Abstract
CAR-T cell therapy is known as an effective therapy in patients with hematological malignancies. Since 2017, several autologous CAR-T cell (auto-CAR-T) drugs have been approved by the US Food and Drug Administration (FDA) for the treatment of some kinds of relapsed/refractory hematological malignancies. However, some patients fail to respond to these drugs due to high manufacturing time, batch-to-batch variation, poor quality and insufficient quantity of primary T cells, and their insufficient expansion and function. CAR-T cells prepared from allogeneic sources (allo-CAR-Ts) can be an alternative option to overcome these obstacles. Recently, several allo-CAR-Ts have entered into the early clinical trials. Despite their promising preclinical and clinical results, there are two main barriers, including graft-versus-host disease (GvHD) and allo-rejection that may decline the safety and efficacy of allo-CAR-Ts in the clinic. The successful development of these products depends on the starter cell source, the gene editing method, and the ability to escape immune rejection and prevent GvHD. Here, we summarize the gene editing technologies and the potential of various cell sources for developing allo-CAR-Ts and highlight their advantages for the treatment of hematological malignancies. We also describe preclinical and clinical data focusing on allo-CAR-T therapy in blood malignancies and discuss challenges and future perspectives of allo-CAR-Ts for therapeutic applications.
Similar content being viewed by others
Introduction
Hematological malignancies (HMs) refer to a category of malignancies that originate in the bone marrow and the lymphatic system. These malignancies are characterized into three main groups: leukemia, lymphoma, and multiple myeloma (MM) [1]. Although chemotherapy, radiotherapy, and immunotherapy are used to treat HMs, some patients develop relapsed/refractory (R/R) disease over time.
The emergence of chimeric antigen receptor (CAR) T cell therapy has created a breakthrough in the treatment of R/R HMs. The CAR comprises an extracellular targeting domain, an scFv (single chain fragment variable), nanobody, or a natural ligand/receptor [2,3,4,5,6,7], which is linked to the signaling endo-domains through a spacer and transmembrane domain, respectively [8]. Since 2017, several autologous CAR-T cells (auto-CAR-Ts) have been approved by the US Food and Drug Administration (FDA) for the treatment of some types of R/R HMs: Tisagenlecleucel, Axicabtagene Ciloleucel, Brexucabtagene Autoleucel, Lisocabtagene Maraleucel, Idecabtagene Vicleucel and Ciltacabtagene Autoleucel [9]. The manufacturing process of approved autologous CAR-T cells starts with the collecting of peripheral blood mononuclear cells (PBMCs) from a patient using leukapheresis, then primary T cells are genetically reprogrammed ex vivo by viral transduction of CAR to T cells to induce stronger antitumor functions, ultimately modified T-cells back into the patient [10, 11]. This process takes more than two weeks [12, 13]. For example, the process of making potent auto-CAR-Ts from CD8+ cells of patients with B cell tumors under long-term chemotherapy, from leukapheresis to injection, can take more than three months [14]. This extended period is impacted by the occurrence of lymphopenia in patients, which affects the manufacturing time to obtain sufficient T lymphocytes, and/or the recovery of patients following chemotherapy.
CAR-T cell manufacturing process for HMs can have less complexity than solid tumors because there are fewer undesired cells like circulating myeloid-derived suppressor cells (MDSCs) in the blood of high-risk patients with HMs than in those with solid tumors [15]. Indeed, the high transduction rate of T cells and, consequently, achievement of the therapeutic dosage depends on the purity of T cells harvested by leukapheresis.
Although all of the marketed CAR-T cells have autologous origin, they are not fit for all patients. Approximately 10–20% of patients fail to respond to the autologous CAR-T cell therapy [16,17,18,19,20]. On the one hand, the manufacturing procedure of auto-CAR-Ts is long [12, 13], and cancer may progress rapidly before the treatment, especially in high-risk patients [21,22,23]. There are some protocols that have reduced the manufacturing time of autoCAR-Ts to less than 2 days to improve the autoCAR-Ts’ efficacy and the patients’ accessibility [24, 25]. However, starting material potency varies from patient to patient and is lower than that of healthy donors. In addition, the manufacturing of auto-CAR-Ts may be associated with the risk of failure. For example, the manufacturing failure rates for Novartis’ Kymriah have been 4% [26] because most patients with leukemia and lymphoma suffer from lymphopenia resulting from intensive chemotherapy before CAR-T cell therapy. It has been implied that only the collected PBMCs with a CD3+ cell count of ≥ 150 cells/µl can be an indication for successful manufacturing of an autologous CAR-T cell product in hematological cancer therapy [15]. Given clinical data in HMs, another reason for the treatment failure is related to the specifications of the apheresis product because pre-treating with chemotherapy selectively lowers early lineage T cells (e.g., central memory or stem cell-like memory T cells) that are associated with effective CAR-T cells expansion in vitro and in vivo [27,28,29]. Despite the fact that the manufacturing protocol for each of the approved CAR-T cells, like Kymriah, is the same, patients have shown different clinical responses to the drug because the starter T cell phenotype varies from patient to patient [28, 30]. Cell number, viability, purity, and CAR expression, which are generally the critical points in standard manufacturing workflows, will be significantly variable from one batch to another in auto-CAR-Ts. The consequent product variability and the absence of reference standards can complicate the safety and efficacy evaluation [31, 32]. All of these make auto-CAR-T therapy one of the most expensive treatment options in the world, limiting cancer patients’ access to treatment [33, 34].
Currently, allogeneic CAR-T cells (allo-CAR-Ts) are being developed to combat challenges related to auto-CAR-T therapy. In contrast to auto-CAR-Ts, allo-CAR-Ts do not have limitations related to the T cell’s fitness and cell sources. Since T cell lymphopenia in patients with HMs either excludes eligibility of some patients to receive auto-CAR-Ts or makes re-dosing impossible [35], using healthy donor T cells can be a good solution. The healthy donor T cells can be stored at different dosages with “fitter” T cells than autologous T cells. Moreover, they have not undergone multiple iterations of anti-cancer therapy and are more tolerant of harvesting and ex vivo manipulation [35, 36]. Furthermore, several factors, such as age, chronic infection, and pre-treatments, can affect an individual’s T cell fitness [37]. Allo-CAR-T therapy provides an opportunity to select donors with the greatest T cell fitness, to scale up the manufacturing process, to make different ready-to-use therapeutic doses to avoid manufacturing delays at the time of need, and to verify the product through quality control tests. Therefore, allo-CAR-Ts may increase the efficacy of CAR-T cell therapy and lower manufacturing costs [38].
Here, we summarize how allo-CAR-Ts are produced and specifically focus on advantages and preclinical and clinical studies of them in HMs. Since the adverse effects of allo-CAR-T therapy can be a barrier to their translation into the clinic, we highlight some strategies to overcome them.
Allogeneic CAR-T cells
In contrast to auto-CAR-Ts, allo-CAR-Ts are raised from a healthy donor’s PBMCs, which include both T and B lymphocytes. Then, primary T cells are isolated using leukapheresis. There are two groups of T cells, called αβ T cells, and γδ T cells, which are distinguished by the surface expression of the chains of TCR-α and TCR-β, or TCR-γ and TCR-δ, respectively. Out of all the T cells in circulation, 95% are αβ T cells, while the remaining 5% are γδ T cells [39]. Unlike γδ T cells, αβ T cells recognize antigens through their TCR only in context of HLAs [40]. This renders αβ T cells susceptible to causing graft-versus-host disease (GVHD), which is dependent on HLA [40]. Therefore, to avoid adverse effects resulting from allogeneic T cell engraftment such as serious GvHD, primary T cells must be ex vivo knocked out for a reactive antigen like TCR. GvHD occurs when allo-CAR-Ts attack the host tissue through recognition of the host’s normal tissues with TCR [41]. Moreover, allo-CAR-Ts’ manufacturing provides an opportunity to either overcome resistance mechanisms such as fratricide [42] or prevent allogeneic rejection (allo-rejection) risk resulted from the host’s immune system attack on allo-CAR-Ts due to the recipient anti-allo-CAR-T responses against HLA-mismatched graft. The disruption of the HLA complex (β2-microglobulin (β2M) domain) and TRAC (T cell receptor α constant) or TRBC (T cell receptor β constant) domains eliminate allo-rejection and GvHD, respectively.
Different gene editing tools have been well adopted with primary T cells [43], enabling researchers to specifically knock-out the potentially alloreactive antigens and knock-in a desirable gene (e.g., CAR) in a special locus or recruit multiple editing to improve antitumor targeting and activity of T cells. In allo-CAR-Ts manufacturing, the priority of inserting a CAR (usually through transduction) or deleting the reactive antigens affects gene editing efficiency. It was shown that the CAR transduction first and then deletion of HLA and TCR antigens has advantages such as better gene editing efficiency and higher cell viability of CAR-T cells [44].
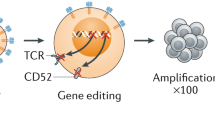
Allo-CAR-Ts with various therapeutic doses can be stored as a ready-to-use drug for any patient, also known as “off-the-shelf” treatments. The overview of allo-CAR-Ts manufacturing process is depicted in Fig. 1. Although the cell source of most allo-CAR-Ts is the primary T cell population, the other sources, including induced pluripotent stem cells (iPSCs), umbilical cord blood (as an iPSCs source), and progenitor cells, have shown suitable potential [22].
Overview of the manufacturing process of allogeneic CAR-T cells (allo-CAR-Ts) for hematological malignancy patients. Allo-CAR-T manufacturing is initiated with the selection of a healthy donor. Then, a suitable amount of T-cells is isolated from the peripheral blood, somatic cell biopsy (reprogramming to induced pluripotent stem cells (iPSCs) and differentiation to T cells), or bone marrow cell separation (differentiation of hematopoietic stem cell (HSCs) or progenitor cells to T cells). After that, T cells are activated via anti-CD3/CD28 beads. After 24 h, the CARs are transduced to T cells, and then TCR/HLA genes are disrupted by transcription activator-like nucleases (TALEN), zinc finger nucleases (ZFN), or clustered regularly interspaced short palindromic repeats-associated protein 9 (CRISPR/Cas9) systems to generate allo-CAR-Ts. Allo-CAR-Ts are expanded ex vivo, and TCR+ T-cells are removed. The final product is formulated with different therapeutic dosages and stored as an off-the-shelf drug. When a patient is enrolled to receive the drug, the allo-CAR-Ts are thawed under controlled conditions and injected into the patient immediately after thawing
Alternative cell sources for allo-CAR-T production
Although the primary T cells are the most conventional cells applied in CAR-T cell therapy [45], the gene manipulation of these primary mature cells is very challenging because they should be modified for simultaneous manipulation of CAR expression and HLA deficiency. Peripheral blood cell apheresis and bone marrow aspiration are two standard methods to achieve a high count of T cells. Also, different types of T cells (i.e., αβ T cells and γδ T cells) are capable of generating allo-CAR-Ts [46]. γδ T cells are a subset of effector T cells with high cytolytic activity. In spite of αβ T cells that recognize the HLA-presented antigens of host cells via αβ TCR, γδ T cells contain γδ TCRs that recognize the target antigen independently of HLA-presentation. Therefore, γδ T cells can be a suitable source for the generation of allo-CAR-Ts without causing GvHD. A major challenge facing the application of γδ T cells to generate allo-CAR-Ts is their low count (less than 10%) in PBMCs. An example of using γδ T cells as a source of allo-CAR-Ts is glypican-3 (GPC-3)-specific allo-CAR-Ts which were developed to eliminate hepatocellular carcinoma cells. A single-dose of GPC-3-specific allo-CAR-Ts could efficiently control the tumor growth without any hallmark of GvHD [47].
iPSCs are promising cells in regenerative medicine which have the differentiation potential to various cell lineages through reprogramming to the embryonic state (pluripotency) [48, 49]. In an autologous manner, iPSCs, as the potential source of CAR immune cells, were demonstrated to be able to differentiate into various tumor immunosurveillance-associated cells derived from the recipient somatic cells. For the generation of CAR immune cells, iPSCs can self-renew and greatly expand compared to donated T cells. HLA-defined iPSCs stored in cell banks are good sources for HLA-matched CAR immune cell allografting but in a completely allogeneic manner. Moreover, HLA-deficient iPSCs are a promising source for generating HLA-deficient iPSC-derived allo-CAR-Ts. The easier achievement of cell source, more straightforward gene engineering, and higher expandability of the final product are some advantages of allogeneic iPSC-derived CAR-T cells. Despite all their benefits, iPSCs are prone to teratoma formation, limiting the clinical administration of iPSC-derived cell products. However, various studies have established routes to eliminate teratoma formation in these products [50,51,52,53,54]. Despite these advancements in iPSC technology, some ethical concerns are addressed by country-specific regulations, i.e., the derivation of stem cells, the potential for tumorigenicity, and overall ethical concerns regarding stem cell therapy. The European embryonic stem cell registry (hESCreg) assigned an enrollment for the application of iPSCs in therapy. For example, origin of iPSCs (donor iPSC phenotype, cell line generator/distributor), informed consent documentation, regulatory compliance (genotyping of iPSCs, marker expression, and functional pluripotency), and some specific restriction (e.g., gene modification control and subclones) [55]. Also, some good-manufacturing-process (GMP) cell banks are developed for iPSCs, which can be used for generation of allo-CAR-Ts [56].
Engrafting allogeneic hematopoietic stem cells (allo-HSC) is a promising therapy for leukemia patients. Also, HSCs could be differentiated to T lineage to generate allo-CAR-Ts. As an enhanced therapeutic procedure of CAR-T cell therapy, the patient should receive a lymphodepletion regimen before grafting CAR-T cells to avoid GvHD, which leads to an aplastic state due to the loss of HSCs. Therefore, the transplantation of HSCs is required to achieve homeostatic hematopoiesis after/simultaneous CAR-T cell engraftment. Therefore, the generation of allo-HSCs enables us to generate a safe cell product for HSC transplantation, as well as a suitable source for allo-CAR-Ts [57, 58]. Despite the clinical benefits of HSCs as a source for allo-CAR-Ts, there are some challenges facing manufacturing. For example, HSCs are a rare cell population in bone marrow and peripheral blood, especially in leukemic patients. Also, both iPSCs and HSCs, as potent stem cell sources, should be considered for the maintenance of stemness, cell viability, and functionality, avoiding undesired differentiation, gene stability, and safety for a GMP of allo-CAR-Ts [59].
Lymphoid progenitors are another promising source for allo-CAR immune cells. Human lymphoid progenitor lineage is an unipotent stem cell with differentiation potency to T cells. Their self-renewal potency enables the derived CAR-T cells to have a higher expansion rate compared to T/NK cell sources. Recent studies showed that the CAR expression in human lymphoid progenitors can enable them to differentiate into T and NK cells with high cytotoxicity properties [60, 61]. Lymphoid progenitor cells are available in umbilical cord blood and bone marrow.
Advantages of allo-CAR-Ts in hematological malignancy
In addition to the general benefits of allo-CAR-Ts, they have several advantages for treatment of hematological malignancies compared to auto-CAR-Ts. Allo-CAR-Ts have shown less severe cytokine release syndrome (CRS) and similar efficacy compared to auto-CAR-Ts in patients with acute lymphoblastic leukemia (ALL) [62]. Another striking benefit of allo-CAR-Ts, is the elimination of bridging therapy. This kind of therapy is recommended for patients with progressive cancers and is administered in the interval between leukapheresis and autologous injection of CAR-T cells to control the tumor burden of HMs [63, 64]. This therapy incurs additional treatment costs, and its efficacy is limited if patients become resistant to the previous drugs. However, these patients can successfully receive allo-CAR-Ts without requiring bridging therapy within five days after enrollment [65, 66]. Therefore, allo-CAR-T therapy can also reduce the costs of hospitalization and interventions.
The use of allo-CAR-Ts eliminates the risk of CAR gene transfer to hematologic tumor cells during the manufacturing process. B-ALL is an aggressive blood cancer in which lymphoid blast overgrowth in blood and bone marrow. A case report showed that despite the lymphodepletion before auto-CAR-T therapy of B-ALL with Kymriah, a single leukemic blast had unintentionally contaminated lymphocytes that had been isolated from a patient and were transduced with CD19CAR during auto-CAR-T manufacturing [67]. This leads to the development of treatment-resistant tumor cells due to masking CD19 epitope from recognition, disease relapse, and death resulting from progressive leukemia [67]. Although no other cases have been reported so far, the potential risk of inadvertent transduction of a tumor cell in auto-CAR-T manufacturing of patients with different HMs is concerning. Using the cell source of healthy donors can resolve the issue of CAR transduction into tumor cells. Moreover, there is a low quantity of undesired circulating cells like MDSCs in the blood of healthy donors compared to patients with HMs like R/R diffuse large B cell lymphoma (DLBCL) [68] that can potentially improve the transduction rate of T cells and increase the manufacturing success.
Preclinical studies of allo-CAR-Ts in hematological malignancy
Considering the superiority of allo-CAR-Ts over auto-CAR-Ts, this question remains whether this generation of engineered cells can act as an off-the-shelf option for cancer treatment. Several preclinical studies are underway to develop allo-CAR-Ts with the least amount of immunogenicity and the most effectiveness for clinical applications [69].
The selection of the desired tumor antigen plays a key role in successful allo-CAR-T therapy. Most studies of CAR-T cells have focused on antigens such as CD19, CD20, CD22 [70], and BCMA in HMs. Other tumor-associated antigens (TAAs) have been exploited as the target antigens in blood malignancies, including CD23, CD30, CD33, SLAMF7 (signaling lymphocytic activation molecule F7), FLT3 (FMS-like tyrosine kinase 3), ROR1 (receptor tyrosine kinase-like orphan receptor 1), and CD138 [71, 72]. CD33 and FLT3 are suitable candidates for targeting leukemic cells, especially acute myeloid leukemia (AML). SLAMF7, BCMA, and CD138 are tumor antigens that have been targeted for the treatment of MM [73,74,75].
GvHD and allo-rejection are concerning events following allo-CAR-T therapy. GVHD occurs when donor T cells identify recipient’s tissues as foreign and attack them, which leads to the inflammation and tissue damage. This process is caused by the activation of T cells and the release of inflammatory cytokines and disruption of immune responses, resulting in tissue destruction and clinical manifestations of GVHD [76]. Allo-CAR-T rejection is when the host immune system identifies donor T cells as a foreign factor and produces an immune response to eliminate them. This rejection is driven by different mechanisms that include alloreactivity of donor T cells against recipient antigens, host-versus-graft immune responses, and the release of pro-inflammatory cytokines that lead to cytotoxicity [76]. Several strategies have been developed to eliminate these complications. Most of these strategies require extensive suppression of the host’s immune system (such as the use of drugs such as anti-CD52 monoclonal antibody alemtuzumab and fingolimod) for prevention of allo-rejection, which are basically not ideal for use in an immunotherapy approach [43]. The other strategies have been focused on the use of gene-editing-or cell source-based approaches to eliminate GvHD and allo-rejection risks while maintaining the efficacy of allo-CAR-Ts in HMs.
Genome-edited allo-CAR-Ts
The gene modification methods for disrupting the allogeneicity-associated loci are critical in generating an “off-the-shelf” allogeneic CAR-T cell. There are three strategies employed for target-specific gene manipulation, including transcription activator-like nucleases (TALENs), zinc finger nucleases (ZFN), and clustered regularly interspaced short palindromic repeats (CRISPR)/CRISPR-associated protein 9 (Cas9). ZFN and TALEN technologies are based on the protein-guided DNA editing systems used in allogeneic CAR-T cell generation [43]. TALEN is a critical gene-editing tool for HLA deficiency in CAR-T cells to generate an “off-the-shelf” allogeneic product. On the other hand, ZFN is a DNA-cleavage domain fussed to zinc finger DNA-binding domain aimed at site-specific DNA manipulation. In recent studies, ZFN was used to produce the allogeneic adoptive T cells by targeting β2M and TRAC [77]. Also, I-Crel ARCUS® (developed by Precision Biosciences) is a gene-editing platform based on a monomerized I-CreI meganuclease developed for TRAC [78, 79]. TRAC-specific I-Crel ARCUS was subjected to generate allo-CAR-Ts applied in hematologic malignancies, i.e., B-cell non-Hodgkin lymphoma and B-ALL [80]. CRISPR-Cas9 is an RNA-guided DNA editing tool that has been developed with minor off-target gene editing. Also, megaTAL, a meganuclease fused to a transcription activator-like (TAL) domain, is a highly efficient gene modifier to TCR targeting [81].
The CRISPR-Cas9 system is widely used to create allogeneic CAR-T cells by disruption of β2M and TCRαβ loci in donated cells. To loci disruption, conventional CRISPR-Cas9 makes a double-strand break (DSB) in the target site, while non-homology end joining (NHEJ) and homology-directed repair (HDR) come to ligate the nucleotides present in breaks [82]. For the reduction of the off-target effect of the CRISPR system in the generation of allo-CAR-Ts, “Cas-CLOVER” technology was developed as a novel high-fidelity nuclease. In this gene editing tool, an RNA-guided endonuclease including Clo051 nuclease/dead Cas9 (dCas9) fusion is used. The results showed that the off-target activity of Cas-CLOVER was significantly reduced compared to the conventional CRISPR-based editing method without affecting the activation, cytokine secretion, and proliferation of allo-CAR-Ts. Also, in vivo experiments in xenograft models confirmed this finding [83].
Other mechanisms have been developed to overcome this challenge, e.g., dCas9 and nickase-mutated Cas9, which have inactivating mutations in nucleolytic domains. dCas9 can be fused to DNA modifiers, which promote a base alteration without DSB [84, 85]. Therefore, inducing inactivating mutations in β2M and TRAC loci in CAR-T cells via dCas9 could be a promising tool for generating a safe “off-the-shelf” allogeneic CAR immune cell without off-target gene DSB. Also, a multiplex CRISPR-Cas9 could be used for simultaneous loci disruption. For example, it is possible to delete the PDCD-1 locus (encoding PD-1) as well as β2M/TCRαβ loci in a CAR cell to avoid immune checkpoint inhibition in allogeneic CAR-T cells [86].
Overall, TALEN and ZFN have more precision than CRISPR in an off-target manner. The modality of ZFN domains allows customization to enhance target-specific binding to DNA sequences. In this regard, the first generations of CRISPR were potent at binding to similar but not identical sequences. Recently, the development of high-fidelity Cas9 variants reduced the off-target effect of CRISPR. Recent advancements in CRISPR regarding adaptability and simplicity introduce CRISPR-centric tools as suitable technology for further gene manipulation [87].
With the advent of gene editing techniques, a practical and permanent approach has been developed to resolve the immunological reactions by removing the endogenous TCR and HLA class 1 by targeting the constant regions of TCRα/β and β2M regions, respectively [88]. Although there are no detailed studies on the role of HLA class 2 in alloreactive reactions, it has been shown that HLA class 2 has increased expression in activated T cells through class II major histocompatibility complex transactivator (CIITA) [89]. Since donor-driven T cells undergo activation during the process of ex vivo expansion, it is possible that disruption of HLA class 2 along with HLA class 1 play a greater role in dealing with allo-rejection reactions. Disruption of both HLA class 1 and 2, as well as endogenous TCR by genetic deletion of β2M, CIITA, and TRAC regions by the Cas9 system and their transduction by a CD19CAR, has shown that triple knock-out cells have a better survival rate than T cells that are HLA-sufficient without inducing GvHD. So, it was shown that the simultaneous removal of HLA class 1 and 2 contributes to the survival of allogeneic cells and increases their resistance to removal by host PBMCs [90].
Although disrupting the TCR and β2M regions seems to be an attractive approach, it can lead to the elimination of HLA(-) cells when confronted with host NK cells. A universal immune-evasive allo-CAR-T platform called ΔTRACCARΔβ2MHLAE has been developed as a promising strategy to deal with the unfavorable function of host NK cells. This platform has been effectively produced by the disruptive insertions of CAR and HLA-E (a non-polymorphic inhibitor of NK) genes in the TRAC and β2M loci by multiplex gene editing with TALEN and AAV6 promoter-less DNA repair matrix. In this proof-of-concept study, two CAR structures were used against the hematological antigens CD22 and CD123. The efficiency of co-inactivating the TRAC and β2M regions and creating TCRαβ(−) HLA-ABC(−) T cells in this study was about 96%, and the rate of simultaneous expression of CAR and HLA-E in these cells was about 70%. This unbiased method can introduce the CAR complex and HLA-E complex in the desired sites. Allo-CAR-Ts against CD22 and CD123 showed similar antitumor activity against RAJI and MOLM13 target cells, respectively. Moreover, the targeted knock-out of the β2Mlocus protects the engineered cells against the attacks of alloreactive T cells. Finally, evaluations using the hIL-15 NOG mouse model showed that ΔTRACCARΔβ2MHLAE T cells are resistant to NK attacks [91].
Regarding the role of CD47 in the inhibition of macrophage and NK cell-mediated killing, allo-CAR-Ts were designed to eliminate allo-rejection through the CD47 overexpression on engineered T cells. To produce these hypoimmune allo-CD19CARs, the β2M, CIITA, and TCR regions were removed by gene editing, and lentiviral transduction was used to overexpress CD47 and CD19CAR. These allo-CD19CARs were markedly able to evade activated mouse T cells in humanized mice, whereas the transplanted non-hypoimmune allo-CD19CARs lacked this capability. Furthermore, immune cell assays demonstrated that CD47 overexpression protected hypoimmune allo-CD19CARs from allo-rejection by NK cells and macrophages, whereas they retained their cytotoxic properties on B cell leukemia models. The use of an anti-CD47 antibody eliminated this protective effect against NK cells and macrophages, which indicates the importance of CD47 overexpression by allo-CD19CARs. These studies showed that the in vivo antitumor efficacy of hypoimmune allo-CD19CARs was similar to unedited control allo-CD19CARs. Therefore, these hypoimmune allo-CD19CARs can be a good option to use in sensitized patients [92].
Current approaches for engineering cells of allogeneic origin are based on the use of viral vectors. Despite the widespread use of viral vectors to deliver the CAR gene to T cells, an unmet need is felt to cover some of the biosafety considerations that arise in the presence of replication-competent retroviruses. The use of transposons with distinct advantages such as higher gene transfer capacity, cost-effectiveness, and relatively random integration profiles compared with the biased integration pattern of integrating viral vectors has made them an attractive option for replacing viral vectors. For example, Sleeping Beauty (SB) transposons and minicircles (mc) were used to deliver a CD19CAR and TCR gene-specific CRISPR-Cas9 ribonucleoparticles (RNP) to produce allo-CAR-Ts. The effectiveness of this system was confirmed through robust TCR knock-out, high CD19CAR expression, and low cytotoxicity. The use of mc-harboring SB transposons can increase the transfection and transposition rates and reduce the DNA-associated cytotoxicity occurring in plasmid-based SB transposons. This method allows rapid production of TCR-KO CAR-T cells targeting CD19 antigen through transient CAR expression. These SB-engineered allo-CD19CARs indicated potent antitumor activities and alleviated xenogeneic GvHD development in a xenograft model of B-cell leukemia. This study showed for the first time that the combination of SB transposons and CRISPR-Cas9 can be used as an efficient approach to produce allogeneic TCR-disrupted CD19CAR-T cells [93]. Despite the advantages that have made the piggyBac system an option for stable gene integration, attention to its safety aspects and continuous follow-up of patients receiving engineered cells with this method is very important. The results of phase 1 clinical studies to investigate the treatment outcomes in patients receiving donor-derived piggyBac CD19CAR-T cells for B lymphocyte malignancies indicated the development of a secondary malignancy in two cases of the patients involved in the study. The evaluations showed the high transgene copy number per cell and genetic changes such as point mutations and background genomic copy-number variations but no insertion into typical oncogenes [94].
Most allo-CAR-Ts are created by gene editing techniques such as zinc finger nucleases, TALEN, and CRISPR-Cas based on the creation of DNA DSBs, which may lead to unexpected outcomes like unwanted on-target editing. These abnormalities caused by DSBs have been the cause of stopping many allo-CAR-Ts in clinical studies (NCT04416984). The base editing technique is a new technology for programmed induction of single base pair changes at defined genomic loci with high precision and efficiency. Cytosine base editors (CBEs) work by combining the functions of single-stranded DNA deaminase and nickase enzymes to induce C*G to T*A point mutations. To evaluate the potential of CBE technique in creating improved CAR-T cells, it was used for developing 7CAR8, an allo-CAR-T against CD7 surface marker to treat R/R T-ALL. 7CAR8 contains four simultaneous base edits to not express CD52, CD7, PD1, and TCRα proteins. Electroporation of mRNA encoding CBE and four synthetic gRNAs changed all four regions with an efficiency above 90%, and 81.4% of all T cells expressed the CAR receptor in addition to base edits. Unlike the multiple editing of T cells by the previous techniques (e.g., CRISPR/Cas9), multiplexed editing of the cells with CBE mRNA does not affect T cell proliferation, leading to karyotypic abnormalities, or increase the expression of genes involved in DNA damage or proapoptotic pathways. Strong preclinical data of this study using patient-derived xenograft models showed that 7CAR8 can be considered a high-efficiency therapeutic option for T-ALL treatment [95].
On the other hand, simultaneous multiplex editing with CRISPR/Cas9 may make T cells prone to genomic rearrangements and hamper the safety of allo-CAR-Ts. Therefore, designing an efficient CRISPR/Cas9 system that can perform simultaneous multiplex editing while impeding the risk of genomic translocations has remained a challenge. A CRISPR/Cas9 system is designed to overcome this problem through CRISPR nucleases with distinct evolutionary origins, e.g., Cas12a Ultra for CAR knock-in and a Cas9-derived base editor for knock-out of both HLA class 1 and 2 [96]. This system enables the production of safer allo-CAR-Ts with efficient triple-editing in a one-step procedure.
Allo-CAR-Ts besides engineered αβ T cells
In a source-based approach, reprogrammed T-cell-derived induced pluripotent stem cells (TiPS) were used for the large-scale production of off-the-shelf CAR-T cells. Transduction of TiPS with CD19CAR demonstrated that these cells differentiate towards an innate-like CD8αα or CD4−CD8αβ− T cell phenotype, possibly due to the premature expression of TCR or constitutively expression of CAR in TiPS [97]. The attenuation of CAR signaling through inserting point mutations in the immunoreceptor tyrosine activation motifs (ITAM) 2 and 3 of the CD3ζ domain and the regulation of the CAR expression through the TRAC promoter-controlled expression led to the induction of the CD4+CD8αβ+ double-positive T cells. After stimulation with CD19 antigen, double-positive T cells matured to CD8αβ single positive T cells with the ability to exert in vivo antitumor activities against leukemia cells without any GvHD symptoms [97].
Unlike the gene-edited approaches, which require endogenous TCR inactivation to reduce the risk of GvHD, allogeneic Epstein-Barr Virus targeted T (EBV-T) cells represent a therapeutic potential for clinical use. As an allo-CAR-T platform, EBV-T cells show a unique capacity for function and transducibility along with low allo-rejection and low CRS risk without the need to induce complex gene editing [98]. ATA3219 is a next-generation allogeneic CD19CAR-T cell that has combined the characteristics of a non-edited allogeneic EBV-T cell with an improved CAR signaling domain. In this therapy, EBV-T cells were engineered with a CD19CAR containing a modified CD3ζ signaling domain (entitled CD19-1XX-CAR EBV-T cells) and have shown high expression of the chimeric receptor, polyfunctionality, high persistence, and potent antitumor activity against CD19+ tumor cells. In addition, these engineered cells have shown an acceptable safety profile without any toxicity in an animal model of ALL [88].
γδ T cells, which have both innate and adaptive mechanisms for identifying and killing malignant cells, are another cell source that can be an attractive platform for the production of allo-CAR-Ts. Delta One T cells (DOTs), MHC/HLA-independent Vδ1 γδ T cells generated from the peripheral blood of healthy donors, have successfully been used in allogeneic cell therapy.CD123CAR-DOTs, 4-1BB-based CAR-DOTs against AML target antigen CD123, showed higher and stronger cytotoxicity than control cells on AML cell lines and primary samples both in vitro and in vivo. Continuous administration of IL-15 caused long-term persistence of single-dose CD123CAR-DOTs in patient-driven xenograft models. The results of this study have been considered as proof-of-concept for an allogeneic next-generation therapy based on CD123CAR-DOTs for R/R AML patients. Due to their potent cytotoxic activity, the release of stimulating cytokines, and the recruiting of other immune cells to the tumor site, γδ T cells are considered a hopeful cell source for allo-CAR-T manufacturing [99]. Moreover, the results of a study that investigated the ability to produce and function of allogeneic peripheral blood-derived γδ CAR-T cells against hematological marker CD20 provided more valuable information in this field. It was indicated that Vδ1 γδ CD20-CAR-T cells have good intrinsic and acquired antitumor functions, including T-cell proliferation, proinflammatory cytokine secretion, and durable tumor growth inhibition of B-cell lymphoma xenografts in immunodeficient mice. In addition, Vδ1 γδ CD20-CAR-T cells did not induce xenogeneic GvHD or other toxicities in the lymphoma mouse model. The preclinical results of this study introduced ADI-001, the allogeneic Vδ1 γδ CD20-CAR-T cell, as a valuable therapeutic option [100]. Table 1 shows the results of the latest advances in allo-CAR-T preclinical studies.
Clinical outcomes of allo-CAR-Ts in hematological malignancy
Due to the promising results of preclinical studies, there are various clinical trials regarding the application of allo-CAR-Ts in HMs, i.e., myelomas, lymphomas, and leukemias (Table 2). Among them, CD19, CD20, CD22, BCMA, CD7, and CD123 are the most common targeted antigens. Also, TALEN and CRISPR/Cas9 were the safest platforms used in clinical grade allo-CAR-Ts. Among the various undergoing clinical trials on allogeneic CAR-T cell therapy in HMs, there are just two completed phase I clinical trials regarding the application of “UCART19”, universal CD19CAR-T cells (NCT02746952 and NCT02808442) and “ALLO-715”, universal BCMA-CAR-T cells [102, 103].
In UCART19’s study, the allogeneic CD19CAR-T cells were derived from a healthy donor, and TCRαβ and CD52 were disrupted simultaneously via TALEN while all patients received anti-CD52 therapy. This study was divided into two trials: (i) on seven pediatric ALL patients aged six months to 18 years old (NCT02808442), and (ii) on fourteen adult ALL patients aged 18 to 70 years old (NCT02746952). Pediatric ALL patients received 1.1–2.3 × 106 cells/kg, while adult ALL patients received escalating doses (6 × 106, 6–8 × 107, and 1.8–2.4 × 108 cells/kg) to determine the maximum tolerated dose. Also, patients received cyclophosphamide, alemtuzumab, and fludarabine before the trial initiation. Around fourteen days after infusion, the maximum expansion of UCART19 was achieved. The published results of NCT02746952 showed the ORR (overall response rate) was 48% and the overall survival was 13.4 months. Also, CRS (grade 3 or higher) and neurotoxicity were reported in 24% and 4% of patients, respectively [104].
The treatment with UCART19 resulted in some adverse effects comparable to those associated with autologous CD19CAR-T cells. Among 21 treated patients, 91% of patients experienced CRS, 62% showed infection, and 38% showed neurotoxicity. Prolonged cytopenia, associated with the myelosuppressive effects of intensive lymphodepletion, was seen in 32% of patients. Two patients manifested pathology-confirmed skin grade 1 acute GvHD. After the allogeneic stem cell transplantation, four patients showed GvHD (up to grade 3). UCART19 was also applied for two infants with relapsed B-cell ALL. Both children achieved CR and showed 5-year disease-free manifestation. Overall, UCART19 was generally a “safe” off-the-shelf CAR-T cell product compared to autologous CAR-T cells [43].
Another completed clinical study on allo-CAR-Ts was the application of ALLO-715 for treating MM patients. In this study, 320 × 106 ALLO-715 cells were administered to target BCMA+ MM cells after a lymphodepletion regimen by alemtuzumab, fludarabine, and cyclophosphamide. The findings showed that 25% of patients showed complete response, and 45.8% showed partial response. CRS and neurotoxicity were observed in 55.8% and 14% of patients, respectively [105]. The results of these clinical trials showed the promising efficacy of allo-CAR-Ts in R/R HMs.
Besides, auto-CAR-Ts also showed the same adverse effects as allo-CAR-Ts. For example, a clinical trial of Axicabtagene Ciloleucel CD19 auto-CAR-Ts showed 13% CRS (grade 3 or higher) and 28% neurotoxicity [106]. Also, in a clinical trial of KTE-X19 auto-CAR-Ts on R/R mantle-cell lymphoma, 15% CRS (grade 3 or higher) and 31% neurotoxicity were reported [107].
Overall, allo-CAR-Ts showed significant results in the clinical administration of hematological malignancies without any extra adverse effects compared to conventional CAR-T cell therapy. However, allo-CAR-T therapy for patients with HMs is not without challenges. Despite the TCR ablation in allo-CAR-Ts, different clinical data have shown various occurrences of GvHD in treated patients. For example, although allo-CAR-Ts with disrupted TCR against R/R MM have shown no GvHD side effects, TCR-disrupted allo-CAR-Ts against R/R leukemia led to GvHD grades 1 or 2 [43, 102, 108]. The GvHD frequency and intensity could be reduced by applying T cells from UCB instead of adult blood T cells. Actually, UCB cells can have lower reactivity owing to a reduced Th1/Th2 cytokine profile as well as the lower activation of the NFAT pathway after primary antigenic stimuli, thus leading to the lower production of several proinflammatory cytokines [109,110,111]. Also, using other non-αβ cell sources such as mucosal-associated invariant T (MAIT) cells, NK, or γδ T-cells may eliminate GvHD risk [112,113,114].
On the other hand, in spite of lymphodepletion with fludarabine and cyclophosphamide, allo-CAR-T therapy was not effective in some leukemic patients because allo-CAR-Ts were not able to expand and showed no antitumor activity [102]. It is likely due to the allo-rejection of the engineered lymphocytes because patients showed antitumor responses and in vivo expansion only if an extra lymphodepletion agent like an anti-CD52 antibody was administered. Indeed, in addition to knocking-out the TCR, these allo-CAR-Ts were engineered for the disruption of the CD52 locus, which is expressed on the surface of lymphocytes, to allow lymphodepletion through alemtuzumab without affecting the allo-CAR-Ts [115]. This can also help to eliminate the unmodified CAR-T cells by an antibody-based selection. Therefore, alongside the allo-CAR-Ts infusion, administration of an anti-CD52 antibody can control the allo-rejection and potentially enhance the persistence and efficacy of the injected allo-CAR-Ts [116]. Nevertheless, it may expose the patients to an increased risk of severe sepsis and cytopenia due to the blocking of the host’s T-cell responses [43]. Preclinical data revealed that allo-CAR-Ts expressing an anti-4-1BB receptor, called alloimmune defense receptor (ADR), can overcome allo-rejection through the selective elimination of the host’s activated lymphocytes, including T and NK cells while maintaining resting T and NK cells [117].
The potential use of allo-CAR-T cells in the treatment of solid tumors
The nature of heterogenous and hostile tumor microenvironment (TME) with multi-suppressive factors of solid tumors are obstacles that limit effectiveness of autoCAR-T therapy as well as their translation to clinic. Therefore, targeting simultaneous multiple factors besides advantages of alloCAR-Ts may be an effective strategy to overcome on these challenges. The use of gene editing tools and their ability to target multiple T cell genes provide an opportunity to manufacture allo-CAR-Ts with greater efficiency and safety for solid tumor treatment. For example, simultaneous deletion of genes such as CD52 and TCR, as well as knock-in a CD70CAR, leads to the production of fratricide-resistant allo-CAR-Ts (allo-316) with increased expansion, persistence, and antitumor activity in vitro and in vivo [118]. CD70 is overexpressed in renal cell carcinoma (RCC) and in various malignancies like ALL. CD70 expression in normal tissues is limited to activated T and B lymphocytes and mature dendritic cells [119]. Masking CD70 on the allo-CAR-Ts by CD70CAR renders them resistant to fratricide. Moreover, allo-316 can be a promising treatment for CD70+solid tumors as it showed antitumor activities in RCC [118]. Combining an adenine base editor with a CRISPR-Cas12b nuclease can increase capacity of disruption genes to six genes to manufacture allo-CAR-Ts resistance to solid tumors TME. Disruption of alloreactive antigens such as TCR (CD3E-KO), HLA class-I (B2M-KO) and HLA class-II (CIITA-KO), along with inhibitory factors of biochemical (adenosine, ADORA2A) and immunological (TGFb (TGFBR2) and PD-L1 (PDCD1)) can lead to generation of alloCAR-Ts with superior anti-tumor efficacy against TME [120]. Injection of these alloCAR-Ts into humanized mouse models showed enhanced tumor clearance and survival rates.
CYAD-101 is a non-gene edited alloCAR-T cell that co-express a NKG2D receptor and a TCR inhibitory molecule (TIM). NKG2D receptor, is expressed on NK cells and T cells, can triggers anti-tumor activity of the effector immune cells when bound to its ligands, which overexpressed on human colorectal, cervical, nasopharyngeal carcinomas and stressed cells as well as low-expressed on healthy adult tissues [121,122,123]. To eradicate GVHD, CYAD-101 inhibited signaling TCR via expressing TIM. Clinical results of CYAD-101 in combination with chemotherapy (FOLFOX) showed a good safety profile without any GVHD or treatment-related adverse events ≥ Grade 3 [124]. The efficacy was encouraging, with 13% partial response and 60% stable disease in patients with mCRC [124]. Whereas, a NKG2D-based autoCAR-T cell, CYAD-01, therapy in combination with chemotherapy showed no clinical efficacy (NCT02203825). In the next trial, CYAD-101 administrated with an anti-PD-1 (pembrolizumab) to be enhanced clinical efficacy and durability of responses in patients with mCRC (NCT04991948).
Taken together, AlloCAR Ts can be modified to resist immunosuppressive signals present in the solid TME, such as inhibitory cytokines (TGF-b, IL10), inhibitory molecules (adenosine) and regulatory T cells. This enhancement of T-cell function may improve CAR T-cell persistence and antitumor activity within the hostile tumor milieu. Also, the availability of off-the-shelf allo-CAR-T cell products opens up opportunities for combination therapies with other immunomodulatory agents, such as checkpoint inhibitors (PD1, CTLA4) or cytokines, to further enhance antitumor immune responses and overcome resistance mechanisms in solid tumors.
Conclusions
Allogeneic manufacturing of CAR-T cells can address some of the limitations of auto-CAR-Ts. Less manufacturing time (time is saved for more than six weeks in allo-CAR-T therapy compared to auto-CAR-Ts [108]), fitter cell sources, simple scaling up, standardization of manufacturing process in the GMP context, and storing different therapeutic dosages of allo-CAR-Ts make them as cost-effective and affordable drugs than auto-CAR-Ts. Allo-CAR-Ts can reduce the cost of CAR-T cell therapy from $300,000-$475,000 per dose to $3990-$10,000 [31, 125, 126]. Furthermore, allo-CAR-Ts have the advantage of eliminating the need for bridging therapy and the risk of unintentional contamination of CAR-T cells with tumor cells in patients with hematological malignancies. The gene editing or cell-based strategies can resolve the GvHD and allo-rejection complications of allo-CAR-Ts. Gene editing approaches, including TALEN, CRISPR/Cas, and ZFN, are used to delete immunoreactive markers such as TCR α/βand β2M loci in conventional primary T cells and other cell types. However, the allo-rejection of HLA-deficient T cells can still occur through their targeting by host NK cells. Expression of NK cell inhibitors (e.g., HLA-E) besides deletion of the HLA region in allogeneic T cells can overcome this issue. Preclinical studies showed that multiplex disruption of HLA class 1 and 2 and TCR, along with CAR insertion, can enhance the antitumor efficacy and safety of allo-CAR-Ts. Furthermore, deletion of CD52 in allo-CAR-Ts can prevent allo-rejection if an anti-CD52 antibody is administered along with allo-CAR-Ts for lymphodepletion. However, cytopenia resulting from lymphodepletion can be a possible adverse event in the clinical setting. In cell-based strategies, γδ T cells (e.g., Vδ1 γδ T cells), T-cell-derived induced pluripotent stem cells, lymphoid progenitors, and donor-derived EBV-targeted T cells can be used as the raw material for allo-CAR-Ts manufacturing without any need to gene editing to eliminate GvHD or allo-rejection.
Most allo-CAR-Ts in clinical trials have been submitted for hematological malignancies. It can be due to the lack of tumor-specific antigens in solid tumors and the resulting off-target toxicity, as well as the less complexity of hematological malignancies, including the existence of fewer suppressor cells like circulating MDSCs or regulatory T cells in these patients. On the other hand, despite the simpler CRISPR/Cas system design, most clinical trials have applied the TALEN tool to engineer T cells for allogeneic use. A main potential reason for this can be the off-target and translocation risks of the CRISPR/Cas technique observed in several studies [103, 127, 128]. Novel designs of the CRISPR/Cas system can improve its safety for application in allo-CAR-T manufacturing.
Although allo-CAR-Ts have demonstrated antitumor efficacy and safety profile similar to auto-CAR-Ts in patients with hematological malignancies, more studies are needed for solid tumors. The possibility of multiplex gene editing of allo-CAR-Ts turns them into great candidates with high therapeutic potential for different cancers.
Data availability
not applicable.
References
Rodriguez-Abreu D, Bordoni A, Zucca E. Epidemiology of hematological malignancies. Ann Oncol. 2007;18(Suppl 1):i3–8.
Maali A, Gholizadeh M, Feghhi-Najafabadi S, Noei A, Seyed-Motahari SS, Mansoori S, Sharifzadeh Z. Nanobodies in cell-mediated immunotherapy: on the road to fight cancer. Front Immunol. 2023;14:1012841.
Hajari Taheri F, Hassani M, Sharifzadeh Z, Behdani M, Arashkia A, Abolhassani M. T cell engineered with a novel nanobody-based chimeric antigen receptor against VEGFR2 as a candidate for tumor immunotherapy. IUBMB Life. 2019;71(9):1259–67.
Hassani M, Hajari Taheri F, Sharifzadeh Z, Arashkia A, Hadjati J, van Weerden WM, Modarressi MH, Abolhassani M. Construction of a chimeric antigen receptor bearing a nanobody against prostate a specific membrane antigen in prostate cancer. J Cell Biochem. 2019;120(6):10787–95.
Wong DP, Roy NK, Zhang K, Anukanth A, Asthana A, Shirkey-Son NJ, Dunmire S, Jones BJ, Lahr WS, Webber BR, et al. A BAFF ligand-based CAR-T cell targeting three receptors and multiple B cell cancers. Nat Commun. 2022;13(1):217.
Mansoori S, Gholizadeh M, Abdoli S, Ajdary S, Shokrgozar MA, Basiri M, Sharifzadeh Z. Design and development of CAR-T cells for cancer therapy. 2023.
Zheng Z, Li S, Liu M, Chen C, Zhang L, Zhou D. Fine-tuning through generations: advances in structure and production of CAR-T therapy. Cancers (Basel) 2023, 15(13).
Sharifzadeh Z, Rahbarizadeh F, Shokrgozar MA, Ahmadvand D, Mahboudi F, Jamnani FR, Moghimi SM. Genetically engineered T cells bearing chimeric nanoconstructed receptors harboring TAG-72-specific camelid single domain antibodies as targeting agents. Cancer Lett. 2013;334(2):237–44.
Jain MD, Coney P, Locke FL. Bringing CAR-T to the clinic. Gene Cell Immunotherapy Cancer 2022:165–80.
Arcangeli S, Falcone L, Camisa B, De Girardi F, Biondi M, Giglio F, Ciceri F, Bonini C, Bondanza A, Casucci M. Next-Generation Manufacturing protocols enriching T(SCM) CAR T cells can overcome Disease-specific T cell defects in Cancer patients. Front Immunol. 2020;11:1217.
Bonig H, Chabannon C, Lozano M. Providing the Starting Material to the Manufacturer of an Approved and Commercially Available Autologous CAR-T Cell Treatment. In: The EBMT/EHA CAR-T Cell Handbook Edited by Kroger N, Gribben J, Chabannon C, Yakoub-Agha I, Einsele H. Cham (CH); 2022: 31–36.
Papathanasiou MM, Stamatis C, Lakelin M, Farid S, Titchener-Hooker N, Shah N. Autologous CAR T-cell therapies supply chain: challenges and opportunities? Cancer Gene Ther. 2020;27(10–11):799–809.
Kohl U, Arsenieva S, Holzinger A, Abken H. CAR T cells in trials: recent achievements and challenges that remain in the production of modified T cells for clinical applications. Hum Gene Ther. 2018;29(5):559–68.
Jensen MC, Popplewell L, Cooper LJ, DiGiusto D, Kalos M, Ostberg JR, Forman SJ. Antitransgene rejection responses contribute to attenuated persistence of adoptively transferred CD20/CD19-specific chimeric antigen receptor redirected T cells in humans. Biol Blood Marrow Transpl. 2010;16(9):1245–56.
Shah NN, Fry TJ. Mechanisms of resistance to CAR T cell therapy. Nat Rev Clin Oncol. 2019;16(6):372–85.
Munshi NC, Anderson LD Jr., Shah N, Madduri D, Berdeja J, Lonial S, Raje N, Lin Y, Siegel D, Oriol A, et al. Idecabtagene Vicleucel in Relapsed and Refractory multiple myeloma. N Engl J Med. 2021;384(8):705–16.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, Bader P, Verneris MR, Stefanski HE, Myers GD, et al. Tisagenlecleucel in Children and Young adults with B-Cell lymphoblastic leukemia. N Engl J Med. 2018;378(5):439–48.
Park JH, Riviere I, Gonen M, Wang X, Senechal B, Curran KJ, Sauter C, Wang Y, Santomasso B, Mead E, et al. Long-term follow-up of CD19 CAR therapy in Acute Lymphoblastic Leukemia. N Engl J Med. 2018;378(5):449–59.
Tbakhi B, Reagan PM. Chimeric antigen receptor (CAR) T-cell treatment for mantle cell lymphoma (MCL). Ther Adv Hematol. 2022;13:20406207221080738.
Abramson JS, Palomba ML, Gordon LI, Lunning MA, Wang M, Arnason J, Mehta A, Purev E, Maloney DG, Andreadis C, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839–52.
Delgado J, Roddie C, Schmitt M. Point-of-Care Production of CAR-T Cells. In: The EBMT/EHA CAR-T Cell Handbook Edited by Kroger N, Gribben J, Chabannon C, Yakoub-Agha I, Einsele H. Cham (CH); 2022: 45–49.
Castella M, Caballero-Banos M, Ortiz-Maldonado V, Gonzalez-Navarro EA, Sune G, Antonana-Vidosola A, Boronat A, Marzal B, Millan L, Martin-Antonio B, et al. Point-Of-Care CAR T-Cell production (ARI-0001) using a closed semi-automatic bioreactor: experience from an academic phase I clinical trial. Front Immunol. 2020;11:482.
Schubert ML, Schmitt A, Sellner L, Neuber B, Kunz J, Wuchter P, Kunz A, Gern U, Michels B, Hofmann S, et al. Treatment of patients with relapsed or refractory CD19 + lymphoid disease with T lymphocytes transduced by RV-SFG.CD19.CD28.4-1BBzeta retroviral vector: a unicentre phase I/II clinical trial protocol. BMJ Open. 2019;9(5):e026644.
Engels B, Zhu X, Yang J, Price A, Sohoni A, Stein AM, Parent L, Greene M, Niederst M, Whalen J. Preservation of T-cell stemness with a novel expansionless CAR-T manufacturing process, which reduces manufacturing time to less than two days, drives enhanced CAR-T cell efficacy. Blood. 2021;138:2848.
Ghassemi S, Durgin JS, Nunez-Cruz S, Patel J, Leferovich J, Pinzone M, Shen F, Cummins KD, Plesa G, Cantu VA, et al. Rapid manufacturing of non-activated potent CAR T cells. Nat Biomed Eng. 2022;6(2):118–28.
Rodrigues M, Duran E, Eschgfaeller B, Kuzan D, Habucky K. Optimizing commercial manufacturing of tisagenlecleucel for patients in the US: a 4-year experiential journey. Blood. 2021;138:1768.
Singh N, Perazzelli J, Grupp SA, Barrett DM. Early memory phenotypes drive T cell proliferation in patients with pediatric malignancies. Sci Transl Med. 2016;8(320):320ra323.
Netsrithong R, Wattanapanitch M. Advances in adoptive cell therapy using Induced pluripotent stem cell-derived T cells. Front Immunol. 2021;12:759558.
Blaeschke F, Stenger D, Kaeuferle T, Willier S, Lotfi R, Kaiser AD, Assenmacher M, Doring M, Feucht J, Feuchtinger T. Induction of a central memory and stem cell memory phenotype in functionally active CD4(+) and CD8(+) CAR T cells produced in an automated good manufacturing practice system for the treatment of CD19(+) acute lymphoblastic leukemia. Cancer Immunol Immunother. 2018;67(7):1053–66.
Fraietta JA, Lacey SF, Orlando EJ, Pruteanu-Malinici I, Gohil M, Lundh S, Boesteanu AC, Wang Y, O’Connor RS, Hwang WT, et al. Determinants of response and resistance to CD19 chimeric antigen receptor (CAR) T cell therapy of chronic lymphocytic leukemia. Nat Med. 2018;24(5):563–71.
Jenkins MJ, Farid SS. Cost-effective bioprocess design for the manufacture of allogeneic CAR-T cell therapies using a decisional tool with multi-attribute decision-making analysis. Biochem Eng J. 2018;137:192–204.
MacLeod DT, Antony J, Martin AJ, Moser RJ, Hekele A, Wetzel KJ, Brown AE, Triggiano MA, Hux JA, Pham CD, et al. Integration of a CD19 CAR into the TCR Alpha Chain Locus streamlines production of allogeneic gene-edited CAR T cells. Mol Ther. 2017;25(4):949–61.
Bach PB. National Coverage Analysis of CAR-T therapies - Policy, evidence, and payment. N Engl J Med. 2018;379(15):1396–8.
Fiorenza S, Ritchie DS, Ramsey SD, Turtle CJ, Roth JA. Value and affordability of CAR T-cell therapy in the United States. Bone Marrow Transpl. 2020;55(9):1706–15.
Bartolo-Ibars A, Uribe-Herranz M, Munoz-Sanchez G, Arnaldos-Perez C, Ortiz-Maldonado V, Urbano-Ispizua A, Pascal M, Juan M. CAR-T after Stem Cell Transplantation in B-Cell Lymphoproliferative Disorders: Are They Really Autologous or Allogenic Cell Therapies? Cancers (Basel) 2021, 13(18).
Qasim W. Allogeneic CAR T cell therapies for leukemia. Am J Hematol. 2019;94(S1):S50–4.
Mehta PH, Fiorenza S, Koldej RM, Jaworowski A, Ritchie DS, Quinn KM. T cell fitness and autologous CAR T cell therapy in Haematologic Malignancy. Front Immunol. 2021;12:780442.
Graham C, Jozwik A, Pepper A, Benjamin R. Allogeneic CAR-T Cells: More than Ease of Access? Cells 2018, 7(10).
Lozano-Ojalvo D, Lopez-Fandino R, Lopez-Exposito I. PBMC-Derived T Cells. In: The Impact of Food Bioactives on Health: in vitro and ex vivo models Edited by Verhoeckx K, Cotter P, Lopez-Exposito I, Kleiveland C, Lea T, Mackie A, Requena T, Swiatecka D, Wichers H. Cham (CH); 2015: 169–180.
Radestad E, Wikell H, Engstrom M, Watz E, Sundberg B, Thunberg S, Uzunel M, Mattsson J, Uhlin M. Alpha/beta T-cell depleted grafts as an immunological booster to treat graft failure after hematopoietic stem cell transplantation with HLA-matched related and unrelated donors. J Immunol Res. 2014;2014:578741.
Wehler TC, Nonn M, Brandt B, Britten CM, Grone M, Todorova M, Link I, Khan SA, Meyer RG, Huber C, et al. Targeting the activation-induced antigen CD137 can selectively deplete alloreactive T cells from antileukemic and antitumor donor T-cell lines. Blood. 2007;109(1):365–73.
Cooper ML, Choi J, Staser K, Ritchey JK, Devenport JM, Eckardt K, Rettig MP, Wang B, Eissenberg LG, Ghobadi A, et al. An off-the-shelf fratricide-resistant CAR-T for the treatment of T cell hematologic malignancies. Leukemia. 2018;32(9):1970–83.
Qasim W, Zhan H, Samarasinghe S, Adams S, Amrolia P, Stafford S, Butler K, Rivat C, Wright G, Somana K et al. Molecular remission of infant B-ALL after infusion of universal TALEN gene-edited CAR T cells. Sci Transl Med 2017, 9(374).
Liu X, Zhang Y, Cheng C, Cheng AW, Zhang X, Li N, Xia C, Wei X, Liu X, Wang H. CRISPR-Cas9-mediated multiplex gene editing in CAR-T cells. Cell Res. 2017;27(1):154–7.
Depil S, Duchateau P, Grupp SA, Mufti G, Poirot L. Off-the-shelf’ allogeneic CAR T cells: development and challenges. Nat Rev Drug Discov. 2020;19(3):185–99.
Cutmore LC, Marshall JF. Current Perspectives on the Use of off the Shelf CAR-T/NK Cells for the Treatment of Cancer. Cancers (Basel) 2021, 13(8).
Makkouk A, Yang XC, Barca T, Lucas A, Turkoz M, Wong JTS, Nishimoto KP, Brodey MM, Tabrizizad M, Gundurao SRY et al. Off-the-shelf Vdelta1 gamma delta T cells engineered with glypican-3 (GPC-3)-specific chimeric antigen receptor (CAR) and soluble IL-15 display robust antitumor efficacy against hepatocellular carcinoma. J Immunother Cancer 2021, 9(12).
Maali A, Atashi A, Ghaffari S, Kouchaki R, Abdolmaleki F, Azad M. A review on Leukemia and iPSC Technology: application in Novel Treatment and Future. Curr Stem Cell Res Ther. 2018;13(8):665–75.
Maali A, Maroufi F, Sadeghi F, Atashi A, Kouchaki R, Moghadami M, Azad M. Induced pluripotent stem cell technology: trends in molecular biology, from genetics to epigenetics. Epigenomics. 2021;13(8):631–47.
Kotini AG, de Stanchina E, Themeli M, Sadelain M, Papapetrou EP. Escape mutations, Ganciclovir Resistance, and teratoma formation in human iPSCs expressing an HSVtk suicide gene. Mol Ther Nucleic Acids. 2016;5(2):e284.
Chang YL, Chen SJ, Kao CL, Hung SC, Ding DC, Yu CC, Chen YJ, Ku HH, Lin CP, Lee KH, et al. Docosahexaenoic acid promotes dopaminergic differentiation in induced pluripotent stem cells and inhibits teratoma formation in rats with Parkinson-like pathology. Cell Transpl. 2012;21(1):313–32.
Bedel A, Beliveau F, Lamrissi-Garcia I, Rousseau B, Moranvillier I, Rucheton B, Guyonnet-Dupérat V, Cardinaud B, de Verneuil H, Moreau-Gaudry F, et al. Preventing Pluripotent Cell Teratoma in Regenerative Medicine Applied to Hematology disorders. Stem Cells Transl Med. 2017;6(2):382–93.
Kim A, Lee SY, Kim BY, Chung SK. Elimination of Teratogenic Human Induced Pluripotent Stem cells by Bee Venom via Calcium-Calpain Pathway. Int J Mol Sci 2020, 21(9).
Park J, Lee DG, Lee NG, Kwon MG, Son YS, Son MY, Bae KH, Lee J, Park JG, Lee NK, et al. Monoclonal antibody K312-based depletion of pluripotent cells from differentiated stem cell progeny prevents teratoma formation. BMB Rep. 2022;55(3):142–7.
Kurtz A, Stacey G, Kidane L, Seriola A, Stachelscheid H, Veiga A. Regulatory insight into the European human pluripotent stem cell registry. Stem Cells Dev. 2014;23(Suppl 1Suppl 1):51–5.
Sullivan S, Stacey GN, Akazawa C, Aoyama N, Baptista R, Bedford P, Bennaceur Griscelli A, Chandra A, Elwood N, Girard M, et al. Quality control guidelines for clinical-grade human induced pluripotent stem cell lines. Regen Med. 2018;13(7):859–66.
Arias J, Yu J, Varshney M, Inzunza J, Nalvarte I. Hematopoietic stem cell- and induced pluripotent stem cell-derived CAR-NK cells as reliable cell-based therapy solutions. Stem Cells Transl Med. 2021;10(7):987–95.
Guillaume T, Gaugler B, Chevallier P, Delaunay J, Ayari S, Clavert A, Rialland F, Le Gouill S, Blin N, Gastinne T, et al. Escalated lymphodepletion followed by donor lymphocyte infusion can induce a graft-versus-host response without overwhelming toxicity. Bone Marrow Transpl. 2012;47(8):1112–7.
George B. Regulations and guidelines governing stem cell based products: clinical considerations. Perspect Clin Res. 2011;2(3):94–9.
Caldwell KJ, Gottschalk S, Talleur AC. Allogeneic CAR cell therapy-more than a Pipe Dream. Front Immunol. 2020;11:618427.
Hojjatipour T, Sharifzadeh Z, Maali A, Azad M. Chimeric antigen receptor-natural killer cells: a promising sword against insidious tumor cells. Hum Cell 2023.
Hu Y, Wang J, Zhang Y, Wei G, Xu H, Wu W, Yu J, Luo Y, Shi J, Liu S. Comparison of chimeric antigen receptor T cells from allogenic or autologous sources in patients with acute lymphoblastic leukemia. In.: American Society of Hematology Washington, DC; 2018.
Manier S, Jurczyszyn A, Vesole DH. Bridging Chemotherapy: Multiple Myeloma. In: The EBMT/EHA CAR-T Cell Handbook Edited by Kroger N, Gribben J, Chabannon C, Yakoub-Agha I, Einsele H. Cham (CH); 2022: 127–129.
Ladbury C, Dandapani S, Hao C, Fabros M, Amini A, Sampath S, Glaser S, Sokolov K, Yeh J, Baird JH et al. Long-term Follow-Up of bridging therapies prior to CAR T-Cell therapy for Relapsed/Refractory large B cell lymphoma. Cancers (Basel) 2023, 15(6).
Mailankody S, Matous JV, Liedtke M, Sidana S, Malik S, Nath R, Oluwole OO, Karski EE, Lovelace W, Zhou X. Universal: an allogeneic first-in-human study of the anti-BCMA ALLO-715 and the anti-CD52 ALLO-647 in relapsed/refractory multiple myeloma. Blood. 2020;136:24–5.
Neelapu SS, Nath R, Munoz J, Tees M, Miklos DB, Frank MJ, Malik SA, Stevens D, Shin CR, Balakumaran A. ALPHA study: ALLO-501 produced deep and durable responses in patients with relapsed/refractory non-hodgkin’s lymphoma comparable to autologous CAR T. Blood. 2021;138:3878.
Ruella M, Xu J, Barrett DM, Fraietta JA, Reich TJ, Ambrose DE, Klichinsky M, Shestova O, Patel PR, Kulikovskaya I, et al. Induction of resistance to chimeric antigen receptor T cell therapy by transduction of a single leukemic B cell. Nat Med. 2018;24(10):1499–503.
Jiménez-Cortegana C, Palazón-Carrión N, Garcia-Sancho AM, Nogales-Fernandez E, Carnicero-González F, Ríos-Herranz E, de la Cruz-Vicente F, Rodríguez-García G, Fernández-Álvarez R, Dominguez AR. Circulating myeloid-derived suppressor cells and regulatory T cells as immunological biomarkers in refractory/relapsed diffuse large B-cell lymphoma: translational results from the R2-GDP-GOTEL trial. J Immunother Cancer 2021, 9(6).
DiNofia AM, Grupp SA. Will allogeneic CAR T cells for CD19(+) malignancies take autologous CAR T cells ‘off the shelf’? Nat Rev Clin Oncol. 2021;18(4):195–6.
Marhelava K, Krawczyk M, Firczuk M, Fidyt K. CAR-T cells shoot for new targets: Novel approaches to boost adoptive cell therapy for B Cell-Derived malignancies. Cells 2022, 11(11).
Zhang X, Zhu L, Zhang H, Chen S, Xiao Y. CAR-T cell therapy in hematological malignancies: current opportunities and challenges. Front Immunol. 2022;13:927153.
Lu J, Jiang G. The journey of CAR-T therapy in hematological malignancies. Mol Cancer. 2022;21(1):194.
Sun C, Mahendravada A, Ballard B, Kale B, Ramos C, West J, Maguire T, McKay K, Lichtman E, Tuchman S, et al. Safety and efficacy of targeting CD138 with a chimeric antigen receptor for the treatment of multiple myeloma. Oncotarget. 2019;10(24):2369–83.
Cho SF, Anderson KC, Tai YT. Targeting B Cell Maturation Antigen (BCMA) in multiple myeloma: potential uses of BCMA-Based immunotherapy. Front Immunol. 2018;9:1821.
Sommer C, Cheng HY, Nguyen D, Dettling D, Yeung YA, Sutton J, Hamze M, Valton J, Smith J, Djuretic I, et al. Allogeneic FLT3 CAR T cells with an off-switch exhibit potent activity against AML and can be depleted to Expedite Bone Marrow Recovery. Mol Ther. 2020;28(10):2237–51.
Khurana A, Lin Y. Allogeneic Chimeric Antigen Receptor Therapy in Lymphoma. Curr Treat Options Oncol. 2022;23(2):171–87.
Lee GK, Liu P-q, Gandhi N, Truong L, Reik A, Lam S, Hinkley SJ, Miller JC, Paschon DE, Zhang L. 641. Highly efficient, ZFN-Driven knockout of Surface expression of the T-Cell receptor and HLA class I proteins in human T-Cells for enhancing allogeneic adoptive cell therapies. Mol Ther. 2016;24:S254.
Thompson AJ, Yuan X, Kudlicki W, Herrin DL. Cleavage and recognition pattern of a double-strand-specific endonuclease (I-creI) encoded by the chloroplast 23S rRNA intron of Chlamydomonas reinhardtii. Gene. 1992;119(2):247–51.
Dwivedi S, Purohit P, Vasudeva A, Kumar M, Agrawal R, Sheikh NA, Misra R, Kishore S, Misra S. Gene therapy and gene editing in healthcare. In: Biotechnology in Healthcare Elsevier; 2022: 147–175.
Shah BD, Jacobson C, Solomon SR, Jain N, Johnson MC, Vainorius M, Yu L, Heery CR, List AF, He F. Allogeneic CAR-T PBCAR0191 with intensified lymphodepletion is highly active in patients with relapsed/refractory B-cell malignancies. Blood. 2021;138:302.
Osborn MJ, Webber BR, Knipping F, Lonetree CL, Tennis N, DeFeo AP, McElroy AN, Starker CG, Lee C, Merkel S, et al. Evaluation of TCR gene editing achieved by TALENs, CRISPR/Cas9, and megaTAL nucleases. Mol Ther. 2016;24(3):570–81.
Zhao J, Lin Q, Song Y, Liu D. Universal CARs, universal T cells, and universal CAR T cells. J Hematol Oncol. 2018;11(1):132.
Madison BB, Patil D, Richter M, Li X, Tong M, Cranert S, Wang X, Martin R, Xi H, Tan Y, et al. Cas-CLOVER is a novel high-fidelity nuclease for safe and robust generation of T(SCM)-enriched allogeneic CAR-T cells. Mol Ther Nucleic Acids. 2022;29:979–95.
Xu X, Qi LS. A CRISPR-dCas Toolbox for Genetic Engineering and Synthetic Biology. J Mol Biol. 2019;431(1):34–47.
Brezgin S, Kostyusheva A, Kostyushev D, Chulanov V. Dead Cas systems: types, principles, and applications. Int J Mol Sci 2019, 20(23).
Stadtmauer EA, Fraietta JA, Davis MM, Cohen AD, Weber KL, Lancaster E, Mangan PA, Kulikovskaya I, Gupta M, Chen F et al. CRISPR-engineered T cells in patients with refractory cancer. Science 2020, 367(6481).
Shamshirgaran Y, Liu J, Sumer H, Verma PJ, Taheri-Ghahfarokhi A. Tools for efficient genome editing; ZFN, TALEN, and CRISPR. Methods Mol Biol. 2022;2495:29–46.
Ren J, Liu X, Fang C, Jiang S, June CH, Zhao Y. Multiplex Genome Editing to Generate Universal CAR T Cells Resistant to PD1 inhibition. Clin Cancer Res. 2017;23(9):2255–66.
Holling TM, van der Stoep N, Quinten E, van den Elsen PJ. Activated human T cells accomplish MHC class II expression through T cell-specific occupation of class II transactivator promoter III. J Immunol. 2002;168(2):763–70.
Kagoya Y, Guo T, Yeung B, Saso K, Anczurowski M, Wang CH, Murata K, Sugata K, Saijo H, Matsunaga Y, et al. Genetic ablation of HLA Class I, Class II, and the T-cell receptor enables allogeneic T cells to be used for adoptive T-cell therapy. Cancer Immunol Res. 2020;8(7):926–36.
Jo S, Das S, Williams A, Chretien AS, Pagliardini T, Le Roy A, Fernandez JP, Le Clerre D, Jahangiri B, Chion-Sotinel I, et al. Endowing universal CAR T-cell with immune-evasive properties using TALEN-gene editing. Nat Commun. 2022;13(1):3453.
Hu X, Dao M, White K, Gattis C, Clarke R, Landry S, Basco R, Tham E, Tucker A, Luo E. Engineered hypoimmune allogeneic CAR T cells exhibit innate and adaptive immune evasion even after sensitization in humanized mice and retain potent anti-tumor activity. Blood. 2021;138:1690.
Tipanee J, Samara-Kuko E, Gevaert T, Chuah MK, VandenDriessche T. Universal allogeneic CAR T cells engineered with sleeping Beauty transposons and CRISPR-CAS9 for cancer immunotherapy. Mol Ther. 2022;30(10):3155–75.
Micklethwaite KP, Gowrishankar K, Gloss BS, Li Z, Street JA, Moezzi L, Mach MA, Sutrave G, Clancy LE, Bishop DC, et al. Investigation of product-derived lymphoma following infusion of piggybac-modified CD19 chimeric antigen receptor T cells. Blood. 2021;138(16):1391–405.
Diorio C, Murray R, Naniong M, Barrera L, Camblin A, Chukinas J, Coholan L, Edwards A, Fuller T, Gonzales C, et al. Cytosine base editing enables quadruple-edited allogeneic CART cells for T-ALL. Blood. 2022;140(6):619–29.
Glaser V, Flugel C, Kath J, Du W, Drosdek V, Franke C, Stein M, Pruss A, Schmueck-Henneresse M, Volk HD, et al. Combining different CRISPR nucleases for simultaneous knock-in and base editing prevents translocations in multiplex-edited CAR T cells. Genome Biol. 2023;24(1):89.
van der Stegen SJC, Lindenbergh PL, Petrovic RM, Xie H, Diop MP, Alexeeva V, Shi Y, Mansilla-Soto J, Hamieh M, Eyquem J, et al. Generation of T-cell-receptor-negative CD8alphabeta-positive CAR T cells from T-cell-derived induced pluripotent stem cells. Nat Biomed Eng. 2022;6(11):1284–97.
Pham C, Spindler T, Hwang E, Brito A, Bulliard Y, Aftab BT. ATA3219: a potent next-generation allogeneic off-the-Shelf CD19-CAR T therapy without the need for gene-editing. Blood. 2020;136:9.
Sanchez Martinez D, Tirado N, Mensurado S, Martinez-Moreno A, Romecin P, Gutierrez Aguera F, Correia DV, Silva-Santos B, Menendez P. Generation and proof-of-concept for allogeneic CD123 CAR-Delta one T (DOT) cells in acute myeloid leukemia. J Immunother Cancer 2022, 10(9).
Nishimoto KP, Barca T, Azameera A, Makkouk A, Romero JM, Bai L, Brodey MM, Kennedy-Wilde J, Shao H, Papaioannou S, et al. Allogeneic CD20-targeted gammadelta T cells exhibit innate and adaptive antitumor activities in preclinical B-cell lymphoma models. Clin Transl Immunol. 2022;11(2):e1373.
Orgilles BA, Chion-Sotinel I, Grudman S, Mumford B, Dixon C, Duchateau P, Galetto R, Gouble A, Poirot L. P1420: PRE-CLINICAL PROOF OF CONCEPT DEMONSTRATES ROBUST ACTIVITY OF UCART20X22 DUAL CAR T-CELLS FOR THE TREATMENT OF B-CELL MALIGNANCIES. HemaSphere 2022, 6(Suppl).
Benjamin R, Graham C, Yallop D, Jozwik A, Mirci-Danicar OC, Lucchini G, Pinner D, Jain N, Kantarjian H, Boissel N, et al. Genome-edited, donor-derived allogeneic anti-CD19 chimeric antigen receptor T cells in paediatric and adult B-cell acute lymphoblastic leukaemia: results of two phase 1 studies. Lancet. 2020;396(10266):1885–94.
Mailankody S, Matous JV, Chhabra S, Liedtke M, Sidana S, Oluwole OO, Malik S, Nath R, Anwer F, Cruz JC et al. Publisher correction: allogeneic BCMA-targeting CAR T cells in relapsed/refractory multiple myeloma: phase 1 UNIVERSAL trial interim results. Nat Med 2023.
Benjamin R, Jain N, Maus MV, Boissel N, Graham C, Jozwik A, Yallop D, Konopleva M, Frigault MJ, Teshima T, et al. UCART19, a first-in-class allogeneic anti-CD19 chimeric antigen receptor T-cell therapy for adults with relapsed or refractory B-cell acute lymphoblastic leukaemia (CALM): a phase 1, dose-escalation trial. Lancet Haematol. 2022;9(11):e833–43.
Mailankody S, Matous JV, Chhabra S, Liedtke M, Sidana S, Oluwole OO, Malik S, Nath R, Anwer F, Cruz JC, et al. Allogeneic BCMA-targeting CAR T cells in relapsed/refractory multiple myeloma: phase 1 UNIVERSAL trial interim results. Nat Med. 2023;29(2):422–9.
Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, Braunschweig I, Oluwole OO, Siddiqi T, Lin Y, et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory large B-Cell lymphoma. N Engl J Med. 2017;377(26):2531–44.
Wang M, Munoz J, Goy A, Locke FL, Jacobson CA, Hill BT, Timmerman JM, Holmes H, Jaglowski S, Flinn IW, et al. KTE-X19 CAR T-Cell therapy in relapsed or Refractory Mantle-Cell Lymphoma. N Engl J Med. 2020;382(14):1331–42.
Mailankody S, Matous JV, Chhabra S, Liedtke M, Sidana S, Oluwole OO, Malik S, Nath R, Anwer F, Cruz JC. Allogeneic BCMA-targeting CAR T cells in relapsed/refractory multiple myeloma: phase 1 UNIVERSAL trial interim results. Nat Med. 2023;29(2):422–9.
Kaminski BA, Kadereit S, Miller RE, Leahy P, Stein KR, Topa DA, Radivoyevitch T, Veigl ML, Laughlin MJ. Reduced expression of NFAT-associated genes in UCB versus adult CD4 + T lymphocytes during primary stimulation. Blood. 2003;102(13):4608–17.
Ma Q, Garber HR, Lu S, He H, Tallis E, Ding X, Sergeeva A, Wood MS, Dotti G, Salvado B, et al. A novel TCR-like CAR with specificity for PR1/HLA-A2 effectively targets myeloid leukemia in vitro when expressed in human adult peripheral blood and cord blood T cells. Cytotherapy. 2016;18(8):985–94.
Nitsche A, Zhang M, Clauss T, Siegert W, Brune K, Pahl A. Cytokine profiles of cord and adult blood leukocytes: differences in expression are due to differences in expression and activation of transcription factors. BMC Immunol. 2007;8:18.
Fang Y, Zhu Y, Kramer A, Chen Y, Li YR, Yang L. Graft-versus-host Disease Modulation by Innate T Cells. Int J Mol Sci 2023, 24(4).
Du Z, Zhu S, Zhang X, Gong Z, Wang S. Non-conventional allogeneic Anti-BCMA chimeric Antigen receptor-based Immune Cell therapies for multiple myeloma treatment. Cancers (Basel) 2023, 15(3).
Sanber K, Savani B, Jain T. Graft-versus-host disease risk after chimeric antigen receptor T-cell therapy: the diametric opposition of T cells. Br J Haematol. 2021;195(5):660–8.
Kim DW, Cho JY. Recent advances in allogeneic CAR-T cells. Biomolecules 2020, 10(2).
Panowski S, Srinivasan S, Van Blarcom T, Sommer C, Cheng H-Y, Pertel T, Santaguida MA, Galetto R, Dunlop A, Benjamin R. Investigation of Allocar TTM Targeting CD70 as a potential therapy for an array of hematological malignancies. Blood. 2019;134:5157.
Mo F, Watanabe N, McKenna MK, Hicks MJ, Srinivasan M, Gomes-Silva D, Atilla E, Smith T, Ataca Atilla P, Ma R, et al. Engineered off-the-shelf therapeutic T cells resist host immune rejection. Nat Biotechnol. 2021;39(1):56–63.
Srour S, Kotecha R, Curti B, Chahoud J, Drakaki A, Tang L, Goyal L, Prashad S, Szenes V, Norwood K. Abstract CT011: a phase 1 multicenter study (TRAVERSE) evaluating the safety and efficacy of ALLO-316 following conditioning regimen in pts with advanced or metastatic clear cell renal cell carcinoma (ccRCC). Cancer Res. 2023;83(8Supplement):CT011–011.
Srinivasan S, Tan N, Cheng H-Y, Zhang Y, Tacheva-Grigorova S, Van Blarcom T, Sommer C, Nguyen D, Sasu B, Panowski S. Investigation of ALLO-316: a fratricide-resistant allogeneic CAR T targeting CD70 as a potential therapy for the treatment of AML. Blood. 2020;136:23.
Murray R, Navarrete NRR, Desai K, Chowdhury MR, Chilakapati SR, Chong B, Messana A, Sobon H, Rocha J, Musenge F. Comprehensive genome editing confers off-the-shelf CAR-T cells superior efficacy against solid tumors. bioRxiv 2023:2023.2008. 2003.551705.
Schmiedel D, Mandelboim O. NKG2D Ligands-Critical Targets for Cancer Immune Escape and Therapy. Front Immunol 2018, 9:2040.
Lanier LL. NKG2D receptor and its ligands in host defense. Cancer Immunol Res. 2015;3(6):575–82.
Liu H, Wang S, Xin J, Wang J, Yao C, Zhang Z. Role of NKG2D and its ligands in cancer immunotherapy. Am J Cancer Res. 2019;9(10):2064–78.
Prenen H, Dekervel J, Hendlisz A, Anguille S, Ahmad A, Cerf E, Lonez C, Breman E, Dheur M, Alcantar-Orozco E. Updated data from the alloSHRINK phase 1 first-in-human study evaluating CYAD-101, an innovative non-gene-edited allogeneic CAR-T, in metastatic colorectal cancer. J Clin Oncol. 2021;39:74.
Choe JH, Yu T, Abramson JS, Abou-El-Enein M. Cost-effectiveness of second-line lisocabtagene maraleucel in relapsed or refractory diffuse large B-cell lymphoma. Blood Adv. 2024;8(2):484–96.
Harrison RP, Zylberberg E, Ellison S, Levine BL. Chimeric antigen receptor-T cell therapy manufacturing: modelling the effect of offshore production on aggregate cost of goods. Cytotherapy. 2019;21(2):224–33.
Ran FA, Hsu PD, Lin CY, Gootenberg JS, Konermann S, Trevino AE, Scott DA, Inoue A, Matoba S, Zhang Y, et al. Double nicking by RNA-guided CRISPR Cas9 for enhanced genome editing specificity. Cell. 2013;154(6):1380–9.
Kosicki M, Tomberg K, Bradley A. Repair of double-strand breaks induced by CRISPR-Cas9 leads to large deletions and complex rearrangements. Nat Biotechnol. 2018;36(8):765–71.
Acknowledgements
We gratefully acknowledge the Immunology Department of Pasteur Institute of Iran for their technical assistance.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
ZS conceived the review and revised the manuscript. SM developed the theory and took the lead in writing the manuscript. SM, AN, AM and SS contributed to data collection, literature review, and manuscript drafting. All authors contributed to the article and approved the final version submitted for publication.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval is not applicable for this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mansoori, S., Noei, A., Maali, A. et al. Recent updates on allogeneic CAR-T cells in hematological malignancies. Cancer Cell Int 24, 304 (2024). https://doi.org/10.1186/s12935-024-03479-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-024-03479-y