Abstract
Background
Ischemia and no obstructive coronary artery disease (INOCA) is increasingly recognized and associated with poor outcomes. The triglyceride-glucose (TyG) index is a reliable alternative measure of insulin resistance significantly linked to cardiovascular disease and adverse prognosis. We investigated the association between the TyG index and myocardial ischemia and the prognosis in INOCA patients.
Methods
INOCA patients who underwent both coronary angiography and myocardial perfusion imaging (MPI) were included consecutively. All participants were divided into three groups according to TyG tertiles (T1, T2, and T3). Abnormal MPI for myocardial ischemia in individual coronary territories was defined as summed stress score (SSS) ≥ 4 and summed difference score (SDS) ≥ 2. SSS refers to the sum of all defects in the stress images, and SDS is the difference of the sum of all defects between the rest images and stress images. All patients were followed up for major adverse cardiac events (MACE).
Results
Among 332 INOCA patients, 113 (34.0%) had abnormal MPI. Patients with higher TyG index had a higher rate of abnormal MPI (25.5% vs. 32.4% vs. 44.1%; p = 0.012). Multivariate logistic analysis showed that a high TyG index was significantly correlated with abnormal MPI in INOCA patients (OR, 1.901; 95% CI, 1.045–3.458; P = 0.035). During the median 35 months of follow-up, 83 (25%) MACE were recorded, and a higher incidence of MACE was observed in the T3 group (T3 vs. T2 vs. T1: 36.9% vs. 21.6% vs. 16.4%, respectively; p = 0.001). In multivariate Cox regression analysis, the T3 group was significantly associated with the risk of MACE compared to the T1 group (HR, 2.338; 95% CI 1.253–4.364, P = 0.008).
Conclusion
This study indicates for the first time that the TyG index is significantly associated with myocardial ischemia and poor prognosis among INOCA patients.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Symptoms and signs of myocardial ischemia have multifactorial factors, with obstructive coronary artery disease (CAD) being the predominant and widely recognized cause [1, 2]. However, approximately up to half of symptomatic patients are found to have non-obstructive CAD on invasive coronary angiography (CAG) [3, 4]. This chronic coronary syndrome, termed ischemia and no obstructive CAD (INOCA), is increasingly acknowledged as a significant contributor to major adverse cardiovascular events (MACE) [5, 6]. INOCA presents an intermediate prognosis when compared to obstructive CAD, with the highest risk of MACE [7]. However, it is important to note that the MACE risk of INOCA is higher than individuals with minimal or no atherosclerosis [5, 8, 9]. Furthermore, individuals with INOCA frequently encounter substantial physical restrictions, frequent hospitalizations for chest pain, and a diminished quality of life [10, 11]. However, they often lack appropriate medical management due to inadequate diagnosis and prognostic evaluation [12]. Multiple studies have demonstrated that coronary microvascular dysfunction (CMD), coronary vasospasm, or both are the main endotypes of INOCA and are related to MACE [5]. Unfortunately, few cardiac catheterization laboratories stock specialized coronary wires to evaluate CMD or conduct provocative vasospasm testing. Thus, it is crucial to explore widely applicable indicators for assessing myocardial ischemia and prognosis in patients with INOCA.
The triglyceride glucose (TyG) index, calculated from fasting blood glucose (FBG) and triglyceride (TG) levels, is regarded as an easily accessible surrogate marker for insulin resistance (IR) [13, 14]. It is practical to measure in primary care settings with laboratory capacity. As a synthetic parameter of FBG and TG in individuals, the TyG index has been shown to be associated with an increased risk of cardiovascular diseases (CVD), including atherosclerosis, CAD, and myocardial infarction (MI) [15,16,17,18]. Additionally, several studies have demonstrated the predictive role of the TyG index with regard to mortality and adverse cardiovascular outcomes [19,20,21]. While there is considerable heterogeneity in INOCA patients, there is evidence supporting an association between diabetes or chronic hyperglycemia and the onset of INOCA, which subsequently increases the risk of adverse prognosis [22,23,24]. However, it remains unclear whether the TyG index, as a potential cardiovascular event marker, is related to the occurrence of myocardial ischemia and adverse prognosis in INOCA patients.
Therefore, the primary objective of this study was to evaluate the correlation between the TyG index and myocardial ischemia based on myocardial perfusion imaging (MPI) in INOCA patients. Additionally, we sought to explore the potential impact of the TyG index in assessing the prognosis risk associated with INOCA, aiming to enhance the convenience and efficiency of managing these patients in clinical settings.
Methods
Study population
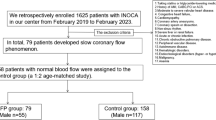
This retrospective observational study recruited all consecutive INOCA patients who underwent CAG and stress-rest MPI with D-SPECT within 3 months at Shanghai Tenth People’s Hospital from February 2017 to June 2019.
We included aged > 18 years old patients who were diagnosed with myocardial ischemia based on cardiovascular risk profiles, clinical ischemic symptoms and/or signs, and electrocardiogram (ECG) findings and whose coronary stenosis < 50% (including 0% stenosis) in all epicardial arteries and major branch arteries > 2.0 mm in diameter confirmed by CAG. The exclusion criteria included: (1) Obstructive CAD, that is, any naive coronary artery stenosis ≥ 50%; (2) History of percutaneous coronary interventions (PCI), coronary artery bypass graft (CABG), or MI; (3) hemodynamic instability; (4) heart failure; (5) severe heart disease requiring surgical operation; (6) serious concomitant hepatic or renal insufficiency; (7) malignancy or other severe medical illnesses with short, expected survival time;
Our study conformed to the Helsinki Declaration and was approved by the Ethics Committee of Shanghai Tenth People’s Hospital (ethical number: SHSY-IEC-5.0/23K112/P01). Informed consent was obtained from all participants.
Data collection and definitions
Cardiovascular risk factors, demographics, medical history, laboratory indices, electrocardiogram, echocardiography information, medication use, and the data of CAG were collected in detail from medical files. Blood samples for analyzing FBG, hemoglobin A1c (HbA1c), total cholesterol (TC), TG, low-density lipoprotein-C (LDL-C), high-density lipoprotein-cholesterol (HDL-C), serum creatinine, C-reactive protein (CRP) levels, cardiac troponin T (cTnT), creatine kinase-MB (CK-MB), myoglobin (MYO), N-terminal pro-brain natriuretic peptide (NT-proBNP) were obtained after fasting for more than 8 h.
DM was diagnosed when random plasma glucose ≥ 11.1 mmol/L, FBG ≥ 7.0 mmol/L, 2‑hour plasma glucose ≥ 11.1 mmol/L after OGTT, or HbA1c ≥ 6.5% [25]. The hypertension diagnosis was based on systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg at rest or on antihypertensive treatments. Body mass index (BMI) was computed as weight (kg) /height2 (m2).
The TyG index was calculated with the following equation: TyG index = Ln [fasting TG (mg/dL) × FBG (mg/dL)/2] [26]. INOCA Patients were divided into three groups (T1/T2/T3) based on their TyG index tertiles.
D-SPECT examination and analysis
Myocardial ischemia was evaluated by MPI, which was detected using the D-SPECT cardiac scanner (Spectrum Dynamics, Biosensors, Caesarea, Israel). Details of the detection and analysis of D-SPECT have been described previously [27]. All patients were given a single-day rest/stress imaging protocol with the use of 99mTc-sestamibi (99mTc-MIBI). Stress testing was performed by intravenous adenosine triphosphate (ATP) in our Department of Nuclear Medicine. After injection of 99mTc-MIBI (3 MBq/kg) for about 1 h, the rest image acquisition began, and the acquisition time was 6 min. At 30 min after the rest image acquisition, each patient was injected intravenously with ATP (140 µg/kg/min, for 6 min), followed by an injection of the 99mTc-MIBI (9 MBq/kg) 3 min later. After an interval of 30–45 min, the stress image was collected, and the collection time was 6 min. Finally, we reoriented the images into short-axis, horizontal, and vertical long-axis slices with QPS software (Cedars-Sinai Medical Center, LA, CA).
MPI images were independently analyzed using QPS software by two experienced nuclear cardiologists who were unaware of the patient’s characteristics and outcomes. The scores were calculated according to the 17-segment model and the five-point scale (“0, 1, 2, 3, 4” in turn stands for “normal, equivocal, moderate, severe, absence tracer uptake “) [28]. The summed rest score (SRS) was obtained by adding all defects in the rest images, and the summed stress score (SSS) was obtained by adding all defects in the stress images. The difference between SRS and SSS calculated the summed difference score (SDS). In addition, we calculated the stress total perfusion defect (TPD). Abnormal MPI for myocardial ischemia in individual coronary territories was defined as SSS ≥ 4 and SDS ≥ 2 [29, 30]. QPS software was also used to measure left ventricular functions such as end-diastolic volume (EDV), end-systolic volume (ESV), transient ischemic dilation (TID), peak ejection rate (PER), and peak filling rate (PFR).
Follow-up and endpoints
Follow-up data was collected by trained cardiologists through reviewing medical records, outpatient visits, and making phone calls. In our study, the median (interquartile range) follow-up duration was 35 (31–37) months. The clinical endpoint of our study was MACE, which was defined as cardiovascular death, nonfatal MI, heart failure, angina-related rehospitalization, nonfatal stroke, and ischemia-driven revascularization. Cardiovascular death was the death caused by MI, severe arrhythmia, heart failure, or other cardiovascular diseases. Nonfatal MI was defined if they had (1) positive cardiac biomarkers and (2) either typical symptoms of ischemia and/or dynamic ECG changes [31]. Heart failure was diagnosed following previous guidelines [32]. Angina-related rehospitalization refers to the chest pain or dynamic ECG changes associated with chest pain but normal cardiac biomarkers, and it is characterized by new onset angina, rest symptoms, or increasing severity or duration of the earlier stable angina symptoms. The diagnosis of nonfatal stroke was confirmed according to imaging examination and clinical symptoms or signs. Ischemia-driven revascularization was the coronary revascularization owing to a positive test for myocardial ischemia or clinical deterioration.
Statistical analysis
The statistical analysis of this study was performed using the Statistical Package for Social Sciences (SPSS) v.22. and GraphPad software 8.0.1. The mean ± standard deviation with a normal distribution and medians (interquartile range) with non-normal distribution were used for continuous variables. The t-test or ANOVA was used to compare continuous variables with a normal distribution between groups, and the Mann-Whitney U-test or Kruskal-Wallis test was used to analyze intergroup comparisons of continuous variables with a non-normal distribution. Categorical variables were presented as counts and percentages (%) and compared using Pearson’s chi-squared (χ2) or Fisher’s exact test. Logistic regression analysis evaluated the association between abnormal MPI and clinical risk factors in INOCA patients. The correlation between the TyG index and scores of myocardial perfusion was performed by Pearson or Spearman correlation analysis. The MACE-free survival rates were evaluated with Kaplan–Meier survival curves and compared using the log-rank test. Cox proportional regression analysis determined the relationship between the TyG index and clinical outcome in INOCA patients. The multivariate analysis included the univariate predictors with P < 0.10 in logistic regression and Cox proportional regression. We excluded the highly correlated variables when we performed multivariate regression analysis. All analysis was conducted two-sided, and the P-value < 0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 368 INOCA patients who underwent D-SPECT and CAG were included, in which 36 patients lost to follow-up or missed important data. Finally, 332 patients were enrolled in our study (Fig. 1).
Clinical characteristics of the INOCA patients stratified by the TyG index are shown in Table 1. The INOCA patients in the T3 group tended to have diabetes, dyslipidemia, lower HDL-C, LVEF, and higher BMI, TG, FBG, HbA1c, TC, LDL-C, and beta-blocker use.
Table 2 shows the D-SPECT data of INOCA patients stratified by TyG index. Of 332 INOCA patients, 113 (34.0%) had abnormal MPI. INOCA patients with higher TyG index had a higher rate of abnormal MPI (25.5% vs. 32.4% vs. 44.1%; p = 0.012). Compared to the lower TyG index groups, the T3 group had significantly higher SSS, SRS, stress TPD, and lower resting PFR. INOCA patients with abnormal MPI had higher TyG index than those with normal MPI [8.73 (8.37,9.25) vs. 8.54 (8.21,8.93); P = 0.001] (Fig. 2).
Association between TyG index and MPI in INOCA patients
Table 3 presents the association between clinical risk factors and abnormal MPI in INOCA patients. Univariable logistic regression analysis showed that females, high TyG index, TG, and low LVEF were significantly correlated with abnormal MPI in INOCA patients, and the T3 group had a 2.315-fold risk of abnormal MPI compared to the T1 group (OR, 2.315; 95% CI 1.309–4.091; P = 0.004). In the multivariate analysis, a high TyG index was still significantly associated with abnormal MPI in INOCA patients (OR, 1.901; 95% CI, 1.045–3.458; P = 0.035). In addition, gender also remained correlated with abnormal MPI. The correlation between the TyG index and scores of myocardial perfusions, such as SSS, SRS, SDS, and stress TPD, was examined. The results indicated that the TyG index correlated well with SSS, SRS, SDS, and stress TPD among INOCA patients (r = 0.168, r = 0.189, r = 0.135, and r = 0.167, respectively) (Fig. 3).
Outcome of INOCA patients according to the TyG index
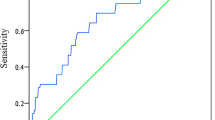
To explore the influence of the TyG index on the clinical outcome of INOCA patients, we compared the outcomes of patients with different TyG index levels. Over the follow-up period, 83 (25%) MACE were recorded among the INOCA patients, including 1 cardiovascular death, 2 nonfatal MI, 11 heart failure, 57 Angina-related rehospitalizations, 10 nonfatal stroke, and 2 ischemia-driven revascularizations. A higher incidence of MACE was observed in the INOCA patients with higher TyG index (T3 vs. T2 vs. T1: 36.9% vs. 21.6% vs. 16.4%, respectively; p = 0.001) (Table 4). In Fig. 4, Kaplan-Meier curves showed that the patients in the T3 group had the highest risk of MACE compared to those in the T1 and T2 groups (log-rank P = 0.002).
Association between TyG index and clinical outcomes in INOCA patients
The Cox regression analysis for MACE of INOCA patients is shown in Table 5. In the univariate Cox regression analysis, a high TyG index (T3 group) was significantly associated with the risk of MACE (HR, 2.478; 95% CI 1.424–4.314; P = 0.001). Gender, BMI, hypertension, serum creatinine, LVEF, and abnormal MPI were also the predictive factors of MACE. After adjusting for the univariate predictors with P < 0.10, the T3 group still had a 2.338-fold risk of MACE compared with the T1 group (adjusted HR, 2.338; 95% CI 1.253–4.364, P = 0.008), in addition, hypertension and abnormal MPI also remained associated with the risk of MACE.
Discussions
The main findings of our investigation were: (1) A notable association was observed between high TyG index and abnormal MPI in patients with INOCA. (2) The incidence of MACE was significantly elevated in the high TyG compared to the low TyG index. (3) The TyG index emerged as an independent prognostic factor linked to an unfavorable prognosis in INOCA patients. Our research findings highlight the prognostic relevance of the TyG index in predicting both myocardial ischemia and the occurrence of MACE in individuals with INOCA.
INOCA refers to individuals who manifest symptoms and signs indicative of myocardial ischemia but lack clear evidence of coronary artery obstruction [5]. Initially, INOCA was not deemed a pathologically significant condition; however, recent research has indicated that individuals with INOCA exhibit a comparable risk of MACE while experiencing a lower quality of life in comparison to patients with obstructive CAD [33, 34]. Furthermore, a meta-analysis encompassing patients diagnosed with INOCA revealed elevated rates of all-cause mortality and nonfatal myocardial infarction in comparison to the general population [35]. Consequently, the precise stratification of risk among patients with INOCA and the timely identification of associated risk factors are paramount in clinical settings.
As of now, there is compelling evidence highlighting a close association between abnormal myocardial perfusion and the prognosis of individuals diagnosed with INOCA [24, 27]. Many studies have explored the significance of radionuclide myocardial perfusion imaging in assessing the risk of patients with INOCA. Our previous investigation demonstrated that INOCA patients exhibiting perfusion defects indicative of abnormal MPI correlate with an unfavorable prognosis [27]. Similarly, Zampella et al. observed that abnormal MPI effectively identifies INOCA patients at a heightened risk of cardiac events [36].
Traditional risk factors such as diabetes mellitus, hypertension, age, and smoking may all be associated with INOCA and CMD [3, 5]. In particular, individuals with diabetes are more susceptible to endothelial dysfunction, inflammation, and oxidative stress, which are significant pathophysiological drivers involved in INOCA [37]. Studies have demonstrated reduced myocardial flow reserve and worse microvascular dysfunction in diabetic patients [22, 38, 39]. Equally important, diabetes or hyperglycemia have been shown to predict worse outcomes in INOCA patients, including increased all-cause mortality [24, 40, 41]. However, some studies have indicated that diabetes is not commonly found among INOCA patients, and some patients without traditional risk factors may still develop INOCA and CMD [42]. This highlights the importance of identifying novel risk factors for INOCA in the general population prior to the onset of diabetes.
IR often manifests before the presence of traditional risk factors, and IR serves as a crucial intermediate process of metabolic disorders, diabetes mellitus, and coronary artery disease [43, 44]. It represents a central aspect of disruptions in blood glucose homeostasis and has been substantiated as a robust risk factor for CVD [45, 46]. Beyond its role in the onset of CVD, IR significantly influences the prognostication of individuals with these conditions [45, 47, 48]. Consequently, the detection of IR holds crucial clinical significance in stratifying the risk of CVD.
Currently, there are few methods for detecting IR. The euglycemic insulin clamp and intravenous glucose tolerance testing is accurate but expensive and invasive. As for the homeostasis model assessment-estimated insulin resistance (HOMA-IR) index, there is very little value in patients treated with insulin or those without functioning beta cells, although it’s currently widely used [49]. Notably, the TyG index, an emerging marker of IR, has recently been advocated as a convenient and reliable substitute for assessing IR [50, 51]. Compared with traditional methods for detecting IR, the TyG index is a convenient, low-cost, and reliable surrogate, regardless of insulin treatment [49, 52]. Moreover, the TyG index has garnered attention recently due to its potential prognostic significance across various CVDs [49, 53]. Liu et al. observed that an elevated TyG index was potentially linked to a heightened incidence of CAD and MI in the general population [21]. Numerous studies have also identified a positive correlation between the TyG index and the severity of CAD. This finding suggests a potential association between TyG and the severity of the disease and the presence of ischemic symptoms [54, 55]. Nevertheless, the association between the TyG index and myocardial ischemia in individuals with INOCA remains unclear. In the current investigation, we observed that individuals with INOCA who belonged to the higher TyG index group (T3) demonstrated a heightened occurrence of abnormal MPI. Furthermore, the highest TyG index was significantly associated with an increased risk of abnormal MPI in INOCA patients. Additionally, we identified a significant correlation between the TyG index and ischemic parameters, including SSS, SRS, SDS, and TPD, in individuals diagnosed with INOCA, suggesting that the TyG index may possess predictive value for potential myocardial ischemia in individuals with INOCA. Prior investigations have suggested that IR may compromise vascular endothelial function [56, 57], potentially contributing to cardiac microcirculatory dysfunction and ultimately culminating in myocardial ischemia. An alternate explanation posits that IR could restrict glucose bioavailability, instigating alterations in fatty acid metabolism. This, in turn, may elevate myocardial oxygen consumption and diminish myocardial compensatory capacity, thereby precipitating myocardial ischemia [58]. Our findings may align with prior research, indicating a possible correlation between the TyG index and myocardial ischemia in individuals with INOCA. The heightened occurrence of abnormal MPI in the higher TyG index group, coupled with significant associations with ischemic parameters, suggests that the TyG index may serve as a predictive marker for potential myocardial ischemia in individuals with INOCA.
The TyG index has demonstrated independent predictive capabilities for cardiac events across diverse patient populations [17, 49, 54, 59,60,61]. A large retrospective study in China suggested that the TyG index could serve as a valuable marker for risk stratification and prognosis in patients with diabetes and acute coronary syndrome [19]. Additionally, findings from the ACROSS-China registration study indicated that a higher TyG index was correlated with an increased risk of stroke recurrence and mortality [62]. However, its specific association with prognosis in individuals diagnosed with INOCA has not been thoroughly elucidated. During the follow-up period, 83 MACEs were recorded in our study. Notably, a higher incidence of MACE was observed in the high TyG group compared to the low TyG group. In the present study, our data was consistent with previous relevant research, which indicated that a higher TyG index is independently associated with an increased incidence of atherosclerotic cardiovascular diseases, CAD, and stroke in the general population [17, 21]. In the adjusted Cox regression analysis, the high TyG group exhibited a substantial association with an increased risk of MACE. The specific mechanisms underlying the association between the TyG index and adverse events in individuals with INOCA remain uncertain. The observed heightened abnormal and significant correlation between the TyG index and ischemic parameters in individuals with INOCA, especially in the higher TyG index group (T3), suggests a potential link between IR and adverse cardiovascular outcomes. IR, reflected by the TyG index, may contribute to microvascular dysfunction, leading to a higher prevalence of abnormal MPI and an increased risk of MACE in INOCA patients. Further studies are warranted to validate these findings and explore the potential link between the TyG index and adverse outcomes in individuals with INOCA.
This study found that the TyG index was closely related to myocardial ischemia and adverse prognosis in INOCA patients. The elevated TyG index was related to myocardial ischemia and an independent predictor of MACE in patients with INCOA. This suggests that the TyG index has broad clinical application prospects in INOCA patients, and the TyG index can be used to stratify the risk of INOCA patients, identify high-risk patients, and provide targeted treatment to improve the clinical outcome of patients. In addition, since the TyG index is an indicator to evaluate IR, whether the treatment for IR can improve the prognosis of INOCA patients is worthy of further exploration.
Strengths and limitations
The strength of our research lies in its clear demonstration of the prognostic value of the TyG index in individuals with INOCA. By establishing a robust association between the TyG index and both myocardial ischemia and the incidence of MACE, our findings provide a concise and clinically relevant insight into the predictive capabilities of TyG in this specific population. This succinct yet impactful observation has the potential to inform healthcare practices, assisting clinicians in risk assessment and timely interventions for individuals with INOCA, ultimately enhancing patient care and outcomes. Nevertheless, it is essential to acknowledge several limitations in our study. First, being a retrospective and observational analysis of INOCA patients selected for MPI using a D-SPECT camera and CAG, inherent biases associated with such study designs need consideration. Second, being a single-center clinical study, its generalizability to other institutions and different camera designs, such as CZT and conventional camera designs, may be limited. Third, the study’s participants were exclusively Chinese INOCA patients, limiting the direct generalizability of the results to INOCA patients of other races. Despite these limitations, our study suggests that the TyG index might serve as a promising method for risk stratification and prognosis prediction in patients with INOCA, though confirmation through large-sample, prospective, multicenter studies are warranted.
Conclusion
In conclusion, this study presents the inaugural evidence of a significant association between the TyG index and myocardial ischemia in individuals with INOCA. Furthermore, our findings propose that the TyG index has the potential to serve as a valuable predictor for MACE among INOCA patients. These results imply that the TyG index holds promise as a useful indicator for risk stratification in individuals with INOCA.
Data availability
The data analyzed in this study can be obtained from the corresponding author with a reasonable request.
Abbreviations
- INOCA:
-
ischemia and no obstructive coronary artery disease
- TyG index:
-
triglyceride-glucose index
- MPI:
-
myocardial perfusion imaging
- CAD:
-
coronary artery disease
- CAG:
-
coronary angiography
- MACE:
-
major adverse cardiac events
- CMD:
-
coronary microvascular dysfunction
- FBG:
-
fasting blood glucose
- TG:
-
triglycerides
- IR:
-
insulin resistance
- CVD:
-
cardiovascular disease
- CKD:
-
chronic kidney disease
- COPD:
-
chronic obstructive pulmonary disease
- MI:
-
myocardial infarction
- ECG:
-
electrocardiogram
- PCI:
-
percutaneous coronary intervention
- CABG:
-
coronary artery bypass graft
- LVEF:
-
left ventricular ejection fraction
- HbA1c:
-
hemoglobin A1c
- TC:
-
total cholesterol
- LDL:
-
low-density lipoprotein
- HDL:
-
high-density lipoprotein
- CRP:
-
C-reactive protein
- cTnT:
-
cardiac troponin T
- CK-MB:
-
creatine kinase-MB
- MYO:
-
myoglobin
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- BMI:
-
body mass index
- SRS:
-
summed rest score
- SSS:
-
summed stress score
- SDS:
-
summed difference score
- TPD:
-
total perfusion defect
- EDV:
-
end-diastolic volume
- ESV:
-
end-systolic volume
- TID:
-
transient ischemic dilation
- PER:
-
peak ejection rate
- PFR:
-
peak filling rate
References
Virani SS, Newby LK, Arnold SV, Bittner V, Brewer LC, Demeter SH, AHA/ACC/ACCP/ASPC et al. /NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2023. 148(9): e9-e119.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77.
Beltrame JF, Tavella R, Jones D, Zeitz C. Management of ischaemia with non-obstructive coronary arteries (INOCA). BMJ. 2021;375:e060602.
Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886–95.
Kunadian V, Chieffo A, Camici PG, Berry C, Escaned J, Maas A, et al. An EAPCI Expert Consensus Document on Ischaemia with non-obstructive coronary arteries in collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41(37):3504–20.
Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and no obstructive coronary artery Disease (INOCA): developing evidence-based therapies and Research Agenda for the Next Decade. Circulation. 2017;135(11):1075–92.
Jespersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33(6):734–44.
Mehta PK, Johnson BD, Kenkre TS, Eteiba W, Sharaf B, Pepine CJ et al. Sudden Cardiac Death in Women With Suspected Ischemic Heart Disease, Preserved Ejection Fraction, and No Obstructive Coronary Artery Disease: A Report From the Women’s Ischemia Syndrome Evaluation Study. J Am Heart Assoc. 2017. 6(8).
van Rosendael AR, Bax AM, Smit JM, van den Hoogen IJ, Ma X, Al’Aref S, et al. Clinical risk factors and atherosclerotic plaque extent to define risk for major events in patients without obstructive coronary artery disease: the long-term coronary computed tomography angiography CONFIRM registry. Eur Heart J Cardiovasc Imaging. 2020;21(5):479–88.
Schumann CL, Mathew RC, Dean JL, Yang Y, Balfour PC Jr., Shaw PW, et al. Functional and economic impact of INOCA and Influence of Coronary Microvascular Dysfunction. JACC Cardiovasc Imaging. 2021;14(7):1369–79.
Gulati M, Khan N, George M, Berry C, Chieffo A, Camici PG, et al. Ischemia with no obstructive coronary artery disease (INOCA): a patient self-report quality of life survey from INOCA international. Int J Cardiol. 2023;371:28–39.
Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC State-of-the-art review. J Am Coll Cardiol. 2018;72(21):2625–41.
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347–51.
Khan SH, Sobia F, Niazi NK, Manzoor SM, Fazal N, Ahmad F. Metabolic clustering of risk factors: evaluation of triglyceride-glucose index (TyG index) for evaluation of insulin resistance. Diabetol Metab Syndr. 2018;10:74.
Li J, Dong Z, Wu H, Liu Y, Chen Y, Li S, et al. The triglyceride-glucose index is associated with atherosclerosis in patients with symptomatic coronary artery disease, regardless of diabetes mellitus and hyperlipidaemia. Cardiovasc Diabetol. 2023;22(1):224.
da Silva A, Caldas APS, Hermsdorff HHM, Bersch-Ferreira ÂC, Torreglosa CR, Weber B, et al. Triglyceride-glucose index is associated with symptomatic coronary artery disease in patients in secondary care. Cardiovasc Diabetol. 2019;18(1):89.
Ding X, Wang X, Wu J, Zhang M, Cui M. Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: a meta-analysis of cohort studies. Cardiovasc Diabetol. 2021;20(1):76.
Mirjalili SR, Soltani S, Heidari Meybodi Z, Marques-Vidal P, Kraemer A, Sarebanhassanabadi M. An innovative model for predicting coronary heart disease using triglyceride-glucose index: a machine learning-based cohort study. Cardiovasc Diabetol. 2023;22(1):200.
Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. 2020;19(1):80.
Lopez-Jaramillo P, Gomez-Arbelaez D, Martinez-Bello D, Abat MEM, Alhabib KF, Avezum Á, et al. Association of the triglyceride glucose index as a measure of insulin resistance with mortality and cardiovascular disease in populations from five continents (PURE study): a prospective cohort study. Lancet Healthy Longev. 2023;4(1):e23–33.
Liu X, Tan Z, Huang Y, Zhao H, Liu M, Yu P, et al. Relationship between the triglyceride-glucose index and risk of cardiovascular diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;21(1):124.
Sara JD, Taher R, Kolluri N, Vella A, Lerman LO, Lerman A. Coronary microvascular dysfunction is associated with poor glycemic control amongst female diabetics with chest pain and non-obstructive coronary artery disease. Cardiovasc Diabetol. 2019;18(1):22.
Zhang W, Singh S, Liu L, Mohammed AQ, Yin G, Xu S, et al. Prognostic value of coronary microvascular dysfunction assessed by coronary angiography-derived index of microcirculatory resistance in diabetic patients with chronic coronary syndrome. Cardiovasc Diabetol. 2022;21(1):222.
Mone P, Lombardi A, Salemme L, Cioppa A, Popusoi G, Varzideh F, et al. Stress hyperglycemia drives the risk of hospitalization for chest Pain in patients with ischemia and nonobstructive coronary arteries (INOCA). Diabetes Care. 2023;46(2):450–4.
Petersmann A, Müller-Wieland D, Müller UA, Landgraf R, Nauck M, Freckmann G, et al. Definition, classification and diagnosis of diabetes Mellitus. Exp Clin Endocrinol Diabetes. 2019;127:01.
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13:146.
Liu L, Abdu FA, Yin G, Xu B, Mohammed AQ, Xu S, et al. Prognostic value of myocardial perfusion imaging with D-SPECT camera in patients with ischemia and no obstructive coronary artery disease (INOCA). J Nucl Cardiol. 2021;28(6):3025–37.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne H. J. ASNC imaging guidelines for SPECT nuclear cardiology procedures: stress, protocols, and tracers. J Nucl Cardiol. 2016;23(3):606–39.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97(6):535–43.
Sharir T, Germano G, Kang X, Lewin HC, Miranda R, Cohen I, et al. Prediction of myocardial infarction versus cardiac death by gated myocardial perfusion SPECT: risk stratification by the amount of stress-induced ischemia and the poststress ejection fraction. J Nucl Med. 2001;42(6):831–7.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–64.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Mehta PK, Huang J, Levit RD, Malas W, Waheed N. And Bairey Merz C. N. Ischemia and no obstructive coronary arteries (INOCA): a narrative review. Atherosclerosis. 2022;363:8–21.
Li L, Pang Z, Wang J, Chen Y, Chu H, He Z et al. Prognostic value of myocardial flow reserve measured with CZT cardiac-dedicated SPECT low-dose dynamic myocardial perfusion imaging in patients with INOCA. J Nucl Cardiol. 2023.
Radico F, Zimarino M, Fulgenzi F, Ricci F, Di Nicola M, Jespersen L, et al. Determinants of long-term clinical outcomes in patients with angina but without obstructive coronary artery disease: a systematic review and meta-analysis. Eur Heart J. 2018;39(23):2135–46.
Zampella E, Mannarino T, D’Antonio A, Assante R, Gaudieri V, Buongiorno P, et al. Prediction of outcome by (82)rb PET/CT in patients with ischemia and nonobstructive coronary arteries. J Nucl Cardiol. 2023;30(3):1110–7.
Konst RE, Guzik TJ, Kaski JC, Maas A, Elias-Smale SE. The pathogenic role of coronary microvascular dysfunction in the setting of other cardiac or systemic conditions. Cardiovasc Res. 2020;116(4):817–28.
Sørensen MH, Bojer AS, Pontoppidan JRN, Broadbent DA, Plein S, Madsen PL, et al. Reduced myocardial Perfusion Reserve in Type 2 diabetes is caused by increased perfusion at Rest and decreased maximal perfusion during stress. Diabetes Care. 2020;43(6):1285–92.
Li XM, Shi R, Shen MT, Yan WF, Jiang L, Min CY, et al. Subclinical left ventricular deformation and microvascular dysfunction in T2DM patients with and without peripheral neuropathy: assessed by 3.0 T cardiac magnetic resonance imaging. Cardiovasc Diabetol. 2023;22(1):256.
Cortigiani L, Rigo F, Gherardi S, Galderisi M, Bovenzi F, Sicari R. Prognostic meaning of coronary microvascular disease in type 2 diabetes mellitus: a transthoracic Doppler echocardiographic study. J Am Soc Echocardiogr. 2014;27(7):742–8.
Murthy VL, Naya M, Foster CR, Gaber M, Hainer J, Klein J, et al. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation. 2012;126(15):1858–68.
Sara JD, Widmer RJ, Matsuzawa Y, Lennon RJ, Lerman LO, Lerman A. Prevalence of coronary microvascular dysfunction among patients with chest Pain and Nonobstructive Coronary Artery Disease. JACC Cardiovasc Interv. 2015;8(11):1445–53.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C. Zuñiga F. A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
Tian X, Chen S, Xu Q, Xia X, Zhang Y, Wang P, et al. Magnitude and time course of insulin resistance accumulation with the risk of cardiovascular disease: an 11-years cohort study. Cardiovasc Diabetol. 2023;22(1):339.
Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10(5):293–302.
Mancusi C, de Simone G, Best LG, Wang W, Zhang Y, Roman MJ, et al. Myocardial mechano-energetic efficiency and insulin resistance in non-diabetic members of the strong heart study cohort. Cardiovasc Diabetol. 2019;18(1):56.
Uetani T, Amano T, Harada K, Kitagawa K, Kunimura A, Shimbo Y, et al. Impact of insulin resistance on post-procedural myocardial injury and clinical outcomes in patients who underwent elective coronary interventions with drug-eluting stents. JACC Cardiovasc Interv. 2012;5(11):1159–67.
da Silva AA, do, Carmo JM, Li X, Wang Z, Mouton AJ, Hall JE. Role of Hyperinsulinemia and Insulin Resistance in Hypertension: Metabolic Syndrome Revisited. Can J Cardiol. 2020. 36(5): 671–682.
Tao LC, Xu JN, Wang TT, Hua F, Li JJ. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. 2022;21(1):68.
Tahapary DL, Pratisthita LB, Fitri NA, Marcella C, Wafa S, Kurniawan F, et al. Challenges in the diagnosis of insulin resistance: focusing on the role of HOMA-IR and Tryglyceride/glucose index. Diabetes Metab Syndr. 2022;16(8):102581.
Hong S, Han K, Park CY. The insulin resistance by triglyceride glucose index and risk for dementia: population-based study. Alzheimers Res Ther. 2021;13(1):9.
Placzkowska S, Pawlik-Sobecka L, Kokot I, Piwowar A. Indirect insulin resistance detection: current clinical trends and laboratory limitations. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2019;163(3):187–99.
Alizargar J, Bai CH, Hsieh NC, Wu SV. Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients. Cardiovasc Diabetol. 2020;19(1):8.
Wang X, Xu W, Song Q, Zhao Z, Meng X, Xia C, et al. Association between the triglyceride-glucose index and severity of coronary artery disease. Cardiovasc Diabetol. 2022;21(1):168.
Zhao J, Fan H, Wang T, Yu B, Mao S, Wang X, et al. TyG index is positively associated with risk of CHD and coronary atherosclerosis severity among NAFLD patients. Cardiovasc Diabetol. 2022;21(1):123.
Jia G, DeMarco VG, Sowers JR. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat Rev Endocrinol. 2016;12(3):144–53.
Molina MN, Ferder L. and, Manucha W. Emerging role of nitric oxide and heat shock proteins in insulin resistance. Curr Hypertens Rep. 2016;18(1):1.
Riehle C, Abel ED. Insulin signaling and heart failure. Circ Res. 2016;118(7):1151–69.
Su WY, Chen SC, Huang YT, Huang JC, Wu PY, Hsu WH et al. Comparison of the Effects of Fasting Glucose, Hemoglobin A(1c), and Triglyceride-Glucose Index on Cardiovascular Events in Type 2 Diabetes Mellitus. Nutrients. 2019. 11(11).
Xu L, Wu M, Chen S, Yang Y, Wang Y, Wu S, et al. Triglyceride-glucose index associates with incident heart failure: a cohort study. Diabetes Metab. 2022;48(6):101365.
Huang R, Wang Z, Chen J, Bao X, Xu N, Guo S, et al. Prognostic value of triglyceride glucose (TyG) index in patients with acute decompensated heart failure. Cardiovasc Diabetol. 2022;21(1):88.
Yang X, Wang G, Jing J, Wang A, Zhang X, Jia Q, et al. Association of triglyceride-glucose index and stroke recurrence among nondiabetic patients with acute ischemic stroke. BMC Neurol. 2022;22(1):79.
Acknowledgements
We are indebted to all members who contributed to this work.
Funding
This work was supported by in part by Chinese National Natural Science Foundation (82170521), Shanghai Natural Science Foundation of China (21ZR1449500), Foundation of Shanghai Municipal Health Commission (202140263), Tibet Natural Science Foundation of China (XZ2022ZR-ZY27(Z), XZ202301ZR0032G), Foundation of Chongming (CKY2021-21, CKY2020-29), Clinical Research Plan of Shanghai Tenth People’s Hospital (YNCR2A001), Clinical Research Plan of SHDC (SHDC2020CR4065), and Foundation of the Science and Technology Commission of Shanghai Municipality (Grant No.20dz1207200).
Author information
Authors and Affiliations
Contributions
W.Z., L.L., F.A., G.Y., and W.C. designed the study. L.X., X.L., J.G., and C.W. collected the data. T.S., A.M., R.M., and A.M. were involved in data cleaning, follow-up, and verification. F.A., F.Y., and W.C. drafted the manuscript and revised it critically for important intellectual content. W.C. and F.A. approved the final version of the manuscript. All authors contributed to manuscript revision, read, and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Our study was carried out in accordance with the Helsinki Declaration and was approved by the ethical review board of Shanghai Tenth People’s Hospital. Each participating patient in this study recruited written informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, W., Liu, L., Yin, G. et al. Triglyceride-glucose index is associated with myocardial ischemia and poor prognosis in patients with ischemia and no obstructive coronary artery disease. Cardiovasc Diabetol 23, 187 (2024). https://doi.org/10.1186/s12933-024-02230-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02230-1