Abstract
Background
This study aimed to investigate the risks of all-cause and cardiovascular mortality associated with blood pressure (BP) levels of 130–139/80–89 mmHg in Chinese adults with different glucose metabolism, during a long-term follow-up of over 20 years.
Methods
A prospective population-based cohort of 2,132 adults in Shanghai was established in 2002 and followed for 21 years. The association between BP categories and mortality was assessed, and the risk was further analyzed using multiple Cox regression analysis by combining BP and blood glucose categories.
Results
The final analysis included 2,004 participants, with 397 all-cause and 166 cardiovascular mortality. The incidence of all-cause and cardiovascular mortality per 1,000 person-years for different BP categories were as follows: BP < 130/80 mmHg (4.5 and 1.3), 130–139/80–89 mmHg (7.7 and 2.9), and ≥ 140/90 mmHg or treated groups (19.9 and 8.7), respectively. After adjusting for age, sex, and other factors, BP ≥ 140/90 mmHg was significantly associated with a higher risk of mortality across different blood glucose categories. However, using BP < 130/80 mmHg and normoglycemia as the reference, a BP of 130–139/80–89 mmHg was significantly associated with higher risks of all-cause (hazard ratio 3.30 [95% confidence interval 1.48–7.38], P < 0.01) and cardiovascular mortality (9.60 [1.93–47.7], P < 0.01) in diabetes, but not in those with normoglycemia or prediabetes.
Conclusions
BP of 130–139/80–89 mmHg may lead to a significantly higher risk of all-cause and cardiovascular mortality in Chinese adults with diabetes, but not in those with normoglycemia or prediabetes. This suggests that the targeted BP for people with diabetes should be < 130–139/80–89 mmHg.
Similar content being viewed by others
Background
Observational studies have consistently demonstrated a strong correlation between elevated blood pressure (BP) and the development of cardiovascular disease (CVD) [1, 2]. These studies have provided valuable insights into the relationship between BP and CVD risk, highlighting the importance of maintaining optimal BP levels for long-term cardiovascular health. A comprehensive meta-analysis of 61 prospective studies further supports these findings by revealing a clear dose-response relationship between BP levels and CVD risk [1]. The analysis showed that individuals with systolic blood pressure (SBP) levels below 115 mmHg and diastolic blood pressure (DBP) levels below 75 mmHg had the lowest risk of CVD. As BP levels increased beyond these thresholds, the risk of developing CVD increased logarithmically.
In recent years, several hypertension guidelines have been released, [3,4,5,6] and there is growing concern about blood pressure levels of 130–139/80–89 mmHg. According to the 2017 AHA/ACC guidelines, [3] this range is classified as stage 1 hypertension and requires therapy initiation if accompanied by clinical atherosclerotic cardiovascular disease or an estimated 10-year CVD risk of ≥ 10%. However, the 2018 Chinese hypertension guidelines, [4] 2020 ISH guidelines, [5] and 2023 European guidelines [6] consider 130–139/80–89 mmHg as “prehypertension” or “high normal” or an overlap between the two. Nevertheless, the recent guidelines all recommend a target blood pressure of 130/80 mmHg for hypertensive patients, either alone or in combination with other cardiovascular risk factors [6, 7].
Hypertension often coexists with other cardiovascular risk factors, such as impaired glucose metabolism. There is a higher prevalence of hypertension among individuals with type 2 diabetes (T2D), and vice versa, which increases the risk of CVD events [8]. Accumulated evidence strongly suggests that reducing BP in individuals with T2D can have a substantial positive impact on cardiovascular outcomes [9, 10]. Guidelines from organizations such as ACC/AHA,[3] AACE/ACE,[11] ESC/EASD,[12] and ADA [13] recommend a BP target of < 130/80 mmHg for patients with T2D. The ESC/EASD guidelines also provide recommendations for managing BP in individuals with diabetes and prediabetes [12]. However, there are still some studies with varying conclusions regarding BP targets for diabetes and prediabetes. Recent meta-analyses demonstrated that a BP target range of > 130/80 to < 140/90 mmHg may be optimal for patients ≥ 65 years with T2D, but specific targets may need to be individualized based on patients’ unique circumstances [14]. Reducing diastolic BP, particularly below 60 mmHg, is associated with increased risk of all-cause mortality [15]. Moreover, at early stage of diabetes, a slightly elevated systolic BP (140–150 mmHg) is transiently associated with better beta-cell function in T2D patients with HbA1c ≥ 10% but not in those with HbA1c < 10% [16]. This is a significant gap in our understanding, considering the increasing prevalence of prediabetes and its potential implications for both clinical management and public health.
In our previous study, we investigated the risk of CVD events in Chinese adults with a BP range of 130–139/80–89 mmHg and varying glucose metabolism [17]. By conducting a follow-up study for over 20 years, we collected data on vital status and cause of death, allowing us to investigate the long-term associations between blood pressure levels of 130–139/80–89 mmHg and mortality from all causes and cardiovascular diseases among Chinese adults with different glucose metabolism. We hypothesize that the BP range of 130–139/80–89 mmHg in patients with diabetes may result in a significantly increased risk of mortality, similar to the risk observed for CVD events in our previous study.
Methods
Study design and participants
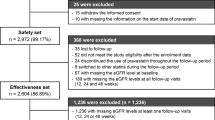
The prospective population-based cohort of 2,132 adults in Shanghai was established in 2002, and the study design had been described previously [17,18,19,20,21]. The first examination was conducted from November 2002 to January 2003. At baseline, all participants underwent physical examination and were interviewed with standardized questionnaires. Data were collected on physician diagnosed diabetes and hypertension, family history of diabetes, educational background, cigarette smoking, alcohol consumption, and currently used medications for hypertension and diabetes. An oral glucose tolerance test and serum lipid profile were assayed in all participants. Till now, 4 times follow-up were conducted in 2004, 2013–2014, 2018–2020, and 2022–2023, respectively. All participants at follow-up were interviewed with the same standardized questionnaires. At last, after excluding 128 participants lost to follow-up over four follow-up periods, a total of 2,004 participants were followed among 21 years’ follow-up, and were included in the final analysis, including 397 all-cause mortality and 166 cardiovascular mortality. Cardiovascular mortality included deaths attributable to stroke, myocardial infarction, and other cardiovascular diseases. Information on all-cause mortality and cardiovascular mortality were firstly obtained during this follow-up from the family members of the deceased people, and then were confirmed from the official death certificates of the district. This study was approved by Ruijin Hospital ethics committee and written informed consent was obtained from each participant.
Measurements and definition of variables
BP was measured three times using a mercury sphygmomanometer while the participant was in a sitting position after a 5-minute rest. SBP and DBP were determined as the average of the last two of the three measurements. BP categories were defined as follows: <130/80 mmHg, 130–139/80–89 mmHg, and ≥ 140/90 mmHg or treated. Plasma glucose levels were measured during a 75-g oral glucose tolerance test. Diabetes was defined by a fasting plasma glucose (FPG) level ≥ 7.0 mmol/L and/or a 2-hour post-challenge glucose (2hPG) level ≥ 11.1 mmol/L, a previous physician diagnosis of diabetes, or the use of antidiabetic medication at baseline. Prediabetes was defined as FPG between 5.6 and 7.0 mmol/L and/or 2hPG between 7.8 and 11.1 mmol/L [22]. Normoglycemia was defined by FPG < 5.6 mmol/L and 2hPG < 7.8 mmol/L. Triglycerides (TG), total serum cholesterol (TC), HDL, and LDL levels were measured enzymatically.
Anthropometric measurements were conducted by 20 trained nurses or clinical postgraduates. Smoking and alcohol consumption, educational background, diet, and physical activity were acquired through well designed questionnaires. Family history of diabetes was defined as at least one first-degree relative or grandparents with diabetes. Smoking and drinking status were classified as currently, formerly, and never consumed. Physical activity was calculated as the product of the duration and frequency of each activity (in hours per day) weighted by an estimate of the metabolic equivalent of that activity. Ten-year atherosclerotic CVD (ASCVD) risk was estimated using prediction equations validated by the Prediction for ASCVD Risk in China project, [23] which evolved from The Framingham Heart Study, but is more suitable for Chinese people. In the prediction equations, the following major risk factors are included: age, treated or untreated SBP, total cholesterol, HDL-C, current smoking, and diabetes mellitus. Additionally, for men, 4 additional variables—waist circumference, geographic region, urbanization, and family history of ASCVD—have been added to the equation. For women, 2 additional variables—waist circumference, and geographic region—have been included [23].
Statistical analysis
We used SAS 9.4 software for database management and statistical analysis. Data are expressed as mean ± SD, %, geometric mean with 95% limits, or hazard ratios (HRs) with 95% CIs. All statistical tests were two-sided, with P < 0.05 considered significant. Serum TG values were log-transformed before analysis because of skewed distribution. Multiple Cox regression analysis was performed to compute HRs (95% CIs). The log-rank test was used to compare the cumulative incidence of mortality between groups, with the Kaplan Meier survival function used to show the time to events. Proportionality assumptions for the Cox models were assessed by diagnostic plots of the scaled Schoenfeld residuals and log-minus-log survival plots. Substantial deviations from proportionality were not observed. We considered individuals with BP < 130/80 mmHg (or with normoglycemia, if considered) as the reference group. Dummy variables were used to compute HRs (95% CIs) for each subgroup against the reference group.
Results
Baseline characteristics
The median of follow-up time was 16.5 (interquartile range, 10.8 to 20.2) years. The mean values of anthropometric data and metabolic variables by BP category at baseline are presented in Table 1. Participants with a BP of 130–139/80–89 mmHg and ≥ 140/90 mmHg or treated were more likely to be male and to have more cigarette or alcohol consumption.
Compared with those with BP < 130/80 mmHg, age, FPG, 2hPG, LDL, TC, TG, BMI, waist circumference, and waist-to-hip ratio were higher among participants with BP 130–139/80–89 mmHg and the highest among participants with BP ≥ 140/90 mmHg or treated. Inverse relationship was observed between the prevalence of diabetes family history and BP categories. No significant difference was found in physical activity among these three groups. Moreover, we compared the baseline characteristics between participants who attended follow-up with those lost to follow-up and found no significant difference in glucose levels, blood lipid profile, BP, and any other factors between the two groups (data not shown).
Among the 1077 participants with hypertension at baseline, 379 (35.2%) were currently taking antihypertensive medications. Among the 309 participants with T2D, 181 (58.6%) were currently taking antidiabetic medications. Among those taking antidiabetic medications, 55.2% were using metformin (17% in combination with insulin, 37% in combination with sulfonylurea, and 10% in combination with glucosidase inhibitors), 23.3% were using insulin, 43.1% were using sulfonylurea, 21.5% were using glucosidase inhibitors, and 42.5% were using two or more drugs.
BP categories and all-cause and cardiovascular mortality
During a median follow-up of 16.5 years, there were 397 deaths from all causes and 166 deaths from cardiovascular causes among the 2,004 subjects, with a total of 29,395 person-years. The corresponding incidence of all-cause mortality per 1,000 person-years for the BP < 130/80 mmHg, 130–139/80–89 mmHg, and ≥ 140/90 mmHg or treated groups were 4.5, 7.7 and 19.9, respectively, and of cardiovascular mortality were 1.3, 2.9 and 8.7, respectively (Fig. 1).
Using BP < 130/80 mmHg as the reference, the group with BP 130–139/80–89 mmHg showed significantly higher risks of all-cause and cardiovascular mortality in the crude model, but not in the adjusted model. After adjusting for age, sex, BMI, and other factors, multiple Cox regression analysis showed that BP ≥ 140/90 mmHg or treated was significantly associated with higher risks of all-cause mortality (HR 2.45 [95%CI 1.65–3.63]) and cardiovascular mortality (3.40 [1.65-7.00]) (Table 2). Figure 2 shows the Kaplan-Meier survival curve for all-cause and cardiovascular mortality according to BP category at baseline. The cumulative survival rates for all-cause and cardiovascular mortality were significantly lower in participants with BP ≥ 140/90 mmHg or treated.
BP categories combined with blood glucose categories and all-cause and cardiovascular mortality
We assessed the risk for all-cause and cardiovascular mortality among participants stratified according to three BP categories (< 130/80 mmHg, 130–139/ 80–89 mmHg, and ≥ 140/90 mmHg or treated) and three blood glucose categories (normoglycemia, prediabetes, and diabetes) combined. Table 3 shows the adjusted HRs and 95% CIs for all-cause and cardiovascular mortality according to the various BP and blood glucose categories combined, using BP < 130/80 mmHg and normoglycemia as the reference. As expected, the coexistence of BP ≥ 140/90 mmHg or treated and diabetes were associated with the most significant increases in the all-cause mortality (HR 4.44 [95% CI 2.42–8.16]) and cardiovascular mortality (HR 11.8 [95% CI 2.86–48.7]). When compared with the reference group, BP of 130–139/80–89 mmHg combined with diabetes increased the all-cause mortality by 3.3 times and cardiovascular mortality by 9.6 times. BP ≥ 140/90 mmHg or treated and prediabetes in the same individual considerably increased the risk for all-cause mortality (adjusted HR 2.82 [1.54–5.16]) and cardiovascular mortality (adjusted 5.64 [1.36–23.4], respectively. However, BP of 130–139/80–89 mmHg combined with prediabetes was not associated with an elevated risk of all-cause and cardiovascular mortality in the crude and adjusted models. Figure 3 presents the effect of various categories of BP and glucose metabolism categories combined on the prevalence of all-cause and cardiovascular mortality among Chinese adults. Rates per 1,000 person-years were calculated in these nine groups.
Sensitivity analysis of the risks of all-cause and cardiovascular mortality for 130–139/80–89 mmHg
Sensitivity analysis was conducted to explore the impact of different baseline characteristics of the study population on the risk of all-cause and cardiovascular mortality for BP levels of 130–139/80–89 mmHg compared to BP levels below 130/80 mmHg. No significant differences in predictive values were observed across groups based on age, sex, BMI, smoking, drinking, and baseline 10-year ASCVD risk of ≥ 10% or not (Table 4).
Discussion
In this comprehensive study, we thoroughly investigated the potential risks of all-cause and cardiovascular mortality among a Chinese population-based cohort with a BP range of 130–139/80–89 mmHg. Our groundbreaking findings implied that individuals falling within this BP range face a notably higher risk of both all-cause and cardiovascular mortality when accompanied by a diagnosis of diabetes. Importantly, these risks persist over an extended follow-up period of more than 20 years, emphasizing the long-term implications of elevated BP levels in this specific population.
BP targets and CVD risk
BP of 130–139/80–89 mmHg has different definitions in various guidelines. These definitions are primarily based on the differing understanding of the long-term effects of BP in this range on outcomes, such as cardiovascular events and mortality. Several individual studies and meta-analyses of observational data have reported a progressively higher risk of CVD from < 120/80 to 130–139/80–89 mmHg [24,25,26]. In many of these meta-analyses, the hazard ratios for coronary heart disease and stroke ranged from 1.1 to 1.5 for BP of 120–129/80–84 mmHg, and from 1.5 to 2.0 for BP of 130–139/85–89 mmHg compared to < 120/80 mmHg. However, there is still controversy regarding the association of BP of 130–139/80–89 mmHg with all-cause mortality. A meta-analysis of prospective cohort studies showed that BP of 120–139/80–89 mmHg increased the risk of CVD by 55% and cardiovascular mortality by 17%, but not increase the risk of all-cause mortality [26]. Another pooled analysis of three prospective Chinese cohorts with a total follow-up of 1,718,089 person-years showed that BP of 130–139/80–89 mmHg increased the risk of cardiovascular mortality by 40%, but not of all-cause mortality (HR 1.04, 95% CI 0.89–1.21), compared to BP < 120/80 mm Hg [27]. In our study, we found that BP of 130–139/80–89 mmHg was not significantly with all-cause and cardiovascular mortality in Chinese adults, whether in crude models or when adjusted for age, sex, BMI, family history of diabetes, physical activity, and cigarette smoking and alcohol status. These finding are consistent with our previous finding on CVD events [17].
BP target in patients with diabetes
There has been extensive discussion over the past decade about individualized blood pressure targets for patients with diabetes and hypertension. In fact, hypertension and optimal blood pressure targets are more complex in patients with diabetes than in those with hypertension alone. Hypertension and impaired glucose metabolism have distinct genomic characteristics, emphasizing the need for studies on the impact of genomic features on pure and combined forms of the diseases [28]. In a meta-analysis of randomized controlled trials involving patients with diabetes or prediabetes, lowering systolic blood pressure to ≤ 135 mmHg was associated with a 10% reduction in all-cause mortality compared to lower intensity control, while more intensive blood pressure control (≤ 130 mmHg) was more strongly associated with a reduction in stroke risk but did not lower other events [29]. For years, guidelines have recommended keeping patients’ blood pressure controlled below 130/80 mm Hg [30, 31]. The basis for these guidelines is the UK Prospective Diabetes Study 3610, UK Prospective Diabetes Study [32], the Hypertension Optimal Treatment (HOT) trial [33], the Appropriate Blood Pressure Control in Diabetes (ABCD) trial [34], and the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) study [35]. However, after the publication of the Action to Control Cardiovascular Risk in Diabetes (ACCORD)-BP study [36], the treatment target for patients with diabetes was changed in 2013 to a blood pressure lower than 140/90 mm Hg, leading to updates in multiple hypertension guidelines [30, 31] Subsequent systematic reviews concluded that treating individuals with blood pressure already below 140 mm Hg is associated with a reduced risk of stroke and albuminuria [37], thus questioning the relaxation of guidelines. In an observational study conducted in Japan, it was found that a home SBP of at least 125 mmHg in the morning was an independent predictor of cardiovascular events in individuals with diabetes. It has been proposed that diabetic East Asians should aim for a home morning SBP below 125 mmHg [38]. The latest hypertension guidelines recommend controlling blood pressure targets below 130/80 mm Hg for patients with diabetes [6, 7].
To determine the optimal BP threshold among patients with diabetes and hypertension, it is crucial to consider its influence on long-term outcomes. In this study, which spanned 21 years and involved a population-based prospective cohort, we examined the incidence of all-cause and cardiovascular mortality among individuals with a BP of 130–139/80–89 mmHg and either diabetes or prediabetes. After assessing the association between BP categories and the risk of all-cause mortality and cardiovascular mortality, we further analyzed the risk of mortality by combining BP categories with blood glucose categories. As expected, we found that individuals with a BP ≥ 140/90 mmHg (or treated) and diabetes had the highest incidence of all-cause mortality (HR 4.51) and cardiovascular mortality (HR 12.0). Of note, individuals with a BP of 130–139/80–89 mmHg combined with diabetes had a 3.26 times higher risk of all-cause mortality and a 9.53 times higher risk of cardiovascular mortality. Interestingly, a BP of 130–139/80–89 mmHg combined with prediabetes did not show an increased risk of all-cause and cardiovascular mortality in both crude and adjusted models. To our knowledge, this study provides the first data on the occurrence of all-cause and cardiovascular mortality among Chinese adults with a BP of 130–139/80–89 mmHg and either diabetes or prediabetes in a population-based prospective cohort.
BP target in individuals with prediabetes
Prediabetes is an intermediate glycemic state between normal glycemia and diabetes, and it affects about half of the population in China. There is inconsistent association between prediabetes and CVD disease, as well as cardiovascular and all-cause mortality [39, 40]. The association between prediabetes and CVD risk may be affected by hypertension status. Two earlier studies conducted in China showed that individuals with prediabetes and hypertension had a higher risk of CVD events compared to those without prediabetes or hypertension [18, 41]. However, a recent study conducted on 3,313 black adults in the Jackson Heart Study (JHS) without diabetes or a history of CVD at baseline found that prediabetes was not associated with an increased risk of cardiovascular or all-cause mortality, regardless of hypertension status [42]. The present study shows that individuals with prediabetes combined with a BP of ≥ 140/90 mmHg or who are being treated for hypertension indeed have a higher risk of cardiovascular and all-cause mortality.
Strengths and limitations
Our study should be interpreted within the context of its strengths and limitations. One of the strengths of our study is a population-based prospective cohort with the extensive follow-up period of 21 years, allowing us to track outcomes over a long period of time. However, it is important to acknowledge the limitations of our analyses as well. Firstly, not all participants underwent a baseline HbA1c test in 2002, which may have resulted in some cases of diabetes being missed if they were only detected by HbA1c. This potential oversight could have affected the overall picture of diabetes prevalence in our study. Nevertheless, it is worth noting that the clinical diagnosis of both prediabetes and diabetes was primarily based on FPG and 2hPG levels. HbA1c was not included in the diagnostic criteria until 2010, so our findings are based on the established criteria at the time of the study. Secondly, our study used office BP measurements instead of 24-hour ambulatory BP monitoring. It has been shown that 24-h ambulatory systolic BP, but not office BP, is independently associated with cardiac remodeling, coronary microvascular dysfunction, and diastolic dysfunction among asymptomatic individuals with Diabetes Mellitus [43]. Thirdly, our study has a relatively small sample size and includes participants who are relatively young. Despite a follow-up period of over 20 years, the number of deaths in certain subgroups is still low. This limitation may result in the analysis lacking sufficient statistical power for these subgroups. Given the relatively small sample size in this study, we are unable to distinguish statistically whether the observed risk is primarily attributed to blood pressure or diabetes. However, we can observe the additive effect of both blood pressure and diabetes status. Forth, since serum creatinine and urinary albumin levels were not measured at baseline, it was not possible to evaluate the related information of chronic kidney disease in participants with a BP of 130–139/80–89 mmHg. Finally, it is important to note that this study is solely observational in nature. Therefore, further research in the form of randomized controlled clinical trials is needed to evaluate the potential benefits derived from antihypertensive treatment among this specific patient population.
Conclusions
In conclusion, our findings of this study suggest that individuals with diabetes and a BP of 130–139/80–89 mmHg may face a significantly higher risk of all-cause and cardiovascular mortality over an extended follow-up period of more than 20 years. This highlights the importance of maintaining a target BP level below 130/80 mmHg for individuals with diabetes.
Data Availability
All data generated or analyzed during this study are available in this published article.
References
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and Hypertension. Nat Rev Cardiol. 2021;18:785–802.
Whelton PK, Carey RM, Aronow WS et al. 2017 acc/aha/aapa/abc/acpm/ags/apha/ash/aspc/nma/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension. 2018;71:e13-e115.
Joint Committee for Guideline R. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of Chinese guidelines for prevention and treatment of Hypertension. J Geriatric Cardiology: JGC. 2019;16:182–241.
Unger T, Borghi C, Charchar F, et al. 2020 international society of Hypertension global Hypertension practice guidelines. J Hypertens. 2020;38:982–1004.
Mancia G, Kreutz R, Brunström M, et al. Authors/Task Force Members:. 2023 ESH guidelines for the management of arterial Hypertension the Task Force for the management of arterial Hypertension of the European Society of Hypertension Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41(12):1874–2071.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ ESH guidelines for the management of arterial Hypertension: the Task Force for the management of arterial Hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104.
Ferrannini E, Cushman WC. Diabetes and Hypertension: the bad companions. Lancet. 2012;380:601–10.
Stahl CH, Novak M, Lappas G, Wilhelmsen L, Bjorck L, Hansson PO, Rosengren A. High-normal blood pressure and long-term risk of type 2 Diabetes: 35-year prospective population based cohort study of men. BMC Cardiovasc Disord. 2012;12:89.
Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular Complications of type 2 Diabetes (ukpds 36): prospective observational study. BMJ. 2000;321:412–9.
Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American associ- ation of clinical endocrinologists and American College of Endo- crinologyeclinical practice guidelines for developing a Diabetes Mellitus comprehensive care plane2015. Endocr Pract. 2015;21(Suppl 1):1e87.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, ESC Scientific Document Group. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
Seidu S, Hambling CE, Kunutsor SK, Topsever P. Associations of blood pressure with cardiovascular and mortality outcomes in over 2 million older persons with or without Diabetes Mellitus: a systematic review and meta-analysis of 45 cohort studies. Prim Care Diabetes. 2023 Oct 6: S1751-9918(23)00166-3.
Siddiqi TJ, Usman MS, Siddiqui A, Salman A, Talbot N, Khan LA, Shabbir A, Hall ME, Taffet GE. Association of Low Diastolic Blood Pressure with Cardiovascular outcomes and all-cause mortality: a Meta-analysis. Curr Probl Cardiol. 2023 Oct;20:102131.
Xia Z, Song L, Fang D, You W, Li F, Zheng D, Li Y, Lin L, Dou J, Su X, Zhai Q, Zuo Y, Zhang Y, Gaisano HY, Jiang J, He Y. Higher systolic blood pressure is specifically associated with better islet beta-cell function in T2DM patients with high glycemic level. Cardiovasc Diabetol. 2022;21(1):283.
Tian J, Sheng CS, Sun W, et al. Effects of High Blood Pressure on Cardiovascular Disease events among Chinese adults with different glucose metabolism. Diabetes Care. 2018;41:1895–900.
Qiu M, Shen W, Song X, et al. Effects of prediabetes mellitus alone or plus Hypertension on subsequent occurrence of Cardiovascular Disease and Diabetes Mellitus: longitudinal study. Hypertension. 2015;65:525–30.
Tian J, Qiu M, Li Y, et al. Contribution of birth weight and adult waist circumference to Cardiovascular Disease risk in a longitudinal study. Sci Rep. 2017;7:9768.
Song X, Qiu M, Zhang X, et al. Gender-related affecting factors of prediabetes on its 10-year outcome. BMJ open Diabetes Research & care. 2016;4:e000169.
Tian JY, Cheng Q, Song XM, et al. Birth weight and risk of type 2 Diabetes, abdominal obesity and Hypertension among Chinese adults. Eur J Endocrinol. 2006;155:601–7.
American Diabetes Association. Diagnosis and classification of Diabetes Mellitus. Diabetes Care. 2010;33(Suppl 1):62–S69.
Yang X, Li J, Hu D, et al. Predicting the 10-year risks of atherosclerotic Cardiovascular Disease in Chinese population: the china-par project (prediction for ascvd risk in China). Circulation. 2016;134:1430–40.
Guo X, Zhang X, Guo L, et al. Association between pre-hypertension and cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Curr Hypertens Rep. 2013;15:703–16.
Huang Y, Wang S, Cai X, et al. Prehypertension and incidence of Cardiovascular Disease: a meta-analysis. BMC Med. 2013;11:177.
Wang S, Wu H, Zhang Q, Xu J, Fan Y. Impact of baseline prehypertension on cardiovascular events and all-cause mortality in the general population: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;168:4857–60.
Liu N, Yang JJ, Meng R, et al. Associations of blood pressure categories defined by 2017 acc/aha guidelines with mortality in China: pooled results from three prospective cohorts. Eur J Prev Cardiol. 2020;27:345–54.
Barragan JTC, Kubota LT. Nanostructured cupric oxide electrode: an alternative to amperometric detection of carbohydrates in anion-exchange chromatography. Anal Chim Acta. 2016;906:89–97.
Grenet G, Le H, Bejan-Angoulvant T, et al. Association between difference in blood pressure reduction and risk of cardiovascular events in a type 2 Diabetes population: a meta-regression analysis. Diabetes Metab. 2019;45:550–6.
Chobanian AV, Bakris GL, Black HR, Blood Institute Joint National Committee on Prevention DE, Treatment of High Blood P, National High Blood Pressure Education Program Coordinating C, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of High Blood Pressure: the jnc 7 report. JAMA. 2003;289:2560–72.
Mancia G, De Backer G, Dominiczak A, et al. 2007 guidelines for the management of arterial Hypertension: the task force for the management of arterial Hypertension of the European society of Hypertension (esh) and of the European society of cardiology (esc). Eur Heart J. 2007;28:1462–536.
Tight blood pressure control. And risk of macrovascular and microvascular Complications in type 2 Diabetes: Ukpds 38. Uk prospective Diabetes study group. BMJ. 1998;317:703–13.
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with Hypertension: principal results of the Hypertension optimal treatment (hot) randomised trial. Hot study group. Lancet. 1998;351:1755–62.
Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular Complications in patients with Hypertension and type 2 Diabetes. Diabetes Care. 2000;23(Suppl 2):B54–64.
Patel A, Group AC, MacMahon S, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 Diabetes Mellitus (the advance trial): a randomised controlled trial. Lancet. 2007;370:829–40.
Group AS, Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 Diabetes Mellitus. N Engl J Med. 2010;362:1575–85.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 Diabetes: a systematic review and meta-analysis. JAMA. 2015;313:603–15.
Eguchi K, Hoshide S, Kario K, J-HOP Study Group. Target home morning SBP be below 125 mmHg in type 2 Diabetes patients. J Hypertens. 2018;36(6):1284–90.
Ford ES, Zhao G, Li C. Pre-diabetes and the risk for Cardiovascular Disease: a systematic review of the evidence. J Am Coll Cardiol. 2010;55:1310–7.
Yeboah J, Bertoni AG, Herrington DM, Post WS, Burke GL. Impaired fasting glucose and the risk of incident Diabetes Mellitus and cardiovascular events in an adult population: Mesa (multi-ethnic study of Atherosclerosis). J Am Coll Cardiol. 2011;58:140–6.
Liu HH, Cao YX, Li S, et al. Impacts of prediabetes mellitus alone or plus Hypertension on the coronary severity and cardiovascular outcomes. Hypertension. 2018;71:1039–46.
Hubbard D, Colantonio LD, Tanner RM, et al. Prediabetes and risk for Cardiovascular Disease by Hypertension status in black adults: the jackson heart study. Diabetes Care. 2019;42:2322–9.
Yeo JL, Gulsin GS, Brady EM, Dattani A, Bilak JM, Marsh AM, Sian M, Athithan L, Parke KS, Wormleighton J, Graham-Brown MPM, Singh A, Arnold JR, Lawson C, Davies MJ, Xue H, Kellman P, McCann GP. Association of ambulatory blood pressure with coronary microvascular and cardiac dysfunction in asymptomatic type 2 Diabetes. Cardiovasc Diabetol. 2022;21(1):85.
Acknowledgements
The authors acknowledge all staff and volunteers from three hospital who attend this study.
Funding
This work was supported by the Chinese National Natural Science of Foundation (82270452, 82088102, 81770418, 81270935, 82370902 and 81400346), Shanghai Talent Development Fund (2021087), Ministry of Health (2016YFC1300103 and 2016YFC0905001), and the Foundation of National Infrastructures for Translational Medicine (Shanghai) (TMSK 2021 − 506).
Author information
Authors and Affiliations
Contributions
JT and GN contributed to the study design. CSS and JT contributed to the statistical analysis and interpretation of the results, as well as writing the manuscript. JT, CSS, YL, and HW were involved in data acquisition and research. HW, YL, YL, TH, MQ, SS, JY, and XS participated in project discussions. JT is the guarantor of this work and had full access to all the data in the study, taking responsibility for data integrity and accuracy of analysis.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by Ruijin Hospital ethics committee and written informed consent was obtained from each participant.
Consent for publication
Not applicable.
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sheng, CS., Wang, H., Liu, Y. et al. Long-term effects of blood pressure 130–139/80–89 mmHg on all-cause and cardiovascular mortality among Chinese adults with different glucose metabolism. Cardiovasc Diabetol 22, 353 (2023). https://doi.org/10.1186/s12933-023-02088-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-02088-9