Abstract
Objective
Population-based national data on the trends in expenditures related to coexisting atherosclerotic cardiovascular diseases (ASCVD) and diabetes is scarce. We assessed the trends in direct health care expenditures for ASCVD among individuals with and without diabetes, which can help to better define the burden of the co-occurrence of diabetes and ASCVD.
Methods
We used 12-year data (2008–2019) from the US national Medical Expenditure Panel Survey including 28,144 U.S individuals aged ≥ 18 years. Using a two-part model (adjusting for demographics, comorbidities and time), we estimated mean and adjusted incremental medical expenditures by diabetes status among individuals with ASCVD. The costs were direct total health care expenditures (out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources) from various sources (office-based visits, hospital outpatient, emergency room, inpatient hospital, pharmacy, home health care, and other medical expenditures).
Results
The total direct expenditures for individuals with ASCVD increased continuously by 30% from $14,713 (95% confidence interval (CI): $13,808–$15,619) in 2008–2009 to $19,145 (95% CI: $17,988–$20,301) in 2008–2019. Individuals with diabetes had a 1.5-fold higher mean expenditure that those without diabetes. A key driver of the observed increase in direct costs was prescription drug costs, which increased by 37% among all individuals with ASCVD. The increase in prescription drug costs was more pronounced among individuals with ASCVD and diabetes, in whom a 45% increase in costs was observed, from $5184 (95% CI: $4721–$5646) in 2008–2009 to $7501 (95% CI: $6678–$8325) in 2018–2019. Individuals with ASCVD and diabetes had $5563 (95% CI: $4643–$6483) higher direct incremental expenditures compared with those without diabetes, after adjusting for demographics and comorbidities. Among US adults with ASCVD, the estimated adjusted total direct excess medical expenditures were $42 billion per year among those with diabetes vs. those without diabetes.
Conclusions
In the setting of ASCVD, diabetes is associated with significantly increased health care costs, an increase that was driven by marked increase in medication costs.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Atherosclerotic cardiovascular disease (ASCVD) is associated with a substantial burden of morbidity and mortality in the US [1]. Over time, the burden of ASCVD has remained high, and its costs are heightened by the implementation of an increasing number of life-prolonging therapies [1]. Indeed, the costs related to CVD are projected to continue to increase, reaching annual figures of $818 billion for direct costs and $276 billion for indirect costs by 2030 [2]. Diabetes increases the risk of CVD by at least twofold, as compared to the general population [3]. Indeed, ASCVD are the most common complications among individuals with diabetes, including peripheral artery disease, stable angina, nonfatal myocardial infarction and stroke [4].
Managing ASCVD in combination with comorbidities such as diabetes mellitus, complicates the expenses. Hitherto, the extant studies on ASCVD-related costs have seldom examined the overall impact of comorbidities such as diabetes on the direct costs [5,6,7,8,9,10]. Furthermore, these studies have been limited to short time period, focused on a single aspect of expenses (mainly in-hospital costs) or have not always had a national reach [5,6,7,8,9,10]. The extent to which the coexistence of diabetes with ASCVD affect direct medical costs (hospitalizations, outpatient visits, and other medical services) largely remain unclear. Indeed, most prior studies predated the widespread use of novel medications with robust cardioprotective effects such as the glucagon-like peptide -1 (GLP-1) receptor agonists (GLP-1RAs), the sodium glucose co-transporter -2 (SGTL2) inhibitors and the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, all of which may have contributed to the rise in costs. Overall, there is a lack of nationally representative data over a prolonged time period to reliably assess the trends in resource use among ASCVD patients in the US, including in subgroups defined by diabetes status.
Using the Medical Expenditure Panel Survey Household Component (MEPS-HC) [11], the largest nationally representative survey of medical costs the United States, we examined the changes over time in direct health care expenditures among U.S. adults with ASCVD with and without diabetes from 2008 to 2019, with the aim of assessing how the burden of diabetes has affected the care of ASCVD in the US.
Methods
Study population
We used data from the 2008–2019 Medical Expenditure Panel Survey (MEPS) for this investigation. The data from these surveys is provided by the Agency for Healthcare Research and Quality and is a publicly available, nationally representative panel dataset. The MEPS includes several waves of national surveys of families and individuals, their medical providers, and employers in the U.S. MEPS samples data on an average of 39,000 individuals per year to estimate the use of medical resources in the U.S. population. The MEPS sample is drawn from reporting units in the previous year’s National Health Interview Survey, a nationally representative sample (with oversampling for Black and Hispanic individuals) of the US civilian non-institutionalized population. The MEPS has a complex design consisting of clustering, stratification, and multistage and disproportionate sampling with oversampling of certain population groups to ensure representativeness. The dataset contains information on demographic and socioeconomic attributes, health insurance coverage, healthcare utilization, expenditures, sources of payment, health status and functioning, along with other healthcare related information in the non-institutionalized civilian US population. Medical use and expenditures were collected from both household respondents and their medical providers. We pooled 12-year data to ensure sufficient sample size and increase precision of our estimates.
Our study focused on adults aged at least 18 years of age, with a diagnosis of ASCVD. When available, information from both the full-year consolidated data files and the medical conditions files were utilized to determine the presence of medical conditions, thereby maximizing the sensitivity of our definitions. The medical conditions and procedures reported by the MEPS-HC related to ASCVD were recorded by an interviewer as verbatim text and then converted by professional coders to International Classification of Disease codes. MEPS reports the first three digits of International Classification of Disease (ICD)-9 codes (until 2015) and ICD-10 codes (2016 onwards) in the household component. Respondents were included in the study based on the availability of an ASCVD diagnosis at any time during the year; with no requirement for hospital admission to be included in the study [12].
ASCVD and diabetes status definitions
ASCVD and diabetes were defined on the basis of self-report that led to medical visits or treatment within the interview year. The self-reported conditions were transcribed and classified with ICD-9 and ICD 10-codes. Information on each respondent is annualized, in which a calendar year is the duration of time for which information is reported in MEPS.
In brief, ASCVD was determined by the presence of any coronary heart disease, myocardial infarction or angina, stroke, or peripheral vascular disease (as per the ICD codes). Diabetes was defined based on the relevant ICD codes. The ICD -9 and ICD-10 codes used to define ASCVD and diabetes are detailed Supplementary Table 1.
Outcomes
Our primary outcome of interest was the annual overall healthcare related costs. These are direct medical costs including the total direct health care expenditures for the calendar year for each individual. These overall costs were also further stratified into two mutually-exclusive contributing components corresponding to prescription drug costs and overall healthcare costs besides prescription drug costs (“medical costs”). The direct medical costs were estimated by point of service, with the following point-of-service categories used: hospital (inpatient, outpatient, and emergency department), physician (office-based visits), prescription, home health, and other (including nursing home, rehabilitation, vision, medical supplies, dental). The costs include out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources; medical expenditures including office-based medical provider, hospital outpatient, emergency room (ER), inpatient hospital (including zero-night stays), pharmacy, dental, home health care, and other medical expenditures reported during the calendar year. The costs were adjusted to 2019 values using the Personal Health Care Expenditure (PHCE) component of the National Health Expenditure Accounts, provided by the U.S. Department of Health and Human Services [13].
We used the 12-year pooled cross-sectional data and accounted for analytic sampling weight by dividing it by the number of years being pooled, as recommended for MEPS. We combined 12 years of data (2008–2019), as over each year these have a common variance structure necessary to ensure compatibility of our variables within the complex sample design.
Covariates
The covariates defined on the basis of self-report included demographic and clinical variables. These included: age, sex, race/ethnicity, marital status, region of the country, insurance type, family income, calendar year and comorbidities—arthritis, asthma, high cholesterol, any cancer, chronic obstructive pulmonary disease, depression, hypertension and heart failure.
Statistical analyses
The baseline characteristics of patients are presented by diabetes status, as absolute numbers and percentages for categorical variables.
We estimated the unadjusted mean direct medical expenditures for individuals with ASCVD overall and by diabetes status. We derived the excess costs imposed by diabetes among individuals with ASCVD, which was determined via the incremental expenditure regression-based approach [14]. In our regression model, the outcome variable was expenditure (overall, medical or prescription drug costs) and the primary independent variable was the presence of comorbid diabetes. The regression approach implemented was a two-part model wherein the first part was logistic regression, and the outcome was any expenditure (binary), and the second part was a model for which the outcome was the all-cause expenditure amount. The model used for the second part was a generalized linear model (GLM), with a log function and a distribution as determined by the modified Park test [15,16,17]. These procedures were implemented via the ‘twopm’ and ‘glmdiag’ STATA commands, and the marginal incremental costs across the two parts was determined via the delta method [18, 19]. The covariates in adjusted models included age, insurance coverage, sex, race/ethnicity, marital status, family income, region of the country, year, and comorbid conditions (arthritis, asthma, high cholesterol, any cancer, chronic obstructive pulmonary disease, depression, hypertension, and heart failure).
Throughout the analyses, the complex survey design of the data was considered and the appropriate analytical procedures (SURVEYFREQ, SURVEYMEANS, domain statements, and svy) were implemented [20]. The Personal Health Care Expenditure (PHCE) component of the National Health Expenditure Accounts, provided by the U.S. Department of Health and Human Services, was utilized to adjust costs to 2019 values [13].
For all the analyses, we accounted for the complex sampling design of MEPS dataset by using sampling weight, variance estimation stratum and primary sampling unit (clustering). A p value < 0.05 was considered statistically significant. All analyses were performed using SAS 9.4 and STATA MP 16.
Results
Characteristics of the study participants
The characteristics of US adults with ASCVD with and without diabetes during the 2008–2019 period are shown in Table 1. The final study sample consisted of 28,144 individuals with ASCVD, of which 9,599 had diabetes. Compared to individuals without diabetes, individuals with ASCVD and comorbid diabetes were older (67.30 years vs. 65.27 years), more likely to be Black (24.33% vs. 18.70%) or Hispanic (20.53% vs. 15.30%) individuals, to have a larger proportion of individuals on public insurance (54.18% vs. 43.86%) and had a higher prevalence of all comorbidities examined, except for cancer. The prevalence of diabetes among individuals with ASCVD increased from 28.37% in 2008–2009 to 32.10% in 2018–2019.
Unadjusted costs among ASCVD individuals with and without diabetes
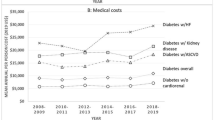
The detailed results on the unadjusted costs among individuals with ASCVD have been presented in Fig. 1 and Supplementary Tables 2, 3 and 4.
The total mean unadjusted direct expenditures for individuals with ASCVD increased continuously by 30% from $14,713 (95% confidence interval (CI): $13,808, $15,619) in 2008–2009 to $19,145 (95% CI: $17,988, $20,301) in 2018–2019 (Fig. 1A and Supplementary Table 2). There was a corresponding increase of 26% in overall cost, which was higher to begin with, among individuals with ASCVD and comorbid diabetes—from $20,539 (95% CI: $18,688, $22,389) in 2008–2009 to $25,878 (95% CI: $23,496, $28,260) in 2018–2019 through the study period (Fig. 1A and Supplementary Table 2).
The changes in medical costs among ASCVD individuals over time are shown in Fig. 1B and Supplementary Table 3. A key driver of the observed increase in costs was prescription drug costs. These drug costs increased by 37% from $3378 (95% CI: $3162, $3594) in 2008–2009 to $4618 (95% CI: $4172, $5064) in 2018–2019 among all individuals with ASCVD (Fig. 1C and Supplementary Table 4). The increase in prescription drug costs over the study period was more pronounced among individuals with ASCVD and diabetes, in whom a 45% increase in costs was observed—from $5184 (95% CI: $4721, $5646) in 2008–2009 to $7501 (95% CI: $6678, $8325) in 2018–2019 (Fig. 1C and Supplementary Table 4).
Adjusted costs among ASCVD individuals with and without diabetes
Accounting for demographics, socio-economic factors, the effect of time and comorbidities (Table 2), the adjusted mean annual overall incremental cost related to the presence of diabetes among individuals with ASCVD was estimated to be $5563 (95% CI: $4643, $6483) based on the regression-based approach. The corresponding costs for medical care and prescription drugs were $3071 (95% CI: $2278, $3865) and $2493 (95% CI: $2238, $2748), respectively (Table 2). Prescription drug costs were responsible for almost 45% of the incremental overall cost of diabetes among these patients with ASCVD (Table 2).
Economic burden of diabetes and ASCVD in the US
We extrapolated the individual costs estimates, to the entire US population, as shown in Supplementary Table 5. Based on the unadjusted mean, the annual aggregate cost during the 2008–2019 period among adults with ASCVD was estimated at $394 billion for the entire US population. These are unadjusted costs and represent all-cause costs among ASCVD patients. At the population level, the adjusted total incremental cost due to diabetes among individuals with ASCVD was $42 billion per year, when comparing individuals with diabetes to those without diabetes.
Discussion
We demonstrated that direct health care expenditures among adults with ASCVD with and without diabetes increased from 2008–2009 through 2018–2019 (by ~ 30%). Individuals with diabetes and ASCVD had ~ 1.5 times higher total direct health care expenditures compared with those without diabetes during the 2008–2019-time frame. These trends may reflect a number of factors including a longer survival of individuals with ASCVD and a better management over time with an implementation of quality of care standards, which include drug prescription. Indeed, the temporal trends for increased total medical expenditures was driven largely by prescription drugs, with a relatively modest contribution for other types of expenditures. An important proportion of cardioprotective drugs are now prescribed among those with ASCVD, especially among those with diabetes. Indeed, important diabetes medications with cardioprotective effects include GLP-1RAs and SGLT2 inhibitors. Moreover, the prevalence of diabetes increased over the study period [21], which may partially explain the increase in the costs in those with comorbid diabetes. During the study period there was also a surge in the number of diabetes medications with an effect on the cardiovascular system. In our regression models, other comorbidities did not influence the ASCVD related costs to the same extent as diabetes.
Our study provides important insights into factors associated with ASCVD expenditures, thus has important implications for providing value-driven care to ASCVD patients. The observed trends can be used to evaluate the effectiveness of the CVD control and prevention programs, and point to the potential needs for a shift in the delivery of care to a more comprehensive approach to the management of ASCVD that includes concomitant management of metabolic comorbidities. The disproportionately elevated costs of ASCVD especially in the setting of diabetes points to the need for community-based efforts aimed at preventing metabolic conditions, which might affect both the occurrence and progression of ASCVD. Such preventive efforts are highly needed given the projected increases in direct or indirect costs of CVD by 2030 [2].
Our study is unique as it comprehensively examines US national trends in expenditures related to ASCVD, over a substantially long period of time (more than a decade), including data on inpatient, outpatient, ER visits and prescription medication use, and also examining subgroups by diabetes status. To our knowledge, studies have seldom or not used national level data to examine the trend of the financial burden of ASCVD from the patients’ or payers’ perspective, including prescriptions and non-prescription drug costs, and accounting for the diabetes status. Our results are consistent with those of a prior study using claims data and examining the costs of care for ASCVD among patients with and without type 2 diabetes [5]. Other prior studies on the costs of ASCVD have tended to focus on either shorter periods of time (a few years), in-patient care/hospital costs only, or the use of lipid-lowering medications only [6,7,8,9,10]. Furthermore, the aforementioned prior studies have mainly predated the widespread use of novel cardioprotective medication such as the PCSK9 inhibitors, SGLT2 inhibitors and GLP-1 receptor agonists, which have costs that can potentially outweighs all the other ASCVD costs. Indeed, recent data indicates very high costs related to the use of SGLT2 inhibitors and GLP-1 receptor agonists among individuals with diabetes in particular [22], as well as for PCSK9 inhibitor therapy in the overall ASCVD population [23].
The strengths of our study include the examination of trends in costs over more than a decade using a nationally representative sample, including multiple cost categories (inpatient, outpatient, prescription medications, dental, ER, and home health expenditures) and the use of a robust cost estimation method to assess incremental costs (including those related to the presence of diabetes) accounting for a variety of comorbidities and thus evaluating the independent effect of diabetes. Furthermore, the 12-year study period allows us to account for the changing landscape in the management of diabetes and ASCVD; especially the introduction of new therapeutic modalities including entirely new medication classes and changes in guidelines for the management of diabetes.
Our study had some limitations. First, comorbidities were based on self-report, thus a potential for bias. However, self-report of several comorbidities have been shown to be reliable [24]. Second, our estimates may be lower than the actual ASCVD costs, as an important proportion of people in the community have subclinical or asymptomatic CVD and/or undetected diabetes (up to 25% of individuals with diabetes in the community are undiagnosed [21]), which can impact the costs. Third, institutionalized individuals were not included in MEPS, they tend to be sicker but with a lower survival, but with potentially higher expenditures. Fourth, the costs were derived using survey data, with the possible sampling error; thus, there is a residual uncertainty in our point estimates, which is difficult to quantify. Fifth, we did not investigate the indirect costs of lost productivity from morbidity or premature mortality; these costs can be substantial [25]. Our analysis did not also examine types of ASCVD; the relative contribution of each type (coronary artery disease, stroke or peripheral arterial disease) to costs could have changed over time, given the continuous refinement in to the diagnosis and management of diagnose ASCVD conditions. Finally, we also lacked information on the contribution of costs devices used for diabetes (such as continuous glucose monitors and pumps and costs related to lifestyle intervention such as nutritional interventions) or for ASCVD (e.g., device for adaptation at home after stroke) management.
Conclusion
This study provides insights into high burden of ASCVD-related costs in the United States over time, as well as the influence of diabetes on the high expenditures. Diabetes greatly contributes to the increase in ASCVD-related health costs in the U.S. population, indicating the potential savings from interventions to prevent and manage diabetes in those with ASCVD. Specifically, interventions directed towards preventing and managing metabolic factors, such as diabetes could have a significant impact on the trajectory of the overall ASCVD-related costs. Improved care access, systems of care, awareness on diet and physical activity, and reducing ASCVD risk factors such as diabetes are ways to minimize the substantial burden. The high costs of ASCVD related to the concomitant diabetes points to the need for a shift of care towards a more comprehensive approach including an integrated management of cardiometabolic disease.
Data availability
The database used is publicly available.
References
Martin SS, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. 2024 Heart disease and stroke statistics: a Report of US and Global data from the American Heart Association. Circulation United States. 2024;149:e347-913.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation United States. 2011;123:933–44.
Sarwar N, Gao P, Seshasai SRK, Gobin R, Kaptoge S, Di Angelantonio E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 19 million people. Lancet Diabetes Endocrinol. 2015;3:105–13.
Weng W, Tian Y, Kong SX, Ganguly R, Hersloev M, Brett J, et al. Impact of atherosclerotic cardiovascular disease on healthcare resource utilization and costs in patients with type 2 diabetes mellitus in a real-world setting. Clin Diabetes Endocrinol. 2020;6:5.
Sidelnikov E, Dornstauder E, Jacob C, Maas C, Pinto L, Leidl R, et al. Healthcare resource utilization and costs of cardiovascular events in patients with atherosclerotic cardiovascular disease in Germany—results of a claims database study. J Med Econ England. 2022;25:1199–206.
Nichols GA, Brown JB. The impact of cardiovascular disease on medical care costs in subjects with and without type 2 diabetes. Diabetes Care. 2002;25:482–6.
Power TP, Ke X, Zhao Z, Bonine NG, Cziraky MJ, Grabner M, et al. Clinical characteristics, patterns of lipid-lowering medication use, and health care resource utilization and costs among patients with atherosclerotic cardiovascular disease. Vasc Health Risk Manag. 2018;14:23–36.
Zhao Z, Zhu Y, Fang Y, Ye W, McCollam P. Healthcare resource utilization and costs in working-age patients with high-risk atherosclerotic cardiovascular disease: findings from a multi-employer claims database. J Med Econ. 2015;18:655–65.
Malone M, Lau NS, White J, Novak A, Xuan W, Iliopoulos J, et al. The effect of diabetes mellitus on costs and length of stay in patients with peripheral arterial disease undergoing vascular surgery. Eur J Vasc Endovasc Surg. 2014;48:447–51.
Cohen JW, Cohen SB, Banthin JS. The medical expenditure panel survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47:S44-50.
Agency for Healthcare Research and Quality (AHRQb). Medical Expenditure Panel Survey, 2011 Medical conditions 2013b. http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h146/h146doc.pdf. Accessed 20 Jun 2016.
U.S. Department of Health and Human Services. National Health Expenditure Accounts: Methodology Paper. 2019.
Coughlan D, Yeh ST, O’Neill C, Frick KD. Evaluating direct medical expenditures estimation methods of adults using the medical expenditure panel survey: an example focusing on head and neck cancer. Value Health. 2014;17:90–7.
Park RE. Estimation with heteroscedastic error terms. Econom. 1966;34:888.
Deb P, Norton EC. Modeling health care expenditures and use. Annu Rev Public Health United States. 2018;39:489–505.
Deb P, Norton EC, Manning WG. Health Econometrics Using Stata. Stata Pres. Stata Press. 2017. https://www.routledge.com/Health-Econometrics-Using-Stata/Deb-Norton-Manning/p/book/9781597182287
Belotti F, Deb P, Manning WG, Norton EC. twopm: two-part models. Stata J. 2015;15:3–20.
Bieler GS, Williams RL. Ratio estimates, the delta method, and quantal response tests for increased carcinogenicity. Biometrics. 1993;49:793–801.
Machlin S, Y W, Zodet M. Computing Standard Errors for MEPS Estimates. Agency Healthc. Res. Qual. Rockville, MD. Agency for Healthcare Research and Quality.
Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314:1021–9.
Luo J, Feldman R, Callaway Kim K, Rothenberger S, Korytkowski M, Hernandez I, et al. Evaluation of Out-of-Pocket Costs and Treatment Intensification With an SGLT2 Inhibitor or GLP-1 RA in Patients With Type 2 Diabetes and Cardiovascular Disease. JAMA Netw open United States. 2023;6:e2317886.
Navar AM, Taylor B, Mulder H, Fievitz E, Monda KL, Fievitz A, et al. Association of prior authorization and out-of-pocket costs with patient access to PCSK9 inhibitor therapy. JAMA Cardiol United States. 2017;2:1217–25.
Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–103.
Carter HE, Schofield D, Shrestha R. Productivity costs of cardiovascular disease mortality across disease types and socioeconomic groups. Open Heart. 2019;6:e000939.
Acknowledgements
None.
Funding
Dr Justin B. Echouffo-Tcheugui is funded by NIH/NHLBI grant K23 HL153774.
Author information
Authors and Affiliations
Contributions
Concept and design: Chintal Shah and Justin B. Echouffo Tcheugui. Acquisition, analysis, or interpretation of data: Chintal Shah, Gregg C. Fonarow and Justin B. Echouffo Tcheugui, Drafting of the manuscript: Chintal Shah and Justin B. Echouffo Tcheugui, Critical revision of the manuscript for important intellectual content: Chintal Shah, Gregg C. Fonarow and Justin B. Echouffo Tcheugui, Statistical analysis: Chintal Shah and Justin B. Echouffo Tcheugui Obtained funding: Justin B. Echouffo Tcheugui. Administrative, technical, or material support: Chintal Shah and Justin B. Echouffo Tcheugui. Supervision: Justin B. Echouffo Tcheugui and Gregg C. Fonarow.
Corresponding author
Ethics declarations
Competing interests
Dr Fonarow reports consulting for Abbott, Amgen, AstraZeneca, Bayer, Boehinger Ingelheim, Cytokinetics, Eli Lilly Janssen, Medtronic, Merck, Novartis, and Pfizer. Dr Shah now works for Takeda Pharmaceuticals. No other potential conflicts of interest relevant to this article were reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shah, C.H., Fonarow, G.C. & Echouffo-Tcheugui, J.B. Trends in direct health care costs among US adults with atherosclerotic cardiovascular disease with and without diabetes. Cardiovasc Diabetol 23, 238 (2024). https://doi.org/10.1186/s12933-024-02324-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02324-w