Abstract
Background
To date, data on the efficacy of targeted therapies for mucosal melanoma (MM) are limited. In this study, we analyzed genetic alterations according to the primary site of origin, which could provide clues for targeted therapy for MM.
Methods
We conducted a retrospective cohort study of 112 patients with MM. Targeted sequencing was performed to analyze genetic aberrations. Kaplan–Meier analysis was conducted with the log-rank test to compare the significance among subgroups.
Results
In total, 112 patients with MM were included according to the anatomic sites: 38 (33.9%) in the head and neck, 22 (19.6%) in the genitourinary tract, 21 (18.8%) in the anorectum, 19 (17.0%) in the esophagus, 10 (8.9%) in the uvea, and 2 (1.8%) in the small bowel. The most significantly mutated genes included BRAF (17%), KIT (15%), RAS (15%), TP53 (13%), NF1 (12%), SF3B1 (11%), GNA11 (7%), GNAQ (5%), and FBXW7 (4%). A large number of chromosomal structural variants was found. The anatomic sites of esophagus and small bowel were independent risk factors for progression-free survival (PFS, hazard ratio [HR] 4.78, 95% confidence interval [CI] 2.42–9.45, P < 0.0001) and overall survival (OS, HR 5.26, 95% CI 2.51–11.03, P < 0.0001). Casitas B-lineage lymphoma (CBL) mutants showed significantly poorer PFS and OS. In contrast, MM patients who received immune checkpoint inhibitors (ICIs) had a significantly more favorable OS (HR 0.39, 95% CI 0.20–0.75, P = 0.008).
Conclusions
Our findings reveal the genetic features of patients with MM, mainly across six anatomic sites, offering a potential avenue for targeted therapies.
Similar content being viewed by others
Background
Primary mucosal melanomas (MM), arising from melanocytes in mucosal tissues lining the head and neck, respiratory, gastrointestinal, and urogenital tracts, account for 26% of all melanomas in Asian populations [1]. Atypical symptoms are commonly observed in the early stage because of the occult anatomic locations, and the median age at presentation is 70 years, which is later than that for cutaneous melanomas [2]. Moreover, the clinical presentation of MM is more aggressive and has a poorer prognosis, regardless of the stage at diagnosis, with a 5-year survival rate of 25% owing to the lack of effective targeted therapies [3].
Importantly, MM is markedly different from cutaneous melanoma in terms of biological aspects. Recently, whole-genome and exome sequencing have revealed the molecular landscape and potential oncogenic drivers of MM, which are characterized by greater copy number (CN) variations, structural variations (SVs), and a lower tumor mutation burden (TMB) [4]. Targeted therapy with BRAF/MEK tyrosine kinase inhibitors improves patient survival [5]. However, BRAF mutations are less frequent in MM and are susceptible to resistance, resulting in a lower effectivity of BRAF/MEK inhibitors [6]. Immune checkpoint inhibitors (ICIs) are also beneficial for MM, with a median progression-free survival (PFS) of only 3.9 months [7]. Although BRAF, RAS, KIT, NF1, and SF3B1 have been identified as significantly mutated genes [4], there remains a lack of understanding and identification of oncogenic drivers in MM, probably owing to the rarity of samples and lack of preclinical models.
To further explore the molecular profiles of MM, we performed targeted next-generation sequencing (NGS) of 112 MM patients to explore the clinical significance of genetic characteristics potentially providing molecular targets and individualized treatments and provide a better mechanistic understanding of MM biology across the anatomic sites of MM.
Methods
Study participants
A total of 112 MM samples were collected from patients treated or consulted at the Sun Yat-sen University Cancer Center (SYSUCC, Guangzhou, China) between April 2007 and April 2022. Patients with cutaneous melanoma that had metastasized to the mucosa were excluded. The staging standard that we used followed the newest proposal for all anatomical sites published in April 2022 [8]. For all cases, the diagnoses were reviewed and confirmed by two experienced pathologists (Y. L. and F. W.). Clinical follow-up and treatment information as well as telephone interview data were available from the medical records of inpatients and outpatients (Supplementary Table S1). The study protocol was designed in accordance with the principles of the Declaration of Helsinki and approved by the Research Ethics Committee of the SYSUCC (No. B2016-069-01).
DNA extraction
Formalin-fixed and paraffin-embedded (FFPE) tissue blocks were assessed using hematoxylin-eosin (H&E) staining, and regions containing minimum of 20% tumor cells in unstained sections were selected for microdissection and subsequent experiments. Genomic DNA was extracted from tumors and patient-matched normal tissues or white blood cells using a QIAamp DNA FFPE Tissue Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions [9]. The extracted DNA was then quantified using a Qubit dsDNA BR assay (Life Technologies, USA) [10] according to the manufacturer’s instructions.
Targeted sequencing and data processing
As described previously [11], we used the two targeted sequencing assays: (1) the 295 OncoScreen panel containing whole exons of 287 genes and selected introns of 22 genes (Burning Rock Biotech Ltd., Guangzhou, China) and (2) the 1021-gene panel containing whole exons and selected introns of 288 genes and selected regions of 733 genes (Geneplus-Beijing, Beijing, China). Detailed methods for preparing the DNA, sequencing libraries, and data processing have been previously described [11].
Statistical analysis
TMB comparison among the different subsets of patients was performed using the Wilcoxon rank-sum test. The Kaplan–Meier method was used to estimate overall survival (OS) and PFS, and differences were compared using the log-rank test. Cox proportional hazards regression analyses were used to evaluate the independently predictive factors of each biological and clinical features associated with OS and/or PFS. Statistical significance was defined as a two-tailed P-value of < 0.05. All the statistical analyses were performed using IBM SPSS V.25.0 (Chicago, Armonk, NY, USA).
Results
Patients’ characteristics
In total, 112 patients with MM who underwent tumor sequencing were identified: 86 patients (76.8%) with primary tumors, 17 (15.2%) with metastatic tumors, and 9 (8.0%) with recurrent tumors. A total of 51 patients underwent 295-gene panel sequencing, and 61 underwent 1021-gene panel sequencing for further analysis (Supplementary Table S1). Table 1 summarizes the clinicopathological characteristics of the 112 patients with MM with a median age of 56 years (range 23–82 years); 56.3% were women and 43.8% were men. The anatomic sites of the MM were the head and neck in 33.9% of the patients, genitourinary tract in 19.6%, anorectum in 18.8%, esophagus in 17.0%, uvea in 8.9%, and small bowel in 1.8%. Histologically, 79 cases (70.5%) showed an epithelioid morphology, 8 (7.1%) showed a spindle morphology, and 21 (18.8%) showed a mixed morphology. Forty-six of the 112 (41.1%) patients with clinical stage were unknown due to the unavailability of invasion depth. The median PFS and follow-up times were 7.5 and 23.9 months, respectively. For treatment, 106 patients underwent surgical operations with a gross resection of primary or recurrent lesions (106/112, 94.6%), and 92 patients received various adjuvant treatments, including chemotherapy, radiotherapy, targeted therapy, and/or ICIs (92/112, 82.1%). Importantly, 67.0% (75/112) patients received ICIs and 32.1% (36/112) did not (Table 1).
TMB in MM
Detailed information on the genetic variation in MM is provided in Supplementary Table S2. The TMB per megabase was relatively low, with a median of 3.1 (range 0–68.2). A significantly lower TMB was observed in primary tumor samples than in recurrent/metastatic tumors (Wilcoxon rank-sum test, P = 0.015, Fig. 1A). There were no significant differences among the primary sites, morphological types, and survival status (Fig. 1B-D).
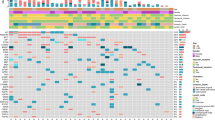
Genetic profiling and related pathways of MM
The frequent mutations were sequentially observed in BRAF (19/112, 17%), KIT (17/112, 15%), MYC (17/112, 15%), RAS (16/112, 14%), TP53 (15/112, 13%), NF1 (13/112, 12%), SF3B1 (12/112 11%), TERT (11/112, 10%), GNA11 (8/112, 7%), CBL (7/112, 6%), GNAQ (6/112, 5%) and FBXW7 (5/112, 4%) (Fig. 2). Furthermore, according to the Kyoto Encyclopedia of Genes and Genomes (KEGG) database, the most significantly altered pathway was the MAPK signaling pathway (73%), followed by the ErbB (58%), p53 (55%), Wnt (49%), mTOR (36%), and Notch (23%) signaling pathways (Fig. 2).
The mutational landscape of 112 patients with MM, including point mutation and SVs. From top to bottom: the total tumor mutational burden; the clinicopathological features, such as anatomic site, sex, and sample origins; the landscape of genes mutation (copy number variations, SNVs, indels, fusion gene, 5’UTR); the significantly activated pathway; the potential targeted therapy, each actionable mutation is colored by evidence level: A (NCCN guidelines and FDA guidelines), B (late trials), C (early trials), D (case report). Abbreviations: MM, mucosal melanoma; SVs, structural variants; SNVs, single nucleotide variations; UTR, untranslated regions; NCCN, national comprehensive cancer network; FDA, Food and Drug Administration
The frequencies of these common mutations varied according to the origin of MM. Higher percentages of BRAF, RAS, NF1, and CBL mutations were observed in patients with melanoma in the head and neck than in patients with melanoma in the other five sites. Additionally, higher percentages of GNAQ and GNA11 mutations were observed in patients with uveal melanoma, and a higher percentage of SF3B1 mutations in patients with esophageal and uveal melanoma (Fig. 3, Supplementary Figure S1).
Additionally, previous studies reported that other genes are frequently mutated in melanoma and other cancer types [4, 12,13,14], including BRCA2 (9/112, 8%), LRP1B (9/112, 8%), MET (8/112, 7%), PRKDC (7/112, 6%), NOTCH4 (7/112, 6%), CCND3 (6/112, 5%), and FGF3/4/19 (6/112, 5%). Germline mutations were observed in two cases (2/112, 2%) with BRCA2 (p.W1692Mfs*3) and ATM (c.331 + 5G > A).
Somatic copy number and structural events
Next, we observed that MM had a large number of chromosomal SVs, including somatic CN changes, fusions, and the telomere length-associated genes TERT and ATRX.
Somatic CN amplification was observed in 143 genes from 85 different chromosomal regions in 73 patients (Supplementary Figure S2). The frequently amplified regions included 6p21 (18/73, 25%), 8q24 (17/73, 23%), 4q12(14, 19%), 8q21 (11/73, 15%), 12q14 (11/73, 15%), 12q15 (10/73, 14%), 11q13 (9/73, 12%), 1q32 (8/73, 11%), and 7q31 (6/73, 8%), along with the recurrently amplified genes MYC (16/73, 22%), KIT (13/73, 28%), DAXX (11/73, 15%), KDR (11/72, 15%), NBN (11/72, 15%), CDK4 (11/72, 15%), MDM2 (10/73, 14%), PDGFRA (9/73, 12%), CCND1 (7/73, 10%), MDM4 (7/73, 10%), CCND3 (6/73, 8%), FGF19 (6/73, 8%), MET (6/73, 8%), FGF3 (5/73, 7%), FGF4 (5/73, 7%), FANCE (5/73, 7%), IRF4 (5/73, 7%), CDK6 (5/73, 7%), BRAF (5/73, 7%), NOTCH1 (4/73, 5%), and NOTCH2 (4/73, 5%). We also found several CN variations and the co-occurrence of KIT, KDR, PDGFRA, FGF3/4/19, FANCE, DAXX, and NOTCH clustered in the same chromosomal segment in one case, whereas CN deletions were detected in 14 cases. For example, CIC and PTEN deletions were more frequent in three and two cases, respectively.
Novel, recurrently fused genes were observed in nine cases (9/112, 8%), among which RNF43-IFLTD1, KCTD15-BRAF, and WDR64-AKT3 had a higher mutational abundance of 25%. The last two fusion genes encode tyrosine kinases, which may activate the MAPK pathway [15].
Finally, highly prevalent TERT mutations were identified in 11 cases (11/112, 10%), all with TERT promoter mutations containing c.146 C > T (4/11, 36%), c.124 C > T (4/11, 36%), c.-124 C > T (2/11, 18%), and c.-58-u68_-58-u66delCCCinsTCT (1/11,9%). Most ATRX variations had single nucleotide alterations or small fragment deletions. Loss of function was only detected in six cases (6/112, 5%). Interestingly, none of the cases had mutations in either TERT or ATRX, indicating they are mutually exclusive in MM, similar to those observed in gliomas [16].
Patients’ survival and clinical response to ICIs
As shown in Table 2; Fig. 4, multivariate and Kaplan–Meier analyses revealed that the anatomic sites of MM in the esophagus and small bowel (PFS: hazard ratio [HR] = 4.78, 95% confidence interval [CI] = 2.42–9.45, P < 0.001; OS: HR = 5.26, 95% CI = 2.51–11.03, P < 0.001) and CBL mutations (PFS: HR = 3.54, 95% CI = 1.46–8.56, P = 0.005; OS: HR = 5.57, 95% CI = 2.04–15.19, P = 0.001) were independently risk factors for survival. In addition, we found that mitotic activity with ≥ 10/mm2 (HR = 2.76, 95% CI = 1.22–6.25, P = 0.015) was an independent risk factor for OS. There were no associations between other factors and PFS or OS (Supplementary Figures S3 and S4).
Kaplan–Meier survival analysis in MM. Forest plot and Kaplan–Meier survival curves for PFS (A-E) and OS (F-J) were performed for the primary tumor site, mitotic activity, CBL mutations, and with/without ICIs treatment. Significance shown as P < 0.05. Abbreviations: MM, mucosal melanoma; PFS, progression-free survival; OS, overall survival; CBL, Casitas B-lineage lymphoma; ICI, immune checkpoint inhibitor
The suggested therapy modalities are listed in the bottom panel of Fig. 2, and mTOR, PD1, MEK, CDK4/6, KIT, PARP, VEGF, BRAF inhibitors may have pharmacological effects on targetable treatment [17,18,19,20,21]. In our study, we found that receiving ICIs (HR = 0.39, 95% CI = 0.20–0.75, P = 0.005, Table 2; Fig. 4J) was a favorable factor for OS (Table 2), suggesting that patients with MM may benefit from ICIs treatment.
Discussion
In this retrospective cohort study, we used two commercially customized NGS panels to describe the molecular spectrum of 112 MM patients and explore potential targets for prognosis prediction and further individualized immunotherapy in these patients.
Consistent with previous reports, which revealed that acral melanoma and MM had limited DNA mutational burden [14, 22,23,24], we observed a low TMB in this study. As previously reported [4, 14, 25,26,27], we found that a substantial proportion of MM had alterations in the genes involved in the MAPK pathway, including frequent mutations in BRAF, KIT, RAS, and NF1. It is well known that a BRAF mutation provides a targeted therapy for melanoma with good efficacy [28]. Nevertheless, small bowel melanoma in this study harbored only two in-frame mutations in BRAF (p.T599_V600insT and p.T244_L245delinsS), whereas no V600 mutations were observed. Mutations in other genes, such as KIT, RAS, and NF1, were found in the primary sites of the head and neck, esophagus, anorectum, and genitourinary tract in our cohort. Notably, we found that SF3B1 mutations as recurrent genetic events in MM were more common in esophageal and uveal melanomas, which is similar to that reported in recent studies [29,30,31]. In addition, mutations in GNAQ and GNA11 occurred in the majority of uveal melanomas found in this study, which is consistent with the findings of previous research [29, 32].
A previous whole-genome study showed that the SV load had the feature of complexity and diversity in MM [4]. Not surprisingly, we also found that most patients with MM harbored frequent CN variations and MYC amplification, which exemplified their role in MM pathogenesis and was in line with the results of other investigations [4, 33, 34]. For instance, high MYC expression is associated with aggressive biological behavior in cancers [35]. Additionally, many of the CN amplifications in well-known pathogenic genes (KIT, PDGFRA, MDM2, and MDM4) and cell cycle genes, such as CDK4/6 and CCND1, were found in this study, similar to those reported in previous studies [33, 34]. Bucheit et al. have demonstrated that complete PTEN loss correlates with poor survival in stage III melanoma [36]. In this study, we found PTEN deletion in MM, suggesting a tumorigenic role for progression in MM. The activation of TERT and inactivation of ATRX commonly and exclusively occurred in MM, which has been reported previously, indicating the importance of telomerase activation or alternative telomere lengthening mechanisms in reducing length in MM [4, 14].
A cohort of 466 Chinese patients with melanoma showed that MM was more aggressive and was associated with shorter survival than cutaneous lesions [37]. MM arises from different anatomic sites, and a population-based epidemiological analysis showed that MM from different anatomical sites exhibit different survival outcomes, likely due to the diverse environmental exposures associated with each site [38]. Here, we demonstrated that the anatomic sites of esophagus and small bowel melanomas may be a risk factor for survival, which concurs with the findings of a previous study [39]. However, a cohort of 706 MM patients did not show significant differences in prognosis among the anatomic sites of MM, primarily due to lack of cases of MM in the esophagus and small bowel [40].
We identified CBL mutations in patients with MM; these were risk factors for poor OS and PFS, which are infrequent in published melanoma exome studies but frequent in desmoplastic melanoma [41]. Recurrent CBL mutations occur in myeloid malignancies and have been associated with poor prognosis [42]. Ebert et al. recently identified that the oncogenic function of CBL mutants drive PI3K/AKT signaling and provide a rationale for therapeutic targets in myeloid malignancies [43]. Another study identified that inhibiting CBL mutations can activate the innate immune system to restrain cancer metastasis and improve the sensitivity to immunotherapy [44]. Finally, we found that MM patients receiving ICI treatment experienced a favorable impact on survival, especially OS, which is consistent with the findings of a previous study [45]. Taken together, CBL mutations might be promising targets for MM immunotherapy.
Our study had some limitations. First, the sample size was small owing to the rarity of this disease, especially small bowel melanoma. Second, for molecular profiling in MM, we used targeted NGS, which only targeted genomic regions of partial genes and, therefore, could not reveal novel pathogenic point mutations, rearrangements, or epigenetic changes. Thus, the whole-exome sequencing in a larger cohort is required to comprehensively depict the molecular profile of MM. A better understanding of the molecular mechanisms is required to explore additional avenues for immunotherapy in MM.
Conclusions
Our study demonstrates the molecular landscape of Chinese patients with MM based on targeted sequencing. Our finding on the genetic characteristics of MM among different anatomic sites reveal that CBL mutations in MM are potential targets. Further studies are warranted to elucidate the mechanisms that link CBL mutations to immunotherapy responses, which may provide a rationale for immunotherapy.
Data Availability
The key raw data were deposited into the Research Data Deposit, with the approval number of RDDA2022535268, and the datasets used in this study are publicly available.
References
Byeon S, Cho HJ, Jang KT, Kwon M, Lee J, Lee J, Kim ST. Molecular profiling of asian patients with advanced melanoma receiving check-point inhibitor treatment. ESMO Open. 2021;6(1):100002.
Yde SS, Sjoegren P, Heje M, Stolle LB. Mucosal melanoma: a literature review. Curr Oncol Rep. 2018;20(3):28.
Lerner BA, Stewart LA, Horowitz DP, Carvajal RD. Mucosal melanoma: New Insights and Therapeutic Options for a unique and aggressive disease. Oncol (Williston Park). 2017;31(11):e23–e32.
Newell F, Kong Y, Wilmott JS, Johansson PA, Ferguson PM, Cui C, Li Z, Kazakoff SH, Burke H, Dodds TJ, et al. Whole-genome landscape of mucosal melanoma reveals diverse drivers and therapeutic targets. Nat Commun. 2019;10(1):3163.
Teixido C, Castillo P, Martinez-Vila C, Arance A, Alos L. Molecular markers and targets in Melanoma. Cells 2021, 10(9).
Dumaz N, Jouenne F, Delyon J, Mourah S, Bensussan A, Lebbe C. Atypical BRAF and NRAS Mutations in Mucosal Melanoma. Cancers (Basel) 2019, 11(8).
Shoushtari AN, Munhoz RR, Kuk D, Ott PA, Johnson DB, Tsai KK, Rapisuwon S, Eroglu Z, Sullivan RJ, Luke JJ, et al. The efficacy of anti-PD-1 agents in acral and mucosal melanoma. Cancer. 2016;122(21):3354–62.
Cui C, Lian B, Zhang X, Wu D, Li K, Si L, Yang Y, Tian H, Zhou L, Chi Z, et al. An evidence-based staging system for mucosal melanoma: a proposal. Ann Surg Oncol. 2022;29(8):5221–34.
Wang F, Diao XY, Zhang X, Shao Q, Feng YF, An X, Wang HY. Identification of genetic alterations associated with primary resistance to EGFR-TKIs in advanced non-small-cell lung cancer patients with EGFR sensitive mutations. Cancer Commun (Lond). 2019;39(1):7.
Wang HY, Li F, Liu N, Liu XY, Yang XH, Guo YM, Bei JX, Zeng YX, Shao JY. Prognostic implications of a molecular classifier derived from whole-exome sequencing in nasopharyngeal carcinoma. Cancer Med. 2019;8(6):2705–16.
Wang HY, Deng L, Li YQ, Zhang X, Long YK, Zhang X, Feng YF, He Y, Tang T, Yang XH, et al. Pan-cancer analysis of Tumor Mutational Burden and homologous recombination DNA damage repair using targeted next-generation sequencing. Cancer Res Treat. 2021;53(4):973–82.
Aydin IT, Melamed RD, Adams SJ, Castillo-Martin M, Demir A, Bryk D, Brunner G, Cordon-Cardo C, Osman I, Rabadan R, et al. FBXW7 mutations in melanoma and a new therapeutic paradigm. J Natl Cancer Inst. 2014;106(6):dju107.
Yu J, Yan J, Guo Q, Chi Z, Tang B, Zheng B, Yu J, Yin T, Cheng Z, Wu X, et al. Genetic aberrations in the CDK4 pathway are Associated with Innate Resistance to PD-1 blockade in chinese patients with non-cutaneous melanoma. Clin Cancer Res. 2019;25(21):6511–23.
Hayward NK, Wilmott JS, Waddell N, Johansson PA, Field MA, Nones K, Patch AM, Kakavand H, Alexandrov LB, Burke H, et al. Whole-genome landscapes of major melanoma subtypes. Nature. 2017;545(7653):175–80.
Botton T, Yeh I, Nelson T, Vemula SS, Sparatta A, Garrido MC, Allegra M, Rocchi S, Bahadoran P, McCalmont TH, et al. Recurrent BRAF kinase fusions in melanocytic tumors offer an opportunity for targeted therapy. Pigment Cell Melanoma Res. 2013;26(6):845–51.
Killela PJ, Reitman ZJ, Jiao Y, Bettegowda C, Agrawal N, Diaz LA Jr, Friedman AH, Friedman H, Gallia GL, Giovanella BC, et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci U S A. 2013;110(15):6021–6.
Stanland LJ, Ang HX, Hoj JP, Chu Y, Tan P, Wood KC, Luftig MA. CBF-beta mitigates PI3K-alpha-specific inhibitor killing through PIM1 in PIK3CA mutant gastric cancer. Mol Cancer Res 2023.
Ascierto PA, Dummer R, Gogas HJ, Arance A, Mandala M, Liszkay G, Garbe C, Schadendorf D, Krajsova I, Gutzmer R et al. Contribution of MEK Inhibition to BRAF/MEK inhibitor combination treatment of BRAF-Mutant melanoma: part 2 of the Randomized, Open-Label, phase III COLUMBUS Trial. J Clin Oncol 2023:JCO2202322.
Pettitt SJ, Shao N, Zatreanu D, Frankum J, Bajrami I, Brough R, Krastev DB, Roumeliotis TI, Choudhary JS, Lorenz S et al. A HUWE1 defect causes PARP inhibitor resistance by modulating the BRCA1-∆11q splice variant. Oncogene 2023.
Garutti M, Targato G, Buriolla S, Palmero L, Minisini AM, Puglisi F. CDK4/6 inhibitors in Melanoma: a Comprehensive Review. Cells 2021, 10(6).
Bannoud N, Stupirski JC, Cagnoni AJ, Hockl PF, Perez Saez JM, Garcia PA, Mahmoud YD, Gambarte Tudela J, Scheidegger MA, Marshall A, et al. Circulating galectin-1 delineates response to bevacizumab in melanoma patients and reprograms endothelial cell biology. Proc Natl Acad Sci U S A. 2023;120(3):e2214350120.
Buchbinder EI, Weirather JL, Manos M, Quattrochi BJ, Sholl LM, Brennick RC, Bowling P, Bailey N, Magarace L, Ott PA, et al. Characterization of genetics in patients with mucosal melanoma treated with immune checkpoint blockade. Cancer Med. 2021;10(8):2627–35.
Furney SJ, Turajlic S, Stamp G, Thomas JM, Hayes A, Strauss D, Gavrielides M, Xing W, Gore M, Larkin J, et al. The mutational burden of acral melanoma revealed by whole-genome sequencing and comparative analysis. Pigment Cell Melanoma Res. 2014;27(5):835–8.
Tang B, Yan X, Sheng X, Si L, Cui C, Kong Y, Mao L, Lian B, Bai X, Wang X, et al. Safety and clinical activity with an anti-PD-1 antibody JS001 in advanced melanoma or urologic cancer patients. J Hematol Oncol. 2019;12(1):7.
Si L, Kong Y, Xu X, Flaherty KT, Sheng X, Cui C, Chi Z, Li S, Mao L, Guo J. Prevalence of BRAF V600E mutation in chinese melanoma patients: large scale analysis of BRAF and NRAS mutations in a 432-case cohort. Eur J Cancer. 2012;48(1):94–100.
Furney SJ, Turajlic S, Stamp G, Nohadani M, Carlisle A, Thomas JM, Hayes A, Strauss D, Gore M, van den Oord J, et al. Genome sequencing of mucosal melanomas reveals that they are driven by distinct mechanisms from cutaneous melanoma. J Pathol. 2013;230(3):261–9.
Sekine S, Nakanishi Y, Ogawa R, Kouda S, Kanai Y. Esophageal melanomas harbor frequent NRAS mutations unlike melanomas of other mucosal sites. Virchows Arch. 2009;454(5):513–7.
Lee KH, Goh J, Kim YJ, Kim K. Identification of synthetic chemosensitivity genes paired with BRAF for BRAF/MAPK inhibitors. Sci Rep. 2020;10(1):20001.
Harbour JW, Roberson ED, Anbunathan H, Onken MD, Worley LA, Bowcock AM. Recurrent mutations at codon 625 of the splicing factor SF3B1 in uveal melanoma. Nat Genet. 2013;45(2):133–5.
Yang HM, Hsiao SJ, Schaeffer DF, Lai C, Remotti HE, Horst D, Mansukhani MM, Horst BA. Identification of recurrent mutational events in anorectal melanoma. Mod Pathol. 2017;30(2):286–96.
Hintzsche JD, Gorden NT, Amato CM, Kim J, Wuensch KE, Robinson SE, Applegate AJ, Couts KL, Medina TM, Wells KR, et al. Whole-exome sequencing identifies recurrent SF3B1 R625 mutation and comutation of NF1 and KIT in mucosal melanoma. Melanoma Res. 2017;27(3):189–99.
Jager MJ, Shields CL, Cebulla CM, Abdel-Rahman MH, Grossniklaus HE, Stern MH, Carvajal RD, Belfort RN, Jia R, Shields JA, et al. Uveal melanoma. Nat Rev Dis Primers. 2020;6(1):24.
Forschner A, Hilke FJ, Bonzheim I, Gschwind A, Demidov G, Amaral T, Ossowski S, Riess O, Schroeder C, Martus P et al. MDM2, MDM4 and EGFR Amplifications and Hyperprogression in Metastatic Acral and Mucosal Melanoma. Cancers (Basel) 2020, 12(3).
Hilke FJ, Sinnberg T, Gschwind A, Niessner H, Demidov G, Amaral T, Ossowski S, Bonzheim I, Rocken M, Riess O et al. Distinct mutation patterns reveal Melanoma Subtypes and Influence Immunotherapy Response in Advanced Melanoma Patients. Cancers (Basel) 2020, 12(9).
Lin X, Sun R, Zhao X, Zhu D, Zhao X, Gu Q, Dong X, Zhang D, Zhang Y, Li Y, et al. C-myc overexpression drives melanoma metastasis by promoting vasculogenic mimicry via c-myc/snail/Bax signaling. J Mol Med (Berl). 2017;95(1):53–67.
Bucheit AD, Chen G, Siroy A, Tetzlaff M, Broaddus R, Milton D, Fox P, Bassett R, Hwu P, Gershenwald JE, et al. Complete loss of PTEN protein expression correlates with shorter time to brain metastasis and survival in stage IIIB/C melanoma patients with BRAFV600 mutations. Clin Cancer Res. 2014;20(21):5527–36.
Hao M, Zhao G, Du X, Yang Y, Yang J. Clinical characteristics and prognostic indicators for metastatic melanoma: data from 446 patients in north China. Tumour Biol. 2016;37(8):10339–48.
Bishop KD, Olszewski AJ. Epidemiology and survival outcomes of ocular and mucosal melanomas: a population-based analysis. Int J Cancer. 2014;134(12):2961–71.
Sun H, Gong L, Zhao G, Zhan H, Meng B, Yu Z, Pan Z. Clinicopathological characteristics, staging classification, and survival outcomes of primary malignant melanoma of the esophagus. J Surg Oncol. 2018;117(4):588–96.
Cui C, Lian B, Zhou L, Song X, Zhang X, Wu D, Chi Z, Si L, Sheng X, Kong Y, et al. Multifactorial analysis of prognostic factors and Survival Rates among 706 mucosal melanoma patients. Ann Surg Oncol. 2018;25(8):2184–92.
Shain AH, Garrido M, Botton T, Talevich E, Yeh I, Sanborn JZ, Chung J, Wang NJ, Kakavand H, Mann GJ, et al. Exome sequencing of desmoplastic melanoma identifies recurrent NFKBIE promoter mutations and diverse activating mutations in the MAPK pathway. Nat Genet. 2015;47(10):1194–9.
Katzav S, Schmitz ML. Mutations of c-Cbl in myeloid malignancies. Oncotarget. 2015;6(13):10689–96.
Belizaire R, Koochaki SHJ, Udeshi ND, Vedder A, Sun L, Svinkina T, Hartigan C, McConkey M, Kovalcik V, Bizuayehu A, et al. CBL mutations drive PI3K/AKT signaling via increased interaction with LYN and PIK3R1. Blood. 2021;137(16):2209–20.
Paolino M, Choidas A, Wallner S, Pranjic B, Uribesalgo I, Loeser S, Jamieson AM, Langdon WY, Ikeda F, Fededa JP, et al. The E3 ligase Cbl-b and TAM receptors regulate cancer metastasis via natural killer cells. Nature. 2014;507(7493):508–12.
Zhang S, Zhang J, Guo J, Si L, Bai X. Evolving treatment approaches to mucosal melanoma. Curr Oncol Rep. 2022;24(10):1261–71.
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing. We thank our colleagues and reviewers for their experimental support and critical discussions.
Funding
This work was partially supported by the Natural Science Foundation of Guangdong Province (grant number 2020A1515010313).
Author information
Authors and Affiliations
Contributions
Conceptualization and design: FW, KHG, HYW; Formal analysis: HYW, KHG, FW; Conducting experiments: LZ, XYL, JJY, LD, KJ, XYW; Acquisition of data: HYW, CFH; Writing the manuscript: HYW, FW. All authors contributed to the planning, data analysis, writing, and the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that may have influenced the work reported in this study.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Research Ethics Committee of SYSUCC (No. B2016-069-01). Written informed consent was obtained from all patients.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, HY., Liu, Y., Deng, L. et al. Clinical significance of genetic profiling based on different anatomic sites in patients with mucosal melanoma who received or did not receive immune checkpoint inhibitors. Cancer Cell Int 23, 187 (2023). https://doi.org/10.1186/s12935-023-03032-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-023-03032-3