCC erythrocytes, leading to reduced levels of parasite proteins in the erythrocyte cytosol and membrane [69]. Another study by La Monte et al. [70] proposes an entirely different mechanism whereby specific host micro RNAs, which are more abundant in HbAS and HbSS cells, are translocated into the parasite and fuse with parasite mRNA, inhibiting normal translation of parasite proteins. While the potential role of parasite protein trafficking and micro RNA in HbE and thalassaemia has not been investigated, it seems quite plausible that these may be a common mechanism explaining the reduced malaria susceptibility provided by these erythrocyte disorders.
Plasmodium falciparum growth is also impaired in spherocytotic and elliptocytotic erythrocytes. Schulman et al. [59] report that the degree of growth impairment correlates with the extent of spectrin deficiency or spectrin dimer content in spherocytotic and elliptocytotic erythrocytes respectively. This growth inhibition was not due to metabolic effects or haemolysis, and instead seems to be caused exclusively by the abnormal cytoskeleton. These results were supported by a later study, where reduced parasite growth in elliptocytotic erythrocytes was observed [54]. Finally, mice carrying a heterozygous mutation in Ank1, which results in severe spherocytosis in homozygotes, have an increase in terminal deoxynucleotidyl transferase dUTP nick end labelling (TUNEL) of intraerythrocytic parasites [57]. TUNEL staining indicates the presence of fragmented DNA, which has been associated with reduced growth and is likely an indication of parasite death [71]. Growth impairment in these conditions could be due to disruptions in interactions between parasite proteins and the host cytoskeleton, several of which have been well documented [72–76].
While haem biosynthesis only occurs in erythroid progenitor cells, small amounts of the enzymes used in the biosynthetic pathway remain in the mature erythrocyte [77, 78]. It has been hypothesized that the parasite may hijack these enzymes for its own haem synthesis, a notion driven by the fact that the parasite haem biosynthesis pathway is dispensable [79, 80], and that a number of these host enzymes are imported into the parasite during growth [81–83]. A recent study of ferrochelatase (Fech), which catalyses the final step in haem biosynthesis, indicates the parasite may largely depend on the erythrocyte enzyme. Fech-deficient mice (homozygous for a ferrochelatase knockdown mutation) were more resistant to P. chabaudi infection with parasite growth reduced, while P. falciparum growth was significantly impaired in cultures using Fech deficient-erythrocytes from patients with erythropoietic protoporphyria. Furthermore, erythrocytes in which ferrochelatase was inhibited pharmacologically also impeded parasite growth [84]. Another line of evidence indicates that the parasite utilizes the host kinases PAK-1 and MEK-1 to facilitate growth. They are specifically activated in infected erythrocytes and highly specific PAK-1 and MEK-1 inhibitors are potent inhibitors of parasite growth [85]. A different study has demonstrated a requirement for erythrocyte calpain-1 during parasite egress. Depletion or pharmaceutical inhibition of the enzyme prevented this stage of the parasite growth cycle [86]. Calpain-1 activation is likely initiated through a host signalling pathway involving protein kinase C (PKC). It is postulated that parasite GPCR ligands overstimulate host GPCRs, leading to G-protein alpha-q mediated activation of PKC, which in turn compromises the erythrocyte cytoskeleton through the phosphorylation of adducin and activation of the cation channel TRPC6. Rapid calcium influx through TRPC6 leads to the activation of calpain-1, which facilitates breakdown of the cell membrane and parasite egress. In support of a central role of PKC in this process, inhibitors of PKC show strong antimalarial activity during in vivo rodent malaria infection [87]. Finally, while not directly proven to be required for parasite growth, the host antioxidant enzymes superoxide dismutase [88] and peroxiredoxin-2 [89] are imported into the parasite and they retain their biological activity. In the case of peroxiredoxin-2, more than half of the parasite’s peroxide degradation capacity was estimated to derive from the host enzyme [89].
Cytoadherence and splenic clearance of parasitized erythrocytes
The Plasmodium parasite distinguishes itself from most other pathogens in that its target cell, at least in mammals, is enucleate and lacks the intracellular pathogen sensing machinery present in most other cells of the body. The host must therefore rely on immune mechanisms that allow extracellular recognition (and removal) of parasitized cells.
The spleen is responsible for the removal of abnormal and senescent erythrocytes, and is also a major component in the host recognition and clearance of parasitized cells [90]. It is a highly vascularized organ comprising of inter-endothelial slits through which all erythrocytes in circulation pass (on average once every 100–200 min) [90, 91]. Erythrocytes not sufficiently deformable to pass through the slits are retained and are phagocytized by macrophages [92–94]. As the Plasmodium parasite grows within the erythrocyte, the cell deformability decreases [95–98], so that it may similarly be retained by the spleen and removed; even relatively immature ring-stage parasitized cells undergo an appreciable degree of splenic retention [96, 99]. However, parasites avoid splenic retention by expressing molecules that promote cell adhesion, both to other erythrocytes (called rosetting) and to endothelial cells. This results in the so-called sequestering of parasitized cells within microvasculature tissue beds, where they can continue to grow and replicate in relative isolation. In the case of P. falciparum, the adhesive properties are largely imparted by the interaction of PfEMP proteins with endothelial cell surface molecules such as ICAM1 and CD36 [100] and chondroitin sulphate in the placental vasculature [101]. Although the pathological consequences of P. falciparum sequestration are still debated (for review see Rowe et al. [102]), binding of infected cells to the endothelium has been demonstrated to promote coagulation, endothelial dysfunction, and inflammation, ultimately causing blood vessel obstruction, while sequestration in the brain microvasculature is linked to the life threatening cerebral malaria syndrome [103].
Several studies have shown that P. falciparum parasitized HbAS [104] [69], HbSS [104], HbAC [105] [69], HbCC [105] [69], and alpha thalassaemic [106] erythrocytes do not bind as readily to human microvascular endothelial cells in vitro (compared with parasitized HbAA erythrocytes). It was found that parasitized HbAC and HbCC erythrocytes had reduced levels of surface PfEMP-1 [105], despite displaying a normal amount of another parasite-expressed membrane associated protein; knob-associated histidine-rich protein (KHARP) [63]. Additional molecular studies indicate that parasite protein trafficking across the parasitophorous vacuole is impaired within HbAC and HbAS cells, and parasites growing within these cells form aberrant Maurer’s clefts. Together, these impairments may inhibit PfEMP-1 trafficking to the erythrocyte membrane, and explain the reduced cytoadherence of these cells [68, 69].
In contrast, SAO parasitized erythrocytes have been shown to display an increased affinity for the endothelial host receptor CD36 under flow conditions [107]. Although this seems contradictory to the known protective effect of SAO during severe malaria, it is worth noting that CD36 is an important immune cell receptor, and has been implicated in the binding and removal of parasitized erythrocytes by both platelets [108] and phagocytic cells [109]. The exact effects of increased CD36 affinity in determining resistance to malaria in SAO remain to be determined.
Erythrocyte disorders that modify the cytoadherent properties of infected cells may result in not only increased immune cell recognition, but also advantageously reduce blood vessel obstruction, coagulation, and inflammation. While good evidence implicates this protective mechanism in the aforementioned disorders, investigations of other erythrocyte abnormalities associated with malaria resistance remain to be undertaken.
Erythrocyte senescence
Erythrocytes undergo several age-related physiological changes during their normal lifespan, which eventually trigger their phagocytosis and recycling by macrophages. This senescence is characterized by cell shrinkage, increased density and rigidity, and changes to erythrocyte surface proteins. Two major models for erythrocyte senescence are commonly reported in the literature. In the first model, here referred to as “band 3 senescence”, a build-up of haemichromes (products of haemoglobin degradation) results in crosslinking between cytoplasmic domains of band 3 proteins and formation of aggregates [110, 111]. Aggregation is facilitated by phosphorylation of band 3, another hallmark of senescence, which reduces its affinity for the cytoskeletal protein, ankyrin, and increases its mobility in the membrane [112]. Aggregated band 3 is recognized by naturally occurring antibodies, which in turn promotes complement protein C3 binding and activation [111]. This finally results in complement-mediated phagocytosis of the senescent cell [113]. The second model, referred to here as “eryptosis”, is characterized by increased intracellular calcium, activation of proteases and phosphatidylserine (PS) exposure on the external surface of the plasma membrane; the term eryptosis recognizes that these features are shared with apoptosis in nucleated mammalian cells [114]. PS exposure leads to phagocytosis of the eryptotic cell [115]. Both eryptosis and band 3 senescence are elevated in parasitized erythrocytes [93, 116–118], and in direct correlation with increasing parasite maturation [116, 119]. An increased oxidative burden imparted on the cell by the parasite is believed to be a central cause of these phenomena [116, 119]. Naturally occurring antibodies to band 3 are associated with improved malaria outcome, indicating that accelerated band 3 senescence may be an important contributor to host defence [120].
In several of the haemoglobinpathies, aberrant haemoglobin is thought to contribute towards the build-up of haemichromes in erythrocytes, thereby accelerating band 3 aggregation [121]. In ring stage infected erythrocytes, senescence of HbAS, HbH, and beta thalassaemic cells occurs more rapidly than equivalently infected normal erythrocytes [122]. This renders ring stage parasites within these cells more susceptible to phagocytosis, which could contribute toward the resistance phenotype conveyed by these disorders. Eryptosis is also enhanced in HbAS and beta thalassaemia [123, 124], and contributes to the early clearance of parasitized cells through PS exposure and phagocytosis [125].
Glucose-6-phosphate dehydrogenase (G6PDH) is a key enzyme involved in controlling oxidative stress in the erythrocyte. Polymorphisms in the X-linked G6PDH gene that result in reduced enzyme activity are relatively frequent in malaria afflicted populations, and there is good evidence that these variants are associated with a decreased risk of severe malaria [3, 126–128]. While early investigations on the potential protective mechanism reported that parasite growth is impaired within G6PD deficient erythrocytes [129, 130], this was not supported by more recent studies [131]. Instead, it seems more likely that elevated oxidative stress in the erythrocyte results in increased haemichrome formation, which results in an increased susceptibility of ring stage parasitized cells to senescence and phagocytosis [131]. G6PD deficient erythrocytes are also more susceptible to eryptosis, which may be an additional factor mediating their early clearance when parasitized [124]. Genetic-based deficiencies of pyruvate kinase (PK), a glycolytic enzyme involved in the production of ATP, have been associated with reduced susceptibility to both rodent and human malaria [132, 133]. Similar to G6PD deficiency, increased oxidative stress in these defective erythrocytes is thought to accelerate ring stage erythrocyte senescence, resulting in enhanced phagocytic clearance of parasites [134]. It has also been recently reported that parasitized O-blood group erythrocytes display increased susceptibility to band 3 senescence and phagocytosis, indicating that this mechanism may be responsible for the increased malaria resistance that has been observed for people of O-blood type [135, 136].
Integrated mechanisms
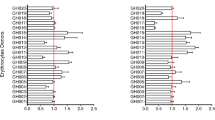
This review has described a number of ways in which erythrocyte disorders may be advantageous to host during malarial infection. It is notable that in several cases multiple mechanisms have been attributed to a single disorder (Table 1). It should also be considered that these effects are not mutually exclusive, although in some cases they may be closely linked. A good example of this is HbAS. In this condition, parasite growth is believed to be inhibited in HbAS cells by the actions of both micro RNAs [70], aberrant actin remodelling [68], and impaired protein trafficking across the parasitophorous vacuole [69]. These mechanisms may also explain the reduced surface expression of PfEMP-1 and associated reduction in cytoadherence [104]. Simultaneously, elevated levels of oxidized haemoglobin in HbAS cells leads to increased deposition of haemichromes on band 3 [122], causing accelerated senescence characterized by band 3 aggregation and binding of naturally occurring antibodies and complement to the erythrocyte surface. The combination of decreased cytoadherence and increased opsonization collectively results in increased phagocytosis of parasitized cells [122]. In addition, increased uptake of parasitized erythrocytes may lead to improved presentation of surface antigens, resulting in the improved antibody response against PfEMP-1 and other parasite surface antigens observed in HbAS individuals [137–139]. Antibodies against PfEMP-1 may further inhibit cytoadherence and facilitate phagocytosis in subsequent infections, which may explain why the protective effect of HbAS increases with age [140, 141] (Figure 1).
Multiple mechanisms of resistance in sickle cell trait (HbAS). Increased oxidative stress and host microRNAs in HbAS erythrocytes inhibit normal parasite development (1). This leads to inhibition of parasite transcription and protein expression (2). The formation of Maurer’s clefts is impaired due to aberrant actin morphology, which prevent normal protein trafficking (3). Binding of parasite proteins which reach the erythrocyte membrane is inhibited by haemichromes, resulting in reduced surface expression of PfEMP (4). Reduced PfEMP expression results in less cytoadherence, which results in increased susceptibility to splenic clearance via phagocytosis (5). Oxidative stress also results in increased haemachrome formation (6), inducing band 3 mediated senescence and phagocytosis (7). Enhanced phagocytosis promotes an immune response (8). Increased production of antibodies against parasite proteins further inhibits cytoadherence and amplifies the effect (9).
It is also plausible that multiple interacting mechanisms involving growth, cytoadherence, and senescence may be the basis for malaria resistance in other erythrocyte disorders. For example, erythrocyte senescence is reported to be accelerated in G6PD deficiency [131], and similar to HbAS cells, increased levels of haemichromes due to oxidative stress are also observed [142]. But it is not yet known if these abnormalities interfere with protein trafficking in the parasite, or concomitantly, its cytoadherent properties. This may also be the case for other disorders where erythrocyte oxidative stress is affected. Interestingly, an early study indicated that parasitized HbAE and HbEE erythrocytes show an increased susceptibility to phagocytosis, however the mechanism behind this was not determined [143]. Given the similarities between HbAE and the other haemoglobinopathies it would be of interest to determine if analogous mechanisms involving senescence are responsible for this phenotype.
Implications for malaria treatment
The aforementioned mechanisms of malaria resistance conveyed by erythrocyte disorders, particularly those involving invasion, have highlighted several potential parasite proteins suitable for therapeutic targeting. As discussed below, many of these are being developed as potential vaccine targets. An alternate, less conventional approach is the development of host directed therapies (HDTs), which could potentially be designed to mimic the protective effects exhibited by naturally occurring erythrocyte disorders. While targeting the parasite directly is less likely to cause off target effects due to the inherent differences between parasite and human biology, it is hampered by substantial variability between parasite strains, and the remarkable ability of parasites to rapidly mutate and develop drug resistance. HDTs could potentially avoid this problem, as manipulation of the therapeutic target would be outside of direct parasite genetic control. Indeed, erythrocyte disorders have imparted malaria resistance consistently for thousands of years, as opposed to parasite directed antimalarials, some of which have lost effectiveness after as little as 2–3 years of wide-spread use [144]. A caveat to this is that HDTs would be at risk of reproducing the deleterious effects sometimes associated with erythrocyte disorders, although if designed correctly HDTs should theoretically be able to avoid this. In fact, many erythrocyte disorders have little or no clinical symptoms, and yet provide substantial resistance to malaria infection. Additionally, HDTs would only affect the host during short-term treatment regimes, as opposed to genetic mutations, which must be tolerated for life. In this review, four major mechanisms have been described by which erythrocyte disorders can convey malaria resistance. Each of these mechanisms could potentially be exploited therapeutically, either through conventional targeting of parasite proteins, or through HDT.
One strategy is to block erythrocyte receptor interactions required for merozoite invasion, either using vaccines or small molecules. For P. vivax, protein structure–function studies have pinpointed the Duffy-antigen binding site of PvDBP to a specific domain called PvDBPII [145], and development of PvDBPII as a vaccine is underway [146]. However, this approach may be challenging due to significant variability in PvDBPII observed amongst different P. vivax isolates [147]. More recently, an X-ray crystal structure of the Duffy-PvDBPII complex has been determined, which may help to identify conserved, critical binding sites suitable for therapeutic targeting [148]. Studies with Plasmodium knowlesi, which also invades erythrocytes via interactions with the Duffy receptor [149], have shown that a Duffy binding chemokine, melanoma growth stimulating activity (MGSA), can block merozoite invasion by this parasite [150]. Furthermore, as MGSA also binds to type B IL-8 receptor (IL-8RB) and activates neutrophils [151], a mutant form of MGSA was identified that was able to inhibit P. knowlesi invasion without cross-reacting with IL-8RB [152]. This result highlights the potential of developing small molecule inhibitors which specifically block the merozoite binding site of the Duffy receptor while avoiding off-target effects, and a screen for these inhibitors has been proposed [153].
Several invasion blocking vaccines for P. falciparum are under development. Many are based on the interactions originally identified through the study of naturally occurring erythrocyte disorders, such as the glycophorin deficiencies. Vaccines against the P. falciparum merozoite glycophorin binding ligands, PfEBL-1, PfEBA-140 and PfEBA-175 are all under development [22, 154–156]. However, the discovery of glycophorin independent invasion pathways, including CR1-PfRh4 [26] and GYPA-band 3-RhopH3-MSP1 [157], will likely complicate the effectiveness of such approaches. A more ideal vaccine target in this respect may be the basigin-PfRh5 interaction. Antibodies targeting this complex have been shown to completely block erythrocyte invasion by all P. falciparum strains tested to date [29, 158, 159]. Preliminary studies have also have indicated that vaccine induced antibodies to PfRh5 inhibit the growth of PfRh5 polymorphic P. falciparum strains in vitro [158, 160], and PfRh5 vaccinated Aotus monkeys were protected from experimental infection [161]. In terms of HDTs, antibody blocking of basigin as opposed to PfRh5 has been demonstrated to be more efficacious in preventing invasion [28, 162]. This is possibly due to the fact that merozoite antigens are only exposed for seconds while erythrocyte receptors are continuously exposed, allowing binding to reach equilibrium [162]. Mimicking protective cytoskeletal abnormalities is also an appealing, but probably more challenging approach. However, artificial inhibition of band 3 mobility has already been demonstrated to prevent merozoite invasion [53], opening up the possibility of achieving this in a clinically relevant manner.
The parasite depends on a wide range of host factors in order to facilitate its development and survival within the erythrocyte, and natural protective mechanisms that affect such factors indicate a number of potential targets. In some cases inhibitors for such factors have already been developed, and preclinical efficacy demonstrated. For example, G6PD deficiency is known to reduce malaria susceptibility, and recent chemical screens have identified inhibitors for both human G6PD [163], and P. falciparum G6PD [164], with the later demonstrated to reduce parasite growth in vitro. Inhibitors for the host kinase MEK1 have also shown anti-malarial properties, and it has been suggested these compounds may act against the parasite in a host directed manner [85]. Erythrocyte enzymes that are imported by the parasite have also been examined as potential antimalarial targets. Studies have shown that the parasite imports and utilizes the host erythrocyte enzyme Fech [165], and that the parasite-expressed Fech is dispensable [79]. More recently it was demonstrated that parasite growth is reduced in both mouse and human erythrocytes with reduced Fech activity, and that a Fech inhibitor N-methylprotoporphyrin completely prevented parasite growth in vitro [84]. Taken together, this suggests that anti-Fech agents can act against the parasite in a host directed manner. In another example, parasite growth is blocked in erythrocytes treated with an irreversible inhibitor of peroxiredoxin [166]; the parasite normally imports and utilizes host peroxiredoxin-2 during its development [89]. Sotrastaurin is a PKC inhibitor that is currently undergoing Phase II clinical trials for the treatment of psoriasis and in liver transplant [167, 168]. The drug is also highly protective in mice infected with Plasmodium berghei and P. yoelii, and inhibits P. falciparum growth in vivo [87]. Interestingly, no parasite orthologue for the PKC enzyme exists, suggesting the drug may act in a host-directed manner against erythrocyte PKC.
Cytoadherence of infected erythrocytes is another attractive therapeutic target, given it has been implicated in the resistance mechanisms of several erythrocyte disorders. Fucosylated chondroitin sulfate was found to inhibit cytoadherence to human lung endothelial cells by P. falciparum infected erythrocytes, including clinical isolates, highlighting its potential therapeutic value [169]. The anthelmintic drug levamisole hydrochloride has been shown to reduce cytoadherence of infected erythrocytes to CD36 [170], however, in a recent randomized controlled trial no clinical benefit was gained when given as an adjuvant to artesunate [171]. This result may indicate that CD36 binding is not detrimental during malaria infection, a notion supported by the fact that the malaria protective condition SAO enhances CD36 binding [107]. In another study, erythrocyte casein kinase II, which is involved in phosphorylation of PfEMP-1, has been pharmacologically inhibited to reduce cytoadherence of infected erythrocytes [172].
Erythrocyte senescence has also proven to be a practical antimalarial target, and compounds designed to accelerate this process have shown potential, with several producing protective effects during the course of malaria infection. These include chlorpromazine [173], paclitaxel [174], the NO synthase inhibitor L-NAME [175], the hormone analogue 16 alpha-bromoepiandrosterone [176], and, indolone-N-oxides [177]. The later are currently undergoing clinical trials for their antimalarial activity. As these compounds induce oxidative stress in the erythrocyte, it would be of interest to determine if they may concurrently inhibit parasite protein trafficking and reduce cytoadherence, as is demonstrated for erythrocyte disorders such as sickle cell trait.
Conclusions
Studies of erythrocytic genetic disorders associated with host resistance to malaria have arguably been the most important source of knowledge regarding the Plasmodium-erythrocyte interaction to date. These studies have not only facilitated the discovery of many of the host-parasite protein interactions involved in merozoite invasion of erythrocytes, but have also provided clues as to what host factors are important for the intraerythrocytic development of the parasite. It is a testament to the complexity of this delicate interaction that even after nearly 70 years of research, entirely new mechanisms for host resistance in conditions such as sickle cell trait, as well as completely novel host-parasite receptor interactions, are being elucidated. Indeed, much about the Plasmodium-erythrocyte interaction in erythrocytic genetic disorders remains unclear. As parasite resistance to antimalarials becomes increasingly prevalent, the development of novel therapies will be more important than ever. Research into the mechanisms of resistance provided by erythrocyte disorders is highlighting the key factors required for parasite survival, and the potential for targeting these therapeutically, both through conventional parasite-directed treatments, or through HDT.
References
Beet EA (1946) Sickle cell disease in the Balovale District of Northern Rhodesia. East Afr Med J 23:75–86
Kwiatkowski DP (2005) How malaria has affected the human genome and what human genetics can teach us about malaria. Am J Hum Genet 77:171–192
Malaria Genomic Epidemiology Network (2014) Reappraisal of known malaria resistance loci in a large multicenter study. Nat Genet 46:1197–1204
Allison AC (2009) Genetic control of resistance to human malaria. Curr Opin Immunol 21:499–505
Verra F, Mangano VD, Modiano D (2009) Genetics of susceptibility to Plasmodium falciparum: from classical malaria resistance genes towards genome-wide association studies. Parasite Immunol 31:234–253
Gilson PR, Crabb BS (2009) Morphology and kinetics of the three distinct phases of red blood cell invasion by Plasmodium falciparum merozoites. Int J Parasitol 39:91–96
Wright GJ, Rayner JC (2014) Plasmodium falciparum erythrocyte invasion: combining function with immune evasion. PLoS Pathog 10:e1003943
Tournamille C, Colin Y, Cartron JP, Le Van Kim C (1995) Disruption of a GATA motif in the Duffy gene promoter abolishes erythroid gene expression in Duffy-negative individuals. Nat Genet 10:224–228
Wertheimer SP, Barnwell JW (1989) Plasmodium vivax interaction with the human Duffy blood group glycoprotein: identification of a parasite receptor-like protein. Exp Parasitol 69:340–350
Barnwell JW, Nichols ME, Rubinstein P (1989) In vitro evaluation of the role of the Duffy blood group in erythrocyte invasion by Plasmodium vivax. J Exp Med 169:1795–1802
Culleton RL, Mita T, Ndounga M, Unger H, Cravo PV, Paganotti GM et al (2008) Failure to detect Plasmodium vivax in West and Central Africa by PCR species typing. Malar J 7:174
Gething PW, Elyazar IRF, Moyes CL, Smith DL, Battle KE, Guerra CA et al (2012) A long neglected world malaria map: Plasmodium vivax endemicity in 2010. PLoS Negl Trop Dis 6:e1814
Howes RE, Patil AP, Piel FB, Nyangiri OA, Kabaria CW, Gething PW et al (2011) The global distribution of the Duffy blood group. Nat Commun 2:266
Ménard D, Barnadas C, Bouchier C, Henry-Halldin C, Gray LR, Ratsimbasoa A et al (2010) Plasmodium vivax clinical malaria is commonly observed in Duffy-negative Malagasy people. Proc Natl Acad Sci USA 107:5967–5971
Lo E, Yewhalaw D, Zhong D, Zemene E, Degefa T, Tushune K et al (2015) Molecular epidemiology of Plasmodium vivax and Plasmodium falciparum malaria among Duffy-positive and Duffy-negative populations in Ethiopia. Malar J 14:84
Zimmerman PA, Ferreira MU, Howes RE, Mercereau-Puijalon O (2013) Red blood cell polymorphism and susceptibility to Plasmodium vivax. Adv Parasitol 81:27–76
Miller LH, Haynes JD, McAuliffe FM, Shiroishi T, Durocher JR, McGinniss MH (1977) Evidence for differences in erythrocyte surface receptors for the malarial parasites, Plasmodium falciparum and Plasmodium knowlesi. J Exp Med 146:277–281
Tolia NH, Enemark EJ, Sim BKL, Joshua-Tor L (2005) Structural basis for the EBA-175 erythrocyte invasion pathway of the malaria parasite Plasmodium falciparum. Cell 122:183–193
Orlandi PA, Klotz FW, Haynes JD (1992) A malaria invasion receptor, the 175-kilodalton erythrocyte binding antigen of Plasmodium falciparum recognizes the terminal Neu5Ac(α2-3)Gal-sequences of glycophorin A. J Cell Biol 116:901–909
Baldwin MR, Li X, Hanada T, Liu SC, Chishti AH (2015) Merozoite surface protein 1 recognition of host glycophorin A mediates malaria parasite invasion of red blood cells. Blood 125:2704–2711
Mayer DC, Cofie J, Jiang L, Hartl DL, Tracy E, Kabat J et al (2009) Glycophorin B is the erythrocyte receptor of Plasmodium falciparum erythrocyte-binding ligand, EBL-1. Proc Natl Acad Sci USA 106:5348–5352
Li X, Marinkovic M, Russo C, McKnight CJ, Coetzer TL, Chishti AH (2012) Identification of a specific region of Plasmodium falciparum EBL-1 that binds to host receptor glycophorin B and inhibits merozoite invasion in human red blood cells. Mol Biochem Parasitol 183:23–31
Maier AG, Duraisingh MT, Reeder JC, Patel SS, Kazura JW, Zimmerman PA et al (2003) Plasmodium falciparum erythrocyte invasion through glycophorin C and selection for Gerbich negativity in human populations. Nat Med 9:87–92
Dolan SA, Proctor JL, Alling DW, Okubo Y, Wellems TE, Miller LH (1994) Glycophorin B as an EBA-175 independent Plasmodium falciparum receptor of human erythrocytes. Mol Biochem Parasitol 64:55–63
Spadafora C, Awandare GA, Kopydlowski KM, Czege J, Moch JK, Finberg RW et al (2010) Complement receptor 1 is a sialic acid-independent erythrocyte receptor of Plasmodium falciparum. PLoS Pathog 6:e1000968
Tham WH, Schmidt CQ, Hauhart RE, Guariento M, Tetteh-Quarcoo PB, Lopaticki S et al (2011) Plasmodium falciparum uses a key functional site in complement receptor type-1 for invasion of human erythrocytes. Blood 118:1923–1933
Cockburn IA, Mackinnon MJ, O’Donnell A, Allen SJ, Moulds JM, Baisor M et al (2004) A human complement receptor 1 polymorphism that reduces Plasmodium falciparum rosetting confers protection against severe malaria. Proc Natl Acad Sci USA 101:272–277
Crosnier C, Bustamante LY, Bartholdson SJ, Bei AK, Theron M, Uchikawa M et al (2011) Basigin is a receptor essential for erythrocyte invasion by Plasmodium falciparum. Nature 480:534–537
Wright KE, Hjerrild KA, Bartlett J, Douglas AD, Jin J, Brown RE et al (2014) Structure of malaria invasion protein RH5 with erythrocyte basigin and blocking antibodies. Nature 515:427–430
Tran TM, Ongoiba A, Coursen J, Crosnier C, Diouf A, Huang CY et al (2014) Naturally acquired antibodies specific for Plasmodium falciparum reticulocyte-binding protein homologue 5 inhibit parasite growth and predict protection from malaria. J Infect Dis 209:789–798
Egan ES, Jiang RH, Moechtar MA, Barteneva NS, Weekes MP, Nobre LV et al (2015) Malaria. A forward genetic screen identifies erythrocyte CD55 as essential for Plasmodium falciparum invasion. Science 348:711–714
Storry JR, Reid ME, Yazer MH (2010) The Cromer blood group system: a review. Immunohematology 26:109–118
Genomes Project C, Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM et al (2012) An integrated map of genetic variation from 1,092 human genomes. Nature 491:56–65
Kuma H, Abe Y, Askin D, Bruce LJ, Hamasaki T, Tanner MJ et al (2002) Molecular basis and functional consequences of the dominant effects of the mutant band 3 on the structure of normal band 3 in Southeast Asian ovalocytosis. Biochemistry 41:3311–3320
Che A, Cherry RJ, Bannister LH, Dluzewski AR (1993) Aggregation of band 3 in hereditary ovalocytic red blood cell membranes. Electron microscopy and protein rotational diffusion studies. J Cell Sci 105(Pt 3):655–660
Schofield AE, Reardon DM, Tanner MJ (1992) Defective anion transport activity of the abnormal band 3 in hereditary ovalocytic red blood cells. Nature 355:836–838
Mohandas N, Lie-Injo LE, Friedman M, Mak JW (1984) Rigid membranes of Malayan ovalocytes: a likely genetic barrier against malaria. Blood 63:1385–1392
Saul A, Lamont G, Sawyer WH, Kidson C (1984) Decreased membrane deformability in Melanesian ovalocytes from Papua New Guinea. J Cell Biol 98:1348–1354
Dluzewski AR, Nash GB, Wilson RJ, Reardon DM, Gratzer WB (1992) Invasion of hereditary ovalocytes by Plasmodium falciparum in vitro and its relation to intracellular ATP concentration. Mol Biochem Parasitol 55:1–7
Liu SC, Zhai S, Palek J, Golan DE, Amato D, Hassan K et al (1990) Molecular defect of the band 3 protein in southeast Asian ovalocytosis. N Engl J Med 323:1530–1538
Tilley L, Nash GB, Jones GL, Sawyer WH (1991) Decreased rotational diffusion of band 3 in Melanesian ovalocytes from Papua, New Guinea. J Membr Biol 121:59–66
Mirchev R, Lam A, Golan DE (2011) Membrane compartmentalization in Southeast Asian ovalocytosis red blood cells. Br J Haematol 155:111–121
Booth PB, Serjeantson S, Woodfield DG, Amato D (1977) Selective depression of blood group antigens associated with hereditary ovalocytosis among melanesians. Vox Sang 32:99–110
Smythe JS, Spring FA, Gardner B, Parsons SF, Judson PA, Anstee DJ (1995) Monoclonal antibodies recognizing epitopes on the extracellular face and intracellular N-terminus of the human erythrocyte anion transporter (band 3) and their application to the analysis of South East Asian ovalocytes. Blood 85:2929–2936
Genton B, Al-Yaman F, Mgone CS, Alexander N, Paniu MM, Alpers MP et al (1995) Ovalocytosis and cerebral malaria. Nature 378:564–565
Allen SJ, O’Donnell A, Alexander ND, Mgone CS, Peto TE, Clegg JB et al (1999) Prevention of cerebral malaria in children in Papua New Guinea by southeast Asian ovalocytosis band 3. Am J Trop Med Hyg 60:1056–1060
Amato D, Booth PB (1977) Hereditary ovalocytosis in Melanesians. P N G Med J 20:26–32
Kidson C, Lamont G, Saul A, Nurse GT (1981) Ovalocytic erythrocytes from Melanesians are resistant to invasion by malaria parasites in culture. Proc Natl Acad Sci USA 78:5829–5832
Cortes A, Benet A, Cooke BM, Barnwell JW, Reeder JC (2004) Ability of Plasmodium falciparum to invade Southeast Asian ovalocytes varies between parasite lines. Blood 104:2961–2966
Okoye VC, Bennett V (1985) Plasmodium falciparum malaria: band 3 as a possible receptor during invasion of human erythrocytes. Science 227:169–171
Goel VK, Li X, Chen H, Liu SC, Chishti AH, Oh SS (2003) Band 3 is a host receptor binding merozoite surface protein 1 during the Plasmodium falciparum invasion of erythrocytes. Proc Natl Acad Sci USA 100:5164–5169
Clough B, Paulitschke M, Nash GB, Bayley PM, Anstee DJ, Wilson RJ et al (1995) Mechanism of regulation of malarial invasion by extraerythrocytic ligands. Mol Biochem Parasitol 69:19–27
Tilley L, Foley M, Anders RF, Dluzewski AR, Gratzer WB, Jones GL et al (1990) Rotational dynamics of the integral membrane protein, band 3, as a probe of the membrane events associated with Plasmodium falciparum infections of human erythrocytes. Biochim Biophys Acta 1025:135–142
Chishti AH, Palek J, Fisher D, Maalouf GJ, Liu SC (1996) Reduced invasion and growth of Plasmodium falciparum into elliptocytic red blood cells with a combined deficiency of protein 4.1, glycophorin C, and p55. Blood 87:3462–3469
Lelliott PM, Lampkin S, McMorran BJ, Foote SJ, Burgio G (2014) A flow cytometric assay to quantify invasion of red blood cells by rodent Plasmodium parasites in vivo. Malar J 13:100
Lelliott PM, McMorran BJ, Foote SJ, Burgio G (2015) In vivo assessment of rodent Plasmodium parasitemia and merozoite invasion by flow cytometry. J Vis Exp (98):e52736. doi:10.3791/52736
Greth A, Lampkin S, Mayura-Guru P, Rodda F, Drysdale K, Roberts-Thomson M et al (2012) A novel ENU-mutation in Ankyrin-1 disrupts malaria parasite maturation in red blood cells of mice. PLoS One 7:e38999
Facer CA (1995) Erythrocytes carrying mutations in spectrin and protein 4.1 show differing sensitivities to invasion by Plasmodium falciparum. Parasitol Res 81:52–57
Schulman S, Roth EF Jr, Cheng B, Rybicki AC, Sussman II, Wong M et al (1990) Growth of Plasmodium falciparum in human erythrocytes containing abnormal membrane proteins. Proc Natl Acad Sci USA 87:7339–7343
Taylor SM, Cerami C, Fairhurst RM (2013) Hemoglobinopathies: slicing the Gordian knot of Plasmodium falciparum malaria pathogenesis. PLoS Pathog 9:e1003327
Friedman MJ, Roth EF, Nagel RL, Trager W (1979) The role of hemoglobins C, S, and Nbalt in the inhibition of malaria parasite development in vitro. Am J Trop Med Hyg 28:777–780
Olson JA, Nagel RL (1986) Synchronized cultures of P falciparum in abnormal red cells: the mechanism of the inhibition of growth in HbCC cells. Blood 67:997–1001
Fairhurst RM, Fujioka H, Hayton K, Collins KF, Wellems TE (2003) Aberrant development of Plasmodium falciparum in hemoglobin CC red cells: implications for the malaria protective effect of the homozygous state. Blood 101:3309–3315
Nagel RL, Raventos-Suarez C, Fabry ME, Tanowitz H, Sicard D, Labie D (1981) Impairment of the growth of Plasmodium falciparum in HbEE erythrocytes. J Clin Invest 68:303–305
Friedman MJ (1979) Oxidant damage mediates variant red cell resistance to malaria. Nature 280:245–247
Ifediba TC, Stern A, Rieder RF (1985) Plasmodium falciparum in vitro: diminished growth in hemoglobin H disease erythrocytes. Blood 65:452–455
Brockelman CR, Wongsattayanont B, Tan-Ariya P, Fucharoen S (1987) Thalassemic erythrocytes inhibit in vitro growth of Plasmodium falciparum. J Clin Microbiol 25:56–60
Cyrklaff M, Sanchez CP, Kilian N, Bisseye C, Simpore J, Frischknecht F et al (2011) Hemoglobins S and C interfere with actin remodeling in Plasmodium falciparum-infected erythrocytes. Science 334:1283–1286
Kilian N, Srismith S, Dittmer M, Ouermi D, Bisseye C, Simpore J et al (2015) Hemoglobin S and C affect protein export in Plasmodium falciparum-infected erythrocytes. Biol Open 4:400–410
LaMonte G, Philip N, Reardon J, Lacsina JR, Majoros W, Chapman L et al (2012) Translocation of sickle cell erythrocyte microRNAs into Plasmodium falciparum inhibits parasite translation and contributes to malaria resistance. Cell Host Microbe 12:187–199
McMorran BJ, Marshall VM, de Graaf C, Drysdale KE, Shabbar M, Smyth GK et al (2009) Platelets kill intraerythrocytic malarial parasites and mediate survival to infection. Science 323:797–800
Maier AG, Rug M, O’Neill MT, Brown M, Chakravorty S, Szestak T et al (2008) Exported proteins required for virulence and rigidity of Plasmodium falciparum-infected human erythrocytes. Cell 134:48–61
Foley M, Corcoran L, Tilley L, Anders R (1994) Plasmodium falciparum: mapping the membrane-binding domain in the ring-infected erythrocyte surface antigen. Exp Parasitol 79:340–350
Pei X, An X, Guo X, Tarnawski M, Coppel R, Mohandas N (2005) Structural and functional studies of interaction between Plasmodium falciparum knob-associated histidine-rich protein (KAHRP) and erythrocyte spectrin. J Biol Chem 280:31166–31171
Pei X, Guo X, Coppel R, Bhattacharjee S, Haldar K, Gratzer W et al (2007) The ring-infected erythrocyte surface antigen (RESA) of Plasmodium falciparum stabilizes spectrin tetramers and suppresses further invasion. Blood 110:1036–1042
Kats LM, Proellocks NI, Buckingham DW, Blanc L, Hale J, Guo X et al (2015) Interactions between Plasmodium falciparum skeleton-binding protein 1 and the membrane skeleton of malaria-infected red blood cells. Biochim Biophys Acta 1848:1619–1628
Pasini EM, Kirkegaard M, Mortensen P, Lutz HU, Thomas AW, Mann M (2006) In-depth analysis of the membrane and cytosolic proteome of red blood cells. Blood 108:791–801
Pasini EM, Kirkegaard M, Salerno D, Mortensen P, Mann M, Thomas AW (2008) Deep coverage mouse red blood cell proteome: a first comparison with the human red blood cell. Mol Cell Proteomics 7:1317–1330
Nagaraj VA, Sundaram B, Varadarajan NM, Subramani PA, Kalappa DM, Ghosh SK et al (2013) Malaria parasite-synthesized heme is essential in the mosquito and liver stages and complements host heme in the blood stages of infection. PLoS Pathog 9:e1003522
Yeh E, DeRisi JL (2011) Chemical rescue of malaria parasites lacking an apicoplast defines organelle function in blood-stage Plasmodium falciparum. PLoS Biol 9:e1001138
Bonday ZQ, Taketani S, Gupta PD, Padmanaban G (1997) Heme biosynthesis by the malarial parasite. Import of delta-aminolevulinate dehydrase from the host red cell. J Biol Chem 272:21839–21846
Bonday ZQ, Dhanasekaran S, Rangarajan PN, Padmanaban G (2000) Import of host delta-aminolevulinate dehydratase into the malarial parasite: identification of a new drug target. Nat Med 6:898–903
van Dooren GG, Kennedy AT, McFadden GI (2012) The use and abuse of heme in apicomplexan parasites. Antioxid Redox Signal 17:634–656
Smith CM, Jerkovic A, Puy H, Winship I, Deybach JC, Gouya L et al (2015) Red cells from ferrochelatase-deficient erythropoietic protoporphyria patients are resistant to growth of malarial parasites. Blood 125:534–541
Sicard A, Semblat JP, Doerig C, Hamelin R, Moniatte M, Dorin-Semblat D et al (2011) Activation of a PAK-MEK signalling pathway in malaria parasite-infected erythrocytes. Cell Microbiol 13:836–845
Chandramohanadas R, Davis PH, Beiting DP, Harbut MB, Darling C, Velmourougane G et al (2009) Apicomplexan parasites co-opt host calpains to facilitate their escape from infected cells. Science 324:794–797
Millholland MG, Mishra S, Dupont CD, Love MS, Patel B, Shilling D et al (2013) A host GPCR signaling network required for the cytolysis of infected cells facilitates release of apicomplexan parasites. Cell Host Microbe 13:15–28
Fairfield AS, Meshnick SR, Eaton JW (1983) Malaria parasites adopt host cell superoxide dismutase. Science 221:764–766
Koncarevic S, Rohrbach P, Deponte M, Krohne G, Prieto JH, Yates J et al (2009) The malarial parasite Plasmodium falciparum imports the human protein peroxiredoxin 2 for peroxide detoxification. Proc Natl Acad Sci USA 106:13323–13328
Buffet PA, Safeukui I, Deplaine G, Brousse V, Prendki V, Thellier M et al (2011) The pathogenesis of Plasmodium falciparum malaria in humans: insights from splenic physiology. Blood 117:381–392
Groom AC, Schmidt EE, MacDonald IC (1991) Microcirculatory pathways and blood flow in spleen: new insights from washout kinetics, corrosion casts, and quantitative intravital videomicroscopy. Scanning Microsc 5:159–173
Looareesuwan S, Ho M, Wattanagoon Y, White NJ, Warrell DA, Bunnag D et al (1987) Dynamic alteration in splenic function during acute falciparum malaria. N Engl J Med 317:675–679
Turrini F, Ginsburg H, Bussolino F, Pescarmona GP, Serra MV, Arese P (1992) Phagocytosis of Plasmodium falciparum-infected human red blood cells by human monocytes: involvement of immune and nonimmune determinants and dependence on parasite developmental stage. Blood 80:801–808
Lutz HU (2004) Innate immune and non-immune mediators of erythrocyte clearance. Cell Mol Biol (Noisy-le-grand) 50:107–116
Maier AG, Cooke BM, Cowman AF, Tilley L (2009) Malaria parasite proteins that remodel the host erythrocyte. Nat Rev Microbiol 7:341–354
Cranston HA, Boylan CW, Carroll GL, Sutera SP, Williamson JR, Gluzman IY et al (1984) Plasmodium falciparum maturation abolishes physiologic red cell deformability. Science 223:400–403
Nash GB, O’Brien E, Gordon-Smith EC, Dormandy JA (1989) Abnormalities in the mechanical properties of red blood cells caused by Plasmodium falciparum. Blood 74:855–861
Mills JP, Diez-Silva M, Quinn DJ, Dao M, Lang MJ, Tan KS et al (2007) Effect of plasmodial RESA protein on deformability of human red blood cells harboring Plasmodium falciparum. Proc Natl Acad Sci USA 104:9213–9217
Safeukui I, Correas JM, Brousse V, Hirt D, Deplaine G, Mule S et al (2008) Retention of Plasmodium falciparum ring-infected erythrocytes in the slow, open microcirculation of the human spleen. Blood 112:2520–2528
Ockenhouse CF, Ho M, Tandon NN, Van Seventer GA, Shaw S, White NJ et al (1991) Molecular basis of sequestration in severe and uncomplicated Plasmodium falciparum malaria: differential adhesion of infected erythrocytes to CD36 and ICAM-1. J Infect Dis 164:163–169
Fried M, Duffy PE (1996) Adherence of Plasmodium falciparum to chondroitin sulfate A in the human placenta. Science 272:1502–1504
Rowe JA, Claessens A, Corrigan RA, Arman M (2009) Adhesion of Plasmodium falciparum-infected erythrocytes to human cells: molecular mechanisms and therapeutic implications. Expert Rev Mol Med 11:e16
Moxon CA, Wassmer SC, Milner DA Jr, Chisala NV, Taylor TE, Seydel KB et al (2013) Loss of endothelial protein C receptors links coagulation and inflammation to parasite sequestration in cerebral malaria in African children. Blood 122:842–851
Cholera R, Brittain NJ, Gillrie MR, Lopera-Mesa TM, Diakite SA, Arie T et al (2008) Impaired cytoadherence of Plasmodium falciparum-infected erythrocytes containing sickle hemoglobin. Proc Natl Acad Sci USA 105:991–996
Fairhurst RM, Baruch DI, Brittain NJ, Ostera GR, Wallach JS, Hoang HL et al (2005) Abnormal display of PfEMP-1 on erythrocytes carrying haemoglobin C may protect against malaria. Nature 435:1117–1121
Krause MA, Diakite SA, Lopera-Mesa TM, Amaratunga C, Arie T, Traore K et al (2012) alpha-Thalassemia impairs the cytoadherence of Plasmodium falciparum-infected erythrocytes. PLoS One 7:e37214
Cortes A, Mellombo M, Mgone CS, Beck HP, Reeder JC, Cooke BM (2005) Adhesion of Plasmodium falciparum-infected red blood cells to CD36 under flow is enhanced by the cerebral malaria-protective trait South-East Asian ovalocytosis. Mol Biochem Parasitol 142:252–257
McMorran BJ, Wieczorski L, Drysdale KE, Chan JA, Huang HM, Smith C et al (2012) Platelet factor 4 and Duffy antigen required for platelet killing of Plasmodium falciparum. Science 338:1348–1351
McGilvray ID, Serghides L, Kapus A, Rotstein OD, Kain KC (2000) Nonopsonic monocyte/macrophage phagocytosis of Plasmodium falciparum-parasitized erythrocytes: a role for CD36 in malarial clearance. Blood 96:3231–3240
Low PS, Waugh SM, Zinke K, Drenckhahn D (1985) The role of hemoglobin denaturation and band 3 clustering in red blood cell aging. Science 227:531–533
Lutz HU, Bussolino F, Flepp R, Fasler S, Stammler P, Kazatchkine MD et al (1987) Naturally occurring anti-band-3 antibodies and complement together mediate phagocytosis of oxidatively stressed human erythrocytes. Proc Natl Acad Sci USA 84:7368–7372
Ferru E, Giger K, Pantaleo A, Campanella E, Grey J, Ritchie K et al (2011) Regulation of membrane-cytoskeletal interactions by tyrosine phosphorylation of erythrocyte band 3. Blood 117:5998–6006
Pantaleo A, Giribaldi G, Mannu F, Arese P, Turrini F (2008) Naturally occurring anti-band 3 antibodies and red blood cell removal under physiological and pathological conditions. Autoimmun Rev 7:457–462
Bratosin D, Estaquier J, Petit F, Arnoult D, Quatannens B, Tissier JP et al (2001) Programmed cell death in mature erythrocytes: a model for investigating death effector pathways operating in the absence of mitochondria. Cell Death Differ 8:1143–1156
Föller M, Bobbala D, Koka S, Huber SM, Gulbins E, Lang F (2009) Suicide for survival—death of infected erythrocytes as a host mechanism to survive malaria. Cell Physiol Biochem 24:133–140
Giribaldi G, Ulliers D, Mannu F, Arese P, Turrini F (2001) Growth of Plasmodium falciparum induces stage-dependent haemichrome formation, oxidative aggregation of band 3, membrane deposition of complement and antibodies, and phagocytosis of parasitized erythrocytes. Br J Haematol 113:492–499
Eda S, Sherman IW (2002) Cytoadherence of malaria-infected red blood cells involves exposure of phosphatidylserine. Cell Physiol Biochem 12:373–384
Schwartz RS, Olson JA, Raventos-Suarez C, Yee M, Heath RH, Lubin B et al (1987) Altered plasma membrane phospholipid organization in Plasmodium falciparum-infected human erythrocytes. Blood 69:401–407
Huber SM, Uhlemann AC, Gamper NL, Duranton C, Kremsner PG, Lang F (2002) Plasmodium falciparum activates endogenous Cl(−) channels of human erythrocytes by membrane oxidation. EMBO J 21:22–30
Hogh B, Petersen E, Crandall I, Gottschau A, Sherman IW (1994) Immune responses to band 3 neoantigens on Plasmodium falciparum-infected erythrocytes in subjects living in an area of intense malaria transmission are associated with low parasite density and high hematocrit value. Infect Immun 62:4362–4366
Arese P, Turrini F, Schwarzer E (2005) Band 3/complement-mediated recognition and removal of normally senescent and pathological human erythrocytes. Cell Physiol Biochem 16:133–146
Ayi K, Turrini F, Piga A, Arese P (2004) Enhanced phagocytosis of ring-parasitized mutant erythrocytes: a common mechanism that may explain protection against falciparum malaria in sickle trait and beta-thalassemia trait. Blood 104:3364–3371
de Jong K, Emerson RK, Butler J, Bastacky J, Mohandas N, Kuypers FA (2001) Short survival of phosphatidylserine-exposing red blood cells in murine sickle cell anemia. Blood 98:1577–1584
Lang KS, Roll B, Myssina S, Schittenhelm M, Scheel-Walter HG, Kanz L et al (2002) Enhanced erythrocyte apoptosis in sickle cell anemia, thalassemia and glucose-6-phosphate dehydrogenase deficiency. Cell Physiol Biochem 12:365–372
Lang PA, Kasinathan RS, Brand VB, Duranton C, Lang C, Koka S et al (2009) Accelerated clearance of Plasmodium-infected erythrocytes in sickle cell trait and annexin-A7 deficiency. Cell Physiol Biochem 24:415–428
Allison AC (1960) Glucose-6-phosphate dehydrogenase deficiency in red blood cells of East Africans. Nature 186:531–532
Luzzatto L, Usanga FA, Reddy S (1969) Glucose-6-phosphate dehydrogenase deficient red cells: resistance to infection by malarial parasites. Science 164:839–842
Bienzle U, Ayeni O, Lucas AO, Luzzatto L (1972) Glucose-6-phosphate dehydrogenase and malaria. Greater resistance of females heterozygous for enzyme deficiency and of males with non-deficient variant. Lancet 1:107–110
Usanga EA, Luzzatto L (1985) Adaptation of Plasmodium falciparum to glucose 6-phosphate dehydrogenase-deficient host red cells by production of parasite-encoded enzyme. Nature 313:793–795
Roth EF Jr, Raventos-Suarez C, Rinaldi A, Nagel RL (1983) Glucose-6-phosphate dehydrogenase deficiency inhibits in vitro growth of Plasmodium falciparum. Proc Natl Acad Sci USA 80:298–299
Cappadoro M, Giribaldi G, O’Brien E, Turrini F, Mannu F, Ulliers D et al (1998) Early phagocytosis of glucose-6-phosphate dehydrogenase (G6PD)-deficient erythrocytes parasitized by Plasmodium falciparum may explain malaria protection in G6PD deficiency. Blood 92:2527–2534
Min-Oo G, Fortin A, Tam MF, Nantel A, Stevenson MM, Gros P (2003) Pyruvate kinase deficiency in mice protects against malaria. Nat Genet 35:357–362
Ayi K, Min-Oo G, Serghides L, Crockett M, Kirby-Allen M, Quirt I et al (2008) Pyruvate kinase deficiency and malaria. N Engl J Med 358:1805–1810
Chan M, Sim TS (2005) Functional analysis, overexpression, and kinetic characterization of pyruvate kinase from Plasmodium falciparum. Biochem Biophys Res Commun 326:188–196
Wolofsky KT, Ayi K, Branch DR, Hult AK, Olsson ML, Liles WC et al (2012) ABO blood groups influence macrophage-mediated phagocytosis of Plasmodium falciparum-infected erythrocytes. PLoS Pathog 8:e1002942
Cserti CM, Dzik WH (2007) The ABO blood group system and Plasmodium falciparum malaria. Blood 110:2250–2258
Marsh K, Otoo L, Hayes RJ, Carson DC, Greenwood BM (1989) Antibodies to blood stage antigens of Plasmodium falciparum in rural Gambians and their relation to protection against infection. Trans R Soc Trop Med Hyg 83:293–303
Cabrera G, Cot M, Migot-Nabias F, Kremsner PG, Deloron P, Luty AJ (2005) The sickle cell trait is associated with enhanced immunoglobulin G antibody responses to Plasmodium falciparum variant surface antigens. J Infect Dis 191:1631–1638
Verra F, Simpore J, Warimwe GM, Tetteh KK, Howard T, Osier FH et al (2007) Haemoglobin C and S role in acquired immunity against Plasmodium falciparum malaria. PLoS One 2:e978
Williams TN, Mwangi TW, Roberts DJ, Alexander ND, Weatherall DJ, Wambua S et al (2005) An immune basis for malaria protection by the sickle cell trait. PLoS Med 2:e128
Gong L, Maiteki-Sebuguzi C, Rosenthal PJ, Hubbard AE, Drakeley CJ, Dorsey G et al (2012) Evidence for both innate and acquired mechanisms of protection from Plasmodium falciparum in children with sickle cell trait. Blood 119:3808–3814
Pantaleo A, Ferru E, Carta F, Mannu F, Simula LF, Khadjavi A et al (2011) Irreversible AE1 tyrosine phosphorylation leads to membrane vesiculation in G6PD deficient red cells. PLoS One 6:e15847
Bunyaratvej A, Butthep P, Yuthavong Y, Fucharoen S, Khusmith S, Yoksan S et al (1986) Increased phagocytosis of Plasmodium falciparum-infected erythrocytes with haemoglobin E by peripheral blood monocytes. Acta Haematol 76:155–158
Sibley CH, Price RN (2012) Monitoring antimalarial drug resistance: applying lessons learned from the past in a fast-moving present. Int J Parasitol Drugs Drug Resist 2:126–133
Chitnis CE, Miller LH (1994) Identification of the erythrocyte binding domains of Plasmodium vivax and Plasmodium knowlesi proteins involved in erythrocyte invasion. J Exp Med 180:497–506
Sampath S, Carrico C, Janes J, Gurumoorthy S, Gibson C, Melcher M et al (2013) Glycan masking of Plasmodium vivax Duffy Binding Protein for probing protein binding function and vaccine development. PLoS Pathog 9:e1003420
Ntumngia FB, McHenry AM, Barnwell JW, Cole-Tobian J, King CL, Adams JH (2009) Genetic variation among Plasmodium vivax isolates adapted to non-human primates and the implication for vaccine development. Am J Trop Med Hyg 80:218–227
Batchelor JD, Malpede BM, Omattage NS, DeKoster GT, Henzler-Wildman KA, Tolia NH (2014) Red blood cell invasion by Plasmodium vivax: structural basis for DBP engagement of DARC. PLoS Pathog 10:e1003869
Miller LH, Mason SJ, Dvorak JA, McGinniss MH, Rothman IK (1975) Erythrocyte receptors for (Plasmodium knowlesi) malaria: Duffy blood group determinants. Science 189:561–563
Horuk R, Chitnis CE, Darbonne WC, Colby TJ, Rybicki A, Hadley TJ et al (1993) A receptor for the malarial parasite Plasmodium vivax: the erythrocyte chemokine receptor. Science 261:1182–1184
Horuk R, Colby TJ, Darbonne WC, Schall TJ, Neote K (1993) The human erythrocyte inflammatory peptide (chemokine) receptor. Biochemical characterization, solubilization, and development of a binding assay for the soluble receptor. Biochemistry 32:5733–5738
Hesselgesser J, Chitnis CE, Miller LH, Yansura DG, Simmons LC, Fairbrother WJ et al (1995) A mutant of melanoma growth stimulating activity does not activate neutrophils but blocks erythrocyte invasion by malaria. J Biol Chem 270:11472–11476
Handel TM, Horuk R (2010) Duffy antigen inhibitors: useful therapeutics for malaria? Trends Parasitol 26:329–333
Sim BKL, Orlandi PA, Haynes JD, Klotz FW, Carter JM, Camus D et al (1990) Primary structure of the 175K Plasmodium falciparum erythrocyte binding antigen and identification of a peptide which elicits antibodies that inhibit malaria merozoite invasion. J Cell Biol 111:1877–1884
Jiang L, Gaur D, Mu J, Zhou H, Long CA, Miller LH (2011) Evidence for erythrocyte-binding antigen 175 as a component of a ligand-blocking blood-stage malaria vaccine. Proc Natl Acad Sci USA 108:7553–7558
Healer J, Thompson JK, Riglar DT, Wilson DW, Chiu YH, Miura K et al (2013) Vaccination with conserved regions of erythrocyte-binding antigens induces neutralizing antibodies against multiple strains of Plasmodium falciparum. PLoS One 8:e72504
Baldwin M, Yamodo I, Ranjan R, Li X, Mines G, Marinkovic M et al (2014) Human erythrocyte band 3 functions as a receptor for the sialic acid-independent invasion of Plasmodium falciparum. Role of the RhopH3-MSP1 complex. Biochim Biophys Acta 1843:2855–2870
Douglas AD, Williams AR, Knuepfer E, Illingworth JJ, Furze JM, Crosnier C et al (2014) Neutralization of Plasmodium falciparum merozoites by antibodies against PfRH5. J Immunol 192:245–258
Reddy KS, Amlabu E, Pandey AK, Mitra P, Chauhan VS, Gaur D (2015) Multiprotein complex between the GPI-anchored CyRPA with PfRH5 and PfRipr is crucial for Plasmodium falciparum erythrocyte invasion. Proc Natl Acad Sci USA 112:1179–1184
Douglas AD, Williams AR, Illingworth JJ, Kamuyu G, Biswas S, Goodman AL et al (2011) The blood-stage malaria antigen PfRH5 is susceptible to vaccine-inducible cross-strain neutralizing antibody. Nat Commun 2:601
Douglas AD, Baldeviano GC, Lucas CM, Lugo-Roman LA, Crosnier C, Bartholdson SJ et al (2015) A PfRH5-based vaccine is efficacious against heterologous strain blood-stage Plasmodium falciparum infection in Aotus monkeys. Cell Host Microbe 17:130–139
Williams AR, Douglas AD, Miura K, Illingworth JJ, Choudhary P, Murungi LM et al (2012) Enhancing blockade of Plasmodium falciparum erythrocyte invasion: assessing combinations of antibodies against PfRH5 and other merozoite antigens. PLoS Pathog 8:e1002991
Preuss J, Richardson AD, Pinkerton A, Hedrick M, Sergienko E, Rahlfs S et al (2013) Identification and characterization of novel human glucose-6-phosphate dehydrogenase inhibitors. J Biomol Screen 18:286–297
Preuss J, Maloney P, Peddibhotla S, Hedrick MP, Hershberger P, Gosalia P et al (2012) Discovery of a Plasmodium falciparum glucose-6-phosphate dehydrogenase 6-phosphogluconolactonase inhibitor (R, Z)-N-((1-ethylpyrrolidin-2-yl)methyl)-2-(2-fluorobenzylidene)-3-oxo-3,4-dihydr o-2H-benzo[b][1,4]thiazine-6-carboxamide (ML276) that reduces parasite growth in vitro. J Med Chem 55:7262–7272
Varadharajan S, Sagar BK, Rangarajan PN, Padmanaban G (2004) Localization of ferrochelatase in Plasmodium falciparum. Biochem J 384:429–436
Brizuela M, Huang HM, Smith C, Burgio G, Foote SJ, McMorran BJ (2014) Treatment of erythrocytes with the 2-cys peroxiredoxin inhibitor, Conoidin A, prevents the growth of Plasmodium falciparum and enhances parasite sensitivity to chloroquine. PLoS One 9:e92411
Wagner J, von Matt P, Faller B, Cooke NG, Albert R, Sedrani R et al (2011) Structure-activity relationship and pharmacokinetic studies of sotrastaurin (AEB071), a promising novel medicine for prevention of graft rejection and treatment of psoriasis. J Med Chem 54:6028–6039
Pascher A, De Simone P, Pratschke J, Salame E, Pirenne J, Isoneimi H et al (2015) Protein kinase C inhibitor sotrastaurin in de novo liver transplant recipients: a randomized phase II trial. Am J Transplant 15:1283–1292
Bastos MF, Albrecht L, Kozlowski EO, Lopes SC, Blanco YC, Carlos BC et al (2014) Fucosylated chondroitin sulfate inhibits Plasmodium falciparum cytoadhesion and merozoite invasion. Antimicrob Agents Chemother 58:1862–1871
Dondorp AM, Silamut K, Charunwatthana P, Chuasuwanchai S, Ruangveerayut R, Krintratun S et al (2007) Levamisole inhibits sequestration of infected red blood cells in patients with falciparum malaria. J Infect Dis 196:460–466
Maude RJ, Silamut K, Plewes K, Charunwatthana P, Ho M, Abul Faiz M et al (2014) Randomized controlled trial of levamisole hydrochloride as adjunctive therapy in severe falciparum malaria with high parasitemia. J Infect Dis 209:120–129
Hora R, Bridges DJ, Craig A, Sharma A (2009) Erythrocytic casein kinase II regulates cytoadherence of Plasmodium falciparum-infected red blood cells. J Biol Chem 284:6260–6269
Koka S, Lang C, Boini KM, Bobbala D, Huber SM, Lang F (2008) Influence of chlorpromazine on eryptosis, parasitemia and survival of Plasmodium berghei infected mice. Cell Physiol Biochem 22:261–268
Koka S, Bobbala D, Lang C, Boini KM, Huber SM, Lang F (2009) Influence of paclitaxel on parasitemia and survival of Plasmodium berghei infected mice. Cell Physiol Biochem 23:191–198
Koka S, Lang C, Niemoeller OM, Boini KM, Nicolay JP, Huber SM et al (2008) Influence of NO synthase inhibitor L-NAME on parasitemia and survival of Plasmodium berghei infected mice. Cell Physiol Biochem 21:481–488
Ayi K, Giribaldi G, Skorokhod A, Schwarzer E, Prendergast PT, Arese P (2002) 16alpha-bromoepiandrosterone, an antimalarial analogue of the hormone dehydroepiandrosterone, enhances phagocytosis of ring stage parasitized erythrocytes: a novel mechanism for antimalarial activity. Antimicrob Agents Chemother 46:3180–3184
Pantaleo A, Ferru E, Vono R, Giribaldi G, Lobina O, Nepveu F et al (2012) New antimalarial indolone-N-oxides, generating radical species, destabilize the host cell membrane at early stages of Plasmodium falciparum growth: role of band 3 tyrosine phosphorylation. Free Radic Biol Med 52:527–536
Chotivanich K, Udomsangpetch R, Pattanapanyasat K, Chierakul W, Simpson J, Looareesuwan S et al (2002) Hemoglobin E: a balanced polymorphism protective against high parasitemias and thus severe P. falciparum malaria. Blood 100:1172–1176
Authors’ contributions
PML performed the literature survey. PML and BJM wrote the paper. SJF and GB reviewed the paper and assisted in its preparation. All authors read and approved the final manuscript.
Acknowledgements
We acknowledge funding support from the National Health and Medical Research Council (Grant APP605524, 490037 and 1047082), the Australian Research Council (Grant DP12010061), the National Collaborative Research Infrastructure Strategy of Australia and the Education investment fund from the Department of Innovation, Industry, Science and Research. PML is a recipient of an Australian Postgraduate award.
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lelliott, P.M., McMorran, B.J., Foote, S.J. et al. The influence of host genetics on erythrocytes and malaria infection: is there therapeutic potential?. Malar J 14, 289 (2015). https://doi.org/10.1186/s12936-015-0809-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-015-0809-x