Abstract
Background
Metastasis accounts for ninety percent of breast cancer (BrCa) mortality. Cortactin, Ras homologous gene family member A (RhoA), and Rho-associated kinase (ROCK) raise cellular motility in favor of metastasis. Claudins (CLDN) belong to tight junction integrity and are dysregulated in BrCa. Thus far, epidemiologic evidence regarding the association of different pro-metastatic genes with pathological phenotypes of BrCa is largely inconsistent. This study aimed to determine the possible transcriptional models of pro-metastatic genes incorporate in holding the integrity of epithelial cell–cell junctions (CTTN, RhoA, ROCK, CLDN-1, CLDN-2, and CLDN-4), for the first time, in association with clinicopathological features of primary BrCa.
Methods
In a consecutive case-series design, 206 newly diagnosed non-metastatic eligible BrCa patients with histopathological confirmation (30–65 years) were recruited in Tabriz, Iran (2015–2017). Real-time RT-PCR was used. Then fold changes in the expression of target genes were measured.
Results
ROCK amplification was associated with the involvement of axillary lymph node metastasis (ALNM; ORadj. = 3.05, 95%CI 1.01–9.18). Consistently, inter-correlations of CTTN-ROCK (β = 0.226, P < 0.05) and RhoA-ROCK (β = 0.311, P < 0.01) were determined among patients diagnosed with ALNM+ BrCa. In addition, the overexpression of CLDN-4 was frequently observed in tumors identified by ALNM+ or grade III (P < 0.05). The overexpression of CTTN, CLDN-1, and CLDN-4 genes was correlated positively with the extent of tumor size. CTTN overexpression was associated with the increased chance of luminal-A positivity vs. non-luminal-A (ORadj. = 1.96, 95%CI 1.02–3.77). ROCK was also expressed in luminal-B BrCa tumors (P < 0.05). The estrogen receptor-dependent transcriptions were extended to the inter-correlations of RhoA-ROCK (β = 0.280, P < 0.01), ROCK-CLDN-2 (β = 0.267, P < 0.05), and CLDN-1-CLDN-4 (β = 0.451, P < 0.001).
Conclusions
For the first time, our findings suggested that the inter-correlations of CTTN-ROCK and RhoA-ROCK were significant transcriptional profiles determined in association with ALNM involvement; therefore the overexpression of ROCK may serve as a potential molecular marker for lymphatic metastasis. The provided binary transcriptional profiles need more approvals in different clinical features of BrCa metastasis.
Similar content being viewed by others
Background
Breast cancer (BrCa) is globally the most common malignancy in women. BrCa is a heterogeneous disease with incident rate of 46.3 per 100,000 and mortality rate of 13.0 per 100,000 in 2018 worldwide, according to GLOBOCAN [1]. BrCa incidence in developing countries is increased due to cultural transition toward a sedentary lifestyle, Western diet, and increased rate of smoking, urbanization, and air pollutions [2,3,4]. It is accepted that estrogen leads to BrCa progression. Estrogen signaling is a therapeutic target for BrCa [5]; identifying pro-metastatic gene expression in different molecular subtypes (hormone receptors) with unique prognostic features may help elucidating new more personalized therapies. Furthermore, some important studies have documented evidence about preclinical diagnostic markers from predisposing mutations to raise the risk of BrCa [6], and the effect of some interventions on molecular targets have been assessed in solid tumors [7,8,9,10]. These could support lacking a consensus to support pro-metastatic genes in association with advanced features. Metastasis is considered for 90% of BrCa mortality which involves a complex multi-stage process, initially breaking away of tumor cells from primary tumor (dissociation step), degrading the proteins incorporate in the integrity of extracellular matrix (invasion step), transmigrate through vascular and/or lymph vessel (intravasation and extravasation steps), and cell-to-cell and cell–matrix adhesions with certain affinity to make organ-specific target metastasis (organotropism) [11].
Cortactin regulates actin cytoskeleton arrangement–a prerequisite for metastasis progressions—by binding to actin-related protein complex and facilitating releasing activated Wiskott Aldrich syndrome proteins [12]. Cortactin is an important regulator of cancer cell motility and mesenchymal movement [13]. Invadopodia, forming cellular actin-based protrusions, is mediated by cortactin activation and accompanies the invasion of cancer cells to the mesenchymal layer [14]. The overexpression of CTTN was associated with lymph node metastasis [15,16,17,18,19], advanced histologic grades [16, 20, 21], and larger tumor size [15, 16] in various cancers suggesting that cortactin might have prognostic impacts on different cancers but less paid attention to BrCa. One study reported a significant correlation between the protein expression of cortactin and lymphatic metastasis of breast tumors [22]. Therefore, the CTTN expression in association with histologic grade and tumor size of BrCa is largely missing. Of the few earlier reports on cortactin expression in BrCa regarding molecular subtypes [23, 24], a meta-cohort of primary BrCa reported CTTN overexpression in hormone receptor-positive samples [24].
There is a bifunctional activity between cortactin and Ras homologous gene family member A/Rho-associated kinase (RhoA/ROCK) complex in integration for enhancing actin stress fiber formation [12, 25]. RhoA belongs to the small GTPase family [25]. It triggers cell motility and amoeboid movement via the extensive formation of actin stress fiber and actomyosin contractility regulation [25]. ROCK activity—a major downstream effector of RhoA—is to stabilize actin filament and phosphorylate myosin light chain to eventually raise reforming rates of actomyosin contractility [26]. RhoA or ROCK overexpression predicts shorter survival rates of BrCa [27, 28]. RhoA overexpression was observed in advanced histologic grade [29], larger tumor size [27], and stages II-III of BrCa [30]. ROCK overexpression was correlated with nodal involvement and advanced histologic grade of BrCa [28, 31]. Significant results were not reported regarding the association of RhoA and ROCK expression with lymphatic metastasis and tumor size of BrCa, respectively. Studies could rarely provide evidence to show the association of molecular subtype of BrCa and the expression of RhoA or ROCK.
Claudins (CLDNs)—membrane transport proteins—have critical functions in forming and maintaining cell-to-cell adhesion complexes, so-called tight junctions [32]. CLDNs generally connect to actin cytoskeleton, and their functions may be regulated by Rho/ROCK pathway [33]. CLDNs dysregulation is documented in epithelial-derived cancers [32]. Different isoforms of CLDNs present in a tissue-specific manner. Their various functions highly depend on cell’s microenvironment [34]. The protein expression of CLDN-1 was reported to be associated with poor prognosis [35], larger tumor size [36], and advanced histologic grade of BrCa [36, 37]. However, positive or negative protein expression of CLDN-1 was reported to be correlated to the lymph node metastasis of BrCa [36, 38]. While the positive protein expression of CLDN-2 was associated with poor prognosis [38, 39], its loss of expression was related to nodal involvement of BrCa [34]. No study reported a significant correlation between CLDN-2 expression and histologic grade and tumor size of BrCa patients. Several reports indicated a positive protein expression of CLDN-4 connected to poor prognosis [37, 40], advanced grade [37, 40,41,42,43], and lymphatic metastasis [19, 41] of BrCa. However, positive or negative protein expression of CLDN-4 was reported to be correlated to a larger tumor size of BrCa [37, 43]. CLDNs expression was dependent on the molecular subtypes of breast tumors [35,36,37,38, 40, 41, 43, 44]. The data on the association of CLDNs expression and clinicopathological parameters remains inconclusive.
Sufficient information is not available to interpret pro-metastatic genes interaction in association with pathologic features in non-metastatic conditions. Therefore, this study aimed (i) to assess the correlation of pro-metastatic genes ‒ CTTN, RhoA, ROCK, CLDN-1, CLDN-2, and CLDN-4 ‒ with clinicopathological parameters, (ii) to determine the inter-correlation of pro-metastatic genes in primary BrCa.
Methods
Study population
This study is a part of ongoing large prospective cohort of consecutive case-series of BrCa patients-Breast Cancer Risk and Lifestyle (BCRL)- who were histopathologically diagnosed with primary malignancy. The BCRL is a multicenter study designed to assess lifestyle-related factors in association with BrCa risk prevention, regional to Northwestern Iran. The present study is a part of this cohort with ongoing recruitment began in May 2009. Participants with newly diagnosed and histologically confirmed BrCa (N = 206), who were admitted to the surgical wards of Nour-Nejat Hospital, Shams Hospital, Shahid Ghazi Educational-Oncology Hospital, and several oncology clinics located in Tabriz, Iran from May 2015 to January 2017. These are referral hospitals for oncologic surgeries with patients from different Northwestern Iran provinces (East and West Azerbaijan, Ardabil, Hamadan, and Zanjan). Participants were recruited from BrCa candidates before mastectomy surgery. The participants were 30-65 years old at the time of BrCa diagnosis. Eligible participants were mostly recruited from pre-menopausal women who had lymph node(s) positivity, invasive ductal carcinoma (IDC), and stages I-III. Other inclusion criteria mainly consisted of a completed written informed consent form and no subjective medical history, including benign breast diseases, other malignancy, and any oncologic surgery. Exclusion criteria were reported in our previous reports [3, 4, 45, 46] which were depicted in Fig. 1. Family history of breast and other cancers in first- and second-degree relatives were asked to lay out related pedigree analysis. Anthropometric measurements were examined as well.
Pathologic data
Histopathologic data, including tumor size, histological subtype (IDC and non-ductal carcinoma), axillary lymph node metastasis (ALNM), and histological tumor grade, were obtained from objective medical records. The tumor size was considered the greatest diameter of tumor [47] Evaluating the histologic grades was determined by reviewing the stained microtones of paraffin-embedded tumor samples according to the Nottingham combined grading system to detect grades based on tubule formation, nuclear grade, and mitotic activity [47]. Immunohistochemical staining was carried out for human epidermal growth factor receptor-2 (HER2), estrogen receptor (ER), and progesterone receptor (PR) (Fig. 2). For HER2 positivity, the membrane and cytoplasmic staining ≥ 10% of breast tumor cells were considered weak or high intensity [47]. Immunohistochemistry results obtained by nuclear antibody staining when accounted for above 1% of tumor cells indicated the positivity of ER and PR staining [48]. Molecular subtypes were classified based on the protocol summarized by Wu et al. [47]. Clinical staging was defined according to the American Joint Committee on Cancer; 8th BC staging guidelines [49]. Neither BrCa patients with contralateral ALNM classified as distant metastases (M1) nor BrCa patients with distant metastasis (M1; stage IV) were recruited [49]. Some pathological data were not available due to missing.
Quantitative real-time reverse transcriptase-polymerase chain reaction (qRT-PCR)
Before mastectomy surgery, fresh frozen tumor tissue and normal adjacent tissue were collected. Surgical tumor tissue section (core biopsy) consisted of 85% tumor cells with microscopic examinations [50]. QIAzol (Qiagen, USA) was applied to extract total mRNA and then evaluated using NanoDrop 2000 (Thermo Scientific, Germany), accounting for the absorbance at 260/280 nm. Total mRNA was converted into cDNA using QuantiTect reverse transcriptase (Qiagen, USA), based on the manufacturer’s protocol. The expression levels of target genes were determined by qRT-PCR, using LightCycler 480II (Roche, Germany). Materials used for PCR were composed of 12.5 μl from 10 × SYBER Green Master Mix (Nanohelix, South Korea), each primer solution (~ 10 pmol/μl), template cDNA (~ 100–200 ng/μl), and DEPC-treated water. PCR steps included an initial denaturation (15 min at 95 °C), followed by 40 cycles of denaturation (24 s at 95 °C) and annealing (35 s at 62 °C). Each sample was amplified in duplicate reactions. The amplification of hypoxanthine–guanine phosphoribosyltransferase was as an internal control (Additional file 1: Figure S1). Fold changes in the expression of target genes (CTTN, RhoA, ROCK, CLDN-1, CLDN-2, and CLDN-4) were calculated using a 2−ΔΔct formula [51]. PCR primers for relevant genes were listed in Additional file 2: Table S1.
Statistical analysis
A sample size including 158 subjects was calculated based on information provided by Dales et al. [52] regarding type I error (alpha) at 0.05 and the power of analysis (1 − β) at 90%. Outlier data were detected using the box plots. Kolmogorov–Smirnov test and histogram plot were carried out to assess the normal distribution of continuous variables. After using Chi square test, the correlation between two sets of categorical variables was interpreted. Fold change in the expression of gene was compared among sub-categories of clinicopathological (molecular subtypes, histologic grades, tumor size, and ALNM) by conducting the one-way analysis of covariance (ANCOVA) set at posthoc Bonferroni method, and the results were represented by bar diagram. Linear regression analysis was performed to present standardized β-coefficients (β) among genes in certain clinical stages (I and II-III) and binary status of hormone receptors, and ALNM features. Also, scatter plots were illustrated to show the correlations between targeted genes and tumor size. Standardized β out of linear regression analysis was accompanied by scatter plots in crude (β) and adjusted models (βadj.). Fold changes in the expression of genes were dichotomized using (1) median values, and (2) cutoff points determined by plotting receiver operating characteristic (ROC) curve based on ALNM status (as reference). Odds ratio (OR) and 95% confidence interval (95% CI) were obtained by logistic regression analysis to explore interesting genes as independent determinants of clinicopathological outcomes. The primary criteria for selecting a confounder in a model were identifying a significant univariate analysis concerning dependent variable. A certain model was identified for each gene using multivariate logistic regression analysis. The adjusted confounding factors were listed in Additional file 3: Table S2. Statistical analyses were performed using SPSS software, version 16 (SPSS Inc., USA). All two-tailed P-values < 0.05 were considered significant.
Results
The clinicopathological characteristics of 206 patients were summarized in Table 1. The mean age in diagnosing these patients was 46.65 ± 8.61 years. Patients were frequently younger than 24 years at first pregnancy (60.6%, P < 0.01) and were older than 13 years at menarche (80.1%, P < 0.001). They were pre-menopause (66.5%) and histopathologically identified with IDC (92.0%), ER + (87.3%), PR + (85.1%), and HER2- (79.6%) in the total study population (P < 0.001). Histologically, the most frequent dimension of the tumor was T2 (2 cm < size ≤ 5 cm) (61.3%, P < 0.001). Stage II BrCa was more frequent among the participants (65.7%). Histologic grade II tumors (67.4%) and ALNM involvement (65.2%) were the most observed histological features (P < 0.001). A significant agreement existed between BrCa frequency diagnosed with ALNM and lymphatic invasion status (P < 0.001), indicating the acceptable accuracy of data represented as ALNM status (Additional file 4: Table S3).
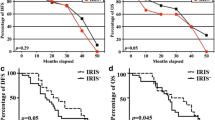
Figure 3 illustrates bar diagrams comparing the fold changes in the expression of relevant genes among categorical dependent factors including tumor size (≤ 2, and > 2 cm), ALNM (+/-), histologic grades (I, II, and III), and molecular subtypes. Larger tumor size (> 2 cm) showed higher expression levels of CTTN, CLDN-1, and CLDN-4 than those in smaller tumors (P < 0.05). Overexpressions of ROCK and CLDN-4 were observed in ALNM + tumors more than BrCa counterparts lacking ALNM (P < 0.05). The expression levels of CTTN among the patients with grade II were higher than grade I (P < 0.05). There was an increasing trend in CLDN-4 expression level among rising grades (P < 0.05). Of luminal A tumors, the fold change in the expression level of ROCK was found out less than those in luminal B and triple-negative tumors (P < 0.01).
Comparing fold changes in the expression of studied genes (mean ± S.E.) across different histo-pathological features of non-metastatic primary BrCa patients. P-values were obtained using ANCOVA (post hoc Bonferroni method). CTTN cortactin, RhoA ras homolog gene family member A, ROCK rho-associated kinase, CLDN claudin, S.E. standard error, ALNM axillary lymph node metastasis, HER2 human epidermal growth factor receptor 2. aAdjusted for pregnancy (number), lactation (number), surgical treatment (number), x-ray exposure (number), BMI (kg/m2), waist circumference (cm), waist to hip ratio, and physical activity (MET-h/week); bAdjusted for age at menarche (year), surgical treatment (number), waist circumference (cm), and physical activity (MET-h/week); cAdjusted for age at diagnosis (year), duration of oral contraceptive usage (month), lactation (number), BMI (kg/m2), hip circumference (cm), and waist to hip ratio; dAdjusted for the weight (kg) and the age at menarche (year). A significant result was indicated by *P < 0.05 or #P < 0.01
The scatter plots indicating the correlations among the genes of interest and tumor size were shown in Fig. 4. CTTN overexpression (βadj. = 0.253, P < 0.05), CLDN-1 (βadj. = 0.345, P < 0.01), and CLDN-4 (βadj. = 0.338, P < 0.01) were significantly correlated to the larger tumor dimension in the models adjusted for potential covariates.
Scatter plots showing linear regression coefficients (standardized β) were depicted to present correlations between fold changes in the expression of studied genes and tumor size of BrCa (n = 186). CTTN cortactin, RhoA ras homolog gene family member A, ROCK rho-associated kinase, CLDN claudin, βadj adjusted β. aAdjusted for abortion (number), pregnancy (number), and hip circumference (cm); bAdjusted for age at diagnosis (year) and BMI (kg/m2); cAdjusted for age at diagnosis (year) and waist to hip ratio; dAdjusted for abortion (number), lactation (number), the age at menarche (year), and duration of oral contraceptive usage (month); eAdjusted for waist circumference (cm) and age at first pregnancy (year); fAdjusted for age at menarche (year), BMI (kg/m2), abortion (number), and duration of oral contraceptive usage (month). A significant result was indicated by *P < 0.05
OR and 95% CI estimated to represent the associations between the expression levels of genes and ALNM status (Table 2) and tumor grades (Table 3) using unadjusted (crude) and multivariate-adjusted models. According to high expression levels of ROCK in lymph node-positive (Fig. 3), ROCK overexpression was significantly associated with ALNM + after adjustments for potential covariates (OR Median-based cutoff = 3.05, 95%CI 1.01–9.18) (Table 2). The overexpressions of CTTN (OR ROC-based cutoff = 4.33, 95%CI 1.64–11.43) and ROCK (OR ROC-based cutoff = 2.92, 95%CI 1.18-7.24) were associated with developed grade II breast carcinoma (Table 3). Multivariate adjusted models showed positive associations between CTTN (OR ROC-based cutoff = 5.08, 95%CI 1.75–14.69), ROCK (OR ROC-based cutoff = 2.86, 95%CI 1.14–7.14), and grade II tumors vs. considering grade I as reference (Table 3). Moreover, the overexpressions of CTTN and ROCK were associated with grade III in crude (CTTN: OR ROC-based cutoff = 3.90, 95%CI 1.10–13.81; ROCK: OR ROC-based cutoff = 4.40, 95%CI 1.33–14.48) and adjusted (CTTN: OR ROC-based cutoff = 5.08, 95%CI 1.32–19.44; ROCK: OR ROC-based cutoff = 4.22, 95%CI 1.26–14.07) models (Table 3).
Since luminal A was the predominant sub-class of molecular subtypes in the present study, CTTN overexpression was significantly associated with luminal A vs. other molecular subtypes after adjustment for related confounders (OR Median-based cutoff = 1.96, 95%CI 1.02–3.77) (Table 4). Tumors characterized by luminal B (vs. non-luminal B) was remarkable in tumors overexpressed ROCK (OR ROC-based cutoff = 2.76, 95%CI 1.07–7.11). ROCK expression levels were also associated with triple-negative status compared to non-triple negative subtypes (OR ROC-based cutoff = 6.29, 95% CI 1.27–31.11) (Table 4).
Linear regression analysis was performed to obtain correlation coefficients (β) among the genes of interest and subgroup analyses due to hormonal receptor status, ALNM feature, and clinical staging, and presented in Table 5. For the total study population, findings indicated positive associations among the expression levels of ROCK and RhoA (β = 0.246, P < 0.001, CTTN (β = 0.170, P < 0.05), and CLDN-2 (β = 0.237, P < 0.05) as dependent variables (Table 5). CLDN-1 expression levels was strongly correlated to CLDN-4 as well (β = 0.411, P < 0.001) (Table 5).
In the case of ER + tumors (PR +/-), ROCK up-regulation was significantly correlated to RhoA (β = 0.280, P < 0.01) and CLDN-2 (β = 0.267, P < 0.05). Of tumors characterized by ER positivity, CLDN-1 was significantly associated with CLDN-4 (β = 0.411, P < 0.001) (Table 5). In ER-negative patients, the expression levels of CTTN and CLDN-2 were strongly intercorrelated (β = 0.655, P < 0.05) (Table 5).
ROCK overexpression was significantly associated with up-regulation at RhoA (β = 0.311, P < 0.01) and CTTN (β = 0.226, P < 0.05) when there was the involvement of ALNM. The expression levels of CLDN-1 and CLDN-4 were inter-correlated in sub-population defined by the presence of ALNM (β = 0.377, P < 0.001) and absent ALNM at diagnosis (β = 0.522, P < 0.001) (Table 5). In the absence of ALNM development, ROCK expression levels was strongly associated with CLDN-2 (β = 0.733, P < 0.001) (Table 5).
Of patients at stage I, ROCK up-regulation was strongly correlated to CTTN (β = 0.519, P < 0.01) and CLDN-2 (β = 0.741, P < 0.001) (Table 5). Moreover, RhoA-ROCK inter-correlation was significantly found out in clinical stages II-III (β = 0.308, P < 0.01). The overexpression of CLDN-1 was significantly observed concerning CLDN-4 among patients diagnosed with disease at stages I (β = 0.389, P < 0.01) and II-III (β = 0.429, P < 0.001) (Table 5).
Discussion
For the first time, the results of this molecular epidemiologic study provided insights about the inter-correlations of CTTN-ROCK and RhoA-ROCK in association with the involvement of ALNM. It can substantiate ROCK over-regulation as a molecular determinant of tumor outgrowth and spread to axillary lymph nodes. The inter-correlation of RhoA-ROCK was associated with advanced clinical stages of primary BrCa. Moreover, the overexpression of CTTN, CLDN-1, and CLDN-4 genes was positively correlated with the extent of tumor size, particularly in ER + status. CLDN-4 up-regulation was notable in advanced histologic tumor grade and lymph node involvement.
Lymphatic metastasis
A significant correlation was observed between ROCK overexpression and positive axillary lymph node involvement. Similar to our findings, Lane et al. [28] showed that protein and mRNA expression levels of ROCK were significantly correlated to nodal involvement. Bottino et al. [31] reported ROCK overexpression in breast tissue specimens (IDC) of patients who were diagnosed with ALNM. ROCK belongs to a family of serine/threonine kinases are recognized to promote actomyosin contractility by direct phosphorylation of myosin light chain [26]. Therefore, ROCK can promote the motility and adhesion of cancer cells in extravasation, thus might hold tumor dissemination possibility in lymphatic metastasis [53].
RhoA up-regulation was observed in tumors with lymph node metastasis in the cervical [54] and colorectal cancers [55, 56]. An earlier study indicated RhoA overexpression in clinical stages II and III of BrCa [30]. The co-transcription of the RhoA/ROCK complex was reported in human cancers [54, 57]. Here, the co-transcription of RhoA-ROCK was observed in patients diagnosed with clinical stages II-III. This finding describes the possible contribution of RhoA and ROCK to potentiate tumor cells to develop invasive stages of BrCa, including local lymph node metastasis [53]. To the best of our knowledge, this is the first study that indicated RhoA-ROCK inter-correlation in association with ALNM +, which supports the possible contribution of RhoA expression to its downstream effector molecule, i.e., the over-regulation of ROCK, thereby likely to evoke the biological response related to metastasis [14, 25, 53].
Cortactin can potentially promote the polymerization and rearrangement of actin in the cellular cortex, which modulates actin cytoskeleton and related dynamics [13]. Findings of experimental animal models compared to MCF-7 tumor cells indicated that the mRNA level of CTTN might drive tumor cells to disseminate into lymphatic vessels and develop lymph node metastasis [58]. One study reported a significant correlation between the protein expression of cortactin and lymph node metastasis of breast tumors [22]. The present findings provide new evidence showing that inter-correlation of CTTN-ROCK could be significantly correlated to positive lymph node involvement. In addition, cortactin effects on actin remodeling and subsequent degradation of the extracellular matrix occur in cancerous dissemination might be mediated by GTPase RhoA activity [59, 60]. Studies for supporting CTTN-ROCK interaction are limited; however, Croucher et al. [60] indicated that cortactin is competent to induce RhoA transcription in a dose-dependent manner in the case of CTTN overexpression which is revealed in head and neck squamous cells. A considerable dose of cortactin may overcome the distorted link between cortactin and RhoA by negative co-effectors [60]. Also, cortactin-related RhoA activity is documented to show cellular proliferation in head and neck squamous cell carcinoma [60]. GTP-RhoA (active form) interacts with the C-terminal part of coiled-coil domain and activates ROCK which is the main downstream target of active RhoA [26]. Nevertheless, a few pieces of evidence represented a background for cortactin-related RhoA activation, regardless of metastatic features, this study suggests evidence indicating the association between CTTN and ROCK expressions in favor of ALNM development.
The overexpression of CLDN-4 was observed in patients with lymphatic metastasis subgroup which is in agreement with previous reports of BrCa patients [19, 41]. The CLDN-4-dependent up-regulation of matrix metalloproteinase (MMP)-2 and MMP-9 and increased invasiveness might be another clue responsible for lymphatic metastasis [61].
Histologic grades and tumor size
This is the first study to indicate the higher mRNA expression levels of CTTN in significant correlations with larger tumor size and histologic grade II of primary BrCa. Similarly, the mRNA expression levels of CTTN was correlated to a larger tumor size in colon cancer [15] and non-small cell lung cancers [16]. Moreover, previous studies reported that protein expression of cortactin could be associated with advanced histologic grades and poor differentiation in the cancers of colon [20], pancreas [21], and lung [16]. Overexpressed CTTN might induce the expression of S-phase kinase-associated protein-2 (SKP-2) to promote the cellular proliferation of head and neck squamous cell carcinoma [60], which was associated with larger tumor size observed in BrCa patients [62, 63]. Besides, cortactin-related SKP-2 signaling and subsequent down-regulation of cyclin-dependent kinase inhibitors might promote rapid cellular proliferation to result in increased tumor size. On the other hand, Clark et al. [64, 65] explained that cortactin is a transcriptional regulator of MMPs. Insulin-like growth factors and epidermal growth factor are potential tumor growing effectors released by MMP’s proteolytic activities, and likely MMPs can enhance cellular proliferation [66]. The findings indicated CTTN expression associated with larger tumor size of BrCa could describe cortactin as an effective variable and call to question its role in advanced histologic grade of breast carcinoma for future studies.
The present findings showed that mRNA expression of CLDN-1 was positively correlated to larger tumor size in our population of BrCa. Similarly, in a previous study, the overexpression of CLDN-1 was reported in association with a larger tumor size [36]. CLDN-1 can interact with the epithelial to mesenchymal transition (EMT) related markers such as zinc finger protein SNAI-1 (Snail-1), zinc finger protein SNAI-2 (Slug), and zinc finger E-box binding homeobox-1 (Zeb-1) in human BrCa cell lines [44, 67, 68] and therefore can suppress E-cadherin which is an essential molecule incorporating into an active EMT. CLDN-1 might enhance Zeb-1 levels through phosphatidylinositol-3 kinase (PI3K)/protein kinase B (Akt) pathway and Wnt/β-catenin pathway to suppress E-cadherin-related EMT pathogenesis in colon cancer [69]. Furthermore, the overexpression of CLDN-1 might be connected to MMP-9/Notch signaling to describe cellular proliferation in colorectal cancer [70]. Notch signaling is another aspect that gives rise to the overexpression of cyclins (A, B, and D) which they incorporate in cell cycle progression [71]. Moreover, overexpressed CLDN-1 might improve MMP-2-mediated proliferation of vascular smooth muscle cells [72] which might enhance angiogenesis to integrate CLDN-1 to tumorigenesis. Also, the anti-apoptotic effect of CLDN-1 was indicated in tamoxifen-treated MCF-7 cell lines [73]. Our findings showed a positive correlation between CLDN-4 expression and larger tumor size. Likewise, the positive protein expression of CLDN-4 was reported in correlation with larger tumor size of BrCa of Egyptian women [43]. CLDN-4 integration into tight junctions might be reduced by phosphorylation‒one of the post-translational modifications of CLDNs ‒ and therefore leads to gate function loss in various cancer cell lines [74, 75]. It might be a possible mechanism for CLDN-4 overexpression in BrCa, as well. An in vivo assay in nude mice was transplanted by CLDN-4-silenced MCF-7 cells indicated the regression in breast tumor size [42]. A meta-analysis confirmed the elevated protein levels of CLDN-4 in larger tumor size in gastric carcinoma [76]. Consistent with earlier studies [37, 40,41,42,43], CLDN-4 overexpression was associated with advanced histologic grade in present BrCa patients. The protein expression of CLDN-4 was positively correlated to Ki-67 labeling index among BrCa patients [37, 43], indicating that CLDN-4 might be contributed to proliferative pathways and cellular differentiation. Therefore, further studies in laboratory and epidemiologic outlooks are warranted to confirm further the association between CLDNs and advanced stages of BrCa.
Hormone receptors
The higher mRNA expression level of CTTN was found in luminal A than non-luminal A subtypes. Accordingly, a large-scale cohort of primary BrCa patients indicated CTTN overexpression in association with BrCa metastasis in ER + samples [24]. Cortactin might increase the risk of breast adenocarcinoma metastasis to bone marrow mediated by hyaluronan/cluster of differentiation-44 (CD44) signaling in MCF-7 cell lines indicating that the expression level of CTTN can be positively regulated by CD44 [77]. Karamanou and colleagues [78] indicated less expression levels of CD44 and cortactin in ERα + MCF-7 than levels observed in ERβ + MDA-MB-231 BrCa cells [78]. Magalhaes et al. [79] reported that the tyrosine phosphorylation of cortactin increased recruitment of Na+/H+ exchanger-1 (NHE-1) in MDA-MB-231 cell lines. The overactivation of NHE-1 ‒ a plasma membrane glycoprotein that controls intracellular pH ‒ could result in an acidic extracellular microenvironment leading to breast tumor cell invasion and the development of metastasis [80]. It could collectively support our findings showing the overexpression of CTTN in luminal A subtype of BrCa, particularly when CTTN up-regulation was evident in pre-menopause BrCa patients.
The hyaluronan/CD44 signaling was also correlated to the activation of RhoA/ROCK pathway and subsequent the phosphorylation of NHE-1, leading to breast tumor cell invasion [81]. Consistent with Oviedo et al. [82] indicated that the presence of estradiol could result in increased protein and mRNA expression levels of RhoA in human umbilical vein endothelial cells; our findings represented an additional insight expressing the inter-correlation of RhoA-ROCK in association with ER positivity. We also demonstrated that the luminal B subtype was remarkable in tumors overexpressed ROCK, suggesting that high expression level of ROCK may be affected by HER2 expression of breast tumors. Exposure to physiological concentrations of 17β-estradiol in human umbilical vein endothelial cells resulted in the interaction between ERα and Gα13 (heterotrimeric G protein) to induce RhoA/ROCK activity [83]. The RhoA/ROCK signaling pathway could be activated by nuclear factor erythroid 2-related factor 2 (NRF-2) [84]. The treatment with estradiol could activate PI3K/glycogen synthase kinase-3 beta pathway to increase the activity of NRF-2 in MCF-7 cells [85]. A meta-analysis of clinical studies reported that NRF2 overexpression was associated with a worse clinical outcomes of BrCa patients [86]. Another mechanism explains that in the presence of 17β-estradiol, ER may interact with c-Src to activate PI3K/Akt/RhoA pathway in human T47-D BrCa cells [87]. However, still, laboratory studies are insufficient to prove RhoA/ROCK bi-functionalities associated with the presence of certain molecular subtypes of BrCa.
ROCK may act as an upstream regulator to control CLDNs transcription [33]. The present study revealed a positive inter-correlation between ROCK-CLDN-2 in the case of ER positivity of tumors. In addition, the inter-correlation of CLDN-1-CLDN-4 was found abundant among the present ER + tumors. CLDN-4 up-regulation was seen in the estrogen-related tissues such as the breast and ovaries [88, 89]. Blanchard et al. [44] reported protein expression of CLDN-1 in positive association with CLDN-4 in basal-like and non-basal breast tumors. Akimoto et al. [90] represented a positive correlation between the activity of estrogen-dependent G protein-coupled receptor 30/Akt-related pathway and CLDN-1 expression in cervical adenocarcinoma cells [90]. The contradictory results from studies which addressed CLDNs expression concerning molecular subtypes [35,36,37,38, 40, 41, 43, 44], present findings could add an insight focusing on the association of CLDN-1-CLDN-4 and ROCK-CLDN-2 connected to breast tumors characterized by hormone receptor-positive.
The present significant correlation between RhoA and ROCK among breast tumors would give rise to the importance of ROCK transcription in accounting the present variation of RhoA expression. Several previous studies have considered ROCK expression as a reliable reference to determine the accuracy of RhoA expression in Her2-rich breast tissues [30], cervical cancer [54], and bladder cancer [57]. Consistent with the present findings, the protein expression of CLDN-1 was previously suggested as a biomarker to determine the accuracy of CLDN-4 expression in BrCa [44].
This study had some limitations. First, the sample size was small for subgroup analysis. Second, pathologic data were collected prospectively after surgery; therefore, data were not available for some cases. Third, the correction for multiplicity testing was a statistical approach warranted for future studies to provide better clusters of genes interdependently associated with the invasive pathological features of BrCa. Fourth, this study could not provide information about diagnostic accuracy based on the area under the curve of ROC, sensitivity, specificity, likelihood ratio, or other statistical parameters to interpret the diagnostic accuracy of pro-metastatic genes in detection or predicting BrCa features. Thereafter, we could not precisely address the accuracy of biomarkers to predict other disease diagnoses. The present findings provided some new evidence; further studies need to determine their prognostic impact on pathological characteristics in BrCa using a gold standard as reference. Accordingly, evidence should support pro-metastatic genes in association with advanced features before conducting any assessment for diagnostic accuracy of biomarkers. Microarray techniques could be suggested for future studies to assess a broader number of genes encompasses several pathways such as genes involved in controlling antioxidant defense system in association with RhoA transcription.
Conclusions
In summary, findings could suggest the binary settings of pro-metastatic genes, including CTTN-ROCK and RhoA-ROCK in association with a breast tumor diagnosed with infiltration into axillary lymph nodes which is representative of local breast metastasis. Findings put emphasize on ROCK transcription as a contributor to ALNM of IDC -BrCa. The present findings indicated the overexpression of CTTN, CLDN-1, and CLDN-4 in association with advanced stages of primary non-metastatic BrCa, which is highly evident in ER + status of breast tumors. Endocrine therapy might correlate with ER/PR related pro-metastatic genes that need further implications by future studies. However, further experimental studies are necessary to reveal mechanisms underlying gene-to-gene interactions in association with the molecular events representative of metastatic hallmarks of BrCa.
Availability of data and materials
Data cannot be shared publicly due to legal restrictions imposed by the Ethics Committee of Tabriz University of Medical Sciences. Data are available by the Ethics Committee of Tabriz University of Medical Sciences (research-vice@tbzmed.ac.ir), for researchers who meet the criteria for access to confidential data.
Abbreviations
- ALNM:
-
Axillary lymph node metastasis
- ANCOVA:
-
One-way analysis of covariance
- BrCa:
-
Breast cancer
- BMI:
-
Body mass index
- CLDN:
-
Claudin
- CTTN:
-
Cortactin
- CI:
-
Confidence interval
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor-2
- MMP:
-
Matrix metalloproteinase
- PR:
-
Progesterone receptor
- qRT-PCR:
-
Quantitative real-time reverse transcriptase-polymerase chain reaction
- OR:
-
Odds ratio
- RhoA:
-
Ras homolog gene family member-A
- ROCK:
-
Rho-associated kinase
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Rayegani SM, Tabibian E, Dehgolan SR. A review on the role of physical activity in cancer prevention: middle east reports. Int J Cancer Manag. 2017;10(7):e8992.
Mehdipour P, Pirouzpanah S, Sarafnejad A, Atri M, Tahereh Shahrestani S, Haidari M. Prognostic implication of CDC25A and cyclin E expression on primary breast cancer patients. Cell Biol Int. 2009;33(10):1050–6.
Mehdipour P, Pirouzpanah S, Kheirollahi M, Atri M. Androgen receptor gene CAG repeat polymorphism and breast cancer risk in Iranian women: A case-control study. Breast J. 2011;17(1):39–46.
Saha T, Makar S, Swetha R, Gutti G, Singh SK. Estrogen signaling: an emanating therapeutic target for breast cancer treatment. Eur J Med Chem. 2019;177:116–43.
Kumar B, Chand V, Ram A, Usmani D, Muhammad N. Oncogenic mutations in tumorigenesis and targeted therapy in breast cancer. Curr Mol Biol Rep. 2020:1-10.
Mohammad N, Malvi P, Meena AS, Singh SV, Chaube B, Vannuruswamy G, et al. Cholesterol depletion by methyl-β-cyclodextrin augments tamoxifen induced cell death by enhancing its uptake in melanoma. Mol Cancer. 2014;13(1):204.
Mohammad N, Singh SV, Malvi P, Chaube B, Athavale D, Vanuopadath M, et al. Strategy to enhance efficacy of doxorubicin in solid tumor cells by methyl-β-cyclodextrin: involvement of p53 and Fas receptor ligand complex. Sci Rep. 2015;5:11853.
Singh S, Chouhan S, Mohammad N, Bhat MK. Resistin causes G1 arrest in colon cancer cells through upregulation of SOCS 3. FEBS Lett. 2017;591(10):1371–82.
Muhammad N, Steele R, Isbell TS, Philips N, Ray RB. Bitter melon extract inhibits breast cancer growth in preclinical model by inducing autophagic cell death. Oncotarget. 2017;8(39):66226.
Chen W, Hoffmann AD, Liu H, Liu X. Organotropism: new insights into molecular mechanisms of breast cancer metastasis. NPJ Precis Oncol. 2018;2(1):1–12.
Kirkbride KC, Sung BH, Sinha S, Weaver AM. Cortactin: a multifunctional regulator of cellular invasiveness. Cell Adh Migr. 2011;5(2):187–98.
Jeannot P, Besson A. Cortactin function in invadopodia. Small GTPases. 2018:1-15.
Beaty BT, Condeelis J. Digging a little deeper: the stages of invadopodium formation and maturation. Eur J Cell Biol. 2014;93(10–12):438–44.
Ni Q-F, Yu J-W, Qian F, Sun N-Z, Xiao J-J, Zhu J-W. Cortactin promotes colon cancer progression by regulating ERK pathway. Int J Oncol. 2015;47(3):1034–42.
Noh SJ, Baek HA, Park HS, Jang KY, Moon WS, Kang MJ, et al. Expression of SIRT1 and cortactin is associated with progression of non-small cell lung cancer. Pathol Res Pract. 2013;209(6):365–70.
Rothschild BL, Shim AH, Ammer AG, Kelley LC, Irby KB, Head JA, et al. Cortactin overexpression regulates actin-related protein 2/3 complex activity, motility, and invasion in carcinomas with chromosome 11q13 amplification. Cancer Res. 2006;66(16):8017–25.
Luo M-L, Shen X-M, Zhang Y, Wei F, Xu X, Cai Y, et al. Amplification and overexpression of CTTN (EMS1) contribute to the metastasis of esophageal squamous cell carcinoma by promoting cell migration and anoikis resistance. Cancer Res. 2006;66(24):11690–9.
Abd El-Aziz YS, Megahed EM, Mostafa WA, Ezzo IM. Role of CD44 and cortactin in metastasis of oral squamous cell carcinoma. Tanta Dent J. 2017;14(2):62–7.
Kim YN, Choi JE, Bae JS, Jang KY, Chung MJ, Moon WS, et al. Expression of cortactin and focal adhesion kinase in colorectal adenocarcinoma: correlation with clinicopathologic parameters and their prognostic implication. Korean J Pathol. 2012;46(5):454–62.
Tsai WC, Lin CK, Lee HS, Gao HW, Nieh S, Chan DC, et al. The correlation of cortactin and fascin-1 expression with clinicopathological parameters in pancreatic and ampulla of Vater adenocarcinoma. Apmis. 2013;121(3):171–81.
Dedes KJ, Lopez-Garcia M-A, Geyer FC, Lambros MB, Savage K, Vatcheva R, et al. Cortactin gene amplification and expression in breast cancer: a chromogenic in situ hybridisation and immunohistochemical study. Breast Cancer Res Treat. 2010;124(3):653–66.
Sheen-Chen S-M, Huang C-Y, Liu Y-Y, Huang C-C, Tang R-P. Cortactin in breast cancer: analysis with tissue microarray. Anticancer Res. 2011;31(1):293–7.
Meirson T, Genna A, Lukic N, Makhnii T, Alter J, Sharma VP, et al. Targeting invadopodia-mediated breast cancer metastasis by using ABL kinase inhibitors. Oncotarget. 2018;9(31):22158–83.
O’Connor K, Chen M. Dynamic functions of RhoA in tumor cell migration and invasion. Small GTPases. 2013;4(3):141–7.
Manser EJ. Rho Family GTPases: Springer Science & Business Media; 2005.
Li M, Liu Y-p, Zhang X-h, Geng C-z, LI Z-h. Relationship of RhoA signaling activity with ezrin expression and its significance in the prognosis for breast cancer patients. Chin Med J. 2013;126(2):242-7.
Lane J, Martin TA, Watkins G, Mansel RE, Jiang WG. The expression and prognostic value of ROCK I and ROCK II and their role in human breast cancer. Int J Oncol. 2008;33(3):585–93.
Fritz G, Brachetti C, Bahlmann F, Schmidt M, Kaina B. Rho GTPases in human breast tumours: expression and mutation analyses and correlation with clinical parameters. Br J Cancer. 2002;87(6):635–44.
Murakami E, Nakanishi Y, Hirotani Y, Ohni S, Tang X, Masuda S, et al. Roles of Ras homolog A in invasive ductal breast carcinoma. Acta Histochem Cytochem. 2016:131-40.
Bottino J, Gelaleti GB, Maschio LB, Jardim-Perassi BV, de Campos Zuccari DAP. Immunoexpression of ROCK-1 and MMP-9 as prognostic markers in breast cancer. Acta Histochem. 2014;116(8):1367–73.
Tabariès S, Siegel P. The role of claudins in cancer metastasis. Oncogene. 2017;36(9):1176–91.
Hu Y-J, Wang Y-D, Tan F-Q, Yang W-X. Regulation of paracellular permeability: factors and mechanisms. Mol Biol Rep. 2013;40(11):6123–42.
Kim TH, Huh JH, Lee S, Kang H, Kim GI, An HJ. Downregulation of claudin 2 in breast carcinomas is associated with advanced disease. Histopathology. 2008;53(1):48–55.
Blanchard AA, Skliris GP, Watson PH, Murphy LC, Penner C, Tomes L, et al. Claudins 1, 3, and 4 protein expression in ER negative breast cancer correlates with markers of the basal phenotype. Virchows Arch. 2009;454(6):647–56.
Abd-Allah M, El-Sebaaie A, Omar E, Saad E, Youssef S. Evaluation of Claudin-1 and Ki-67 in different molecular subtypes of breast ductal carcinoma: immunohistochemical Study. Med J Cairo Univ. 2019;87(March):517–26.
Kolokytha P, Yiannou P, Keramopoulos D, Kolokythas A, Nonni A, Patsouris E, et al. Claudin-3 and claudin-4: distinct prognostic significance in triple-negative and luminal breast cancer. Appl Immunohistochem Mol Morphol. 2014;22(2):125–31.
Ma F, Ding X, Fan Y, Ying J, Zheng S, Lu N, et al. A CLDN1-negative phenotype predicts poor prognosis in triple-negative breast cancer. PLoS ONE. 2014;9(11):e112765.
Kimbung S, Kovács A, Bendahl P-O, Malmström P, Fernö M, Hatschek T, et al. Claudin-2 is an independent negative prognostic factor in breast cancer and specifically predicts early liver recurrences. Mol Oncol. 2014;8(1):119–28.
Lanigan F, McKiernan E, Brennan DJ, Hegarty S, Millikan RC, McBryan J, et al. Increased claudin-4 expression is associated with poor prognosis and high tumour grade in breast cancer. Int J Cancer. 2009;124(9):2088–97.
Logullo AF, Pasini FS, Nonogaki S, Rocha RM, Soares FA, Brentani MM. Immunoexpression of claudins 4 and 7 among invasive breast carcinoma subtypes: a large diagnostic study using tissue microarray. Mol Clin Oncol. 2018;9(4):377–88.
Ma X, Miao H, Jing B, Pan Q, Zhang H, Chen Y, et al. Claudin-4 controls the proliferation, apoptosis, migration and in vivo growth of MCF-7 breast cancer cells. Oncol Rep. 2015;34(2):681–90.
Abd-Elazeem MA, Abd-Elazeem MA. Claudin 4 expression in triple-negative breast cancer: correlation with androgen receptors and Ki-67 expression. Ann Diagn Pathol. 2015;19(1):37–42.
Blanchard AA, Ma X, Dueck KJ, Penner C, Cooper SC, Mulhall D, et al. Claudin 1 expression in basal-like breast cancer is related to patient age. BMC Cancer. 2013;13(1):268.
Pirouzpanah S, Varshosaz P, Fakhrjou A, Montazeri V. The contribution of dietary and plasma folate and cobalamin to levels of angiopoietin-1, angiopoietin-2 and Tie-2 receptors depend on vascular endothelial growth factor status of primary breast cancer patients. Sci Rep. 2019;9(1):1–18.
Shokri A, Pirouzpanah S, Foroutan-Ghaznavi M, Montazeri V, Fakhrjou A, Nozad-Charoudeh H, et al. Dietary protein sources and tumoral overexpression of RhoA, VEGF-A and VEGFR2 genes among breast cancer patients. Genes Nutr. 2019;14(1):22–38.
Wu Y, Sahin AA. Prognostic and predictive factors of invasive breast cancer. In: Aydiner A, İğci A, Soran A, editors. Breast Disease: Diagnosis and Pathology. 1. Switzerland: Springer; 2016. p. 187-206.
Brock JE, Hornick JL, Richardson AL, Dillon DA, Lester SC. A comparison of estrogen receptor SP1 and 1D5 monoclonal antibodies in routine clinical use reveals similar staining results. Am J Clin Pathol. 2009;132(3):396–401.
Hortobagyi GN, Connolly JL, D’Orsi CJ, Edge SB, Mittendorf EA, Rugo HS, et al. Breast. In: Amin MB, editor. AJCC Cancer Staging Manual. 8th ed. Chicago: American College of Surgeons; 2017. p. 589–636.
Wilkerson MD, Schallheim JM, Hayes DN, Roberts PJ, Bastien RR, Mullins M, et al. Prediction of lung cancer histological types by RT-qPCR gene expression in FFPE specimens. J Mol Diagn. 2013;15(4):485–97.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2 − ΔΔCT method. Methods. 2001;25(4):402–8.
Dales J-P, Garcia S, Meunier-Carpentier S, Andraca-Meyer L, Haddad O, Lavaut M-N, et al. Overexpression of hypoxia-inducible factor HIF-1a predicts early relapse in breast cancer: retrospective study in a series of 745 patients. Int J Cancer. 2005;116(5):734–9.
Rodriguez-Hernandez I, Cantelli G, Bruce F, Sanz-Moreno V. Rho, ROCK and actomyosin contractility in metastasis as drug targets. F1000Res. 2016;5.
Liu X, Chen D, Liu G. Overexpression of RhoA promotes the proliferation and migration of cervical cancer cells. Biosci Biotechnol Biochem. 2014;78(11):1895–901.
Wang H-b, Liu X-p, Liang J, Yang K, Sui A-h, Liu Y-j. Expression of RhoA and RhoC in colorectal carcinoma and its relations with clinicopathological parameters. Clin Chem Lab Med. 2009;47(7):811-7.
Takami Y, Higashi M, Kumagai S, Kuo PC, Kawana H, Koda K, et al. The activity of RhoA is correlated with lymph node metastasis in human colorectal cancer. Dig Dis Sci. 2008;53(2):467–73.
Kamai T, Tsujii T, Arai K, Takagi K, Asami H, Ito Y, et al. Significant association of Rho/ROCK pathway with invasion and metastasis of bladder cancer. Clin Cancer Res. 2003;9(7):2632–41.
Harrell JC, Dye WW, Harvell DM, Pinto M, Jedlicka P, Sartorius CA, et al. Estrogen insensitivity in a model of estrogen receptor–positive breast cancer lymph node metastasis. Cancer Res. 2007;67(21):10582–91.
Hoshino D, Tomari T, Nagano M, Koshikawa N, Seiki M. A novel protein associated with membrane-type 1 matrix metalloproteinase binds p27kip1 and regulates RhoA activation, actin remodeling, and matrigel invasion. J Biol Chem. 2009;284(40):27315–26.
Croucher DR, Rickwood D, Tactacan CM, Musgrove EA, Daly RJ. Cortactin modulates RhoA activation and expression of Cip/Kip cyclin-dependent kinase inhibitors to promote cell cycle progression in 11q13-amplified head and neck squamous cell carcinoma cells. Mol Cell Biol. 2010;30(21):5057–70.
Hwang TL, Changchien TT, Wang CC, Wu CM. Claudin-4 expression in gastric cancer cells enhances the invasion and is associated with the increased level of matrix metalloproteinase-2 and-9 expression. Oncol Lett. 2014;8(3):1367–71.
Liu J, Wei X-L, Huang W-H, Chen C-F, Bai J-W, Zhang G-J. Cytoplasmic Skp2 expression is associated with p-Akt1 and predicts poor prognosis in human breast carcinomas. PLoS ONE. 2012;7(12):e52675.
Ravaioli A, Monti F, Regan M, Maffini F, Mastropasqua M, Spataro V, et al. p27 and Skp2 immunoreactivity and its clinical significance with endocrine and chemo-endocrine treatments in node-negative early breast cancer. Ann Oncol. 2008;19(4):660–8.
Clark ES, Whigham AS, Yarbrough WG, Weaver AM. Cortactin is an essential regulator of matrix metalloproteinase secretion and extracellular matrix degradation in invadopodia. Cancer Res. 2007;67(9):4227–35.
Clark ES, Brown B, Whigham AS, Kochaishvili A, Yarbrough WG, Weaver AM. Aggressiveness of HNSCC tumors depends on expression levels of cortactin, a gene in the 11q13 amplicon. Oncogene. 2009;28(3):431–44.
Gialeli C, Theocharis AD, Karamanos NK. Roles of matrix metalloproteinases in cancer progression and their pharmacological targeting. FEBS J. 2011;278(1):16–27.
Martínez-Estrada OM, Cullerés A, Soriano FX, Peinado H, Bolós V, Martínez FO, et al. The transcription factors Slug and Snail act as repressors of Claudin-1 expression in epithelial cells. Biochem J. 2006;394(2):449–57.
Zhou B, Blanchard A, Wang N, Ma X, Han J, Schroedter I, et al. Claudin 1 promotes migration and increases sensitivity to tamoxifen and anticancer drugs in luminal-like human breast cancer cells MCF7. Cancer Invest. 2015;33(9):429–39.
Singh AB, Sharma A, Smith JJ, Krishnan M, Chen X, Eschrich S, et al. Claudin-1 up-regulates the repressor ZEB-1 to inhibit E-cadherin expression in colon cancer cells. Gastroenterology. 2011;141(6):2140–53.
Pope JL, Bhat AA, Sharma A, Ahmad R, Krishnan M, Washington MK, et al. Claudin-1 regulates intestinal epithelial homeostasis through the modulation of Notch-signalling. Gut. 2014;63(4):622–34.
Acar A, Simões BM, Clarke RB, Brennan K. A role for notch signalling in breast cancer and endocrine resistance. Stem Cells Int. 2016;2016:1–6.
Belo V, Guimarães DA, Castro MM. Matrix metalloproteinase 2 as a potential mediator of vascular smooth muscle cell migration and chronic vascular remodeling in hypertension. J Vasc Res. 2015;52(4):221–31.
Akasaka H, Sato F, Morohashi S, Wu Y, Liu Y, Kondo J, et al. Anti-apoptotic effect of claudin-1 in tamoxifen-treated human breast cancer MCF-7 cells. BMC Cancer. 2010;10(1):548.
Tanaka M, Kamata R, Sakai R. EphA2 phosphorylates the cytoplasmic tail of Claudin-4 and mediates paracellular permeability. J Biol Chem. 2005;280(51):42375–82.
D’Souza T, Indig FE, Morin PJ. Phosphorylation of claudin-4 by PKCε regulates tight junction barrier function in ovarian cancer cells. Exp Cell Res. 2007;313(15):3364–75.
Chen X, Zhao J, Li A, Gao P, Sun J, Song Y, et al. Clinicopathological significance of claudin 4 expression in gastric carcinoma: a systematic review and meta-analysis. Onco Targets Ther. 2016;9:3205–12.
Hill A, McFarlane S, Mulligan K, Gillespie H, Draffin J, Trimble A, et al. Cortactin underpins CD44-promoted invasion and adhesion of breast cancer cells to bone marrow endothelial cells. Oncogene. 2006;25(45):6079–91.
Karamanou K, Franchi M, Onisto M, Passi A, Vynios DH, Brézillon S. Evaluation of lumican effects on morphology of invading breast cancer cells, expression of integrins and downstream signaling. FEBS J. 2020;8:1–19.
Magalhaes MA, Larson DR, Mader CC, Bravo-Cordero JJ, Gil-Henn H, Oser M, et al. Cortactin phosphorylation regulates cell invasion through a pH-dependent pathway. J Cell Biol. 2011;195(5):903–20.
Amith SR, Wilkinson JM, Baksh S, Fliegel L. The Na +/H + exchanger (NHE1) as a novel co-adjuvant target in paclitaxel therapy of triple-negative breast cancer cells. Oncotarget. 2015;6(2):1262.
Bourguignon LY, Singleton PA, Diedrich F, Stern R, Gilad E. CD44 interaction with Na + -H + exchanger (NHE1) creates acidic microenvironments leading to hyaluronidase-2 and cathepsin B activation and breast tumor cell invasion. J Biol Chem. 2004;279(26):26991–7007.
Oviedo PJ, Sobrino A, Laguna-Fernandez A, Novella S, Tarín JJ, García-Pérez M-A, et al. Estradiol induces endothelial cell migration and proliferation through estrogen receptor-enhanced RhoA/ROCK pathway. Mol Cell Endocrinol. 2011;335(2):96–103.
Simoncini T, Scorticati C, Mannella P, Fadiel A, Giretti MS, Fu X-D, et al. Estrogen receptor α interacts with Gα13 to drive actin remodeling and endothelial cell migration via the RhoA/Rho kinase/moesin pathway. Mol Endocrinol. 2006;20(8):1756–71.
Zhang C, Wang H-J, Bao Q-C, Wang L, Guo T-K, Chen W-L, et al. NRF2 promotes breast cancer cell proliferation and metastasis by increasing RhoA/ROCK pathway signal transduction. Oncotarget. 2016;7(45):73593.
Wu J, Williams D, Walter GA, Thompson WE, Sidell N. Estrogen increases Nrf2 activity through activation of the PI3K pathway in MCF-7 breast cancer cells. Exp Cell Res. 2014;328(2):351–60.
Almeida M, Soares M, Ramalhinho AC, Moutinho JF, Breitenfeld L, Pereira L. The prognostic value of NRF2 in breast cancer patients: a systematic review with meta-analysis. Breast Cancer Res Treat. 2020;179(3):523–32.
Zheng S, Huang J, Zhou K, Zhang C, Xiang Q, Tan Z, et al. 17β-Estradiol enhances breast cancer cell motility and invasion via extra-nuclear activation of actin-binding protein ezrin. PLoS One. 2011;6(7).
Seth P, Porter D, Lahti-Domenici J, Geng Y, Richardson A, Polyak K. Cellular and molecular targets of estrogen in normal human breast tissue. Cancer Res. 2002;62(16):4540–4.
Hough CD, Sherman-Baust CA, Pizer ES, Montz F, Im DD, Rosenshein NB, et al. Large-scale serial analysis of gene expression reveals genes differentially expressed in ovarian cancer. Cancer Res. 2000;60(22):6281–7.
Akimoto T, Takasawa A, Takasawa K, Aoyama T, Murata M, Osanai M, et al. Estrogen/GPR30 signaling contributes to the malignant potentials of ER-negative cervical adenocarcinoma via regulation of claudin-1 expression. Neoplasia. 2018;20(10):1083–93.
Committee NEA. Ethical guidelines for observational studies: observational research, audits and related activities. New Zealand2012. http://neac.health.govt.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Acknowledgements
The authors would like to thank all the subjects involved in this study for their participation and the staff members of Nour-Nejat Hospital and Nemoone laboratory.
Funding
This study was financially supported by Shiraz University of Medical Sciences, Shiraz, Iran (SUMS; Registration no.: 94-01-84-10880; http://research.sums.ac.ir). It was also funded by the Stem Cell Research Center, Tabriz University of Medical Sciences, Tabriz, Iran (TUMS; Registration no.: 5/D/962552; https://scrc.tbzmed.ac.ir).
Author information
Authors and Affiliations
Contributions
SM Supervision; Investigation; Resources; Writing–review & editing; MF Formal analysis; Investigation; Methodology; Software; Writing-original draft; VM Supervision; Conceptualization; Methodology; GT Investigation; Resources; AF Investigation; Resources; HN Investigation; Resources; SP Supervision; Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Validation; Visualization; Writing-review & editing. This article was extracted using a dataset out of a Ph.D. thesis titled “The association between dietary pattern and expression levels of HIF-1α, ROCK, and CTTN genes in breast cancer patients”, registered at SUMS, Shiraz, Iran (Registration no.: 94-01-84-10880) and TUMS, Tabriz, Iran (Registration no.: 5/D/962552).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Before interviewing, written consent was obtained from all participants. The study was designed and carried out according to the Ethical Guidelines for Observational Studies [91]. The full study protocol was reviewed and approved by the ethics committee of both Tabriz University of Medical Sciences (Ethics no: IR.TBZMED.REC.1396.438) and Shiraz University of Medical Sciences (Ethics no: IR.SUMS.REC.1395.S378). This report was prepared in compliance with the STROBE statements [92].
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Fig S1.
The overexpression of pro-metastatic genes were associated with clinicopathologic features of breast cancer. CLDN claudin, CTTN cortactin, HGPRT hypoxanthine–guanine phosphoribosyltransferase, NTC non-template control, RhoA ras homolog gene family member A, ROCK rho-associated kinase, N normal, T tumor.
Additional file 2: Table S1.
Primer sequences used for qRT-PCR amplification.
Additional file 3: Table S2.
General characteristics of patients with invasive breast cancer (N = 206).
Additional file 4: Table S3.
Associations between lymphatic invasion and the involvement of axillary lymph node metastasis (ALNM).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mazloomi, SM., Foroutan-Ghaznavi, M., Montazeri, V. et al. Profiling the expression of pro-metastatic genes in association with the clinicopathological features of primary breast cancer. Cancer Cell Int 21, 6 (2021). https://doi.org/10.1186/s12935-020-01708-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-020-01708-8